Abstract
This study examined links between aspects of parenting and children’s cortisol and whether those links varied by child behavioral problems and ethnicity. Participants included children ages 9 to 15 (N = 159, 75% Latinx) and their primary caregivers from the Los Angeles Family and Neighborhood Survey (L.A.FANS; Wave 2). Children provided saliva at wake, 30 minutes after wake, and at bedtime which was analyzed for cortisol. Analyses revealed associations between parenting behavior and cortisol were greater among children who had behavioral problems and these associations were stronger among non-Latinx White children compared to Latinx children. This study moves beyond the current literature by investigating these important associations in a predominately Latinx urban sample of children.
Keywords: ethnicity, cortisol, parent-child relationship, parenting, behavioral problems
The parent-child tie represents an important source of support as well as strain for children. Children exposed to negative parenting (e.g., maltreatment, harsh parenting) have more depressive symptoms, worse school performance, and poorer physical health (Troxel & Matthews, 2004). Likewise, supportive parenting often predicts positive outcomes among children such as better academic performance and less externalizing problems (Pettit, Bates, & Dodge, 1997). Indeed, a lack of parental support may have a cascading effect on children that influences their physical and psychological well-being for years to come (Shaw, Krause, Chatters, Connell, & Ingersoll-Dayton, 2004). In addition, children with greater internalizing (e.g., withdrawal) or externalizing (e.g., aggression) behavior problems exhibit dysregulation of stress and may be more vulnerable to particular family environments (Cicchetti, Rogosch, Gunnar, & Toth, 2010; Boyce & Ellis, 2005; O’Neal et al., 2010; Spies, Margolin, Susman, & Seeman 2011). There has been an impetus in the research literature to understand the mechanism by which stressful or supportive parenting ‘get under the skin’ to influence children’s health. One major pathway is the Hypothalamic Pituitary Adrenal (HPA) axis or the physiological stress response system. Indeed, research reveals links between parenting behavior and children’s cortisol patterns, an important marker of the HPA axis (O’Neal et al., 2010; DePasquale, Raby, Hoye, & Dozier, 2018; Lupien, King, Meaney, & McEwen, 2000)
Although studies have established links between parenting and children’s cortisol, much of the work has focused on mainly non-Latinx White middle-class children. (In this study, we use the gender-inclusive term Latinx, rather than Latino/a or Hispanic, to refer to people whose cultural background originated in Latin America.) The present study examines links between parenting behavior and children’s cortisol among a predominately Latinx urban sample of children ages 9 to 15 years. The Latinx population in the United States is growing rapidly (Passel, Cohn, & Lopez, 2011) with one-quarter of children identifying as ethnically Latinx in 2016 (Child Trends, 2018). One distinct difference between Latinx families and their White counterparts is the socialization of cultural norms such as family-oriented values as well as experiences of culturally-related stressors (Cauce & Domenech-Rodríguez, 2002; Figge et al., 2021), which may affect parenting, behavioral problems, and the stress response. In the present study, we examine associations between positive and negative aspects of parenting behavior and children’s cortisol and whether these links are moderated by children’s behavioral problems and ethnicity.
Theoretical Frameworks, Environmental Contexts, and the Cortisol Response
This study first uses the biopsychosocial model to understand how parenting behavior influence children’s cortisol. According to the biopsychosocial model, contextual and social factors affect psychological systems, which in turn influence biological systems (Taylor, Repetti, & Seeman, 1997). This study in particular examines links between the parenting behavior, children’s behavioral problems, and children’s biological stress response (i.e., diurnal cortisol). Parenting behavior varies in the extent to which it is loving and supportive (positive characteristics) as well as the extent to which it is conflictual and hurtful (negative characteristics), which can impact children’s stress response.
After a stressful stimulus is perceived, the hypothalamus releases corticotropin-releasing hormone stimulates the anterior pituitary to release adrenocorticopic hormone (ACTH). ACTH then stimulates the adrenal cortex to release glucocorticoids (which in humans consists primarily of cortisol). This cascade of events has been termed the ‘stress response’ (Sapolsky, Romero, & Munck, 2000). In short, the body responds to an acute stressful event with elevated levels of circulating glucocorticoids, which serve to mobilize energy reserves and curtail non-essential metabolic processes. The ‘stress response’ is functional in response to acute challenges because it mobilizes energy for immediate use in an effort to bring the body back to homeostasis—a process known as allostasis. However, a continued and chronic stress response is harmful and is often referred to as allostatic load (McEwen & Seeman, 1999). Allostatic load may result from the inability to calm down after a stressful event and/or the inability to adapt to a repeated stressful event. Increased cortisol is associated with distress, withdrawal, and avoidance and cortisol increases when events are perceived as uncontrollable (Dickerson & Kemeny, 2004).
Another framework that provides insights as to why children experience diverse reactions to stress is biological sensitivity-to-context theory. Along with extant research, it posits that children differ in their psychobiological reactivity to stress due to variation in susceptibility to their environment (Boyce & Ellis, 2005; Cicchetti et al., 2010; Fisher et al., 2007). Children with internalizing (e.g., anxiety, depression, withdrawal) and externalizing (e.g., impulsivity, aggression) behavioral problems may be more vulnerable to both positive and negative contexts such as parenting. In response to such contexts, they may display heightened or depressed diurnal cortisol reactivity (Cicchetti et al., 2010; O’Neal et al., 2010; Spies et al., 2011).
Children’s differential reactions to stress suggests the existence of two competing hypotheses regarding the link between family stress and the HPA axis: 1) hypercortisolism suggests that children will have a greater stress response to family conflict over time (i.e., higher biological sensitivity to context), whereas 2) hypocortisolism suggests that children will have a suppressed stress response to family conflict over time due to a blunting of the stress response (i.e., lower biological sensitivity to context). The HPA axis adapts to prolonged stress by down regulating cortisol, which is proposed to be initially adaptive because it leads to less damage of physiological systems (Fries, Hesse, Hellhammer, & Hellhammer, 2005). But over time, a blunted HPA response is linked to negative outcomes such as increased physical, psychological, and behavioral problems (Adam et al., 2017; Ruttle et al., 2011).
The present study uses multiple measures of the diurnal cortisol rhythm to assess these hypotheses: cortisol awakening response, daily decline, and overall cortisol levels. Cortisol has a normal diurnal rhythm over the course of the day in which it begins to increase before waking, reaches a peak level at about 30 minutes after waking (cortisol awakening response [CAR]) and steadily declines thereafter until bedtime (daily decline [DEC] or slope; Fries, Dettenborn, & Kirschbaum, 2009; Pruessner et al., 1997). The CAR represents the anticipation of the coming day or a boost of energy to ready the person for the day (Almeida, Piazza, & Stawski, 2009; Fries et al., 2009). Overall cortisol levels are assessed with the area under the curve (AUC) which provides an index of the amount of cortisol secreted over a designated time period, which is defined as one day in the current study (Pruessner et al., 2003).
The CAR, DEC, and AUC each have implications for health and well-being. For example, greater CAR in childhood and adolescence is associated with later depression (Adam et al., 2010). Likewise, flatter DEC is associated with poor emotional health (Adam et al., 2017) including increased stress in children (Wolf, Nicholls, & Chen, 2008) and behavioral problems in adolescents (Klimes-Dougan, Hastings, Granger, Usher, & Zahn-Waxler, 2001). In addition, having a higher overall cortisol level (i.e., greater AUC) is associated with greater negative emotion (e.g., anger, stress, and anxiety) and poorer well-being (Adam, Klimes-Dougan, & Gunnar, 2007; Goodyer, Tamplin, Herbert, & Altham, 2000). Interestingly, a meta-analysis by Adam and colleagues (2017) found that flatter DEC showed larger effect sizes in its associations with externalizing symptoms (r = .254) compared to internalizing symptoms (r = .129). But in a study of young children, infants with higher CAR, flatter DEC, and greater AUC were more likely have higher levels of internalizing problem behavior, but not externalizing behavior, as preschoolers (Saridjan et al., 2016). These individual elements of the diurnal cortisol rhythm are essential to healthy HPA axis functioning and provide complementary information regarding the stress mechanisms that influence physical and mental health outcomes (see Adam et al., 2017).
Positive and Negative Aspects of Parenting Behavior and Children’s Cortisol
The family context determines lifespan developmental pathways of resilience and vulnerability. One of the major pathways that may account for these links is the quality of parent-child interactions through parenting behavior, which has implications for the HPA axis. Greater positive parenting behavior is often associated with hypercortisolism (i.e., steeper diurnal cortisol rhythms) whereas less positive parenting is associated with hypocortisolism (i.e., flatter diurnal cortisol rhythms). In a sample of economically disadvantaged families, young children whose mothers were more supportive toward them during a collaborative laboratory task had steeper cortisol rhythms over the course of one day (waking, 20 minutes after wake, and every two hours until bedtime; Fisher et al., 2007). Similarly, Pendry and Adam (2007) found that more positive mother parenting behaviors (involvement, warmth) were associated with steeper cortisol curve slopes using waking and bedtime cortisol over two days in children and adolescents. However, there is also some evidence that more positive parenting is associated with less cortisol reactivity among children living in poverty (Brown et al., 2020).
