In November 2021, a new SARS-CoV-2 variant emerged in South Africa and was designated the fifth variant of concern and named Omicron. It was detected in more than 26 countries worldwide, including China. The Omicron variant is highly transmissible and has extensive morbidity, which has raised concerns related to antiviral therapy. Recent reports have revealed that the Omicron variant exhibits a longer cycle of viral shedding and a decreased replication capacity and results in substantially attenuated lung pathology, indicating that the pathogenic ability of the Omicron variant is lower than that of previous variants.1 Omicron has the largest number (>30) of substitutions, deletions, or insertions, with a mutation frequency of higher than 1% in the spike (S) protein. Mutation studies of the spike protein receptor-binding domain have provided a plausible explanation for the increased transmissibility and antibody resistance of this variant. However, the molecular basis for its attenuated pathogenicity and replication capacity remains elusive. The envelope protein of SARS-CoV-2 (2-E) forms a homopentameric cation channel that is important for viral pathogenicity.2 Our previous study demonstrated that the 2-E channel alone is sufficient to induce cell death, provoke a cytokine storm, and even cause acute respiratory distress syndrome-like damage in vivo.2 A channel inhibitor was found to exhibit excellent antiviral activity in vivo.2 Here, we focus on mutations in the 2-E channel, one of the most enigmatic and least studied structural proteins.
Four high-quality E protein sequences of Omicron variants (BA.1, BA.1.1, BA.2, and BA.3; https://cov-lineages.org/index.html) in the CNCB database as of April 9th, 2022, were comprehensively analyzed, and the mutation 2-ET9I (T9I, threonine to isoleucine) caught our attention. Among the more than 100 identified 2-E mutations in the Omicron variant compared with the original Wuhan reference strain, T9I shows a much higher frequency than the rest of the mutations. In addition, the allele frequency of T9I in all statistical samples was higher than 99.49%. In Omicron strain BA.3, the allele frequency was found to increase to 100.00% (Figures 1A and 1B). According to the solved NMR structure, T9 is located at the top of the transmembrane domain of the 2-E protein.3 The influences of T9I have not yet been studied.
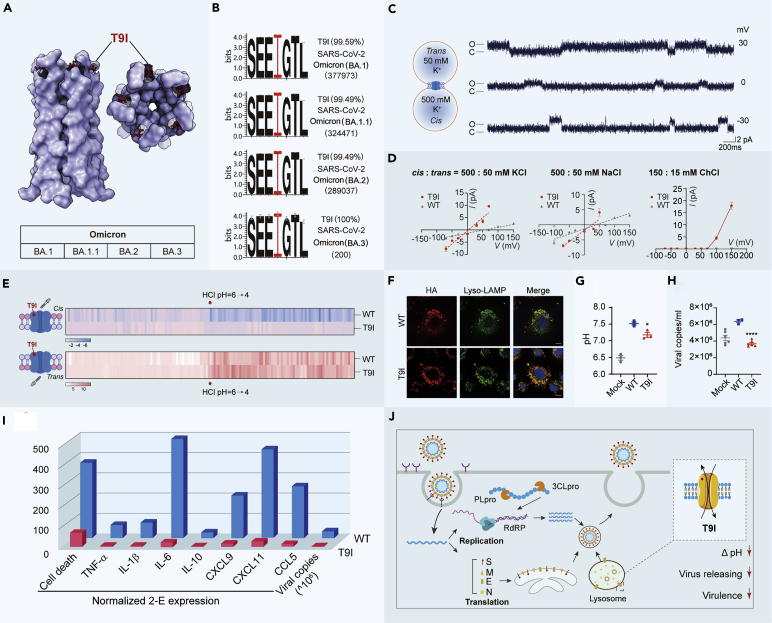
Figure 1.
The single point mutation T9I in the envelope protein of the SARS-CoV-2 Omicron variant changes channel properties and attenuates virus production and virulence
(A) Structure of the 2-E transmembrane domain.3
(B) Amino acid sequence logo of the SARS-CoV-2 Omicron variant 2-E protein. The I9 residues are marked in red.
(C) Single-channel current recording of T9I after reconstitution in lipid bilayers with PC:PS = 3:2 at the indicated potentials and in the indicated solutions.
(D) I-V curves of T9I in asymmetric potassium chloride, sodium chloride, and choline chloride solutions (n ≥ 3).
(E) Single-channel current recording in 500:500 mM KCl solutions with proton titration resulting in different pH values (cis or trans). The red arrows represent titration with HCl. The heatmap shows the transition of the currents under proton titration.
(F) Cellular immunofluorescence staining of WT or T9I (red) and the lysosome marker LAMP (green). Both WT and T9I are colocalized with lysosomes.
(G) The lysosomal pH in Vero E6 cells transfected with WT, T9I, or Mock plasmids. ∗p < 0.05; ∗∗p < 0.01; ∗∗∗p < 0.001;∗∗∗∗p < 0.0001; unpaired Student’s t test. All error bars are SEM.
(H) Viral copies in the supernatant were determined by qRT-PCR. The MOI of SARS-CoV-2 was 0.01. ∗p < 0.05; ∗∗p < 0.01; ∗∗∗p < 0.001;∗∗∗∗p < 0.0001; unpaired Student’s t test. All error bars are SEM.
