Abstract
Purpose:
We sought to aggregate common barriers and facilitators to screening adolescents for sensitive health topics (e.g., depression, chlamydia) in primary care, as well as those that are unique to a given health topic.
Methods:
We conducted a literature search of three databases (PsycInfo, MEDLINE, and CINAHL) and reference lists of included articles. Studies focused on barriers and facilitators to screening adolescents (ages 12–17 years) for sensitive health topics in primary care that are recommended by national guidelines. Articles were peer-reviewed, presented empirical data, and published in English in 2006–2021. We coded barriers and facilitators using the Consolidated Framework for Implementation Research, a well-established framework within implementation science.
Results:
In total, 39 studies met inclusion criteria and spanned several health topics: depression, suicide, substance use, Human Immunodeficiency Virus (HIV), and chlamydia. We found common barriers and facilitators to screening across health topics, with most relating to characteristics of the primary care clinics (e.g., time constraints). Other factors relevant to screening implementation ranged from confidentiality concerns to clinician knowledge. Barriers and facilitators specific to certain health topics, such as the availability of on-site laboratories for HIV screening, were also noted.
Conclusions:
Findings can guide refinements to screening implementation.
Keywords: adolescents, screening, primary care, implementation science
National guidelines recommend that pediatric primary care providers (PCPs) screen young people for a growing number of health topics [1,2,3,4] and literature suggests there are numerous barriers to conducting such screening (e.g., reimbursement, limited time) [5,6]. However, most research on factors that impede or facilitate screening in primary care focuses on a single health topic (e.g., substance use) [7], which likely leads to overlooking common factors related to implementation of screening across health topics in this setting. Understanding similarities in barriers and facilitators to screening in primary care has the potential to accelerate the process of designing and testing generalizable strategies for enhancing screening implementation efforts broadly. In the current scoping review, we aggregate research on factors that enable and hinder screening adolescents for sensitive health topics (e.g., substance use, sex, and mental health) [8] in primary care. We focus on sensitive health topics during adolescence given the heightened vulnerability to a number of mental health concerns and risky behaviors that occurs during this developmental period [9,10,11,12] and the fact that discussion of sensitive health topics has been linked to adolescents’ active role in treatment and positive perceptions of their PCPs [8]. Thus, routine screening and follow-up for sensitive health topics is crucial for adolescents’ physical and mental health.
Applying Implementation Science Frameworks to Identify Barriers and Facilitators to Screening
A key issue in implementation science, or the study of methods to foster the uptake of evidence-based practices into routine health services to improve quality of care [13], is that efforts to understand barriers and facilitators to implementation are often lengthy and focused on one health topic [14]. The current scoping review represents one avenue for addressing this issue and promotes streamlining of knowledge on common factors related to screening implementation in primary care.
Implementation science offers frameworks for classifying determinants (i.e., barriers and facilitators) of implementation [15]. A key focus of such frameworks is the importance of the fit between an evidence-based practice and the setting in which it is to be implemented [16,17]. One prominent framework, the Consolidated Framework for Implementation Research (CFIR) [17], highlights the complex, multi-level contextual factors associated with implementation of an evidence-based practice, ranging from aspects of the healthcare organization to clinicians’ beliefs. Because screening adolescents in primary care inherently involves similar contextual factors, including the setting itself (e.g., workflow within a primary care office) and the types of clinicians providing these services (e.g., resident and attending physicians), barriers and facilitators to screening are likely shared across diverse health topics and different clinics. In addition to identifying common barriers and facilitators, uncovering factors that are unique to a specific health topic in the current review can facilitate tailoring of implementation strategies for enhancing uptake of screening procedures for that topic. For example, ensuring practice protocols include reliable ways to identify sexually active adolescents may be important for implementing risk-based screening, such as screening for chlamydia and gonorrhea.
Screening Adolescents for Sensitive Health Topics in Primary Care
Guidelines from leading medical organizations have encouraged screening youth for a variety of health topics [2,3,4,18]. The U.S. Preventive Services Task Force (USPSTF), which assigns letter grades to designate screening priorities, is a major source of the guidelines for adolescent screening [2]. Many of the USPSTF’s recommendations regarding adolescent screening fall within the scope of sensitive health topics [9,19]. Studies have delineated barriers and facilitators to screening adolescents for many of the health topics recommended by the USPSTF. For instance, studies on specific health topics (e.g., suicide, depression, substance use) have found knowledge levels and time constraints to be relevant to implementing screening [7,20,21]. Despite some unique barriers that likely exist given differences in the types of screening involved for various sensitive health topics (e.g., lab tests for HIV vs. paper-and-pencil measures for depression, universal screening for depression vs. screening sexually active females for chlamydia and gonorrhea), there are potentially many common barriers and facilitators to screening adolescents for sensitive health topics in primary care, such as discomfort associated with discussing these topics and confidentiality issues [7,22].
The Present Study
Our scoping review synthesizes information on barriers and facilitators to screening in order to streamline implementation processes. Optimizing screening implementation in primary care is crucial given that screening is an important means of symptom detection that can spark linkages to care to prevent the onset or escalation of physical and mental health problems.
Methods
Literature Search
We conducted a scoping review given that this type of review is best suited for determining the coverage of a body of literature on a topic and providing an overview of key concepts and types of evidence to summarize findings and identify gaps in research [23,24,25]. See the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [26] checklist in Appendix File S1. To increase the rigor of our approach, our scoping review was guided by the Arksey and O’Malley framework [23], which provides structured steps for scoping studies. We completed a comprehensive literature search using three databases: PsycInfo, MEDLINE, and CINAHL; abstracts of articles retrieved from this literature search were compiled in Rayyan QCRI software and those articles containing relevant content based on the abstract/title then underwent full article review (see Figure 1). The reference lists of articles retrieved via database searches that met inclusion criteria were also searched to identify additional articles for inclusion. The initial search was restricted to peer-reviewed manuscripts available in English that were published between January 2006 and October 2019. The starting point was chosen to reflect the fact that 2006 marks the beginning of the journal Implementation Science. This year functionally demarcates the launch of the implementation science field, and thus, we expected that 2006 would also signify the beginning of formal approaches to assessing barriers and facilitators to implementation. We conducted an updated literature search from November 1 2019 through August 17 2021. All included studies were conducted in the United States and presented empirical data (qualitative, quantitative, multiple, or mixed methods).
Figure 1.