The associations between negative parent-child interactions and the HPA axis show mixed evidence of both hyper and hypocortisolism. Multiple studies demonstrate that infants, children, and adolescents of depressed mothers have high cortisol levels (Azak, Murison, Wentzel-Larsen, Smith, & Gunnar, 2013; Halligan, Herbert, Goodyer, & Murray, 2004; Lupien et al., 2000). Contrarily, Booth and colleagues (2008) found that adolescent girls with poor parental acceptance had lower overall cortisol levels (over the course of two days at wake) although there were no associations among children or adolescent boys. In a longitudinal study, Roisman and colleagues (2009) found that exposure to higher levels of maternal insensitivity in early childhood predicted lower awakening cortisol in adolescents. Likewise, studies of more extreme forms of negative parenting often document hypocortisolism. For example, children who were severely maltreated (e.g., neglect, emotional maltreatment, physical abuse) in the first five years of life had flatter daily cortisol declines than those who had not been maltreated (Cichetti et al., 2010). Two studies indicated that internationally adopted children exhibited a blunted cortisol response pattern, likely to due to experiencing early adversity, but that later sensitive and nurturing parenting was associated with children’s greater cortisol reactivity (i.e., higher waking cortisol, steeper decline) (DePasquale et al., 2018; Raby, Bernard, Gordon, & Dozier, 2020). The present study considers more normative aspects of positive (e.g., praise) and negative (e.g., stress) parenting behavior and their links with children’s diurnal cortisol rhythms.
Children’s Internalizing and Externalizing Behavior Problems and Cortisol
Children with behavioral problems may be more sensitive to certain parenting and family environments and thus display greater diurnal variation in cortisol levels. Using saliva collected at four time points over the course of the day, Van Ryzin et al. (2009) found that children with high internalizing behavior problems demonstrated higher cortisol levels if parents scored low on parenting quality (e.g., sensitivity, structuring). However, youth with internalizing behavior problems may display different diurnal rhythms depending on the amount of time since the onset of behaviors (Ruttle et al., 2011). Initial stress exposure may elicit a hypercortisolism response but long-term exposure may lead to a pattern of hypocortisolism (Ruttle et al., 2011).
In terms of externalizing behavior problems, Alink and colleagues (2013) found that maltreated children who were low on prosocial behavior and exhibited aggressive behaviors had lower morning cortisol levels one year later. Similarly, a sample of nonmaltreated boys with externalizing problems showed low levels of morning and average cortisol, suggestive of hypocortisolism (Cicchetti & Rogosch, 2001). Ruttle et al. (2011) noted that youth with more externalizing behaviors in childhood had flattened diurnal cortisol rhythms as adolescents. Children with behavioral problems may be especially vulnerable to stressful environments.
Variations by Ethnicity
This study benefits from having data on both Latinx and non-Latinx youth. Although Latinx families are quite diverse, many share and prioritize similar values. Familismo emphasizes the importance of family solidarity and obligation (Cauce & Domenech-Rodríguez, 2002) and strong family cohesion, relationships, and support may serve as a protective factor for Latinx families (Figge et al., 2021; Leidy, Guerra, & Toro, 2010). Latinx parents and children often encounter cultural stress or the “strain associated with navigating multiple cultural contexts as a member of a minority group, which can include language difficulties, incongruent cultural values and traditions […], and discrimination, among other stressors” (Figge et al., 2021, p. 1036). Racism, a multi-level systemic stressor, can impact individuals’ health through pathways such as increased negative emotions and allostatic load (Cheadle et al., 2020; Paradies et al., 2015). Links between racism and negative health outcomes are particularly strong for Latinx Americans (Paradies et al., 2015). Latinx families’ experiences of cultural stress is related to lower positive and involved parenting (Leidy et al., 2010; Lorenzo-Blanco et al., 2016) and increased child behavioral problems (McCord, Draucker, & Bigatti, 2019; Wu, Marsiglia, Ayers, Cutrín, & Vega-López, 2020). Consequently, relations among parenting, behavioral problems, and cortisol may be greater for Latinx children compared to their non-Latinx White counterparts.
Present Study
The majority of cortisol research has focused on samples of predominately non-Latinx White American children. This study seeks to examine whether positive and negative aspects of parenting behavior are associated with children’s diurnal cortisol rhythms over the course of the day in a more ethnically diverse random sample, representative of a large U.S. metropolitan area. The purpose of this study was to answer three research questions.
Are positive and negative aspects of parenting behavior associated with variations in children’s cortisol? We predicted that children experiencing more positive aspects of parenting would have steeper cortisol rhythms consistent with hypercortisolism (i.e., steeper CAR and DEC) but lower overall cortisol scores indicative of less stress (i.e., lower AUC). Conversely, we predicted that children experiencing more negative aspects of parenting would have flatter cortisol rhythms consistent with hypocortisolism (i.e., flatter CAR and DEC) but higher overall cortisol scores indicative of greater stress (i.e., higher AUC).
Does the link between positive and negative aspects of parenting behavior and cortisol vary by children’s behavioral problems? We hypothesized that children with more internalizing and externalizing problems would be more sensitive to parenting and have stronger associations between cortisol and positive parenting behavior (i.e., even steeper CAR and DEC and flatter AUC) and negative parenting behavior (i.e., even flatter CAR and DEC and higher AUC) than children with fewer internalizing and externalizing problems.
Do links among positive and negative aspects of parenting behavior, child behavioral problems, and cortisol vary by ethnicity? We predict that parenting and behavioral problems will be more highly associated with cortisol among Latinx children (e.g., even steeper, or even flatter cortisol response depending on the type of parenting and children’s behavioral problems) compared to among non-Latinx White children.
Method
Participants
The data are from the second wave of the Los Angeles Family and Neighborhood Survey (L.A.FANS) which is a study of adults and children in Los Angeles County conducted between 2006 and 2008. Data are available through the Inter-university Consortium for Political and Social Research (ICPSR; https://www.icpsr.umich.edu/web/DSDR/series/846) (Pebley & Sastry, 2019). The Institutional Review Board of the University of Michigan reviewed and approved this study. Participants are from a stratified random sample of 65 neighborhoods (strata: very poor, poor, and non-poor).
In each household, interviews were conducted of at least one randomly selected adult and one randomly selected child. If the randomly selected adult was not the child’s mother and/or primary caregiver, an interview was conducted with the mother/primary caregiver. If the child had siblings, an interview was conducted of a randomly selected sibling. At the time of initial contact with parents and children, oral consent was obtained for parent participation followed by collecting written consent from the parent and oral assent from the child for child participation. This study focused on the sample of children ages 9 to 15 (53% female; 75% Latinx) who provided useable saliva samples and had self-reports as well as primary caregiver reports of the parent-child tie (n = 159). Primary caregivers included biological mothers (n = 148) and fathers (n = 3), adoptive mothers (n = 4) fathers (n = 1), stepmothers (n = 1), aunts (n = 1), and foster parents (n = 1). Hereafter we refer to caregivers as parents.
In L.A.FANS, 489 children aged 3 to 17 had at least one saliva sample and reported their ethnicity as Latinx or non-Latinx White. Only children aged 9 to 17 reported on their relationship with their parents and only parents with children aged 15 and younger reported on amount of physical affection with their children. Therefore, we chose a sample size of children aged 9 to 15 (n = 316). Children were then removed from this sample because of cortisol values with errors (n = 85, these specific errors are described in further detail in the Measures) or because they did not have enough cortisol samples to make at least one of the outcome variables (n = 20). An additional 52 children were removed for having missing data on the following predictor variables and covariates: parent report of praising child, physical affection, and parent stress; child report of negative parenting; child internalizing/externalizing behavior; day of the week cortisol was collected; wake time; and whether the child took medication for asthma. This resulted in a selected analytic sample of 159 children.
We conducted a series of independent samples t-tests and chi-square tests to assess whether there were variations between the selected sample and the sample that was not selected in aspects of parenting behavior, behavioral problems, or demographics. The selected sample was less stressed on the parental stress measure (t = 2.46, p < .05), older (t = −2.95, p < .01), and less likely to be Latinx (χ2 = 4.92, p < .05). There were no variations between the samples in gender, parent education, parent reports of physical affection and praise, children’s reports of positive and negative parenting, or children’s internalizing or externalizing behavioral problems.
Measures
Cortisol.
Parents were provided the sample collection kits along with an information sheet that explained how to label the collection times, how to store the samples, and return them. Interviewers trained the parents how to collect the saliva. Interviewers were specifically trained to go over the instruction sheet with participants and help them prepare their tubes for collection including writing the dates and times on the tubes. Children provided saliva samples at waking, 30 minutes after waking, and bedtime. Interviewers were trained to stress the importance of collecting the 30 minute post waking saliva sample on time, using a timer, writing the time on each tube, and providing adult supervision. Parents were instructed to ensure children avoided dental work within 24 hours, waited for gum or mouth wounds to heal before taking the sample, and avoided alcohol for 24 hours. Parents were also instructed to monitor their children’s behavior in the period immediately before saliva sample collection with the following guidelines: no brushing teeth within 2 hours, no eating a major meal within 60 minutes, avoiding dairy products within 30 minutes, and no eating acidic or high sugar foods within 30 minutes.
Salivary samples were collected from children by the parent with a Sorbette collection device (a small, arrowhead-shaped hydrocellulose sponge attached to a plastic shaft) on the day after the interview, refrigerated, and mailed to the lab. Each sample was divided and assayed for salivary cortisol in parallel using a highly sensitive enzyme immunoassay (Salimetrics, State College, PA). The average of the two samples were used in the analyses. The test requires 25µl of saliva and has a range of sensitivity from 0.007 to 3.0 µg/dl, and average intra-and inter-assay coefficients of variation of 5% and 10%, respectively. Cortisol was converted to nmol/L for consistency with other studies (by multiplying the samples by 27.59) and was then transformed with the natural log transformation to reduce skew.
