Abstract
Background and objectives
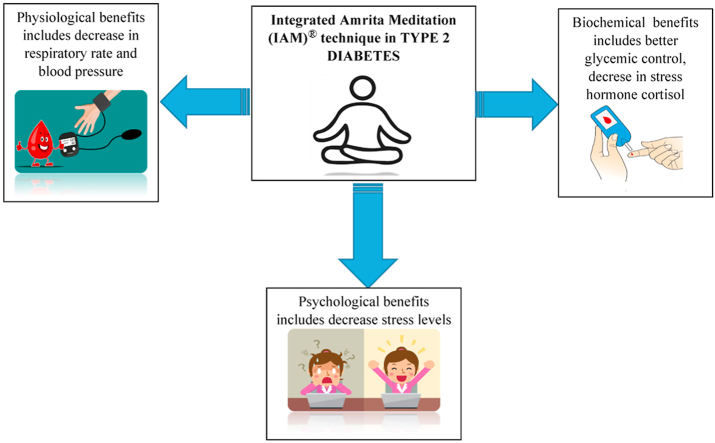
In type 2 diabetic subjects, psychological stress worsens glycemic regulation. This study put forward the various psychophysiological and biochemical benefits of the Integrated Amrita Meditation (IAM®) technique in type 2 diabetic subjects in achieving a better quality of life
Methods
This was a clinical trial conducted in the Endocrinology department of Amrita Institute of Medical Sciences. 85 type 2 diabetic subjects between the age group of 30–65 years were recruited for the study. They were randomly allocated to IAM (n = 43) and the control group (n = 42). All the physiological, biochemical, and psychological variables were assessed at baseline, 3 months, and 6 months
Results
Within the experimental group there was statistically significant reduction in heart rate, respiratory rate, blood pressure, fasting blood glucose, HbA1c, insulin and insulin resistance (p < 0.05). The average percentage changes of these variables between the groups were also significant. HDL showed an increase within the IAM®group (p < 0.001) while there was an increase in LDL and total cholesterol in the control group. Between the groups, the mean percentage changes in stress hormones cortisol and adrenaline were also significant. IgA (p = 0.002) and GABA (p = 0.007) significantly increased in the experimental group. Psychological stress assessed by perceived stress scale also showed a significant drop after the intervention in the test group and the change in perceived stress was again significant between the 2 groups comparison
Conclusion
Along with the standard treatment regimens, diabetic patients can incorporate mind-body relaxation techniques as an effective adjunctive therapy
Keywords: Diabetes, Stress, Glycemic control, Yoga, Meditation, IAM®
Graphical abstract
Highlights
-
•
This is the first study of Integrated Amrita Meditation (IAM)® Technique on diabetic subjects
-
•
Definite trend for improvement in physiological, biochemical, and psychological factors related to glycemic management
-
•
Our findings could help a lot of diabetic patients who are coping with chronic stress
List of abbreviations
- IAM®
Integrated Amrita Meditation
- T2DM
Type 2 Diabetes Mellitus
- HPA
Hypothalamic Pituitary Adrenal
- BMI
Body Mass Index
- K2EDTA
Di Potassium Ethylene Diamine Tetra Acetic acid
- FBG
Fasting Blood Glucose
- HR
Heart Rate
- RR
Respiratory Rate
- SBP
Systolic Blood Pressure
- DBP
Diastolic Blood Pressure
- HPLC
High Pressure Liquid Chromatography
- IR
Insulin resistance
- HOMA
Homeostatic Model Assessment
- CRP
C Reactive Protein
- IL6
Interleukin 6
- GABA
Gamma Amino Butyric Acid
- PSS
Perceived Stress Scale
- SD
Standard Deviation
- HDL
High Density Lipoprotein
- LDL
Low Density Lipoprotein
- IgA
Immunoglobulin A
- MDA
Malondialdehyde
- SOD
Superoxide dismutase
1. Introduction
1.1. Background and purpose of the study
In India diabetes is approaching the status of a potential epidemic as is evident from the statistics projected by International Diabetes Federation.1 Stress has long been suspected of having a significant impact on the development of diabetes.2 It was Hans Selye who introduced and popularized stress as a medical and scientific idea.3 Since type 2 diabetes mellitus (T2DM) is a psychosomatic illness, treating the somatic and symptomatic aspects of the disease alone will not help in curing the patient. The psychiatric aspect of the disease, particularly stress, must be addressed. Though we have several medications to reduce the complications of diabetes, no effective pharmacological measures are developed which can completely cure the psychological aspect of the disease i.e., stress which eventually worsens the disease4
Integrated Amrita Meditation (IAM®) technique is a form of meditation whose core lies within Indian Tantric practices. It is well suited for the people of the modern era surviving with various stress-related diseases since it encompasses yogic postures, breathing exercise, and meditation, all 3 components which can be practiced easily within 20 min. Thus, understanding the potential of the IAM® technique in stress management,5 this study was planned on diabetic subjects. The objective of the study was to determine the psychological, physiological, and biochemical modulations brought about by stress reduction in type 2 diabetic subjects
1.2. Psycho-physiological benefits of yoga and meditation
Herbert Benson gave one of the first scientific conceptualizations of meditation, describing it as a method that produces a “relaxation reaction”.6 Andrew Newberg and J Iversen published a path-breaking paper on meditation in 2003 which proved that higher meditative states are associated with actual neurobiological events.7 A decrease in activation of sympathoadrenal system and the hypothalamic-pituitary adrenal (HPA) axis, as well as an enhanced parasympathetic activity are the possible postulated pathways that bring about positive changes in the individual8,9
1.3. Significance of the study
Maintaining the psychosocial wellbeing of diabetic patients is important clinically since diabetes is a chronic illness that requires continuous support in terms of both medical care and self-care management. Relaxation exercises such as meditation can be easily learned and practiced as it is safe, non-invasive and demanding very little in terms of equipment or professional training.4Although there have been several yoga and meditation studies looking at stress reduction in diabetics, most of the studies have been limited by unclear methodology and interventions, absence of control group, relatively small sample size, short term follow up, and poor compliance. In this study, we attempted to incorporate as many parameters as feasible that are likely to be influenced by chronic stress in type 2 diabetic patients. We also offered long-term follow-up for the subjects by organizing regular refresher classes in the presence of an IAM® practitioner. Yoga, meditation, and breathing exercises are all part of the IAM® approach. And, in particular, it has all of the ashtanga yoga steps in a capsule format that can be accomplished by anyone in 20 min. The worldwide reproducibility of our technique is very important. The technique is patented and is taught free of cost throughout the world by Mata Amritanandamayi Math (MAM). We hypothesize that regular practice of the Integrated Amrita Meditation (IAM®) technique would improve glycemic control, decrease insulin resistance and psychological stress, and increase the levels of Gamma Amino Butyric Acid (GABA) and Immunoglobulin A (IgA) in type 2 diabetic subjects when compared to a control group
