Abstract
People who are homeless experience higher rates of vaccine-preventable disease, including COVID-19, than the general population, and poorer associated health outcomes. However, delivering vaccinations to people who are homeless is complex, and there is a lack of evidence to inform practice in this area. The aim of this systematic review is to: (a) identify, (b) analyse the characteristics of, and (c) evaluate the outcomes of, strategies to improve vaccination rates in people who are homeless.
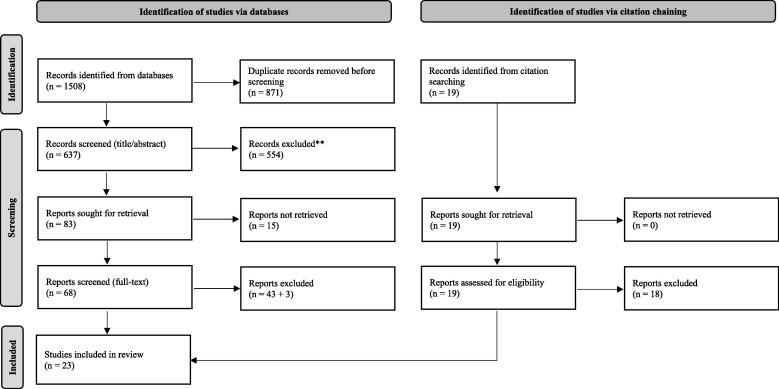
Literature was retrieved from eight electronic databases. Studies undertaken in high-income countries, published in English, in a peer-reviewed journal, and in full-text were considered. No limits were placed on study design or date. A total of 1,508 articles were retrieved and, after the removal of duplicates, 637 were screened. Twenty-three articles, reporting on nineteen separate vaccination strategies for hepatitis A/B, influenza, herpes zoster, invasive pneumococcal disease, and diphtheria in people who are homeless, were selected for inclusion.
All the strategies were effective at improving vaccination rates in, people who are homeless. Most strategies involved vaccination clinics and most were delivered, at least in part, by nurses. Other characteristics of successful strategies included: delivering vaccinations at convenient locations; using accelerated vaccination schedules (if available); vaccinating at the first appointment, regardless of whether a person’s vaccination history or serological status were known (if clinically safe); operating for a longer duration; offering training to staff about working with people who are homeless; widely promoting clinics; considering education, reminders, incentives, and co-interventions; ensuring no out-of-pocket costs; and working collaboratively with stakeholders, including people who are homeless themselves. These findings will inform evidence-based vaccination strategies, including for COVID-19, in people who are homeless, and improve associated health outcomes in this at-risk, hard-to-reach group.
Keywords: Vaccination, Vaccine, Immunisation, Homeless, Hepatitis, Influenza
1. Introduction
‘Homelessness’ occurs when a person lacks access to suitable housing.(1) People who are homeless may be unsheltered, or they may live in temporary, overcrowded, substandard, untenable, or unsafe housing.(1) In OECD countries, rates of homelessness range from 0.004% in Japan to 0.86% in New Zealand.(1) In one-third of OECD countries, rates of homelessness are increasing, and this increase is likely to be amplified by the COVID-19 pandemic.
In comparison to the general population, people who are homeless experience poorer health and health outcomes, including in relation to vaccine-preventable diseases. People who are homeless experience higher rates of vaccine-preventable diseases including hepatitis A/B,[2], [3], [4] influenza,(5)invasive pneumococcal disease,[6], [7], [8] tuberculosis,[9], [10], [11], [12] and COVID-19.[13], [14], [15], [16], [17], [18], [19] People who are homeless who are diagnosed with COVID-19 are > 20 times more likely to be hospitalised, >10 times more likely to need intensive care, and > 5 times more likely to die.(20).
There is a strong case for prioritising people who are homeless for vaccination.(21) However, delivering vaccination to people who are homeless is challenging. People who are homeless often lack information on vaccination, (22) they may consider vaccination a low priority,[22], [23] they may not have the means to travel to a vaccination clinic, and they may be reluctant to trust (and so be unwilling to actively present to) clinics.(24) In comparison to the general population, people who are homeless have lower rates of vaccination.(25) There are no existing reviews about strategies to improve vaccination rates in people who are homeless and, so, a lack of evidence to inform practice in this area. This is problematic considering the world’s largest vaccination effort, for COVID-19, is underway. This systematic review will address this gap. The review aims to: (a) identify, (b) analyse the characteristics of, and (c) evaluate the outcomes of, strategies to improve vaccination rates in people who are homeless.
2. Methods
2.1. Eligibility criteria
The PICO framework was used to develop eligibility criteria for this review. The ‘population’ was any person, of any age, considered ‘homeless’ using the OECD definition.(1) The ‘intervention’ was any strategy implemented to improve vaccination rates in people who are homeless. The ‘comparator’, if relevant, was standard approaches to vaccination. The ‘outcome’ was the strategy’s: (a) characteristics, and (b) outcomes. Only studies undertaken in high-income countries, published in English, in a peer-reviewed journal, and in full-text were considered. All study designs were considered. The searches were not date-limited.
2.2. Information sources
The databases searched were CINAHL, ClinicalTrials.gov, Cochrane Library, Embase, MEDLINE, PsycINFO, Scopus, and Web of Science. Citation chaining was undertaken.
2.3. Search strategy
The searches used two groups of keywords: those related to (a) ‘homelessness’, and (b).
‘vaccination’ (including ‘immunisation’). Index terms and subject headings were used if available on the databases. The search strategy is provided in Supplement 1.
2.4. Selection process
Search results were exported into EndNote X9. Duplicate items were removed. Items were screened in two steps: (a) for all items: by reading the title/abstract, then (b) for the remaining items: by reading the full text. Each step was completed by one researcher (LM) and checked by a second researcher (AE); where needed, agreement was achieved through discussion.
2.5. Data collection process
Data was extracted into an electronic table. Extraction was completed by one researcher (LM) and checked by a second researcher (AE); where needed, agreement was achieved through discussion. The items extracted included data about: (a) the study, (b) the study participants, (c) the strategy’s characteristics, and (d) the strategy’s outcomes.
2.6. Risk of bias in individual studies
Literature selected for inclusion was evaluated for risk of bias and quality. Randomised controlled trials (RCTs) were evaluated using the revised Cochrane Risk-of-Bias Tool for Randomised Controlled Trials (RoB 2),(26) cohort studies were evaluated using the Risk of Bias in Non-Randomised Studies of Interventions (ROBINS-1) tool,(27) and cross-sectional studies were evaluated using the Appraisal Tool or Cross-Sectional Studies (AXIS) tool.(28).
2.7. Data synthesis
Quantitative analysis (e.g. meta-analysis) of the results was planned. If quantitative analysis was not possible, the results were to be analysed narratively using a thematic approach.
3. Results
3.1. Searches
The selection process is shown in Fig. 1 , as a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram [29]. The searches were conducted in two rounds to July 10, 2021, and returned 1508 articles. Eight hundred and seventy-one duplicates were removed, leaving 637 unique articles for screening. During the screening of titles and abstracts, 554 articles were removed, leaving 83 articles. Approximately 10% of the articles excluded at this step were checked by a second researcher, and there was 100% concordance.
Fig. 1.
PRISMA diagram showing the literature selection process.
Sixty-eight of the remaining articles were available in full-text. During the screening of full-texts, 43 articles were excluded. Articles were excluded primarily because they were not full-text, peer-reviewed articles (e.g. they were conference posters or abstracts), or because they did not separate outcomes for people who are homeless from other groups. The reference lists of the remaining articles were then manually searched. An extra 19 articles were screened by title/abstract, and nine were read in full-text. One was selected for inclusion.(30).
The selected articles were then, again, checked by a second researcher. After robust discussion, the researchers agreed to exclude three articles which had initially been included: one which reported vaccine effectiveness as the primary outcome,(31) one which reported on a screening program where vaccination was not a key component,(32) and one where ‘immunisations’ were discussed without any detail.(33) A final total of 23 articles were included.[30], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55].
3.2. Studies
Details about the studies are shown in Table 1 . The studies were published between 1998,(36) and 2021.(55) The majority (N = 16) were undertaken in the US, and there were also studies from Australia,[40], [48] Canada,[36], [42] France,(30) the Netherlands,(51) and the UK.(54). All were quantitative studies, either cross-sectional or longitudinal. There were seven RCTs.[53], [56], [43], [44], [45], [46], [47] Some studies included a qualitative component,(41) or a cost analysis.(53) The studies were highly heterogeneous, and this precluded quantitative analysis. Data was instead analysed narratively, in themes according to the study characteristics and outcomes.Table 1A. .
Table 1.
Study and population characteristics.
| Reference | Year of Publication |
Location | Type of Study | Number of Participants (People Experiencing Homelessness) |
Type of Homeless | Age | Sub-Population |
|---|---|---|---|---|---|---|---|
| Nyamathi et al. | 2009a | United States (Los Angeles) |
Randomised controlled trial |
865 | Sheltered | Adults, 18–65 years | Nil |
| Nyamathi et al. | 2009b | United States (Los Angeles) |
Randomised controlled trial |
865 | Sheltered | Adults, 18–65 years | Nil |
| Nyamathi et al. | 2012 | United States (Los Angeles) |
Randomised controlled trial |
297 | Sheltered | Adults, 18–65 years | People with a history of incarceration |
| Nyamathi et al. | 2015 | United States (Los Angeles) |
Randomised controlled trial |
345 | Not reported | Adults, 18–60 years | Men recently released on parole |
| Nyamathi et al. | 2016 | United States (Los Angeles) |
Randomised controlled trial |
600 | Not reported | Adults, 18–60 years | Men recently released on parole |
| Schwarz et al. | 2008 | United States (Baltimore) |
Randomised controlled trial |
328 | Sheltered | Children and adolescents, ≤18 years (+adult caregivers to consent) |
Nil |
| Zhang et al. | 2018 | United States (San Diego) |
Randomised controlled trial with cost analysis | 451 | Not reported | Adults, 18–46 years | Gay/bisexual men, and transgender women, who abused stimulants (amphetamine, meth-amphetamine, cocaine) |
Table 1A.