We created three scores that represented the cortisol awakening response (CAR); the daily decline (DEC); and the area under the curve (AUC) (Pruessner, Kirschbaum, Meinlschmid, & Hellhammer, 2003). The CAR was calculated by taking the difference between the log transformed 30 minutes after wake and wake cortisol divided by the difference between the time the 30 minutes after wake and wake samples were collected (Almeida et al., 2009). CAR had four outliers but skew (0.62) and kurtosis (3.26) were within acceptable range. The DEC was calculated by taking the difference between the log transformed bed time and 30 minutes after wake cortisol divided by the difference between the time the bedtime and 30 minutes after wake samples were collected. DEC had three outliers but skew (.74) and kurtosis (.66) were within acceptable range. The AUC was calculated using Pruessner’s formula for determining area under the curve in response to ground: (30 minute after wake cortisol + wake time cortisol)/2 * time difference between 30 minute after wake and wake sample collection + (bedtime cortisol + 30 minutes after wake cortisol)/2 * time difference between bedtime and 30 minutes after wake sample collection (Pruessner et al., 2003). AUC had six outliers but skew (1.19) and kurtosis (3.94) were within acceptable range.
Consistent with previous research on cortisol, we removed cortisol data with errors using casewise deletion (n = 85; Birditt, Kim, Zarit, Fingerman, & Loving, 2016; Birditt, Manalel, Kim, Zarit, & Fingerman, 2017). These errors included children who provided their samples in the incorrect order, children who provided the 30 minute sample less than 15 minutes or more than 60 minutes after waking, children who were awake less than 12 or more than 20 hours, children who woke past noon, children for whom there was missing time of collection information, and children who provided saliva samples across different days rather than the same day. Saliva samples at all three time points (i.e., waking, 30 minutes after waking, and bedtime) in the same day are required to calculate diurnal cortisol rhythms over one day.
Parent report on aspects of parenting behavior.
Parents were asked about two positive parenting behaviors: “In the past week, about how many times have you praised {CHILD NAME} for doing something worthwhile?” and “In the past week, have you shown {CHILD NAME} physical affection (for example: kisses, hugs, stroking hair, etc.)?” Items were rated from 1 (never) to 3 (almost every day). Items were modified from the Panel Study of Income Dynamics-Child Development Supplement (PSID-CDS; Hoffereth, Davis-Kean, Davis, & Finkelstein, 1998) and were examined separately due to low internal consistency (α = .59).
Parents also reported on their parental stress. They reported the degree to which they experienced stress as a result of parenting with four items such as: “Being a parent is harder than I thought it would be” and “I feel trapped in my responsibilities as a parent”. Each item was rated on a scale from 1 (completely false) to 5 (completely true). Items were adapted from the PSID-CDS (Hoffereth et al., 1998). Items were averaged to create a parental stress score (α = .72).
Child report on aspects of parenting behavior.
Children reported on the positive and negative aspects of their mother’s and father’s parenting behavior. Positive items included “How often does your mother/father say good things about you for doing well?”, “How often does your mother/father help you with things that are important to you?”, and “How often does your mother/father know who you are with when you are not at home?”. The negative item included “How often does your mother/father say bad things about you or your ideas?”. Item responses ranged from 1 (never) to 4 (often). Items were modified from the NLSY 97 (Bureau of Labor Statistics, n.d.). Mother and father positive and negative parenting items were averaged to create positive (α = .68) and negative (α = .71) parent scores.
Behavioral problems index.
Parents were asked about children’s behavioral problems which included 30 items (Peterson & Zill, 1986) and formed two subscales: internalizing behavior problems (15 items; α = .82) and externalizing behavior problems (15 items; α = .88). Examples of internalizing items included “Child has been fearful or anxious”, “Child has been withdrawn”, and “Child has been unhappy, depressed”. Examples of externalizing problems included “Child has been impulsive”, “Child has strong temper, loses it easily”, and “Child has been disobedient”. Parents responded to items on a scale of 1 (often true), 2 (sometimes true), or 3 (not true). Items were reverse coded so that higher scores reflect more behavior problems.
Ethnicity.
Ethnicity was coded as −1 (non-Latinx White) and 1 (Latinx).
Covariates.
Several covariates were considered: children’s gender (1 = girl, −1 = boy), continuous child age (range: 9 to 15 years), continuous primary caregiver years of education, asthma medication (1 = asthma medication, −1 = no asthma medication), weekend cortisol (1 = weekend, −1 = weekday), and wake time (descriptive statistics are presented in Table 1).
Table 1.
Description of Children who Provided Cortisol and their Caregivers in the Los Angeles Family and Neighborhood Study (weighted data)
| Children (N = 159) | Primary caregiver (N = 159) | |
|---|---|---|
| Gender | ||
| Female (%) | 53.1 | 96.7 |
| Ethnicity and Race | ||
| Latinx (%) | 75.1 | 75.6 |
| Non-Latinx | ||
| White (%) | 24.9 | 23.9 |
| Native American (%) | - | 0.5 |
| Age (M, SD) | 12.32 (1.97) | 40.51 (6.63) |
| Education (M, SD) | 6.35 (2.08) | 11.34 (4.42) |
| Asthma medication use (%) | 11.5 | n/a |
| Weekend collection (%) | 35.4 | n/a |
| Wake time collection (M, SD) | 7.57 (1.38) | n/a |
| 30 min. after wake time collection (M, SD) | 8.10 (1.39) | |
| Bedtime collection (M, SD) | 20.85 (4.49) |
Note. Cortisol collection times are presented in military time.
Analysis Strategy
Analyses were conducted in SAS. Data are weighted as not all respondents who agreed to saliva collection actually provided samples (i.e., non-response). The weight takes into account demographic and socioeconomic factors that are associated with the sampling design of L.A.FANS as well as the patterns of non-response of children who agreed to provide saliva.
We used linear regressions to examine whether cortisol varied by parenting behavior, child behavioral problems, and ethnicity. The models were estimated separately for CAR, DEC, and AUC but were otherwise identical in terms of predictor variables and covariates. Models included three steps: 1) main effects of aspects of parenting behavior (both parent and child reports) and main effects of child behavioral problems, 2) interactions between the parenting behavior variables and child behavioral problems, and 3) all two-way and three-way interactions with ethnicity (Latinx vs. non-Latinx White). Models examined child internalizing and externalizing behaviors separately. Due to the complexity of the interactions, each aspect of parenting behavior (i.e., parent reports of praise, physical affection, stress, and child reports of positive and negative parenting) were tested in ten separate models (as internalizing and externalizing behaviors were also separate) for both steps 2 and 3. Based on preliminary models predicting CAR, DEC, and AUC with all the covariates, we retained covariates that were significantly associated with at least one cortisol value (p < .05) which included age and weekend cortisol. All continuous variables were centered on the grand mean and categorical variables were effect coded (−1, 1). Significant interactions were graphed and simple slopes tests were used to assess whether the slopes were significantly different from zero (Dawson, 2014). To account for multiple comparisons, we used the Bonferonni procedure to adjust the significance level by the number of outcomes (p = .05/3 = .0167; Bender & Lange, 2001). All results presented remain significant after the correction.
Results
Description of Parenting Behavior and Cortisol
Children on average had a normal diurnal rhythm of cortisol characterized by a cortisol awakening response (CAR) and a decline (DEC) until bedtime (descriptives presented in Table 2). We also examined whether there were ethnic differences in positive and negative parenting behavior, child behavioral problems, and cortisol levels. Latinx parents reported less praise, physical affection, and positive parenting than non-Latinx White parents (Table 2). The correlations between parent and child reports of parenting were low to moderate ranging from .05 to .17 (correlations presented in Table 3). The correlation between CAR and DEC was r = −.38 (p < .001), between area under the curve (AUC) and CAR was r = .22 (p < .01), and between AUC and DEC was r = .18 (p < .05).
Table 2.
Description of Cortisol and Parent-Child Tie Variables
| Total Sample (N = 159) | Latinx (n = 119) | Non-Latinx Whites (n = 40) | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | M | SD | t | |
| Cortisol (nmols) | |||||||
| Waking | 10.28 | 15.27 | 10.68 | 17.16 | 8.93 | 5.14 | 0.80 |
| Thirty minutes after wake | 11.97 | 13.02 | 12.09 | 14.47 | 11.62 | 7.21 | 0.24 |
| Bedtime | 1.96 | 4.47 | 2.13 | 5.06 | 1.47 | 1.81 | 1.05 |
| AUC | 102.55 | 114.87 | 103.95 | 127.54 | 97.89 | 55.52 | 0.35 |
| CAR | 3.53 | 13.64 | 3.23 | 14.17 | 4.55 | 11.82 | −0.52 |
| DEC | −0.72 | 0.79 | −0.72 | 0.86 | −0.72 | 0.54 | −0.01 |
| Cortisol (natural log) | |||||||
| AUC | 16.36 | 9.71 | 16.40 | 9.99 | 16.23 | 8.83 | -- |
| CAR | 0.37 | 1.32 | 0.38 | 1.24 | 0.36 | 1.56 | -- |
| DEC | −0.16 | 0.09 | −0.15 | 0.08 | −0.17 | 0.10 | -- |
| Parent report | |||||||
| Praise child | 2.05 | 0.78 | 1.89 | 0.79 | 2.53 | 0.51 | −5.67*** |
| Physical affection | 2.57 | 0.67 | 2.47 | 0.72 | 2.86 | 0.36 | −4.32*** |
| Parent stress | 2.53 | 0.70 | 2.54 | 0.71 | 2.47 | 0.68 | 0.58 |
| Child report | |||||||
| Positive parenting | 3.48 | 0.56 | 3.43 | 0.58 | 3.62 | 0.51 | −2.02* |
| Negative parenting | 2.11 | 0.92 | 2.17 | 0.98 | 1.94 | 0.68 | 1.62 |
| Externalizing behavior | 6.63 | 5.75 | 6.83 | 6.07 | 6.03 | 4.66 | 0.78 |
| Internalizing behavior | 3.03 | 3.57 | 3.33 | 3.60 | 2.10 | 3.35 | 1.73 |
Note. The following data with errors were removed: children who provided their samples in the incorrect order, children who provided the 30 minute sample less than 15 minutes or more than 60 minutes after waking, children who were awake less than 12 or more than 20 hours, children who woke past noon, children for whom there was missing time of collection information, and children who provided saliva samples across different days rather than the same day. AUC = area under the curve, CAR = cortisol awakening response, DEC = daily decline.
p < .05,
p < .01,
p < .001
Table 3.
