Abstract
We report an extremely rare case of mesocardia with double inferior vena cava (IVC) in this case report. The patient’s associated atrial septal defect (ASD) with left to right shunt leading to pulmonary congestion and recurrent episodes of pneumonia was the leading diagnosis for which care was sought at our hospital. The diagnoses of these rare congenital cardiac anomalies were uncovered only after a thorough workup. Mesocardia is extremely rare and accounts for only 0.2% of congenital anomalies. Its association with other cardiac and vascular anomalies, however, warrants a meticulous workup for the identification of such associated conditions—ASD and double IVC being two such anomalies in our patient. The dictum of working up a case of congenital cardiac anomaly for other congenital cardiaovascular anomalies, therefore, found merit in our case.
Keywords: Cardiothoracic surgery, Paediatric Surgery, Vascular surgery
Background
Mesocardia is an abnormal location of the heart in which the heart is in a midline position and longitudinal axis of the heart lies in mid saggital plane. While it is extremely rare, and mostly under-reported, it is associated with other congenital cardiac and vascular anomalies and, therefore, needs further investigation to uncover them. Mesocardia per se may be clinically inconsequential and might be an incidental finding while working up the patient for other diseases. We report a case of mesocardia (situs solitus) with associated ostium secundum atrial septal defect and double inferior vena cava.
Case presentation
A toddler born out of non-consanguineous marriage presented to the paediatric emergency department with fever and increased work of breathing since the past 3 days. The child had presented four times with similar reports in the past, the first time being at 8 months of age. The child has a history significant for ostium secundum atrial septal defect, detected at 1 year of age. The mother denies any episodes of bluish discolouration of the lips and mucous membranes or dusky discolouration of the skin. There is no history for recurrent diarrhoea. Primary and secondary immunodeficiency disorders as well as structural disorders of the lung and tracheobronchial tree were ruled out. The mother states that her index antenatal and natal period was uneventful. There was no history of diabetes, substance abuse or other teratogenic drug intakes by his mother during pregnancy. The child received BCG, polio, hepatitis B, HiB, DPT and MMR vaccines as per the National Immunization Schedule of India
On physical examination, the child appeared restless and anxious. His temperature was 99.6 ° F, pulse rate was 128/min with regular rhythm and normal volume and no radioradial or radiofemoral delay. Blood pressure was 110/60 mm Hg in all four limbs. SpO2 was 97% in room air and the respiratory rate was 35/min. On cardiovascular examination, apical impulse was palpated in right fifth intercostal space 2 cm from mid sternal line. There was hyper dynamic apex with no palpable thrill. Auscultation showed normal S1 and fixed wide S2 split at site of apex beat.
Investigations
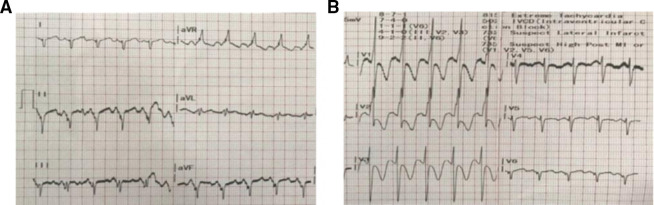
ECG was ordered and showed inverted P and QRS in lead II, positive P and QRS waves in aVR (figure 1A) and reverse progression of QRS from lead V1 to V6 (figure 1B).
Figure 1.
(A) Showing inverted P wave in lead II and positive P and QRS complexes in lead aVR. (B) Depicting tall R waves in V1 and reverse progression of QRS complexes from V1 to V6.
Chest X-ray was ordered (figure 2A). Echocardiography demonstrated mesocardium with situs solitus and moderate ostium secundum atrial septal defect with left to right shunt and dilated right atrium and right ventricle. CT thoracic angiography was done to evaluate other vascular structure anomalies—a double inferior vena cava was seen joining above renal veins (figure 2B, C). Findings of mesocardium with situs solitus (figure 2D) and ostium secundum atrial septal defect (figure 2E white arrow pointing atrial septal defect) were confirmed with this modality. A final diagnosis of mesocardia with ostium second atrial septal defect and double IVC anomaly was made.
