Abstract
Objectives
To investigate the association between occupational lifting and the risk of rhegmatogenous retinal detachment (RRD) using data from a large population of men.
Methods
We used data from a national cohort of 49 321 Swedish men conscripted for compulsory military service in 1969–1970. We collected information on surgically treated RRD from the National Patient Register and we followed up the cohort between 1991 and 2009 at ages 40–60 years. Exposure to occupational lifting was assessed by applying a job exposure matrix to occupational data from the 1990 census. Incidence rate ratios (IRRs) and 95% CIs were estimated through Poisson regression models adjusted by degree of myopia, income and education level.
Results
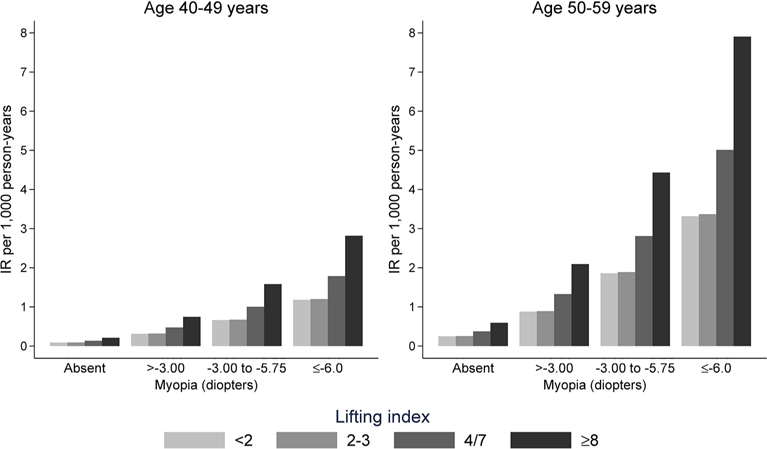
We observed 217 cases of RRD in 7 80 166 person-years. In univariate analyses we did not observe an association between occupational lifting and RRD. However, after adjustment for myopia and socioeconomic factors, we found an increased risk of RRD (IRR 2.38, 95% CI 1.15 to 4.93) for subjects in the highest category of exposure compared with those in the lowest one. The incidence rate of RRD among subjects lifting heavy loads at least twice per week, aged between 50 years and 59 years, and affected by severe myopia was as high as 7.9 cases per 1000 person-years, compared with an overall rate of 0.28.
Conclusions
Our study supports the hypothesis that heavy occupational lifting is a risk factor for RRD. Information on myopia degree and socioeconomic status is necessary when studying the association between occupational lifting and RRD.
INTRODUCTION
Rhegmatogenous retinal detachment (RRD), a potentially blinding pathology, occurs when the neurosensory retina separates from the underlying retinal pigmented epithelium due to a full thickness retinal break that allows the accumulation of liquefied vitreous in the subretinal space.1
Age, male gender, myopia, ocular surgery and blunt traumas of the eye and the head are well known determinants of RRD.2 Recent epidemiological literature has suggested several additional risk factors, although the evidence is not conclusive. These include recent oral fluoroquinolones use,3 and hypertension and obesity.4
The current line of research was triggered by the finding by Mattioli and colleagues that occupational lifting might be a risk factor for surgically treated RRD, possibly due to intraocular pressure spikes during the Valsalva manoeuvre.5–7 Their case-control study found that intense occupational lifting was more common among patients who had received surgery for RRD than a reference group of outpatients referred to an ophthalmological clinic. The same group of authors indirectly confirmed the association between lifting and RRD through a population study of hospital discharge records, which documented higher rates of RRD among Tuscan manual workers compared with non-manual workers.8 However, a recent population-based register study of Danish workers did not show any evidence of an association between RRD and being employed in jobs expected to entail a high frequency of heavy lifting.9 Based on their findings, these authors questioned the positive findings from earlier studies from Mattioli and colleagues. Nevertheless, the Danish study presents two important methodological limitations. First, the exposure assessment relied entirely on expert opinion of the likely degree of heavy lifting in occupations, allowing only crude comparisons between occupations where frequent heavy lifting was considered highly likely and other manual and non-manual works. Second, the register did not include information on myopia (near-sightedness), the most important risk factor for RRD at the population level, which may introduce negative confounding into the studied association—as near-sightedness may be more frequent among people with a higher level of education and belonging to upper socioeconomic classes.10–12
We conducted an analysis of data from a very large national cohort of Swedish conscripts with information on myopia and socioeconomic status gathered at age 18 years. Our primary aim was to assess the association between occupational lifting and RRD. As a secondary aim, we evaluated whether myopia and socioeconomic risk factors are relevant confounders of the studied association.