Correlations among main study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. AUC | -- | |||||||||
| 2. CAR | .22** | -- | ||||||||
| 3. DEC | .18* | −.38*** | -- | |||||||
| 4. Praise child | −.13 | .05 | −.07 | -- | ||||||
| 5. Physical affection | −.25** | .10 | −.25** | .48*** | -- | |||||
| 6. Parent stress | −.01 | −.02 | .16* | −.23** | −.23** | -- | ||||
| 7. Positive parenting | .05 | −.05 | −.00 | .05 | .08 | .10 | -- | |||
| 8. Negative parenting | .02 | −.08 | .17* | −.17* | −.04 | .16* | −.14 | -- | ||
| 9. Externalizing behavior | .18* | −.04 | .12 | −.18* | −.24** | .24** | −.21** | .03 | -- | |
| 10. Internalizing behavior | −.02 | −.02 | .01 | −.09 | −.16* | .23** | −.21** | .10 | .72*** | -- |
p < .05,
p < .01,
p < .001
Do Positive and Negative Aspects of Parenting Behavior Predict Variations in Children’s Cortisol?
First, we examined links between positive and negative aspects of parenting behavior and cortisol, but found very few significant main effects (Tables 4–6: Step 1). Consistent with our hypothesis, parents who reported more physical affection with their children had children with steeper DEC (Table 5) and lower AUC (Table 6). There were no associations between parenting behavior and CAR (Table 4).
Table 4.
Children’s CAR as a Function of Parent-Child Tie, Child Behavioral Problems, and Ethnicity
| Model 1 Internalizing | Model 2 Externalizing | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| n = 148 | b | SE | Adj. R2 | b | SE | Adj. R2 |
| Step 1 | ||||||
| Intercept | 0.24 | 0.14 | .02 | 0.24 | 0.14 | .03 |
| Child Behavior | −0.01 | 0.03 | −0.01 | 0.02 | ||
| Latinx | 0.07 | 0.14 | 0.06 | 0.14 | ||
| Parent Report | ||||||
| Praise | −0.07 | 0.17 | −0.08 | 0.17 | ||
| Physical affection | 0.27 | 0.18 | 0.26 | 0.18 | ||
| Stress | 0.03 | 0.16 | 0.05 | 0.16 | ||
| Child Report | ||||||
| Positive parent | −0.19 | 0.22 | −0.21 | 0.21 | ||
| Negative parent | −0.18 | 0.13 | −0.18 | 0.13 | ||
| Step 2 | ||||||
| Child Behavior x Praise | 0.05 | 0.05 | .02 | 0.00 | 0.03 | .02 |
| Child Behavior x Physical affection | 0.05 | 0.05 | .02 | 0.03 | 0.03 | .03 |
| Child Behavior x Stress | 0.01 | 0.04 | .02 | −0.01 | 0.03 | .02 |
| Child Behavior x Positive | 0.01 | 0.05 | .02 | −0.01 | 0.03 | .02 |
| Child Behavior x Negative | −0.08 | 0.03 | .05 | −0.02 | 0.02 | .03 |
| Step 3 | ||||||
| Ch. Beh x Praise x Lat. | 0.19 | 0.08 | .05 | 0.05 | 0.05 | .04 |
| Ch. Beh x Phys. Affection x Lat. | −0.90*** | 0.23 | .12 | 0.05 | 0.07 | .05 |
| Ch. Beh x Stress x Lat. | −0.14 | 0.05 | .06 | −0.02 | 0.04 | .03 |
| Ch. Beh x Positive x Lat. | −0.18 | 0.14 | .02 | −0.02 | 0.08 | .03 |
| Ch. Beh x Negative x Lat. | 0.00 | 0.08 | .03 | −0.08 | 0.04 | .06 |
Note. Models controlled for age and weekend cortisol. 2-way and 3-way interactions were tested in separate models. Models with 3-way interactions controlled for all relevant 2-way interactions. CAR = cortisol awakening response.
p < .0167,
p < .01,
p < .001
Table 6.
Children’s AUC as a Function of Parent-Child Tie, Child Behavioral Problems, and Ethnicity
| Model 1 Internalizing | Model 2 Externalizing | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| n = 143 | b | SE | Adj. R2 | b | SE | Adj. R2 |
| Step 1 | ||||||
| Intercept | 16.02*** | 0.98 | .09 | 16.00*** | 0.96 | .11 |
| Child Behavior | 0.04 | 0.24 | 0.31 | 0.15 | ||
| Latinx | −0.50 | 1.01 | −0.32 | 1.00 | ||
| Parent Report | ||||||
| Praise | −1.28 | 1.22 | −1.04 | 1.20 | ||
| Physical affection | −3.27* | 1.32 | −3.05 | 1.31 | ||
| Stress | −1.54 | 1.19 | −2.01 | 1.17 | ||
| Child Report | ||||||
| Positive parent | 1.34 | 1.57 | 1.86 | 1.53 | ||
| Negative parent | −0.54 | 0.95 | −0.49 | 0.93 | ||
| Step 2 | ||||||
| Child Behavior x Praise | −0.41 | 0.35 | .09 | −0.46* | 0.18 | .15 |
| Child Behavior x Physical affection | 0.17 | 0.37 | .08 | −0.47 | 0.22 | .14 |
| Child Behavior x Stress | 0.18 | 0.30 | .08 | 0.00 | 0.22 | .11 |
| Child Behavior x Positive | 0.24 | 0.35 | .08 | 0.26 | 0.19 | .12 |
| Child Behavior x Negative | 0.16 | 0.25 | .08 | −0.01 | 0.16 | .11 |
| Step 3 | ||||||
| Ch. Beh x Praise x Lat. | 0.62 | 0.57 | .10 | 0.15 | 0.36 | .15 |
| Ch. Beh x Phys. Affection x Lat. | 0.05 | 1.78 | .06 | 0.58 | 0.51 | .13 |
| Ch. Beh x Stress x Lat. | −0.07 | 0.37 | .07 | −0.04 | 0.31 | .09 |
| Ch. Beh x Positive x Lat. | −0.86 | 0.98 | .07 | −0.51 | 0.58 | .11 |
| Ch. Beh x Negative x Lat. | 0.28 | 0.57 | .09 | 0.11 | 0.28 | .11 |
Note. Models controlled for age and weekend cortisol. 2-way and 3-way interactions were tested in separate models. Models with 3-way interactions controlled for all relevant 2-way interactions. AUC = area under the curve.
p < .0167,
p < .01,
p < .001
Table 5.
Children’s DEC as a Function of Parent-Child Tie, Child Behavioral Problems, and Ethnicity
| Model 1 Internalizing | Model 2 Externalizing | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| n = 154 | b | SE | Adj. R2 | b | SE | Adj. R2 |
| Step 1 | ||||||
| Intercept | −0.16*** | 0.01 | .06 | −0.16*** | 0.01 | .06 |
| Child Behavior | −0.00 | 0.00 | 0.00 | 0.00 | ||
| Latinx | 0.01 | 0.01 | 0.00 | 0.01 | ||
| Parent Report | ||||||
| Praise | 0.02 | 0.01 | 0.02 | 0.01 | ||
| Physical affection | −0.04** | 0.01 | −0.03* | 0.01 | ||
| Stress | 0.01 | 0.01 | 0.01 | 0.01 | ||
| Child Report | ||||||
| Positive parent | 0.00 | 0.01 | 0.01 | 0.01 | ||
| Negative parent | 0.02 | 0.01 | 0.02 | 0.01 | ||
| Step 2 | ||||||
| Child Behavior x Praise | −0.00 | 0.00 | .05 | 0.00 | 0.00 | .06 |
| Child Behavior x Physical affection | 0.00 | 0.00 | .05 | −0.00 | 0.00 | .06 |
| Child Behavior x Stress | −0.00 | 0.00 | .05 | −0.00 | 0.00 | .07 |
| Child Behavior x Positive | 0.00 | 0.00 | .06 | 0.00 | 0.00 | .06 |
| Child Behavior x Negative | 0.00 | 0.00 | .06 | 0.00 | 0.00 | .06 |
| Step 3 | ||||||
| Ch. Beh x Praise x Lat. | 0.00 | 0.01 | .04 | 0.00 | 0.00 | .06 |
| Ch. Beh x Phys. Affection x Lat. | 0.04* | 0.02 | .13 | 0.01** | 0.00 | .18 |
| Ch. Beh x Stress x Lat. | 0.00 | 0.00 | .04 | 0.00 | 0.00 | .08 |
| Ch. Beh x Positive x Lat. | 0.00 | 0.01 | .04 | 0.00 | 0.00 | .06 |
| Ch. Beh x Negative x Lat. | 0.00 | 0.01 | .05 | 0.01** | 0.00 | .12 |
Note. Models controlled for age and weekend cortisol. 2-way and 3-way interactions were tested in separate models. Models with 3-way interactions controlled for all relevant 2-way interactions. DEC = daily decline.
p < .0167,
p < .01,
p < .001
Does the Link between Positive and Negative Aspects of Parenting Behavior and Cortisol vary by Children’s Behavioral Problems?
