Abstract
Background
Takotsubo cardiomyopathy (TC) or stress-induced cardiomyopathy is a transient heart condition that clinically resembles an acute coronary syndrome. This study aims to assess the incidence of life-threatening arrhythmias in patients with Takotsubo cardiomyopathy and evaluate the outcomes of patients with life-threatening arrhythmias (LTAs) in Takotsubo cardiomyopathy compared with those without LTA.
Methods
We comprehensively searched the PubMed, Google Scholar, and Embase databases from inception to February 2021. The primary aim of the study was to determine the incidence of LTAs in TC patients. Other outcomes of interest were the odds of in-hospital, long-term mortality, and cardiogenic shock (CS) in TC patients with LTAs versus those without LTAs. For all statistical analyses, ReviewManager and MedCalc were used.
Results
Eighteen studies were included in this study involving 55,557 participants (2,185 with LTAs and 53,372 without LTAs). The pooled incidence of LTAs in the patients of TC was found to be 6.29% (CI: 4.70–8.08%; I2 = 94.67%). There was a statistically significant increased risk of in-hospital mortality (OR = 4.74; CI: 2.24–10.04; I2 = 77%, p < 0.0001) and cardiogenic shock (OR = 5.60; CI: 3.51–8.95; I2 = 0%, p < 0.00001) in the LTA group versus the non-LTA group. LTA was not associated with long-term mortality (OR = 2.23; CI: 0.94–5.28; I2 = 53%, p = 0.07).
Conclusion
The pooled incidence of life-threatening arrhythmias in the patients of TC was found to be 6.29%. In the group of TC patients with LTAs, the odds of in-hospital mortality and CS, was higher than in the TC patients without LTAs.
Keywords: Takotsubo cardiomyopathy, Life-threatening arrhythmias, Mortality
1. Introduction
Takotsubo cardiomyopathy (TC) is non-ischemic cardiomyopathy first described in 1990. Also named apical ballooning or stress cardiomyopathy, it is characterized by reversible left ventricular systolic dysfunction with no evidence of obstructive epicardial coronary disease. Clinical symptoms and electrocardiographic findings resemble those of an acute myocardial infarction with approximately 2.0% of acute ST-segment elevations presentations representing TC.1 Post-menopausal women are more frequently affected, usually following emotional distress.2 Nevertheless, other triggers include subarachnoid hemorrhage, ischemic stroke, severe head injury, acute medical illness, or acute pheochromocytoma crisis.3
The pathophysiology is not entirely understood but may involve catecholamine toxicity and vasospasm3 orchestrated by central neurogenic mechanisms, thereby explaining psychological stress as a precipitant. On biopsy, inflammatory infiltrates and contraction bands distinguish TC from coagulative necrosis seen on myocardial infarction caused by coronary artery occlusion,2 explaining minimal myocardial enzyme release in the setting of Takotsubo cardiomyopathy.1
Whereas the prognosis is generally favorable, and improvement of left ventricular function ensues within 3–4 weeks,4 significant morbidity and mortality can be associated with TC.5 Heart-failure, left ventricular free wall rupture and fatal arrhythmias are among the possible complications.6 Although mild ST-segment elevation extending beyond the distribution of a single coronary artery and T-wave inversions are the most common findings on admission,7 marked QT prolongation with increased risk of life-threatening arrhythmias (LTAs) can also occur.8
In particular, the incidence of LTAs has been reported as 1.8%–13.5% of hospitalized patients with TC.8, 9, 10, 11, 12 Ventricular tachycardia, ventricular fibrillation, asystole, and pulseless electrical activity are included among LTAs. There is also an increased risk of developing atrial arrhythmias due to transient left atrial dysfunction in the acute phase of the disease. Furthermore, patients with atrial fibrillation in the setting of TC may have a lower long-term prognosis.13 Schneider et al reported a 15% prevalence of atrial fibrillation and an 8% incidence of ventricular tachycardia in patients with TC. However, given the reversible nature of TC, data regarding the optimal management of arrhythmias in this setting is lacking and the need for device implantation is controversial.
Different studies report a highly variable incidence of life-threatening arrhythmias in patients with Takotsubo cardiomyopathy, making the incidence of LTAs in TC unclear, thereby necessitating this meta-analysis. This research also aims to gauge whether life-threatening arrhythmias increase the risk of in-hospital mortality, long-term mortality, and cardiogenic shock in patients with Takotsubo cardiomyopathy as compared to the non-LTAs group.
2. Methods
In conducting this systematic review and meta-analysis, we adopted the Cochrane Collaboration guidelines and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis).14,15
2.1. Data source and study selection
A rigorous literature search was conducted using PubMed, Google Scholar, and Embase from their inception to February 2021, without any language restrictions. Following search terms were used: life-threatening arrhythmias OR LTAs OR ventricular arrhythmias AND Takotsubo syndrome OR Takotsubo cardiomyopathy OR Apical ballooning syndrome OR Broken heart syndrome OR stress cardiomyopathy AND incidence AND mortality. Additional related studies were found in the reference lists of the included studies. The articles found through the systematic search were exported to the EndNote Reference Library software, where duplicates were identified and removed. Two independent investigators reviewed the titles and abstracts of studies and subsequently assessed the full texts of the retrieved articles to reaffirm relevance. Only those articles that met our predefined inclusion criteria were included.