METHODS
Study design and population
A detailed description of the cohort has been reported else-where.13 14 Briefly, we analysed data from a nationwide cohort of 499231 Swedish men born in 1949–1951 and conscripted for military service in 1969–1970. By law at that time, all men were required to undergo 2 days of examinations which included a thorough eye examination.
Using unique identification numbers, the conscripts’ cohort was linked to data from the National Population and Housing Census (1985 and 1990 editions), the 1990 edition of the Longitudinal Database of Education, Income and Employment (LOUISE), the National Patient Register (data available from 1973), the Cause of Death Register and the Register of the Total Population. As information on occupation used in the main analysis was collected in the 1990 census, the follow-up time of each subject started on 1 January 1991 and ended at first incident RRD, date of death or first emigration, or the end of the study (31 December 2009, the last available cohort update). The timeline of the study is summarised in online supplementary table 1.
We classified as incident cases those subjects who had received a primary surgical procedure for an RRD. Case identification was based on the International Classification of Diseases used in the studied period: between 1973 and 1986, code 376.00 (ICD-8); 1987–1996, 361.0* (ICD-9); and from 1997 through 2009, H33.0* (ICD-10).
Exposure assessment and covariates
Data on occupations from the 1985 and 1990 National Population and Housing Census were classified according to the 1983 version of the Nordic Classification of Occupation (Nordisk Yrkesklassificering, NYK-83). Based on the job codes, we attributed a level of exposure to occupational lifting through a job exposure matrix (JEM). This classification was based on a three-digit system which codes 320 different job titles. The JEM was constructed using information from the Swedish Work Environment Surveys 1989–97, including data on almost 49 000 men and women. These surveys included information on occupational title for each participant and specific questions on occupational lifting: how often do you lift or carry weights of 25 kg or more (195 and 1997 editions); how often do you lift or carry weights of 20 kg or more (1989, 1991, and 1993 editions). The participants were asked to answer these questions based on the following scale: (A) every day; (B) a couple of days per week; (C) 1 day per week; (D) a couple of days per month; (E) not at all/rarely. Assuming five working days per week and 4 weeks per month, we scored the answers according to the monthly frequency as follows: A=20; B=8; C=4; D=2; E=0.25. We then calculated a Lifting Index by occupational title as the geometrical mean (the exponential of the average of the log-transformed values) of the scored answers. Finally, we categorised this Lifting Index based on a priori cut-offs:<2 (occupations where heavy lifting occurs less than twice per month); 2–3 (at least twice per month but less than once per week); 4–7 (at least once per week but less than twice per week); ≥8 (at least twice per week). Because the JEM was constructed using data collected between 1989 and 1997, we considered our exposure variable directly applicable to the data on occupation collected during the 1990 census. Hence, in the main analysis (follow-up starting on 1 January 1991 and ending on 31 December 2009), we assigned the exposure value to each member of our cohort based on the occupational title reported in the 1990 census.
We identified a priori myopia and socioeconomic factors as potential confounders of the association between occupational lifting and RRD risk.2 15 The putative roles of education level and income as confounders of the association between RRD and occupational lifting are presented graphically in online supplementary figue 2. While part of their influence on RRD risk is probably mediated by myopia,10–12 socioeconomic factors could also have direct effects on the observed incidence of surgically treated RRD. This hypothesis is based on the observation that an important gradient in the severity of surgically treated RRD was observed among quintiles of deprivation in Scotland.15 Hence, high socioeconomic status might be associated with the probability of receiving a surgical treatment and/or might affect the timing of the surgery—and this could translate into a spurious change in the relative risk when performing a survival analysis. Grades of myopia were defined as follows: absent (including hypermetropic and emmetropic); mild myopia (greater than −3.0 dioptres); moderate myopia (−3.0 to −6.0 dioptres); severe myopia (less than −6.0 dioptres) (see online supplementary table 1). We included in all multivariable models myopia degree, education level and individual income. Also, based on evidence from our previous analysis of RRD in this cohort, we evaluated as potential confounders IQ and cardiovascular risk factors (namely, body mass index, blood pressure levels and cigarette smoking).4 16
Age was not considered a potential relevant confounder of the studied association because of the study design (age-matched cohort); the inclusion of age as a time-dependent covariate in the regression models did not change materially the estimates of interest. However, we calculated age-specific incidence rates (IRs) of RRD, because this condition is strongly age-related.2
To increase the comparability of our findings with previous studies that presented estimates stratified by broad occupational categories,8 9 we calculated separately the IR for manual and non-manual workers (identified based on the socioeconomic classification made by Statistics Sweden and the NYK-83 occupational codes).