Figure 2.
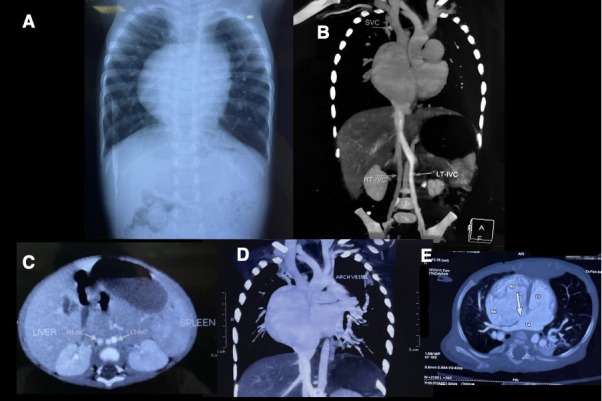
(A) Chest X-ray anteroposterior view. (B) Double inferior vena cavaanomaly. (C) CT abdomen transverse view depicting double IVC anomaly with situs solitus (liver on right and spleen on left). (D) Depicting mesocardia (situs solitus). (E) White arrow pointing to the atrial septal defect.
Outcome and follow-up
The toddler was on furosemide 1 mg/kg/day and tablet spironolactone 1.5 mg/kg/day since 1 year for congestive heart failure. He was haemodynamically stabilised and managed symptomatically at our unit. Ceftriaxone 70 mg/kg/day was given for 3 days for pneumonia. He was discharged with instructions to continue same dose of furosemide and spironolactone and parents were advised to review after 1 week. He underwent corrective surgical repair of the atrial septal defect 2 days after discharge at a different hospital.
Discussion
Mesocardia is rare congenital anomaly with very few cases reported in the literature. It accounts for 0.2% of congenital heart diseases and has strong male preponderance—men to women ratio being 11:5.1 This altered anatomy is rarer compared with dextrocardia. In one study, an analysis of 3000 autopsy specimens revealed that 65 had cardiac malposition with 43 being dextrocardia and only 7 being mesocardiac.2 Under normal embryologic conditions, after the heart has completely formed and reached a size of 20–25 mm, there is no true apex and it has shape similar to that of a heart in mesocardia. This event in morphogenesis is then followed by one of the last phases of cardiac development, which involves looping of heart—responsible for apex pointing right or left.3 Failure of this process results in midline heart. Stanger et al in their clinical study involving 13 cases of mesocardia reported abdominal situs with situs solitus (eight cases) and situs inversus (five cases).4 Splenic abnormalities were also reported involving presence of accessory spleen (four cases) and polysplenia (one case). The abdominal situs was solitus in this case with liver in the right and the spleen in the left hypochondrium. Mesocardia can also be associated with other structural cardiovascular anomalies. Atrial septal defects or ventricular septal defects and persistent left superior vena cava were observed in case reports of mesocardia.2 We report a case of mesocardia with associated double inferior vena cava, which has not been reported in the literature to this date. CT angiogram showed double inferior vena cava with better contrast enhancement in left inferior vena cava compared with right. Inferior vena cava usually develops during 7–10 weeks of gestation. Inferior vena cava duplication is due to persistent left supracardinal vein. Isolated cases of double inferior vena cava and right vena cava have been reported in recent times, but this is the first case (after extensive review of published literature) where the three congenital cardiac abnormalities—mesocardia, ASD and double IVC, were found in the same patient. No definite association between congenital heart disease and inferior vena cava anomalies has been established due to lack of sufficient research and reporting.3 A double IVC is usually an incidental detection, which is often identified during the evaluation of genitourinary anomalies with an estimated incidence reported to be 0.2%–3%.5 The patient’s associated atrial septal defect of ostium secundum variant with left to right shunt leading to pulmonary congestion and recurrent episodes of pneumonia, which was the leading diagnosis for which he sought care at our hospital. The diagnoses of these rare congenital cardiac anomalies were uncovered during the workup of this patient at our facility.
