Australia is a vast country encompassing major cities along with smaller rural and remote communities often separated by substantial distance. Approximately 28% of the Australian population live in rural and remote areas, defined as regions outside of major cities. Smaller local hospitals in these areas can provide general medical services; however, certain outpatient subspeciality care, including haematology, is often provided by so-called fly-in fly-out specialists running outreach clinics, or requires travel to more urban areas for appointments. Patients requiring inpatient subspecialist management are transferred to the nearest tertiary referral hospital.
Rural and remote populations are a vulnerable group with adverse cancer mortality outcomes. Although great therapeutic advances are being made across the field of haematology, patients from rural and remote communities frequently have limited access to these developments. The COVID-19 pandemic has amplified this health-care access disparity.
Our institution (St Vincent's Hospital, Sydney; a large metropolitan centre) provides outreach haematology services to two large regional catchment areas, Griffith and Wagga Wagga, which are located 478 km and 460 km away, respectively. Patients with haematological malignancies are often immunocompromised and can deteriorate rapidly, so regular clinical reviews and investigations are vital. Therefore, in 2017, the rural and remote paper-based medical records were converted to electronic health records (EHRs) by extending the metropolitan EHRs to rural centres, creating a unified EHR between the metropolitan site and the two regional centres. This process allowed for safe remote chemotherapy prescribing, clinical monitoring, and multidisciplinary management of patients with haematological conditions.
The COVID-19 pandemic posed substantial challenges to health-care systems. Telemedicine has been utilised worldwide to mitigate infection risks for patients and health-care staff. In outreach services, the suitability of this approach is limited by a lack of access to on-site patient records, pathology and radiology results, and ways to remotely initiate therapy safely. In Australia during the COVID-19 pandemic, flights to rural and remote areas abruptly ceased. Border closures and flight restrictions were imposed with little warning. This situation effectively denied these communities access to specialist care. There was an urgent shift to telemedicine consultations with either telephone or video calls, which would have been impossible without the previously instituted unified EHR. The added advantage of the EHR was the ability to monitor service activity and disruptions due to COVID-19.
We reviewed the clinical service activity at these two regional haematology outreach services over a 2-year period, including the 12 months before and after the sudden COVID-19 pandemic-related travel restrictions in April, 2020. We assessed clinical activity of the regional haematology clinics, outpatient and chemotherapy treatment centres, and patient admission rates to the metropolitan tertiary referral centre.
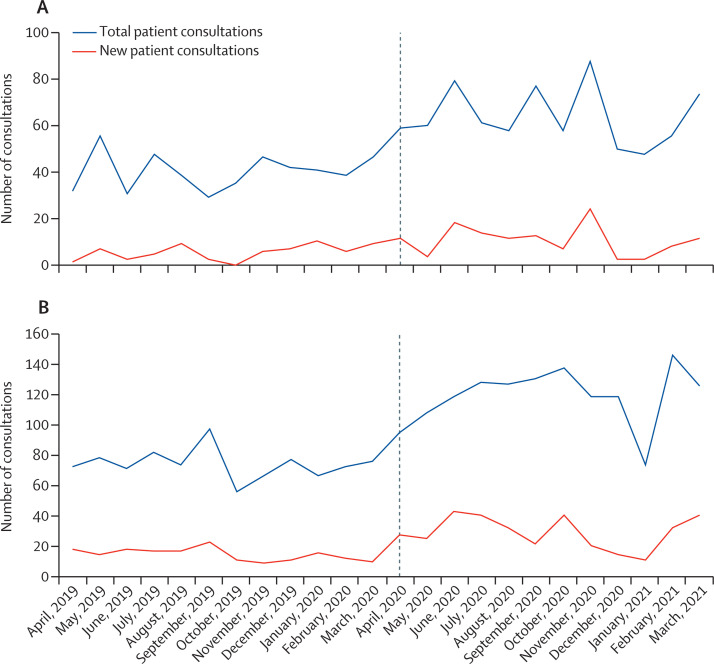
Total patient consultations at both regional sites increased after the transition to telemedicine-only patient reviews (figure ). An average of 39 patients were seen in the Griffith clinic each month (total=479) before the pandemic, compared with an average of 63 per month after the change to telehealth (total=760), representing a 58% increase in patient consultations. In Wagga Wagga, an average of 74 patients were reviewed each month (total=890) before the pandemic compared with an average of 119 patients per month in the following 12-month period (total = 1430), representing an increase of 60%. The number of new patients reviewed also increased at both locations after the transition to telemedicine only (figure). Delivery of chemotherapy and supportive treatments was not substantially reduced after the change to telehealth, with plasma cell myeloma and non-Hodgkin lymphoma treatments accounting for the largest proportion over the study period.
