Abstract
Study Objective:
Buprenorphine treatment for opioid use disorder provided in the emergency department with subsequent buprenorphine treatment by community prescribers is associated with improved outcomes, but the frequency with which this occurs is unknown. We examined rates of subsequent buprenorphine treatment for buprenorphine naïve individuals filling a buprenorphine prescription from an emergency physician and initiated buprenorphine treatment and how such rates varied before and during the COVID-19 pandemic.
Methods:
Using pharmacy claims capturing an estimated 92% of prescriptions filled at U.S. retail pharmacies, we identified buprenorphine prescriptions filled between February 1, 2019, and November 30, 2020, written by emergency physicians. In this observational study, we calculated the rate at which patients subsequently filled buprenorphine prescriptions from another non-emergency clinicians, the frequency with which subsequent filled prescriptions were from different types of prescribers, and changes in the rate of subsequent prescriptions following declaration of the COVID-19 public health emergency.
Results:
We identified 22,846 prescriptions written by emergency physicians filled by buprenorphine naïve patients. They were most commonly paid for by Medicaid and were in metropolitan counties; 28.5% of patients subsequently filled a buprenorphine prescription written by another clinician. Adult primary care physicians and advanced practice providers (e.g., physician assistants and nurse practitioners) were responsible for most of the subsequent prescriptions. Rates of subsequent prescriptions were 3.5% lower after the COVID-19 public health emergency declaration.
Conclusion:
The majority of patients filling buprenorphine prescriptions written by emergency physicians do not subsequently fill a prescription written by another clinician, and rates of subsequent prescriptions were lower after declaration of the COVID-19 public health emergency. These findings highlight the need for a system of care that improves buprenorphine treatment continuity of care for patients with opioid use disorder from emergency settings to community treatment providers.
INTRODUCTION
Background:
In the U.S., emergency departments averaged over 222 opioid-related emergency department visits per 100,000 population visits in 2018, over 720,000 visits.1 This tally includes increasing numbers of individuals experiencing an overdose2 as well as many other individuals with opioid use disorder (OUD) for whom the emergency department is their primary source of contact with the healthcare system3 and source of care for opioid-related issues.1,4
Medication treatment for opioid use disorder (MOUD) is the standard of care for OUD,5 improving quality of life and decreasing fatal overdose rates.6–11 Unfortunately, fewer than 12% of individuals treated in an emergency department for a non-fatal opioid overdose subsequently receive MOUD,11–13 despite more than 5% of individuals receiving treatment in an emergency department dying in the subsequent year.14
One promising strategy is for emergency departments to provide medication treatment to individuals with OUD who are not currently receiving MOUD and then link the patient to non-emergency department providers who can provide subsequent ongoing treatment for OUD.15–21 Such “bridge” models of care commonly use buprenorphine as it can be readily provided by clinicians in the emergency department. Randomized clinical trials have found that providing buprenorphine treatment for OUD in the emergency department, with subsequent handoff for continued treatment by another prescribing clinician, is associated with sustained engagement in care for substance use disorder20 and reduced illicit opioid use at 60 days, compared to referral for treatment or a brief intervention.19 Prescribing buprenorphine treatment in the emergency department reduces barriers to care often experienced by individuals seeking MOUD in other treatment settings,22,23 facilitating access to effective treatment at a time when individuals may be more receptive to starting it. A cost-effective practice18 that has been replicated in non-academic settings,24,25 providing buprenorphine in the emergency department holds substantial promise for improving access to and utilization of sustained medication treatment for OUD.
The COVID-19 pandemic disrupted access to care for many individuals, especially historically disadvantaged populations,26–29 and has seen the highest fatal overdose rates ever and increased emergency department visits for opioid overdose.30–33 While overall use of buprenorphine did not appear to decrease during the pandemic, several studies have found decreases in the number of individuals beginning buprenorphine treatment after the start of the pandemic.34,35 As a result, we hypothesized that rate of patients filling buprenorphine prescriptions from emergency physicians subsequently filling buprenorphine prescriptions from clinicians other than emergency physicians would be lower after the declaration of the COVID-19 public health emergency than before the declaration.
Importance:
We are unaware of national studies examining to what extent patients filling buprenorphine prescriptions from emergency physicians subsequently fill buprenorphine prescriptions from clinicians other than emergency physicians or how these rates may have been influenced by the COVID-19 pandemic. To address this knowledge gap, we used data on filled buprenorphine prescriptions in 2019 and 2020 from a national dataset of retail pharmacy fills to examine these issues.
Goals of This Investigation:
The study’s primary objective was to determine the frequency with which buprenorphine naïve patients filling buprenorphine prescriptions written by emergency physicians subsequently filled a buprenorphine prescription from a different clinician and to examine if the rates of such subsequent buprenorphine prescription fills changed following the declaration of the COVID-19 public health emergency in March 2020.
METHODS
Study design and setting
We used January 1, 2019, through December 31, 2020, de-identified pharmacy claims from the IQVIA Real World Data – Longitudinal Prescriptions36 to identify filled buprenorphine prescriptions written by emergency physicians identified in the IQVIA data. IQVIA is a health technology company which compiles prescription dispensation data from retail pharmacies. These data, which capture an estimated 92% of all prescriptions filled at retail pharmacies in all 50 U.S. states and the District of Columbia, contain information on the prescription, payer, patient demographics, and prescribing provider specialty and geographic location. The study was approved with a waiver of consent by the corresponding author’s Institutional Review Board.
