Abstract
Background
Sars-CoV2 can cause severe pneumonia and acute respiratory distress syndrome (ARDS). In COVID-19-associated respiratory failure, lung transplantation might be an option (Bharat A).
Case report
A previously healthy 63-year-old man with a nasopharyngeal swab positive for SarsCoV2 and radiological evidence of interstitial lung consolidations developed acute respiratory distress that required intubation and veno-venous extracorporeal membrane oxygenation support (VV ECMO). Because of no recovery of his lung function, he underwent a bilateral lung transplant. ICU stay was complicated by several episodes of bacterial superinfections and an increase of liver function tests (LFTs). Afterward, he faced a progressive clinical worsening associated to severe anemia, further rise of indices of cholestasis, hypertriglyceridemia and hyperferritinemia. Bone marrow smear showed a picture compatible with haemophagocytic lymphohistocytosis (HLH) and first and second line therapy were started. In addition, a transjugular hepatic biopsy was performed with histopathological evidence of portal and periportal fibrosis, compatible with Covid 19-related cholangiopathy. During the hospital stay, he developed several MDR opportunistic infections. The patient died few months later from multiorgan failure secondary to septic shock. A post-mortem confirmed a diagnosis of cholangiopathy, and medullary erythro-haemophagocytosis.
Conclusion
Post Covid19 syndrome is a clinical entity that includes novel and old sequelae following recovery from Sars-CoV2 infections. Early identification of these diseases is crucial for adequate management and might influence the long term prognosis of these patients.
Keywords: Sars-CoV2, Post Covid19 syndrome, Haemophagocytic lymphohistocytosis, Post COVID-19 Cholangiopathy
Introduction
Sars-CoV2 causes coronavirus disease 2019 (COVID-19), a syndrome causing severe interstitial pneumonia, acute respiratory distress syndrome (ARDS) and death. In patients with persistent COVID-19-associated respiratory failure, possibly due to fibrotic evolution of acute lung damage, lung transplantation might be an option. Preliminary data showed that the early post-transplant outcomes of patients were similar to that of patients transplanted for other causes (Bharat et al. 2021). Bacterial and viral infections may complicate the post-transplant period; also new critical illnesses included in the definition of Post Covid 19 syndrome may influence the long-term outcome of transplanted patients. Post-COVID-19 Cholangiopathy may occur after receiving treatment in intensive care units (ICUs), was described in lung-transplant patients and recently was described in three patients recovered from Covid19 (Roth et al. 2021); COVID-19 was also recognized as causative form of secondary haemophagocytic lymphohistocytosis (sHLH) in relation to the expression of features of systemic hyper-inflammation or cytokine storm (Mcgonagle et al. 2020). HLH is an aggressive and life-threatening syndrome in which excessive immune activation affects vital organs. It can be triggered by a secondary event that disrupts immune homeostasis, like infections and solid organ transplant (SOT). We present a case of a healthy 63-year-old man with a diagnosis of COVID-19 ARDS who after receiving bi-lung transplantation had a clinical course complicated by HLH, Covid-19 secondary sclerosing cholestasis, several episodes of septic shock by multi-drug resistant (MDR) bacteria. The patient died few months later for septic shock.
Case
In November 2020 a healthy 63-year-old man, with a history of arterial hypertension and no history of liver disease, was admitted with cough, fever and dyspnoea to Ospedale Centrale of Bozen (Italy). RT-qPCR test on nasopharyngeal swab sample was positive for Sars-Cov2 with radiological evidence of interstitial lung consolidations. The patient developed a distress respiratory syndrome that required intubation and a veno-venous extracorporeal membrane oxygenation support (VV ECMO). In the absence of lung function recovery, in January 2021 he underwent a bilateral lung transplant. After transplant surgery, ICU stay was complicated by acute renal failure (AKI III); critical illness polyneuropathy (CIP); several episodes of bacterial superinfections and lastly, passenger lymphocyte syndrome (PLS), characterized by severe haemolysis, for which he received multiple transfusion with red cells. During ICU stay, an increase of liver function test (LFTs) with a cholestatic pattern was observed (Total Bilirubin 22 mg/dl, GGT 894 U/l, ALP 104 U/l). Several abdominal ultrasound scans resulted inconclusive. The hepatic dysfunction was thought to be caused by multiple effects of multiorgan failure, sepsis and long ICU stay. High bilirubin levels were treated with Cytosorb filter, with temporary reduction of bilirubin level. At the end of February 2021, during his stay in a respiratory rehabilitation center, the patient faced a progressive clinical worsening characterized by abdominal soreness in right hypochondrium associated with severe anemia (Hb 6.6 g/dl) and further rise of indices of cholestasis, hyperbilirubinemia (total bilirubin 21.50 mg/dl, conjugated bilirubin 16.6 mg/dl, AST 63 U/l, ALT 105 U/l), elevation of gamma-glutamyl transferase (GGT 1532 U/l), hypertriglyceridemia and hyperferritinemia (21845 mg/dl).