Next, we assessed whether interactions between positive and negative aspects of parenting and child behavioral problems vary when predicting children’s cortisol (Tables 4–6: Step 2). The average natural log values of the three diurnal cortisol measures are found in Table 2. There was a two-way interaction between parent reports of praise and child externalizing behavioral problems predicting AUC (Table 6). As hypothesized, more praise was associated with lower AUC among children with greater externalizing problems (b = −3.33, p < .05). The sample average AUC was a natural log of 16.4, but children with high externalizing behaviors and lower parent reports of praise had an AUC around 20, whereas children with higher parent reports of praise had an AUC closer to 15 (see Figure 1). The slope for those with low externalizing problems was not significant. There were no other two-way interactions between the parenting behavior and behavioral problems predicting cortisol.
Figure 1.
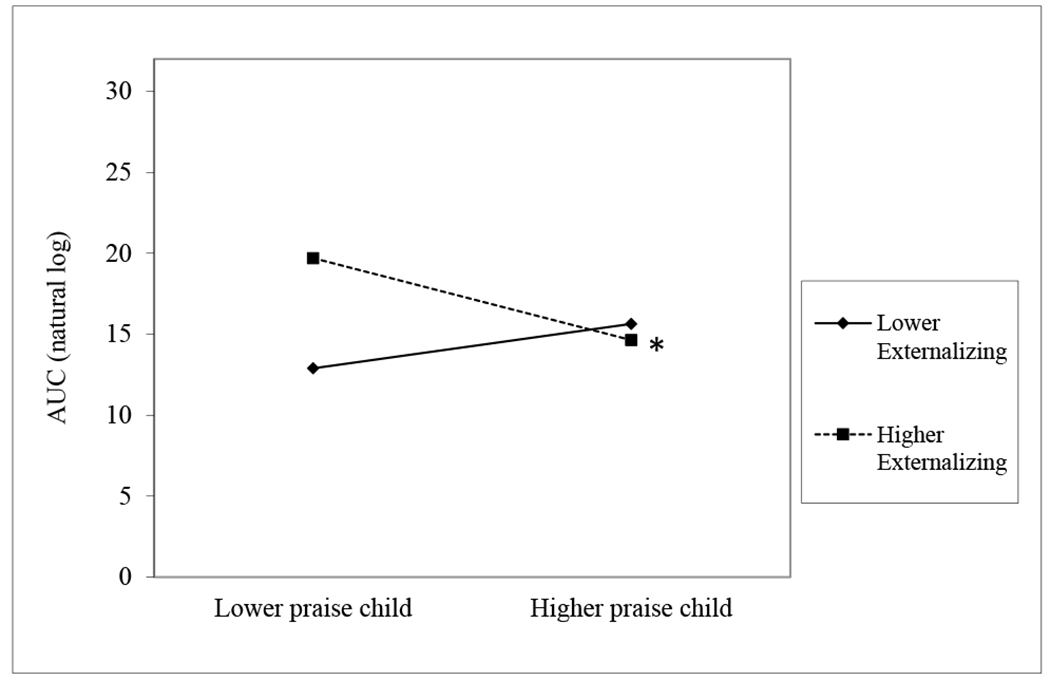
Parenting Behavior, Child Behavioral Problems, and Cortisol
Do Links among Positive and Negative Aspects of Parenting Behavior, Child Behavioral Problems, and Cortisol vary by Ethnicity?
We then assessed whether associations among positive and negative aspects of parenting, child behavioral problems, and children’s cortisol vary by ethnicity (Tables 4–6: Step 3; see Table 2 for the average natural log values of the cortisol measures). There were significant three-way interactions among parent reports of physical affection, internalizing behavioral problems, and ethnicity predicting CAR and DEC that were inconsistent with our hypotheses. More physical affection was associated with a steeper CAR among non-Latinx White children with greater internalizing problems (b = 11.06, p < .001) and a flatter CAR among non-Latinx White children with lower internalizing problems (b = −1.95, p < .05; Figure 2a). The average CAR for non-Latinx White children was a natural log of 0.36, but children with greater internalizing problems and more physical affection from parents had a CAR around 3, whereas children non-Latinx White children with lower internalizing problems and more physical affection from parents had a CAR slightly less than 0 (see Figure 2a). Further, more physical affection was associated with a steeper DEC among Latinx (b = −0.03, p < .05) and non-Latinx White children with greater internalizing problems albeit to a greater degree among non-Latinx White children (b = −0.57, p < .01). The average DEC for Latinx children was a natural log of −0.15, but Latinx children with greater internalizing problems and more physical affection from parents had a DEC of −0.16 (see Figure 2b). The average DEC for non-Latinx White children was a natural log of −0.17, but non-Latinx White children with greater internalizing problems and more physical affection from parents had a DEC of −0.26.
Figure 2.
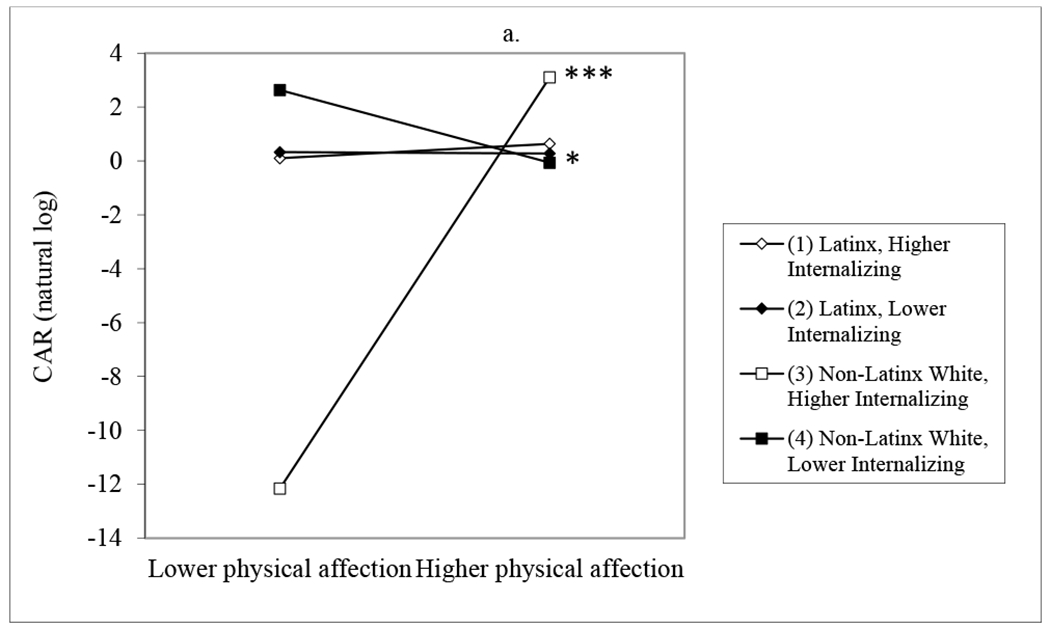
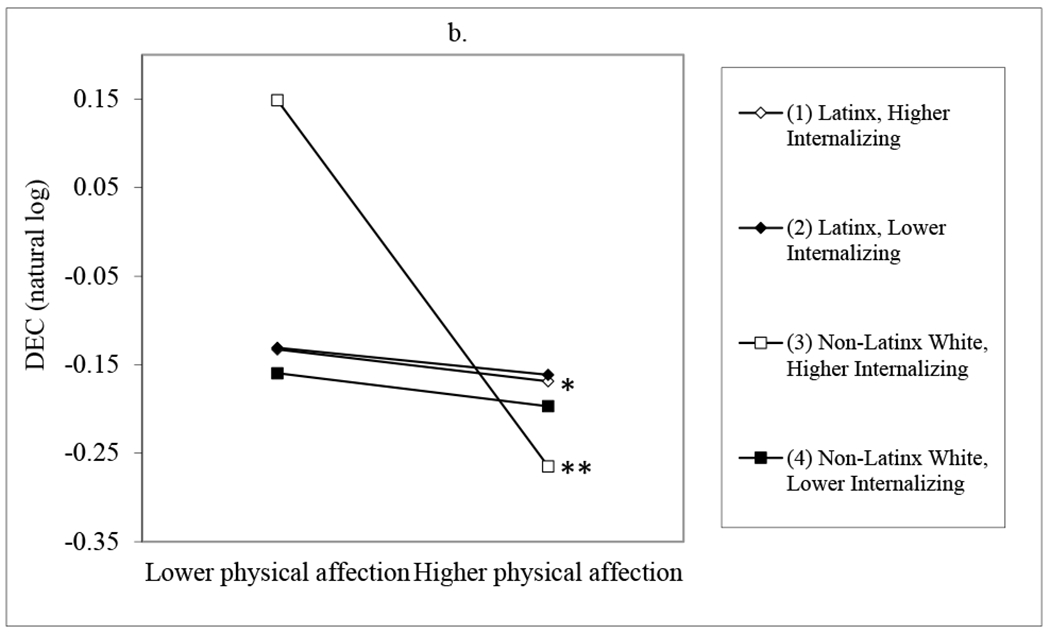
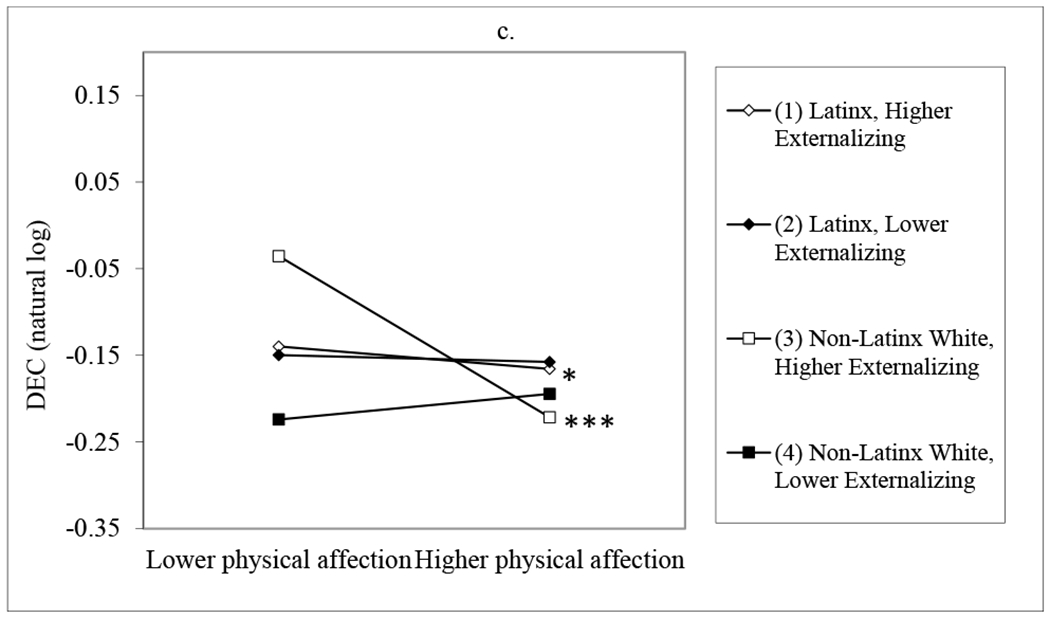
Parenting Behavior, Child Behavioral Problems, and Cortisol by Ethnicity
There was also an interaction among parent reports of physical affection, child externalizing behavioral problems, and ethnicity predicting DEC. Greater physical affection was associated with a steeper DEC among Latinx (b = −0.03, p < .05) and non-Latinx White children (b = −0.29, p < .001) with more externalizing problems but to a greater degree among non-Latinx White children, which does not support our hypothesis. Latinx children with more externalizing problems and greater physical affection had a natural log DEC of −0.16 compared to the average of −0.15 and non-Latinx White children with more externalizing problems and greater physical affection had a natural log DEC of −0.22 compared to their average of −0.17 (see Figure 2c).