Study and population characteristics: Randomised controlled trials.
| Reference | Year of Publication |
Location | Type of Study | Number of Participants (People Experiencing Homelessness) |
Type of Homeless | Age | Sub-Population |
|---|---|---|---|---|---|---|---|
| Beers et al. | 2019 | United States (rural Midwest) |
Before-and-after |
54 | Not specified | Adults, 18–80 years |
Nil |
| Brouqui et al. | 2010 | France (Marseille) |
Cross-sectional |
249 | Sheltered | Not reported | Nil |
| Brown et al. |
2021 | United States (Nashville) |
Longitudinal | 228 | Sheltered, unsheltered | Not reported | Nil |
| Castillo et al. | 2018 | United States (San Diego) |
Before-and-after |
1129 | Not reported | Not reported | Nil |
| Haley et al. | 1998 | Canada (Montreal) |
Longitudinal |
681 | Unsheltered | Youth, 14–25 years | Nil |
| James et al. | 2009 | United States (Boston) |
Cross-sectional |
90 | Not reported | Adults, >21 years | Nil |
| Kang et al. | 2020 | United States (San Diego) |
Cross-sectional | 1385 | Not reported | Not reported | Nil |
| Kaplan-Weisman et al. |
2018 | United States (New York) |
Cross-sectional | 93 | Sheltered | Older adults, ≥60 years | Nil |
| Kong et al. | 2020 | Australia (Melbourne) |
Cross-sectional | 295 | Not reported | Not reported | Nil |
| Metcalfe & Sexton | 2014 | United States (unspecified) |
Cross-sectional with qualitative component |
60 | Not reported | Adults, >18 years | Nil |
| Moses et al. | 2002 | Canada (Winnipeg) |
Longitudinal |
533 | Unsheltered | Adults, 26–65 years; Youth, 11–25 years |
Nil |
| Poulos et al. | 2010 | Australia (Sydney) |
Longitudinal |
201 | Not reported | Adults, ≥16 years | Nil |
| Steele et al. | 2003 | United States (New Orleans) |
Cross-sectional |
Not specified | Not reported | ‘Adolescents’ | Nil |
| Tjon et al. | 2005 | The Netherlands (Rotterdam) |
Cross-sectional |
1800 | Not reported | Adults, 18–87 years | People currently using drugs |
| Washington-Brown & Cirilo |
2020 | United States (Miami-Dade County) |
Longitudinal |
209 | Not reported | Adults, ≥18 years | Nil |
| Wright et al. |
2002 | United Kingdom (Leeds) |
Longitudinal | 90 | Not reported | Not reported | People with a current or past history of drug use |
3.3. Population
The sample sizes in the studies ranged from 54 (34) to 1800 people.(51) They included people who were homeless in sheltered and unsheltered settings. Most studies (N = 12) focused on adults, defined as people aged ≥ 18 years (and sometimes as ≥ 16 years or ≥ 21 years), though there were also studies which included only children/youth/adolescents,[36], [49], [50] only older adults,(39) or a mix of age-groups.(42) Some studies focused on specific homeless sub-populations, including people using drugs,[51], [54] people with a history of incarceration,(45) stimulant-using gay/bisexual men or transgender women,(53) and men on parole.[46], [47].
3.4. Intervention characteristics
Details about the intervention characteristics outlined in this section are shown in Table 2 :Table 2A. .
Table 2.
Intervention characteristics.
| Reference | Intervention | Infectious Disease | Site(s) | Vaccination Schedule | Strategy (not study) Duration |
Staffing | Staff Training | Promotion | Education | Reminder | Incentive | Co-intervention | Funding: Vaccine | Funding: Strategy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nyamathi et al., 2009a; 2009b; 2012 | Vaccination clinic | Hepatitis A; Hepatitis B (ROUTINE) | Shelters, residential drug treatment facilities, clinics |
Standard (3x dose) or accelerated (2x dose); vaccination given at participant’s second appointment (+2 weeks) | Duration of study | Nurses; outreach teams | Not specified | ‘Detailed information’ provided to eligible people | Intervention #1: Education: 7x sessions of nurse case management + 1x targeted education session + local community resource guide Reminder: tracking by outreach worker Incentive: USD $5 per vaccine dose Intervention #2: Education: 1x targeted education session + local community resource guide Reminder: tracking by outreach worker Incentive: USD $5 per vaccine dose Intervention #3: Education: 1x targeted education session + local community resource guide Reminder: none Incentive: USD $5 per vaccine dose |
Serological testing; drug and alcohol use behaviours; depressive/ mental health symptom screening | Participants reimbursed for vaccine | Not specified | ||
| [45], 2016 | Vaccination clinic | Hepatitis A; Hepatitis B (ROUTINE) |
1x residential drug treatment facility | Accelerated schedule (0,7,21–30 days); vaccination given at second appointment (+1 week) |
Duration of study | Nurses; peer coaches | Not specified | Not specified | Intervention #1: Education: weekly 45-minute peer coaching + 8x 20-min nurse case management sessions Reminder: reminders at appointment (or via telephone call) + appointment cards Incentive: none Intervention #2: Education: weekly 45-minute peer coaching + brief hepatitis A/B education from nurse Reminder: reminders at appointment (or via telephone call) + appointment cards Incentive: none Intervention #3: Education: 1x brief counselling/health promotion session + brief encouragement from nurses to complete vaccination Reminder: reminders at appointment (or via telephone call) + appointment cards Incentive: none |
Not specified | Not specified | Not specified | ||
| [48] | Vaccination clinic | Hepatitis B (ROUTINE) | Multiple shelters | Accelerated (3monthschedule); vaccination given at participant’s second appointment (+4 weeks) |
Not specified | Nurses | Not specified | Not specified | Intervention #1: Education: 8-min video on hepatitis B + 5-min Powerpoint summary + information sheet + opportunity to discuss with health staff Reminder: reminder card, in a pouch which could be work as a necklace Incentive: at visits 1/2/3, USD$10/$10/$30; gift packages for children/youth and care-givers with cosmetics, candy, toothbrushes Intervention #2: Education: 8-min video on smoking + 5-min Powerpoint summary + information sheet + opportunity to discuss with health staff Reminder: reminder card, in a pouch which could be work as a necklace Incentive: at visits 1/2/3, USD$10/$10/$30; gift packages for children/youth and care-givers with cosmetics, candy, toothbrushes |
Depression screening | Free to participants | Not specified | ||
| [52] | Vaccination clinic | Hepatitis A; Hepatitis B (ROUTINE) | 1x community-based substance abuse treatment centre |
Vaccination given at second appointment (+7–10 days) | 16 weeks, then 4-month and 8-month follow-ups | Nurses, peer health educators | Not specified | Flyers in public locations with details about program site/times; interested persons met with research staff on-site | Intervention #1: Education: 8x 20-min case management meetings with a nurse + 8x hepatitis education sessions with a peer health educator Reminder: not specified Incentive: USD$10-$35 per episode of participation Intervention #2: Education: 1x 20-min health education session provided by a health educator Reminder: not specified Incentive: USD$10-$35 per episode of participation |
Serological testing; counselling about risk | Free to participants | Not specified | ||
Table 2A.
Intervention characteristics: Randomised controlled trials.