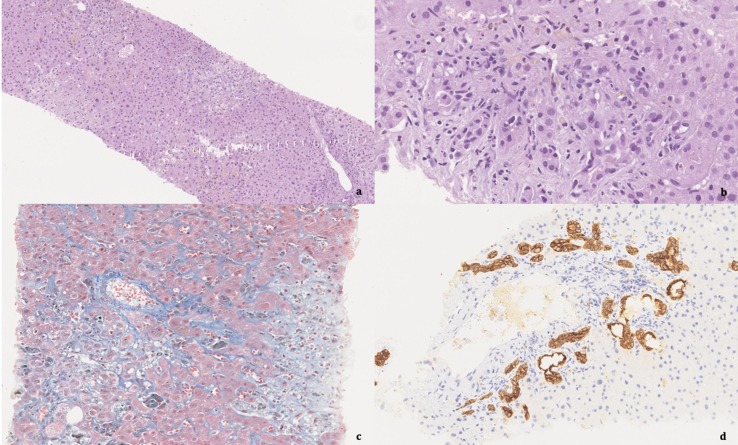
The patient was referred to the ICU division of Ospedale San Matteo of Pavia to continue the diagnostic process. A bone marrow biopsy (BOM) was performed, and the medullary smear showed multiples histiocytes with intracytoplasmic hemosiderin and erythrocytes consistent with a clinical picture of HLH syndrome. Thus, a steroid treatment with dexamethasone was started. For persistent and abundant secretions, a bronchoalveolar lavage (BAL) was performed documenting an extensively drug resistant carbapenem-producing Klebsiella pneumoniae (KPC XDR). Thus, treatment with meropenem/vaborbactam was started, with the resolution of the acute respiratory infection. Because of persistence of bilirubin fluctuation, the patient underwent plasma exchange-cycles with partial improvement. Despite antibiotic therapy and resolution of respiratory symptoms, fever recurred with rising CMV-DNA. As a result, a pre-emptive therapy with ganciclovir was also initiated but it was complicated by neutropenia. During the hospital stay the patient developed other several MDR opportunistic infections and at the end of April, two septic episodes with isolation of KPC XDR on blood culture treated with meropenem/vaborbactam complicated the course. LFTs continued to deteriorate and in the face of worsening of hepatic function, a transjugular hepatic biopsy was performed with histopathological evidence of moderate portal and periportal fibrosis and intraparenchymal cholestasis with cholangiopathy and vasculopathy, compatible with the diagnosis of COVID-19 cholangiopathy. On biopsy, microbiological investigations including EBV DNA and CMV DNA, HHV6-DNA, HSV-DNA, Sars-CoV2, RNA and mycobacteria were negative. For persistence of alteration in blood values (total bil. 13.69 mg/dl, Hb 8.6 g/dl, ferritinemia 5608 mg/dl) a first line therapy for HLH syndrome was started (metilprednisolone plus IgG) with temporary increased of blood values (Carter, Tattersall, and Ramanan 2019). On April, for persisting alteration of LFTs and pancytopenia, a second line therapy with Anakinra (anti-IL-1 receptor) was started (Carter, Tattersall, and Ramanan 2019). Contemporaneously, due to persisting decline of liver function, five cycles of Cytosorb were started with no benefit. The patient died in June, after another septic episode characterized mainly by fever and hypotension, with negative blood culture results and treated with broad-spectrum antibiotic and antifungal therapy. Post-mortem examination provided evidence of ectasia of entire extrahepatic biliary tract, with thickened intraluminal biliary material, marked cholestatic liver disease in fibrotic evolution, medullary erythro-haemophagocytosis (Fig. 1 ).
Fig. 1.
Autopsy images. Description: a: 10x, H&E.Intra and extracellular cholestasis with feathery degeneration of liver cells. b: 40x, H&E. Portal tract with marked ductular reaction and morphological alterations of bile duct epithelia. c: 20x, Masson trichrome. Centrilobular and pericellular fibrosis, cholestasis, bile infarcts. d: 20x, Cytokeratin 7 immunostain. Portal and periportal ductular reaction.
