Abstract
Objective:
Industry relationships drive technologic innovation in interventional radiology and offer opportunities for professional growth. Women are underrepresented in interventional radiology despite the growing recognition of the importance of diversity. This study characterized gender disparities in financial relationships between industry and academic interventional radiologists.
Subjects and Methods:
In this retrospective cross-sectional study, U.S. academic interventional radiology physicians and their academic ranks were identified by searching websites of practices with accredited interventional radiology fellowship programs. Publicly available databases were queried to collect each physician’s gender, years since medical school graduation, h index, academic rank, and industry payments in 2018. Wilcoxon and chi-squared tests compared payments between genders. A general linear model assessed the impact of academic rank, years since graduation, gender, and h index on payments.
Results:
Of 842 academic interventional radiology physicians, 108 (13%) were women. A total $14,206,599.41 was received by 686 (81%) doctors; only $147,975.28 (1%) was received by women. A lower percentage of women (74%) than men (83%) received payments (p=0.047); median total payments were lower for women ($535) than men ($792) (p=0.012). Academic rank, h index, years since graduation, and male gender were independent predictors of higher payments. Industry payments supporting technologic advancement were made exclusively to men.
Conclusions:
Women interventional radiology physicians received fewer and lower industry payments, earning 1% of total payments despite constituting 13% of physicians. Gender independently predicted industry payments, regardless of h index, academic rank, or years since graduation. Gender disparity in interventional radiology physician-industry relationships warrants further investigation and correction.
Introduction
Partnerships with industry drive important technologic progress in the field of radiology [1, 2], and provide individual radiologists with opportunities for professional growth and additional compensation [3]. Male doctors in other specialties receive greater industry payments compared to female doctors, indicating that they may earn more supplemental income and participate to a greater extent in technologic advancement, and this gender gap may be larger in fields that are more male-dominated [4, 5].
Interventional radiology (IR) is among the most male-dominated of all medical specialties, with women comprising fewer than 10% of academic IR faculty in the US in 2012, and roughly 15% of IR fellows in training [6]. Women academic radiologists earn similar salaries compared with men [7], and female IR physicians publish and earn grants in proportion to their numbers in the field [8] and perform equally complex procedures compared to male IR doctors [9]. Despite these similarities, and a growing recognition of the importance of maintaining a diverse workforce [10], the number of women pursuing careers in IR is currently small, possibly due to its male-dominated nature [11, 12]. One possible manifestation of the underrepresentation of women in IR may be disparities in industry ties. Such a disparity could indicate an undervaluation of the input of women to technological advancement in IR. This study sought to determine whether there is a gender gap in industry payments in academic IR and whether that gap is associated with academic rank or productivity.
Subjects and Methods
Academic IR physicians in the U.S. were identified by searching the online faculty rosters provided by every radiology department with an Accreditation Council for Graduate Medical Education (ACGME)-accredited IR fellowship program [13]. The study focused on academic IR physicians, because 1) a disproportionate amount of industry payments are made to academic compared with private practice doctors in other fields [14], and 2) there is no available listing of all current and past IR doctors in the U.S. by practice type, due to the historical variability in training pathways and certification and licensing of IR physicians. All faculty in each academic IR department or division were identified by each program’s website in January 2019, and faculty members’ academic ranks were recorded whenever they were available. For several institutions, academic rank was not available publicly online; in these cases, faculty members at that institution were contacted by email or telephone to ascertain academic ranks. Institutional review board approval and consent were not required for this study, which analyzed public data.
Each academic IR physician’s national practitioner identification number (NPI), gender, and practice location were determined by searching the Centers for Medicare and Medicaid Services (CMS) National Plan and Provider Enumeration System’s database, using its December 2018 data dissemination [15]. NPIs were then used to locate each physician’s entry in CMS’s Physician Compare database [16], to determine the year in which he or she graduated from medical school. The number of years in practice was estimated as the number of years between medical school graduation and 2019. These searches were performed using automated software that was created for use in this study, and automated searches were supplemented by manual search when they failed to match any physician, or matched more than one physician.
