Abstract
Primary tumors of the omentum, let alone omental lipomas, are rare causes of a large intra-abdominal mass. We report a case of an adult male presenting with an intra-abdominal mass, representative of a giant omental lipoma radiologically, confirmed on histopathology after complete resection at laparotomy. The case highlights the preoperative workup of a suspected omental lipoma, including the utility of various radiological modalities in differentiating from malignant pathologies, and anatomical characterization of the lesion for surgical planning.
INTRODUCTION
Primary tumors of the omentum, let alone omental lipomas, are rare causes of a large intra-abdominal mass limited to case reports in the literature [1–4]. Differentiation between benign and malignant etiologies as well as anatomical characterization of the lesion are paramount in guiding surgical management. We report on a case of a giant omental lipoma in an adult male presenting as a large intra-abdominal mass and the preoperative investigation undertaken, including the utility of different radiological modalities.
CASE REPORT
A 36-year-old male presented with several months of dull abdominal pain and fullness. There were no other significant symptoms. His past medical history was unremarkable. Examination revealed a soft abdomen with no discrete mass palpable. Blood cell counts and biochemistry were within normal limits.
Abdominal ultrasound (US) revealed a well-demarcated, mildly hyperechogenic mass lesion apparently occupying the left lobe of the liver and measuring 6 × 25 × 24 cm. Both contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) demonstrated a well-circumscribed lipomatous mass within the greater omentum, measuring 9 × 24 × 27 cm, without discrete enhancing soft tissue components or local invasive features (Fig. 1). There were several foci of internal coarse calcification on CT corresponding with areas of low T1 and T2 signals and thin peripheral rim enhancement on MRI suggestive of focal fat necrosis. Intra-abdominal mass effect was evident but without acute complications. No metabolically active disease was demonstrated on fluorodeoxyglucose positron emission tomography (FDG-PET) (Fig. 2).
Figure 1.
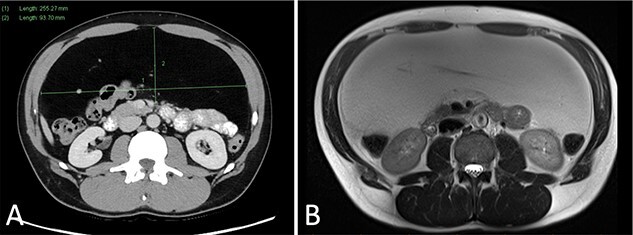
(A) CT portal venous phase axial slice demonstrating a well-circumscribed lipomatous lesion within the greater omentum measuring 9 × 26 × 24 cm; (B) MRI T2-weighted axial slice demonstrating intermediate T2 signal of the lesion.
Figure 2.
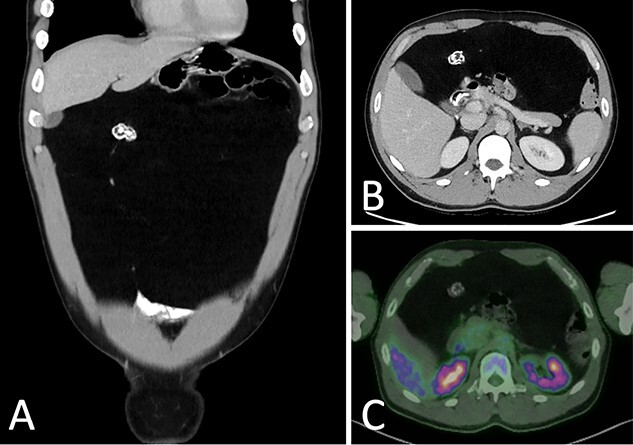
CT portal venous phase (A) coronal slice (B) axial slice demonstrating a focus of coarse calcification and intra-abdominal mass effect; (C) FDG-PET CT axial slice demonstrating a non-metabolically active lesion.
Given the rarity of omental lesions and possibility of a malignant process, the patient was discussed in a surgical oncology multidisciplinary meeting. A consensus for curative surgical resection without prior biopsy was reached, given the radiological findings and bleeding risk of biopsy. At laparotomy, the mass was confirmed to arise from the greater omentum, which was easily separated from the transverse colon and transected with a margin of macroscopically normal tissue using a LigaSure.
Macroscopic examination revealed a 3.35-kg yellow, thinly encapsulated lipomatous mass measuring 7 × 29 × 24 cm (Fig. 3). On histopathology, mature adipocytes were present with focal areas of fat necrosis. No atypical features or lipoblasts were identified. These findings were consistent with an omental lipoma.
Figure 3.
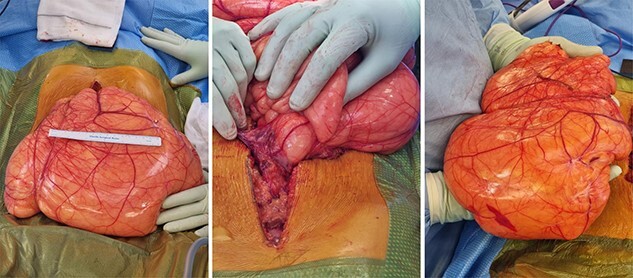
Large lipomatous mass arising from the greater omentum, measuring 7 × 29 × 24 cm and weighing 3.35 kg.
DISCUSSION
Lipomas are benign, encapsulated tumors comprised of mature adipocytes. While collectively they are common mesenchymal tumors capable of arising from any part of the body, omental lipomas are rare and limited to case reports in the literature [1].