Measurements
We identified prescriptions for a buprenorphine formulation with an FDA-approved indication for OUD treatment (e.g., sublingual buprenorphine, buprenorphine/naloxone, extended-release buprenorphine) written by an emergency physician that were filled from February 1, 2019, through November 30, 2020. Emergency physicians were identified using the IQVIA data, with specialty confirmed using information on clinician specialty in the National Plan and Provider Enumeration System (NPPES) data.37 We excluded prescriptions written by an emergency physician if in the 30-day period prior to the filled prescription from an emergency physician the patient had medication from a previously filled buprenorphine prescription, focusing on patients not currently receiving buprenorphine treatment (hereafter buprenorphine naïve). To exclude prescriptions written by emergency physicians who may have been “moonlighting” (providing ongoing buprenorphine treatment in a non-acute setting),24 we excluded prescriptions if the emergency physician prescribed two or more consecutive filled prescriptions that supplied more than 14 total days of buprenorphine. January 2019 data was used to ensure patients had not filled a buprenorphine prescription in the 30 days prior to the first observed prescription fill from an emergency physician, and we excluded prescriptions filled in December 2020 data to ensure we could identify prescriptions filled in the 30 days subsequent to a prescription filled from an emergency physician.
We identified the clinician, other than an emergency physician, who was the prescriber of a second buprenorphine prescription filled within 30 days of the buprenorphine fill from the emergency physician, adopting the same time frame as used in the HEDIS measure for follow-up care following high intensity care for substance use disorder.38 Recognizing that in some situations a patient may return to the emergency department for a second bridge prescription if unable to engage in care, in situations in which an emergency physician wrote the second filled prescription and the total days’ supply of the first two prescriptions was 14 days or less, we identified the prescriber of the third filled prescription. We categorized subsequent prescribers by specialty: addiction specialists (e.g., addiction medicine and addiction psychiatry), adult primary care physician (e.g., internal medicine and family practice (PCPs)); advance practice providers (e.g., nurse practitioners and physician assistants {APPs)); psychiatrists; pain specialists (e.g., anesthesiologists and neurologists); and other physicians.
We categorized patients filling a buprenorphine prescription written by an emergency physician by sex and age group (12–17 years, 18–25, 26–35, 36–45, 46–55, 56–65 and over 65 years), and the source of payment for the buprenorphine prescription (Medicaid; Medicare; commercial insurance; cash payment; pharmacy prescription discount cards/prescription coupons/vouchers; or other, which included Tricare and workers compensation). We used the 5-digit FIPS code of the emergency physician to determine the county in which the buprenorphine treatment episode occurred. As in prior research, we determined county urbanicity based on Rural-Urban Continuum Codes (RUCC) from the Area Health Resources Files (AHRF), with counties classified as “urban” (RUCC 1, 2, or 3), “rural adjacent” (RUCC 4, 6, or 8), or “rural remote” (RUCC 5, 7, or 9). We calculated county drug overdose rates as the per capita rate of overdose deaths due to any drug, using the 2018 restricted multiple-cause-of-death mortality file from the Centers for Disease Control and Prevention;39 we calculated a county’s percentage of Black and Hispanic residents using the American Community Survey. We designated the period before the federal declaration of the COVID pandemic on March 13, 2020, as pre-COVID-19 public health emergency; we categorized the period after that date as COVID-19 public health emergency.
Analysis
We first calculated the number and percentages of filled buprenorphine prescriptions written by emergency physicians by patient and county characteristics. Our primary outcome was the percentage of these prescriptions with a subsequent filled buprenorphine prescription written by another clinician. We present the monthly numbers of individuals with filled buprenorphine prescriptions written by emergency physicians and the percentage of those filled prescriptions for which the individual filled a subsequent buprenorphine prescription written by another clinician within 30 days. Finally, we conducted a bivariate analysis to examine if there was a significant difference before and after the declaration of the COVID-19 public health emergency with respect to patient or county characteristics of filled buprenorphine prescriptions written by emergency physicians or the rate at which individuals filling such prescriptions subsequently filled another buprenorphine prescription written by another prescriber. All analyses were done in SAS 9.4.
RESULTS
We identified 22,846 buprenorphine prescriptions written by emergency physicians and filled by buprenorphine naïve patients between February 1, 2019, and November 30, 2020. Compared with other populations, such prescriptions were more common among males (59.6%) and among individuals 26 to 35 years of age (39.8%); prescriptions were most commonly paid for by Medicaid (44.5%) (Table 1). Most of the emergency physicians whose prescriptions were filled by buprenorphine naïve patients were from metropolitan counties (88.6%). Emergency physicians in the counties in the quartile with the highest fatal overdose rate in the prior year were responsible for 57.3% of the buprenorphine prescriptions.
Table 1.
