Abstract
Coronary stent thrombosis is a life-threatening condition induced by multiple factors, including allergic reactions. A 64-year-old man presented with stent thrombosis in the left anterior descending artery and multiple cardiorespiratory arrests immediately after the first dose of the BNT162b1 mRNA vaccine. He underwent emergent percutaneous coronary intervention. Anaphylaxis-induced stent thrombosis, or type III Kounis syndrome, is a highly possible diagnosis. Cardiogenic shock can hide the skin manifestations of anaphylaxis, making this syndrome challenging to diagnose. This clinical case underscores the importance of surveillance for at least 30 minutes after vaccine administration, especially in patients at risk.
Keywords: Anaphylaxis, COVID-19, Kounis syndrome, myocardial infarction, stent thrombosis, vaccine
Coronary stent thrombosis is a rare and life-threatening complication of percutaneous coronary intervention, and the clinical presentation is an acute coronary syndrome that ranges in severity depending mainly on the location of the stent. We classify stent thrombosis as early if it occurs within 1 month of stent placement; late, if it occurs between 1 and 12 months; and very late, if it occurs after 12 months. We report a unique case of early stent thrombosis and repeated cardiorespiratory arrest immediately after BNT162b1 mRNA COVID-19 vaccine dose administration.
CASE PRESENTATION
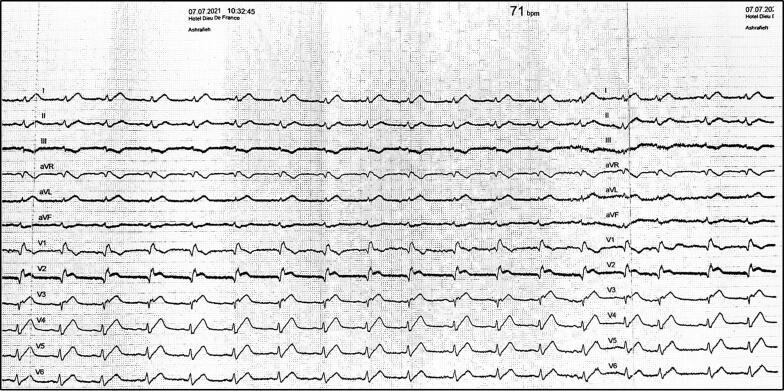
A 64-year-old man presented to our hospital for his first dose of the BNT162b1 mRNA COVID-19 vaccine (Pfizer, New York). One month earlier, he had an anterior wall ST-elevation myocardial infarction, and a second-generation drug-eluting stent was implanted in the proximal left anterior descending artery (LAD). Medications included aspirin and clopidogrel. Fifteen minutes after receiving the vaccine dose, he had chills, chest pain, pallor, diaphoresis, and hypotension. The medical team of the COVID-19 vaccine unit transferred the patient to the emergency department. An electrocardiogram showed ST-segment elevation in the anteroseptal precordial leads (Figure 1). He had multiple episodes of pulseless ventricular tachycardia and ventricular fibrillation treated with electrical defibrillation during his transfer to the catheterization laboratory. Coronary angiography showed stent thrombosis in the proximal segment of the LAD and TIMI grade 0 flow (Figure 2a). Aspiration thrombectomy and balloon angioplasty were performed along with intracoronary tirofiban injection. We achieved recanalization up to the second segment of the LAD with a persistent low flow in the distal LAD (Figure 2b). The arterial pressure was stable after the procedure, with no need for vasopressors. An echocardiogram showed anterior and apical akinesis with an estimated left ventricular ejection fraction of 30%, which did not improve on follow-up. The patient received an implantable cardioverter-defibrillator.
Figure 1.
Electrocardiogram on presentation showing ST segment elevation in the anteroseptal leads.
Figure 2.
(a) Coronary angiogram demonstrating a stent thrombosis of the left anterior descending artery (asterisk) (see also Supplemental Video 1). (b) Coronary angiogram following aspiration thrombectomy and balloon angioplasty along with intracoronary tirofiban injection in the left anterior descending artery (asterisk) with persistent thrombi (arrow) (see also Supplemental Video 2).