| Reference | Intervention | Infectious Disease | Site(s) | Vaccination Schedule | Program (not study) Duration |
Staffing | Staff Training | Promotion | Education | Reminder | Incentive | Co-intervention | Funding: Vaccine | Funding: Program |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [34] | Vaccination clinic | Influenza – seasonal (ROUTINE) |
1x shelter; 1x church-based meal site; 1x primary care clinic | Not applicable | 3 months; duration of influenza season At shelter and meal site: frequency not specified; at primary care clinic: 3x clinics over 3 months |
Nurse practitioner; registered nurses; program director | Two-sided summary information sheet about vaccination rates in people who are homeless; 1x 20-minute educational program at a staff meeting; modification of clinic policy (all patients offered vaccination) |
Approached by staff and invited; program director volunteered at shelter/meal site and was known to participants | Co-designed information handout; OR verbal education from staff | Not applicable | None | None | Patient insurance; if patient was uninsured, funding from local health department OR primary care clinic | Local health department for registered nurses to deliver vaccine |
| Brouqui et al., 2010 | Vaccination clinic | Influenza – seasonal; Influenza – pandemic (ROUTINE) |
1x shelter | Not applicable | 1 day at the site | Infectious diseases doctors; interns; medical students |
Not specified | People in shelter were ‘informed’ 3 days prior | Written consent form | Not applicable | None | None | Conseil General 13; French Ministry of Health | Not specified |
|
[54] |
Student-run clinic | Influenza – seasonal (ROUTINE) |
1x clinic for un(der)-insured patients; outreaches at outdoor locations, refuges, shelters, and churches |
Not applicable | Late-September to January; duration of the influenza season | Medical students; nursing students; pharmacy students; physicians; nurse practitioners; pharmacists |
The previous year’s student coordinators train the incoming student coordinators; students are taught how to administer and record vaccines |
One-to-one conversations with potential patients about the influenza vaccine (using interpreters if needed) | One-to-one conver-sations; vaccine information Statements in various languages | Not applicable | None | None | Community-based grant of approx. US$25,000 per season | Community-based grant of approx. US$25,000 per season |
| [35] | Automated computerised alert in emergency department; prompted providers to offer vaccine to people who are homeless and has a ‘quick’ button to order vaccine from pharmacy |
Hepatitis A (OUTBREAK) | 1x hospital emergency department |
Not applicable | Not specified | Healthcare workers in emergency department |
Not specified | Vaccination offered to eligible people at presentation at emergency department |
Not specified | Not applicable | None | None | Not specified | Not specified |
| [36] | Vaccination clinic | Hepatitis B (ROUTINE) |
7x sites frequented by homeless youth (drop-in centres, food banks, shelters, etc.) |
Accelerated (0,1,4months) | Not specified; 2 to 3 clinics per week at rotating sites | Outreach worker; community workers involved with homeless youth |
Information sessions with community workers about Hepatitis B and vaccination; led to collaborative design of vaccination program | Outreach worker gave youth information about Hepatitis B/ vaccination; colourful flyers and posters with vaccination schedules displayed in public areas; personalised letters to community organisation directors; cards with outreach worker’s contact details |
Outreach worker gave youth information about Hepatitis B/ vaccination | Pocket-sized reminder card with contact details of outreach worker; active recall system: youth completed a form with their contact information, entered into an automated system, 3x attempts at contact made and then ongoing periodic contact, also follow-up through social/ rehabilitation/ correctional organisations; youth who had left the city directed to alternative vaccination programs |
Third visit: food voucher, t-shirt or movie pass | Referrals for other medical concerns (e.g. testing, medical/ psychological care, social services, etc.) | Not specified | Not specified; incentives donated to program |
| [37] | Automated computerised alert in emergency department | Hepatitis A (OUTBREAK) | 1x hospital emergency department |
Not applicable | 4 months; duration of Hepatitis A outbreak |
Healthcare workers in emergency department (doctors [faculty, residents], nurses, pharmacists) |
15-minute presentation for nurses and physicians about Hepatitis A/ vaccination (6x offered in 2 days to capture all staff); posters and flyers placed in clinical areas; coloured/ laminated vaccination protocol cards for staff to wear with ID badges |
Vaccination offered to eligible people at presentation |
Information sheet about Hepatitis A | Vaccination card provided with first vaccination | None | None | Public Health Commission | Material costs funded by Public Health Commission (e.g. posters, vaccine logs, patient eligibility sheets, etc.); staff costs funded by hospital. |
| [38] | Automated computerised alert in emergency department (see [35]; coincided with mass vaccination events, foot vaccination teams, mobile vaccination vans, targeted vaccinations at healthcare centres |
Hepatitis A (OUTBREAK) | 1x hospital emergency department |
Not applicable | 18 months; duration of Hepatitis A outbreak |
Healthcare workers in emergency department |
Regularly-scheduled emails to staff about Hepatitis A outbreak and vaccinations | Communi-cations on hepatitis A published in community newsletters; nurses distributed information to at-risk populations; vaccination offered to eligible people at presentation |
Communi-cations on hepatitis A published in community newsletters; nurses distributed information to at-risk populations | Not applicable | None | Vaccination of emergency department staff | Not specified | Not specified |
| [39] | Vaccination clinic | Herpes zoster (ROUTINE) | 1x homeless shelter clinic | Not applicable; vaccination given at participant’s third appointment |
2 years and 10 months, 5x immunisation days where vaccines administered | Family physician; nurse | Not specified | Vaccination offered to eligible people at health appointments |
Physician delivered a 30-minute talk to shelter residents | Not applicable | None | Alternative immunisation options – to be vaccinated at national retail chain pharmacy nearby, or to bring vaccination frozen from any outside pharmacy |
Participant insurance/co-payment; uninsured = vaccine manufacturer |
Not specified |
|
[5] |
Vaccination clinic |
Influenza – seasonal (ROUTINE) |
1x crisis centre |
Not applicable | At least 1 day per site | Nurse immunisers | Not specified | Promotional materials sent to each site before each visit; vaccines were offered to clients at each site |
Not specified | Not applicable | None | None | Federal government funded under National Immunisation Program | Not specified |
|
[40] |
Vaccination clinic | Influenza – seasonal (ROUTINE) | 1x day shelter | Not applicable | 1 day | Nursing students, supervising registered nurse |
Not specified | Health students visited people in parks, shelters, bus stations to promote vaccination; posters placed in shelters; ‘flu vouchers’ with vaccine information and a map |
Not specified |
Not applicable | Free ‘flu vouchers’ | Vaccination of staff, volunteers | Not specified | Not specified |
|
[41] |
Vaccination clinic | Hepatitis B (ROUTINE) |
11x ‘sentinel’ sites frequented by people who are homeless |
Standard: 0, 1, 6 months; vaccination given at participant’s second appointment | Not specified | Nurses; physicians | Not specified | Not specified |
Educational session; provided with literature; counselled about risk/ lifestyle choices |
Participants ‘asked to return’ for subsequent doses of vaccine | None | Serological testing | Not specified | Not specified |
| [47] | Vaccination clinic | Hepatitis A; Hepatitis B (ROUTINE) | 1x medical clinic specifically for homeless/ disadvantaged persons | Standard or accelerated; vaccination given at participant’s first OR second appointment (+2 weeks) |
Not specified | Physicians; nurses | Not specified | Vaccination offered to eligible people at presentation |
Clients offered information; counselling/ education | Written reminder about subsequent vaccination date; reminders at clinic visits | None | Serological testing and counselling on risk factors | Funded by federal government | Funded by federal government |
| [49] | Vaccination clinic | Hepatitis B; tetanus; diphtheria (ROUTINE) |
1x shelter/ transitional living facility | Not specified | Not specified | Medical students; nurses | Not specified | Patients offered program when they presented for intake |
Not specified | Not specified | None | Health history/ physical examination; drug screening; screening and treatment for sexually transmitted infections; risk counselling |
Medical assistance programs; care provided without reimburse-ment until participant employed |
Not specified |
| [50] | Mass vaccination campaign |
Hepatitis A (OUTBREAK) | Various | Not applicable | 3 weeks; duration of Hepatitis A outbreak |
Not specified | Not specified | Not specified | Not specified | Not applicable | None | Vaccination of volunteers, staff | Not specified | Not specified |
| [51] | Vaccination clinic | Invasive pneumococcal disease (ROUTINE) |
1 × primary care clinic | Not applicable | Twice per month at each location, ongoing | Nurse practitioners; nursing students | Training on receiving, storing, administering vaccines, monitoring, document-ation |
Face-to-face promotion; offered to eligible people at intake; offered during weekly group shelter meetings | Provided a Vaccine Information Statement; educational classes with audio-visual aids; 1 h session per week offered for 6 months prior to program; breakout groups taught by students |
Not applicable | Combinations of branded t-short, cap, backpack, water bottle, hand wipes, hand sanitiser, toothbrush, toothpaste, fresh fruit, food bar, deodorants, body wash, vitamins, rubber shower shoes |
Not specified | State provides financial assistance to eligible people who are uninsured/ unfunded | Local/state/ national grants; pharma-ceutical industry grant for materials (Patient Assistance Program); community donations |
|
[53] |
Vaccination clinic | Hepatitis B (ROUTINE) | 1 × primary care centre | Standard [1], [6] or accelerated (0,7,21days); vaccination given at first appointment |
Not specified | Practice nurse | Not specified | Patients offered program when they presented for care and reported current/past drug use |
Not specified | Next vaccination date flagged in person’s electronic health record and ‘oppor-tunistic verbal reminders’ given if people attended the clinic |
None | Serological testing | Not specified | Not specified |
Intervention: Most studies (N = 20) involved vaccination clinics, either as stand-alone interventions or part of a broader public health initiative. Three studies involved strategies to identify people experiencing homelessness as they presented to hospital emergency departments, to flag them for vaccination.[35], [37], [38] There were three instances where data from a single strategy was reported in > 1 article, so nineteen unique strategies are examined.
Infectious diseases: Most studies (N = 16) involved hepatitis A and/or B vaccination, and the others involved vaccination for seasonal and/or pandemic influenza,[30], [34], [40], [41], [55] herpes zoster,(39) invasive pneumococcal disease,(52) and diphtheria.(50) Most (N = 19) involved vaccination for routine disease prevention; others involved disease outbreaks.[35], [37], [38], [51].
Location: The studies reported on vaccination strategies delivered at locations frequented by, or easily accessible to, people who are homeless. Locations reported included shelters,[30], [34], [36], [49], [55], [43], [44], [45] day shelters,(41) transitional housing programs,(50) community/drop-in/crisis centres,[36], [40] residential drug treatment facilities,[53], [43], [44], [45], [46], [47] churches,(55) and meal programs or food banks.[34], [36] Some strategies were delivered in healthcare settings, including primary clinics (standard or for under-served groups),[34], [48], [52], [54], [43], [44], [45] a clinic in a shelter,(39) and emergency departments.[35], [37], [38] One study reported vaccinations being delivered via pharmacies, hospitals, mass vaccination events, foot teams, and mobile vans.(38).