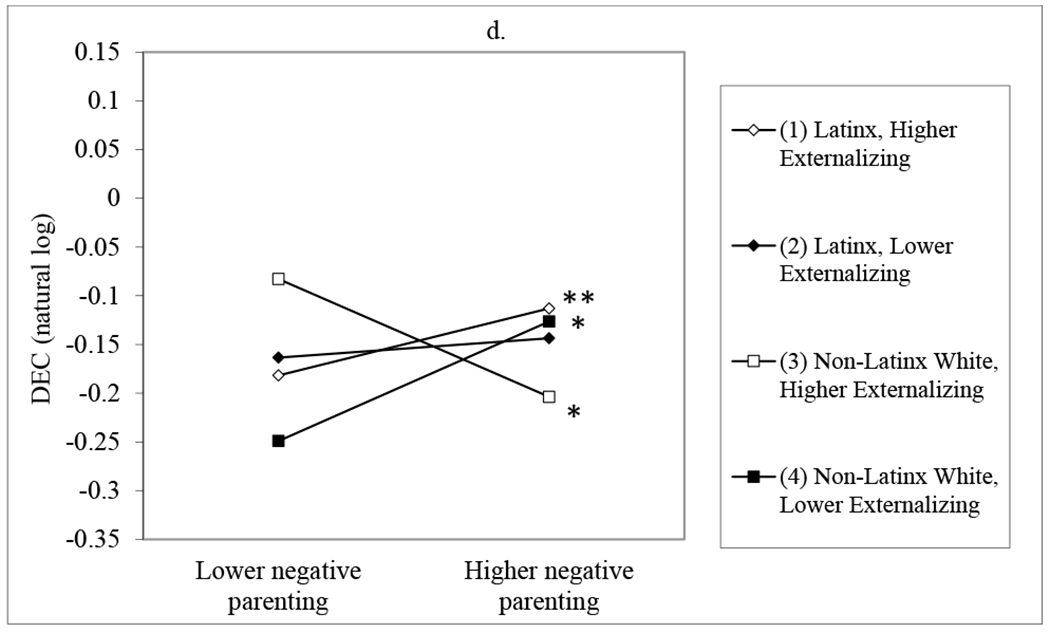
Lastly, there was an interaction among child reports of negative parenting, child externalizing behavioral problems, and ethnicity predicting DEC. As hypothesized, more negative parenting was associated with a flatter DEC among Latinx children with greater externalizing behaviors (b = 0.04, p < .01). Latinx children with greater externalizing behaviors and more negative parenting had a natural log DEC of −0.11 compared to their average of −0.15. Inconsistent with our hypothesis, more negative parenting was associated with a steeper DEC for non-Latinx White children with greater externalizing behaviors (b = −0.07, p < .05). Non-Latinx White children with greater externalizing behaviors and more negative parenting had a natural log DEC of −0.20 compared to their average of −0.17. More negative parenting was associated with a flatter DEC among non-Latinx White children with less externalizing behaviors (b = 0.07, p < .05). Non-Latinx White children with less externalizing behaviors and more negative parenting had a natural log DEC of −0.13 compared to their average of −0.17 (see Figure 2d).
Sensitivity and Posthoc Analyses
We conducted sensitivity analyses to model the diurnal cortisol decline using the wake-to-bed slope method, which eliminates cortisol awakening response variance. This method captures the change in cortisol from immediately upon waking to late evening or bedtime (Adam et al., 2017). Using the wake-to-bed slope measure, there was one significant three-way interaction among parent report of physical affection, externalizing behavioral problems, and ethnicity predicting decline. More physical affection was associated with a steeper wake-to-bed slope among non-Latinx White children with more externalizing problems (b = −0.27, p < .001). The association was not significant for Latinx children or non-Latinx White children with less externalizing problems. This finding indicates that it is important to consider the CAR as well as DEC when examining the associations between parenting, behavioral problems, and cortisol. The majority of children had primary caregivers who were their biological mothers (n = 148) with a smaller subsample consisting of fathers, other relatives, and foster parents (n = 11). We conducted posthoc analyses to only include children whose biological mother was their primary caregiver to determine if results would be similar without the non-biological mother caregivers. One new finding emerged among mothers’ reports of stress, internalizing behavioral problems, and ethnicity predicting CAR. More maternal stress was marginally associated with a steeper CAR among non-Latinx White children with more internalizing problems (b = 0.89, p = .085). More maternal stress was marginally associated with a flatter CAR among non-Latinx White children with less internalizing problems (b = −0.82, p = .084).
Discussion
Consistent with the biopsychosocial model and biological sensitivity-to-context theory, parenting was related to children’s HPA axis functioning and children with behavioral problems appeared to be more sensitive to the positive and negative aspects of their parent’s behavior. In addition, these links varied by ethnicity as White children were more reactive to their environment than non-White Latinx children.
Positive and Negative Aspects of Parenting Behavior and Children’s Cortisol
This study used both parents’ and children’s reports of positive and negative parenting behavior and found few direct associations between parenting and children’s cortisol. Children with parents who reported more physical affection had steeper daily decline and lower overall cortisol scores over the course of the day consistent with the hypercortisolism hypothesis. Thus, positive parent-child relations were associated with cortisol levels indicating lower levels of stress. Our hypothesis regarding negative parenting behavior and decline was not supported which is inconsistent with previous studies showing that children exposed to negative parenting have flatter cortisol curves (Fisher et al., 2007; Pendry & Adam, 2007). Much of the previous research on negative parenting behaviors has focused on extreme forms of harsh caregiving (e.g., Cicchetti, 2010). This study, however, used parental stress and parents’ contempt of children’s ideas to characterize negative parenting. These two items are more normative experiences of families unlike the severe maltreatment studied in prior research that demonstrated effects on children’s cortisol. Less severe, but more common, negative parenting behaviors may have less of an influence on children’s cortisol response compared to more extreme behavior.
Positive and Negative Aspects of Parenting Behavior, Cortisol, and Behavioral Problems
Children with externalizing behavioral problems, but not internalizing behavior problems, appeared to be more sensitive to the quality of parent’s behavior. As expected, children with greater externalizing behavioral problems seemed to benefit more from positive parenting compared to children with lower levels of externalizing problems. However, children with greater externalizing problems only had lower overall cortisol levels when their parents reported praising them, rather than when providing physical affection. These findings add important evidence to the conflicting literature on whether verbal and nonverbal parental responses are more or less beneficial for children with externalizing behavior (Owen, Slep, & Heyman, 2012). Parents who rate their children as having more externalizing behavior problems are often less likely to report praising their child (Swenson et al., 2016). However, Ware and colleagues (2008) found that increased parental praise led to increased child compliance in children with behavior issues after parents participated in a training course. Children with externalizing behavior problems may be especially responsive, both behaviorally and physiologically, to verbal praise that they do not often receive. Parents, as well as behavioral training programs, should consider children’s differential responses to parenting based on their emotion state and regulation.
Parenting Behavior, Child Behavioral Problems, and Cortisol varies by Ethnicity
Contrary to our hypotheses, there were far more similarities than differences between the non-Latinx White and the Latinx samples. There were no differences in cortisol, negative aspects of parenting, or child behavioral problems by ethnicity. Yet, non-Latinx White parents reported more positive parenting behavior (i.e., praise and physical affection) than Latinx parents, which may be reflective of external stressors. Latinx families may have reported lower positive parenting because they often experience high levels of social and financial disadvantage and discrimination, particularly when compared to non-Latinx White families (García Coll & Pachter, 2005; Leidy et al., 2010; Lorenzo-Blanco et al., 2016). According to social information processing theory, parents with high stress may assess their child’s behavior more negatively than they would in more relaxed, less stressful conditions (Crick & Dodge, 1994). Research demonstrates that in Latinx families, stress is related to less praise and more negative parenting behaviors (Planos, Zayas, & Busch-Rossnagel, 1997; Uno, Florsheim, & Uchino, 1998). Additionally, Latinx families may express love and support in ways that are not captured by survey measures based on primarily White samples.