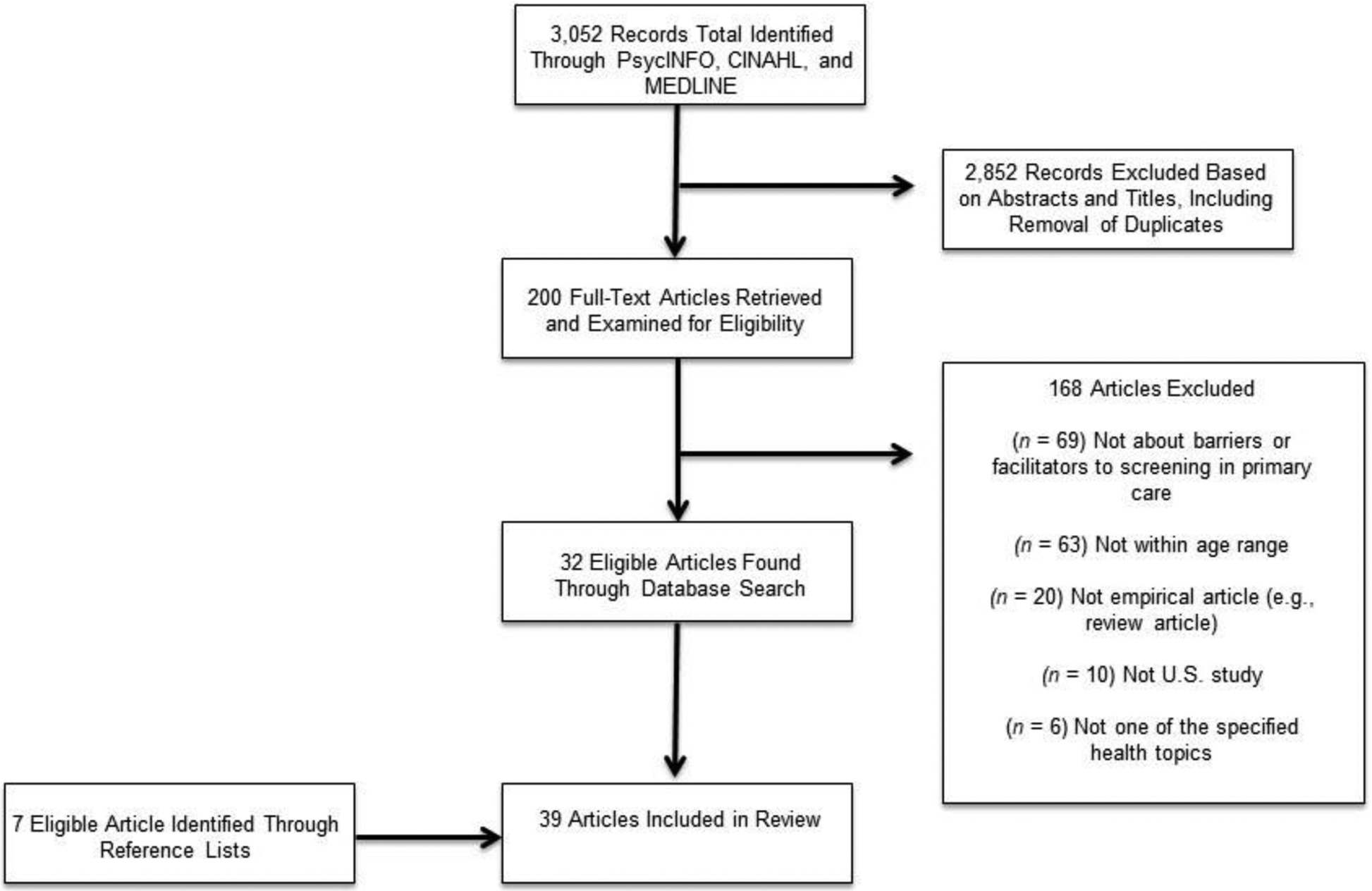
Flowchart depicting the literature search process.
The present review focused on screening for adolescents ages 12–17, based on the Centers for Disease Control and Prevention’s parameters for defining this developmental period [27,28]. Similar to an approach used by Ranney and colleagues [29], studies were included if at least 1/3 of the sample fell within the 12–17 range. If the percentages of individuals within different age ranges were not provided, studies could still be included if the mean age for the sample was between 12 and 17. Furthermore, studies of clinicians who worked with adolescents were included.
Health topics included in this review were drawn from the published USPSTF ratings available in October 2019. In particular, those topics that were designated as grade A (i.e., “Strongly Recommended”), B (“Recommended”), or I (“Insufficient Evidence to Make a Recommendation”) for adolescent screening were reviewed. Topics under consideration were: gestational diabetes, Hepatitis B, high blood pressure, illicit drug use, bacterial vaginosis, HIV, elevated blood lead levels, unhealthy alcohol use, intimate partner violence, syphilis, adolescent idiopathic scoliosis, obesity, celiac disease, lipid disorders, depression, iron deficiency anemia, chlamydia and gonorrhea, suicide, and Rh(D) incompatibility. From those topics, we selected those that can be defined as sensitive health topics based on the extant literature, including mood, substance use, sexuality, getting along with other people, and family problems [8]. Topics designated as “I” by the USPSTF (i.e., illicit drug use, suicide risk, and alcohol use) were included in the present review given that the American Academy of Pediatrics has advocated for screening for these topics in primary care [1,30]. This led to the inclusion of 10 health topics in our literature search: chlamydia, gonorrhea, depression, Hepatitis B, Human Immunodeficiency Virus (HIV), intimate partner violence, syphilis, illicit drug use, suicide risk, and alcohol use [10,19,31–37].
For our initial search, the search term combinations covered the following categories: implementation determinants (e.g., “barrier(s),” “facilitator(s)”), screening (e.g., “screen,” “questionnaire(s)”), health domain (e.g., “depression,” “chlamydia”), setting (e.g., “primary care”), and age group (e.g., “pediatric,” “adolescent”). See Appendix File S2 for a full list of search terms.
In our updated search, we maintained the same health topic terms we used previously. To minimize the number of erroneous hits and streamline the search process, we pared down some of our search terms to focus on “barrier,” “facilitator,” “screening,” “primary care,” and “adolescent.” Reference lists of included articles were again searched to identify additional articles.