The diagnosis and identification of double IVC holds importance when taking up the patient for any planned procedure of the IVC or abdominal vasculature in the future. Thrombosis and inadvertent iatrogenic injury of the IVC are potential complications. Rarely, double IVC can be misdiagnosed as a para-aortic lymphadenopathy and should also be suspected in cases of recurrent pulmonary embolism following the placement of an IVC filter. The dictum of working up a case of congenital cardiac anomaly (as in the case of heterotaxy)—for other congenital cardiaovascular anomalies found merit in our case. It was only after working up the patient of mesocardia with ASD for further anomalies of the vasculature, did we uncover the diagnosis of double inferior vena cava.
Patient‘s perspective.
I was very appalled to find out about the rare condition that our little boy harboured within his body. It was a tough time for our family. The hospital has become the second home for our kid ever since he started developing recurrent respiratory tract infections. We took a lot of time to build courage and face the reality, but the doctors and nurses helped us a lot coping with the situation. We are now mentally at peace knowing the options that we have with us and also understanding what to expect in future regarding this rare heart condition of our child.
Learning points.
Mesocardia is one of the rarer outcomes of abnormal morphogenesis of the heart.
It is often associated with other congenital cardiac and extracardiac defects of vasculature as well as organ isomerism.
While extremely rare and with questionable prognostic significance, its association with other cardiac and vascular anomalies warrants a workup for the identification of such associated conditions—atrial septal defect and double inferior vena cava being two such anomalies in our patient.
Acknowledgments
Dr Srikanth, Assistant Professor of Pediatrics at Gandhi Hospital and a senior paediatric consultant, countersigned the consent form after patient counselling, as per the requirements of BMJ.
Footnotes
Twitter: @shreyas_rn, @wumb0logist, @Ornate_Brute
Contributors: SKu and SRN were involved in working up the patient and obtaining imaging studies for him. They cared for the patient for a period of 10 days and regularly charted vitals and prepared the preliminary report of case findings and presentations. SI and SKa were provided insights on how to prepare a case report, proofread preliminary versions of the case report and gave opinion regarding what to further elaborate in history of presenting illness. This helped guide the workup of the patient and helped form a broader differential. All authors were involved in extensive review of published literature to help build the narrative of this unique case that hasn’t been extensively published yet.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained from parent(s)/guardian(s)
References
- 1.Männer J. The anatomy of cardiac looping: a step towards the understanding of the morphogenesis of several forms of congenital cardiac malformations. Clin Anat 2009;22:21–35. 10.1002/ca.20652 [DOI] [PubMed] [Google Scholar]
- 2.Ertuğrul İlker, Doğan V, Örün UA, et al. A rare association: inferior vena cava anomalies and congenital heart diseases. Turk Kardiyol Dern Ars 2015;43:717-9. 10.5543/tkda.2015.64509 [DOI] [PubMed] [Google Scholar]
- 3.Lev M, Liberthson RR, Golden JG, et al. The pathologic anatomy of mesocardia. Am J Cardiol 1971;28:428–35. 10.1016/0002-9149(71)90006-3 [DOI] [PubMed] [Google Scholar]
- 4.Stanger P, Rudolph AM, Edwards JE. Cardiac malpositions. An overview based on study of sixty-five necropsy specimens. Circulation 1977;56:159–72. 10.1161/01.CIR.56.2.159 [DOI] [PubMed] [Google Scholar]
- 5.Coco D, Cecchini S, Leanza S, et al. Inferior vena cava duplication: incidental case in a young woman. Case Rep Radiol 2016;2016:1–4. 10.1155/2016/3071873 [DOI] [PMC free article] [PubMed] [Google Scholar]