Abstract
Femoroacetabular impingement (FAI) has emerged as a common cause of hip pain, especially in young patients. While the exact cause of FAI is unknown, it is thought to result from repetitive microtrauma to the proximal femoral epiphysis leading to abnormal biomechanics. Patients typically present with groin pain that is exacerbated by hip flexion and internal rotation. Diagnosis of FAI is made through careful consideration of patient presentation as well as physical exam and diagnostic imaging. Use of radiographs can help diagnose both cam and pincer lesions, while the use of MRI can diagnose labral tears and cartilage damage associated with FAI. Both non-operative and surgical options have their role in the treatment of FAI and its associated labral tears; however, hip arthroscopy has had successful outcomes when compared with physical therapy alone. Unfortunately, chondral lesions associated with FAI have had poorer outcomes with a higher conversion rate to arthroplasty. Capsular closure following hip arthroscopy has shown superior clinical outcomes and therefore should be performed if possible. More recently, primary labral reconstruction has emerged in the literature as a good option for irreparable labral tears. While non-operative management may have its role in treating patients with FAI, hip arthroscopy has developed a successful track record in being able to treat cam and pincer lesions, chondral damage, and labral injuries.
Keywords: femoroacetabular impingement, cam lesion, pincer lesion, labral tear, hip arthroscopy, labral reconstruction
Introduction
Hip pain is a common ailment that has an effect on patients of all ages. While there are many different diagnoses that result in hip pain, femoroacetabular impingement (FAI) has emerged as a common cause, especially in young patients, and therefore needs to be evaluated. FAI is a result of abnormal contact pressure between the femoral head neck junction and the acetabulum leading to abnormal biomechanics. It is a collection of symptoms caused by an excess of bone growth at the head of the femur (cam-type) or the acetabular margin (pincer type). It is often distinguished as a cam deformity or pincer deformity, though recent literature has identified lesions with mixed cam and pincer morphology to be most prevalent among symptomatic patients.1 While FAI can lead to hip pain, it is important to note that cam and pincer morphology can also be seen in asymptomatic patients.2 In addition to FAI itself, the abnormal contact between the femoral head neck junction and the acetabulum can lead to labral tears, thus exacerbating the symptoms experienced by the patient. It has been reported that labral tears in the setting of FAI can be as high as 59%.3 Given the high prevalence of FAI-associated labral tears, it is understandable that there has been a recent increase in literature on the topic, allowing for improved treatment of patients with this ailment. Improved surgical techniques have allowed for improved outcomes following hip arthroscopy.
FAI Etiology, Epidemiology, and Presentation
Until the early 2000s, when Ganz et al. published their study suggesting femoroacetabular impingement led to osteoarthritis of the hip joint, there was little in the orthopedic literature about the significance of FAI as a clinical entity.4,5 The exact cause of FAI (cam, pincer, or combined) continues to remain unknown. The leading theory on FAI suggests that repetitive microtrauma to the proximal femoral epiphysis and abnormally high loading forces during skeletal development lead to the bony overgrowth seen in FAI.4,6,7 Cam type FAI occurs when there is an abutment of the femoral neck against the acetabulum due to a morphological abnormality of the femoral head and neck junction, whereas pincer impingement occurs when an abnormal excess growth of the acetabular margin leads to impingement against the femoral neck, with both types leading to damage of the articular cartilage and labrum of the hip joint.4,8–13
While the patient population impacted by FAI is often young, patients are typically also recreational or elite athletes presenting with hip pain and loss of range of motion.4,9,10 There have been many studies demonstrating a relationship between high load activity in young athletes across sports and FAI morphology.6,10,11 A higher prevalence of cam-type FAI is seen in males, and particularly male athletes, compared with the general population (41% compared with 17% for male controls).2,8,14,15 The pelvis and hips mature differently in males and females, with earlier ossification of the secondary ossification centers and closure of the growth plates in females than in males, leading to a longer time period for young male athletes to apply abnormal loads on their femoral epiphyses, thus leading to the higher rate of FAI seen in males.2,8,11,14,15 High load sports activities such as hockey, football, basketball, and American football, performed more often by males than females, affect the growth plates.11 Carter et al. found that age at menarche, which corresponds with delayed closure of growth plate, is strongly associated with FAI development.6 Athletes have been shown to reach menarche later than the general population, although ages vary by sport, position, and specialization within the sport.6,16
In female athletes, a higher rate of pincer FAI and hip instability is seen, whereas in male athletes, a higher rate of combined FAI, larger alpha angles, and more extensive acetabular cartilage damage and concomitant microfracture treatment has been observed.2,15 These differences in pathology may be attributable to inherent differences in competitive sport – female athletes competed more often in flexibility (4/38, 11%; P = 0.047) and endurance (9/38, 24%) sports, while male athletes were involved in cutting (14/42, 33%), contact (6/42, 14%), and asymmetric (13/42, 31%) sports more often.17
FAI can present insidiously, with mild to severe pain most often with activities requiring hip flexion such as plyometric workouts.18,19 Pain can also be reported at rest with activities such as sitting at a desk. While location of pain is often variable, most often it involves the groin, but can include the lateral and posterior hip, anterior and posterior thigh, and the lumbar spine.20 Other symptoms include stiffness, clicking, snapping, or catching.
Labral Tears in FAI: Etiology and Diagnosis
The acetabular labrum is a fibrocartilaginous ring that lines the acetabular rim and forms a seal around the femoral head. It plays an important role in distributing compressive loads throughout the hip joint and securing the femoral head within the acetabular socket. Structural deformities of the hip joint, including FAI anatomy, have been implicated in tears of the labrum. The prevalence of labral tears in patients with hip and groin pain, the most common presenting symptoms of FAI, has been estimated at around 22–55% in various studies.21 However, Vahedi et al. found that labral tears were detectable in about 41–43% of patients with asymptomatic FAI, which raises the possibility of an even higher prevalence of tears in the broader FAI population.22,23 In both cam-type and pincer-type impingement, labral tearing is linked to stresses exerted on the labral tissue due to abnormal contact between the femoral head-neck junction and acetabular rim. However, there are notable differences in the tear patterns associated with each impingement type. Cam-type impingement typically causes shearing of the labrum at the chondrolabral junction, resulting in separation of labrum from cartilage in the anterosuperior region without damage to the labrum itself in the early stages.24–27 By contrast, pincer-type morphology causes repetitive “pinching” of the labrum between the acetabular rim and femoral neck, resulting in intrasubstance tearing with sparing of the tip of the labrum.24,27–29 While pincer lesions are typically associated with damage to the anterosuperior labrum, much like cam lesions, they may also present with contrecoup injuries due to posterior subluxation of the femoral head secondary to acetabular overcoverage.27 FAI anatomy can also exhibit characteristics of both cam and pincer-type morphologies, which is referred to as mixed impingement.