Some of these locations required participants to travel to staff, and others required staff to travel to participants. There was a roughly equal mix of single-site and multi-site strategies. In a cross-sectional study which compared vaccination strategies delivered at ‘non-traditional’ sites (e.g. shelters) and at ‘traditional sites’ (e.g. primary health clinics), it was found that a greater percentage of people experiencing homelessness were vaccinated at non-traditional sites.(34).
Vaccination schedules: Eight of the studies involving multi-dose hepatitis B vaccines offered an accelerated vaccination schedule, as standard or as an option, with the aim of increasing rates of completion of the vaccine series.[36], [54], [43], [44], [45], [46], [47], [48], [49] In an RCT which compared an accelerated schedule (2x doses over 2 months) versus a standard schedule (3x doses over 6 months), more people completed the accelerated schedule (73.0% vs. 54.0%).(44) A longitudinal study testing an accelerated schedule also reported a similar finding.(54).
Most strategies (N = 15) gave the vaccine, or the first dose, at the participant’s first appointment, even if their vaccination history or serological status were unknown. The remaining strategies required participants to wait until a second appointment, at one week,[46], [47] seven to ten days,(53) two weeks,[43], [44], [45] or four weeks(49) after the first. In one strategy, participants waited until a third appointment, as there was an additional planned delay associated with obtaining the vaccine from a pharmacy.(39) In a study involving vaccination at a second appointment two weeks after the first, it was found that 29.0% of participants failed to re-present for their second dose.(43) However, another study about Hepatitis B vaccination found, via serological testing, that 42.0% of participants were already immune at their first appointment, and so received a vaccine unnecessarily.(56).
Duration: The studies reported on vaccination strategies which operated for various lengths of time. Most of the strategies appeared to be ongoing, although the study itself was time-limited. Some strategies ran for a single day at each site.[30], [40], [41] Other strategies ran for the duration of the influenza season,[34], [55] or for the duration of an outbreak of disease.[37], [38], [51].
The strategies were operated in a variety of formats. For example: one involved three 3-hour clinics per week,(35) and another involved bi-monthly clinics.(52) Another strategy operated two to three days per week at rotating sites.(36) Another involved a mass immunisation day when there were ≥ 6 people ready to be vaccinated, to save on vaccine shipping costs.(39).
Staffing: The studies which described staffing identified nurses (including students, nursing assistants, registered nurses, nurse immunisers, nurse practitioners, and research nurses) as key staff members.[34], [37], [52], [53], [55], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50] Many strategies also involved physicians.[30], [34], [37], [39], [42], [48], [54], [55] Other professionals including pharmacists, outreach workers, mental health workers, social workers, laboratory workers, administration staff, program coordinators/directors, and computer support analysts were also involved. A number of the studies used ‘gatekeepers’, or people with access to people who are homeless.[34], [36], [40].
Staff training: Six of the vaccination strategies began by training the staff involved – for example: about the signs/symptoms of an infectious disease, the behaviours which may increase infection risk in people who are homeless, the importance of vaccination for people who are homeless, and responsibilities related to receiving, storing, administering, and documenting vaccines. Training was typically delivered via information sessions and handouts.[34], [36], [37], [52] One study describes having coloured, laminated vaccination protocol cards for staff to wear.(37).
Promotion: There were a variety of initiatives to promote vaccination. Some strategies used promotional materials – for example: cards, flyers, and posters with program times and locations, in locations frequented by people who are homeless.[36], [40], [41], [53], [43], [44], [45] In one study, staff handed out ‘flu vaccine vouchers’ with a map to the clinic.(41) Some strategies which relied on gatekeepers directed promotional materials to them.[36], [40] Others utilised outreach workers, who visited people to talk about vaccination.[36], [41] Often, people were told about vaccination in a health appointment or intake assessment.[35], [48], [52], [55], [37], [38], [39].
Education: All the strategies offered education to people who are homeless, about infectious diseases and/or vaccination. Often, education and promotion (above) took place simultaneously. Education was frequently brief and intended only to facilitate informed consent. Sometimes, education was more robust and aimed at improving vaccine uptake.[34], [36], [39], [42], [52] For example: one strategy had a physician deliver a 30-minute talk to residents of a shelter immediately prior to the commencement of a vaccination strategy in the shelter.(39) Sometimes, written information was also used, including standardised vaccine statements produced by the Centres for Disease Control and Prevention (CDC).(55) One strategy distributed handouts about vaccination co-designed by people who are homeless.(34) In a study which compared a short video about hepatitis B versus a video about smoking on hepatitis B vaccine uptake, it was found the hepatitis B video increased uptake by 17.2%.(56).
Reminders: Many (N = 11) of the strategies involving the multi-dose hepatitis B vaccination implemented strategies to remind people to present for their next dose. Often, this involved providing people with a reminder card, perhaps in a protective pouch, with details of their next appointment.[36], [37], [48], [49], [56] Other studies implemented systems to remind people about their next vaccination, either routinely or opportunistically, if they presented to a clinic in-between vaccination doses.[48], [54] One study describes using ‘active recall’, which included contacting people by telephone and locating them through other services and facilities.(36).
Incentives: Ten strategies offered an incentive to people for presenting for vaccination, or for re-presenting for subsequent doses in a vaccine series. Incentives included cash payments, ranging from USD$5 to USD$35 per episode of care.[53], [56], [43], [44], [45] Other incentives included clothing, toiletries, food vouchers, snacks, vitamins, and movie passes.[36], [52], [56].
Seven RCTs tested combinations of education, reminders, and incentives. For example: one hepatitis A/B vaccination strategy involved 1x 20-minute nurse-led group education session, plus active recall by an outreach worker, plus incentives of USD$5 per dose.[43], [44], [45] These RCTs found that people receiving education, reminders, and incentives were more likely to complete a vaccine series, when compared with standard care (i.e. limited education, and/or limited or no tracking, and/or limited or no incentives), however this was not significant.
Co-interventions: Twelve strategies involved interventions in addition to vaccination (‘co-interventions’). This included laboratory-based serological testing (with or without counselling) for the disease being vaccinated against or other diseases, mental and physical health screening, and/or drug and alcohol screening, with subsequent referrals if required.[36], [53], [54], [42], [43], [44], [45], [48], [49], [50] A number of the strategies also provided vaccinations to volunteers and staff.[38], [41], [51].
Vaccine funding: Vaccines were funded in a variety of ways. In many of the US studies, vaccines were funded by a participants’ health insurance, sometimes with an out-of-pocket co-payment (ranging from <$10 to $100).[34], [39] If a person was un(der)insured, a clinic, health department, and/or vaccine manufacturer might fund the vaccine.[34], [39], [55] In other studies, vaccines were fully-funded by governments and/or vaccine manufacturers.[30], [37], [40], [48], [50], [52], [53] Lack of health insurance was a key reason for people declining vaccines.[39], [41].
Strategy funding: Of the strategies which reported funding, all were government-funded.[34], [37], [48], [52] Two of the RCTs costed the strategies they reported on.[47], [53] These identified the major cost to be associated with staffing, with additional costs associated with purchasing vaccines, serological testing, incentives, educational resources, and facility hire.[47], [53] Both RCTs identified greater costs associated with strategies which combined education, reminders, and incentives; costs ranged from USD$159 to $167 per patient.(47).
3.5. Intervention outcomes
Details about the intervention outcomes outlined in this section are shown in Table 3 :Table 3A. .
Table 3.
Intervention outcomes.