2.2. Eligibility criteria
Studies were included if they met the following inclusion criteria: (1) studies that reported the incidence of life-threatening arrhythmias, detected either on admission or during hospital stay, in the patients of Takotsubo cardiomyopathy, (2) studies that reported the mortality in Takotsubo cardiomyopathy patients with and without life-threatening arrhythmias, and (3) studies with patients ≥18 years and a sample size of ≥10 patients. The definition of Life-threatening arrhythmias (LTAs) was accepted as reported by the individual studies. Across all studies, LTAs included ventricular tachycardia (VT), ventricular fibrillation (Vfib), ventricular flutter, second-degree atrioventricular (AV) block type II, third-degree AV block, pulseless electrical activity, asystole, Torsade de Pointes (TdP), and high degree sinoatrial (SA) block. The exclusion criteria were pre-determined as follows: (1) duplicate publications, (2) studies that included information about atrial arrhythmias only, (3) studies that did not mention the outcomes of atrial and ventricular arrhythmias in TC patients separately, and (4) commentaries, reviews, and posters.
2.3. Data extraction and quality assessment
Two researchers independently extracted and entered the following data and into a standard Excel form: name of the first author, publication year, study design, inclusion/exclusion criteria, sample sizes, in-hospital mortality, long-term mortality, and cardiogenic shock. Any discrepancies in data were resolved by consulting a third investigator. The Newcastle–Ottawa Quality Assessment Scale was deployed to assess the quality of the selected studies and the risk of bias.16
2.4. Statistical analysis
ReviewManager (Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and MedCalc® Statistical Software version 19.6.4 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2021) used for all statistical analyses. Incidence were pooled using random effect model using DerSimonian and Laird estimator of Tau2. The Mantel-Haenszel random-effects model was used to pool odds ratios (ORs) with 95% confidence intervals (CIs). The I2 statistics were used to assess the heterogeneity of effect size estimates across these studies with I2 (low heterogeneity: I2 ≤ 25%; moderate: 25–50%; high >75%). A leave-one-out sensitivity analysis was also carried out to assess the effects of individual studies on the statistical results. Publication bias was explored using funnel plots and Egger's regression test and Begg-Mazumdar's rank correlation test.
3. Results
3.1. Literature search results
The initial database searches yielded 2812 potential records. After removing duplicates and screening titles and abstracts, 59 full-text articles were reviewed. Finally, Finally, 18 observational, including 55,557 participants (2,185 with LTAs and 53,372 without LTAs), were eligible for inclusion in the study.8,9,23, 24, 25, 26, 27, 28, 29, 30,10,11,17, 18, 19, 20, 21, 22 The selection process is outlined in the PRISMA flow chart (Supplementary Figure 1). Studies from institutions which were part of the GEIST registry we excluded from the present analysis. Only the latest national inpatient sample study was included in the present study. Measures were taken to not include studies with same patient cohort.
3.2. Study characteristics and quality assessment
Table 1 summarizes the study characteristics of the included studies. Clinical characteristics of included studies are outlined in Table 2. As shown in Supplementary Table 3, all included studies were of high quality.
Table 1.
Study characteristics of the included studies.
| First author | Country | Study Design | Total Population (n) | Inclusion criteria | Exclusion criteria |
|---|---|---|---|---|---|
| Auzel O et al, 2016 | France | Retrospective case study | 90 |
|
|
| Dib C et al, 2008 | United States | Case-control study | 105 |
|
|
| El-Battrawy I et al, 2020 | Germany and Italy | Prospective cohort study | 906 | TC defined as being a transient systolic dysfunction with marked LV contraction abnormality due to akinesia or dyskinesia of the LV apical and/or midventricular or basal segments extending beyond a single coronary perfusion bed | – |
| Jesel L et al, 2018 | France | Retrospective study | 214 |
|
– |
| Madias C et al, 2011 | United States | Cohort | 93 |
|
– |
| Malanchini G et al, 2020 | Italy | Retrospective study | 10,861 |
|
– |
| Song BG et al, 2010 | Korea | Retrospective study | 87 |
|
– |
| Sharkey SW et al, 2010 | United States | Cohort | 136 |
|
– |
| Brinjikji W et al, 2012 | United States | Retrospective study | 24,701 |
|
– |
| Regnante RR et al, 2009 | United States | Cohort study | 70 |
|
– |
| Bento D et al, 2019 | Portugal | Cohort study | 234 |
|
|
| Tsuchihashi K et al, 2001 | Japan | Retrospective study | 88 |
|
Patients with idiopathic cardiomyopathy, febrile disorders, pheochromocytoma or prior history of myocardial infarction and those receiving coronary revascularization therapy were excluded from this study. |
| Pant S et al 2013 | United States | Retrospective study | 16,450 |
|
Patients with ACS, ischemic heart disease or any other form of cardiomyopathy were excluded. |
| Murakami T et al 2013 | Japan | Retrospective study | 107 |
|
Patients with pheochromocytoma or myocarditis were excluded |
| Migliore F et al, 2012 | Italy | Prospective study | 61 |
|
– |
| Templin C et al, 2015 | Switzerland | Prospective and retrospective, observational study | 1750 |
|
Patients with the presence of coexisting coronary artery disease, the presence of a wall-motion abnormality that was congruent with a single coronary artery territory in a patient matching all other criteria and death during the acute phase before wall-motion recovery were excluded |
| Citro R et al, 2012 | Italy | Partially retrospective, partially prospective observational study | 190 |
|
– |
| Sharkey SW et al, 2015 | United States | Prospective | 249 |
|
– |
ABS: Apical ballooning syndrome, ACS: acute coronary syndrome, CAG: coronary angiogram, CMR: cardiovascular magnetic resonance, ECG: electrocardiogram, LTAs: life-threatening arrhythmias, LV: left ventricle, SC: stress cardiomyopathy, SCM: stress cardiomyopathy, SD: standard deviation, TLVBS: transient left ventricular ballooning syndrome, TC: takotsubo cardiomyopathy, VA: ventricular arrhythmias, VF: ventricular fibrillation, VT: ventricular tachycardia.