2. Materials and methods
2.1. Estimation of minimum sample size
A pilot study10 was conducted to estimate the minimum sample size as well as to standardize all the items and tools required for main study. Based on the results, the minimum sample size was estimated as 30 in each group. Considering the chances of drop out we recruited more than the required sample size for the first visit
2.2. Selection of study subjects
The study protocol received Institutional Human Research Ethical Committee and Scientific Advisory Committee clearance before the commencement. Type 2 diabetic subjects from the department of Endocrinology, Amrita Institute of Medical Sciences and Research Centre were recruited for the study. Subjects aged between 30–65 years, HbA1C level between 7 %–10 %, and a history of duration of diabetes for 1–10 years were included in the study. Patients above 65 years, practicing other forms of physical exercise/yoga/meditation, patients who have ongoing psychiatric treatment, and those diagnosed with advanced diabetic complications such as ongoing treatment for retinopathy/renal impairment/symptomatic or unstable heart disease/uncontrolled BP were excluded from the study. Based on the inclusion and exclusion criteria and adhering to the ethical principles and those willing to participate in the study were randomly assigned to any of the 2 groups
2.3. Study groups
Group 1/IAM®: Diabetic patients receiving standard medical care and undergoing IAM®.
Group 2/Control: Diabetic patients receiving standard medical care alone and not undergoing meditation
Both groups were instructed lifestyle modification by a trained social worker which includes diet modifications, exercises, and psychological counseling according to the requirement of the patient. Test group subjects in addition were trained to practice IAM® daily. Every 3 months the participants in both groups had visits with the physician and social worker who reviewed their blood glucose levels to identify hypoglycemic risk and to confirm the adherence to lifestyle modification. There was no change in medication during the 6 month study period in either group
The test group patients were asked to report for the meditation class at 8 a.m. after an overnight fast of 8–12 hours. Age,sex, height, and weight were noted, and Body Mass Index (BMI) was calculated. The subjects were given the psychological questionnaire to complete before beginning the meditation. The fasting blood samples for analysis of various biochemical parameters were collected under prescribed aseptic conditions. 2 ml of blood was collected in K2EDTA (Di potassium ethylene diamine tetra acetic acid) vacuette for Fasting Blood Glucose (FBG) and 4 ml of blood was collected using sodium fluoride vacuette for HbA1c analysis. For all the other biochemical variables two BD®vacutainers of 4 ml containing clot activator PLUS were used for blood collection. From the collected blood samples in the vacutainers, the serum was separated using a centrifuge (Eppendorf™ 5810 R Germany) and the serum was collected in 2 ml storage vials and stored at −20 °C in a deep freezer for analysis. All the subjects were then called up to report for the second visit after 3 months and then after 6 months and all the baseline variables were repeated
2.4. Study variables and laboratory investigations
The physiological study variables included in our study were weight, BMI, heart rate (HR), respiratory rate (RR), systolic blood pressure (SBP), and diastolic blood pressure (DBP). The biochemical variables were FBG (estimation by hexokinase method), HbA1c (analyzed by High -Pressure Liquid Chromatography - HPLC), fasting serum insulin (HPLC),11 Insulin resistance (IR) (calculated through HOMA (Homeostatic Model Assessment) 2 calculator, version 2.2.3 Diabetes Trials Unit, University of Oxford), lipid profile (analyzed by colorimetric enzymatic test), cortisol (estimated by Chemiluminescent microparticle immunoassay method),11 adrenaline (analyzed by EPI(Epinephrine/Adrenaline) ELISA kit), IgA (analyzed by turbidimetry method), C–Reactive Protein (analyzed by immunoturbidimetry),11 Interleukin 6 (IL-6) (analyzed by Human IL6 ELISA kit), Gamma Amino Butyric Acid (GABA) (analyzed by γABA ELISA kit). The psychological variable included in the study was the Perceived Stress Scale (PSS)12 which is a widely used psychological instrument for measuring the perception of stress
2.5. IAM®technique
IAM® is a blend of yoga, meditation, and breathing exercises that has been developed and protected under a registered trade mark in order to preserve the original form of this meditation and avoid exploitation by unauthorized and unqualified teachers. The IAM® approach consists of up to 8 min of yogic postures, 2 min of relaxation, and 13 min of meditation. The subjects are requested to remain silent for 5 min at the end of the technique. IAM®technique which is taught by certified teachers, can be comfortably performed by anyone in just 20 min per day.5,13,14 Though the technique appears to be simple, it is a powerful technique that incorporates all of the steps of ashtanga yoga into a capsule format. that can be completed within a brief period of time. The methodology is a hybrid of conventional, tried-and-true procedures that are tailored to modern man's mental state, time limits, and necessities. The following are the main elements of the technique: Yogic postures/relaxation exercises: These exercises gradually relax the muscles and joints, as well as the mind. It also provides a reviving, all-encompassing impact. Breathing exercises: These breathing exercises draw attention to the way one breathes, prompts a more complete breathing. Awareness: Throughout the procedure, awareness is the most important factor. It is recommended that one be aware of all the nuances of each step. One section focuses on the flow of breath in particular. Visualization is an important part of this approach since the mind is focused on an internal point rather than an external physical object. This strategy is believed to alleviate stress and extend thinking in general, allowing the subject to be more creative13