Physical Examination and Imaging of FAI and Associated Labral Tears
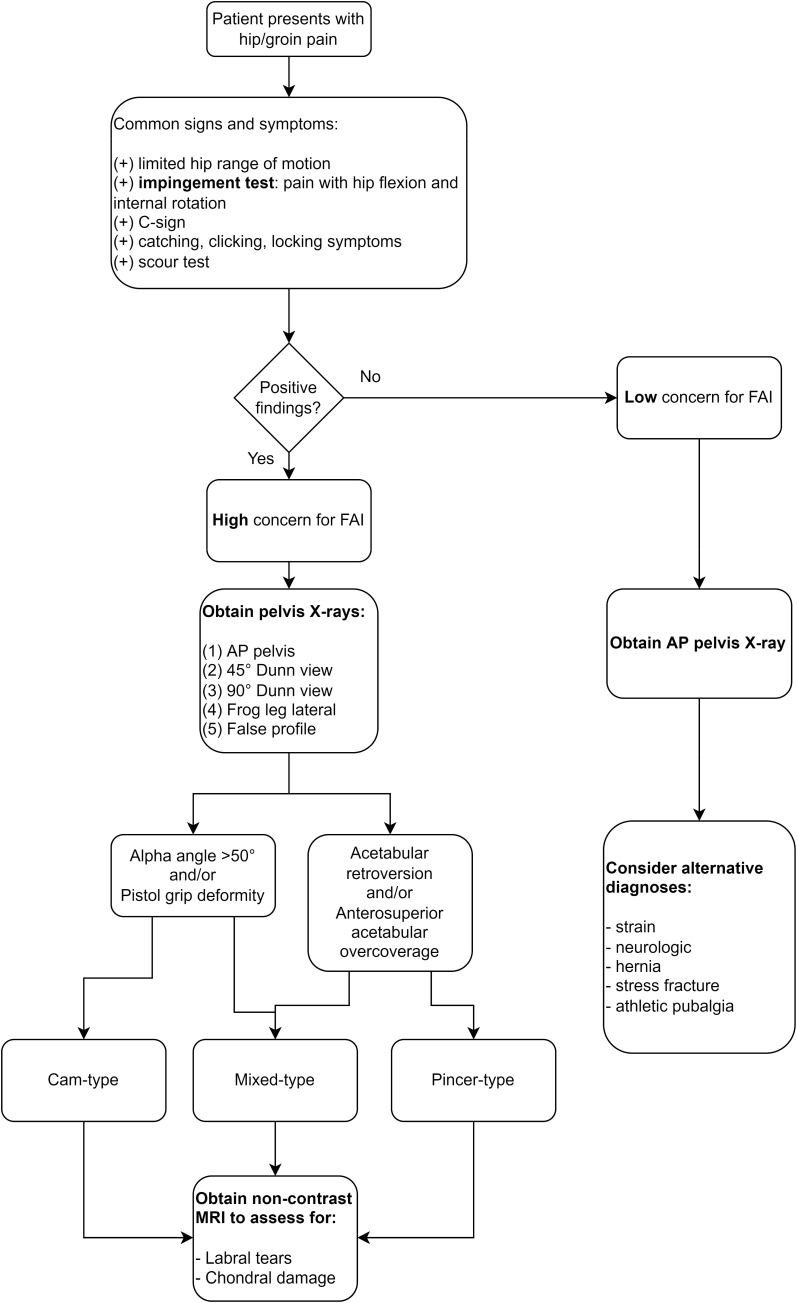
Preoperative diagnosis of labral tears in the setting of FAI is made using a combination of physical exam findings and imaging (Figure 1). Patient-reported symptoms of hip pain exacerbated by flexion and internal rotation and/or anterolateral groin pain that radiates to the thigh (i.e. “C sign”) are concerning for FAI, while the additional symptoms of catching, clicking, or locking in the hip may suggest the presence of a labral tear.30–32 The most commonly used physical exam maneuver for diagnosis of FAI is the impingement test, in which the examiner attempts to elicit pain through hip flexion to 90°, adduction, and internal rotation (often abbreviated as FADIR or FADDIR).21,30,31 The scour test, in which the labrum is stressed by moving an adducted and externally rotated hip into adduction, internal rotation, and extension, has been used to detect labral tears.31 Other maneuvers for FAI and/or labral tear diagnosis such as the flexion-abduction-external rotation (FABER) test, internal rotation with overpressure test, and McCarthy test have been described in the literature. However, it should be noted that none of these tests, including the widely used FADIR maneuver, are considered confirmatory tests for FAI or labral tears as they may be positive in other intra-articular hip pathologies. A meta-analysis by Reiman et al. found that while the FADIR and flexion-internal rotation tests possessed excellent sensitivity (>90%), neither could be confirmed as specific for FAI and/or labral pathology and thus may only be suitable for screening purposes.21
Figure 1.
The senior author’s (TY) preferred algorithm for workup and diagnosis of femoroacetabular impingement (FAI) and comorbid conditions.
Imaging of FAI anatomy and associated labral tears is typically multimodal. First-line evaluation of FAI is performed with plain hip radiographs of the following views: anteroposterior (AP), 45° and 90° Dunn, cross-table lateral, frog-leg lateral (Lauenstein), and/or false profile (Lequesne).32–34 Lateral center edge angle (LCEA) and alpha angle are among the most common radiographic measurements used to assess for the presence of FAI hip anatomy, and recent literature has found both to be associated with labral tear severity as well. Dumont et al. reported that increased LCEA and alpha angle were associated with larger labral tear size among a predominantly young adult cohort. Likewise, Youngman et al. found that increased alpha angle was significantly correlated with increased length of tear and severity of labral disease among adolescent patients with FAI.35 In contrast to imaging for FAI, MRI and MRA are the preferred modalities for imaging of labral tears due to their superior visualization of soft-tissue structures and lesions compared with X-rays. While MRA has been shown to have higher sensitivity to labral tears than MRI, its invasive nature, higher learning curve, and use of radiation are major drawbacks.33,36,37 Czerny et al. developed the most commonly used radiographic classification system for labral tears, divided into three stages based on MRA.37 Matcuk et al. found Czerny staging to have fair inter-rater agreement for labral tears, but Blankenbaker et al. reported poor correlation with arthroscopic Lage classification for labral tears.38,39 More recently, Morgan et al. have proposed a simplified version of the Beck arthroscopic scale, adapted for MRI, for use as a sensitive predictor of reparable labral pathology.40 This modified Beck scale includes six grades of labral tears with grades I, II, and VI considered non-operative tears and grades III–V considered operative tears. The authors found the modified scale to have high sensitivity for potentially reparable tears (85.5–96.0%) but poor inter-rater reliability.