Industry payments to academic IR physicians were identified by searching the Open Payments Database [17]. CMS maintains Open Payments as a compendium of payments that manufacturers and group purchasing organizations are required to report by the Physician Sunshine Payment Act [18]. Payment data were available from the date of the program’s commencement, August 1, 2013, through the end of 2018, and were derived from CMS data released on June 28, 2019. Again, this search was performed using automated software that was created for use in this study, supplemented by manual searching when necessary. The nature of each payment and the name of each corporate payer were recorded. The types of payments to IR physicians in 2018 included: research, consulting, honoraria, grants, royalties and licenses, accredited faculty services (i.e., compensation for services as a faculty at an accredited continuing education program), unaccredited faculty services (i.e., compensation for services as a faculty at an unaccredited continuing education program), education, entertainment, food and beverage, travel and lodging, gifts, and ownership/investment (i.e., current or prospective ownership or investment interest, defined as “ownership or investment interests currently held by physicians and teaching hospitals, as well as ownership interests or investments that physicians and teaching hospitals have not yet exercised” on the Open Payments website). Research, royalties and licenses, and ownership/investment were considered to reflect payments directly supporting technological advancement, per CMS’s description of the payment categories [19]. Consulting fees were not included as payments directly supporting technological advancement, as they are defined as “Payments made to physicians for advice and expertise on a particular medical product or treatment, typically provided under a written agreement and in response to a particular business need. These payments often vary depending on the experience of the physician being consulted.” Consulting fees are not specific to research and development and are associated with increased prescribing of the payer’s products [20].
Each IR physician’s academic productivity was measured using the h index, a statistic that reflects the quantity and citation impact of an author’s published works [21]. H indices were obtained by manually searching a commercially maintained database [22]. In cases where there was more than one apparent author profile for a specific name, the author profile with the affiliation that matched the fellowship program affiliation was used.
Statistical analysis was performed using R 3.4.4, (R Foundation for Statistical Computing, Vienna, Austria) [23]. Because the list of academic IR physicians was based on information currently available in 2019, statistical analysis was focused on payments made in 2018, which was the most recent year for which payment data were available. For each type of payment in 2018, the mean (±standard deviation) and median (+range and interquartile range) amount paid were calculated separately for male IR physicians, female IR physicians, and all IR physicians. Mean and median years since medical school graduation, h index, and total payments in 2018 were also calculated. A Wilcoxon test was used to compare medians when >5 subjects were available. The median differences in payments between men and women and corresponding 95% confidence intervals (CI) were calculated with quantile regression. The proportions of academic ranks for men and women were calculated; the mean h index and years since medical school graduation were calculated for men and women at different academic ranks. Counts were compared with a chi-square or Fisher’s exact test. After evaluating the association between various variables, the effect of gender, years since graduation, academic rank and h index on the logarithmized total sum of payments was tested with a general linear model (formula: log(total pay)~gender+years since graduation+h index+academic rank). Due to the log transformation of the total payments, the estimates are given in exponentiated form (10estimate). All tests were two-tailed. A p-value of 0.05 was considered indicative of statistically significant differences. Payments made in the preceding years (2014—2017) were graphically summarized and qualitatively evaluated.
Results
In total, 842 academic IR physicians were identified at 97 U.S. academic institutions. Of these, 734 (87%) were men and 108 (13%) were women. There was regional heterogeneity in the relative proportions of men and women, with several states devoid of women IR physicians (Fig 1). Compared to their male counterparts, women had significantly fewer years since medical school graduation (median: 12 vs 17 years; p<0.001) and lower h indices (median: 4 vs 6; p=0.024). The proportions in each academic rank were similar between men and women IR physicians (Table 1). For each academic rank, women tended to have lower h indices and years since medical school graduation compared to men (Table 1).
Fig 1 —
Gender composition by state. States with no academic IR fellowship programs are presented in white. The gender quota for each state was calculated by dividing the number of women by the number of men IR physicians in that state.
Table 1.
Male and female IR physician characteristics. SD: standard deviation. “None” for h index indicates that the physician had no publications. “None” for academic rank indicates that no rank was assigned to that physician by his or her institution; “N/A” indicates that the academic rank could not be ascertained.