Characteristics of Buprenorphine Treatment Episodes initiated by an Emergency physician, January 1 2019–November 30, 2020
| Overall % | Overall N | Pre-COVID Public Health Emergency N (%) | Post-COVID Public Health Emergency N (%) | |
|---|---|---|---|---|
| Total | 22,846 | 14,456 | 8,390 | |
| Sex | ||||
| Female | 40.4 | 9,232 | 5,993 (41.8) | 3,239 (38.6) |
| Male | 59.6 | 13,614 | 8,463 (58.2) | 5,151 (61.4) |
| Age Cohort | ||||
| 12–17 | 0.1 | 31 | 19 (0.1) | 12 (0.1) |
| 18–25 | 9.0 | 2,046 | 1,217 (8.4) | 829 (9.9) |
| 26–35 | 39.8 | 9,098 | 5,714 (39.5) | 3,384 (40.3) |
| 36–45 | 29.2 | 6,669 | 4,261 (29.5) | 2,408 (28.7) |
| 46–55 | 13.3 | 3,036 | 1,995 (13.8) | 1,041 (12.4) |
| 56–65 | 6.6 | 1,518 | 963 (6.7) | 555 (6.6) |
| 66+ | 2.0 | 448 | 287 (2.0) | 161 (1.9) |
| First Buprenorphine prescription payer | ||||
| Medicare | 5.5 | 1,253 | 820 (5.7) | 433 (5.2) |
| Medicaid | 44.5 | 10,167 | 6,240 (43.2) | 3,927 (46.8) |
| Commercial | 14.7 | 3,346 | 2,238 (15.5) | 1,108 (13.2) |
| Cash | 9.6 | 2,181 | 1,386 (9.6) | 795 (9.5) |
| Discount card/ Voucher | 15.3 | 3,498 | 2,131 (14.7) | 1,367 (16.3) |
| Other | 9.7 | 2,226 | 1,517 (10.5) | 709 (8.5) |
| Emergency Department Prescriber County Urban-Rural Status | ||||
| Metropolitan | 88.6 | 20,237 | 12,666 (87.6) | 7,571 (90.2) |
| Rural Adjacent | 8 | 1,823 | 1,241 (8.6) | 582 (6.9) |
| Rural Remote | 3.4 | 786 | 549 (3.8) | 237 (2.8) |
| 2018 county OD rate quartile | ||||
| Lowest | 8.1 | 1,854 | 1,192 (8.3) | 662 (7.9) |
| 2 | 12.6 | 2,877 | 1,987 (13.8) | 890 (10.6) |
| 3 | 22 | 5,014 | 3,421 (23.7) | 1,593 (19.0) |
| Highest | 57.3 | 13,101 | 7,856 (54.3) | 5,245 (62.5) |
Emergency physicians wrote 14,456 buprenorphine prescriptions filled by buprenorphine naïve patients from February 2019 through March 12, 2020. The COVID-19 public health emergency was declared on March 13, 2020, and emergency physicians wrote 8390 buprenorphine prescriptions filled by buprenorphine naïve patients from that date through November 30, 2020. In the first several months of the pandemic, there was a decline in the number of filled prescriptions written by emergency physicians, but by June 2020, the monthly number of filled prescriptions was comparable to pre-pandemic numbers. (Figure 1) Prescriptions filled after the public health emergency was declared were more likely than prescriptions filled before the public health emergency was declared to be filled by males (61.4% vs. 58.5%; a 2.8% difference (95% CI 1.5 to 4.2)), paid for by Medicaid (46.8% vs 43.2%; a 3.6% difference (95% CI 5.0 to 2.3)), and written by prescribers in metropolitan counties (90.2% vs 87.6%; a 2.6% difference (95% CI 1.8 to 3.5)),and in counties in the top quartile of 2018 fatal overdose rate (62.5% vs 54.3%; a 8.2% difference (95% CI 6.9 to 9.5)). (Table 1)
Figure 1.
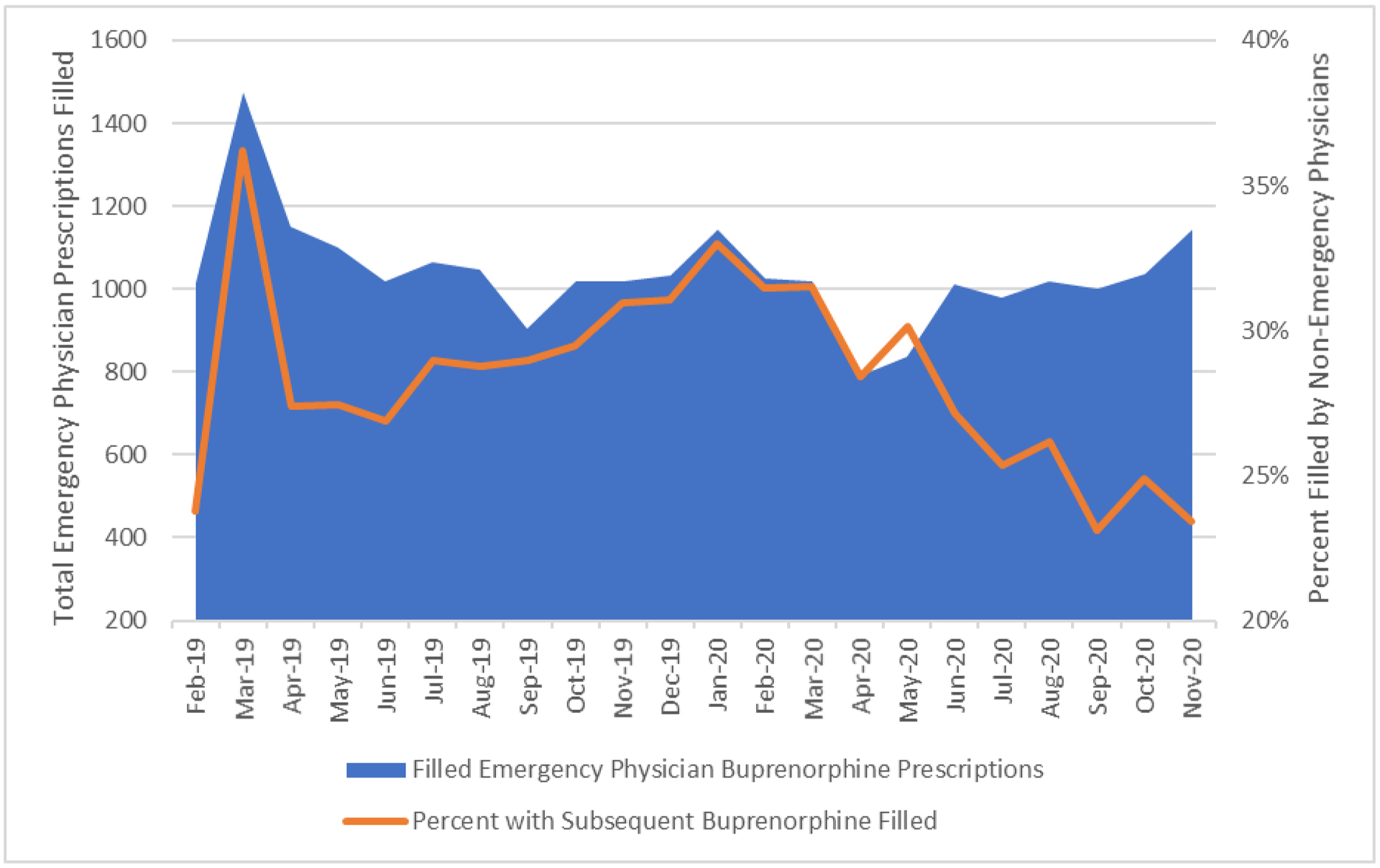
Number of filled buprenorphine prescriptions written by emergency physicians and the precent of those prescriptions with a prescription filled in 30 days written by another clinician, 2019–2020
Subsequent filled buprenorphine prescriptions
We found that 71.5% of filled buprenorphine prescriptions written by an emergency physician were not followed by the patient filling a buprenorphine prescription written by another clinician within 30 days; prescriptions filled after the declaration of the public health emergency were less likely to have a subsequent filled prescription than buprenorphine prescriptions filled before the public health emergency (73.7% vs 70.2%; a 3.6% difference (95% CI 2.4 to 4.8)) (Table 2) In contrast to the pattern observed for filled prescriptions written by emergency physicians, which returned to pre-pandemic levels by June 2020, the percentage of prescriptions written by an emergency physician that subsequently had the patient filling a buprenorphine prescription written by another clinician continued to decline overall throughout the rest of the period we observed. (Figure 1) Adult PCPs wrote 12.6% (n=2872) of subsequent buprenorphine prescriptions filled during 2019 and 2020, with APPs writing 7.0% of subsequent buprenorphine prescriptions filled. After declaration of the public health emergency, subsequent buprenorphine prescriptions were slightly more likely to be written by APPs and less likely to be written by physicians. There were only modest differences with respect to the rate of subsequently filled prescriptions with respect to patient demographics, payer, and characteristics of the prescriber county. (Table 2)