Data Analysis
First, we extracted general information (e.g., author, title, year, results specific to barriers and facilitators) from articles that met the aforementioned inclusion criteria. We then developed a codebook guided primarily by CFIR [17]. CFIR outlines various levels of context (e.g., culture of the healthcare organization, clinician knowledge; see Appendix File S3 for a list of constructs and operational definitions for the current study) that can affect implementation of best practices. CFIR categories were operationalized within the codebook based on definitions of CFIR constructs outlined in the literature [17]. We provide examples relevant to screening accompanying those definitions in the codebook to facilitate application of the codes to the data. For instance, as described in Appendix File S3, for the Outer Setting code, we state, “This code refers to the economic, political, and social context in which the organization resides. This includes factors such as external policies and incentives (e.g., Medicaid billing, USPSTF guidelines regarding screening), opportunities (or lack thereof) for linkages to care, population served by the clinic/health system, and clinic location.” With guidance from a review by Williams and Beidas [38], we further drew upon individual-level factors highlighted in leading implementation science frameworks [17,39,40,41] to provide fine-grained details on clinician factors linked to implementation. Furthermore, in line with the work of Safaeinili and colleagues [42], who note the need to adapt CFIR [17] to augment its focus on patient needs, we included a code to encompass patient and family factors pertinent to screening implementation (e.g., patient age). To parallel the patient and family factors code and capture clinician factors that were not encompassed in other codes, we also added a code for clinician demographics. The patient and family factors and clinician demographics codes were both derived inductively based on review of included studies to ensure sufficient coverage of key concepts. See code definitions in Appendix File S3; the application of codes to specific studies is detailed in Appendix Table S1.
Full text articles were then coded to categorize barriers and facilitators to screening. Consistent with qualitative matrix analysis techniques [43], data were displayed in a matrix to organize key dimensions and discern trends across cells. Each study comprised a row, and columns were comprised of the study’s health topic(s), applicable codes, and related barriers and/or facilitators. Barrier and/or facilitator cells included key qualitative themes and/or quantitative results from the text. To ensure rigor in our approach, two authors double-coded eight studies (21%) to determine reliability (i.e., agreement on presence or absence of each code). We chose to double code approximately 20% of the included articles since 20% is commonly used as the threshold in empirical literature to establish inter-rater reliability [44,45]. For the double-coded articles, authors discussed discrepancies to reach consensus. Reliability was calculated prior to consensus discussions and percent agreement was 91% across all codes for the eight double-coded studies. The authors independently coded the remainder of the files and met regularly to discuss questions to avoid coder drift. The coders also consulted one of the senior authors as discrepancies arose to facilitate consensus decisions. After coding was complete, we then grouped barriers and facilitators for each code by health topic and identified concepts (e.g., uncertainty related to management of positive screens) that were common across health topics. We also counted the codes observed (e.g., number of studies in which outer setting factors were coded as barriers/facilitators). Recurrent concepts that spanned at least two health topics are highlighted in our narrative synthesis of results as common barriers/facilitators, and unique features of specific health topics are then presented. In addition to providing numeric counts for our results, we highlight example articles illustrating each point.
Results
See Figure 1 for a visual depiction of the literature search process (initial and updated search results combined). In total, 39 articles met inclusion criteria and were coded for barriers and facilitators to screening. Many (n=22) studies represented clinician perspectives, 7 articles represented patient perspectives, and 3 studies included both perspectives. One study focused on clinic staff (e.g., administrators, clinicians). Six studies were conducted at the clinic- or visit-level. The majority (n=33) of studies reported quantitative data, with fewer utilizing qualitative methods (n=4) mixed methods (n=1) or multiple methods (n=1). Study characteristics such as the sample size and screening measures used are provided in Appendix Table S1. The included articles mainly focused on substance use (n=18) and depression (n=17) and also covered the health domains of suicide (n=7), HIV (n=6), and chlamydia (n=1). Among those studies, some (n=7) focused on more than one of the included health topics. We first will review the primary common barriers and facilitators that were described across multiple health topics (i.e., at least two) in the included studies, and then highlight some distinctive factors unique to a single health topic (i.e., HIV, depression, and suicide). See Appendix File S3 for detailed definitions of the codes discussed below.
Commonalities
Inner Setting
The most commonly-cited barriers and facilitators across studies and health topics related to the inner setting (n=28) [17], meaning characteristics of the primary care clinics themselves (e.g., workflows, resources). Time constraints were consistently described as a major barrier to screening efforts (n=14) [7,46,37,48]; approaches to overcoming time constraints such as conducting screening before the visit began and using technology (e.g., computerized screening) to facilitate screening were noted [47,49,50,51]. Established clinic procedures for screening, such as in the context of universal implementation or other practice protocols facilitated screening (n=6) [52]. The availability of resources in the clinic (n=14) [53], including designated staff to conduct screening [5], was identified as a key factor for adoption of routine screening into clinical practice. Given the competing demands of managing pressing health concerns during sick visits, clinicians were more likely to screen during well visits (n=5) [7,54]; this aligns with many systems-level recommendations that annual screenings occur during adolescent well-visits [45].
Outer Setting
The economic, political, and social context of the primary care clinics, referred to within CFIR as the outer setting [17], was also a common barrier (n=10) [20,55,56]. Payment processes arose as being pertinent to whether or not screening was performed (n = 4) [5,54]. For instance, lack of reimbursement for screening was one barrier [5]. There were also concerns raised about limited options for, and information about, treatment referrals in the community following screening, as well as extended wait times for treatment (n=4) [6,7,49]. Additionally, some studies noted screening rates varied by clinic location (e.g., urban vs. suburban, Northeast vs. West) (n=3) [20,56].
Clinician Factors
With regard to common clinician factors associated with screening (n=23), clinicians expressed discomfort discussing sensitive health topics and uncertainty about how to handle positive screens (n=6) [46,49,57]. Nonetheless, clinicians tended to endorse responsibility for identifying concerns involving these health topics (n=7) [58,59]. Whereas opportunities for training, and therefore enhanced knowledge, facilitated screening for multiple health topics, gaps in knowledge and training were also described as barriers (n=15) [20,21,60,61]. Confidentiality concerns pervaded multiple levels of implementation (n=8). In addition to serving as a barrier in terms of the outer setting (e.g., disclosure via billing) and inner setting (e.g., documentation in the electronic health record) [46], clinicians also expressed concerns about how to proceed when parents do not allow confidential conversations with adolescents to take place [7] and discomfort deciding when to break an adolescent’s confidentiality [20].