Presentations of omental lipoma are non-specific and variable, depending on the size, location and presence of complications. They may be asymptomatic and are found incidentally on physical examination or radiological imaging [1]. A protracted course of progressive symptoms is often due to the intra-abdominal mass effect and include abdominal pain, distention, early satiety, anorexia, vomiting and constipation [5]. Acute presentations typically reflect complications, with reports in the literature of torsion and infarction of the lipoma, exacerbation of hernias and intra-abdominal hemorrhage from aberrant vessels [2, 3, 6, 7].
Differential diagnoses to consider for primary omental tumors include benign and malignant pathologies, such as leiomyoma, fibroma, leiomyosarcoma, fibrosarcoma, liposarcoma and mesothelioma [5]. While rare altogether, they are most commonly of smooth muscle origin, accounting for 37% of cases, compared to omental lipomas making up for 7–9% of cases [1, 3]. However, lipomatous lesions >5 cm or in deep-seated locations have an increased risk of being malignant [8]. For these reasons, multidisciplinary input and additional imaging with MRI and FDG-PET assists in further characterizing the nature of the lesion, its anatomical relations and guide subsequent management [6, 9].
US typically demonstrates a well-demarcated, homogenous lesion with increased echogenicity. On CT, a lesion with fat attenuation values is seen, and thin fibrous septations and calcifications may be present [4]. On MRI, there is homogenous high T1 and intermediate T2 signals consistent with fat, while thin, fibrous intra-lesional septations have low T1 and T2 signal intensities [5, 6]. Both CT and MRI allows for better appreciation of localization within the omentum, relationships with adjacent structures and features suspicious for malignancy, including enhancing soft tissue components, thickened and enhancing septations, irregular margins, infiltration into surrounding structures and lymphadenopathy [4–6].
Yet lipomas may remain difficult to distinguish from well-differentiated liposarcomas radiologically [5, 6]. There is evidence to support the use of FDG-PET in these circumstances, with generally higher avidity found in well-differentiated liposarcomas compared to lipomas [10]. While histopathological diagnosis may be required in radiologically indistinguishable cases, core needle biopsy is controversial due to potential tumor cell seeding along the tract [3, 6].
Definitive treatment of omental lipomas is complete surgical resection, and despite their size, they are usually easily removed due to their encapsulated nature and absence of local invasion [5]. While laparotomy is most often described in the literature, laparoscopic approaches have been reported for smaller lesions [1, 7]. Margins required for complete resection and recurrence rates thereafter remains unclear.
Omental lipomas are rare entities limited to case reports in the literature [1]. To our knowledge, the case presented is among the few giant omental lipomas reported in the adult population [1–4]. Malignant pathology, particularly well-differentiated liposarcoma, should be considered and can be difficult to distinguish from omental lipomas radiologically. Multidisciplinary input, MRI and FDG-PET may assist in formulating an appropriate strategy for surgical management.
Contributor Information
Jia Xi Julian Li, Department of Surgery, St Vincent’s Hospital Sydney, Darlinghurst, New South Wales, Australia.
Hugh Lewis Giddings, Department of Surgery, St Vincent’s Hospital Sydney, Darlinghurst, New South Wales, Australia.
Gareth Owen, Department of Surgery, St Vincent’s Hospital Sydney, Darlinghurst, New South Wales, Australia.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1. Shiroshita H, Komori Y, Tajima M, Bandoh T, Arita T, Shiraishi N, et al. Laparoscopic examination and resection for giant lipoma of the omentum: a case report and review of related literature. Surg Laparosc Endosc Percutan Tech 2009;19:e217–20. [DOI] [PubMed] [Google Scholar]
- 2. Turk E, Karagulle E, Oguz H, Toprak E. Indirect hernial sac containing the uterus, ovary, and fallopian tube in association with a giant intraabdominal lipoma: report of a case. Hernia 2012;16:593–5. [DOI] [PubMed] [Google Scholar]
- 3. Beattie GC, Irwin ST. Torsion of an omental lipoma presenting as an emergency. Int J Clin Pract 2005;59:130–1. [DOI] [PubMed] [Google Scholar]
- 4. Sen D, Chakrabarti R, Ranjith M, Gulati D. Giant omental lipoma in an elderly female patient. Med J Armed Forces India 2018;74:377–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ozcan NC, Edizsoy A, Colak T. Giant abdominal lipoma in adult. Case Rep Surg 2021;2021:6610533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tirukonda P, Wu S, Brar J, Ng KS, Mirsadraee S. Trans arterial embolization of spontaneous intra-abdominal haemorrhage from omental lipoma. Case Rep Radiol 2018;2018:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kinjo Y, Adachi Y, Seki K, Tsubono M. Laparoscopic resection for torsion of an omental lipoma presenting as an acute abdomen in a 5-year-old girl. J Surg Case Rep 2014;2014:rju072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Serpell JW, Chen RY. Review of large deep lipomatous tumours. ANZ J Surg 2007;77:524–9. [DOI] [PubMed] [Google Scholar]
- 9. Hashimoto S, Arai J, Nishimuta M, Matsumoto H, Fukuoka H, Muraoka M, et al. Resection of liposarcoma of the greater omentum: a case report and literature review. Int J Surg Case Rep 2019;61:20–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Suzuki R, Watanabe H, Yanagawa T, Sato J, Shinozaki T, Suzuki H, et al. PET evaluation of fatty tumors in the extremity: possibility of using the standardized uptake value (SUV) to differentiate benign tumors from liposarcoma. Ann Nucl Med 2005;19:661–70. [DOI] [PubMed] [Google Scholar]