Information on potential confounders of the association between occupational lifting and the risk of RRD was derived from the conscription examination (refractive error, body mass index, cigarette smoking, blood pressure levels and IQ), LOUISE (educational level and income) and the 1990 census (occupational group). See online supplementary table 1 for further details on all covariates.
Statistical analysis
In the analyses of descriptive statistics (table 1), we presented categorical variables as numbers and percentages and continuous variables as medians and IQRs. The linear trend of Lifting Index across myopia degree categories was analysed with the Cuzick non-parametrical test.
Table 1.
Baseline characteristics of the study population by Lifting Index category. Swedish men born in 1949–1951 and conscripted for compulsory military service in 1969–1970
| Lifting Index |
||||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | <2 (n=30 461, 72.4%) |
2/3 (n=6055, 14.4%) |
4/7 (n=4575, 10.9%) |
≥8 (n=972, 2.3%) |
||||
|
| ||||||||
| Myopia degree, (dioptres) | ||||||||
| Absent (≥0), n (%) | 25,788 | (84.7) | 5,556 | (91.8) | 4,211 | (92.0) | 906 | (93.2) |
| Mild (−2.75,−0.25), n (%) | 2,958 | (9.7) | 314 | (5.2) | 245 | (5.4) | 47 | (4.8) |
| Moderate (−5.75,−3.00), n (%) | 1,457 | (4.8) | 152 | (2.5) | 105 | (2.3) | 19 | (2.0) |
| Severe (≤−6.00), n (%) | 258 | (0.8) | 33 | (0.5) | 14 | (0.3) | 0 | (0.0) |
| Education level (years) | ||||||||
| Primary (≤9), n (%) | 5,491 | (18.0) | 2,884 | (47.6) | 1,995 | (42.7) | 398 | (40.9) |
| Secondary (11–12), n (%) | 13,440 | (44.1) | 2,940 | (48.6) | 2,418 | (52.9) | 542 | (55.8) |
| University (≥14), n (%) | 11,530 | (37.9) | 231 | (3.8) | 202 | (4.4) | 32 | (3.3) |
| Income (SEK/week), median (IQR) | 1956 | (1589–2475) | 1578 | (1370–1822) | 1562 | (1210–1846) | 1785 | (1544–1999) |
SEK, Swedish krona.
The IR ratios (IRRs) of RRD and 95% CIs were estimated by fitting multivariable Poisson regression models including case status as the dependent variable and the logarithm of the person-years at risk as the offset. Because the exposure variable (ie, Lifting Index) was measured at the occupational group level, we assumed a random intercept (gamma distributed) to account for within-occupation dependence.17 Linear trend across Lifting Index categories was evaluated using the Wald test, treating the variable in the model with one degree of freedom. In line with our study aims, the estimates were adjusted by myopia degree. We further fitted regression models including education and income. Finally, we explored the role of other potential covariates (ie, IQ, body mass index, blood pressure levels and cigarette smoking) in the absence of a priori hypothesis on their role in the studied causal pathway. We applied a change-in-estimates strategy to assess whether these factors should be considered in our multivariable models or not,18 but none of them reached the a priori threshold for inclusion (10% change in the IRR for the Lifting Index); hence they were not included in the final analysis. To explore a possible non-linearity of the association between income and RRD, we fitted a univariate cubic spline regression model; as we did not observed any evidence suggesting non-linearity, income was included in the multivariable models as a continuous predictor.19 The IR of RRD was computed as the average marginal effect after fitting the Poisson regression model.
Statistical analyses were performed using Stata V.14.1 SE (Stata Corp, College Station, Texas, USA). We defined as statistically significant a two-sided p value <0.05.