| Reference |
Outcome(s) | Determinants of Uptake | Enablers and/or Barriers |
|---|---|---|---|
| Nyamathi et al., 2009a | 68% of Intervention #1 participants received 3x vaccinations (i.e. complete vaccine series), 61% of Intervention #2 received 3x vaccinations, 54% of Intervention #3 received 3x vaccinations. Intervention #1 participants had almost 2x greater odds of completing vaccination than Intervention #2 participants, and 1.5x greater odds than Intervention 3 participants; this was not statistically-significant. |
Completers: more likely to be chronically homeless, have a significant other, be older, have participated in a self-help substance abuse program, and report fair or poor health. Non-completers: more likely to report male homosexual behaviours, to be White, to be male, and to have participated in a non-residential substance abuse program. |
Enablers: Not reported Barriers: Not reported |
| Nyamathi et al., 2009b | Standard schedule: 68% of Intervention #1 participants received 3x vaccinations (i.e. complete series), 61% of Intervention #2 received 3x vaccinations, 54% of Intervention #3 received 3x vaccinations. Accelerated schedule: 81% of Intervention #1 participants received 2x vaccinations (i.e. complete series), 78% of Intervention #2 received 2x vaccinations, 73% of Intervention #3 received 2x vaccinations. Intervention #1 participants were significantly more likely to complete 2 of 3 doses, as well as the full 3 dose vaccine program. |
Compared to the three-dose vaccine completers, two-dose vaccine completers were less likely to report chronic homelessness. They were less likely to be male and more likely to be younger and have participated in a self-help substance abuse program. |
Enablers: Not reported Barriers: Not reported |
| [44] | 61% of Intervention #1 participants received 3x vaccinations, 55% of Intervention #2 participants received 3x vaccinations, and 53% of Intervention #3 participants received 3x vaccinations. |
Completers: more likely to be older than 40 years, and to have been homeless for 1 year or longer. Non-completers: more likely to have engaged in binge-drinking. |
Enablers: Not reported Barriers: Not reported |
| [45] | 75.4% of Intervention #1 participants received 3x vaccinations, 71.8% of Intervention #2 participants received 3x vaccinations, and 71.9% of Intervention #3 participants received 3x vaccinations. |
Completers: more likely to have 6 + friends, to have high instrumental coping, to have completed alcohol treatment, to have used cocaine within 6 months of incarceration, and to be hepatitis C positive. Non-completers: more likely to have been taken away from parents, to have spent time in juvenile detention, to have been hospitalised for mental health problems, or to have used intravenous drugs. |
Enablers: Not reported Barriers: Not reported |
| [46] | The amount of cash spent on program activities was $32,583 for the Intervention #1 participants (M=$167.09; SD=$79.51), $33,375 for Intervention #2 participants (M=$170.28; SD=$76.20), and $33,293 for Intervention #3 participants (M = 159.30; SD=$76.61). |
Not reported. |
Enablers: Not reported Barriers: Not reported |
| [48] | Vaccine coverage increased from 68% to 85%. Only 54% completed the vaccine series. Overall, 89/104 (86%) accepted 1 + vaccination and 54% completed the vaccine series. Of the 104 children and adolescents who needed a hepatitis B vaccine at the beginning of the study, 62.3% (N = 33/53) of the hepatitis B video group completed the vaccine series by the end of the study vs. 45.1% (N = 23/51) of the alternative anti-smoking video group (p = 0.16). The PowerPoint presentation plus discussion was associated with higher hepatitis B vaccine acceptance rates at visits 2 and 3 (p = 0.06). |
Not reported. |
Enablers: Educational materials (video) targeted to population (children/youth) Accelerated schedule suited transient population Barriers: 42.0% were later shown to have full coverage at baseline, and so were administered vaccination unnecessarily Parents often mistakenly believed child had been vaccinated Parents refused the vaccine because they did not believe their child was at-risk for hepatitis, because they preferred to be vaccinated by their own doctor, and because their child/ren ‘refused to cooperate’ |
| [52] | Of the 170 people eligible for vaccination, 85.0% completed the three-dose series (Intervention #1 = 85.9%, Intervention #2 = 84.8%). Cost analysis favoured the simpler, less labour-intensive Intervention #2. 65.0% of participants completed the Intervention #1 education sessions, and 99.0% completed the Intervention #2 sessions. |
Not reported. |
Enablers: Initial contact to introduce people to healthcare/ vaccination services, prior to recruitment Simpler, less-expensive interventions more feasible The vaccination clinic was conveniently located Barriers: Not reported |
Table 3A.
Intervention outcomes: Randomised controlled trials.
| Reference |
Outcome(s) | Determinants of Uptake | Enablers and/or Barriers |
|---|---|---|---|
| [34] | There was a decrease in vaccination rate at the clinic site (24.8% in 2017–18 vs. 23.9% in 2018–19). There was a 115% increase in vaccination rate at the shelter/meal sites (N = 13 in 2017–18 vs. N = 28 in 2018–19). Vaccination refusal rate for people included in the intervention was 39.5%, and for people not included in the intervention was 51.9%. |
Vaccine acceptance not correlated with gender, age, participation in the intervention, or positive history of vaccination. |
Enablers: Multiple vaccination sites; provider collaboration Barriers: Delay in receipt of influenza vaccine from supplier, until after the start of the influenza seasonLack of regular feedback about vaccination rates to staff (slowing impetus to promote vaccination) Medical/social acuity levels of participants may have prevented nurses focusing on preventive care People who are homeless interact with healthcare providers on an irregular/limited basis; mistrust high Lack of confidence in vaccine; lack of consistent emphasis about importance of vaccination; lack of up-to-date information about vaccination Misinformation about vaccination/influenza is prevalent Single nurse unable to see all eligible patients |
| Brouqui et al., 2010 | 46.9% (N = 117/249) people received a pandemic flu vaccination, N = 26 received seasonal + pandemic flu vaccination. |
Not reported. |
Enablers: Participants had good knowledge about benefits of influenza vaccination; participants were “more afraid [of] the disease than … possible vaccine side effect[s]” Barriers: Nil reported |
|
[54] |
Patients experiencing homelessness or living in temporary accommodation were administered 120 vaccines in 2015–16, 55 vaccines in 2016–17, 78 vaccines in 2017–18, and 228 vaccines in 2018–19. |
Not reported |
Enablers: Use of student volunteersDelivered vaccinations at convenient locations (e.g. beneath a well-trafficked city bridge) Barriers:Need to cold-chain the vaccine (2 °C-8 °C)Need to use personal protective equipment (PPE) and screen patients for COVID-19 symptoms prior to entry |
| [35] | 0 vaccinations in historical period, 23 vaccinations in pre-intervention period (vaccination program but no alert), 465 in intervention period (vaccination program and alert). This is equivalent to 0, 9, 184 vaccinations per 1,000 visits by homeless persons. During intervention period, 77.5% of visits where patient received the vaccine, had already received it or it was not indicated; 22.5% of visits where alert was activated but patient did not receive vaccine (e.g. because the vaccine was refused (40.8%) or no reason given). Vaccination rates declined over time, likely due to other vaccination programs operating in the region. |
Not reported. |
Enablers: Coincided with mass Hepatitis A/vaccination education campaign operated by local public health agency Barriers:Potential impacts on staff work load (e.g. alert fatigue) May have disrupted patient flow/length of stay Delays with pharmacist needing to review vaccine orders |
| [36] | 681 participants received 1/3 doses, 79.1% received 2/3 doses, 50.4% received 3/3 doses. | 2 doses: more likely to be female, more likely to be involved in prostitution; 3 doses: more likely to be involved in prostitution. Completion not associated with men who have sex with men, intravenous drug use. |
Enablers: Clinics scheduled for the late afternoon/evening to match the times most participants tended to present to sites Clinic times were arranged around the other activities taking place at each site, to avoid disruption Strong links with community workers with access to various hard-to-reach groups of homeless youth Barriers: Participants used clinic/outreach worker to seek assistance outside program scope (e.g. referrals, shelter, etc.) Reaching all eligible participants may take several years |
| [37] | 122 patients, 74% of whom were homeless (N = 90), received a vaccine. |
Not reported for people who are homeless. |
Enablers: Stored vaccines in refrigerator in emergency department, allowing staff to dispense independent of pharmacy Actively involved all key stakeholders in emergency dept Paper supplies relevant to program in all triage rooms Emergency departments = accessible to patients Barriers: Involved an additional 5–10 min of time per patient |
| [38] | 10,324 vaccines were administered, of which 1385 (13%) were administered to homeless people. |
Not reported. |
Enablers: Other than the emergency department where vaccines were delivered, patients had limited access to routine care Close coordination between public heath, health, and community agencies to enable outbreak management Barriers: Not reported |
| [39] | Vaccine accepted by 37/93 = 39.8% of eligible patients. | No differences in ethnicity/other demographic characteristics; patients with 3 + comorbidities more likely to accept; women and those who had previously declined other vaccines less-likely to accept. Primary reasons for declining were lack of insurance, or refusal of all vaccines. |
Enablers: Partnering with a local pharmacy Barriers: Participants’ lack of insurance coverage Patient-held beliefs about vaccine necessity/risks Lack of on-site medical freezer Lack of an efficient way to determine vaccine costs and participant insurance coverage First vaccine given at second appointment: there was a need to wait for 5 + doses, or pay $20 shipping fee |
| [5] | N = 295 people received a vaccine at the crisis centres. |
Not reported. |
Enablers: 52% were worried about getting influenza 13% considered getting the vaccine convenient 9% had the vaccine recommended by their doctor Barriers: Not specified |
| [40] | N = 60 (100%) homeless individuals at the shelter received vaccination; this was an increase from 28 vaccinations the previous year. An additional 26 people filled vouchers for vaccination at a local health department. | Not specified. |
Enablers: Not specified Barriers: People reported fears and misperceptions of vaccines 32.0% said they did not feel they needed a vaccine 34.0% said they do not like to receive shots 23.0% said they believed the flu vaccine is unsafe 21.0% said they had a previous bad experience with vaccines 38.0% said they were concerned about side-effects 47.0% said they identified ‘other’ barriers to vaccination (e.g. concerns the government was ‘tracking them’) 59.0% said they did not have the money for a vaccine 53.0% said they did not have relevant health insurance 53.0% said they did not have transportation 24.0% said they had problems with mobility 40.0% said they did not know where to get a vaccine |
| [41] | Of the 533 participants, 528 (98%) received 1x dose of vaccine. After serology, 471 people required vaccination. Of these, 361 (77%) returned for a second dose, and 293 (63%) returned for a third dose. |
People who completed three doses more likely to be > 25 years of age, to engage in unprotected anal sex, and to use solvents. |
Enablers: Not reported Barriers: Not reported |
| [47] | Approximately 49% of eligible clients enrolled in the program. Hepatitis A: 108 people commenced the vaccination schedule; 73% (N = 73/100) of people eligible after serology completed the schedule. Hepatitis B: 102 people commenced the vaccination schedule; 75% (N = 69/92) of people eligible after serology completed the schedule. |
Not reported. |
Enablers: Vaccination was incorporated into routine care The clinic site was considered ‘convenient’ The clinic was already accepted and used by target group Clinic staff/participants were well-known to each otherCounselling (part of pre- and post-serological testing) Barriers: Not reported |
| [49] | Tetanus, diphtheria: offered to all participants not up-to-date; 93% accepted the vaccination. Hepatitis B: of those eligible for vaccination, 9% had coverage on admission, 63% had coverage on follow-up or completion. |
Not reported. |
Enablers: Not reported Barriers: Completing the full series of hepatitis B vaccination was difficult because of the 6-month time period required; 13% refused because it required multiple visits Almost all who initially consented received 2 doses of hepatitis B vaccine, but 41% had left the facility before reaching the 6 months required for the 3rd dose; accelerated schedules are ‘highly desirable’ One quarter of people lacked documentation about previous vaccination outside of the clinic site 1.3% of participants had ‘emotional instability’ and could not be effectively counselled about vaccination People often only seek healthcare in ‘emergencies’; routine healthcare may not be a priority Very few participants qualified for financial assistance |
| [50] | 1515 homeless people were vaccinated actively; 41.0% (N = 627) were vaccinated actively and passively. Vaccination coverage was approximately 83.0% (N = 1515/1800) of homeless population. 1,197 social workers and volunteers who work with the homeless were also vaccinated. The Hepatitis A outbreak in Rotterdam was “terminated”. |
Not reported. |
Enablers: Not reported Barriers: Not reported |
|
[51] |
209 people received a vaccination. | Not reported. |
Enablers: Not reported Barriers: Female participants were reluctant to receive clinic services beyond mandatory intake physical and screening |
|
[53] |
Standard course: 54 patients received a first dose (of those, 52 were eligible for further doses), 23 received a second dose, and 3 received a third dose. Accelerated course: 90 patients received a first dose (of those, 86 were eligible for further doses) , 64 received a second dose, and 35 received a third dose. People receiving the accelerated course were significantly more likely to complete the course (P < 0.0001). |
Vaccine acceptance not correlated with age or gender. |
Enablers: Accelerated dose requires no change to clinical practice, other than the timing of administration No need for costly postal/telephone reminders Barriers: Not reported |
Intervention efficacy: All the vaccination strategies were reported as being ‘effective’. Most reported ‘effectiveness’ in terms of delivering vaccinations to people who are homeless – including as numbers of people receiving a vaccination, numbers of people completing each step in a vaccine series, and/or percentage of eligible people vaccinated in a given timeframe.[30], [36], [37], [38], [39], [40], [42], [43], [44], [45], [46], [47], [48], [50], [51], [52], [53], [54] Some reported ‘effectiveness’ in terms of improving vaccination rates from a known baseline or a previous timepoint.[34], [35], [41], [55], [56].