| Women (n=108) | Men (n=734) | Total (n=842) | p value | |
|---|---|---|---|---|
| Years since graduation | < 0.001 | |||
| Mean (SD) | 16 (9) | 20 (10) | 19 (10) | |
| Median (Q1, Q3) | 13 (8, 22) | 18 (11, 27) | 17 (11, 26) | |
| Min — Max | 6 — 49 | 4 — 52 | 4 — 52 | |
| H index | 0.024 | |||
| Mean (SD) | 7 (8) | 10 (13) | 10 (12) | |
| Median (Q1, Q3) | 4 (2, 9) | 6 (2, 15) | 5 (2, 13) | |
| Min — Max | 0— 43 | 0 — 154 | 0 — 154 | |
| None | 7 | 53 | 60 | |
| Academic rank | 0.248 | |||
| None | 12 (11%) | 50 (7%) | 62 (7%) | |
| Instructor | 3 (3%) | 18 (2%) | 21 (2%) | |
| Assistant | 49 (45%) | 267 (36%) | 316 (38%) | |
| Associate | 13 (12%) | 105 (14%) | 118 (14%) | |
| Professor | 7 (6%) | 82 (11%) | 89 (11%) | |
| N/A | 24 (22%) | 212 (29%) | 236 (28%) | |
| Mean (SD) h index and years in since medical school graduation by academic rank: | ||||
| Instructor | ||||
| n | 3 | 18 | ||
| H index | 0.7 (0.6) | 5.6 (3.4) | ||
| Years since graduation | 9 (3) | 15.1 (7.5) | ||
| Assistant | ||||
| n | 49 | 267 | ||
| H index | 3.6 (3.2) | 5.1 (6.4) | ||
| Years since graduation | 11.2 (6.1) | 15.7 (8.5) | ||
| Associate | ||||
| n | 13 | 105 | ||
| H index | 12.7 (5.5) | 11.9 (8) | ||
| Years since graduation | 21.6 (6.5) | 24.9 (8) | ||
| Professor | ||||
| n | 7 | 82 | ||
| H index | 22.1 (12.7) | 27.5 (20.5) | ||
| Years since graduation | 30.3 (7.8) | 31.1 (7.7) | ||
In 2018, the number of male IR physicians receiving any payment, regardless of the category or amount, was significantly greater than women IR physicians: 606 (83%) of 734 men and 80 (74%) of 108 women received payments of any type (p=0.047). In the categories of consulting and unaccredited faculty services, significantly more men received payments (Table 2). All payments made in 2018 to support technological advancement (research, royalties, and ownership/investment) were received by men and none by women. Analysis of payments data from 2017 revealed a similar pattern (data not shown).
Table 2.
Number of payments and median payments to men and women in 2018 by payment category (in USD). Categories with statistically significant differences are marked in bold, and categories where no women received any payment in italics. For number of payments, data presented as n (% of doctors within each gender category), with statistical significance tested with Fisher’s exact tests and chi-square tests of independence. Median payment amounts presented as median (IQR) and compared with Wilcoxon rank-sum tests. Median differences obtained with quantile regression (50th quantile; 95%-CI given in parentheses).
| Number of Payments | Median Payment Amounts | ||||||
|---|---|---|---|---|---|---|---|
| Payment category | Women (n=108) | Men (n=734) | p-value | Women | Men | p-value | Median difference |
| Research | 0 (0%) | 15 (2%) | - | 0 | $7,200 ($3,672, $18,980) | - | - |
| Consulting | 11 (10%) | 151 (21%) | 0.015 | $3,950 ($1,110, $5,360) | $5,499 ($2,448, $18,742) | 0.2 | $1,549 ($215 – $4,717) |
| Honoraria | 2 (2%) | 36 (5%) | 0.2 | $4,000 ($3,500, $4,500) | $3,000 ($2,000, $8,230) | 0.8 | - |
| Grants | 0 (0%) | 2 (0.3%) | - | 0 | $4,678 ($2,546, $6,809) | - | - |
| Entertainment | 0 (0%) | 5 (1%) | - | 0 | $199 ($94, $474) | - | - |
| Royalties and licenses | 0 (0%) | 10 (1%) | - | 0 | $77,812 ($38,349, $350,371) | - | - |
| Accredited faculty services | 1 (1%) | 29 (4%) | 0.2 | $2,592 (NA) | $4,800 ($1,944, $9,500) | 0.5 | $2,208 (N/A) |
| Unaccredited faculty services | 2 (2%) | 73 (10%) | 0.01 | $8,298 ($6,249, $10,346) | $6,000 ($2,500, $11,935) | 0.7 | -$1,800 (N/A) |
| Education | 4 (4%) | 60 (8%) | 0.15 | $90 ($90, $112) | $62 ($61, $90) | 0.15 | -$28 (-$83 – -$28) |
| Food and beverage | 77 (71%) | 587 (80%) | 0.05 | $326 ($138, $634) | $399 ($146, $877) | 0.2 | $73 (-$22 – $150) |
| Travel and lodging | 31 (29%) | 259 (35%) | 0.2 | $912 ($549, $1,497) | $1,246 ($577, $3,060) | 0.07 | $334 (-$136 – $584) |
| Gifts | 0 (0%) | 2 (0.3%) | - | 0 | $149 ($115, $183) | - | - |
| Ownership/ investment | 0 (0%) | 8 (1%) | - | 0 | $34,209 ($22,167, $405,872) | - | - |
| Any payment/ total payment in 2018 | 80 (74%) | 606 (83%) | 0.047 | $535 ($228, $1,371) | $792 ($245, $4,749) | 0.012 | $242 ($81 – $466) |
The total amount of all payments was significantly (p=0.012) lower for women: Mean and median total payments for women were $1,370.14 and $535.00 respectively, versus $19,153.44 and $792.00 for men, respectively. Subgroup analysis of categories where >5 women had received payments revealed no significant between-gender differences, though men received greater payments in all the categories except education. In the remaining categories, there were large gender differences, but too few women to compute a p-value, as summarized in Table 2.