FAI and Chondral Injury
In addition to labral tearing, FAI is associated with injury to the articular cartilage itself. An analysis of the Danish Hip Arthroscopy Registry (DHAR) found that up to 88% of patients with symptomatic FAI had concomitant chondral injury, predominantly on the acetabular side.41 Chondral injury can occur with any FAI morphology but may be more frequent and severe in cam-type anatomy.42,43 Cartilage damage may range from fraying of the chondral surface to full-thickness cartilage flaps with or without an intact chondrolabral junction.44 Femoral head lesion severity may be classified using the same systems for avascular necrosis, such as the Steinberg classification, while acetabular lesions are usually classified using the Beck and Outerbridge systems.45,46 Sampson proposed a new classification system for both types of chondral lesions that was designed to capture a more granular continuum of damage and guide treatment decisions. In this scheme, femoral head lesions are classified by one of six grades based on lesion depth with increasing grade associated with worse prognosis necessitating more aggressive treatment. Similarly, acetabular cartilage lesions are classified into one of ten grades based on lesion area and depth with higher grades associated with more severe lesions. Though created with the stated aim of facilitating an algorithm for treatment, the Sampson scale has not supplanted use of the Steinberg, Beck, and Outerbridge scales in the wider literature.46
A wide array of arthroscopic techniques have been described for treatment of chondral injuries secondary to FAI. Minor damage such as fraying and surface lesions may be treated with simple debridement.44 For more complex lesions involving delamination, repair is indicated and techniques may be broadly divided into (1) primary repair of the tissue, (2) inducing local production of growth factors that promote cartilage healing, and (3) transplanting graft tissue to the injury site.47 Primary repair may be performed with direct fixation of the flap with a biologic adhesive such as fibrin glue. This technique has shown acceptable clinical outcomes at 1–3 years postoperative,48 though a recent laboratory study has questioned whether fibrin fixation provides stable long-term attachment of the cartilage flap.49 Local healing-based techniques include the microfracture method, in which small holes are drilled into the bone underlying a cartilage defect in order to release progenitor cells and growth factors from the marrow. Most studies to date have associated microfracture with comparable but non-superior outcomes to more conventional repair methods such as suturing and debridement.47 Lastly, several transplant techniques have been adapted from knee cartilage repair including osteochondral allograft (OCA), osteochondral autograft (mosaicplasty), and matrix-autologous chondrocyte implantation (MACI), but the evidence favoring their use is limited to several case series with small sample sizes (<30).50
The existing literature strongly indicates that the presence of cartilage lesions is associated with poorer outcomes and higher rate of conversion to THA following arthroscopic treatment of FAI.51–53 In contrast, a recent prospective analysis by Pansard et al. found that chondral lesion extension or type (barring severe lesions of Tönnis grade >1 or Beck 3) were not associated with worse function (as measured by NAHS) at 1-year follow-up after arthroscopic treatment of FAI.54
Labral Tears in FAI: Non-Operative vs Operative Treatment
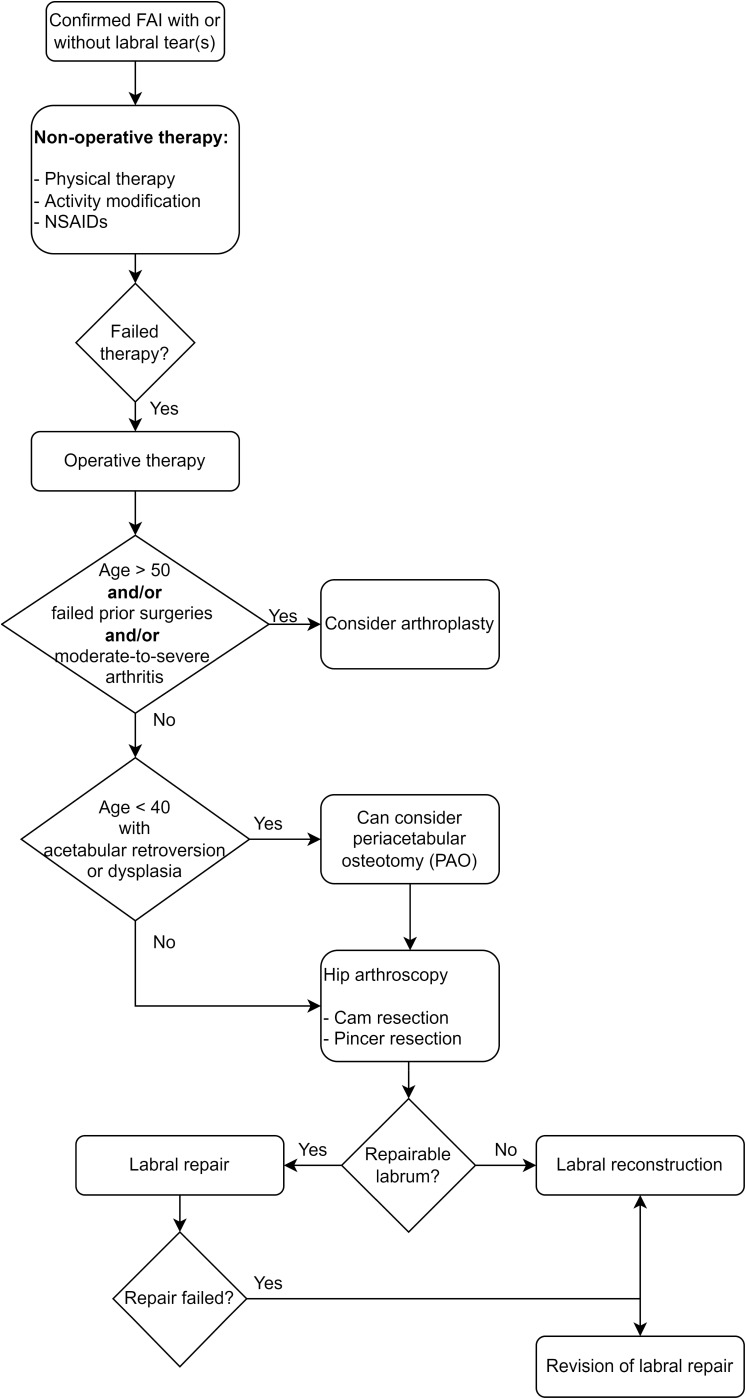
A number of operative and non-operative treatment modalities are available for FAI and associated labral tears (Figure 2). Operative treatment encompasses a variety of open and arthroscopic procedures including osteotomy, osteoplasty, cartilage restoration, and labral debridement, repair and/or reconstruction. Non-operative treatment is generally limited to physical therapy, activity modification, and anti-inflammatory medications (injections or oral). Recent comparative meta-analyses have tended to favor arthroscopic intervention over physical therapy. The largest meta-analysis to date, conducted by Kim et al. found that arthroscopically treated FAI patients had superior International Hip Outcome Tool-33 (iHOT-33) scores at 12-month follow-up compared with their non-operative counterparts.55 Dwyer et al. also found greater pre-to-post treatment improvement in iHOT-33 scores and greater achievement of the minimum clinically significant difference (MCID) at 10-month follow-up among arthroscopic patients compared with non-operative patients.56 Gatz et al. reported superior outcomes on the sport and activities of daily living (ADL) subscales of the Hip Outcome Score (HOS) for arthroscopic patients versus physical therapy patients at 15-month follow-up.57 The relative advantages of arthroscopy for FAI treatment may extend to cost-effectiveness as well; a systematic review by Go et al. found that arthroscopic treatment of FAI resulted in greater gain of quality-adjusted life-years (QALYs) relative to cost compared with non-operative treatment despite the higher upfront cost of surgery.58
Figure 2.