Table 2.
Rates of continuation of buprenorphine episodes initiated by an emergency physician January 1, 2019–November 30, 2020, overall and before and after declaration of the COVID public health emergency
| Overall % | Overall N | Pre-COVID Public Health Emergency N (%) | Post-COVID Public Health Emergency N (%) | |
|---|---|---|---|---|
| Episode Not Continued | 71.5 | 16,331 | 10,144 (70.2) | 6,187 (73.7) |
| Episode Continued | 28.5 | 6,515 | 4,312 (29.8) | 2,203 (26.3) |
| Among episodes continued | ||||
| Episode Continued by | ||||
| Adult PCP | 44.1 | 2,872 | 1,914 (44.4) | 958 (43.5) |
| APP | 24.4 | 1,591 | 914 (21.2) | 677 (30.7) |
| Psychiatrist | 7.1 | 461 | 299 (6.9) | 162 (7.4) |
| Pain Specialist | 2.1 | 134 | 93 (2.2) | 41 (1.9) |
| Addiction Specialist | 1.6 | 103 | 62 (1.4) | 41 (1.9) |
| Other Physician | 20.8 | 1,354 | 1,030 (23.9) | 324 (14.7) |
| Sex | ||||
| Female | 40.5 | 2,640 | 1,759 (40.79) | 881 (39.99) |
| Male | 59.4 | 3,875 | 2,553 (59.2) | 1,322 (60.0) |
| Age Cohort | ||||
| 12–17 | 0.1 | 7 | 3 (0.1) | 4 (0.2) |
| 18–25 | 8.9 | 579 | 362 (8.4) | 217 (9.9) |
| 26–35 | 39.6 | 2,578 | 1,672 (38.8) | 906 (41.1) |
| 36–45 | 29.9 | 1,947 | 1,314 (30.5) | 633 (28.7) |
| 46–55 | 13.6 | 888 | 621 (14.4) | 267 (12.1) |
| 56–65 | 6.3 | 409 | 269 (6.2) | 140 (6.4) |
| 66+ | 1.6 | 107 | 71 (1.7) | 36 (1.6) |
| First Buprenorphine prescription payer | ||||
| Medicare | 6.2 | 406 | 273 (6.3) | 133 (6.0) |
| Medicaid | 51.5 | 3,352 | 2,184 (50.7) | 1,168 (53.0) |
| Commercial | 13.3 | 869 | 592 (13.7) | 277 (12.6) |
| Cash | 7 | 457 | 311 (7.2) | 146 (6.6) |
| Discount card/ Voucher | 10.8 | 706 | 437 (10.1) | 269 (12.2) |
| Other | 8.8 | 576 | 406 (9.4) | 170 (7.7) |
| Emergency Department Prescriber County Urban-Rural Status | ||||
| Metropolitan | 90.9 | 5,920 | 3,894 (90.3) | 2,026 (92.0) |
| Rural Adjacent | 6.4 | 415 | 285 (6.6) | 130 (5.9) |
| Rural Remote | 2.8 | 180 | 133 (3.1) | 47 (2.1) |
| 2018 county OD rate quartile | ||||
| Lowest | 5.9 | 382 | 245 (5.7) | 137 (6.2) |
| 2 | 13.3 | 863 | 607 (14.1) | 256 (11.6) |
| 3 | 22 | 1,435 | 944 (21.9) | 491 (22.3) |
| Highest | 58.9 | 3,835 | 2,516 (58.4) | 1,319 (59.9) |
LIMITATIONS
Our findings must be considered within the context of the study’s limitations. We observed only buprenorphine prescriptions filled at a pharmacy and have no information about buprenorphine dispensed in an emergency department, residential treatment, or inpatient hospitals. We also cannot assess how often prescriptions were written but not filled, which may occur more frequently for prescriptions written in the emergency department or individuals seeing a clinician for the first time than for prescriptions written in settings in which individuals are engaged in routine care. We did not observe situations where physicians refrained from prescribing due to a concern that patients would be unwilling or unable to receive follow-up treatment. We have no information regarding individuals who have had fatal overdoses or died from other causes nor about individuals receiving methadone treatment for OUD. Some patients receiving buprenorphine from emergency physicians may be switched to methadone maintenance treatment, extended-release naltrexone, or non-pharmacologic treatment when seen subsequently, and for some patients with OUD seen in emergency departments, buprenorphine treatment is not appropriate.