Overall, 686 (81%) of the 842 academic IR physicians received industry payments from 142 companies, amounting to a total of $14,206,599.41. Of this sum, $14,058,624.13 (99%) were received by men and $147,975.28 (1%) by women. There were 19 companies that made over $100,000 in total payments in 2018; all but one of these companies invested more than 90% of their payments in male IR physicians, and 12 of those companies made 99% or more of their payments to men (Table 3). There were 21 physicians who received more than $100,000 in 2018, and all were men. Altogether, they received $10,565,472.30, representing 74% of the payments. Among these top earners, median total payment in 2018 was $173,829.78 (range: $102,302.71—$5,542,340.20); median h index was 27 (range: none—82); median years since medical school graduation were 25 (range: 13—51); one (5%) had no academic rank, two (10%) were instructors, one (5%) was an assistant professor, 7 (33%) were associate professors, and 10 (48%) were professors. Of the 842 physicians, the top 80 payees were all men who received $19,000.00 or greater. Of the top 100 earners, three (3%) were women who in total received $49,279.29.
Table 3.
Top corporate payers in 2018. Companies that spent over $100,000.00 in 2018 are presented.
| Name | Total Payments | % to Men |
|---|---|---|
| Penumbra, Inc. | $5,779,360.63 | 99.8% |
| Cook* | $1,146,656.12 | 99.5% |
| BTG** | $1,006,236.50 | 99.2% |
| Boston Scientific Corporation | $763,170.65 | 97.5% |
| AngioDynamics, Inc. | $719,102.35 | 99.7% |
| Sirtex Medical Inc | $571,431.36 | 96.3% |
| Merck Sharp & Dohme Corporation | $508,446.65 | 100.0% |
| Medtronic*** | $421,106.01 | 94.2% |
| Terumo Medical Corporation | $291,102.95 | 98.0% |
| Bard**** | $259,540.02 | 99.3% |
| Siemens Medical Solutions USA, Inc. | $234,726.26 | 99.0% |
| Aspire Bariatrics, Inc. | $234,127.00 | 100.0% |
| Arrow International, Inc. | $213,003.99 | 100.0% |
| W. L. Gore & Associates, Inc. | $155,550.73 | 99.5% |
| Innovative Surgical Designs, Inc. | $127,778.20 | 100.0% |
| Abbott Laboratories | $116,682.73 | 98.6% |
| Philips Electronics North America Corporation | $114,781.92 | 97.4% |
| MicroVention, Inc. | $114,216.52 | 100.0% |
| Guerbet, LLC | $113,193.26 | 87.2% |
Cook includes Cook Incorporated and Cook Research Incorporated
BTG includes Biocompatibles, Inc, and BTG International, Canada
Medtronic includes Medtronic, UCA, Inc. and Medtronic Vascular, Inc.
Bard includes Bard Peripheral Vascular, Inc. and Bard Access Systems, Inc.