The senior author’s (TY) preferred algorithm for treatment of confirmed femoroacetabular impingement (FAI) with or without concomitant labral tears.
In practice, operative and non-operative modalities are often combined in the treatment of FAI and labral tears and may have complementary effects. A randomized controlled trial conducted by Martin et al. recently found that patients older than 40 years with labral tears randomized to combined hip arthroscopy with physical therapy had superior patient-reported outcomes compared with patients receiving physical therapy alone.59 Furthermore, it should be noted that, per Scott et al., both operative and non-operative treatment approaches to labral tears seem to yield similar rates of conversion to total hip arthroplasty (THA).60 Thus, long-term joint preservation may be a less relevant consideration for patients than symptom severity, cost, and/or lifestyle when selecting a treatment approach for FAI. In support of this point, Glaws et al. found initial interest in surgery, younger age, and poorer hip function to be some of the major predictors of patients pursuing surgery for FAI within 90 days of initial evaluation.61
Outcomes
In the long term, sequelae of FAI have been shown to be unfavorable, especially in young patients with FAI, who are 5–10% more likely to develop hip osteoarthritis at an early age. These patients are more likely to require hip arthroscopy and/or total hip replacement.4,5,62–66
Overall, hip arthroscopy is a low-risk procedure, with reported rates of minor complication ranging from 4.5–7.9% and major complications at 0.45–0.65% respectively. The most common major complication seen is extra-articular fluid exacerbation, while common minor complications include chondrolabral damage and temporary nerve injury.67,68
In the short term, results of hip arthroscopy have been quite successful. Mohan et al. reported 92% return to sport at near pre-injury levels in athletes aged 13–23 who underwent hip arthroscopy at 2 years. In addition, they found that patients who underwent labral repair with chondrolabral preservation did better than those who underwent labral repair with takedown and reattachment.69 In a study on professional hockey players who required hip arthroscopic labral repairs, Philippon et al. reported successful outcomes and return to skating and hockey drills at 3.4 months.70 A recent systematic review of patients who underwent hip arthroscopy for various diagnoses highlighted the high rate of return to sport at an average follow-up of 28 months. The highest rate of return to sport was seen in pediatric patients, professional athletes, and patients with a short duration of symptoms prior to surgery.71
Unfortunately, there is a paucity of high-quality evidence supporting a specific post-operative rehabilitation protocol following hip arthroscopy. In a recent systematic review on rehabilitation following hip arthroscopy, Grzybowski et al. found heterogeneous studies that precluded assimilation of rehabilitation protocols.72 More literature is needed in order to find an optimal rehabilitation protocol to improve patient outcomes.
In the long term, the rate of conversion to arthroplasty is as high as 18.5%, and the overall reoperation rate is 20.8%.68 Older adults are more likely to contribute to the conversion rate of hip arthroscopy to arthroplasty for several reasons.73 For example, preexisting osteoarthritis specifically with severe chondral damage is a risk factor for surgical failure, with a failure rate of 52% compared with 12% in the general surgical population. In patients age >50 with <2 mm of joint space, Philippon et al. demonstrated tenfold higher odds of patients requiring arthroplasty.74
Capsular Considerations in Hip Arthroscopy for FAI
In recent decades, the hip joint capsule and its impact on joint biomechanics after arthroscopic surgery have gained great interest.75–77 The capsule itself is a fibrous structure made by three ligaments and circumferential internal fibers and contains several other important hip stabilizers. Several studies suggest that capsular closure at the time of hip arthroscopy may better restore anatomic stability and lead to better hip function outcomes.75 Similarly, Ortiz-Declet et al. conducted a systematic review noting that both clinically and biomechanically, capsular repair results in superior short-term outcomes and stability in comparison to arthroscopy without capsular repair.78 In a study of 1-year outcomes after hip arthroscopy for FAI in the Danish Hip Arthroscopy Registry, Mygind-Klavsen et al. found that patient-reported outcomes (HSAS, EQ-5D, NRS pain (rest and walk), and Copenhagen Hip and Groin Outcome Score (HAGOS) subscales) were significantly improved in the group that underwent capsular closure compared with those who did not.79 Additionally, the capsular closure group had a significantly lower revision arthroscopy rate at 2 years post-index arthroscopy (3.5%) compared with the non-closure group (6.8%). While these results are promising, further prospective study is required to compare outcomes after different types of capsular closure. Frank et al.’s retrospective study comparing complete repair to partial repair of T capsulotomy showed that patients with complete repair had superior patient-reported outcomes including sports-specific outcomes and patient satisfaction at 2 years after index arthroscopy.80 In addition, they found lower rates of revision hip arthroscopy in the complete repair group. Despite the potential benefits of capsular closure, a standard surgical methodology for closure in hip arthroscopy for FAI remains to be determined. Gupta et al. found in a multicenter survey study of hip arthroscopy surgeons that while 88.9% of surgeons performed capsular closure, there was great variability in how and how often closure is performed.81 That said, capsular closure bears significant promise in improving clinical outcomes after hip arthroscopy for FAI.
Future Prospects
In recent years, labral reconstruction over repair in the primary setting has gained some interest among hip arthroscopists (Table 1). Previously, labral reconstruction was reserved mainly for the revision setting, however increasing literature on the subject shows its use in a primary setting under very specific indications may provide good outcomes. In a direct comparison of primary acetabular labral repair and labral reconstruction in 29 patients (labral repair in one hip and labral reconstruction in the opposite hip), White et al. found that the hips that underwent labral repair were more likely to fail treatment compared with the labral reconstruction. It is important to note that patient-reported outcomes among hips that did not fail were similar between the groups.82 This was met with mixed reviews due mainly to the fact that at the time there were no long-term data supporting reconstruction. In addition, there are added risks to reconstruction and therefore this may not be warranted in every patient with a labral tear.
Table 1.