We have no information about non-pharmacological treatment, the emergency physician writing the prescription, nor the clinical setting in which prescriptions were written and are unable to examine physician or clinical setting factors associated with emergency physician prescribing and continuation by other prescribers. We sought to exclude emergency physicians moonlighting as buprenorphine prescribers in non-acute care settings; however, it is possible we included such episodes when the patient did not fill the second or third prescription. We may also have inadvertently excluded some prescriptions written by emergency physicians working in the emergency department, particularly early in the COVID-19 pandemic when it may have been more difficult for patients to obtain services from a buprenorphine prescriber in the community.40 We cannot identify prescriptions written by non-emergency physicians working in an emergency department, an arrangement likely to be more common in more rural communities.41 We also have no information on patient race/ethnicity, factors associated with the likelihood of receiving buprenorphine,42 nor do we have sufficient data to examine buprenorphine treatment duration for individuals filling a prescriptions subsequent to the one filled from the emergency physician. We restricted our analysis to FDA-approved formulations for treating OUD, but those formulations may be used off label to treat pain, and we do not know that individuals are receiving the medication for OUD treatment.
We have no information regarding why individuals who initially filled a buprenorphine prescription written by an emergency physician did not subsequently fill another prescription within 30 days. Specifically, we cannot determine to what extent this occurs due to lack of access to another buprenorphine prescriber, inability to pay, lack of desire to continue buprenorphine treatment, being switched to methadone, or some other reason. Future research examining factors associated with individuals receiving buprenorphine from emergency physicians successfully engaging and continuing to receive buprenorphine treatment or treatment for OUD more generally is needed. Being unaware of existing standards or research examining to what extent the duration of time that passes between discharge from an emergency department to engaging in medication treatment for OUD is associated with successful engagement of positive clinical outcomes, we adopted the 30-day window from the HEDIS measure for follow-up after high intensity care for substance use disorder.38 This is another area on which further research is needed. Finally, IQVIA data capture only 92% of prescriptions filled at retail pharmacies; pharmacy coverage is not known to vary systematically by region or type of organization or entity, but we do not know if our results generalize to prescriptions filled in pharmacies not captured by IQVIA.
DISCUSSION
Despite these limitations, our study provides the first national assessment of the frequency with which individuals filling buprenorphine prescriptions from emergency physicians subsequently fill buprenorphine prescriptions written by other clinicians. As the opioid crisis worsens, opioid-related emergency department visits have increased.43,44 This trend accelerated during the COVID-19 pandemic,30–32 a period which also saw record numbers of fatal overdoses.45 However, we found that during 2019–2020, 71.5% of patients filling a buprenorphine prescription written by an emergency physician did not fill a subsequent buprenorphine prescription from another clinician; the rate of subsequent buprenorphine prescription fills was worse after the COVID-19 public health emergency was declared with a continued decline for the remainder of 2020.
Because OUD is a chronic disorder and the duration of buprenorphine treatment is strongly associated with improved clinical outcomes,46 providing buprenorphine to patients being seen in emergency departments is not enough. Improved outcomes require successfully linking patients to community providers who can provide medication treatment. States and other stakeholders have invested in efforts to increase emergency department delivery of buprenorphine47; our results suggest that it is critical to complement these efforts with initiatives to enhance linkage to ongoing treatment.
