Abstract
Benign metastasizing leiomyoma is a rare condition where benign smooth muscle tumors having a histological appearance similar to uterine leiomyoma are present at distant sites. This entity is commonly associated with a past history of hysterectomy done for uterine fibroids. The knowledge of the presence of significant fluorodeoxyglucose uptake in leiomyoma helped in the diagnosis of this condition in a 47-year-old patient who being evaluated for multiple unusual sites of metastases; this was further confirmed on histopathology.
Keywords: 18F-fluorodeoxyglucose positron emission tomography/contrast-enhanced computed tomography, benign metastasizing leiomyoma, fibroid, hysterectomy
Introduction
FDG PET/CT is an established imaging modality in oncology practice due to its differential uptake in cells with high glucose metabolism like neoplastic cells. Therefore, FDG-PET is a sensitive modality for the diagnosis and staging of several types of malignancies. Benign metastasizing leiomyoma (BML) is a rare disease occurring predominantly in women of reproductive age and usually develops in women with history of hysterectomy or myomectomy for fibroids in past. Since FDG shows significant uptake in leiomyoma, we used this principle and picked up an unusual sites of metastases from BML which was further confirmed on histopathology.
Case Report
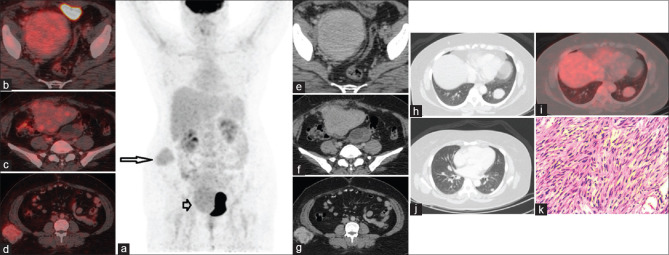
A 47-year-old female with a past history of hysterectomy for dysfunctional uterine bleeding presented with complaints of abdominal pain and distention for 3 months. The patient was evaluated with routine blood parameters and tumor markers (including CA125, CA19-9, and CEA) and computed tomography (CT) which demonstrated a pelvic mass with size of 6 cm × 4.6 cm × 3.6 cm. A suspicion of a malignant etiology was raised and an 18F-fluorodeoxyglucose positron emission tomography/contrast-enhanced CT (18F FDG PET/CECT) was advised in search of possible primary and disease mapping. FDG PET CT MIP image [Figure 1a] showed low grade FDG uptake in the pelvic mass, (arrow) and right abdominal wall (arrow). Well demarcated homogenous lesions with low grade FDG uptakes are seen in the abdomino-pelvic region, largest in pelvis [Figure 1f and i] and subcutaneous region of abdomen [Figure 1g] and lungs [Figure 1h and j] in transaxial fused PET CT images & CT images [Figure 1b-e]. The tumor markers were within the normal limits. Impressing further on past history, it was elicited that the patient had undergone two surgeries for fibroid removal (myoma resection), prior to hysterectomy. The characteristic well-demarcated homogeneous morphology of all lesions and prior history raised a strong suspicion of benign metastasizing leiomyoma (BML). A biopsy was suggested, which was suggestive of smooth muscle tumor confirming the functional radiological diagnosis of BML [Figure 1k]. Pathologically, BML consists of well-differentiated spindle-shaped cells and there is no disorganized growth pattern and mitotic figures. Besides these, Ki67 index for the BML is less than that for leiomyosarcoma.[1,2] Estrogen/progesterone receptor (ER/PR) status was strongly positive, and thus the patient was started on medical castration using luteinizing hormone-releasing hormone analogs.
Figure 1.