Patient and Family Factors
Clinicians screened differentially for various health topics depending on certain patient and family factors (n=10). For example, patients presenting with risk factors perceived as being pertinent to a given health topic (e.g., report of sexually active peers, “warning signs”) were more likely to be screened than peers who were perceived as being lower-risk (n=5) [6,46,62,63]. There were also documented disparities in screening (n=5) based on patient race/ethnicity [54,59], age [46], and gender [21]. For instance, Meredith et al. (2018) found that while older adolescent age was associated with higher odds of screening for substance use, adolescents who identified as Black, Hispanic, Multiracial, or other non-White race/ethnicity had lower odds of being screened [62].
Barriers and Facilitators Unique to a Single Health Topic
While the preponderance of barriers and facilitators identified spanned multiple health topics, some were specific to a given topic, as noted below.
HIV
Because screening for HIV inherently involves physical test results, lack of availability of an on-site laboratory, in addition to barriers related to transportation to an outside laboratory, can hinder HIV screening (n=1) [46]. Furthermore, time required for pre-test and post-test counseling (irrespective of test results) was also identified as a barrier to HIV screening (n=1) [53]. Clinicians cited concern for breached confidentiality via both the electronic health record (e.g., HIV test order printing out on an after visit summary) and insurance companies (e.g., documentation of HIV testing in the explanation of benefits) as a system-level barrier to screening (n=1) [46]. Clinicians’ having information specific to local and state consent laws was a unique facilitator of HIV screening (n=1) [53]. Additionally, adolescents facilitated their own screening with specific requests to clinicians for HIV testing (n=1) [53].
Depression
Whereas reminders (e.g., signs in the clinic, texts/emails) to clinic staff facilitated depression screening, forgetting served as a barrier (n=1) [54]. Of note, clinician self-efficacy in detecting depression and suicide risk can be intertwined [57], which makes sense given that screening for both often occurs using the same measure.
Suicide
A few clinician-level experiences and beliefs were unique to suicide screening. Specifically, Diamond and colleagues [20] found that seeing at least one suicidal adolescent in the past year and clinicians’ belief that talking about suicide did not yield iatrogenic effects served as facilitators.
Discussion
The current scoping review aggregates information on barriers and facilitators to screening adolescents for a variety of sensitive health topics to identify cross-cutting ways to enhance screening implementation. Overall, findings shed light on the many common factors related to implementation of adolescent screening for sensitive health topics in primary care, regardless of the health topic. While our findings suggest more similarities than differences, we also highlighted barriers and facilitators unique to specific health topics that are important to consider when planning future implementation efforts.
The most consistently cited barriers and facilitators were related to the inner setting, meaning the primary care clinics themselves, with clinician factors being a close second. In particular, time constraints were highlighted as a major barrier to screening adolescents for sensitive health topics in primary care [7,46]. This aligns with research that has quantified time constraints in primary care, including findings indicating that about 7.4 hours per working day (or 1773 hours annually) is needed for physicians in primary care to carry out all USPSTF recommendations for preventive services in a practice of 2500 patients with an age and sex distribution similar to that of the U.S. population [64]. While the amount of time spent on adolescent preventative services is likely less given there are more USPSTF guidelines that apply to adults than pediatric populations, this finding still points to the substantial time it can take to implement USPSTF recommendations on top of other visit tasks. A number of inner setting facilitators were also noted in the extant literature, such as the availability of clinic resources and establishment of clinic procedures for screening. Given the shared aspects of the inner setting and similarities in the types of clinicians being tasked with screening, prioritizing strategies that target aspects of the inner setting as well as clinician factors will be especially important for optimizing screening implementation in primary care. For example, assigning tasks related to screening and subsequent follow-up to specific clinic staff and providing reminders about these procedures may streamline workflows and help clinicians remember to screen [5,54]. Results also suggest that clinicians may need additional support navigating difficult conversations with adolescents regarding sensitive health topics [49]. Based on the benefits of training noted in the included studies [21], this may be one important outlet for supporting clinicians. In particular, trainings with experiential components (e.g., role plays and opportunities for live feedback) may be especially helpful for bolstering clinicians’ confidence and skills in discussing sensitive health topics with adolescents. Given that upstream factors like insurer and health system policies can drive inner setting barriers such as time constraints [65], advocacy for changes to the structure of service delivery (e.g., extending time with providers and adjusting reimbursement to compensate for that time, increasing integration of behavioral health services into pediatric primary care; 66,67) may be needed to enhance screening.
We also found other commonalities in barriers and facilitators across health topics, including intervention characteristics and outer setting factors. For example, payment processes were relevant to screening implementation, with funding for screening serving as a facilitator [46] and lack of reimbursement functioning as a barrier [5]. Given that barriers and facilitators at different levels (e.g., clinician- and organization-level factors) are often intertwined [68] and interact to predict clinician practices [69], it will be important that implementation strategies for promoting screening in primary care span multiple levels of context. Implementing a clinical pathway with clear guidance on screening tools to use for each health topic, ages when screening should occur, and steps to take to address a positive screen would not only target inner setting factors related to the importance of having established clinic procedures but would also help to alleviate clinician uncertainty about management of positive screens. Implementation strategies targeting screening for multiple health topics might be a particularly efficient method for augmenting uptake and sustainment of numerous screening procedures in pediatric primary care. Strategies can range from knowledge assessments to gauge clinician understanding after training to lists of billing codes to make the billing process easier [70].
Additionally, the racial and ethnic disparities observed in the current study are likely due to structural determinants based on longstanding issues of systemic racism and racial injustice in the U.S. Thus, efforts to augment implementation of screening or other health services should include a focus on health equity to ensure that services and implementation strategies reach all adolescents and reduce inequities in care [71,72]. Relatedly, additional research is needed to specifically delineate determinants of screening implementation from a health equity perspective (e.g., racism, medical mistrust) [73].
While barriers and facilitators related to characteristics of the screeners themselves (e.g., length of measures) were rarely coded (n=5), this is most likely reflective of the lack of implementation research exploring these characteristics [74]. Close attention to intervention characteristics, such as the complexity of screening measures (e.g., how cumbersome they are to administer and score) will be key for optimizing screening implementation.
Of note, there were also unique barriers and facilitators pertaining to specific health topics. For example, clinicians’ belief that there were not iatrogenic effects of talking about suicide facilitated suicide screening [20]. Similarly, when lab tests were involved in screening as is the case for HIV, unique barriers were noted such as lack of availability of an on-site laboratory [46]. This suggests that some tailoring of strategies for specific health topics is warranted to improve uptake of screening procedures. Tailored strategies could take the form of clinician- and/or patient-facing educational resources focused on a specific health topic, reminders in the electronic health record pertinent to a particular screener, and so forth. It will be important for future research to compare the effectiveness of cross-cutting versus topic-specific implementation strategies.