Determinants of vaccine uptake: Nine studies identified determinants of vaccine uptake and/or vaccine series completion among participants. People accepting a vaccine or completing a vaccine series were more likely to have multiple comorbidities, to rate their health as ‘fair’ or ‘poor’, to be chronically homeless, to have a partner, to be part of a larger social group, and to be of an older age.[36], [39], [42], [43], [45], [46] People not accepting a vaccine or not completing a vaccine series were more likely to be newly homeless, to have used intravenous drugs, to have participated in a non-residential substance abuse program, to have previously declined a vaccine, to have spent time in the out-of-home care and/or juvenile justice systems, and to have been hospitalised for mental illness.[43], [45], [46] One study found no determinants.(34).
Enablers and barriers: The studies reported a variety of enablers and barriers associated with the vaccine strategies. The studies identified key enablers to be the use of multiple, convenient locations and times for vaccine delivery, and the incorporation of vaccination into routine health and social care.[34], [36], [48], [53], [55] These are particularly vital strategies considering one study found that two-fifths of people did not know where to go to receive a vaccine, and more than half of people lacked transportation to enable them to reach a vaccination site.(41).
The studies identified a key barrier as a delay in the receipt of vaccines from manufacturers and dispensing pharmacies, either because of the need for a pharmacist to review a vaccine order or because of lack of suitable on-site storage facilities (i.e. a vaccine freezer).[34], [35], [39] To overcome this, some strategies used a ‘one-click’ electronic system to increase the efficiency of the ordering process.[35], [38] Another strategy stored vaccines in a refrigerator at the vaccination site, so vaccines were dispensed independently of a pharmacy.(37).
Another key barrier identified in the studies was mistrust among people who are homeless – about healthcare generally, and about vaccinations specifically. If people who are homeless interact with healthcare providers on an irregular/limited basis, mistrust is often high.(34) The studies also identified that misinformation about vaccination is common, and that people subsequently misunderstand their infection risk and the importance of vaccination.[34], [56], [39], [40], [41] Delivery of vaccines sites which are readily accepted by people who are homeless, already used by them, and staffed by people known to them may help to overcome these barriers.(48).
Finally, the studies identified that strong partnerships between key stakeholders – including the health and social care staff working with people who are homeless – to be a key enabler.[36], [37], [38], [39] A number of the studies took this further, involving people who are homeless themselves in strategy design and delivery.[34], [36] The co-design process was not evaluated, however.
3.6. Quality assessment
Most (N = 22) studies were of moderate to high quality, with a low risk of bias, and therefore suitable to inform evidence-based practice. The remaining study was evaluated to be of lower quality,(30) though it was published in the form of a short report with relatively limited detail. There were seven RCTs, but the remaining studies were simpler cross-sectional or single-arm longitudinal studies which are inevitably associated with a degree of bias when interpreting effectiveness. The results of the quality assessment are provided in Supplement 2.
4. Discussion
This systematic review identified 19 strategies, reported in 23 journal articles, which improved vaccination rates in people who are homeless. Most strategies were vaccination clinics, either fixed or mobile. Most were delivered, at least in part, by nurses. However, the strategies were diverse in their other characteristics. This emphasises the need for strategies to be responsive to the context in which they operate, and to the particular homeless population(s) they serve.
Although the strategies analysed in this review were diverse, a number of generalisations can be drawn. Firstly, though there are multiple options for vaccine delivery locations, ‘non-traditional’ sites – where staff travel to people who are homeless, in areas convenient to them – are a key consideration. The need for sites which are convenient for people who are homeless is also emphasised in the broader literature.[57], [58], [59] For COVID-19 vaccination, the CDC recommends vaccination at sites like shelters, meal services, and encampments.(60).
The studies in this review emphasised using accelerated vaccination schedules for multi-dose vaccines, if available. They suggested vaccinating a person at their first appointment, regardless of if their vaccination history or serological status are known, if clinically safe. Although the strategies in this review ran for varying durations, the CDC recommends that COVID-19 vaccination strategies use longer durations to allow sufficient time for decision-making.(60).
As noted, most of the vaccination strategies analysed in this review were delivered, at least in part, by nurses. Most began by training staff to work effectively with people who are homeless, if they have not done so before. Nurses who have had limited, or predominately negative, contact with people who are homeless frequently hold stereotyped views of this group.(61) Education may improve nurses’ attitudes towards people who are homeless, and this may improve the willingness of people who are homeless to present (including for vaccination).(62).
Most of the vaccination strategies analysed in this review used one or more methods of promotion. Research consistently shows that between 30% and 40% of people who are homeless do not intend to be vaccinated for COVID-19.[63], [64], [65] Considering the significant misinformation circulating about COVID-19 and COVID-19 vaccines,(66) promotion may be particularly vital for COVID-19 vaccination strategies. The CDC emphasises the need for clear, consistent messaging with people who are homeless about COVID-19 vaccination.(60).
The review returned unclear findings about the effectiveness of education, reminders, and incentives in vaccination strategies for people who are homeless. Studies in the broader population agree that education, reminders, and incentives have variable impacts on vaccination uptake and series completion.[67], [68], [69] The use of these incentives may depend on a strategy’s budget. However, the studies show active recall is important, and the CDC agrees active recall is a vital component of vaccination strategies for people who are homeless.(60).
Many of the strategies analysed in this review included co-interventions. These are important opportunities to ‘capture’ people who are homeless, who are often infrequent healthcare users, as they present to health services. However, many vaccination strategies for people who are homeless have limited funding, staff, and resources and this may impede their ability to effectively deliver co-interventions.(58) A co-intervention which should be considered is the vaccination of volunteers and staff.(60) This may be a vital aspect of COVID-19 vaccination strategies, as rates of COVID-19 infection among volunteers and staff are often high.(13).
In most of the strategies analysed in this review, vaccines were free for people who are homeless – and where this was not the case, cost was a barrier to uptake. That funded vaccines are an enabler to uptake in people who are homeless is also a finding in the broader literature.[58], [70] In a study about the vaccination capability of homeless health services in the US, it was found that most services are confident navigating reimbursement systems.(71).
The studies included in this review identified multiple barriers to vaccination in people who are homeless. They also identified a key enabler: stakeholder collaboration. The broader literature also identifies collaboration as vital to the success of vaccination strategies,(58,71) and it is a key recommendation for COVID-19 vaccination strategies.(60) Collaboration should go beyond service providers, however: research shows that people who are homeless themselves value the opportunity to become involved in activities related to vaccination.(72).
5. Limitations
The review has some limitations. Some studies reported on vaccination strategies secondary to disease outbreaks and/or broader public health activities, and it is possible that similar studies were overlooked if they were not read in full-text. Studies may have also been overlooked if they were not available on one or more of the databases searched. The review only included studies undertaken in higher-income countries, and the results may not be generalised to other contexts. Further, there were no studies about vaccination strategies specific to COVID-19. There was a lack of RCTs, and we were unable to analyse studies using quantitative methods. No studies were identified that considered approaches to catch-up vaccination for multi-dose vaccines.