DISCUSSION
The difficulty in this unique clinical case is to determine whether the vaccine dose caused the coronary event.1 Type III Kounis syndrome is a highly possible diagnosis. Kounis syndrome is an acute coronary syndrome triggered by an allergic reaction. It is underdiagnosed, and its pathophysiology is still not fully elucidated. Different mechanisms can lead to an acute coronary syndrome during an allergic reaction, leading to a classification with four types.2 Coronary spasm in normal coronary arteries characterizes type I, atheromatous plaque rupture or coronary spasm with a preexisting atheromatous disease defines type II, and stent thrombosis defines type III. Recently, Giovannini et al added type IV to the classification, which involves a coronary artery bypass graft thrombosis.2
COVID-19 vaccines can rarely trigger an allergic reaction.3 The allergen in the BNT162b1 mRNA COVID-19 vaccine is polyethylene glycol. Cardiogenic shock can hide the skin manifestations of anaphylaxis by preventing or delaying the released mediators from reaching and acting on the skin to induce redness, rash, or itching.4 This makes type III Kounis syndrome challenging to diagnose in severe presentations. We did not perform a polyethylene glycol skin prick test for ethical reasons.
Tajstra et al previously reported a fatal case of acute coronary syndrome occurring immediately after a BNT162b1 mRNA COVID-19 vaccine dose in an 86-year-old man.5 There have been several other reports of myocardial infarction occurring after different COVID-19 vaccines, some of which occurred 14 days after vaccination.6–10
Supplementary Material
References
- 1.Allam C, Saouma M, Chlawit R.. Kounis syndrome must be considered in the differential diagnosis of myocardial infarction following COVID-19 vaccination. QJM. 2022. doi: 10.1093/qjmed/hcac001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giovannini M, Koniari I, Mori F, Barni S, Novembre E, Kounis NG.. Kounis syndrome: towards a new classification. Int J Cardiol. 2021;341:13–14. doi: 10.1016/j.ijcard.2021.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Kounis NG, Koniari I, de Gregorio C, et al. Allergic reactions to current available COVID-19 vaccinations: pathophysiology, causality, and therapeutic considerations. Vaccines (Basel). 2021;9(3):221. doi: 10.3390/vaccines9030221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kounis NG, Cervellin G, Koniari I, et al. Anaphylactic cardiovascular collapse and Kounis syndrome: systemic vasodilation or coronary vasoconstriction? Ann Transl Med. 2018;6(17):332. doi: 10.21037/atm.2018.09.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tajstra M, Jaroszewicz J, Gąsior M.. Acute coronary tree thrombosis after vaccination for COVID-19. JACC Cardiovasc Interv. 2021;14(9):e103–e104. doi: 10.1016/j.jcin.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maadarani O, Bitar Z, Elzoueiry M, et al. Myocardial infarction post COVID-19 vaccine—coincidence, Kounis syndrome or other explanation—time will tell. JRSM Open. 2021;12(8):20542704211025259. doi: 10.1177/20542704211025259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boivin Z, Martin J.. Untimely myocardial infarction or COVID-19 vaccine side effect. Cureus. 2021;13(3):e13651. doi: 10.7759/cureus.13651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee E, Chew NWS, Ng P, Yeo TJ.. A spectrum of cardiac manifestations post Pfizer-BioNTech COVID-19 vaccination. QJM. 2021;114(9):661–662. doi: 10.1093/qjmed/hcab177. [DOI] [PubMed] [Google Scholar]
- 9.Özdemir İH, Özlek B, Özen MB, Gündüz R, Bayturan Ö.. Type 1 Kounis syndrome induced by inactivated SARS-COV-2 vaccine. J Emerg Med. 2021;61(4):e71–e76. doi: 10.1016/j.jemermed.2021.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aye YN, Mai AS, Zhang A.. Acute myocardial infarction and myocarditis following COVID-19 vaccination. QJM. 2021. doi: 10.1093/qjmed/hcab252. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.