Limitations
Despite contributions of this work to our understanding of barriers and facilitators to screening in primary care, limitations are noted. First, to represent the state of the literature on barriers and facilitators to screening adolescents for sensitive health topics in primary care, we did not require included articles to focus on screening using specific, validated measures. We recognize there may be variability in barriers and facilitators to screening depending on the approach to screening used. As research on this topic continues to accumulate, it would be beneficial to examine barriers and facilitators to administering certain screening measures, such as those recommended by the American Academy of Pediatrics (e.g., Car, Relax, Alone, Forget, Friends, Trouble, Patient Health Questionnaire-9 Modified for Teens; [1,4]). Second, we did not analyze the data based on the type of screening recommendation (i.e., universal vs. risk-based); there may be unique barriers associated with implementing each type of recommendation. For example, risk-based screening hinges on accurate risk assessments (e.g., gathering information on sexual activity before determining whether to screen for chlamydia and gonorrhea), so any obstacles to those assessments will pose additional barriers to screening. Third, based on the literature available, certain health topics are more heavily represented than others in this review. There were also barriers and facilitators (e.g., clinician emotions) outlined in our coding system that were not reflected in the included studies. While this could suggest these determinants are less salient in primary care compared to other settings, it is more likely that they are simply understudied and further research is needed to investigate a more expansive set of barriers and facilitators to screening adolescents for sensitive health topics in primary care. Updating this review in the future will ensure contemporary knowledge of the most pressing barriers and facilitators to screening adolescents for sensitive health topics in primary care are consolidated. Moreover, for health topics that are under-represented in the literature, there is an opportunity to apply what we learned about common barriers and facilitators to designing strategies to enhance implementation of screening for those topics.
Conclusions
In sum, the current scoping review synthesizes barriers and facilitators to screening practices that share common features with regard to general content and setting. Given the extensive lag between the generation of research findings and the application of those findings in clinical practice [75], we need to find ways to use existing research more efficiently to accelerate implementation of essential healthcare services. While we are not suggesting review articles will replace the need for collecting data to understand contextual factors when implementing screening in a new setting or with a new population, it is possible that reviews like this could be used as a tool to rapidly verify previously discovered barriers and facilitators to screening are relevant to current stakeholders before beginning implementation [14]. Comparing the cost-effectiveness and quality of information gathered using reviews such as the current one as the primary means of assessing barriers and facilitators versus conducting in-depth contextual inquiry (e.g., detailed qualitative interviews in a given setting) will be a critical next step for making data-driven decisions about when these different approaches are most appropriate. The current findings, alongside close partnerships with key stakeholders, can be used to enhance existing screening for sensitive health topics among adolescents in primary care.
Supplementary Material
Appendix Table S1. Study characteristics and application of codes.
Appendix File S1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Appendix File S2. Search terms.
Appendix File S3. Codebook used in the present study.
Figure 2.
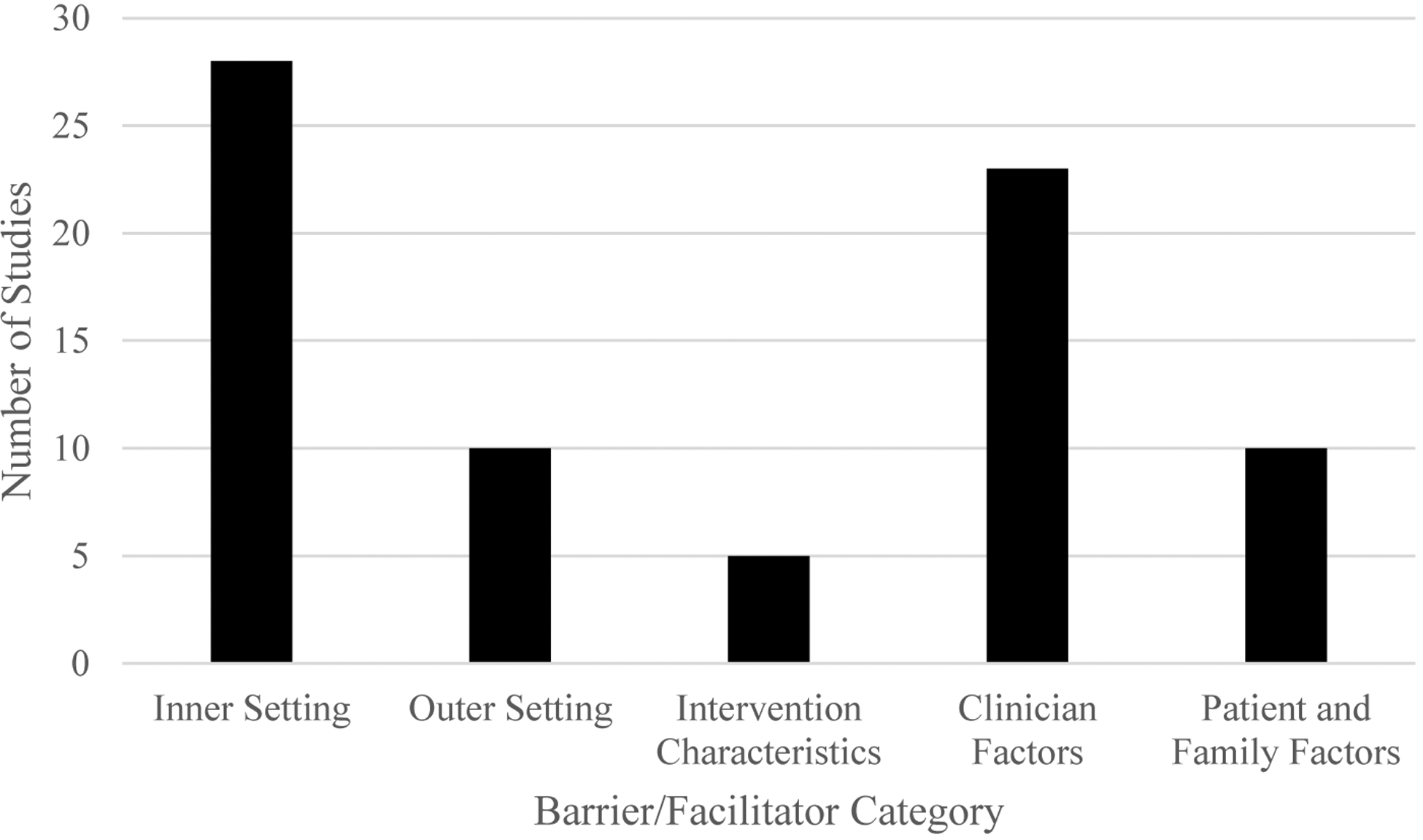
Number of studies coded for each category of barriers/facilitators.