2.6. Subject compliance
A self-maintained diary assessed their compliance on practice. Compliance was also assured telephonically. Practicing the technique minimum of 4 times a week was taken as the standard of compliance. When statistically analyzed the compliance was found to be 88.57 % in the IAM®group
2.7. Statistical analysis
Statistical analysis was done using IBM SPSS Statistics 20 Windows (SPSS Inc., Chicago, USA). For all the continuous variables, the results are given in mean ± sd, and for categorical variables as percentage. To obtain the association of categorical variables, chi-square with fisher's exact test was applied. To compare the mean difference in socio-demographic characteristics of study participants and mean percentage changes of physiological, psychological and, biochemical variables between the groups independent two-sample 't’ test was applied. To test the statistical significance of pre and post-mean changes within groups, paired t-test was used. Repeated measures of ANOVA were used to find the statistically significant comparison of means across one or more variables that are based on repeated observations. A p-value < 0.05 was considered statistically significant
3. Results and Discussion
From a total of 200 type 2 diabetic subjects screened, 70 subjects successfully completed the study (Supplementary Fig. 1). The mean age of study participants was 52.83 ± 7.45 and 49.91 ± 8.67 in IAM®and control group respectively. The sex distribution was comparable with the male: female ratio in the intervention group as 40:60 and in the control group 54.3:45.7. Both the groups were found to be comparable based on age, height, weight, BMI, duration of diabetes, and stress score (p > 0.05)(Supplementary Table 1)
3.1. Physiological and psychological variables
Significant decrease in HR (p < 0.05) and RR (p < 0.001) was observed within test group at the end of 3 and 6 months. RR within control group also showed significant increase at the end of 6 months (p < 0.01). Continuous IAM® practice for 6 months significantly brought down both SBP (p < 0.001) and DBP (p < 0.01) within the experimental group while no significant changes were observed within the control group (Table 1a). When the mean changes and mean percentage changes of all the physiological and psychological variables were compared from baseline to 3 months and baseline to 6 months of study between the groups, significant changes were observed for weight (p < 0.01), BMI (p < 0.01) and HR (p < 0.05) at the end of 6 months. Average percentage changes for RR and SBP between the groups were significant at the end of 3 months (p < 0.05) and 6 months (p < 0.001). The mean changes of DBP from baseline to 6 months between the groups also showed significant changes (p < 0.05)(Table 1a, Table 1b).
Table 1a.
Effect of 6 months of intervention on physiological and psychological variables in IAM®and control group.
|
Variables |
Within group |
Between group |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IAM® group (n = 35) |
Control group (n = 35) |
|||||||||||||
| 0 m (a) |
3 m (b) |
6 m (c) |
∗p (a-b-c) |
Change 0–3 m (a-b) = d ∗∗p |
Change 0–6 m (a-c) = e ∗∗∗p |
0 m (f) |
3 m (g) |
6 m (h) |
∗p (f-g-h) |
Change 0–3 m (f-g) = i ∗∗p |
Change 0–3 m (f-h) = j ∗∗∗p |
p1 (d-i) | p2 (e-j) | |
| Weight (kg) | 65.71 ± 9.21 | 65.55 ± 9.57 | 65.35 ± 9.67 | 0.426 | −0.16 ± 1.79 0.603 |
−0.37 ± 1.97 0.277 |
62.11 ± 12.15 | 62.18 ± 12.49 | 62.71 ± 2.24 | 0.004 | 0.07 ± 1.12 0.726 |
0.60 ± 1.13 0.004∗∗ |
0.529 | 0.014 |
| BMI (Kg/m2) | 25.11 ± 2.89 | 25.03 ± 3.01 | 24.95 ± 3.06 | 0.349 | −0.09 ± 0.69 0.466 |
−0.16 ± 0.76 0.227 |
24.38 ± 2.97 | 24.40 ± 3.15 | 24.63 ± 2.98 | 0.002 | 0.02 ± 0.46 0.797 |
0.25 ± 0.43 0.002∗∗ |
0.451 | 0.008 |
| HR (Beats/min) | 75.43 ± 5.88 | 73.94 ± 5.99 | 73.97 ± 5.77 | 0.025 | −1.49 ± 3.79 0.027 |
−1.46 ± 3.79 0.029 |
75.86 ± 6.39 | 75.74 ± 6.78 | 75.97 ± 6.27 | 0.904 | −0.11 ± 3.35 0.841 |
0.11 ± 2.75 0.807 |
0.113 | 0.051 |
| RR (Breaths/min) | 21.09 ± 2.56 | 20.26 ± 3.08 | 19.74 ± 3.00 | 0.002 | 0.83 ± 2.29 0.040 |
−1.34 ± 2.14 0.001 |
22.06 ± 2.17 | 22.46 ± 2.51 | 22.89 ± 1.88 | 0.005 | 0.40 ± 1.44 0.109 |
0.83 ± 1.42 0.002∗∗ |
0.009 | <0.001 |
| SBP (mmHg) | 143.03 ± 14.70 | 141.17 ± 16.74 | 138.49 ± 14.66 | 0.009 | −1.86 ± 9.49 0.063 |
−4.54 ± 7.27 0.001 |
135.77 ± 16.66 | 136.37 ± 16.66 | 136.63 ± 15.79 | 0.544 | 0.60 ± 5.30 0.507 |
0.86 ± 4.48 0.266 |
0.185 | <0.001 |
| DBP (mmHg) | 84.20 ± 9.51 | 84.11 ± 10.52 | 80.26 ± 8.14 | 0.003 | −0.09 ± 7.22 0.944 |
−3.94 ± 7.67 0.005 |
82.83 ± 10.32 | 83.26 ± 10.16 | 82.60 ± 10.02 | 0.780 | 0.43 ± 4.49 0.507 |
−0.23 ± 7.08 0.850 |
0.722 | 0.039 |
| PSS | 20.49 ± 4.29 | 17.89 ± 3.72 | 17.09 ± 4.44 | <0.001 | −2.60 ± 2.25 <0.001 |
−3.40 ± 3.13 <0.001 |
20.14 ± 4.50 | 20.83 ± 4.66 | 21.43 ± 4.69 | 0.004 | 0.69 ± 2.53 0.118 |
1.29 ± 2.31 0.002 |
<0.001 | <0.001 |
The ∗p-value is for the change by 6 months within each group from baseline - 3 months–6 months (repeated measures); ∗∗The p-value is for the difference in change within IAM® and control group from baseline to 3 months; ∗∗∗ The p-value is for the difference in change within IAM® and control group from baseline to 6 months; p1 and p2, the p-value is for the difference in mean change between IAM® and control groups at 3 months and 6 months respectively. m, months; BMI, body mass index; HR, heart rate; RR, respiratory rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; PSS, perceived stress scale; “-ve” sign indicates a ‘decrease’ in change
Table 1b.