RESULTS
Our cohort included 49 321 Swedish men conscripted during 1959–1960 at the age of 18–20 years. We excluded 1095 subjects who exited the cohort before the start of the follow-up (1 January 1991, figure 1). Also, 6146 subjects were excluded since no occupation was reported in the 1990 census. This is in agreement with official statistics reporting a labour market participation in this age group of less than 90% and a participation rate in 1990 census that was above 98%. Finally, 17 individuals were excluded because of missing information on level of education. Thus, our final study population included 42 063 subjects followed up between 1 January 1991 and 30 December 2009. During this period, 1835 (4.4%) subjects died and 274 (0.6%) were lost to follow-up due to emigration. The median follow-up was 19 years (IQR 19–19 years; 94.5% of the cohort was still under follow-up at the end of the study). We observed 217 cases of RRD in 780 166 person-years (IR 0.28 per 1000 person-years, 95% CI 0.24 to 0.32).
Figure 1.
Flow diagram of the study population. Swedish men born in 1949–1951 and conscripted for compulsory military service in 1969–1970. Followup period 1991–2009. RRD, rhegmatogenous retinal detachment.
As hypothesised, subjects holding job titles where frequent heavy lifting is uncommon tended to have a higher level of education and a higher personal income (table 1). Myopia was much more frequent (15.3%) among workers in the lowest Lifting Index category compared with subjects in the highest category (6.8%). This relationship appears to be monotonic; the greater the myopia, the less lifting in the job (see online supplementary figure 3).
As a preliminary descriptive analysis, and for comparison with the previous Danish Cohort Study,8 we calculated the IRs of RRD by broad occupational class (manual and non-manual workers) (table 2). In crude analyses, manual workers (who presumably perform more heavy lifting) had lower rates of RRD than non-manual workers which contradicts our hypothesis but is consistent with the Danish study. Once the model was adjusted for myopia, the difference in risk between these two broad groups disappeared and both had nearly identical IRs. The JEM allowed us to move beyond these simple categories and analyse the risk across levels of frequent heavy lifting.
Table 2.
IRs (per 1 00 000 person-years) of rhegmatogenous retinal detachment by broad occupational group. Average marginal effects from Poisson regression models. Swedish men born in 1949–1951 and conscripted for compulsory military service in 1969–1970
| Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Occupational group | Cases | Pyrs | IR | (95% CI) | IR | (95% CI) |
|
| ||||||
| Non-manual workers | 128 | 404,389 | 31.7 | (26.6–37.6) | 28.3 | (22.3–33.3) |
| Manual workers | 89 | 375,776 | 23.7 | (19.2–29.2) | 27.4 | (21.6–33.1) |
IR, incidence rate; Pyrs, person-years.
IRs adjusted by degree of myopia.
In univariate analyses, there was no clear sign of an association between the Lifting Index and the risk or RRD (IRR for those in the highest category: 1.54, 95% CI 0.74 to 3.20, p trend=0.78) (table 3). However, the progressive adjustment by myopia degree and socioeconomic factors (ie, education and income) led to a remarkable increase in the observed IRR (table 3). The fully adjusted IRR for subjects in the highest category of exposure was 2.38 (95% CI: 1.15 to 4.93) and a clear positive trend was observed across Lifting Index categories (p trend=0.014)—although there were only eight cases in the highest category (Lifting Index ≥8) (table 3). A graphical representation of these findings (figure 2) shows the strong relationships of RRD absolute risk with age, myopia and heavy lifting. Among myopic subjects in their 50s with Lifting Index ≥8, the IRs were: 2.1 (mild myopia), 4.4 (moderate myopia) and 7.9 (severe myopia) per 1000 person-years. Online supplementary table 2 summarises these differences in tabular form.
Table 3.
IRRs of rhegmatogenous retinal detachment. Estimates from Poisson regression models with random intercept on occupational groups (NYK-83, three-digit level). Swedish men born in 1949–1951 and conscripted for compulsory military service in 1969–1970
| Crude estimates | Estimates adjusted by myopia degree* | Estimates adjusted by myopia degree and socioeconomic factors† | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Lifting Index | Cases | IRR | (95% CI) | p trend | IRR | (95% CI) | p trend | IRR | (95% CI) | p trend |
|
| ||||||||||
| <2 | 161 | 1.00 | (Ref.) | 1.00 | (Ref.) | 1.00 | (Ref.) | |||
| 2/3 | 23 | 0.73 | (0.47–1.13) | 0.89 | (0.57–1.38) | 1.01 | (0.64–1.61) | |||
| 4/7 | 25 | 1.04 | (0.67–1.59) | 1.31 | (0.86–2.01) | 1.51 | (0.97–2.37) | |||
| ≥8 | 8 | 1.54 | (0.74–3.20) | 0.776 | 2.09 | (1.02–4.27) | 0.082 | 2.38 | (1.15–4.93) | 0.014 |
IRR, incidence rate ratio; Ref., reference category.