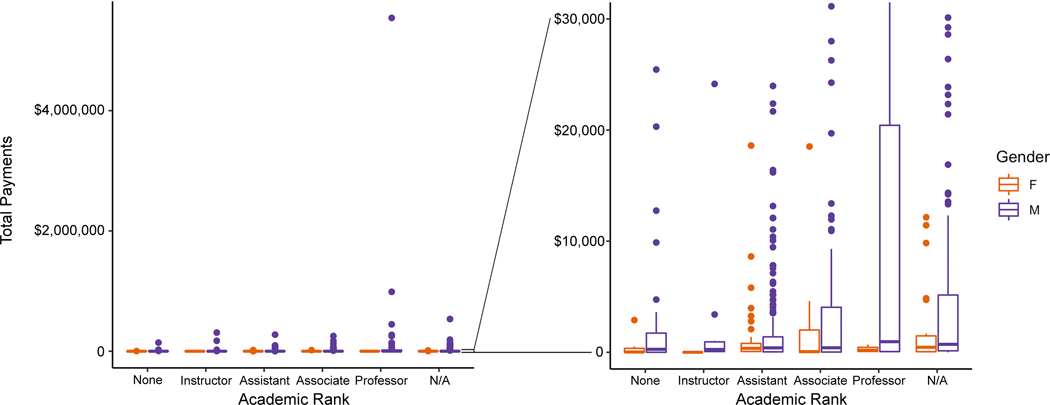
Even though h index (Fig 2A), years since graduation (Fig 2B), and academic rank (Fig 3) significantly influenced the amount of payments that IR physicians received in 2018, female gender was independently associated with lower payment (Table 4, p=0.016). Median total payments to men and women IR physicians have increased over the years for which payment data were available; a gender gap was present in every year’s payments (Fig 4).
Fig 2 —
Total payments in 2018 to IR physicians. Total payments in 2018 are presented for each IR physician by h index (A) and by years since medical school graduation (B). Note that one outlier ($5,542,340.20 received by one male IR physician) was excluded for illustrative purposes.
Fig 3 —
Total Payments in 2018 by academic rank. There are gender differences for the extreme values of industry payments (left) as well as in the quartiles/boxplots (right) for every academic rank. Middle bar denotes the median, boxes denote the 25th and 75th percentile, and whiskers denote the 5th—95th percentile.
Table 4.
General linear model. A multivariate analysis was performed to estimate the impact of gender, years since medical school graduation, h index and academic rank on industry payments in 2018. The model demonstrated that male gender, greater years since graduation, higher h index and higher academic rank are significantly associated with higher industry payments. Estimate: estimate of relationship of each variable on total payments; SE: standard error of the estimate; t stat: t statistic.
| Estimate | SE | t stat | p-value | |
|---|---|---|---|---|
|
| ||||
| Male gender | 2.72 | 0.41 | 2.42 | 0.016 |
| Years since graduation | 0.93 | 0.02 | −3.76 | <0.0001 |
| H index | 1.04 | 0.01 | 2.60 | 0.010 |
|
| ||||
| Academic rank | ||||
|
| ||||
| Instructor | 0.86 | 0.88 | −0.18 | 0.860 |
| Assistant | 1.94 | 0.49 | 1.34 | 0.182 |
| Associate | 3.17 | 0.57 | 2.04 | 0.042 |
| Professor | 7.37 | 0.68 | 2.94 | 0.003 |
Fig 4 —
Median total payments to men and women IR physicians over time (dashed line represents the interquartile range, i.e. 25th—75th quartile).
Discussion
Despite women constituting 13% of academic IR physicians in the U.S. in 2019, only 1% of industry payments in 2018 were received by female physicians. This gender gap may be more extreme compared to those of otolaryngology, ophthalmology, and radiation oncology, for which 12%, 9%, and 5% of payments were received by women who constitute 21%, 20%, and 26% of physicians, respectively [3–5]. Payments to men in IR were more frequent and larger in every reported category except education. Male IR physicians collected more payments at every academic rank, regardless of h index or years since medical school graduation. Payments made to support technological advancement, such as for research, royalties and licenses, were exclusively received by men.
While these data demonstrate a clear association of gender with industry payments, they do not determine a cause for the disparity. On the one hand, it is possible that female IR physicians would prefer to develop closer industry relationships but have fewer opportunities to do so, for at least three potential reasons. First, companies may target men rather than women IR physicians, preferentially making payments to men, believing male IR physicians to be optimal key opinion leaders (KOLs). Companies’ profit motives favor making payments, particularly larger sums, to physicians who are more likely to affect the practices of other physicians, with preference for established doctors with high academic impact and long experience [24]. Gender bias in medicine has long been recognized, with women physicians less likely to be referred to as doctors [25], and most people assuming doctors are male [26]. It is possible that gender bias impacts medical companies’ choices in selecting optimal KOLs who are felt to be most representative of an “IR doctor.”
Second, women may have less time to spend on developing industry relationships. Women physicians on average take on 8.5 additional hours per week of domestic responsibilities [27], potentially limiting their ability to perform additional work such as consulting and speaking for companies. Finally, women may lack access to collaborative relationships. Despite the finding that having a mentor in academic medicine doubles the probability for promotion [28], it is more difficult for women to find mentors than men [29]. The paucity of such professional relationships may reduce referrals for consulting and other types of work with industry leaders.