Note. Clinician factors (e.g., knowledge, demographics) were combined into one overarching category.
Implications and Contributions.
This review highlights common barriers and facilitators to screening adolescents for sensitive health topics (e.g., depression, HIV) in primary care. Findings can be used to enhance screening among adolescents in primary care.
Disclosures and Acknowledgements:
Dr. Rinad Beidas receives royalties from Oxford University Press and has provided consultation to the Camden Coalition of Health Care Providers. She currently provides consultation to United Behavioral Health. She also serves on the Clinical and Scientific Advisory Board for Optum Behavioral Health. Dr. Jami Young receives royalties from Oxford University Press. The authors declare that they have no conflicts of interest relevant to this article to disclose. All authors helped conceptualize and design the review and reviewed and revised the manuscript. Dr. Davis drafted the initial manuscript, with assistance from Dr. Hoskins. Drs. Davis and Hoskins coded articles for barriers and facilitators and interpreted the data. Dr. Davis, Dr. Hoskins, Ms. Phan, Ms. Hoffacker, Ms. Reilly and Ms. Fugo decided on article inclusion/exclusion. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding:
Katelin Hoskins is supported by a National Institute of Mental Health Training Fellowship (T32 MH109433; Mandell/Beidas MPIs). Molly Davis was supported by the same fellowship during the preparation and initial submission of this manuscript. Rinad Beidas is supported by a grant from the National Cancer Institute (P50 CA244690; Beidas, Bekelman, and Schnoll MPIs). The funders had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. The article contents have not been previously presented elsewhere.
Abbreviations:
- PCP
primary care provider
- HIV
Human Immunodeficiency Virus
- USPSTF
U.S. Preventive Services Task Force
- CFIR
Consolidated Framework for Implementation Research
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Hagan JF, Shaw JS, Duncan PM, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 4th ed. American Academy of Pediatrics, 2017. [Google Scholar]
- [2].U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/uspstf/topic_search_results?topic_status=P. Accessed October 7, 2019.
- [3].Burke PJ, Coles MS, Di Meglio G, et al. Sexual and Reproductive Health Care: A position paper of the Society for Adolescent Health and Medicine. J Adolesc Health. 2014;54:491–496. DOI: 10.1016/j.jadohealth.2014.01.010. [DOI] [PubMed] [Google Scholar]
- [4].Zuckerbrot RA, Cheung A, Jensen PS, Stein REK, Laraque D; GLAD-PC Steering Group. Guidelines for adolescent depression in primary care (GLAD-PC): part I. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018;141:e20174081. DOI: 10.1542/peds.2017-4081. [DOI] [PubMed] [Google Scholar]
- [5].Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv. 2019;70:409–412. DOI: 10.1176/appi.ps.201800427. [DOI] [PubMed] [Google Scholar]
- [6].Taliaferro LA, Hetler J, Edwall G, et al. Depression screening and management among adolescents in primary care: factors associated with best practice. Clin Pediatr (Phila). 2013;52:557–567. DOI: 10.1177/0009922813483874. [DOI] [PubMed] [Google Scholar]
- [7].Van Hook S, Harris SK, Brooks T, et al. ; New England Partnership for Substance Abuse Research. The “Six T’s”: barriers to screening teens for substance abuse in primary care. J Adolesc Health. 2007;40:456–461. DOI: 10.1016/j.jadohealth.2006.12.007. [DOI] [PubMed] [Google Scholar]
- [8].Brown JD, Wissow LS. Discussion of sensitive health topics with youth during primary care visits: relationship to youth perceptions of care. J Adolesc Health. 2009;44:48–54. DOI: 10.1016/j.jadohealth.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Shannon CL, Klausner JD. The growing epidemic of sexually transmitted infections in adolescents: a neglected population. Curr Opin Pediatr. 2018;30:137–43. DOI: 10.1097/MOP.0000000000000578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Siu AL; US Preventive Services Task Force. Screening for depression in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2016;137:e20154467. DOI: 10.1542/peds.2015-4467. [DOI] [PubMed] [Google Scholar]
- [11].Hankin B, Young J, Abela J, Smolen A, Jenness J, Gulley L, Technow J, Gottlieb A, Cohen J, Oppenheimer C. Depression from childhood into late adolescence: influence of gender, development, genetic susceptibility, and peer stress. J Abnorm Psychol. 2015;124:803–16. DOI: 10.1037/abn0000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Steinberg L Risk-taking in adolescence: new perspectives from brain and behavioral science. Curr Direct Psychol Sci. 2007;16:55–9. DOI: 10.1111/j.1467-8721.2007.00475.x. [DOI] [Google Scholar]
- [13].Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci. 2006;1:1. DOI: 10.1186/1748-5908-1-1. [DOI] [Google Scholar]
- [14].Davis M, Beidas RS. Refining contextual inquiry to maximize generalizability and accelerate the implementation process. Implement Res Pract. 2021;2:1–4. DOI: 10.1177/2633489521994941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43:337–50. DOI: 10.1016/j.amepre.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health. 2011;38:4–23. DOI: 10.1007/s10488-010-0327-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. DOI: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Committee on Practice and Ambulatory Medicine, Bright Futures Periodicity Schedule Workgroup. 2021 Recommendations for preventive pediatric health care. Pediatrics 2021;147: e2020049776. DOI: 10.1542/PEDS.2020-049776. [DOI] [PubMed] [Google Scholar]
- [19].Owens DK, Davidson KW, Krist AH, et al. ; US Preventive Services Task Force. Screening for HIV infection: US Preventive Services Task Force recommendation statement. JAMA. 2019;321:2326–2336. DOI: 10.1001/jama.2019.6587. [DOI] [PubMed] [Google Scholar]
- [20].Diamond GS, O’Malley A, Wintersteen MB, Peters S, Yunghans S, Biddle V, et al. Attitudes, practices, and barriers to adolescent suicide and mental health screening: a survey of Pennsylvania primary care providers. J Prim Care Community Health. 2012;3:29–35. DOI: 10.1177/2150131911417878. [DOI] [PubMed] [Google Scholar]
- [21].Fallucco EM, Seago RD, Cuffe SP, Kraemer DF, Wysocki T. Primary care provider training in screening, assessment, and treatment of adolescent depression. Acad Pediatr. 2015;15:326–332. DOI: 10.1016/j.acap.2014.12.004. [DOI] [PubMed] [Google Scholar]
- [22].Santelli JS, Klein JD, Song X, et al. : Discussion of potentially sensitive topics with young people. Pediatrics. 2019;143:e20181403. DOI: 10.1542/peds.2018-1403. [DOI] [PubMed] [Google Scholar]
- [23].Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. DOI: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- [24].Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67:1291–4. DOI: 10.1016/j.jclinepi.2014.03.013. [DOI] [PubMed] [Google Scholar]
- [25].Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. DOI: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMAScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. [DOI] [PubMed] [Google Scholar]
- [27].Centers for Disease Control and Prevention. Positive parenting tips: young teens (12–14 years of age). Accessed October 2, 2019. https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/adolescence.html.