Table 2.
Baseline Clinical characteristics of the included studies.
| First Author |
Total Population (n) | Participant description and Mean age (SD) | Type and prevalence of LTAs | In-hospital mortality | Long-term mortality | Follow-up for long-term mortality |
|---|---|---|---|---|---|---|
| Auzel O et al, 2016 | 90 |
|
Ventricular arrhythmias: non-sustained and sustained VT and VF. n = 9 (10%) |
|
– | – |
| Dib C et al, 2008 | 105 |
|
Significant arrhythmia: VF and asystole. n = 6 (5.7%) |
|
|
– |
| El-Battrawy I et al, 2020 | 906 |
|
VT, VF, torsade de pointes (TdP), and asystole or complete atrioventricular block) n = 67 (7.4%) |
|
|
3 years |
| Jesel L et al, 2018 | 214 |
|
LTAs were defined as VT, VF, or sudden cardiac arrest. n = 23 (10.7%) |
- LTA group = 9/23 -No LTA group = 17/191 |
|
1 year |
| Madias C et al, 2011 | 93 |
|
Malignant ventricular arrhythmias: VF and torsades de pointes (TdP). n = 8 (8.6%) |
- LTA group = 0/8 - No LTA group = 4/85 |
- No LTA group = 77% - LTA group = 85% |
2 years |
| Malanchini G et al, 2020 | 10,861 |
|
VF and VT. VF n = 43 (31.1%) VT n = 90 (66.6%) |
241/10,861 (2,2%) | – | – |
| Song BG et al, 2010 | 87 |
|
Third-degree atrioventricular block, VF, VT, and cardiac arrest. Survivors n = 4 (6%) |
8/87 (9%) | 20/87 (23%) | 42 months |
| Sharkey SW et al, 2010 | 136 |
|
– | 2% | – | – |
| Brinjikji W et al, 2012 | 24,701 |
|
– | 4.2% | – | – |
| Regnante RR et al, 2009 | 70 |
|
Sustained ventricular arrhythmias: VF or VT n = 3 (4%) |
|
|
– |
| Bento D et al, 2019 | 234 |
|
VF, VT, and complete atrioventricular block n = 11 (4.7%) |
2.2% | 4.4% | 33 ± 33 months |
| Tsuchihashi K et al, 2001 | 88 |
|
Atrioventricular block, VT and VF n = 12 |
1% | 2% | 13 ± 14 months |
| Pant S et al 2013 | 16,450 |
|
VT, VF, ventricular flutter, and SCA n = 1003 |
|
– | – |
| Murakami T et al 2013 | 107 |
|
Sustained VT, VF, and advanced atrioventricular block n = 5 |
8.4% | – | – |
| Migliore F et al, 2012 | 61 |
|
n = 5 | – | – | 57 ± 23 months |
| Templin C et al, 2015 | 1750 |
|
VT n = 53 | 4.1% | 5.6% per patient-year | 10 years |
| Citro R et al, 2012 | 190 |
|
VT and VF n = 8 | 2.8% | – | – |
| Sharkey SW et al, 2015 | 249 |
|
VF, pulseless electrical activity, and asystole n = 9 | 1.2% | 8% | 4.7 years |
ABS: Apical ballooning syndrome, ACS: acute coronary syndrome, CAG: coronary angiogram, CMR: cardiovascular magnetic resonance, ECG: electrocardiogram, LTAs: life-threatening arrhythmias, LV: left ventricle, SC: stress cardiomyopathy, SCM: stress cardiomyopathy, SD: standard deviation, TLVBS: transient left ventricular ballooning syndrome, TC: takotsubo cardiomyopathy, VA: ventricular arrhythmias, VF: ventricular fibrillation, VT: ventricular tachycardia.