Estimates adjusted by myopia degree.
Estimates adjusted by myopia degree, education level and income.
Figure 2.
IR of rhegmatogenous retinal detachment. Average marginal effect from the fixed part of a Poisson regression model including Lifting Index, myopia degree, education level, income and age (40–49 years vs 50–59 years), and with random intercept on occupational groups (NYK-83, three-digit level). IR, incidence rate.
DISCUSSION
We observed an association between occupational lifting and RRD risk in late middle age in a cohort of Swedish men born between 1949 and 1951; workers performing heavy occupational lifting at least twice per week showed a twofold increase in risk compared with unexposed ones. Our estimates demonstrated that myopia and socioeconomic factors were important confounders of the studied association and crude estimates obtained in this population were substantially biased.
Although the association between lifting and RRD was hypothesised several decades ago,20 the first study specifically designed to investigate this association was conducted by Mattioli and colleagues in 2000.5–7 The authors observed evidence of an increased risk of RRD among subjects with a long history of heavy occupational lifting. Yet this study did not provide definitive evidence due to the limited sample size (61 cases and 98 controls) and the potential for selection bias (the controls were sampled among outpatients of a public eye clinic). To our knowledge, the Danish population-based register study was the second attempt to explicitly investigate the role of occupational lifting in RRD development.9 A trained ergonomist identified job titles characterised by a high probability of frequent occupational lifting and the IR observed in this group was compared with the rate for occupations where occupational lifting is unlikely to occur. No sign of association was observed and the authors concluded that ‘[…] despite its methodological limitations, it seems unlikely that a major hazard would have been missed’.9 Nevertheless, we showed that myopia and socioeconomic factors, which were not accounted for in the Danish study, are important negative confounders of the association between RRD and occupational lifting. Thus, our findings call into question the validity of the estimates from the Danish study. Furthermore, the Danish Study employed a crude classification of exposure. When we linked the population survey to data from a study of biomechanical risk factors, and specifically the frequency of lifting, we improved the accuracy of the study.
The finding of an association of RRD with socioeconomic status has been previously reported. For example, major differences in the incidence of primary RRD were observed across quintiles of an Ecological Deprivation Index based on postal codes in a Scottish study15; the higher rates were estimated for wealthier areas—a setting where we do not expect to find a high prevalence of subjects performing physically strenuous jobs. However, the Scottish Study analysed ecological data, did not include individual information on occupation (the only available data was the percentage of unemployed in the area) and crucially did not have information on myopia. An Italian register-based study of surgically treated RRD showed higher age SIRs among manual workers compared with non-manual workers.8 The authors hypothesised that occupational lifting might have contributed to explain the observed difference. This interpretation is in line with our findings, but the Italian study also lacked information on myopia and socioeconomic factors, and so we might expect this result also to be confounded by myopia.
In line with our observation, several investigations have found that the prevalence of myopia, and also of severe myopia, increases with education level and is more common in the upper socioeconomic classes11 12 20–23; and we are aware of only one study, the EPIC-Norfolk Eye Study, in which a substantial difference in refractive error between manual and non-manual workers was not observed.24 On balance, based on our findings and on prior evidence on the distribution of RRD risk factors, we believe that individual information on myopia and socioeconomic factors is needed to obtain reliable estimates when studying occupational determinants of RRD.
The overall IR of RRD in our study population was 0.28 per 1000 person-years. However, when we considered jointly the effect of age, myopia and lifting (figure 2), we observed that the rate in high-risk subjects (those in the highest Lifting Index category, affected by severe myopia and aged in their 50s) was as high as 7.9 per 1000 person years. The rates decreased to 3.3 cases per 1000 person-years (a decrease of 4.6 cases per 1000 person-years) when we considered 50–60-year-old severe myopic subjects in the lowest Lifting Index category (figure 2 and see online supplementary table 2). These figures shed new light on the need for preventive actions. Indeed, as intense manual material handling is still a common exposure, (eg25)) the prevalence of myopia is growing worldwide,26 and the workforce is ageing in many Western countries,27 the burden of occupation-related retinal detachment might increase in the future—if the hypothesised association with occupational lifting is determined to be causal.