Mean percentage changes of physiological and psychological variables between the groups.
|
Variables |
Visit | n | IAM®Group mean ± sd (a) |
Control Group mean±sd (b) |
Difference in change (a-b) p value |
|---|---|---|---|---|---|
| Weight (kg) | 0–3 m | 35 | −0.29 ± 2.69 | 0.02 ± 1.88 | −0.31 ± 2.320 0.574 |
| 0–6 m | 35 | −0.65 ± 3.00 | 1.00 ± 1.92 | −1.64 ± 2.51 0.008 |
|
| BMI (Kg/m2) | 0–3 m | 35 | −0.37 ± 2.68 | 0.02 ± 1.92 | −0.38 ± 2.33 0.492 |
| 0–6 m | 35 | −0.68 ± 3.00 | 1.05 ± 1.89 | −1.72 ± 2.51 0.005 |
|
| HR (Beats/min) | 0–3 m | 35 | −1.88 ± 4.92 | −0.09 ± 4.64 | −1.78 ± 4.77 0.123 |
| 0–6 m | 35 | −1.81 ± 4.98 | 0.23 ± 3.67 | −2.04 ± 4.37 0.055 |
|
| RR (Breaths/min) | 0–3 m | 35 | −3.73 ± 11.02 | 1.86 ± 6.86 | −5.59 ± 9.17 0.013 |
| 0–6 m | 35 | −6.22 ± 9.95 | 4.13 ± 7.16 | −10.35 ± 8.66 <0.001 |
|
| SBP (mmHg) | 0–3 m | 35 | −1.24 ± 6.70 | 0.52 ± 4.11 | −1.76 ± 5.55 0.012 |
| 0–6 m | 35 | −3.08 ± 5.00 | 0.74 ± 3.26 | −3.82 ± 4.22 <0.001 |
|
| DBP (mmHg) | 0–3 m | 35 | 0.11 ± 8.23 | 0.69 ± 5.59 | −0.57 ± 7.03 0.731 |
| 0–6 m | 35 | −4.18 ± 8.48 | 0.09 ± 8.62 | −4.26 ± 8.55 0.041 |
|
| PSS | 0–3 m | 35 | −12.12 ± 10.06 | 4.01 ± 14.09 | −16.11 ± 12.24 <0.001 |
| 0–6 m | 35 | −16.26 ± 14.73 | 6.98 ± 12.64 | −23.24 ± 13.72 <0.001 |
m, months; BMI, body mass index; HR, heart rate; RR, respiratoryrate; SBP, systolic blood pressure; DBP, diastolic blood pressure; PSS, perceived stress scale.−ve sign indicates a decrease in value
Positive impact of IAM®on HR and RR in normal healthy subjects was proved by Vandana B et al.13 These changes may be due to normalization of autonomic cardiovascular rhythms as a result of increased vagal modulation and/or decreased sympathetic activity and improved baroreflex sensitivity.15 Yogic pranayama breathing has been suggested to reduce the sense of stress, reduce sympathetic drive, and improve cardiovascular function16
Diabetes as a diagnosis itself is stressful for the patient and reduction of stress is an intended outcome of yoga/mediation practice. The experimental group in our study showed a highly significant decrease of perceived stress score at the end of 2nd (p < 0.001) and 3rd visit (p < 0.001). Also significant increase in psychological stress was noted within the control group (p < 0.01). When the mean percentage changes of PSS were compared between the groups from baseline to 3 months and baseline to 6 months, the stress score showed highly significant changes both at 2nd (p < 0.001) and 3rd (p < 0.001) visit. The effect of IAM® in inducing a positive stress response during stress events was studied by Vandana B.5 In concordance with our finding on perceived stress, another study on type 2 diabetic subjects showed a significant reduction of 26.1 % after continuous 4 weeks of guided meditation practice.17 Importantly, regardless of physiological outcomes, the use of yoga or meditation by people with diabetes leads to improved quality of life and reductions in perceived depression18
3.2. Biochemical variables
Significant drop in mean values of FBG, HbA1c (p < 0.01), insulin, HOMA IR (p < 0.05) and cortisol (p < 0.01) was observed in the experimental group at the end of 6 months. (Table 2a). When the mean percentage changes from baseline to 6 months were compared between the two groups, significant changes were observed again for FBG, HbA1c (p < 0.01), insulin, HOMA IR (p < 0.001), cortisol and adrenaline (p < 0.05)(Table 2b). Except for insulin and insulin resistance, similar significant results were observed when the mean changes were compared between the groups (Table 2a). In a study on diabetic subjects, continuous 6 months of yoga have shown highly significant decrease in fasting as well as postprandial blood glucose levels.19 Concordant findings with regard to FBG and HbA1c were observed in a community-based follow-up study20 as well as in a Qi- Gong study.21 Two major pathways have been postulated which can bring forth a positive change through yoga intervention. Firstly, it can promote a feeling of well -being by reducing the activation of the sympatho adrenal system and the hypothalamic-pituitary adrenal (HPA) axis thereby foster positive beneficial effects on neuroendocrine, metabolic and systemic inflammatory responses. Secondly, yoga may enhance parasympathetic activity by directly stimulating the vagus nerve and lead to positive changes in cardiovagal function, mood and energy state. In addition, yoga may act both ways, indirectly by encouraging healthy lifestyle changes and directly by contributing to weight loss and reduced visceral adiposity9,22,23
Table 2a.