4. Results of meta-analysis
1. Incidence of life-threatening arrhythmias in Takotsubo cardiomyopathy:
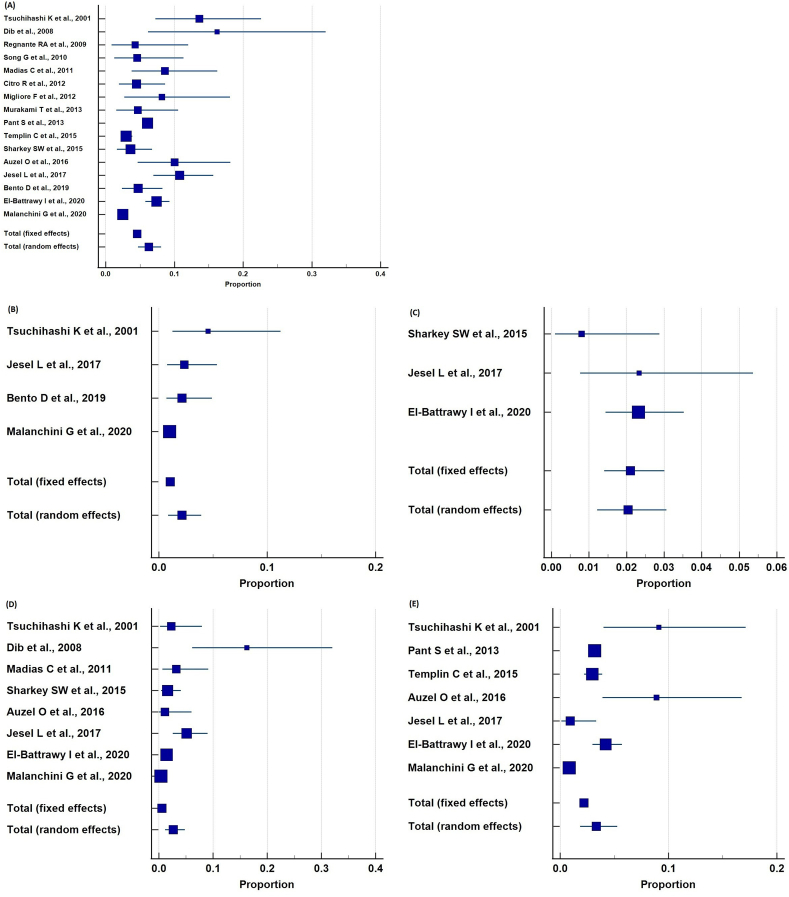
The incidence of LTAs in TC patients was reported by 16 studies. The pooled incidence of life-threatening arrhythmias in the patients of TC was found to be 6.29% (CI: 4.70–8.08%; I2 = 94.67%). The data for the incidence of individual LTAs was also meta-analyzed, as shown in Table 3. Fig. 1 illustrates the forest plots for the pooled incidence of LTAs in TC.
-
2.
In-hospital mortality:
Table 3.
Pooled prevalence of life-threatening arrhythmias in Takotsubo Cardiomyopathy.
| Type of LTA | Number of studies | Sample size | Pooled prevalence |
|---|---|---|---|
| Overall | 16 | 31,475 | 6.285% (CI: 4.698–8.084%; I2 = 94.67%) |
| Complete atrioventricular block | 4 | 11,397 | 2.129% (CI: 0.877–3.912%; p = 0.0116; I2 = 72.76%) |
| Asystole | 3 | 1369 | 2.036% (CI: 1.216–3.061%; p = 0.2739; I2 = 22.84%) |
| Ventricular fibrillation | 8 | 12,538 | 2.674% (CI: 1.159–4.789%; p < 0.0001; I2 = 89.58%) |
| Ventricular tachycardia | 7 | 30,359 | 3.343% (CI: 1.844–5.264%; p < 0.0001; I2 = 97.52%) |
LTA: life-threatening arrhythmia, CI: confidence interval, p: probability value.
Fig. 1.
Pooled incidence of life-threatening arrhythmias in Takotsubo Cardiomyopathy patients (A) Overall LTAs (B) Complete AV-Block (C) Asystole (D) Ventricular fibrillation (E) Ventricular tachycardia.
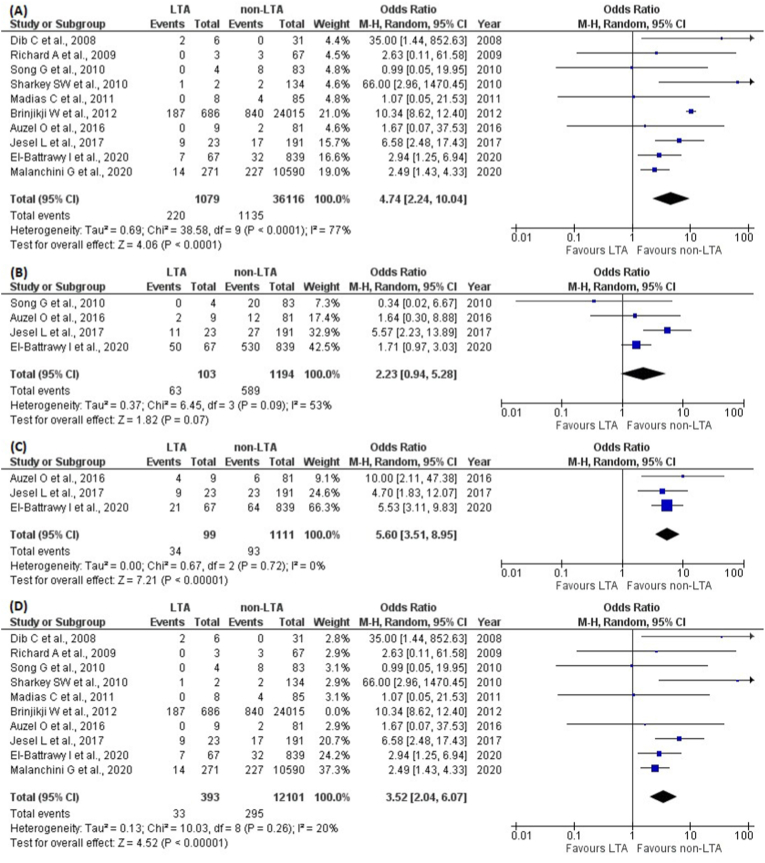
Ten included studies reported in-hospital mortality of TC patients with LTAs compared with TC patients without LTAs. A total of 220 (20.4%) out of 1079 patients in the LTA group had an in-hospital death, while 1135 (3.1%) out of 36,116 patients in the non-LTA group died. There was a statistically significant (p < 0.0001) increased odds of mortality in the LTA group versus the non-LTA group (OR = 4.74; CI: 2.24–10.04; I2 = 77%; Fig. 2(A)).