- [28].Centers for Disease Control and Prevention. Positive parenting tips: young teenagers (15–17 years of age). Accessed October 2, 2019. https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/adolescence2.html.
- [29].Ranney M, Karb R, Ehrlich P, et al. ; FACTS Consortium. What are the long-term consequences of youth exposure to firearm injury, and how do we prevent them? A scoping review. J Behav Med. 2019;42:724–740. DOI: 10.1007/s10865-019-00035-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Shain B; Committee on Adolescence. Suicide and suicide attempts in adolescents. Pediatrics. 2016;138:e20161420. DOI: 10.1542/peds.2016-1420. [DOI] [PubMed] [Google Scholar]
- [31].Curry SJ, Krist AH, Owens DK, et al. ; US Preventive Services Task Force. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;320:1899–1909. DOI: 10.1001/jama.2018.16789. [DOI] [PubMed] [Google Scholar]
- [32].LeFevre ML, U.S. Preventive Services Task Force: Screening for chlamydia and gonorrhea: U.S. preventive service task force recommendation statement. Ann Intern Med. 2014;161:902–910. DOI: 10.7326/M14-1981. [DOI] [PubMed] [Google Scholar]
- [33].Screening for Illicit Drug Use: U.S. Preventive Services Task Force Recommendation Statement US Preventive Services Task Force. Published 2008. Accessed October 8, 2019. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening. [Google Scholar]
- [34].LeFevre ML; US Preventive Services Task Force. Screening for hepatitis B virus infection in nonpregnant adolescents and adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161(1):58–66. DOI: 10.7326/M14-1018. [DOI] [PubMed] [Google Scholar]
- [35].Curry SJ, Krist AH, Owens DK, et al. ; US Preventive Services Task Force. Screening for intimate partner violence, elder abuse, and abuse of vulnerable adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;320:1678–1687. DOI: 10.1001/jama.2018.14741. [DOI] [PubMed] [Google Scholar]
- [36].LeFevre ML, Force USPST Screening for suicide risk in adolescents, adults, and older adults in primary care: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160:719–726. DOI: 10.7326/M14-0589. [DOI] [PubMed] [Google Scholar]
- [37].Bibbins-Domingo K, Grossman DC, Curry SJ, et al. ; US Preventive Services Task Force (USPSTF). Screening for syphilis infection in nonpregnant adults and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(21):2321–2327. DOI: 10.1001/jama.2016.5824 [DOI] [PubMed] [Google Scholar]
- [38].Williams NJ, Beidas RS. Annual research review: the state of implementation science in child psychology and psychiatry: a review and suggestions to advance the field. J Child Psychol Psychiatry. 2019;60:430–450. DOI: 10.1111/jcpp.12960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. DOI: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Flottorp S, Oxman A, Krause J, et al. A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci. 2013;8:35. DOI: 10.1186/1748-5908-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Safaeinili N, Brown-Johnson C, Shaw JG, Mahoney M, Winget M. CFIR simplified: pragmatic application of and adaptations to the Consolidated Framework for Implementation Research (CFIR) for evaluation of a patient-centered care transformation within a learning health system. Learn Health Sys. 2020;4:e10201. DOI: 10.1002/lrh2.10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12:855–866. DOI: 10.1177/104973230201200611. [DOI] [PubMed] [Google Scholar]
- [44].Beidas RS, Marcus S, Wolk CB, et al. A prospective examination of clinician and supervisor turnover within the context of implementation of evidence-based practices in a publicly-funded mental health system. Adm Policy Ment Health. 2016;43:640–649. DOI: 10.1007/s10488-015-0673-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Farley AM, Gallop RJ, Brooks ES, Gerdes M, Bush ML, Young JF Identification and management of adolescent depression in a large pediatric care network. J Dev Behav Pediatr. 2020;41:85–94. DOI: 10.1097/DBP.0000000000000750. [DOI] [PubMed] [Google Scholar]
- [46].Lazar N, Rozansky H, Ely B, Ford CA, Dowshen N. Using chart-stimulated recall to identify barriers and facilitators to routine HIV testing among pediatric primary care providers. J Adolesc Health. 2019;65:410–416. DOI: 10.1016/j.jadohealth.2019.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Olson AL, Gaffney CA, Hedberg VA, Gladstone GR. Use of inexpensive technology to enhance adolescent health screening and counseling. Arch Pediatr Adolesc Med. 2009;163:172–177. DOI: 10.1001/archpediatrics.2008.533. [DOI] [PubMed] [Google Scholar]
- [48].Pidano AE, Kimmelblatt CA, Neace WP. Behavioral health in the pediatric primary care setting: needs, barriers, and implications for psychologists. Psychol Serv. 2011;8:151–165. DOI: 10.1037/a0019535. [DOI] [Google Scholar]
- [49].Sterling S, Kline-Simon AH, Wibbelsman C, Wong A, Weisner C. Screening for adolescent alcohol and drug use in pediatric health-care settings: predictors and implications for practice and policy. Addict Sci Clin Pract. 2012;7:13. DOI: 10.1186/1940-0640-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Stevens J, Kelleher KJ, Gardner W, et al. Trial of computerized screening for adolescent behavioral concerns. Pediatrics. 2008;121:1099–1105. DOI: 10.1542/peds.2007-1878. [DOI] [PubMed] [Google Scholar]
- [51].Zuckerbrot RA, Maxon L, Pagar D, Davies M, Fisher PW, Shaffer D. Adolescent depression screening in primary care: feasibility and acceptability. Pediatrics. 2007;119:101–108. DOI: 10.1542/peds.2005-2965. [DOI] [PubMed] [Google Scholar]
- [52].Monico LB, Mitchell SG, Dusek K, et al. A comparison of screening practices for adolescents in primary care after implementation of screening, brief intervention, and referral to treatment. J Adolesc Health. 2019;65:46–50. DOI: 10.1016/j.jadohealth.2018.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Goyal MK, Dowshen N, Mehta A, Hayes K, Lee S, Mistry RD. Pediatric primary care provider practices, knowledge, and attitudes of human immunodeficiency virus screening among adolescents. J Pediatr. 2013;163:1711–5.e6. DOI: 10.1016/j.jpeds.2013.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Bhatta S, Champion JD, Young C, Loika E. Outcomes of depression screening among adolescents accessing school-based pediatric primary care clinic services. J Pediatr Nurs. 2018;38:8–14. DOI: 10.1016/j.pedn.2017.10.001. [DOI] [PubMed] [Google Scholar]