The pathophysiological mechanism that might link lifting to RRD is unknown. It was previously hypothesised that this association may be mediated by temporary changes of the intraocular pressure,28 as a sudden rise in intraocular pressure has been reported during the Valsalva manoeuvre or during isometric exercise.29–32 However, several pathways could be involved, because three different precursors must occur together in order to have a RRD: liquefied vitreous, tractional forces that can produce and maintain a retinal break, and a break through which fluid gains access to the subretinal space.1 Repeated changes in intraocular pressure might alter the physical characteristics of the vitreous gel (accelerating the vitreous liquefaction), cause a dissection of the vitreous cortex from the internal limiting membrane or even cause direct damage to the retina. At present, knowledge of the exposure-response relationship from epidemiological studies is too crude to provide support to a specific biological model. Our study suggests that lifting heavy loads more than twice per week may increase risk of RRD more than twofold. Due to the limited available information, we could not investigate more frequent exposures; it is possible that a more substantial risk could be observed for subjects lifting heavy loads several times per day. Also, we could apply only a cut-off of 20/25 kg to define heavy lifting; hence, we could not provide information for lifting loads below this value and we could not assess whether the risk is proportional to the lifted weight or not. Additionally, we were not able to investigate exposure windows which might shed light on possible mechanisms.
Study Strengths and limitations
We present the first longitudinal analysis on occupational lifting and RRD which accounted for confounding by myopia and socioeconomic factors. Also, we used a quantitative metric of exposure by applying a JEM derived from previous population surveys with questions on occupational heavy lifting. Thus, our study represents a fundamental step forward compared with previous register-based studies characterised by a crude exposure assessment and the lack of information on potential confounders.8 9 Other strengths of our study are the national representativeness, the long follow-up period (40 years), the low attrition rate (0.6%) and the adoption of standardised procedures for the collection of baseline information.
The main limitation of our study is the absence of detailed individual data on exposure to occupational lifting; we relied on the application of a JEM to the occupational title held at the age of 40 years. In this situation, a non-differential misclassification of the exposure is likely. Also, we could only roughly quantify the frequency of lifting heavy loads, while we had no information on the duration and the intensity of the exposure. On balance, the relatively crude exposure assessment and the potential for misclassification might have biased our estimates, probably towards the null. Also, the lack of detailed information on the exposure did not allowed us to explore the injury mechanism; hence, we could not assess if the disease process is reversible or irreversible and if the damage is proportional to the dose or if it follows a step (discrete) function.33 Finally, the available information is too crude to propose industrial hygiene standards for prevention purposes. Another possible limitation is the lack of information on refractive error after the age of 18 years. Myopia may progress among young adults and its natural history might be influenced by performing close work and working with computers.34–36 Hence, residual confounding by myopia degree might still affect our estimates if myopia at age 18 years may underestimate the prevalence of severe myopia among non-manual workers later in life. Moreover, the causal pathway between myopia and RRD is a complex process possibly mediated by the presence of intermediate conditions, such as ocular staphyloma and macular retinoschisis.20 Hence, knowledge of myopia degree solely without information on associated conditions might not capture all the risk of RRD determined by myopia. This sort of bias should be non-differential with respect to occupational lifting and is likely to have attenuated our risk estimates. Although we had information on some potential confounders, we had no data on other possible causal factors of RRD such as eye surgery and head traumas.2 The most common surgical procedure associated with RRD is cataract surgery.1 We expect that only a minimal proportion of RRD was related to cataract surgery in our relatively young population (aged up to 60 years) and the bias due to the absence of information on this factor should be negligible. Head injuries might be a confounder of the association between occupational lifting and RRD because they could be more common among manual workers. We had access to hospital discharge records for head injuries (ICD10 S00–S09) for the period between 1997 and 2009; in this time window, only two cases (both having a Lifting Index between 2 and 4) were hospitalised for a head injury before receiving a surgical procedure for RRD (data not shown). Thus, we can exclude recent major head injuries for most cases (only 31 out of 217 RRD cases were treated before 1997); however, we cannot rule out the hypothesis that less severe—not requiring hospitalisation—occupational head injuries might be unmeasured confounders in our analysis, probably determining a minor bias away from the null hypothesis. We also could not adjust for non-occupational lifting, which may be important during leisure time activities and housework; this may introduce misclassification of the exposure status in our study population, but we expect that this is likely to have been non-differential. In our cohort, data on race were not available and major differences in the epidemiology of RRD by race are well known (white Caucasians present rates higher than Asians and blacks).2 However, we analysed a cohort of men born in 1949–1951 and conscripted in 1969–1971; at that time immigration from non-European countries was not common in Sweden and the vast majority of our cohort were white Caucasian. An obvious limitation of the present study is that it does not provide information on RRD among women.