On the other hand, besides lack of access to industry relationship opportunities, it is possible that women IR physicians have less desire to participate in industry relationships. There are ethical issues with accepting industry payments, which can influence physicians’ prescribing and device utilization practices [30, 31]. Men may more place greater value on the benefits of industry relationships and/or minimize the potential costs in terms of conflicts of interest or commitment [32–34], whereas women may place greater value on protecting honesty in medicine and preserving unbiased judgment [35, 36] and therefore decline offers to collaborate with companies due to ethical concerns.
Regardless of the cause of the disparity, the underrepresentation of women in industry’s relationship with academic IR may negatively impact the distribution of resources for solving particular health problems and limit the overall progress of technological advancement. Medical device development is difficult and potentially impossible without the collaboration of industry [2]. The finding that not a single payment made for research, royalties and licenses, or ownership and investment were made to women demonstrates that, in IR, women are not participating in technological innovation that drives progress in the field. Diverse groups allow for multiple viewpoints that can help solve problems in novel ways [37], suggesting that the inclusion of women in industry-based research efforts would be beneficial to the field, in general. Women physicians may be more likely to focus on issues in women’s health; the absence of industry resources among women IR physician researchers may perpetuate the underrepresentation of women in clinical trials [38]. Gender diversity has been shown to positively impact business organizations, and is a recognized goal in the setting of academic radiology [10].
Beyond the losses to the field in general, gender inequality in industry payments indicates a loss of potential income and professional impact for individual women IR physicians. Women physicians in academic medicine earn significantly lower salaries compared with men after controlling for years since medical school graduation, academic rank, specialty, and indices of clinical and research productivity [39]. Worse, this disparity is increasing over time [40]. We found that women IR physicians had lower average years since medical school graduation and h indices compared to men at the same academic rank. This may reflect departmental policies aimed at promoting women within the field. Alternatively, other factors, not studied here, may drive promotion of women beyond years in practice or h index, such as women spending more time teaching [41] or providing direct patient contact through clinical encounters [9]. In regard to industry payments in IR, however, we found that gender disparity favoring men has not improved since 2014. Such a trend may undercut other gains made in terms of academic advancement and productivity. Given the negative impact on women’s opportunities in IR and on the field in general, the persistent and pronounced gender disparity in physician-industry relationships is a key issue warranting further investigation and correction.
Our study is limited, in several ways, by the nature of the available data. IR physicians were identified based on websites maintained by each academic program, which may be outdated. Data regarding the nature of each physician’s career track as being research vs clinical practice-predominant was not available. Payments made to private practice IR physicians were not assessed; the focus on academic IR physicians may contribute to the finding that no women IR doctors in our study received payments supporting technological advancement. Data regarding where each physician worked over the prior several years were not available. For this reason, payment data from the most recent years (2017 and 2018) were analyzed. Furthermore, CMS Open Payments may not capture all types of payments. The NPPES NPI Registry relies on self-reported data, which may be outdated or inaccurate. This database provides the medical school graduation year, but not the start date of the physician’s first appointment as an attending physician. Therefore, the exact numbers of years in practice as an attending physician was not available for analysis. Statistical analysis in this study was limited by the small number of women (108), and the very small number and size of payments made to them. The sparsity of payment data precluded some tests for significance; nevertheless, the differences are often readily apparent in tabular and/or graphical form. Finally, the study presents data showing that women receive fewer and lower payments, but does not determine causality. While industry payments can represent professional opportunities, they also entail ethical concerns regarding conflict of interest. Decreased time spent in cultivating industry relationships may reflect more time dedicated to academic and clinical productivity.
Conclusion
In summary, women IR physicians received significantly fewer industry payments, comprising smaller amounts of money, compared to their male colleagues. This disparity was present regardless of academic rank, h index, or years since medical school graduation, and did not appear to be improving with time. Not a single woman received a payment to support technological advancement in the field. Disproportionate industry payment in IR may be a manifestation and perpetuation of a male-dominated culture inhospitable to aspiring academic female physicians. This gender gap implies reduced access to supplemental income, and limited opportunities for collaborative research efforts which may impair career development.
Acknowledgments
We thank Dr. Mithat Gönen, PhD, Chief of the Biostatics Service at Memorial Sloan Kettering Cancer Center, for reviewing the statistical analysis used in this study.