-
3.
Long-term mortality:
Fig. 2.
(A) Pooled Odds Ratios of in-hospital mortality in the LTA group versus the non-LTA group of TC patient (B) Pooled Odds Ratios of long-term mortality in the LTA group versus the non-LTA group of TC patients (C) Pooled Odds Ratios of cardiogenic shock development in the LTA group versus the non-LTA group of TC patients (D) Pooled Odds Ratios of in-hospital mortality in the LTA group versus the non-LTA group of TC patients after sensitivity analysis. CI = confidence interval; M−H = Mantel-Haenszel; df = degrees of freedom.
We also estimated the pooled analysis of long-term mortality in the LTA and the non-LTA groups. Four studies reported long-term mortality. A total of 63 (61.2%) out of 103 patients in the LTA group died, whereas 589 (49.3%) out of 1194 patients in the non-LTA group had long-term mortality. There were similar odds of long-term mortality in the LTA group as compared with the non-LTA group (OR = 2.23; CI: 0.94–5.28; I2 = 53%, p = 0.07; Fig. 2(B)).
-
4.
Cardiogenic shock (CS):
Three studies investigated the number of TC patients who developed cardiogenic shock. A total of 34 (34.3%) out of 99 patients in the LTA group experienced CS, while only 93 (8.37%) out of 1111 patients in the non-LTA group developed it. There was statistically significant (p < 0.00001) increased odds of CS in the LTA group versus the non-LTA group (OR = 5.60; CI: 3.51–8.95; I2 = 0%; Fig. 2(C)).
4.1. Sensitivity analysis
The I2 statistics were used to assess the heterogeneity of effect size estimates across these studies with I2 (low heterogeneity: I2 ≤ 25%; moderate: 25–50%; high >75%). For the in-hospital mortality, I2 = 77% showed significant heterogeneity. The leave-one-out sensitivity analysis confirmed that the data by Brinjki W et al were the main source of heterogeneity in the analysis of the in-hospital mortality. The I2 value dropped to 20% after omitting the data from this study, as shown in Fig. 2(D).
4.2. Publication bias
Supplementary Figure 2 illustrates the funnel plots for the outcomes of in-hospital mortality, long-term mortality, and cardiogenic shock. Assessment of publication bias, using Egger's regression test and Begg-Mazumdar's rank correlation test revealed no significant publication bias for overall incidence of life-threatening arrhythmias in Takotsubo cardiomyopathy (Egger's regression test; p = 0.3982, Begg-Mazumdar's rank correlation test; p = 0.4713).
5. Discussion
Our study aimed to report the incidence of LTAs patients with Takotsubo cardiomyopathy and their outcomes. We found a pooled incidence of 6.29% LTAs in our study, with ventricular tachycardia as the most common arrhythmia (3.43%). Further our study reported an increased odds of in-hospital mortality and cardiogenic shock among TC patients with LTAs compared with those without LTAs. However, there was no difference in the odds of long-term mortality.
Life-threatening arrhythmias in TC have been reported with a varying incidence in literature. While a study from Italy reported a incidence of 8.2% for LTAs during hospitalization for TC,8 results from Stiermaier et al indicate a higher-than-expected incidence at 13.5%.12 A recent study demonstrated that LT ventricular arrhythmias (VAs) were more common in patients that developed sub-acute VAs during hospitalization, occurring in 6% of the total population.31 These LTAs seemed to have a strong clinical impact on the patient outcomes and survival, since mortality was higher in the VAs group than in the non-VAs group (P = 0.03). Additional studies have supporting evidence, such as reported by Jesel et al, in-hospital (39.1%; p < 0.001) and 1-year mortality (47.8%; p < 0.001) was significantly increased in the LTA group19 as compared with non-LTA TC patients. Thus we urge for awareness about this potential complication, since it can be critical for further patient management.