Conclusions
Our findings support the hypothesis that occupational lifting is a risk factor for RRD and the absolute risk of RRD among high-risk subjects—those performing frequent occupational lifting, affected by severe myopia and aged in their 50s—is considerable. We demonstrated that controlling for myopia is very important when studying occupational risk factors of RRD. Further studies aimed at describing the injury mechanism and establishing preventive standards should be considered a research priority.
Supplementary Material
What this paper adds.
A previous Italian case-control study suggested that performing intense occupational lifting might increase the risk of rhegmatogenous retinal detachment (RRD), while a population-based register study of Danish workers failed to find a positive association.
Our analysis of a cohort of men conscripted for compulsory military service in Sweden shows that performing intense occupational lifting might increase the risk of RRD.
Myopia, which is more prevalent among non-manual workers, is an important confounder of the association between occupational lifting and RRD; estimates from former studies which did not account for myopia might be substantially biased towards the null hypothesis.
When studying occupational risk factors of RRD, it is important to control for myopia.
Acknowledgements
The authors thank Magnus Alderling for giving access to the original data used for the job exposure matrix.
Funding This work was supported in part by grant [R01OH 010539] from the U.S. National Institute for Occupational Safety and Health.
Footnotes
Competing interests None declared.
Ethics approval Stockholm’s Regional Ethical Review Board at Karolinska Institutet (reference number 2004/5:9-639/5).
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Ghazi NG, Green WR. Pathology and pathogenesis of retinal detachment. Eye 2002;16:411–21. [DOI] [PubMed] [Google Scholar]
- 2.Mitry D, Charteris DG, Fleck BW, et al. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol 2010;94:678–84. [DOI] [PubMed] [Google Scholar]
- 3.Alves C, Penedones A, Mendes D, et al. A systematic review and meta-analysis of the association between systemic fluoroquinolones and retinal detachment. Acta Ophthalmol 2016;94:e251–e259. [DOI] [PubMed] [Google Scholar]
- 4.Farioli A, Hemmingsson T, Kriebel D. Vascular risk factors and rhegmatogenous retinal detachment: a follow-up of a national cohort of swedish men. Br J Ophthalmol 2015:907–13 (Published Online First: 15 October 2015). [DOI] [PubMed] [Google Scholar]
- 5.Mattioli S, De Fazio R, Buiatti E, et al. Physical exertion (lifting) and retinal detachment among people with myopia. Epidemiology 2008;19:868–71. [DOI] [PubMed] [Google Scholar]
- 6.Mattioli S, Curti S, De Fazio R, et al. Risk factors for retinal detachment. Epidemiology 2009;20:465–6. [DOI] [PubMed] [Google Scholar]
- 7.Mattioli S, Curti S, De Fazio R, et al. Occupational lifting tasks and retinal detachment in non-myopics and myopics: extended analysis of a case-control study. Saf Health Work 2012;3:52–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curti S, Coggon D, Baldasseroni A, et al. Incidence rates of surgically treated rhegmatogenous retinal detachment among manual workers, non-manual workers and housewives in Tuscany, Italy. Int Arch Occup Environ Health 2014;87:539–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curti S, Coggon D, Hannerz H, et al. Heavy lifting at work and risk of retinal detachment: a population-based register study in Denmark. Occup Environ Med 2016;73:51–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Eye Disease Case-Control Study Group. Risk factors for idiopathic rhegmatogenous retinal detachment. Am J Epidemiol 1993;137:749–57. [PubMed] [Google Scholar]
- 11.Foster PJ, Jiang Y. Epidemiology of myopia. Eye 2014;28:202–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teasdale TW, Fuchs J, Goldschmidt E. Degree of myopia in relation to intelligence and educational level. Lancet 1988;2:1351–4. [DOI] [PubMed] [Google Scholar]
- 13.Andreasson S, Allebeck P, Romelsjo A. Alcohol and mortality among young men: longitudinal study of swedish conscripts. Bmj 1988;296:1021–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larsson D, Hemmingsson T, Allebeck P, et al. Self-rated health and mortality among young men: what is the relation and how may it be explained? Scand J Public Health 2002;30:259–66. [DOI] [PubMed] [Google Scholar]