There are several ways that emergency departments can help to connect individuals with subsequent medication treatment for OUD. The American College of Emergency Physicians48 recommends a direct specific referral or scheduling an appointment with a prescriber who accepts the patient’s insurance. This is the model used in a range of studies demonstrating the effectiveness of emergency department delivered buprenorphine.19,20,49,50 However, this approach only works if local clinicians are accepting new buprenorphine patients, and studies suggest that many buprenorphine prescribing clinicians are not treating many patients51 or are not accepting new ones.22,23 Reducing barriers to buprenorphine prescribing, such as federal action to drop training requirements to obtain a waiver to treat up to 30 patients with buprenorphine, may increase access to ongoing treatment. Efforts to support and enhance emergency department efforts are important, but adequately addressing the issue will likely require a range of more concerted workforce, systems, and payer strategies to increase community treatment capacity.52
Given that emergency departments are commonly located within hospitals and health systems, establishing bridge clinics or primary care clinics in the hospital or health system affiliated with the emergency department that can quickly see patients who have first received buprenorphine in the emergency department is a potentially promising model associated with good clinical outcomes.4,19 However, it requires administrative leadership and sufficient resources to establish and adequate ongoing reimbursement from payers. Additional promising non-pharmacologic strategies include delivering a brief intervention in the emergency department designed to enhance a patient’s motivation to engage in treatment53 and using peers to facilitate engagement with subsequent treatment.54 However, emergency departments are not routinely reimbursed for such activities; consequently, they are unlikely to be incorporated when emergency physicians prescribe buprenorphine.
State Medicaid agencies may be particularly well suited to support initiatives to facilitate buprenorphine treatment after a patient receives buprenorphine from an emergency physician, as almost half of such prescriptions were paid for by Medicaid. State Medicaid officials would be able to use claims data to calculate such rates and provide feedback to hospitals and communities. Calculations of such rates of subsequent engagement already occur for emergency department visits for individuals with mental illness,{National Committee for Quality Assurance (NCQA), 2021 #57} and rates of engagement in subsequent treatment are consistent with measures proposed by experts to assess the quality of emergency department treatment of OUD.55 While addiction specialists, pain specialists, and psychiatrists represent approximately a quarter of active buprenorphine prescribers and high-volume buprenorphine prescribers,51 they represent a much smaller percentage of clinicians who had prescriptions filled by patients subsequent to those patients filling buprenorphine prescriptions from emergency physicians. Since clinicians may often have additional training enabling them to better address the needs of more complicated patients such as those who often present to emergency departments, a particular focus on enhancing linkage to such clinicians may be particularly warranted.
We found a modest but statistically significant decrease after the declaration of the COVID-19 public health emergency in the percentage of patients filling a subsequent buprenorphine prescription, but the magnitude of the decrease was much less than seen for many other types of health care services,26–28 and the return to pre-pandemic levels more rapid than seen for many other services. Federal and state officials took a number of actions to facilitate access to buprenorphine treatment after the public health emergency was declared, including relaxing federal guidelines related to telemedicine use as well as a range of state policy changes designed to facilitate access to substance use disorder treatment services.56,57 However, the rate at which individuals filling a prescription subsequently filled a buprenorphine prescription from another clinician continued to decline. Actions taken during the pandemic, such as the relaxation of regulations regarding telehealth and buprenorphine, have the potential of improving rates of subsequent treatment of individuals filling buprenorphine prescriptions written by emergency physicians in communities with insufficient local community buprenorphine prescribers, with the caveat that many of the most vulnerable individuals with OUD may not have the technology necessary to benefit from such policy changes.58
CONCLUSION
The American College of Emergency Physicians has issued a consensus statement recommending initiating buprenorphine to treat OUD and linking patients with OUD to some form of ongoing treatment.48 This consensus, coupled with a quality framework for emergency department treatment of OUD that includes MOUD,55 will likely accelerate the promising trend of increased emergency department buprenorphine prescribing. Yet our findings underscore that there is substantial room for improvement to create a system of care that seamlessly transitions patients from emergency settings to community treatment providers. While there is a strong proof of concept from clinical trials, the remaining challenge is to implement these models across diverse systems and to incentivize policymakers, insurers, and health systems to provide the necessary resources and infrastructure for such programs to be successful.
ACKNOWLEDGEMENTS
The authors thank Mary Vaiana Ph.D. and Hilary Peterson B.A., both of the RAND Corporation, for their feedback and editorial assistance on earlier versions of the manuscript.
Funding Source
This work was supported by the National Institute on Drug Abuse (NIDA) through P50DA046351 (Stein), R01DA045800-01 (Stein, PI) and K01DA042139 (Saloner, PI) and the Fore Foundation (Stein, PI)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors have no conflicts to disclose.
Contributor Information
Bradley D. Stein, RAND Corporation, Pittsburgh PA.
Brendan Saloner, Department of Health Policy and Management, Johns Hopkins University, Baltimore MD.
Rose Kerber, RAND Corporation, Boston, MA.
Mark Sorbero, RAND Corporation, Pittsburgh PA.
Adam J. Gordon, Program for Addiction Research, Knowledge, and Advocacy, University of Utah School of Medicine and VA Salt Lake City Health Care System, Salt Lake City, UT.