Our pooled analysis showed a significantly higher odds of in-hospital mortality in TC patients with LTAs. The majority of the patients had ventricular arrhythmia, for example, ventricular fibrillation (Vfib). Ventricular arrhythmias are thought to be the most common LTA to occur in TC patients and can cause a worse long-term prognosis of the disease.32 Although the exact theory is uncertain, there are some proposed mechanisms such as coronary vasospasm, re-entry, and triggered activity. Catecholamine-induced myocardial stunning can cause abnormal automaticity and depolarization anomalies such as a prolonged QT interval, a known predisposing risk factor for Vfib.33 Conduction defects such as Atrioventricular (AV) Heart Block, although rare, are another recurring LTA in TC patients described across multiple reports.24,34,35 AV blocks can persist long term after TC prsentation, and may require interventions such as a pacemaker; Baranchuk et al reported a patient in whom high-degree AV block was persistent after 1 year of the TC event, eventually resolving after 2 years of follow-up,36 while another case of TC had a high AV block 20 months after the inciting event.37 Hence, it is important to recognize and manage the patient timely, to ensure their safety.
Additionally, our study demonstrates similar odds of long-term mortality for TC patients with LTAs as compared with those who do not. Although cardiovascular abnormalities have been shown in some reports to affect the mortality of Takotsubo Cardiomyopathy patients,38,39 multiple studies have shown that non-cardiac comorbidities and complications seem to play a strong prognostic role in predicting long-term outcomes for these patients.40 A systematic review conducted by Pelliccia et al found that 78% of TC patient deaths were due to non-cardiac causes, while only 22% of deaths were cardiac.41 As collated in a study on 1109 patients, the most common comorbidities in TC patients included psychiatric and psychological illnesses, pulmonary disease, and malignancies, followed by neurological, chronic kidney, and thyroid diseases. These extra-cardiac conditions can also predispose to TC since they can increase catecholamine synthesis as part of the disease process.42 Furthermore, long-term mortality rates of TC exceed those of patients with STEMI as concluded by Stiermaier et al (24.7% vs 15.1%, p = 0.02)43; hence, there is a need to raise awareness regarding the optimal treatment of comorbidities and risk factors, with management aimed at prevention of stressful events.
Our results revealed a significantly higher odds of CS in TC patients with LTAs than in those without an LTA. Although there is a paucity of data available regarding long-term complications of CS in TC patients, it is a severe complication of the acute phase of the disease and requires urgent treatment with otherwise imminent short-term mortality.44 A registry-based study concluded that short-term mortality of CS in TC patients was 29%45(19), while another prospective single-center found their acute fatality rate to be very similar, at 28.6%.43 However, the short-term mortality of CS due to myocardial infarction is still much greater than that of CS-TC. A national representative study found that myocardial infarction-CS had higher in-hospital mortality rates, hospital costs, and lower home discharges often compared with TC-CS admissions.46 This most likely is due to the reversibility of the LV dysfunction in TC patients. Further studies are needed for insight into the long-term effects of CS in TC patients, which will allow for the development of better longitudinal care and lower adverse outcomes.
Our study has several limitations, one of which is the inherent limitations of an observational nature of the studies selected, such as the accuracy of medical documentation and missing information. We were also unable to comment on the co-morbidities of all patients involved; hence, a potential confounder may be present affecting the mortality of TC patients with LTAs. This is a study level meta-analysis and study level pooled estimates are limited in their ability explain heterogeneity of pooled estimates. Further, treatment modalities, medications used in this TC patients were not reported consistently among included studies.
6. Conclusion
The pooled incidence of LTAs in the patients of TC was found to be 6.29%, with ventricular tachycardia being the most common arrhythmia (3.43%). In the group of TC patients with LTAs, the odds of in-hospital mortality and cardiogenic shock were significantly higher than in the TC patients without LTAs. However, there was no significant difference in long-term mortality between the two groups.
Source of funding
No funding sources to declare.