- 15.Mitry D, Charteris DG, Yorston D, et al. ; Scottish RD Study Group. The epidemiology and socioeconomic associations of retinal detachment in Scotland: a two-year prospective population-based study. Invest Ophthalmol Vis Sci 2010;51:4963–8. [DOI] [PubMed] [Google Scholar]
- 16.Sörberg A, Allebeck P, Hemmingsson T. IQ and somatic health in late adolescence. Intelligence 2014;44:155–62. [Google Scholar]
- 17.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using stata. College Station, TX: Stata Press, 2008. [Google Scholar]
- 18.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol 1993;138:923–36. [DOI] [PubMed] [Google Scholar]
- 19.Royston P, Sauerbrei W. Multivariable modeling with cubic regression splines: a principled approach. Stata J 2007;7:45. [Google Scholar]
- 20.Morgan IG, Ohno-Matsui K, Myopia SSM Lancet 2012;379:1739–48. [DOI] [PubMed] [Google Scholar]
- 21.Bar Dayan Y, Levin A, Morad Y, et al. The changing prevalence of myopia in young adults: a 13-year series of population-based prevalence surveys. Invest Ophthalmol Vis Sci 2005;46:2760–5. [DOI] [PubMed] [Google Scholar]
- 22.Au Eong KG. Tay TH, Lim MK. Education and myopia in 110,236 young singaporean males. Singapore Med J 1993;34:489–92. [PubMed] [Google Scholar]
- 23.Rahi JS, Cumberland PM, Peckham CS. Myopia over the lifecourse: prevalence and early life influences in the 1958 british birth cohort. Ophthalmology 2011;118:797–804. [DOI] [PubMed] [Google Scholar]
- 24.Foster PJ, Broadway DC, Hayat S, et al. Refractive error, axial length and anterior chamber depth of the eye in british adults: the EPIC-Norfolk eye study. Br J Ophthalmol 2010;94:827–30. [DOI] [PubMed] [Google Scholar]
- 25.Farioli A, Mattioli S, Quaglieri A, et al. Musculoskeletal pain in Europe: the role of personal, occupational, and social risk factors. Scand J Work Environ Health 2014;40:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rudnicka AR, Kapetanakis VV, Wathern AK, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and guantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol Published Online First: 24 January 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The European Commission. The 2015 ageing report. Luxembourg: Publications Office of the European Union, 2015. http://europa.eu/epc/pdf/ageing_report_2015_en.pdf (accessed 6 Jun 2016).
- 28.Mattioli S, Curti S, Farioli A, et al. Retinal detachment and occupational lifting: rediscovering lost knowledge. In: Venables K, ed. Current topics in occupational epidemiology. Oxford, UK: Oxford University Press, 2013. [Google Scholar]
- 29.Aykan U, Erdurmus M, Yilmaz B, et al. Intraocular pressure and ocular pulse amplitude variations during the valsalva maneuver. Graefes Arch Clin Exp Ophthalmol 2010; 248:1183–6. [DOI] [PubMed] [Google Scholar]
- 30.Brody S, Erb C, Veit R, et al. Intraocular pressure changes: the influence of psychological stress and the valsalva maneuver. Biol Psychol 1999;51:43–57. [DOI] [PubMed] [Google Scholar]
- 31.Rafuse PE, Mills DW, Hooper PL, et al. Effects of valsalva's manoeuvre on intraocular pressure. Can J Ophthalmol 1994;29:73–6. [PubMed] [Google Scholar]
- 32.Bakke EF, Hisdal J, Semb SO. Intraocular pressure increases in parallel with systemic blood pressure during isometric exercise. Invest Ophthalmol Vis Sci 2009;50:760–4. [DOI] [PubMed] [Google Scholar]
- 33.Smith TJ, Kriebel D. A biologic approach to environmental assessment and epidemiology. Oxford, UK: Oxford University Press, 2010. [Google Scholar]
- 34.Goldblum D, Brugger A, Haselhoff A, et al. Longitudinal change of refraction over at least 5 years in 15,000 patients. GraefesArch Clin Exp Ophthalmol 2013;251:1431–6. [DOI] [PubMed] [Google Scholar]
- 35.Fernandez-Montero A, Olmo-Jimenez JM, Olmo N, et al. The impact of computer use in myopia progression: a cohort study in Spain. Prev Med 2015;71:67–71. [DOI] [PubMed] [Google Scholar]
- 36.Ramessur R, Williams KM, Hammond CJ. Risk factors for myopia in a discordant monozygotic twin study. Ophthalmic Physiol Opt 2015;35:643–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.