A Summary of the Recent Literature on Labral Repair and Labral Reconstruction
| Authors | Study Design | Population Included | Key Findings |
|---|---|---|---|
| Martin et al. (2021)59 | Randomized controlled trial with single surgeon; patients were randomized 1:1 to labral repair (SPT) or physical therapy alone (PTA). | n = 90; age >40 with symptomatic MRI-confirmed labral tears, Tönnis grades 0–2 | - 63.6% crossover rate from PTA to SPT group - Greater iHOT-33 and mHHS scores in SPT group than PTA group at 12 months - Difference in scores exceeded MCID |
| Drager et al. (2020)86 | Case-control study; patients with hypotrophic labrum were matched 1:1 by age and BMI to patients with normal labral width | n = 346; patients who underwent primary arthroscopic labral repair for FAI | - No significant differences in HOS, mHHS, and iHOT-12 scores at 1 year - No significant differences in achieving MCID or PASS at 1 year |
| White et al. (2020)85 | Retrospective comparative study; patients who underwent labral reconstruction were compared with patients who underwent labral repair | n = 343 patients (363 hips); age 30–65 and underwent labral reconstruction OR age 40–65 and underwent labral repair | - Failure was 3.29 times more likely for repair group versus reconstruction group at mean 4.2-year follow-up - No difference in rate of conversion to THA - Greater improvement in mHHS among successful reconstruction patients versus successful repair patients |
| Domb et al. (2020)87 | Case-control study; patients who underwent primary circumferential labral reconstruction with tibialis anterior allograft were matched 1:3 on age, sex, and BMI to patients who underwent labral repair | n = 37 patients (37 hips); irreparable labral tears and FAIS, Tönnis grade <2, no dysplasia (LCEA ≤ 18°) | - Circumferential labral reconstruction group had significant improvement in mHHS, NAHS, HOS - Sport-Specific Subscale, iHOT-12, and VAS scores at minimum 2-year follow-up - Improvements in PROs were comparable between reconstruction and repair groups |
| Scanaliato et al. (2018)84 | Prospective cohort study with single surgeon; patients who underwent primary circumferential labral reconstruction with allograft were compared with patients who underwent primary labral repair | n = 162 hips; patients with labral tears that limited desired activity level and failed 6 months of non-operative treatment | - No significant difference in failure rates between repair and reconstruction groups - Significant improvement in mHHS, iHOT-12, SF-12, and VAS scores at mean 2-year follow-up in both groups - No significant difference in improvement in PROs between both groups |
| Chandrasekaran et al. (2019)88 | Retrospective comparative study; patients who underwent primary labral reconstruction were matched 1:2 on age, sex, BMI, capsular treatment, and level of chondral damage (outerbridge grade) to patients who underwent primary labral repair | n = 102; patients with labral tears and minimum 2-year follow-up | - Significant improvement in mHHS, HOS - Sports Subscale, NAHS, and VAS scores in both repair and reconstruction groups at minimum 2-year follow-up - No significant differences in rates of postoperative complications, secondary arthroscopy, or conversion to THA |
Abbreviations: iHOT, International Hip Outcome Tool; mHHS, Modified Harris Hip Score; HOS, Hip Outcome Score; MCID, minimum clinically important difference; PASS, Patient Acceptable Symptom State; THA, total hip arthroplasty; NAHS, Non-Arthritic Hip Score; VAS, Visual Analog Scale.
More recently, other studies have reported similar outcomes between labral repair and reconstruction, with some pointing toward improved outcomes following labral reconstruction in the primary setting. In a multicenter retrospective review, Bodendorfer et al. reported no difference between labral repair, segmental labral reconstruction, and circumferential labral reconstruction at a minimum of 2-year follow-up.83 In addition, Scanaliato et al. showed similar short-term outcomes between labral reconstruction and labral repair.84 White et al. found an increased failure rate of 3.29 times in patients over 40 years old undergoing repair vs reconstruction in the primary setting.85 While limited data do indicate good results in primary labral reconstruction, long-term results are unknown and therefore thoughtful decision making should be employed when considering reconstruction over repair.
Conclusion
In the past 20 years, our understanding of FAI with associated labral tears and its clinical implications has grown immensely. Injuries and biomechanical abnormalities that previously would go undiagnosed are now being recognized and treated sooner, leading to improved outcomes. Understanding which patients are at increased risk, can lead to a more accurate diagnosis and therefore a more successful treatment of their hip pain. Each patient with hip pain is unique and therefore a thorough evaluation and treatment plan needs to be implemented. While hip arthroscopy with labral repair has shown improved outcomes over physical therapy alone in the setting of FAI with labral tears, the best post-operative rehabilitation protocol has not been borne out in the literature. Therefore, post-operative rehabilitation needs to be specific to the patients’ needs whether they are a young athlete or middle-aged mildly active patient. More research is currently needed in order to determine the most optimal rehabilitation protocol. Longer-term studies with functional outcomes is required to determine the efficacy of primary labral reconstruction over labral repair. As of now, hip arthroscopy with labral repair offers great outcomes with high rates of return to play.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hale RF, Melugin HP, Zhou J, et al. Incidence of femoroacetabular impingement and surgical management trends over time. Am J Sports Med. 2021;49(1):35–41. doi: 10.1177/0363546520970914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frank JM, Harris JD, Erickson BJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015;31(6):1199–1204. doi: 10.1016/j.arthro.2014.11.042 [DOI] [PubMed] [Google Scholar]
- 3.Meermans G, Konan S, Haddad FS, Witt JD. Prevalence of acetabular cartilage lesions and labral tears in femoroacetabular impingement. Acta Orthop Belg. 2010;76(2):181–188. [PubMed] [Google Scholar]
- 4.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA, Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed] [Google Scholar]