Effect of 6 months of intervention on biochemical variables in IAM® and control group.
|
Variables |
Within Group |
Between group |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IAM® group (n = 35) |
Placebo group (n = 35) |
|||||||||||||
| 0 m (a) |
3 m (b) |
6 m (c) |
∗p (a-b-c) |
Change (a-b) = d ∗∗p |
Change (a-c) = e ∗∗∗p |
0 m (f) |
3 m (g) |
6 m (h) |
∗p (f-g-h) |
Change (f-g) = i ∗∗p |
Change (f-h) = j ∗∗∗p |
p1 (d-i) |
p2 (e-j) |
|
| FBG (mg/dl) | 151.48 ± 28.20 | 151.40 ± 37.32 | 140.24 ± 28.04 | 0.014 | −0.07 ± 30.73 0.989 |
−11.24 ± 21.33 0.004 |
141.22 ± 24.85 | 143.23 ± 29.31 | 144.26 ± 25.44 | 0.678 | 2.01 ± 21.76 0.589 |
3.04 ± 22.79 0.435 |
0.745 | 0.009 |
| HbA1c(%) | 8.21 ± 1.25 | 8.15 ± 1.29 | 7.70 ± 1.03 | 0.001 | −0.06 ± 0.87 0.710 |
−0.50 ± 0.89 0.002 |
7.99 ± 1.07 | 7.91 ± 1.47 | 8.14 ± 1.28 | 0.382 | −0.09 ± 0.98 0.607 |
0.15 ± 0.84 0.306 |
0.889 | 0.002 |
| Insulin (uIU/ml) | 23.00 ± 12.59 | 21.96 ± 11.30 | 22.65 ± 12.35 | 0.683 | −1.04 ± 4.73 0.118 |
−0.35 ± 8.93 0.033 |
18.07 ± 10.13 | 17.84 ± 10.95 | 20.17 ± 10.42 | 0.01 | −0.22 ± 4.89 0.544 |
2.10 ± 4.11 0.017 |
0.482 | 0.145 |
| HOMA IR | 3.28 ± 1.71 | 3.12 ± 1.62 | 3.14 ± 1.65 | 0.608 | −0.16 ± 0.69 0.063 |
−0.14 ± 1.28 0.014 |
2.52 ± 1.33 | 2.49 ± 1.45 | 2.81 ± 1.38 | 0.007 | −0.03 ± 0.67 0.533 |
0.29 ± 0.54 0.010 |
0.442 | 0.072 |
| HDL (mg/dl) | 34.48 ± 11.98 | 37.22 ± 11.63 | 42.10 ± 12.60 | <0.001 | 2.74 ± 5.45 0.005 |
7.61 ± 8.40 <0.001 |
37.21 ± 10.38 | 38.27 ± 8.07 | 39.17 ± 9.21 | 0.351 | 1.06 ± 6.15 0.315 |
1.95 ± 10.19 0.265 |
0.231 | 0.014 |
| LDL (mg/dl) | 103.08 ± 32.02 | 107.90 ± 32.64 | 111.02 ± 29.56 | 0.176 | 4.82 ± 30.14 0.351 |
7.94 ± 23.04 0.069 |
110.43 ± 37.74 | 116.10 ± 32.97 | 124.56 ± 38.07 | 0.031 | 5.67 ± 26.24 0.210 |
14.13 ± 35.63 0.025 |
0.900 | 0.391 |
| Cholesterol (mg/dl) | 168.47 ± 34.42 | 169.49 ± 36.28 | 169.64 ± 36.80 | 0.964 | 1.03 ± 29.95 0.841 |
1.17 ± 24.47 0.780 |
173.01 ± 41.31 | 175.06 ± 34.15 | 189.77 ± 44.72 | 0.020 | 2.06 ± 31.10 0.698 |
16.76 ± 45.45 0.036 |
0.888 | 0.078 |
| Triglyceride (mg/dl) | 130.41 ± 43.78 | 143.41 ± 49.77 | 147.78 ± 52.10 | 0.066 | 13.01 ± 36.05 0.060 |
17.38 ± 46.79 0.065 |
141.54 ± 53.80 | 140.06 ± 45.00 | 162.26 ± 67.95 | 0.068 | −1.48 ± 49.74 0.861 |
20.71 ± 66.25 0.073 |
0.167 | 0.809 |
| Cortisol (μg/dl) | 16.14 ± 2.90 | 15.36 ± 3.29 | 14.57 ± 3.31 | 0.053 | −0.78 ± 3.66 0.225 |
−1.57 ± 3.32 0.007 |
16.53 ± 2.72 | 15.36 ± 3.34 | 16.33 ± 3.38 | 0.100 | −1.17 ± 3.42 0.245 |
−0.20 ± 3.32 0.935 |
0.643 | 0.059 |
| Adrenaline (pg/ml) | 85.93 ± 82.42 | 86.13 ± 81.91 | 79.41 ± 79.99 | 0.284 | 0.21 ± 31.88 0.980 |
−6.51 ± 27.03 0.095 |
82.08 ± 83.71 | 85.77 ± 86.15 | 94.35 ± 88.64 | 0.188 | 3.69 ± 36.16 0.743 |
12.28 ± 41.34 0.594 |
0.864 | 0.045 |
| IgA (mg/dl) | 274.24 ± 84.95 | 275.63 ± 82.61 | 294.05 ± 85.51 | 0.007 | 1.39 ± 36.82 0.762 |
19.81 ± 47.43 0.002 |
295.36 ± 78.76 | 297.01 ± 77.50 | 299.50 ± 80.97 | 0.840 | 1.65 ± 42.64 0.451 |
4.13 ± 48.64 0..682 |
0.685 | 0.852 |
| CRP (mg/L) | 3.23 ± 3.61 | 3.00 ± 3.42 | 2.88 ± 3.29 | 0.507 | −0.24 ± 1.78 0.439 |
−0.36 ± 1.87 0.266 |
3.34 ± 3.66 | 3.21 ± 3.71 | 3.06 ± 3.32 | 0.890 | −0.13 ± 4.07 0.853 |
−0.28 ± 2.13 0.448 |
0.887 | 0.868 |
| IL-6 (pg/mL) | 10.48 ± 8.91 | 11.00 ± 9.46 | 9.94 ± 7.79 | 0.771 | 0.51 ± 8.36 0.791 |
−0.54 ± 8.27 0.945 |
6.89 ± 7.29 | 6.97 ± 8.28 | 8.86 ± 8.54 | 0.156 | 0.07 ± 6.24 0.870 |
1.97 ± 6.59 0.031 |
0.802 | 0.165 |
| GABA (pg/mL) | 146.38 ± 165.07 | 162.19 ± 171.94 | 195.03 ± 189.39 | 0.034 | 15.81 ± 123.16 0.453 |
48.65 ± 100.14 0.007 |
121.17 ± 111.67 | 101.37 ± 89.63 | 99.28 ± 60.43 | 0.273 | −19.81 ± 92.96 0.216 |
−21.89 ± 99.39 0.201 |
0.177 | 0.004 |
The ∗p value is for the change by 6 months within each group from baseline - 3 months–6 months (repeated measures); ∗∗The p value is for the difference in change within IAM® and control group from baseline to 3 months; ∗∗∗ The p value is for the difference in change within IAM® and control group from baseline to 6 months; p1 and p2, the p value is for the difference in mean change between IAM® and control groups at 3 months and 6 months respectively.m, months; FBG, fasting blood glucose; HOMA IR, homeostatic model assessment insulin resistance; HDL, high density lipoprotein; LDL, low density lipoprotein; IgA, immunoglobulin A; CRP, C reactive protein; IL6, interleukin 6; GABA, gamma amino butyric acid. “-ve” sign indicates a ‘decrease’ in change
Table 2b.