6. Conclusion
This systematic review has identified, analysed the characteristics of, and evaluated the outcomes of, strategies to improve vaccination rates in people who are homeless. The strategies identified were diverse in their characteristics and their outcomes; however, generalisations about ‘what works’ could be made. These are vital to informing evidence-based vaccination practice, and to improving related health outcomes, in people who are homeless.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
LKM is a PhD candidate receiving an Australian Government Research Training Program (RTP) scholarship, and a Menzies Health Institute Queensland (MHIQ) top-up scholarship.
References
- 1.Organisation for Economic Cooperation and Development. HC3.1 Homeless population 2020 [Available from: http://www.oecd.org/els/family/HC3-1-Homeless-population.pdf.
- 2.Peak CM, Stous SS, Healey JM, Hofmeister MG, Lin Y, Ramachandran S, et al. Homelessness and hepatitis A - San Diego County, 2016–2018. Clinical Infectious Diseases. 2019;71(1):14-21. [DOI] [PMC free article] [PubMed]
- 3.Hosseini M., Ding A. Hepatitis A outbreak in San Diego County, 2016–2017: A morphologic and epidemiologic review. Open Forum Infectious Diseases. 2018;5(S1):S646. [Google Scholar]
- 4.Noska A.J., Belperio P.S., Loomis T.P., O'Toole T.P., Backus L.I. Prevalence of human immunodeficiency virus, hepatitis C virus, and hepatitis B virus among homeless and nonhomeless United States veterans. Clin Infect Dis. 2017;65(2):252–258. doi: 10.1093/cid/cix295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kong K.L., Chu S., Giles M.L. Factors influencing the uptake of influenza vaccine vary among different groups in the hard-to-reach population. Aust N Z J Public Health. 2020;44(2):163–168. doi: 10.1111/753-6405.12964. [DOI] [PubMed] [Google Scholar]
- 6.Mosites E., Zulz T., Bruden D., Nolen L., Frick A., Castrodale L., et al. Risk for invasive Streptococcal infections among adults experiencing homelessness, Anchorage, Alaska, USA, 2002–2015. Emerg Infect Dis. 2019;25(10) doi: 10.3201/eid2510.181408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lemay J.A., Ricketson L.J., Zwicker L., Kellner J.D. Homelessess in adults with invasive pneumoccal disease in Calgary. Canada Open Forum Infectious Diseases. 2019;6(40) doi: 10.1093/ofid/ofz362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKee G., Choi A., Madill C., Marriott J., Kibsey P., Hoyano D. Outbreak of invasive Streptococcus pneumoniae among an inner-city population in Victoria, British Columbia, 2016–2017. Can Commun Dis Rep. 2018;44(12):317–323. doi: 10.14745/ccdr.v44i12a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bamrah S., Yelk Woodruff R.S., Powell K., Ghosh S., Kammerer J.S., Haddad M.B. Tuberculosis among the homeless, United States, 1994–2010. International Journal of Tuberculosis and Lung Disease. 2013;17(11):1414–1419. doi: 10.5588/ijtld.13.0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan K., Rea E., McDermaid C., Stuart R., Chambers C., Wang J., et al. Active tuberculosis among homeless persons, Toronto, Ontario, Canada, 1998–2007. Emerg Infect Dis. 2011;17(3):357–365. doi: 10.3201/eid1703.100833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee C.-H., Jeong Y.-J., Heo E.Y., Park J.S., Lee J.S., Lee B.J., et al. Active pulmonary tuberculosis and latent tuberculosis infection among homeless people in Seoul. BMC Public Health. 2013;13(1) doi: 10.1186/1471-2458-13-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Romaszko J., Bucinski A., Kuchta R., Bednarski K., Zakrzewska M. The incidence of pulmonary tuberculosis among the homeless in north-eastern Poland. Central European Journal of Medicine. 2013;8(2):283–285. [Google Scholar]
- 13.Mosites E., Parker E.M., Clarke K.E.N., Gaeta J.M., Baggett T.P., Imbert E., et al. Assessment of SARS-CoV-2 infection prevalence in homeless shelters - Four US cities, March 27-April 15, 2020. Morb Mortal Wkly Rep. 2020;69(17):521–522. doi: 10.15585/mmwr.mm6917e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baggett T., Keyes H., Sporn N., Gaeta J. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. J Am Med Assoc. 2020;323(21):2191–2192. doi: 10.1001/jama.2020.6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tobolowsky F.A., Gonzales E., Self J.L., Rao C.Y., Keating R., Marx G.E., et al. COVID-19 outbreak among three affiliated homeless service sites - King County, Washington, 2020. Morb Mortal Wkly Rep. 2020;69(17):523–526. doi: 10.15585/mmwr.mm6917e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bodkin C., Mokashi V., Beal K., Wiwcharuk J., Lennox R., Guenter D., et al. Pandemic planning in homeless shelters: A pilot study of a COVID-19 testing and support program to mitigate the risk of COVID-19 outbreaks in congregate settings. Clinicial. Infectious Diseases. 2020;8 doi: 10.1093/cid/ciaa743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ralli M., Cedola C., Urbano S., Latini O., Shkodina N., Morrone A., et al. Assessment of SARS-CoV-2 infection through rapid serology testing in the homeless population in the City of Rome, Italy: Preliminary results. Journal of Public Health Research. 2020;9(4) doi: 10.4081/jphr.2020.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Storgaard S., Eiset A., Abdullahi F., Wejse C. First wave of COVID-19 did not reach the homeless population in Aarhus. Danish Medical Journal. 2020;67(12) [PubMed] [Google Scholar]
- 19.Yoon J.C., Montgomery M.P., Buff A.M., Boyd A.T., Jamison C., Hernandez A., et al. COVID-19 prevalence among people experiencing homelessness and homelessness service staff during early community transmission in Atlanta, Georgia, April-May 2020. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richard L., Booth R., Rayner J., Clemens K., Forchuk C., Shariff S. Testing, infection and complication rates of COVID-19 among people with a recent history of homelessness in Ontario, Canada: A retrospective cohort study. Canadian Medical Association Journal Open. 2021;11(9):1–9. doi: 10.9778/cmajo.20200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buccieri K., Gaetz S. Ethical vaccine distribution planning for pandemic influenza: Prioritizing homeless and hard-to-reach populations. Public Health Ethics. 2013;6(2):185–196. doi: 10.1093/phe/pht005. [DOI] [Google Scholar]
- 22.Doroshenko A., Hatchette J., Halperin S.A., MacDonald N.E., Graham J.E. Challenges to immunization: The experiences of homeless youth. BMC Public Health. 2012;12:338. doi: 10.1186/471-2458-12-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Omerov P, Craftman A, Mattsson E, Klarare A. (2019). Homeless persons' experiences of health and social care: A systematic integrative review. Health and Social Care in the Community 28(1):1-11. 0.1111/hsc.12857. [DOI] [PubMed]
- 24.Kryda A.D., Compton M.T. Mistrust of outreach workers and lack of confidence in available services among individuals who are chronically street homeless. Community Ment Health J. 2009;45(2):144–150. doi: 10.1007/s10597-008-9163-6. [DOI] [PubMed] [Google Scholar]
- 25.Wood SP. (2012). Vaccination programs among urban homeless populations: A literature review. Journal of Vaccines and Vaccination 104172/2157-75601000156.
- 26.Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019. [DOI] [PubMed]
- 27.Cochrane Methods. Risk of bias in non-randomised studies of interventions (ROBINS-I) ND [Available from: https://methods.cochrane.org/bias/risk-bias-non-randomized-studies-interventions.