This research was partly funded through the NIH/NCI Cancer Center Support Grant P30 CA008748, and a research grant from the Harvey L. Neiman Health Policy Institute. Dr. Deipolyi reports personal fees from BTG, Inc., personal fees from Dova Pharmaceuticals, outside the submitted work; Dr. Covey reports holding stock from Amgen, personal fees from Accurate Medical, outside the submitted work. All other authors have no disclosures.
No IRB approval was required for this study of publicly available data.
Contributor Information
Amy R. Deipolyi, Interventional Radiology Service, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY, USA 10065.
Anton S. Becker, Department of Radiology, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY, USA 10065.
Anne M. Covey, Interventional Radiology Service, Memorial Sloan Kettering Cancer Center, 1275 York Avenue, New York, NY, USA 10065.
Susan C. Chimonas, Center for Health Policy and Outcomes at Memorial Sloan Kettering, 485 Lexington Avenue, New York, NY, USA, 10017.
Andrew B. Rosenkrantz, Department of Radiology, NYU Langone Medical Center, 660 First Avenue, New York, NY, USA 10016.
Howard P. Forman, School of Management, Yale University, 333 Cedar Street, New Haven, CT, USA 06520.
William A. Copen, Department of Radiology, Massachusetts General Hospital, 55 Fruit Street, Boston, MA, USA 02114; Harvard Medical School, 25 Shattuck Street, Boston, MA, USA 02115.
References
- 1.Gelijns AC, Thier SO. Medical innovation and institutional interdependence: rethinking university-industry connections. JAMA 2002; 287:72–77 [DOI] [PubMed] [Google Scholar]
- 2.Lewin JS. Industrial-academic research relationships: departmental collaborations. Radiology 2009; 250:23–27 [DOI] [PubMed] [Google Scholar]
- 3.Reddy AK, Bounds GW, Bakri SJ, et al. Representation of women with industry ties in ophthalmology. JAMA Ophthalmol 2016; 134:636–643 [DOI] [PubMed] [Google Scholar]
- 4.Eloy JA, Bobian M, Svider PF, et al. Association of gender with financial relationships between industry and academic otolaryngologists. JAMA Otolaryngol Head Neck Surg 2017; 143:796–802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weng JK, Valle LF, Nam GE, Chu FI, Steinberg ML, Raldow AC. Evaluation of sex distribution of industry payments among radiation oncologists. JAMA Netw Open 2019; 2:e187377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgins MC, Hwang WT, Richard C, et al. Underrepresentation of women and minorities in the United States IR academic physician workforce. J Vasc Interv Radiol 2016; 27:1837–1844 e1832 [DOI] [PubMed] [Google Scholar]
- 7.Kapoor N, Blumenthal DM, Smith SE, Ip IK, Khorasani R. Sex differences in radiologist salary in U.S. public medical schools. AJR Am J Roentgenol 2017; 209:953–958 [DOI] [PubMed] [Google Scholar]
- 8.Xiao N, Oliveira DFM, Gupta R. Characterizing the impact of women in academic IR: a 12-year analysis. J Vasc Interv Radiol 2018; 29:1553–1557 [DOI] [PubMed] [Google Scholar]
- 9.Rosenkrantz AB, Englander MJ, Deipolyi AR, Findeiss L, Duszak R Jr. Clinical practice patterns of interventional radiologists by gender. American Journal of Roentgenology 2019; 213:1–8 [DOI] [PubMed] [Google Scholar]
- 10.Lightfoote JB, Fielding JR, Deville C, et al. Improving diversity, inclusion, and representation in radiology and radiation oncology part 1: why these matter. J Am Coll Radiol 2014; 11:673–680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deipolyi AR, Covey AM, Brody LA, Bryce YCD, Li D, Brown KT. Women’s challenges in IR: #ILookLikeAnIR. J Vasc Interv Radiol 2017; 28:1195–1196 [DOI] [PubMed] [Google Scholar]
- 12.Perez YV, Kesselman A, Abbey-Mensah G, Walsh J. A glance at gender-specific preferences influencing interventional radiology selection. J Vasc Interv Radiol 2016; 27:142–143 [DOI] [PubMed] [Google Scholar]
- 13.Accreditation Council for Graduate Medical Education (ACGME) - Public. https://apps.acgme.org/ads/Public/Programs/Search. Accessed January 1, 2019
- 14.Feng H, Wu P, Leger M. Exploring the industry-dermatologist financial relationship: insight from the open payment data. JAMA Dermatol 2016; 152:1307–1313 [DOI] [PubMed] [Google Scholar]