Mean percentage changes of biochemical variables between the groups.
|
Variables |
Visit | n | IAM®Group Mean ± sd (a) |
Control Group Mean±sd (b) |
Change in difference (a-b) p value |
|---|---|---|---|---|---|
| FBG (mg/dl) | 0–3 m | 35 | 0.39 ± 18.56 | 1.90 ± 16.08 | −1.51 ± 17.36 0.716 |
| 0–6 m | 35 | −6.84 ± 12.50 | 3.01 ± 15.25 | −9.84 ± 13.94 0.004 |
|
| HbA1c (%) | 0–3 m | 35 | −0.30 ± 10.16 | −1.14 ± 12.65 | 0.84 ± 11.47 0.761 |
| 0–6 m | 35 | −5.44 ± 9.60 | 2.01 ± 10.81 | −7.44 ± 10.22 0.003 |
|
| Insulin (uIU/ml) | 0–3 m | 35 | −0.89 ± 27.46 | 2.55 ± 31.22 | −3.43 ± 29.40 0.414 |
| 0–6 m | 35 | 4.05 ± 45.36 | 16.06 ± 28.89 | −12.01 ± 38.02 <0.001 |
|
| HOMA IR | 0–3 m | 35 | −1.76 ± 27.88 | 2.59 ± 30.54 | −4.34 ± 29.23 0.394 |
| 0–6 m | 35 | 1.61 ± 45.82 | 15.83 ± 27.92 | −14.22 ± 37.93 0.001 |
|
| HDL (mg/dl) | 0–3 m | 35 | 11.13 ± 18.75 | 6.29 ± 18.93 | 4.83 ± 18.83 0.287 |
| 0–6 m | 35 | 30.24 ± 46.68 | 9.96 ± 26.61 | 20.28 ± 37.99 0.029 |
|
| LDL (mg/dl) | 0–3 m | 35 | 11.08 ± 48.85 | 9.59 ± 23.45 | 1.49 ± 38.31 0.870 |
| 0–6 m | 35 | 13.63 ± 37.51 | 18.84 ± 31.89 | −5.20 ± 34.81 0.534 |
|
| Cholesterol (mg/dl) | 0–3 m | 35 | 1.99 ± 17.99 | 3.42 ± 15.54 | −1.42 ± 16.80 0.724 |
| 0–6 m | 35 | 1.71 ± 15.94 | 12.68 ± 25.53 | −10.96 ± 21.28 0.035 |
|
| Triglyceride (mg/dl) | 0–3 m | 35 | 14.01 ± 34.09 | 6.54 ± 41.77 | 7.46 ± 38.12 0.416 |
| 0–6 m | 35 | 18.46 ± 41.44 | 24.99 ± 58.04 | −6.53 ± 50.42 0.590 |
|
| Cortisol (μg/dl) | 0–3 m | 35 | −2.51 ± 24.69 | −5.62 ± 19.92 | 3.11 ± 22.43 0.846 |
| 0–6 m | 35 | −8.10 ± 21.01 | 0.30 ± 20.59 | −8.40 ± 20.79 0.034 |
|
| Adrenaline (pg/ml) | 0–3 m | 35 | 7.09 ± 42.63 | 10.90 ± 44.97 | −3.80 ± 43.81 0.561 |
| 0–6 m | 35 | −3.73 ± 27.37 | 27.10 ± 78.54 | −30.84 ± 58.81 0.050 |
|
| IgA (mg/dl) | 0–3 m | 35 | 1.48 ± 13.81 | 1.65 ± 13.62 | −0.16 ± 13.71 0.588 |
| 0–6 m | 35 | 8.92 ± 17.06 | 2.95 ± 17.22 | 5.95 ± 17.14 0.885 |
|
| CRP (mg/L) | 0–3 m | 35 | 0.68 ± 64.66 | 94.14 ± 333.21 | −93.46 ± 240.01 0.108 |
| 0–6 m | 35 | 0.24 ± 56.36 | 29.83 ± 160.25 | −29.58 ± 120.11 0.307 |
|
| IL-6 (pg/mL) | 0–3 m | 35 | 25.21 ± 140.23 | 40.02 ± 136.87 | −14.81 ± 138.55 0.585 |
| 0–6 m | 35 | 59.44 ± 236.37 | 130.75 ± 276.15 | −71.31 ± 257.03 0.040 |
|
| GABA (pg/mL) | 0–3 m | 35 | 21.51 ± 63.70 | −4.77 ± 43.06 | 26.27 ± 54.36 0.057 |
| 0–6 m | 35 | 52.10 ± 87.09 | 5.28 ± 69.26 | 46.82 ± 78.68 0.015 |
m, months; FBG, fasting blood glucose; HOMA IR, homeostatic model assessment insulin resistance; HDL, high density lipoprotein; LDL, low density lipoprotein; IgA, immunoglobulin A; CRP, C reactive protein; IL6, interleukin 6; GABA, gamma amino butyric acid
Although in our study the stress hormone cortisol showed significant drop by 6 months, adrenaline did not show significant change within test group. To show a statistically significant decline in adrenaline, a longer period of follow-up may be required. However, between the groups, the mean percentage changes were significant for both cortisol and adrenaline. In a previous study of IAM®on stress hormones in healthy individuals, adrenaline reduced in IAM®group within 48 hours, and cortisol decreased significantly after 8 months of IAM®practice.24 Exposure to stress causes an immediate increase in adrenaline through the HPA pathway.25,26 Walton et al. and Mc Lean et al. have done several studies on the effect of transcendental meditation on cortisol levels27,28
In our study, the effect of meditation on lipid profile within the experimental group was mainly highlighted for HDL. The mean HDL level was highly significant at 3 months (p < 0.01) and 6 months (p < 0.001) within IAM®group. Though LDL and total cholesterol showed an increase in both the groups, significant increase was observed within the control group (p < 0.05)(Table 2a). On between group comparison of the mean percentage changes, HDL (p < 0.05) and total cholesterol (p < 0.05) showed significant changes at baseline to 6 months of study period (Table 2b). Previous yoga studies have reported that yoga helps in redistribution of body fat and reduction in central obesity which leads to insulin resistance.29,30 The improvement in lipid profile with practice of yoga could be due to increased hepatic lipase and lipoprotein lipase activity. This would increase the uptake of triglycerides by adipose tissue and affect the lipoprotein metabolism29