- [55].Ramos MM, Sebastian RA, Murphy M, Oreskovich K, Condon TP. Adolescent substance use: assessing the knowledge, attitudes, and practices of a school-based health center workforce. Subst Abus. 2017; 38:230–236. DOI: 10.1080/08897077.2017.1287149. [DOI] [PubMed] [Google Scholar]
- [56].Zenlea IS, Milliren CE, Mednick L, Rhodes ET. Depression screening in adolescents in the United States: a national study of ambulatory office-based practice. Acad Pediatr. 2014;14:186–191. DOI: 10.1016/j.acap.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Garbutt JM, Leege E, Sterkel R, Gentry S, Strunk RC. Providing depression care in the medical home: what can we learn from attention-deficit/ hyperactivity disorder? Arch Pediatr Adolesc Med. 2012;166:672–673. DOI: 10.1001/archpediatrics.2011.1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Heneghan A, Garner AS, Storfer-Isser A, Kortepeter K, Stein REK, Horwitz SM. Pediatricians’ role in providing mental health care for children and adolescents: do pediatricians and child and adolescent psychiatrists agree? J Dev Behav Pediatr. 2008;29:262–269. DOI: 10.1097/DBP.0b013e31817dbd97. [DOI] [PubMed] [Google Scholar]
- [59].Stein RE, Horwitz SM, Storfer-Isser A, et al. Do pediatricians think they are responsible for identification and management of child mental health problems? Results of the AAP periodic survey. Ambul Pediatr. 2008;8:11–17. DOI: 10.1016/j.ambp.2007.10.006. [DOI] [PubMed] [Google Scholar]
- [60].Arya M, Zheng MY, Amspoker AB, et al. In the routine HIV testing era, primary care physicians in community health centers remain unaware of HIV testing recommendations. J Int Assoc Provid AIDS Care. 2014;13:296–299. DOI: 10.1177/2325957413517140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Levy S, Ziemnik RE, Harris SK, et al. Screening adolescents for alcohol use: tracking practice trends of Massachusetts pediatricians. J Addict Med. 2017;11:427. DOI: 10.1097/ADM.0000000000000340. [DOI] [PubMed] [Google Scholar]
- [62].Meredith LS, Ewing BA, Stein BD, et al. Influence of mental health and alcohol or other drug use risk on adolescent reported care received in primary care settings. BMC Fam Pract. 2018;19:10. DOI: 10.1186/s12875-017-0689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Mullins TK, Braverman PK, Dorn LD, Kollar LM, Kahn JA. Adolescents’ agreement to test for HIV when different testing methods are offered. Int J STD AIDS. 2012;23:173–176. DOI: 10.1258/ijsa.2009.009035. [DOI] [PubMed] [Google Scholar]
- [64].Yarnall KSH, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635–641. DOI: 10.2105/AJPH.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Metzl JM, Hansen HH. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126–133. DOI: 10.1016/j.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Coker TR, Sareen HG, Chung PJ et al. Improving access to and utilization of adolescent preventive health care: The perspectives of adolescents and parents. J Adolesc Health. 2010;47:133–142. DOI: 10.1016/j.jadohealth.2010.01.005. [DOI] [PubMed] [Google Scholar]
- [67].Njoroge WF, Hostutler CA, Schwartz BS, et al. Integrated behavioral health in pediatric primary care. Curr Psychiatry Rep. 2016;18:106. DOI: 10.1007/s11920-016-0745-7. [DOI] [PubMed] [Google Scholar]
- [68].Aarons GA, Glisson C, Green PD, et al. ; Research Network on Youth Mental Health. The organizational social context of mental health services and clinician attitudes toward evidence-based practice: a United States national study. Implement Sci. 2012;7:56. DOI: 10.1186/1748-5908-7-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Becker-Haimes EM, Williams NJ, Okamura KH, et al. Interactions between clinician and organizational characteristics to predict cognitive-behavioral and psychodynamic therapy use. Adm Policy Ment Health. 2019;46:701–712. DOI: 10.1007/s10488-019-00959-6. [DOI] [PubMed] [Google Scholar]
- [70].Thoele K, Ferren M, Moffat L, Keen A, Newhouse R. Development and use of a toolkit to facilitate implementation of an evidence-based intervention: a descriptive case study. Implement Sci Commun. 2020;1:86. DOI: 10.1186/s43058-020-00081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Baumann AA, Cabassa LJ. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv Res. 2020;20:190. DOI: 10.1186/s12913-020-4975-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Chinman M, Woodward EN, Curran GM, Hausmann LRM. Harnessing implementation science to increase the impact of health equity research. Med Care. 2017;55:S16–23. DOI: 10.1097/MLR.0000000000000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Woodward EN, Singh RS, Ndebele-Ngwenya P et al. A more practical guide to incorporating health equity domains in implementation determinant frameworks. Implement Sci Commun. 2021; 2: 61. DOI: 10.1186/s43058-021-00146-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Lyon AR, Bruns EJ. User-centered redesign of evidence-based psychosocial interventions to enhance implementation—hospitable soil or better seeds? JAMA Psychiatry. 2019;76:3–4. DOI: 10.1001/jamapsychiatry.2018.3060. [DOI] [PubMed] [Google Scholar]
- [75].Balas EA, Boren SA. Managing clinical knowledge for health care improvement. In: Yearbook of Medical Informatics 2000: Patient-Centered Systems. Stuttgart, Germany: Schattauer. 2000:65–70. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Table S1. Study characteristics and application of codes.
Appendix File S1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Appendix File S2. Search terms.
Appendix File S3. Codebook used in the present study.