- 15.NPPES NPI Registry. https://npiregistry.cms.hhs.gov/. Accessed January 1, 2019
- 16.Physician Compare Database https://www.medicare.gov/physiciancompare/. Accessed January 1, 2019
- 17.Centers for Medicare and Medicaid Services. https://www.cms.gov/openpayments/. Accessed January 1, 2019
- 18.Agrawal S, Brennan N, Budetti P. The Sunshine Act--effects on physicians. N Engl J Med 2013; 368:2054–2057 [DOI] [PubMed] [Google Scholar]
- 19.Natures of Payment. https://www.cms.gov/openpayments/about/natures-of-payment.html. Accessed January 1, 2019
- 20.Nguyen TD, Bradford WD, Simon KI. Pharmaceutical payments to physicians may increase prescribing for opioids. Addiction 2019; 114:1051–1059 [DOI] [PubMed] [Google Scholar]
- 21.Hirsch JE. An index to quantify an individual’s scientific research output. Proc Natl Acad Sci U S A 2005; 102:16569–16572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scopus. https://www.scopus.com/freelookup/form/author.uri. Accessed January 1, 2019
- 23.Team R. RStudio: Integrated Development for R. RStudio, Inc. 2016; http://www.rstudio.com/ [Google Scholar]
- 24.Sismondo S. Key opinion leaders and the corruption of medical knowledge: what the Sunshine Act will and won’t cast light on. J Law Med Ethics 2013; 41:635–643 [DOI] [PubMed] [Google Scholar]
- 25.Devon KM. Call me by my name: doctor. Ann Surg 2019; 270:29–30 [DOI] [PubMed] [Google Scholar]
- 26.Barlow R. BU Research: A Riddle Reveals Depth of Gender Bias. http://www.bu.edu/today/2014/bu-research-riddle-reveals-the-depth-of-gender-bias/ Accessed January 1, 2019
- 27.Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Annals of internal medicine 2014; 160:344–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beasley BW, Simon SD, Wright SM. A time to be promoted: the prospective study of promotion in academia (prospective study of promotion in academia). Journal of general internal medicine 2006; 21:123–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wietsma AC. Barriers to success for female physicians in academic medicine. Journal of community hospital internal medicine perspectives 2014; 4:24665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeAngelis CD, Fontanarosa PB. Impugning the integrity of medical science: the adverse effects of industry influence. JAMA 2008; 299:1833–1835 [DOI] [PubMed] [Google Scholar]
- 31.Fugh-Berman A, Ahari S. Following the script: how drug reps make friends and influence doctors. PLoS Med 2007; 4:e150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kennedy JA, Kray LJ. Who is willing to sacrifice ethical values for money and social status? Gender differences in reactions to ethical compromises. Social Psychological and Personality Science 2014; 5:52–59 [Google Scholar]
- 33.Kray LJ, Haselhuhn MP. Male pragmatism in ethical decision making. In: UC Berkeley Working Paper Series 2011; https://escholarship.org/uc/item/05n3d6pj [Google Scholar]
- 34.Kray LJ, Haselhuhn MP. Male pragmatism in negotiators’ ethical reasoning. Journal of Experimental Social Psychology 2012; 48:1124–1131 [Google Scholar]
- 35.Fineberg HV. Conflict of interest: why does it matter? Jama 2017; 317:1717–1718 [DOI] [PubMed] [Google Scholar]
- 36.Muehlheusser G, Roider A, Wallmeier N. Gender differences in honesty: groups versus individuals. Economics Letters 2015; 128:25–29 [Google Scholar]
- 37.Page SE. The Difference: How the Power of Diversity Creates Better Groups, Firms, Schools, and Societies-New Edition: Princeton University Press, 2008 [Google Scholar]
- 38.Clancy CM, Massion CT. American women’s health care: a patchwork quilt with gaps. Jama 1992; 268:1918–1920 [PubMed] [Google Scholar]
- 39.Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA internal medicine 2016; 176:1294–1304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Esteves-Sorenson C, Snyder J. The gender earnings gap for physicians and its increase over time. Economics Letters 2012; 116:37–41 [Google Scholar]
- 41.Borges NJ, Navarro MAM, Grover AC. Women physicians: choosing a career in academic medicine. Academic medicine: journal of the Association of American Medical Colleges 2012; 87:105. [DOI] [PMC free article] [PubMed] [Google Scholar]