References
- 1.Healthcare Cost and Utilization Project (HCUP). HCUP Fact Stats: Opioid-Related Hospital Use. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ); September 2021: www.hcup-us.ahrq.gov/faststats/opioid/opioiduse.jsp?radio3=on&location1=US&characteristic1=01&setting1=ED&location2=&characteristic2=01&setting2=ED&expansionInfoState=hide&dataTablesState=show&definitionsState=hide&exportState=hide. Accessed November 29, 2021. [Google Scholar]
- 2.Vivolo-Kantor AM, Seth P, Gladden RM, et al. Vital Signs: Trends in emergency department visits for suspected opioid overdoses - United States, July 2016-September 2017. MMWR Morb Mortal Wkly Rep. 2018;67(9):279–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sohler NL, Wong MD, Cunningham WE, Cabral H, Drainoni ML, Cunningham CO. Type and pattern of illicit drug use and access to health care services for HIV-infected people. AIDS Patient Care STDS. 2007;21 Suppl 1:S68–76. [DOI] [PubMed] [Google Scholar]
- 4.Martin A, Butler K, Chavez T, et al. Beyond buprenorphine: Models of follow-up care for opioid use disorder in the emergeny department. West J Emerg Med. 2020;21(6):257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014(2):CD002207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giacomuzzi SM, Ertl M, Kemmler G, Riemer Y, Vigl A. Sublingual buprenorphine and methadone maintenance treatment: A three-year follow-up of quality of life assessment. ScientificWorldJournal. 2005;5:452–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ponizovsky AM, Margolis A, Heled L, Rosca P, Radomislensky I, Grinshpoon A. Improved quality of life, clinical, and psychosocial outcomes among heroin-dependent patients on ambulatory buprenorphine maintenance. Subst Use Misuse. 2010;45(1–2):288–313. [DOI] [PubMed] [Google Scholar]
- 8.Ponizovsky AM, Grinshpoon A. Quality of life among heroin users on buprenorphine versus methadone maintenance. Am J Drug Alcohol Abuse. 2007;33(5):631–642. [DOI] [PubMed] [Google Scholar]
- 9.Giacomuzzi SM, Riemer Y, Ertl M, et al. Buprenorphine versus methadone maintenance treatment in an ambulant setting: A health-related quality of life assessment. Addiction. 2003;98(5):693–702. [DOI] [PubMed] [Google Scholar]
- 10.Morgan JR, Schackman BR, Weinstein ZM, Walley AY, Linas BP. Overdose following initiation of naltrexone and buprenorphine medication treatment for opioid use disorder in a United States commercially insured cohort. Drug Alcohol Depend. 2019;200:34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Annals of Internal Medicine. 2018;169(3):137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koyawala N, Landis R, Barry CL, Stein BD, Saloner B. Changes in outpatient services and medication use following a non-fatal opioid overdose in the West Virginia Medicaid program. J Gen Intern Med. 2019;34(6):789–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frazier W, Cochran G, Lo-Ciganic WH, et al. Medication-assisted treatment and opioid use before and after overdose in Pennsylvania Medicaid. JAMA. 2017;318(8):750–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiner SG, Baker O, Bernson D, Schuur JD. One-year mortality of patients after emergency department treatment for nonfatal opioid overdose. Ann Emerg Med. 2020;75(1):13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCormack RP, Rotrosen J, Gauthier P, et al. Implementation facilitation to introduce and support emergency department-initiated buprenorphine for opioid use disorder in high need, low resource settings: Protocol for multi-site implementation-feasibility study. Addict Sci Clin Pract. 2021;16(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bogan C, Jennings L, Haynes L, et al. Implementation of emergency department-initiated buprenorphine for opioid use disorder in a rural southern state. J Subst Abuse Treat. 2020;112S:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D’Onofrio G, Hawk KF, Herring A, et al. The design and conduct of a randomized clinical trial comparing emergency department initiation of sublingual versus a 7-day extended-release injection formulation of buprenorphine for opioid use disorder: Project ED Innovation. Contemp Clin Trials. 2021:106359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Busch SH, Fiellin DA, Chawarski MC, et al. Cost-effectiveness of emergency department-initiated treatment for opioid dependence. Addiction. 2017;112(11):2002–2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Onofrio G, Chawarski MC, O’Connor PG, et al. Emergency department-initiated buprenorphine for opioid dependence with continuation in primary care: Outcomes during and after intervention. J Gen Intern Med. 2017;32(6):660–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: A randomized clinical trial. JAMA. 2015;313(16):1636–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin A, Mitchell A, Wakeman S, White B, Raja A. Emergency department treatment of opioid addiction: An opportunity to lead. Acad Emerg Med. 2018;25(5):601–604. [DOI] [PubMed] [Google Scholar]
- 22.Beetham T, Saloner B, Wakeman SE, Gaye M, Barnett ML. Access to office-based buprenorphine treatment in areas with high rates of opioid-related mortality: An audit study. Ann Intern Med. 2019;171(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patrick SW, Richards MR, Dupont WD, et al. Association of pregnancy and insurance status with treatment access for opioid use disorder. JAMA Netw Open. 2020;3(8):e2013456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Edwards FJ, Wicelinski R, Gallagher N, McKinzie A, White R, Domingos A. Treating opioid withdrawal with buprenorphine in a community hospital emergency department: An outreach program. Ann Emerg Med. 2020;75(1):49–56. [DOI] [PubMed] [Google Scholar]
- 25.Brooks D Initiating medication-assisted treatment for patients presenting with opioid withdrawal. ED Manag. 2017;29:85–96. [Google Scholar]
- 26.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: A rebound emerges. The Commonwealth Fund; 2020: https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits. Accessed December 16, 2020. [Google Scholar]
- 27.Martin K, Kurowski D, Given P. The impact of COVID-19 on the use of preventive health care. Health Care Cost Institute. https://healthcostinstitute.org/hcci-research/the-impact-of-covid-19-on-the-use-of-preventive-health-care. Published 2020. Accessed October 26, 2020. [Google Scholar]
- 28.Epic Health Research Network. Expansion of Telehealth during COVID-19 Pandemic. https://ehrnprd.blob.core.windows.net/wordpress/pdfs/Expansions-in-Telehealth-COVID-19. Published 2020. Accessed October 26, 2020.