In our study, IgA levels were found to increase in both test and control groups. However statistically significant increase in IgA was more evident in the experimental group (p < 0.01)(Table 2a). No significant changes were observed on between group comparisons (Table 2b). Previous IAM®study on healthy adults had shown significant changes in IgA levels in the experimental group when compared with control groups.13 Inflammation is hypothesized to play a role in the development of type 2 diabetes. However clinical data addressing this issue are limited. CRP did not show any significant changes in both the groups (Table 2a). Also, in our study, no significant change was observed for IL6 within the test group while there was a significant increase of IL6 observed within control group (p < 0.05) at the end of 6 months (Table 2a). When the mean percentage changes from baseline to 6 months were compared between the two groups, significant changes in IL6 was observed (p < 0.05)(Table 2b). In a study that looked upon the effect of short-term yoga-based lifestyle intervention in overweight individuals, significant change in IL6 was observed at the end of study.31 In our study, serum GABA levels were found to increase in both test and control groups (Table 2a). However, both mean and mean percentage changes showed significant changes between the groups over 6 months (Table 2a, Table 2b). Even though previous literature is available that looked upon brain GABA levels in meditation, studies on serum GABA levels are limited
4. Limitation and scope for future
This study attempted to comprehend the numerous psychophysiological and biochemical changes caused by the IAM® technique in type 2 diabetic patients to attain better mental and physical wellbeing. Though we have collected the baseline socio-demographic characteristics of study participants to know about the sampling fluctuations, data on socio-economic status and Intelligent Quotient (IQ) of subjects at the baseline visits were not recorded. In future research, we would like to examine the plasma levels of malondialdehyde (MDA), superoxide dismutase (SOD), and melatonin in diabetic subjects, to gain a better understanding of the molecular and mechanistic pathways involved in stress-induced diabetes, as well as the potential role of meditation in reducing oxidative stress. Furthermore, in the future, a combination of scientific and philosophical-literary research will be essential to confirm, authenticate, and increase the knowledge and usage of mind-body relaxation techniques for the benefit of humanity
5. Conclusion
Our study has attempted to bring light to the fact that mental health should always be a part of proper diabetic treatment regimen. New research strongly indicates that therapies that help people deal with stress can have a substantial positive impact on the quality of life and glycemic regulation
Conflict of interest disclosure statement
The authors have declared that they have no conflicts of interest with respect to current research.
Funding
This work was funded by seed grant support from Amrita Institute of Medical Sciences, Amrita Vishwa Vidhyapeetham, Kochi, India.
Authors contribution
Contribution of Sarika K S includes literature search, data acquisition, manuscript preparation, and manuscript editing. Contributions of VandanaBalakrishnan and Harish Kumar include the development of concepts, design, and manuscript review. Contribution of Sundaram K R include statistical analysis of data.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtcme.2021.08.005.
Contributor Information
K.S. Sarika, Email: sarikaks@aims.amrita.edu.
Vandana Balakrishnan, Email: vandanabalakrishnan@aims.amrita.edu.
Harish Kumar, Email: harishkumar@aims.amrita.edu.
