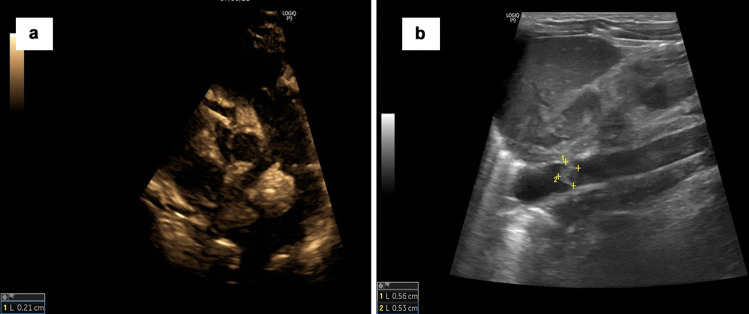
To the Editor: Some of the recent reports suggest the occurrence of multisystem inflammatory syndrome in neonates (MIS-N) [1–4]. We report here two cases of possible MIS-N. In the first case, a term male baby presented at birth with refractory persistent pulmonary hypertension of the newborn (PPHN) with persistent cardiac dysfunction and coagulopathy. Mother had asymptomatic COVID infection in the first trimester and had an exposure again to a COVID-positive family member during her last trimester. Echocardiography revealed dilated, hyperechogenic coronaries (Fig. 1a) with significantly elevated inflammatory markers: troponin T (0.22 ng/mL), ferritin (> 1650 ng/mL), lactate dehydrogenase (LDH, 4402 U/L), N-terminal pro–beta natriuretic peptide (NT-pro-BNP, > 35,000 pg/mL), creatinine phosphokinase (CPK, 3985 U/L), and C-reactive protein (CRP, 3.81). Anti-SARS-CoV-2 IgG antibody titers of neonate were significantly elevated with levels of 91.8 U/mL and negative IgM titers. The baby was treated with mechanical ventilation, intravenous immunoglobulin (IVIG), IV steroids, inhaled nitric oxide (iNO), sildenafil, bosentan, inotropes, vasopressors, antibiotics and diuretics, but could not be saved.
Fig. 1.
a Echocardiography image of the first case showing dilated right coronary artery (RCA) measuring 2.1 mm (+3.58 z score); the baby also had dilated left main coronary artery (LMCA) of 2.1 mm (+2.04 z score) and left anterior descending artery (LAD) of 2 mm (+4.49 z score) (not shown in the figure). b Ultrasound image of the second case showing 5.6 mm × 5.3 mm thrombus in abdominal aorta just above the left renal artery origin
The second case is of a term female baby, presented initially with PPHN requiring iNO and vasodilators, and improved. Later, the baby had unexplained severe cardiac dysfunction and hypertension on day 6 of life associated with aortic and intracardiac thrombosis (Fig. 1b). Mother had COVID-19 just prior to the delivery. Baby had high titers of IgG antibodies (> 250 u/mL) with negative IgM titers. Inflammatory markers were elevated: D-dimer (> 2 ug/mL), ferritin (> 1650 ng/mL), IL-6 (25 pg/mL), troponin T (0.09 ng/mL), and LDH (820 U/L). Baby was treated with IVIG, enoxaparin, aspirin, and antihypertensives, and was successfully discharged. Previously, there were similar reports of probable MIS-N with coronary dilatation [1–3] or thrombus [3, 4].
We conclude that MIS-N should be strongly considered in any unexplained cases of myocardial dysfunction after ruling out the common causes.
Declarations
Conflict of Interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Divekar AA, Patamasucon P, Benjamin JS. Presumptive neonatal multisystem inflammatory syndrome in children associated with coronavirus disease 2019. Am J Perinatol. 2021;38:632–636. doi: 10.1055/s-0041-1726318. [DOI] [PubMed] [Google Scholar]
- 2.Diggikar S, Nanjegowda R, Kumar A, Kumar V, Kulkarni S, Venkatagiri P. Neonatal multisystem inflammatory syndrome secondary to SARS-CoV-2 infection. J Paediatr Child Health. 2021 doi: 10.1111/jpc.15696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pawar R, Gavade V, Patil N, et al. Neonatal multisystem inflammatory syndrome (MIS-N) associated with prenatal maternal SARS-CoV-2: a case series. Children (Basel) 2021;8:572. doi: 10.3390/children8070572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lakshminrusimha S, Hudak ML, Dimitriades VR, Higgins RD. Multisystem inflammatory syndrome in neonates following maternal SARS-CoV-2 COVID-19 Infection. Am J of Perinatol. 2021 doi: 10.1055/a-1682-3075. [DOI] [PubMed] [Google Scholar]