Figure.
Griffith (A) and Wagga Wagga (B) haematology outpatient clinic activity by month, April, 2019, to March, 2021
Dotted line denotes the change to telemedicine consultations due to pandemic-related travel restrictions.
No increase was seen in the number of regional patients with haematological conditions having unplanned admissions to the tertiary referral centre to suggest disruptions in care or serious complications due to treatments delivered in the rural and remote centres. There were 23 unplanned admissions before the travel bans and 21 admissions after. We were able to show that this vulnerable rural and remote high-risk patient group with haematological conditions were appropriately treated and monitored during the COVID-19 pandemic without the need to travel long distances for specialist reviews.
The COVID-19 pandemic has amplified the health-care disparity in cancer care in regional and remote areas of Australia. Our EHR facilitated a rapid shift to telemedicine safely and has improved access to specialist care for regional patients with haematological conditions during a time of disruption in many other aspects of health-care delivery, which has mitigated the potentially catastrophic scenario of no access to critical cancer services for 12 months or more. However, more research is required to investigate the patient experience of telemedicine for those living outside of urban areas, particularly for patients with haematological and oncological conditions with a malignant diagnosis, which is often a time of adjustment and psychological distress.
We acknowledge the limitations of telemedicine that accompany the substantial benefits noted during the COVID-19 pandemic. Telemedicine cannot replace a face-to-face review to assess a patient's clinical status, especially in a new malignant diagnosis before administering chemotherapy treatment, or for the early detection of abnormal clinical examination findings. Certain populations might have particular difficulty adopting alternative modalities to face-to-face reviews, such as older people, people who are deaf or hard of hearing, those who do not have appropriate equipment or technical skills, and those who face language barriers or have poor health literacy. Poor telephone reception or internet connectivity also poses a challenge; however, accessing the necessary technology platforms through a local hospital clinic could be an alternative solution. Conversely, telemedicine can abrogate potentially severe impacts on the timely diagnosis of malignancies for regional patients through increased ease of access to specialists.
Permanent government funding with public reimbursement through the Medicare system for telehealth services was approved in December, 2021, in Australia. We advocate for the widespread adoption of strategies to integrate medical records of outreach rural and remote cancer services where possible, particularly for management of malignant diagnoses, in which close clinical monitoring between reviews is often required. If the unique needs of this vulnerable patient group are not addressed, we run the risk of widening the gap between rural and remote and metropolitan cancer health outcomes. In regions such as Australia, where over a quarter of the population live in rural and remote areas, improving access to high-quality specialist care should be an urgent priority. A hybrid model that includes both face-to-face and telehealth reviews at appropriate time points in patient care could be favourable in reducing waiting times without compromising patient trust and rapport. The question remains of whether the use of telemedicine is associated with any survival implications, and further research is needed to address its possible shortcomings. Early reports investigating this question have been conflicting. However, increased access to specialists through alternative telehealth methods and periodic face-to-face reviews might be beneficial from a patient perspective.
We show how two regional outreach haematology services were able to continue with minimal disruption after the COVID-19 pandemic caused an unexpected transition to exclusively remote patient reviews and chemotherapy management. The use of an integrated digital EHR shared between sites facilitated safe remote telemedicine services, including cancer therapy delivery. Our data suggest that this strategy supports sustainable clinical services in an unpredictable environment to prevent potentially detrimental impacts on already fragile health services.
Acknowledgments
We declare no competing interests.