- 28.Downes M., Brennan M., Williams H., Dean R. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open [Internet] 2016 doi: 10.1136/bmjopen-2016-011458. https://bmjopen.bmj.com/content/6/12/e011458 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Page M., McKenzie J., Bossuyt P., Boutron I., Hoffman T., Cd m,, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br Med J. 2021 doi: 10.1371/journal.pmed.1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brouqui P., Lagier J.-C., Cassir N., Badiaga S., Gadelius H., H1n1, pandemic flu vaccination campaign: The homeless lesson. PLoS currents. 2009;2010:2. doi: 10.1371/currents.RRN1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Watson B., Seward J., Yang A., Witte P., Lutz J., Chan C., et al. Postexposure effectiveness of varicella vaccine. Pediatrics. 2000;105(1):84–88. doi: 10.1542/peds.105.1.84. [DOI] [PubMed] [Google Scholar]
- 32.Bothamley G.H., Rowan J.P., Griffiths C.J., Beeks M., McDonald M., Beasley E., et al. Screening for tuberculosis: The port of arrival scheme compared with screening in general practice and the homeless. Thorax. 2002;57(1):45–49. doi: 10.1136/thorax.57.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Busen N.H., Engebretson J.C. Facilitating risk reduction among homeless and street-involved youth. Journal of the American Academy of Nurse Practitioners. 2008;20(11):567–575. doi: 10.1111/j.1745-7599.2008.00358.x. [DOI] [PubMed] [Google Scholar]
- 34.Beers L., Filter M., McFarland M. Increasing influenza vaccination acceptance in the homeless: A quality improvement project. Nurse Pract. 2019;44(11):48–54. doi: 10.1097/01.NPR.0000586012.31046.c9. [DOI] [PubMed] [Google Scholar]
- 35.Castillo E.M., Chan T.C., Tolia V.M., Trumm N.A., Powell R.A., Brennan J.J., et al. Effect of a computerized alert on emergency department hepatitis A vaccination in homeless patients during a large regional outbreak. J Emerg Med. 2018;55(6):764–768. doi: 10.1016/j.jemermed.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 36.Haley N., Roy E., Belanger L., Crago A. A hepatitis B vaccination outreach project for street youth in Montreal. Canadian Journal of Human Sexuality. 1998;7(4):331–338. [Google Scholar]
- 37.James T.L., Aschkenasy M., Eliseo L.J., Olshaker J., Mehta S.D. Response to hepatitis A epidemic: Emergency department collaboration with public health commission. J Emerg Med. 2009;36(4):412–416. doi: 10.1016/j.jemermed.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Kang M., Horman S.F., Taplitz R.A., Clay B., Millen M., Sitapati A., et al. Public health role of academic medical center in community outbreak of Hepatitis A, San Diego County, California, USA, 2016–2018. Emerg Infect Dis. 2020;26(7):1374–1381. doi: 10.3201/eid2607.191352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaplan-Weisman L., Waltermaurer E., Crump C. Assessing and improving zoster vaccine uptake in a homeless population. Journal of Community Gealth. 2018;43(6):1019–1027. doi: 10.1007/s10900-018-0517-x. [DOI] [PubMed] [Google Scholar]
- 40.Metcalfe S.E., Sexton E.H. An academic-community partnership to address the flu vaccination rates of the homeless. Public Health Nurs. 2014;31(2):175–182. doi: 10.1111/phn.12088. [DOI] [PubMed] [Google Scholar]
- 41.Moses S., Mestery K., Kaita K.D.E., Minuk G.Y. Viral hepatitis in a Canadian street-involved population. Can J Public Health. 2002;93(2):123–128. doi: 10.1007/BF03404552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nyamathi A., Liu Y., Marfisee M., Shoptaw S., Gregerson P., Saab S., et al. Effects of a nurse-managed program on hepatitis A and B vaccine completion among homeless adults. Nurs Res. 2009;58(1):13–22. doi: 10.1097/NNR.0b013e3181902b93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nyamathi A., Sinha K., Saab S., Marfisee M., Greengold B., Leake B., et al. Feasibility of completing an accelerated vaccine series for homeless adults. J Viral Hepatitis. 2009;16(9):666–673. doi: 10.1111/j.1365-2893.2009.01114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nyamathi A.M., Marlow E., Branson C., Marfisee M., Nandy K. Hepatitis A/B vaccine completion among homeless adults with history of incarceration. Journal of Forensic Nursing. 2012;8(1):13–22. doi: 10.1111/j.1939-3938.2011.01123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nyamathi A., Salem B.E., Zhang S., Farabee D., Hall B., Khalilifard F., et al. Nursing case management, peer coaching, and hepatitis a and B vaccine completion among homeless men recently released on parole: randomized clinical trial. Nurs Res. 2015;64(3):177–189. doi: 10.1097/NNR.0000000000000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nyamathi A.M., Zhang S., Salem B.E., Farabee D., Hall B., Marlow E., et al. A randomized clinical trial of tailored interventions for health promotion and recidivism reduction among homeless parolees: outcomes and cost analysis. Journal of Experimental Criminology. 2016;12(1):49–74. doi: 10.1007/s11292-015-9236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Poulos R.G., Ferson M.J., Orr K.J., McCarthy M.A., Botham S.J., Stern J.M., et al. Vaccination against hepatitis A and B in persons subject to homelessness in inner Sydney: vaccine acceptance, completion rates and immunogenicity. Aust N Z J Public Health. 2010;34(2):130–135. doi: 10.1111/j.1753-6405.2010.00496.x. [DOI] [PubMed] [Google Scholar]
- 48.Schwarz K., Garrett B., Lee J., Thompson D., Thiel T., Alter M.J., et al. Positive impact of a shelter-based hepatitis B vaccine program in homeless Baltimore children and adolescents. Journal of Urban Health. 2008;85(2):228–238. doi: 10.1007/s11524-008-9253-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steele R.W., Ramgoolam A., Evans J., Jr Health services for homeless adolescents. Seminars in Pediatric Infectious Diseases. 2003;14(1):38–42. doi: 10.1053/spid.2003.127216. [DOI] [PubMed] [Google Scholar]
- 50.Tjon G.M.S., Götz H., Koek A.G., de Zwart O., Mertens P.L.J.M., Coutinho R.A., et al. An outbreak of hepatitis A among homeless drug users in Rotterdam, The Netherlands. J Med Virol. 2005;77(3):360–366. doi: 10.1002/jmv.20464. [DOI] [PubMed] [Google Scholar]
- 51.Washington-Brown L., Cirilo R.W. Advancing the health of homeless populations through vaccinations. Journal of the American Association of Nurse Practitioners. 2020 doi: 10.1097/JXX.0000000000000509. [DOI] [PubMed] [Google Scholar]
- 52.Zhang S.X., Shoptaw S., Reback C.J., Yadav K., Nyamathi A.M. Cost-effective way to reduce stimulant-abuse among gay/bisexual men and transgender women: a randomized clinical trial with a cost comparison. Public Health. 2018;154:151–160. doi: 10.1016/j.puhe.2017.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wright N.M.J., Campbell T.L., Tompkins C.N.E. Comparison of conventional and accelerated hepatitis B immunisation schedules for homeless drug users. Communicable disease and public health. 2002;5(4):324–326. [PubMed] [Google Scholar]
- 54.Brown S., Fisher E., Taylor A., Neuzil K., Trump S., Sack D., et al. Influenza vaccine community outreach: Leveraging an interprofessional healthcare student workforce to immunise marginalised populations. Prev Med. 2021;147 doi: 10.1016/j.ypmed.2021.106460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vlahov D., Coady M.H., Ompad D.C., Galea S. Strategies for improving influenza immunization rates among hard-to-reach populations. Journal of Urban Health. 2007;84(4):615–631. doi: 10.1007/s11524-007-9197-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sneller V.-P., Fishbein D.B., Weinbaum C.M., Lombard A., Murray P., McLaurin J.A., et al. Vaccinating adolescents in high-risk settings: lessons learned from experiences with hepatitis B vaccine. Pediatrics. 2008;121(Supplement_1):S55–S62. doi: 10.1542/peds.2007-1115G. [DOI] [PubMed] [Google Scholar]
- 57.Centres for Disease Control and Prevention. COVID-19 vaccination for people experiencing homelessness: Frequently asked questions 2021 [Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/homeless-shelters/vaccine-faqs.html.
- 58.Crowe L. Medical-surgical nurses' attitudes towards patients who are homeless: How attitudes develop and transform 2012 [Available from: https://scholarworks.gsu.edu/cgi/viewcontent.cgi?article=1031&context=nursing_diss.
- 59.Parkinson R. Nurses' attitudes towards people who are homeless: A literature review. Diversity and Equality in Health Care 2009;6.
- 60.Longchamps C, Ducarroz S, Crouzet S, Vignier N, Pourtau L, Allaire C, et al. COVID-19 vaccine hesitancy among persons living in homeless shelters in France. Vaccine. 2021. [DOI] [PMC free article] [PubMed]
- 61.Hsu H., Petering R., Onasch-Vera L. Implications of COVID-19 vaccine uptake among young adults experiencing homelessness: A brief report. J Social Distress Homeless. 2021 [Google Scholar]
- 62.Iacoella C., Ralli M., Maggiolini A., Arcangeli A., Ercoli L. Acceptance of COVID-19 vaccine among persons experiencing homelessness in the City of Rome, Italy. Eur Rev Med Pharmacol Sci. 2021;25:3132–3135. doi: 10.26355/eurrev_202104_25568. [DOI] [PubMed] [Google Scholar]
- 63.DeRoo S., Pudalov N., Fu L. Planning for a COVID-19 vaccination program. J Am Med Assoc. 2020;323(24):2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 64.Walkey A.J., Law A., Bosch N.A. Lottery-based incentive in Ohio and COVID-19 vaccination rates. JAMA. 2021;326(8):766. doi: 10.1001/jama.2021.11048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Higgins S.T., Klemperer E.M., Coleman S.R.M. Looking to the empirical literature on the potential for financial incentives to enhance adherence with COVID-19 vaccination. Prev Med. 2021;145:106421. doi: 10.1016/j.ypmed.2021.106421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kreps S., Dasgupta N., Brownstein J.S., Hswen Y., Kriner D.L. Public attitudes toward COVID-19 vaccination: The role of vaccine attributes, incentives, and misinformation. npj Vaccines. 2021;6(1) doi: 10.1038/s41541-021-00335-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith R. Interventions to increase vaccination rates in homeless adults aged 50 years and older in a shelter-based clinic 2016 [Available from: https://athenaeum.uiw.edu/cgi/viewcontent.cgi?article=1008&context=uiw_dnp.
- 68.Lewis J.H., Whelihan K., Roy D., White E.J., Morgan C., Vora R.S., et al. Vaccination capability inventory of community, migrant, and homeless health centers: A survey report. J Public Health Management Practice. 2020;26(2):139–147. doi: 10.1097/PHH.0000000000001073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nyamathi A., Koniak-Griffin D., Tallen L., González-Figueroa E., Levson L., Mosley Y., et al. Use of community-based participatory research in preparing low income and homeless minority populations for future HIV vaccines. J Interprof Care. 2004;18(4):369–380. doi: 10.1080/13561820400011735. [DOI] [PubMed] [Google Scholar]
- 70.Australian Government - Department of Health. What is immunisation? 2018 [Available from: https://www.health.gov.au/health-topics/immunisation/about-immunisation/what-is-immunisation#:∼:text=unimmunised%20person%27s%20recovery.-,Immunisation%20or%20vaccination%20%E2%80%94%20what%27s%20the%20difference%3F,the%20disease%20as%20a%20result.