Fluorodeoxyglucose positron emission tomography and computed tomography maximum intensity projection image (a) showed low grade fluorodeoxyglucose uptake in the pelvic mass (arrow) and right abdominal wall (arrow). Well demarcated homogeneous lesions with low grade fluorodeoxyglucose uptakes are seen in the abdomino pelvic region, largest in the pelvis (b and c) and subcutaneous region of the abdomen (d) and lungs (i) in transaxial fused positron emission tomography computed tomography images and computed tomography images (e-h and j). Histopathology slides confirmed the same(k)
Discussion
Uterine leiomyoma, the most common gynecologic neoplasms, show clinical symptoms in approximately 20%–30% of women older than 35 years,[3,4,5,6] and the characteristic features of a leiomyoma provide an unambiguous radiologic diagnosis. BML is a rare condition characterized by numerous well-differentiated leiomyomas at sites distant from the uterus, however are histologically identical. “Metastases” mostly affect the lungs,[7] whereas the others are the heart, brain, lymph nodes, bone, and skin. The presence of mild-to-moderate FDG uptake in multiple lung lesions without enlarged mediastinal and hilar nodes with or without a pelvic mass and other system involvement in a female patient with a past history of fibroids is predictive of BML as suggested by Lin et al.,[8] though this needs further larger cohort elucidation. The treatment modalities for BML are based on ER/PR suppression and include administering progesterone, medical castration using luteinizing hormone-releasing hormone analog, bilateral oophorectomy, radiation therapy to the ovary, and chemotherapy. If required, the combination of medical and surgical treatment has to be considered to arrive at an effective therapeutic plan.[9] Our case highlights the utility of F18 FDG PET/CT in characterizing the lesions both anatomically and functionally, mapping the disease extent thus helping in arriving at the diagnosis of BML. Thus, it can be said that F18 FDG PET/CT may prove useful in identifying the rare condition of BML.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mayerhofer K, Lozanov P, Bodner K, Bodner-Adler B, Kimberger O, Czerwenka K. Ki-67 expression in patients with uterine leiomyomas, uterine smooth muscle tumors of uncertain malignant potential (STUMP) and uterine leiomyosarcomas (LMS) Acta Obstet Gynecol Scand. 2004;83:1085–8. doi: 10.1111/j.0001-6349.2004.00502.x. [DOI] [PubMed] [Google Scholar]
- 2.Gezginç K, Yazici F, Tavli L. Uterine smooth muscle tumors of uncertain malignant potential: A case presentation. Int J Clin Oncol. 2011;16:592–5. doi: 10.1007/s10147-010-0172-4. [DOI] [PubMed] [Google Scholar]
- 3.Lee AY, Poder L, Qayyum A, Wang ZJ, Yeh BM, Coakley FV. Imaging malignant and apparent malignant transformation of benign gynaecological disease. Clin Radiol. 2010;65:1031–7. doi: 10.1016/j.crad.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Fasih N, Prasad Shanbhogue AK, Macdonald DB, Fraser-Hill MA, Papadatos D, Kielar AZ, et al. Leiomyomas beyond the uterus: Unusual locations, rare manifestations. Radiographics. 2008;28:1931–48. doi: 10.1148/rg.287085095. [DOI] [PubMed] [Google Scholar]
- 5.Szklaruk J, Tamm EP, Choi H, Varavithya V. MR imaging of common and uncommon large pelvic masses. Radiographics. 2003;23:403–24. doi: 10.1148/rg.232025089. [DOI] [PubMed] [Google Scholar]
- 6.Buttram VC, Jr, Reiter RC. Uterine leiomyomata: Etiology, symptomatology, and management. Fertil Steril. 1981;36:433–45. doi: 10.1016/s0015-0282(16)45789-4. [DOI] [PubMed] [Google Scholar]
- 7.Wolff M, Silva F, Kaye G. Pulmonary metastases (with admixed epithelial elements) from smooth muscle neoplasms. Report of nine cases, including three males. Am J Surg Pathol. 1979;3:325–42. doi: 10.1097/00000478-197908000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Lin X, Fan W, Lang P, Hu Y, Zhang X, Sun X. Benign metastasizing leiomyoma identified using 18F-FDG PET/CT. Int J Gynaecol Obstet. 2010;110:154–6. doi: 10.1016/j.ijgo.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Moon H, Park SJ, Lee HB, Kim SR, Choe YH, Chung MJ, et al. Pulmonary benign metastasizing leiomyoma in a postmenopausal woman. Am J Med Sci. 2009;338:72–4. doi: 10.1097/MAJ.0b013e31819c7160. [DOI] [PubMed] [Google Scholar]