Declaration of competing interest
The authors declare they have no conflict of interest.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2022.01.005.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gianni M., Dentali F., Grandi A.M., Sumner G., Hiralal R., Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27:1523–1529. doi: 10.1093/eurheartj/ehl032. [DOI] [PubMed] [Google Scholar]
- 2.Akashi Y.J., Nef H.M., Lyon A.R. Epidemiology and pathophysiology of Takotsubo syndrome. Nat Rev Cardiol. 2015;12:387–397. doi: 10.1038/nrcardio.2015.39. [DOI] [PubMed] [Google Scholar]
- 3.Veillet-Chowdhury M., Hassan S.F., Stergiopoulos K. Takotsubo cardiomyopathy: a review. Acute Card Care. 2014;16:15–22. doi: 10.3109/17482941.2013.869346. [DOI] [PubMed] [Google Scholar]
- 4.Amin H.Z., Amin L.Z., Pradipta A. Takotsubo cardiomyopathy: a brief review. J Med Life. 2020;13:3–7. doi: 10.25122/jml-2018-0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown K.H., Trohman R.G., Madias C. Arrhythmias in takotsubo cardiomyopathy. Card Electrophysiol Clin. 2015;7:331–340. doi: 10.1016/j.ccep.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Jesel L., Berthon C., Messas N., et al. Atrial arrhythmias in Takotsubo cardiomyopathy: incidence, predictive factors, and prognosis. Eur Eur Pacing, Arrhythmias, Card Electrophysiol J Work Groups Card Pacing, Arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol. 2019;21:298–305. doi: 10.1093/europace/euy147. [DOI] [PubMed] [Google Scholar]
- 7.Prasad A., Lerman A., Rihal C.S. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–417. doi: 10.1016/j.ahj.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Migliore F., Zorzi A., Peruzza F., et al. Incidence and management of life-threatening arrhythmias in Takotsubo syndrome. Int J Cardiol. 2013;166:261–263. doi: 10.1016/j.ijcard.2012.09.107. [DOI] [PubMed] [Google Scholar]
- 9.Malanchini G., Del Corral M.P., De Filippo P., Ferrari P., Solomon A., Krepp J. Cardiac arrhythmias and In-hospital mortality amongst patients with takotsubo cardiomyopathy: a retrospective study in an Italian population. Int J Cardiol Hear Vasc. 2020;31:100608. doi: 10.1016/j.ijcha.2020.100608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Templin C., Ghadri J.R., Diekmann J., et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 11.Madias C., Fitzgibbons T.P., Alsheikh-Ali A.A., et al. Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm. 2011;8:555–561. doi: 10.1016/j.hrthm.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 12.Stiermaier T., Eitel C., Denef S., et al. Prevalence and clinical significance of life-threatening arrhythmias in takotsubo cardiomyopathy. J Am Coll Cardiol. 2015;65:2148–2150. doi: 10.1016/j.jacc.2015.02.062. [DOI] [PubMed] [Google Scholar]
- 13.El-Battrawy I., Lang S., Ansari U., et al. Impact of concomitant atrial fibrillation on the prognosis of Takotsubo cardiomyopathy. Eur Eur Pacing, Arrhythmias, Card Electrophysiol J Work Groups Card Pacing, Arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol. 2017;19:1288–1292. doi: 10.1093/europace/euw293. [DOI] [PubMed] [Google Scholar]
- 14.van Tulder M., Furlan A., Bombardier C., Bouter L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa. 1976;28:1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. 2003. [DOI] [PubMed] [Google Scholar]
- 15.Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lo C.K.L., Mertz D., Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:1–5. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Auzel O., Mustafic H., Pillière R., El Mahmoud R., Dubourg O., Mansencal N. Incidence, characteristics, risk factors, and outcomes of takotsubo cardiomyopathy with and without ventricular arrhythmia. Am J Cardiol. 2016;117:1242–1247. doi: 10.1016/j.amjcard.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 18.Dib C., Prasad A., Friedman P.A., et al. Malignant arrhythmia in apical ballooning syndrome: risk factors and outcomes. Indian Pacing Electrophysiol J. 2008;8:182–192. [PMC free article] [PubMed] [Google Scholar]
- 19.Jesel L., Berthon C., Messas N., et al. Ventricular arrhythmias and sudden cardiac arrest in Takotsubo cardiomyopathy: incidence, predictive factors, and clinical implications. Heart Rhythm. 2018;15:1171–1178. doi: 10.1016/j.hrthm.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 20.Song B.G., Hahn J.-Y., Cho S.J., et al. Clinical characteristics, ballooning pattern, and long-term prognosis of transient left ventricular ballooning syndrome. Heart Lung. 2010;39:188–195. doi: 10.1016/j.hrtlng.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 21.Sharkey S.W., Pink V.R., Lesser J.R., Garberich R.F., Maron M.S., Maron B.J. Clinical profile of patients with high-risk tako-tsubo cardiomyopathy. Am J Cardiol. 2015;116:765–772. doi: 10.1016/j.amjcard.2015.05.054. [DOI] [PubMed] [Google Scholar]
- 22.Regnante R.A., Zuzek R.W., Weinsier S.B., et al. Clinical characteristics and four-year outcomes of patients in the Rhode Island Takotsubo Cardiomyopathy Registry. Am J Cardiol. 2009;103:1015–1019. doi: 10.1016/j.amjcard.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 23.Bento D., Azevedo O., Santos R., et al. Short- and medium-term prognosis of Takotsubo syndrome in a Portuguese population. Rev Port Cardiol. 2019;38:349–357. doi: 10.1016/j.repc.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Tsuchihashi K., Ueshima K., Uchida T., et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. 2001;38:11–18. doi: 10.1016/s0735-1097(01)01316-x. [DOI] [PubMed] [Google Scholar]