- 5.Menge TJ, Truex NW. Femoroacetabular impingement: a common cause of hip pain. Phys Sportsmed. 2018;46(2):139–144. doi: 10.1080/00913847.2018.1436844 [DOI] [PubMed] [Google Scholar]
- 6.Carter CW, Campbell A, Whitney D, et al. Characterizing cam-type hip impingement in professional women’s ice hockey players. Phys Sportsmed. 2021;49(2):203–206. doi: 10.1080/00913847.2020.1808434 [DOI] [PubMed] [Google Scholar]
- 7.Aminoff AS, Agnvall C, Todd C, et al. Young elite Alpine and Mogul skiers have a higher prevalence of cam morphology than non-athletes. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1262–1269. doi: 10.1007/s00167-018-5236-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Philippon MJ, Ho CP, Briggs KK, Stull J, LaPrade RF. Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. Am J Sports Med. 2013;41(6):1357–1362. doi: 10.1177/0363546513483448 [DOI] [PubMed] [Google Scholar]
- 9.Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):908–914. doi: 10.1007/s00167-007-0332-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egger AC, Frangiamore S, Rosneck J. Femoroacetabular Impingement: a review. Sports Med Arthrosc Rev. 2016;24(4):e53–e58. doi: 10.1097/JSA.0000000000000126 [DOI] [PubMed] [Google Scholar]
- 11.Leunig M, Juni P, Werlen S, et al. Prevalence of cam and pincer-type deformities on hip MRI in an asymptomatic young Swiss female population: a cross-sectional study. Osteoarthritis Cartilage. 2013;21(4):544–550. doi: 10.1016/j.joca.2013.01.003 [DOI] [PubMed] [Google Scholar]
- 12.Anbar A, Ragab Y, Zeinhom F, et al. Cam versus pincer femoroacetabular impingement. Which type is associated with more hip structural damage? An exploratory cross-sectional study. Curr Orthop Pract. 2017;28(2):188–194. doi: 10.1097/BCO.0000000000000481 [DOI] [Google Scholar]
- 13.Keogh MJ, Batt ME. A review of femoroacetabular impingement in athletes. Sports Med. 2008;38(10):863–878. doi: 10.2165/00007256-200838100-00005 [DOI] [PubMed] [Google Scholar]
- 14.Nepple JJ, Vigdorchik JM, Clohisy JC. What is the association between sports participation and the development of proximal femoral cam deformity? A systematic review and meta-analysis. Am J Sports Med. 2015;43(11):2833–2840. doi: 10.1177/0363546514563909 [DOI] [PubMed] [Google Scholar]
- 15.Mascarenhas VV, Rego P, Dantas P, et al. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: A systematic review. Eur J Radiol. 2016;85(1):73–95. doi: 10.1016/j.ejrad.2015.10.016 [DOI] [PubMed] [Google Scholar]
- 16.Vadocz EA, Siegel SR, Malina RM. Age at menarche in competitive figure skaters: variation by competency and discipline. J Sports Sci. 2002;20(2):93–100. doi: 10.1080/026404102317200800 [DOI] [PubMed] [Google Scholar]
- 17.Shibata KR, Matsuda S, Safran MR. Arthroscopic hip surgery in the elite athlete: comparison of female and male competitive athletes. Am J Sports Med. 2017;45(8):1730–1739. doi: 10.1177/0363546517697296 [DOI] [PubMed] [Google Scholar]
- 18.Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24(12):1407–1421. doi: 10.1016/j.arthro.2008.06.019 [DOI] [PubMed] [Google Scholar]
- 19.Hunt D, Prather H, Harris Hayes M, Clohisy JC. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PM R. 2012;4(7):479–487. doi: 10.1016/j.pmrj.2012.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–644. doi: 10.1007/s11999-008-0680-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reiman MP, Goode AP, Cook CE, Holmich P, Thorborg K. Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: a systematic review with meta-analysis. Br J Sports Med. 2015;49(12):811. doi: 10.1136/bjsports-2014-094302 [DOI] [PubMed] [Google Scholar]
- 22.Vahedi H, Aalirezaie A, Azboy I, Daryoush T, Shahi A, Parvizi J. Acetabular labral tears are common in asymptomatic contralateral hips with femoroacetabular impingement. Clin Orthop Relat Res. 2019;477(5):974–979. doi: 10.1097/CORR.0000000000000567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Domb BG. Insights(R): CORR acetabular labral tears are common in asymptomatic contralateral hips with femoroacetabular impingement. Clin Orthop Relat Res. 2019;477(5):980–982. doi: 10.1097/CORR.0000000000000606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Philippon MJ, Patterson DC, Briggs KK. Hip arthroscopy and femoroacetabular impingement in the pediatric patient. J Pediatr Orthop. 2013;33(Suppl 1):S126–130. doi: 10.1097/BPO.0b013e318274f834 [DOI] [PubMed] [Google Scholar]
- 25.Todd JN, Maak TG, Anderson AE, Ateshian GA, Weiss JA. How does chondrolabral damage and labral repair influence the mechanics of the hip in the setting of cam morphology? A finite-element modeling study. Clin Orthop Relat Res. 2021;480: 10–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leunig M, Beck M, Kalhor M, Kim YJ, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236(1):237–246. doi: 10.1148/radiol.2361040140 [DOI] [PubMed] [Google Scholar]
- 27.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203 [DOI] [PubMed] [Google Scholar]
- 28.Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2(2):105–117. doi: 10.1007/s12178-009-9052-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ejnisman L, Ricioli Junior W, Queiroz MC, Vicente JRN, Croci AT, Polesello GC. Femoroacetabular impingement and acetabular labral tears - part 1: pathophysiology and biomechanics. Rev Bras Ortop. 2020;55(5):518–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Rourke RJ, El Bitar Y. Femoroacetabular impingement. In: StatPearls. Treasure Island, FL, USA: StatPearls Publishing; 2021. [PubMed] [Google Scholar]
- 31.Calcei JG, Safran MR. Evaluation of athletes with hip pain. Clin Sports Med. 2021;40(2):221–240. doi: 10.1016/j.csm.2020.11.001 [DOI] [PubMed] [Google Scholar]
- 32.Polesello GC, Eisjman L, Queiroz MC, Rudelli BA, Rudelli M, Ricioli Junior W. Femoroacetabular impingement and acetabular labral tears - part 2: clinical diagnosis, physical examination and imaging. Rev Bras Ortop. 2020;55(5):523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Y, Lu W, Ouyang K, Deng Z. The imaging evaluation of acetabular labral lesions. J Orthop Traumatol. 2021;22(1):34. doi: 10.1186/s10195-021-00595-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66. doi: 10.2106/JBJS.H.00756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Youngman TR, Wagner KJ 3rd, Montanez B, et al. The association of alpha angle on disease severity in adolescent femoroacetabular impingement. J Pediatr Orthop. 2021;41(2):88–92. doi: 10.1097/BPO.0000000000001703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saied AM, Redant C, Anthonissen J, et al. Conventional versus direct magnetic resonance imaging in detecting labral lesions in femoroacetabular impingment - a retrospective multicenter study. Acta Orthop Belg. 2019;85(1):100–106. [PubMed] [Google Scholar]