Our hypothesis that the associations among positive parent-child dimensions, behavioral problems, and cortisol would vary by ethnicity (i.e., appearing stronger among Latinx children) was mostly unsupported. Consistent with hypercortisolism, greater physical affection was associated with steeper decline among both Latinx and non-Latinx White children with greater externalizing and internalizing behavior problems but the links were stronger among non-Latinx White children. More physical affection was associated with a steeper awakening response among non-Latinx White children with greater internalizing problems. It appears that positive parenting is particularly beneficial for the stress response of children with behavioral problems.
Interestingly, children’s reports of negative parenting had the opposite association with daily decline in cortisol among Latinx and non-Latinx White children with externalizing problems. Greater negative parenting was associated with a steeper decline for non-Latinx White children with high externalizing behavior problems but a flatter decline among Latinx children with high externalizing problems. With mixed support for the hyper and hypocortisolism hypotheses, prior applications of these frameworks may not have considered the role of ethnicity, cultural parenting differences, and societal context.
Overall, non-Latinx White children appeared to be more sensitive to parenting than their Latinx counterparts, which was inconsistent with our hypothesis. However, previous research noted that Latinx youth have flatter diurnal cortisol slopes compared to White youth, which may be due to experiences of discrimination (Deer, Shields, Ivory, Hostinar, & Telzer, 2018). Indeed, Latinx families often experience stressors such as experiencing prejudice and discrimination, navigating the dominant culture, low socioeconomic status, residential segregation, and/or struggling with language barriers (Deer et al., 2019; García Coll & Pachter, 2005). Exposure to chronic stress may lead Latinx children to exhibit a blunted or nonreactive stress response to parenting. Non-Latinx White children may be more reactive as they have not had to respond to these culturally bound stressors. Further, the cultural assets of Latinx families may influence their children’s response to stress. For example, Latinx families emphasize solidarity, reciprocal support, and warm, interpersonal connection (Cauce & Domenech-Rodríguez, 2002). Positive parenting and family cohesion predict improvements in child social self-efficacy (Leidy et al., 2010). More research is warranted to clarify why these associations varied by ethnicity as well as how protective cultural factors play a role in Latinx children’s responses to stress.
Limitations and Future Directions
There are several limitations to this study that provide important directions for future research. First, associations among characteristics of parenting, child behavioral problems, and children’s stress response as measured by cortisol are most likely multidirectional. Cortisol data should be collected from multiple days to examine within-person associations among daily family interactions, behavioral problems, and cortisol. This is difficult, however, in large-scale epidemiological studies when one additional saliva sample results in significant financial costs (Adam & Kumari, 2009). Adding saliva samples can also increase participant burden, especially for children, and impact protocol adherence and study retention (Adam & Kumari, 2009). Lastly, it is important to note that findings on diurnal cortisol rhythm varied depending on type of slope calculated (peak-to-bed compared to wake-to-bed). Findings on daily decline are important contributions to the literature but should be interpreted with caution.
An interesting next step would be to examine father reports and their implications for children’s cortisol as there were very few fathers in the data. Another factor that may influence diurnal cortisol rhythms is pubertal stage but there was no measure of puberty in the dataset for the present study. Additionally, future work should include younger children as well as older adolescents to assess whether these associations vary across developmental stage (Adam et al., 2007). Lastly, the generalizability of findings should be interpreted cautiously as the selected and non-selected samples had a few notable differences (i.e., selected sample had less parental stress and children were older and predominately White). Future research should include samples of parents with more stress and children who are younger and who identify as non-White Latinx.
As previously mentioned, Latinx families possess many strengths but often encounter stressful societal challenges that affect their relationships and health (Leidy et al., 2010; Lorenzo-Blanco et al., 2016). A future step in this research would be to consider the measures of neighborhood contextual exposures available in the L.A.FANS, which likely include substantial variation in exposure to stressors associated with poverty, crime, and safety. Lastly, going beyond Latinx-White comparisons and exploring the rich heterogeneity within and between Latinx subgroups is another important future direction (Cauce & Domenech-Rodríguez, 2002).
Overall, these findings suggest that the HPA axis is linked in important ways to parent and child behavior. Children who have behavioral problems appear to benefit more from positive parenting and these associations are even greater among non-Latinx White children than among Latinx children. Further research on Latinx children is needed to better understand the contextual factors that are important for their physiology.
Acknowledgments
We have no known conflict of interest to disclose. This research is based on data from the Los Angeles Family and Neighborhood Survey, which was funded by grants R01 HD35944 and R01 HD049865 from the National Institute of Child Health and Human Development and grant R01 ES013907 from the National Institute of Environmental Health Sciences to RAND in Santa Monica, California. For further information on L.A.FANS, go to lasurvey.rand.org.
References
- Adam EK, & Kumari M (2009). Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology, 34, 1423–1436. [DOI] [PubMed] [Google Scholar]
- Adam EK, Doane LD, Zinbarg RE, Mineka S, Craske MG, & Griffith JW (2010). Prospective prediction of major depressive disorder from cortisol awakening responses in adolescence. Psychoneuroendocrinology, 35, 921–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam EK, Klimes-Dougan B, & Gunnar MR (2007). Social regulation of the adrenocortical response to stress in infants, children, and adolescents. In Coch D, Dawson G, & Fischer KW (Eds.), Human behavior, learning, and the developing brain: Atypical development (pp. 264–304). The Guilford Press. [Google Scholar]
- Adam EK, Quinn ME, Tavernier R, McQuillan MT, Dahlke KA, & Gilbert KE (2017). Diurnal cortisol slopes and mental and physical health outcomes: A systematic review and meta-analysis. Psychoneuroendocrinology, 83, 25–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alink LR, Cicchetti D, Kim J, & Rogosch FA (2013). Longitudinal associations among child maltreatment, social functioning, and cortisol regulation. Developmental Psychology, 48, 224–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida DM, Piazza JR, & Stawski RS (2009). Interindividual differences and intraindividual variability in the cortisol awakening response: An examination of age and gender. Psychology and Aging, 24, 819–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azak S, Murison R, Wentzel-Larsen T, Smith L, & Gunnar MR (2013). Maternal depression and infant daytime cortisol. Developmental Psychobiology, 55(4), 334–351. [DOI] [PubMed] [Google Scholar]
- Bender R, & Lange S (2001). Adjusting for multiple testing—When and how? Journal of Clinical Epidemiology, 54, 343–349. [DOI] [PubMed] [Google Scholar]
- Birditt KS, Kim K, Zarit SH, Fingerman KL, & Loving TJ (2016). Daily interactions in the parent–adult child tie: Links between children’s problems and parents’ diurnal cortisol rhythms. Psychoneuroendocrinology, 63, 208–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt KS, Manalel JA, Kim K, Zarit SH, & Fingerman KL (2017). Daily interactions with aging parents and adult children: Associations with negative affect and diurnal cortisol. Journal of Family Psychology, 31, 699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth A, Granger DA, & Shirtcliff EA (2008). Gender-and age-related differences in the association between social relationship quality and trait levels of salivary cortisol. Journal of Research on Adolescence, 18, 239–260. [Google Scholar]
- Boyce WT, & Ellis BJ (2005). Biological sensitivity to context: I. An evolutionary–developmental theory of the origins and functions of stress reactivity. Development and Psychopathology, 17(2), 271–301. [DOI] [PubMed] [Google Scholar]
- Brown SM, Schlueter LJ, Hurwich-Reiss E, Dmitreiva J, Miles E & Watamura SE (2020). Parental buffering in the context of poverty: Positive parenting behaviors differentiate young children’s stress reactivity profiles. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. (n.d.). National Longitudinal Survey of Youth: 1997 cohort. Retrieved from https://www.nlsinfo.org/content/cohorts/nlsy97 [Google Scholar]
- Cauce AM, & Domenech-Rodríguez M (2002). Latino families: Myths and realities. In Contreras JM, Kerns KA, & Neal-Barnett AM (Eds.), Praeger series in applied psychology. Latino children and families in the United States: Current research and future directions (p. 3–25). Praeger Publishers/Greenwood Publishing Group. [Google Scholar]
- Cheadle JE, Goosby BJ, Jochman JC, Tomaso CC, Yancey CBK, & Nelson TD (2020). Race and ethnic variation in college students’ allostatic regulation of racism-related stress. Proceedings of the National Academy of Sciences, 117(49), 31053–31062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Child Trends. (2018). Racial and ethnic composition of the child population. Retrieved from https://www.childtrends.org/indicators/racial-and-ethnic-composition-of-the-child-population. [Google Scholar]