K.R. Sundaram, Email: krs1943@yahoo.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Whiting DR, Guariguata L, Weil C, Shaw J. IDF Diabetes Atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 2.Pouwer, F., Kupper, N., Adriaanse M. Does emotional stress cause type 2 diabetes mellitus?. [PubMed]
- 3.Pacák K., Palkovits M. Stressor specificity of central neuroendocrine responses: implications for stress-related disorders. Endocr Rev. 2001;22(4):502–548. doi: 10.1210/er.22.4.502. [DOI] [PubMed] [Google Scholar]
- 4.Care M. Standards of medical care in diabetes - 2013. Diabetes Care. 2013;36(suppl 1) doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vandana B., Suseeladevi G.K., Kumar H., Saraswathy L., Sunadaram K. Meditation induces a positive response during stress events in young Indian adults. Int J Yoga. 2011;4(2):64. doi: 10.4103/0973-6131.85487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Proctor W.H.B., Revolution Relaxation. 2011. The Science and Genetics OfMind Body Healing. [Google Scholar]
- 7.Newberg A.B., Iversen J. The neural basis of the complex mental task of meditation: neurotransmitter and neurochemical considerations. Med Hypotheses. 2003;61(2):282–291. doi: 10.1016/S0306-9877(03)00175-0. [DOI] [PubMed] [Google Scholar]
- 8.Kawakami N., Araki S., Takatsuka N., Shimizu H., Ishibashi H. Overtime, psychosocial working conditions, and occurrence of non-insulin dependent diabetes mellitus in Japanese men. J Epidemiol Community Health. 1999;53(6):359–363. doi: 10.1136/jech.53.6.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knol M.J., Twisk J.W.R., Beekman A.T.F., Heine R.J., Snoek F.J., Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49(5):837–845. doi: 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- 10.Sarika K.S., Balakrishnan V., Sundaram K., Kumar H. The effect of integrated amrita meditation (IAM) technique on glycemic control in type 2 diabetes. Int J Phys. 2019;7(3):218. doi: 10.5958/2320-608x.2019.00118.5. [DOI] [Google Scholar]
- 11.Burtis C.A., Ashwood E.R.B.D. fifth ed. Elsevier; Edinburgh, London: 2012. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. [Google Scholar]
- 12.Cohen S. 1983. Cohen Perceived Stress.http://podcast.uctv.tv/webdocuments/COHEN-PERCEIVED-STRESS-Scale.pdf 2. [Google Scholar]
- 13.Vandana B., Saraswathy L., Suseeladevi G.K., Sundaram K.R., Kumar H. Positive impact of integrated amrita meditation technique on heart rate, respiratory rate and IgA on young healthy adults. Tang [Humanitas Med. 2013;3(2):13.1–13.6. doi: 10.5667/tang.2012.0038. [DOI] [Google Scholar]
- 14.Vandana B., Vaidyanathan K., Saraswathy L.A., Sundaram K.R., Kumar H. 2011. Impact of Integrated Amrita Meditation Technique on Adrenaline and Cortisol Levels in Healthy Volunteers. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhavanani A.B., Sanjay Z., Madanmohan Immediate effect of sukha pranayama on cardiovascular variables in patients of hypertension. Int J Yoga Therap. 2011;21:73–76. doi: 10.17761/ijyt.21.1.y007g51341634172. [DOI] [PubMed] [Google Scholar]
- 16.Wilson T., Kelly K.L., Baker S.E. Review: can yoga breathing exercises improve glycemic response and insulin sensitivity? J Yoga Phys Ther. 2017 doi: 10.4172/2157-7595.1000270. 07(02. [DOI] [Google Scholar]
- 17.Varghese M.P., Balakrishnan R., Pailoor S. Association between a guided meditation practice, sleep and psychological well-being in type 2 diabetes mellitus patients. J Compl Integr Med. 2018;15(4):18–20. doi: 10.1515/jcim-2015-0026. [DOI] [PubMed] [Google Scholar]
- 18.Cai H., Li G., Zhang P., Xu D., Chen L. Effect of exercise on the quality of life in type 2 diabetes mellitus: a systematic review. Qual Life Res. 2017;26(3):515–530. doi: 10.1007/s11136-016-1481-5. [DOI] [PubMed] [Google Scholar]
- 19.Chimkode S.M., Kumaran S.D., Kanhere V.V., Shivanna R. Effect of yoga on blood glucose levels in patients with Type 2 diabetes mellitus. J Clin Diagn Res. 2015;9(4):CC01–CC03. doi: 10.7860/JCDR/2015/12666.5744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Angadi P., Jagannathan A., Thulasi A., Kumar V., Umamaheshwar K.R.N. Adherence to yoga and its resultant effects on blood glucose in type 2 diabetes: a community-based follow-up study. Int J Yoga. 2017;10(1):29. doi: 10.4103/0973-6131.186159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun G.C., Lovejoy J.C., Gillham S., Putiri A., Sasagawa M.B.R. Effects of Qigong on glucose control in type 2 diabetes: a randomized controlled pilot study. Diabetes Care. 2010;33(1):e8. doi: 10.2337/dc09-1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Innes K.E., Vincent H.K. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: a systematic review. Evid base Compl Alternative Med. 2007;4(4):469–486. doi: 10.1093/ecam/nel103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Innes K.E., Bourguignon C., Taylor A.G. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J Am Board Fam Pract. 2005;18(6):491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 24.Vandana B., Vaidyanathan K., Saraswathy L.A., Sundaram K.R., Kumar H. Impact of integrated amrita meditation technique on adrenaline and cortisol levels in healthy volunteers. Evid base Compl Alternative Med. 2011;2011 doi: 10.1155/2011/379645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.eliasson1983 (1).pdf.
- 26.Ganong W.F. twenty-second ed. 2007. Review of Medical Physiology. 22nd ed. (Lange, ed.).; 2007. [Google Scholar]
- 27.Walton K.G., Fields J.Z., Levitsky D.K., Harris D.A., Pugh N.D.S.R. Lowering cortisol and CVD risk in postmenopausal women: a pilot study using the transcendental meditation program. Ann NY Acad Sci. 2004;1032:211–215. doi: 10.1196/annals.1314.023. [DOI] [PubMed] [Google Scholar]
- 28.MacLean C.R.K., Walton K.G., Wenneberg S.R., et al. Effects of the transcendental meditation program on adaptive mechanisms: changes in hormone levels and responses to stress after 4 months of practice. Psychoneuroendocrinology. 1997;22(4):277–295. doi: 10.1016/S0306-4530(97)00003-6. [DOI] [PubMed] [Google Scholar]
- 29.Yoga Lipid profile - PubMed - NCBI. http://www.ncbi.nlm.nih.gov/pubmed
- 30.Skarfors E.T., Wegener T.A., Lithell H., Selinus I. Physical training as treatment for Type 2 (non-insulin-dependent) diabetes in elderly men. A feasibility study over 2 years. Diabetologia. 1987;30(12):930–933. doi: 10.1007/BF00295876. [DOI] [PubMed] [Google Scholar]
- 31.Netam R., Yadav R.K., Khadgawat R., Sarvottam K., Yadav R. Interleukin-6, vitamin D & diabetes risk-factors modified by a short-term yoga-based lifestyle intervention in overweight/obese individuals. Indian J Med Res. 2015;141(June):775–782. doi: 10.4103/0971-5916.160698. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.