- 37.Czerny C, Hofmann S, Neuhold A, et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology. 1996;200(1):225–230. doi: 10.1148/radiology.200.1.8657916 [DOI] [PubMed] [Google Scholar]
- 38.Matcuk GR Jr, Price SE, Patel DB, White EA, Cen S. Acetabular labral tear description and measures of pincer and cam-type femoroacetabular impingement and interobserver variability on 3T MR arthrograms. Clin Imaging. 2018;50:194–200. doi: 10.1016/j.clinimag.2018.04.002 [DOI] [PubMed] [Google Scholar]
- 39.Blankenbaker DG, De Smet AA, Keene JS, Fine JP. Classification and localization of acetabular labral tears. Skeletal Radiol. 2007;36(5):391–397. doi: 10.1007/s00256-006-0240-z [DOI] [PubMed] [Google Scholar]
- 40.Morgan P, Crawford A, Marette S, et al. Using a simplified version of a common surgical grading scale for acetabular labral tears improves the utility of preoperative hip MRI for femoroacetabular impingement. Skeletal Radiol. 2020;49(12):1987–1994. doi: 10.1007/s00256-020-03495-9 [DOI] [PubMed] [Google Scholar]
- 41.Lund B, Nielsen TG, Lind M. Cartilage status in FAI patients - results from the Danish Hip Arthroscopy Registry (DHAR). SICOT J. 2017;3:44. doi: 10.1051/sicotj/2017023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ortiz-Declet V, Maldonado DR, Annin S, et al. Nonarthritic hip pathology patterns according to sex, femoroacetabular impingement morphology, and generalized ligamentous laxity. Am J Sports Med. 2021;50:3635465211056086. [DOI] [PubMed] [Google Scholar]
- 43.Pascual-Garrido C, Li DJ, Grammatopoulos G, Yanik EL, Clohisy JC, Group A. The pattern of acetabular cartilage wear is hip morphology-dependent and patient demographic-dependent. Clin Orthop Relat Res. 2019;477(5):1021–1033. doi: 10.1097/CORR.0000000000000649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ross JR, Clohisy JC, Bedi A, Zaltz I. Why does hip arthroscopy fail? Indications and PEARLS for revision success. Sports Med Arthrosc Rev. 2021;29(1):44–51. doi: 10.1097/JSA.0000000000000300 [DOI] [PubMed] [Google Scholar]
- 45.Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77(1):34–41. doi: 10.1302/0301-620X.77B1.7822393 [DOI] [PubMed] [Google Scholar]
- 46.Sampson TG. Arthroscopic treatment for chondral lesions of the hip. Clin Sports Med. 2011;30(2):331–348. doi: 10.1016/j.csm.2010.12.012 [DOI] [PubMed] [Google Scholar]
- 47.Bagheri K, Sierra F, Jamali AA. Acetabular cartilage repair: state of the art in surgical treatment. J Hip Preserv Surg. 2020;7(2):205–224. doi: 10.1093/jhps/hnaa025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stafford GH, Bunn JR, Villar RN. Arthroscopic repair of delaminated acetabular articular cartilage using fibrin adhesive. Results at one to three years. Hip Int. 2011;21(6):744–750. doi: 10.5301/HIP.2011.8843 [DOI] [PubMed] [Google Scholar]
- 49.Levinson C, Naal FD, Salzmann GM, Zenobi-Wong M, Leunig M. Is there a scientific rationale for the refixation of delaminated chondral flaps in femoroacetabular impingement? A laboratory study. Clin Orthop Relat Res. 2020;478(4):854–867. doi: 10.1097/CORR.0000000000001135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hevesi M, Jacob G, Shimomura K, Ando W, Nakamura N, Krych AJ. Current hip cartilage regeneration/repair modalities: a scoping review of biologics and surgery. Int Orthop. 2021;45(2):319–333. doi: 10.1007/s00264-020-04789-2 [DOI] [PubMed] [Google Scholar]
- 51.Streich NA, Gotterbarm T, Barie A, Schmitt H. Prognostic value of chondral defects on the outcome after arthroscopic treatment of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2009;17(10):1257–1263. doi: 10.1007/s00167-009-0833-x [DOI] [PubMed] [Google Scholar]
- 52.Ward JP, Rogers P, Youm T. Failed hip arthroscopy: causes and treatment options. Orthopedics. 2012;35(7):612–617. doi: 10.3928/01477447-20120621-11 [DOI] [PubMed] [Google Scholar]
- 53.Vahedi H, Yacovelli S, Diaz C, Parvizi J. Surgical treatment of femoroacetabular impingement: minimum 10-Year outcome and risk factors for failure. JB JS Open Access. 2021;6(4). doi: 10.2106/JBJS.OA.20.00176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pansard E, Thaunat M, Vigan M, Wettstein M, Flecher X, Francophone Arthroscopy S. Impact of bone deformities and labral and cartilage lesions on early functional results of arthroscopic treatment of femoroacetabular impingement. Orthop Traumatol Surg Res. 2021;107(8S):103069. doi: 10.1016/j.otsr.2021.103069 [DOI] [PubMed] [Google Scholar]
- 55.Kim CH, Moon JK, Yoon JY, et al. Arthroscopy versus nonoperative treatment of symptomatic femoroacetabular impingement syndrome: a protocol for systematic review and meta-analysis. Medicine. 2020;99(49):e23247. doi: 10.1097/MD.0000000000023247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dwyer T, Whelan D, Shah PS, Ajrawat P, Hoit G, Chahal J. Operative versus nonoperative treatment of femoroacetabular impingement syndrome: a meta-analysis of short-term outcomes. Arthroscopy. 2020;36(1):263–273. doi: 10.1016/j.arthro.2019.07.025 [DOI] [PubMed] [Google Scholar]
- 57.Gatz M, Driessen A, Eschweiler J, Tingart M, Migliorini F. Arthroscopic surgery versus physiotherapy for femoroacetabular impingement: a meta-analysis study. Eur J Orthop Surg Traumatol. 2020;30(7):1151–1162. doi: 10.1007/s00590-020-02675-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Go CC, Kyin C, Chen JW, Domb BG, Maldonado DR. Cost-effectiveness of hip arthroscopy for treatment of femoroacetabular impingement syndrome and labral tears: a systematic review. Orthop J Sports Med. 2021;9(3):2325967120987538. doi: 10.1177/2325967120987538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martin SD, Abraham PF, Varady NH, et al. Hip arthroscopy versus physical therapy for the treatment of symptomatic acetabular labral tears in patients older than 40 years: a randomized controlled trial. Am J Sports Med. 2021;49(5):1199–1208. doi: 10.1177/0363546521990789 [DOI] [PubMed] [Google Scholar]
- 60.Scott BL, Lee CS, Shi LL, Lee MJ, Athiviraham A. Nonoperative management of hip labral tears yields similar total hip arthroplasty conversion rate to arthroscopic treatment. J Arthroplasty. 2020;35(1):23–27 e21. doi: 10.1016/j.arth.2019.08.042 [DOI] [PubMed] [Google Scholar]
- 61.Glaws K, Brown-Taylor L, Pomeroy M, et al. Factors associated with initial interest and treatment selection in patients with femoroacetabular impingement syndrome. PM R. 2020;12(12):1227–1235. doi: 10.1002/pmrj.12344 [DOI] [PubMed] [Google Scholar]