- Cicchetti D, & Rogosch FA (2001). The impact of child maltreatment and psychopathology on neuroendocrine functioning. Development and Psychopathology, 13(4), 783–804. [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Gunnar MR, & Toth SL (2010). The differential impacts of early physical and sexual abuse and internalizing problems on daytime cortisol rhythm in school-aged children. Child Development, 81, 252–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crick NR, & Dodge KA (1994). A review and reformulation of social information-processing mechanisms in children’s social adjustment. Psychological Bulletin, 115, 74–101. [Google Scholar]
- Dawson JF (2014). Moderation in management research: What, why, when and how. Journal of Business and Psychology, 29, 1–19. [Google Scholar]
- Deer LK, Shields GS, Ivory SL, Hostinar CE, & Telzer EH (2018). Racial/ethnic disparities in cortisol diurnal patterns and affect in adolescence. Development and Psychopathology, 30(5), 1977–1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePasquale CE, Raby KL, Hoye J, & Dozier M (2018). Parenting predicts strange situation cortisol reactivity among children adopted internationally. Psychoneuroendocrinology, 89, 86–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson SS, & Kemeny ME (2004). Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin, 130, 355–391. [DOI] [PubMed] [Google Scholar]
- Figge CJ, Martinez-Torteya C, & Kosson DS (2021). Parent cultural stress and internalizing problems in Latinx preschoolers: Moderation by maternal involvement and positive verbalizations. Journal of Immigrant and Minority Health, 1–10. [DOI] [PubMed] [Google Scholar]
- Fisher D, Serbin LA, Stack DM, Ruttle PL, Ledingham JE, & Schwartzman AE (2007). Intergenerational predictors of diurnal cortisol secretion in early childhood. Infant and Child Development, 16, 151–170. [Google Scholar]
- Fries E, Dettenborn L, & Kirschbaum C (2009). The cortisol awakening response (CAR): facts and future directions. International Journal of Psychophysiology, 72, 67–73. [DOI] [PubMed] [Google Scholar]
- Fries E, Hesse J, Hellhammer J, & Hellhammer DH (2005). A new view on hypocortisolism. Psychoneuroendocrinology, 30(10), 1010–1016. [DOI] [PubMed] [Google Scholar]
- García Coll C & Pachter LM (2005). Ethnic and minority parenting. In Bornstein M(Ed.), Handbook of parenting: Social conditions and applied parenting (Vol. 4, pp. 1–20). Lawrence Erlbaum Associates Inc. [Google Scholar]
- Goodyer IM, Tamplin A, Herbert J, & Altham PME (2000). Recent life events, cortisol, dehydroepiandrosterone and the onset of major depression in high-risk adolescents. The British Journal of Psychiatry, 177, 499–504. [DOI] [PubMed] [Google Scholar]
- Halligan SL, Herbert J, Goodyer IM, & Murray L (2004). Exposure to postnatal depression predicts elevated cortisol in adolescent offspring. Biological Psychiatry, 55(4), 376–381. [DOI] [PubMed] [Google Scholar]
- Hofferth SL, Davis-Kean PE, Davis J, & Finkelstein J (1998). Child development supplement to the Panel Study of Income Dynamics: 1997 user guide. Institute for Social Research, University of Michigan. 10.1111/j.1467-8624.2009.01305.x [DOI] [Google Scholar]
- Klimes-Dougan B, Hastings PD, Granger DA, Usher BA, & Zahn-Waxler C (2001). Adrenocortical activity in at-risk and normally developing adolescents: Individual differences in salivary cortisol basal levels, diurnal variation, and responses to social challenges. Development and Psychopathology, 13, 695–719. [DOI] [PubMed] [Google Scholar]
- Leidy MS, Guerra NG, & Toro RI (2010). Positive parenting, family cohesion, and child social competence among immigrant Latino families. Journal of Family Psychology, 24(3), 252. [DOI] [PubMed] [Google Scholar]
- Lorenzo-Blanco EI, Meca A, Unger JB, Romero A, Gonzales-Backen M, Piña-Watson B, & Schwartz SJ (2016). Latino parent acculturation stress: Longitudinal effects on family functioning and youth emotional and behavioral health. Journal of Family Psychology, 30(8), 966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupien SJ, King S, Meaney MJ, & McEwen BS (2000). Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biological Psychiatry, 48(10), 976–980. [DOI] [PubMed] [Google Scholar]
- McCord AL, Draucker CB, & Bigatti S (2019). Cultural stressors and depressive symptoms in Latino/a adolescents: An integrative review. Journal of the American Psychiatric Nurses Association, 25(1), 49–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS, & Seeman T (1999). Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences, 896, 30–47. [DOI] [PubMed] [Google Scholar]
- O’Neal CR, Brotman LM, Huang KY, Gouley KK, Kamboukos D, Calzada EJ, & Pine DS (2010). Understanding relations among early family environment, cortisol response, and child aggression via a prevention experiment. Child Development, 81, 290–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen DJ, Slep AM, & Heyman RE (2012). The effect of praise, positive nonverbal response, reprimand, and negative nonverbal response on child compliance: A systematic review. Clinical Child and Family Psychology Review, 15, 364–385. [DOI] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, & Gee G. (2015). Racism as a determinant of health: a systematic review and meta-analysis. PloS One, 10(9), e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passel JS, Cohn D, & Lopez MH (2011). Hispanics account for more than half of nation’s growth in past decade. Retrieved from https://www.pewresearch.org/hispanic/2011/03/24/hispanics-account-for-more-than-half-of-nations-growth-in-past-decade/ [Google Scholar]
- Pebley AR, & Sastry N (2019). Los Angeles Family and Neighborhood Survey (L.A.FANS), Wave 2, Public Data, 2006–2008. Inter-university Consortium for Political and Social Research [distributor], 2019-07-22. 10.3886/ICPSR37278.v1 [DOI] [Google Scholar]
- Pendry P, & Adam EK (2007). Associations between parents’ marital functioning, maternal parenting quality, maternal emotion and child cortisol levels. International Journal of Behavioral Development, 31, 218–231. [Google Scholar]
- Peterson JL, & Zill N (1986). Marital disruption, parent-child relationships, and behavior problems in children. Journal of Marriage and the Family. 48, 295–307. [Google Scholar]
- Pettit GS, Bates JE, & Dodge KA (1997). Supportive parenting, ecological context, and children’s adjustment: A seven-year longitudinal study. Child Development, 68, 908–923. [DOI] [PubMed] [Google Scholar]
- Planos R, Zayas LH, & Busch-Rossnagel NA (1997). Mental health factors and teaching behaviors among low-income Hispanic mothers. Families in Society: The Journal of Contemporary Social Services, 78, 4–12. [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, & Hellhammer DH (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change.Psychoneuroendocrinology, 28, 916–931. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, Kaspers F, Kirschbaum C (1997). Free cortisol levels after awakening: A reliable biological marker for the assessment of adrenocortical activity. Life Sciences, 61, 2539–2549. [DOI] [PubMed] [Google Scholar]
- Raby KL, Bernard K, Gordon MK, & Dozier M (2020). Enhancing diurnal cortisol regulation among young children adopted internationally: A randomized controlled trial of a parenting-based intervention. Development and Psychopathology, 32(5), 1657–1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roisman GI, Susman E, Barnett-Walker K, Booth-LaForce C, Owen MT, Belsky J, & The NICHD Early Child Care Research Network. (2009). Early family and child-care antecedents of awakening cortisol levels in adolescence. Child Development, 80(3), 907–920. [DOI] [PubMed] [Google Scholar]
- Ruttle PL, Shirtcliff EA, Serbin LA, Ben-Dat Fisher D, Stack DM, Schwartzman AE. Disentangling psychobiological mechanisms underlying internalizing and externalizing behaviors in youth: longitudinal and concurrent associations with cortisol. Horm. Behav 2011;59:123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, & Munck AU (2000). How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews, 21, 55–89. [DOI] [PubMed] [Google Scholar]
- Saridjan NS, Velders FP, Jaddoe VW, Hofman A, Verhulst FC, & Tiemeier H (2014). The longitudinal association of the diurnal cortisol rhythm with internalizing and externalizing problems in pre-schoolers. The Generation R Study. Psychoneuroendocrinology, 50, 118–129. [DOI] [PubMed] [Google Scholar]
- Shaw BA, Krause N, Chatters LM, Connell CM, & Ingersoll-Dayton B (2004). Emotional support from parents early in life, aging, and health. Psychology and Aging, 19, 4–12. [DOI] [PubMed] [Google Scholar]
- Spies LA, Margolin G, Susman EJ, & Gordis EB (2011). Adolescents’ cortisol reactivity and subjective distress in response to family conflict: The moderating role of internalizing symptoms. Journal of Adolescent Health, 49, 386–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swenson S, Ho GW, Budhathoki C, Belcher HM, Tucker S, Miller K, & Gross D (2016). Parents’ use of praise and criticism in a sample of young children seeking mental health services. Journal of Pediatric Health Care, 30(1), 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, Repetti RL, & Seeman T (1997). Health psychology: What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology, 48, 411–447. [DOI] [PubMed] [Google Scholar]
- Troxel WM, & Matthews KA (2004). What are the costs of marital conflict and dissolution to children’s physical health?. Clinical Child and Family Psychology Review, 7, 29–57. [DOI] [PubMed] [Google Scholar]
- Uno D, Florsheim P, & Uchino BN (1998). Psychosocial mechanisms underlying quality of parenting among Mexican-American and White adolescent mothers. Journal of Youth and Adolescence, 27, 585–605. [Google Scholar]
- Van Ryzin MJ, Chatham M, Kryzer E, Kertes DA, & Gunnar MR (2009). Identifying atypical cortisol patterns in young children: The benefits of group-based trajectory modeling. Psychoneuroendocrinology, 34, 50–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware LM, McNeil CB, Masse J, & Stevens S (2008). Efficacy of in-home parent–child interaction therapy. Child & Family Behavior Therapy, 30, 99–126 [Google Scholar]
- Wolf JM, Nicholls E, & Chen E (2008). Chronic stress, salivary cortisol, and α-amylase in children with asthma and healthy children. Biological Psychology, 78, 20–28. [DOI] [PubMed] [Google Scholar]
- Wu S, Marsiglia FF, Ayers S, Cutrín O, & Vega-López S (2020). Familial acculturative stress and adolescent internalizing and externalizing behaviors in Latinx immigrant families of the Southwest. Journal of Immigrant and Minority Health, 22(6), 1193–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]