- 25.Pant S., Deshmukh A., Mehta K., et al. Burden of arrhythmias in patients with Takotsubo cardiomyopathy (apical ballooning syndrome) Int J Cardiol. 2013;170:64–68. doi: 10.1016/j.ijcard.2013.10.041. [DOI] [PubMed] [Google Scholar]
- 26.Murakami T., Yoshikawa T., Maekawa Y., et al. Characterization of predictors of in-hospital cardiac complications of takotsubo cardiomyopathy: multi-center registry from Tokyo CCU Network. J Cardiol. 2014;63:269–273. doi: 10.1016/j.jjcc.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Citro R., Rigo F., Previtali M., et al. Differences in clinical features and in-hospital outcomes of older adults with tako-tsubo cardiomyopathy. J Am Geriatr Soc. 2012;60:93–98. doi: 10.1111/j.1532-5415.2011.03730.x. [DOI] [PubMed] [Google Scholar]
- 28.Sharkey S.W., Windenburg D.C., Lesser J.R., et al. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–341. doi: 10.1016/j.jacc.2009.08.057. [DOI] [PubMed] [Google Scholar]
- 29.El-Battrawy I., Santoro F., Stiermaier T., et al. Prevalence, management, and outcome of adverse rhythm disorders in takotsubo syndrome: insights from the international multicenter GEIST registry. Heart Fail Rev. 2020;25:505–511. doi: 10.1007/s10741-019-09856-4. [DOI] [PubMed] [Google Scholar]
- 30.Brinjikji W., El-Sayed A.M., Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J. 2012;164:215–221. doi: 10.1016/j.ahj.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 31.Pelargonio G., La Rosa G., Di Stasio E., et al. Ventricular arrhythmias in Takotsubo Syndrome: incidence, predictors and clinical outcomes. J Cardiovasc Med. 2021;22:180–189. doi: 10.2459/JCM.0000000000001106. [DOI] [PubMed] [Google Scholar]
- 32.Möller C., Eitel C., Thiele H., Eitel I., Stiermaier T. Ventricular arrhythmias in patients with Takotsubo syndrome. J Arrhythmia. 2018;34:369–375. doi: 10.1002/joa3.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pena Escobar J.A., Aung M., Amin S., Gulraiz A., Gandhi F.R., Malik B.H. Pathogenesis of ventricular arrhythmias and its effect on long-term prognosis in patients with takotsubo cardiomyopathy. Cureus. 2020;12:e11171. doi: 10.7759/cureus.11171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lopes L.R., Vinhas H., Cordeiro P., et al. Five cases of transient left ventricular apical ballooning--the experience of a Portuguese center. Rev Port Cardiol Orgao Of Da Soc Port Cardiol = Port J Cardiol an Off J Port Soc Cardiol. 2008;27:495–502. [PubMed] [Google Scholar]
- 35.Sharkey S.W., Lesser J.R., Zenovich A.G., et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation. 2005;111:472–479. doi: 10.1161/01.CIR.0000153801.51470.EB. [DOI] [PubMed] [Google Scholar]
- 36.Nault M.A., Baranchuk A., Simpson C.S., Redfearn D.P. Takotsubo cardiomyopathy: a novel “proarrhythmic” disease. Anadolu Kardiyol Derg. 2007;7(Suppl 1):101–103. [PubMed] [Google Scholar]
- 37.Sakul N.F.N., Shrestha S., Balabbigari N., Talati S. Complete heart block: a rare complication of takotsubo syndrome. Case Reports Cardiol. 2019;2019:1–5. doi: 10.1155/2019/2576373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parodi G., Bellandi B., Del Pace S., et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011;139:887–892. doi: 10.1378/chest.10-1041. [DOI] [PubMed] [Google Scholar]
- 39.Núñez-Gil I.J., Molina M., Bernardo E., et al. Tako-tsubo syndrome and heart failure: long-term follow-up. Rev Esp Cardiol. 2012;65:996–1002. doi: 10.1016/j.recesp.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 40.Vriz O., Brosolo G., Martina S., et al. In-hospital and long-term mortality in Takotsubo cardiomyopathy: a community hospital experience. J Community Hosp Intern Med Perspect. 2016;6:31082. doi: 10.3402/jchimp.v6.31082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pelliccia F., Pasceri V., Patti G., et al. Long-term prognosis and outcome predictors in takotsubo syndrome: a systematic review and meta-regression study. JACC Heart Fail. 2019;7:143–154. doi: 10.1016/j.jchf.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 42.Pelliccia F., Parodi G., Greco C., et al. Comorbidities frequency in Takotsubo syndrome: an international collaborative systematic review including 1109 patients. Am J Med. 2015;128 doi: 10.1016/j.amjmed.2015.01.016. 654.e11-9. [DOI] [PubMed] [Google Scholar]
- 43.Stiermaier T., Moeller C., Oehler K., et al. Long-term excess mortality in takotsubo cardiomyopathy: predictors, causes and clinical consequences. Eur J Heart Fail. 2016;18:650–656. doi: 10.1002/ejhf.494. [DOI] [PubMed] [Google Scholar]
- 44.Stiermaier T., Eitel C., Desch S., et al. Incidence, determinants and prognostic relevance of cardiogenic shock in patients with Takotsubo cardiomyopathy. Eur Hear Journal Acute Cardiovasc Care. 2016;5:489–496. doi: 10.1177/2048872615612456. [DOI] [PubMed] [Google Scholar]
- 45.Schneider B., Athanasiadis A., Schwab J., et al. Complications in the clinical course of tako-tsubo cardiomyopathy. Int J Cardiol. 2014;176:199–205. doi: 10.1016/j.ijcard.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 46.Vallabhajosyula S., Dunlay S.M., Murphree D.H.J., et al. Cardiogenic shock in takotsubo cardiomyopathy versus acute myocardial infarction: an 8-year national perspective on clinical characteristics, management, and outcomes. JACC Heart Fail. 2019;7:469–476. doi: 10.1016/j.jchf.2018.12.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.