- 62.Melugin HP, Hale RF, Zhou J, et al. Risk factors for long-term hip osteoarthritis in patients with femoroacetabular impingement without surgical intervention. Am J Sports Med. 2020;48(12):2881–2886. doi: 10.1177/0363546520949179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.van Klij P, Heerey J, Waarsing JH, Agricola R. The prevalence of cam and pincer morphology and its association with development of hip osteoarthritis. J Orthop Sports Phys Ther. 2018;48(4):230–238. doi: 10.2519/jospt.2018.7816 [DOI] [PubMed] [Google Scholar]
- 64.Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93(5):580–586. doi: 10.1302/0301-620X.93B5.25236 [DOI] [PubMed] [Google Scholar]
- 65.Wyles CC, Heidenreich MJ, Jeng J, Larson DR, Trousdale RT, Sierra RJ. The John Charnley award: redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res. 2017;475(2):336–350. doi: 10.1007/s11999-016-4815-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hoch A, Schenk P, Jentzsch T, Rahm S, Zingg PO. FAI morphology increases the risk for osteoarthritis in young people with a minimum follow-up of 25 years. Arch Orthop Trauma Surg. 2021;141(7):1175–1181. doi: 10.1007/s00402-020-03522-3 [DOI] [PubMed] [Google Scholar]
- 67.Weber AE, Harris JD, Nho SJ. Complications in hip arthroscopy: a systematic review and strategies for prevention. Sports Med Arthrosc Rev. 2015;23(4):187–193. doi: 10.1097/JSA.0000000000000084 [DOI] [PubMed] [Google Scholar]
- 68.Griffin DW, Kinnard MJ, Formby PM, McCabe MP, Anderson TD. Outcomes of hip arthroscopy in the older adult: a systematic review of the literature. Am J Sports Med. 2017;45(8):1928–1936. doi: 10.1177/0363546516667915 [DOI] [PubMed] [Google Scholar]
- 69.Mohan R, Johnson NR, Hevesi M, Gibbs CM, Levy BA, Krych AJ. Return to sport and clinical outcomes after hip arthroscopic labral repair in young amateur athletes: minimum 2-year follow-up. Arthroscopy. 2017;33(9):1679–1684. doi: 10.1016/j.arthro.2017.03.011 [DOI] [PubMed] [Google Scholar]
- 70.Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99–104. doi: 10.1177/0363546509346393 [DOI] [PubMed] [Google Scholar]
- 71.Memon M, Kay J, Hache P, et al. Athletes experience a high rate of return to sport following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3066–3104. doi: 10.1007/s00167-018-4929-z [DOI] [PubMed] [Google Scholar]
- 72.Grzybowski JS, Malloy P, Stegemann C, Bush-Joseph C, Harris JD, Nho SJ. Rehabilitation following hip arthroscopy - a systematic review. Front Surg. 2015;2:21. doi: 10.3389/fsurg.2015.00021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Domb BG, Linder D, Finley Z, et al. Outcomes of hip arthroscopy in patients aged 50 years or older compared with a matched-pair control of patients aged 30 years or younger. Arthroscopy. 2015;31(2):231–238. doi: 10.1016/j.arthro.2014.08.030 [DOI] [PubMed] [Google Scholar]
- 74.Philippon MJ, Schroder ESBG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28(1):59–65. doi: 10.1016/j.arthro.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 75.Kuhns BD, Weber AE, Levy DM, et al. Capsular management in hip arthroscopy: an anatomic, biomechanical, and technical review. Front Surg. 2016;3:13. doi: 10.3389/fsurg.2016.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wuerz TH, Song SH, Grzybowski JS, et al. Capsulotomy size affects hip joint kinematic stability. Arthroscopy. 2016;32(8):1571–1580. doi: 10.1016/j.arthro.2016.01.049 [DOI] [PubMed] [Google Scholar]
- 77.Chahla J, Mikula JD, Schon JM, et al. Hip capsular closure: a biomechanical analysis of failure torque. Am J Sports Med. 2017;45(2):434–439. doi: 10.1177/0363546516666353 [DOI] [PubMed] [Google Scholar]
- 78.Ortiz-Declet V, Mu B, Chen AW, et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34(1):303–318. doi: 10.1016/j.arthro.2017.06.030 [DOI] [PubMed] [Google Scholar]
- 79.Mygind-Klavsen B, Lund B, Grønbech Nielsen T, et al. Capsular closure in patients with Femoroacetabular Impingement Syndrome (FAIS): results of a matched-cohort study from the Danish hip arthroscopy registry. J Hip Preserv Surg. 2020;7(3):474–482. doi: 10.1093/jhps/hnaa033 [DOI] [Google Scholar]
- 80.Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634–2642. doi: 10.1177/0363546514548017 [DOI] [PubMed] [Google Scholar]
- 81.Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy. 2015;31(9):1722–1727. doi: 10.1016/j.arthro.2015.03.023 [DOI] [PubMed] [Google Scholar]
- 82.White BJ, Patterson J, Herzog MM. Bilateral hip arthroscopy: direct comparison of primary acetabular labral repair and primary acetabular labral reconstruction. Arthroscopy. 2018;34(2):433–440. doi: 10.1016/j.arthro.2017.08.240 [DOI] [PubMed] [Google Scholar]
- 83.Bodendorfer BM, Alter TD, Carreira DS, et al. Multicenter outcomes after primary hip arthroscopy: a comparative analysis of two-year outcomes after labral repair, segmental labral reconstruction, or circumferential labral reconstruction. Arthroscopy. 2021;38(2):352–361. [DOI] [PubMed] [Google Scholar]
- 84.Scanaliato JP, Christensen DL, Salfiti C, Herzog MM, Wolff AB. Primary circumferential acetabular labral reconstruction: achieving outcomes similar to primary labral repair despite more challenging patient characteristics. Am J Sports Med. 2018;46(9):2079–2088. doi: 10.1177/0363546518775425 [DOI] [PubMed] [Google Scholar]
- 85.White BJ, Patterson J, Scoles AM, Lilo AT, Herzog MM. Hip arthroscopy in patients aged 40 years and older: greater success with labral reconstruction compared with labral repair. Arthroscopy. 2020;36(8):2137–2144. doi: 10.1016/j.arthro.2020.04.031 [DOI] [PubMed] [Google Scholar]
- 86.Drager J, Rasio J, Newhouse A, Beck E, Chahla J, Nho SJ. Patients with a hypotrophic labrum achieve similar outcomes after primary labral repair compared with patients with a normal-sized labrum: a matched cohort analysis of 346 patients with femoroacetabular impingement syndrome. Arthroscopy. 2020;36(10):2614–2620. doi: 10.1016/j.arthro.2020.05.039 [DOI] [PubMed] [Google Scholar]
- 87.Domb BG, Kyin C, Rosinsky PJ, et al. Circumferential labral reconstruction for irreparable labral tears in the primary setting: minimum 2-year outcomes with a Nested Matched-Pair Labral Repair Control Group. Arthroscopy. 2020;36(10):2583–2597. doi: 10.1016/j.arthro.2020.02.014 [DOI] [PubMed] [Google Scholar]
- 88.Chandrasekaran S, Darwish N, Mu BH, et al. Arthroscopic reconstruction of the irreparable acetabular labrum: a match-controlled study. Arthroscopy. 2019;35(2):480–488. doi: 10.1016/j.arthro.2018.09.024 [DOI] [PubMed] [Google Scholar]