- 29.Saloner B, Krawczyk N, Solomon K, et al. Experiences with substance use disorder treatment during the COVID-19 pandemic: Findings from a multistate survey. Int J Drug Policy. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soares WE 3rd, Melnick ER, Nath B, et al. Emergency department visits for nonfatal opioid overdose during the COVID-19 pandemic across six US health care systems. Ann Emerg Med. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Root ED, Slavova S, LaRochelle M, et al. The impact of the national stay-at-home order on emergency department visits for suspected opioid overdose during the first wave of the COVID-19 pandemic. Drug Alcohol Depend. 2021;228:108977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(4):372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Drug Overdose Deaths in the U.S. Top 100,000 Annually. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm. Published 2021. Updated November 17. Accessed January 18, 2022.
- 34.Currie JM, Schnell MK, Schwandt H, Zhang J. Prescribing of opioid analgesics and buprenorphine for opioid use disorder during the COVID-19 pandemic. JAMA Netw Open. 2021;4(4):e216147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chalasani R, Shinabery JM, Goetz CT, et al. Buprenorphine dispensing in Pennsylvania during the COVID-19 pandemic, January to October 2020. J Gen Intern Med. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.IQVIA: Real World Data and Insights. https://www.iqvia.com/solutions/real-world-evidence/real-world-data-and-insights. Accessed July 13, 2020.
- 37.National Bureau of Economic Research. National Plan and Provider Enumeration System (NPPES). https://www.nber.org/research/data/national-plan-and-provider-enumeration-system-nppes. Published Undated. Accessed January 18, 2022.
- 38.National Committee for Quality Assurance (NCQA). Follow-Up After High-Intensity Care for Substance Use Disorder (FUI). https://www.ncqa.org/hedis/measures/follow-up-after-high-intensity-care-for-substance-use-disorder/. Published 2021. Accessed January 12, 2022.
- 39.Centers for Disease Control Prevention. Drug Overdose Deaths. https://www.cdc.gov/drugoverdose/data/statedeaths.html. Published 2020. Accessed May 20, 2020.
- 40.Routsolias J, Mycyk M. The coronavirus disease pandemic continues to challenge patients in need of buprenorphine for opioid use disorder. J Emerg Nurs. 2021;47:376–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Banks G, Wingrove P, Petterson SM, Klink K. Family physicians contribute significantly to emergency care of Medicare patients in urban and suburban areas. Am Fam Physician. 2015;92(6):445. [PubMed] [Google Scholar]
- 42.Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76(9):979–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tedesco D, Asch SM, Curtin C, et al. Opioid abuse and poisoning: Trends in inpatient and emergency department discharges. Health Aff (Millwood). 2017;36(10):1748–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guy GP Jr., Pasalic E, Zhang K. Emergency department visits involving opioid overdoses, U.S., 2010–2014. Am J Prev Med. 2018;54(1):e37–e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ahmad F, Rossen L, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics; 2020. [Google Scholar]
- 46.Samples H, Williams AR, Crystal S, Olfson M. Impact of long-term buprenorphine treatment on adverse health care outcomes in Medicaid. Health Aff (Millwood). 2020;39(5):747–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kilaru AS, Lubitz SF, Davis J, et al. A state financial incentive policy to improve emergency department treatment for opioid use disorder: A qualitative study. Psychiatr Serv. 2021;72(9):1048–1056. [DOI] [PubMed] [Google Scholar]
- 48.Hawk K, Hoppe J, Ketcham E, et al. Consensus recommendations on the treatment of opioid use disorder in the emergency department. Ann Emerg Med. 2021;78(3):434–442. [DOI] [PubMed] [Google Scholar]
- 49.Regan S, Howard S, Powell E, et al. Emergency department-initiated buprenorphine and referral to follow-up addiction care: A program description. J Addict Med. 2021. [DOI] [PubMed] [Google Scholar]
- 50.McLane P, Scott K, Suleman Z, et al. Multi-site intervention to improve emergency department care for patients who live with opioid use disorder: A quantitative evaluation. CJEM. 2020;22(6):784–792. [DOI] [PubMed] [Google Scholar]
- 51.Stein BD, Saloner B, Schuler MS, Gurvey J, Sorbero M, Gordon AJ. Concentration of patient care among buprenorphine-prescribing clinicians in the US. JAMA. 2021;325(21):2206–2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Saloner B, Andraka Christou B, Gordon AJ, Stein BD. It will end in tiers: A strategy to include “dabblers” in the buprenorphine workforce after the X-waiver. Subst Abus. 2021;42(2):153–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.D’Onofrio G, Pantalon MV, Degutis LC, Fiellin DA, O’Connor PG. Development and implementation of an emergency practitioner-performed brief intervention for hazardous and harmful drinkers in the emergency department. Acad Emerg Med. 2005;12(3):249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McGuire AB, Powell KG, Treitler PC, et al. Emergency department-based peer support for opioid use disorder: Emergent functions and forms. J Subst Abuse Treat. 2020;108:82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Samuels EA, D’Onofrio G, Huntley K, et al. A quality framework for emergency department treatment of opioid use disorder. Ann Emerg Med. 2019;73(3):237–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Andraka-Christou B, Bouskill K, Haffajee RL, et al. Common themes in early state policy responses to substance use disorder treatment during COVID-19. Am J Drug Alcohol Abuse. 2021;47(4):486–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pessar SC, Boustead A, Ge Y, Smart R, Pacula RL. Assessment of state and federal health policies for opioid use disorder treatment during the COVID-19 pandemic and beyond. JAMA Health Forum. 2021;2(11):e213833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khatri UG, Perrone J. Opioid Use Disorder and COVID-19: Crashing of the Crises. J Addict Med. 2020;14(4):e6–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]