Discussion
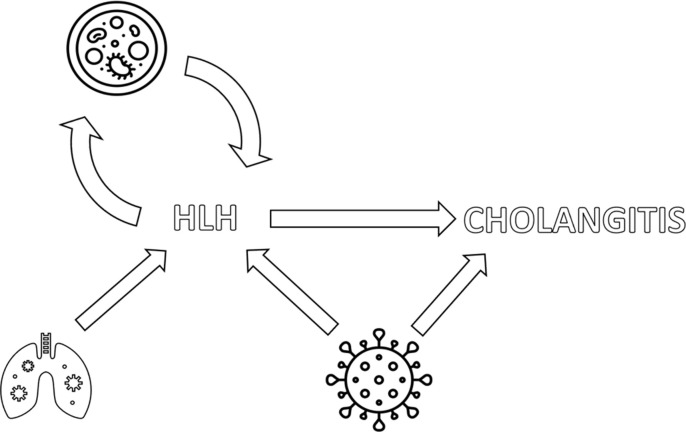
Every day new data are detected, showing new and old diseases that might complicate the course of COVID 19 recovery: different terms are used but “Post Covid 19 Syndrome” is at the moment the more inclusive definition, encompassing acute and chronic complications beyond 4 weeks that may not be attributed to alternative diagnoses (Nalbandian et al. 2021). HLH is an underrecognized condition due to a hyperinflammatory syndrome characterized by fulminant hypercytokinemia with a high mortality burden (Carter, Tattersall, and Ramanan 2019). Immune activation from an infection is a common trigger in secondary HLH sporadic cases with no underlying genetic cause identified. The most common infectious trigger is a viral infection (Naous et al. 2021). As reported by Nalbandian et al, severe COVID-19 is associated with increased levels of inflammatory cytokines, which resembles the cytokine profile observed in cases of secondary HLH (Nalbandian et al. 2021). Recently, Sars-CoV2 infection was recognized as a cause of HLH in severe COVID-19 cases and its occurrence may complicate the recovery of severe COVID-19 patients (Dewaele and Claeys 2020). Prompt diagnosis is needed to have chance to control the disease that might be fatal in COVID-19 patients, but the clinical presentation is complex and it can mimic many other clinical entities (Naous et al. 2021). Using Hscore to estimate the probability of having HLH may be useful to early recognize patients that may benefit from a treatment that inhibit viral inflammation with an immunosuppression therapy (Fardet et al. 2014). Our patient had a score consistent with a very high probability of having the disease and diagnosis was confirmed fulfilling six of eight criteria of HLH2004 study: fever > 38.5 °C, splenomegaly, cytopenia, hypertriglyceridemia > 265 mg/dl, hemophagocytosis in bone marrow, ferritin > 500 ng/ml. The treatments for HLH obviously contributed to impair the patient immunity and they increased the already higher risk of infection of lung transplant recipients. We speculate, therefore, that bacterial and viral infections (KPC XDR, CMV) have acted as a trigger for HLH, thus causing a vicious circle (Fig. 2 ). Furthermore, the continuous use of antibiotics led to the development of resistance, which made infections increasingly difficult to eradicate. Some treatments have necessarily been suspended due to the onset of side effects (like neutropenia with ganciclovir) in an increasingly debilitated and immunosuppressed patient.
Fig. 2.
Possible correlation between lung-transplant, Sars-Cov 2 infection, HLH and cholangitis. Description: Sars-CoV 2 infections led the patient to bi-lung transplant. However, Sars-CoV 2 can be the trigger of both HLH and cholangitis. Also HLH may be associated with cholangitis. Furthermore, HLH treatments contribuited to impair the patient immunity and they increased the already higher risk of infection of lung transplant recipients. So, bacterial and viral infections have acted as a trigger for HLH, thus causing a vicious circle.
In literature, HLH is also considered a rare cause of hyperbilirubinemia. Su Hwan Lee et all, have presented a retrospectively single-centre study about a record of 116 lung transplantation patients of which 33 developed hyperbilirubinemia. Among 33 patients with hyperbilirubinemia, two patients had HLH. These patients underwent imaging studies but did not reveal abnormalities in the biliary tract or liver parenchyma. Our case was characterized by the same diagnostic difficulties described above and also by the same poor prognosis (Lee et al. 2017). Post-Covid cholangiopathy is also described in the literature as a new clinical entity: cholangiocyte express on their surface the angiotensin converting enzyme-2 (ACE2), the host receptor for SARS-CoV2 leading to direct viral damage to cholangiocytes and to chronic liver disease (Roth et al. 2021) (Zhao et al. 2020). Sars-Cov2 RT-PCR study on liver biopsy was negative, as in our case. At the moment, no treatment seems to be effective (Roth et al. 2021).
Conclusion
In this Covid-19 pandemic, new clinical entities are emerging, and they are still poorly described in the literature. HLH and secondary cholangiopathy in this type of patients remain two very rare entities, therefore further studies are needed to understand their mechanism and subsequent early treatment of these conditions associated with Sars-Cov2.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
Funding: this report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical Approval statement: Since data were anonymized no ethics approval was deemed necessary. IRB approval was not required given the retrospective, non-interventional and anonymized nature of the study, but the patient signed a specific written consent for use of clinical data for scientific purpose, according to hospital policy.
References
- Bharat A., Machuca T.N., Querrey M., Kurihara C., Garza-Castillon R., Kim S., Manerikar A., Pelaez A., Pipkin M., Shahmohammadi A., Rackauskas M., Kg S.R., Balakrishnan K.R., Jindal A., Schaheen L., Hashimi S., Buddhdev B., Arjuna A., Rosso L., Palleschi A., Lang C., Jaksch P., Budinger G.R.S., Nosotti M., Hoetzenecker K. Early Outcomes after Lung Transplantation for Severe COVID-19: A Series of the First Consecutive Cases from Four Countries. The Lancet Respiratory Medicine. 2021;9(5):487–497. doi: 10.1016/S2213-2600(21)00077-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter S.J., Tattersall R.S., Ramanan A.V. Macrophage Activation Syndrome in Adults: Recent Advances in Pathophysiology, Diagnosis and Treatment. Rheumatology (United Kingdom) 2019;58(1):5–17. doi: 10.1093/rheumatology/key006. [DOI] [PubMed] [Google Scholar]
- Dewaele K., Claeys R. Hemophagocytic Lymphohistiocytosis in SARS-CoV-2 Infection. Blood. 2020;135(25):2323. doi: 10.1182/BLOOD.2020006505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fardet L., Galicier L., Lambotte O., Marzac C., Aumont C., Chahwan D., Coppo P., Hejblum G. Development and Validation of the Hscore, a Score for the Diagnosis of Reactive Hemophagocytic Syndrome. Arthritis and Rheumatology. 2014;66(9):2613–2620. doi: 10.1002/art.38690. [DOI] [PubMed] [Google Scholar]
- Lee S.H., Park M.S., Lee J.G., Song J.H., Chung K.S., Jung J.Y., Kim E.Y., Kim Y.S., Kim S.K., Chang J., Paik H.C., Kim S.Y. Rare Causes of Hyperbilirubinemia after Lung Transplantation: Our Experience at a Single Center. Journal of Thoracic Disease. 2017;9(12):5030–5039. doi: 10.21037/jtd.2017.11.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcgonagle, Dennis, Kassem Sharif, Anthony O Regan, and Charlie Bridgewood. 2020. “Since January 2020 Elsevier Has Created a COVID-19 Resource Centre with Free Information in English and Mandarin on the Novel Coronavirus COVID- 19 . The COVID-19 Resource Centre Is Hosted on Elsevier Connect , the Company ’ s Public News and Information ,” no. January.
- Nalbandian A., Sehgal K., Gupta A., Madhavan M.V., McGroder C., Stevens J.S., Cook J.R., Nordvig A.S., Shalev D., Sehrawat T.S., Ahluwalia N., Bikdeli B., Dietz D., Der-Nigoghossian C., Liyanage-Don N., Rosner G.F., Bernstein E.J., Mohan S., Beckley A.A., Seres D.S., Choueiri T.K., Uriel N., Ausiello J.C., Accili D., Freedberg D.E., Baldwin M., Schwartz A., Brodie D., Garcia C.K., Elkind M.S.V., Connors J.M., Bilezikian J.P., Landry D.W., Wan E.Y. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi: 10.1038/s41591-021-01283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naous E., Nassani B.M., Yaghi C., Nasr F., Medlej R. Hemophagocytic Lymphohistiocytosis, a New Cause of Death during ‘Post-Acute COVID-19 Syndrome?’ A Case Report. Journal of Hematopathology. 2021;14(3):229–233. doi: 10.1007/s12308-021-00452-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth N.C., Kim A., Vitkovski T., Xia J., Ramirez G., Bernstein D., Crawford J.M. Post-COVID-19 Cholangiopathy: A Novel Entity. The American Journal of Gastroenterology. 2021;116(5):1077–1082. doi: 10.14309/ajg.0000000000001154. [DOI] [PubMed] [Google Scholar]
- Zhao B., Ni C., Gao R., Wang Y., Yang L.i., Wei J., Lv T., Liang J., Zhang Q., Xu W., Xie Y., Wang X., Yuan Z., Liang J., Zhang R., Lin X. Recapitulation of SARS-CoV-2 Infection and Cholangiocyte Damage with Human Liver Ductal Organoids. Protein and Cell. 2020;11(10):771–775. doi: 10.1007/s13238-020-00718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]