(I) The influences of the T9I mutation on cell death and cytokine production (normalized to the 2-E expression level), as well as viral production.
(J) Life cycle diagram of the SARS-CoV-2 Omicron variant. T9I in the envelope protein of Omicron results in the formation of a nonselective ion channel, accompanied by attenuated virulence and viral production.
Whether T9I retains channel activity was investigated. We purified the T9I protein and reconstituted the protein on a planar lipid bilayer membrane (BLM) as previously described.2 The observed T9I-induced typical single-channel currents supported the hypothesis that T9I is also able to form ion channels as the wild-type (WT) 2-E protein does (Figure 1C).2 However, the reversal potential of the T9I channels was shifted to the left, from 57 mV to 3 mV, in an asymmetric KCl solution. Similar shifting of the reversal potential was also detected in an asymmetric NaCl solution (Figure 1D). The reversal potential of close to 0 mV suggests that T9I may have lost its cation selectivity. To determine whether T9I is permeable to chloride, the channel activity of T9I was further examined in an asymmetric 15:150 mM (trans:cis) choline chloride solution. Most cation channels are impermeable to quaternary ammonium choline, and it is thus always used to detect anion permeability. As expected, outward currents were indeed observed when the holding voltage potentials were higher than the theoretical reversal potential for chloride (Erev> 70 mV) (Figure 1D). These results revealed that the ion selectivity of T9I mutant channels is different from that of WT channels.
WT 2-E channels are pH sensitive.2 The influences of pH on T9I channels were evaluated with the same channels using a titration strategy. After the channels were incorporated into membranes, hydrochloric acid (HCl) was titrated into either the cis or trans side to alter the pH to 4 from 6. Consistent with our previous results, a reduction in pH on either the cis or trans side induced a significant increase in the amplitude and open probability of WT channels.2 In contrast, a reduction in pH on the cis side failed to increase the channel activity of T9I channels (Figure 1E). Although we did not have direct evidence to explain how the threonine (T9) site is sensitive to pH changes, the structure of 2-E channels supported the hypothesis that the residues (Glu7 and Glu8) around T9 were sensitive to pH changes and that their side-chain carboxyl could be deprotonated at neutral pH and protonated at acidic pH.3 It has been reported that SARS-CoV-2 traffics to lysosomes for egress by lysosomal deacidification instead of via the classical biosynthetic secretory pathway.4 The envelope (E) protein channels of coronavirus are localized in intracellular organelles.4 The cellular localization of WT and T9I was assessed using immunocytochemistry and confocal microscopy. We found that both WT and T9I were colocalized with the lysosomal marker LAMP (Figure 1F). Given the localization on lysosomes, the influence of WT and T9I on the luminal pH of lysosomes was compared. Flow cytometry was used to analyze the fluorescence intensity ratio of the pH probe (pHluorin). This pH probe consists of a green fluorescent protein pHluorin molecule fused to the lysosome-resident protein CD63. Expression of WT channels robustly neutralized the lysosomal pH, whereas T9I channels exhibited less influence on the luminal pH, consistent with our electrophysiological findings (Figure 1G). Therefore, the deacidification capability of 2-E channels in lysosomes was significantly impeded by the T9I mutation. Based on the above findings, whether the weakened deacidification capability hampers virus production was examined. We transfected Vero E6 cells with WT or T9I plasmids on day 1 and then infected the cells with SARS-CoV-2 on day 2. As determined by qRT-PCR, compared with exogenous expression of the WT protein, exogenous expression of the T9I mutant significantly attenuated the viral load (Figure 1H). It was logical to deduce that some exogenous T9I subunits would coassemble with the WT subunits originating from the virus and form heteromultimers with impaired pH sensitivity, resulting in reduced deacidification of lysosomes and reduced SARS-CoV-2 production.
Finally, the channel activity of the 2-E protein is a virulence determinant. We used Annexin V/PI staining to evaluate the cell lethality of T9I in Vero E6 cells. We found that although the expression level of T9I far exceeded the expression level of WT, it caused cell death similar to that caused by WT (Figure 1I). Similarly, in the mouse macrophage cell line (RAW264.7), much greater expression of T9I induced increases in inflammatory cytokines comparable to those induced by WT (Figure 1I). The correlation between the cell lethality and the expression level was further compared. As shown in Figure 1I, in comparison with that of WT, the cytotoxic ability of T9I was approximately 150-fold lower, as was cytokine production. Notably, according to another recent study, 2-E expression in an Omicron variant was decreased approximately 3-fold, which may further suppress the virulence of Omicron variants. The degree to which the weakened abilities to kill cells and induce cytokine production result in the milder clinical symptoms of Omicron warrants further investigation.
Overall, as SARS-CoV-2 infections are ongoing, there is the chance that the virus will accumulate new mutations. Among the existing antiviral targets—in contrast to the S protein, RNA-dependent RNA polymerase, and 3C-like protease, which mediate viral entry, viral replication, and protein cleavage, respectively—the E protein primarily participates in viral release. Here, we report for the first time that the high-frequency mutation T9I in 2-E of the SARS-CoV-2 Omicron variant results in the formation of a nonselective ion channel with reduced acid sensitivity compared to WT channels. In addition, T9I decreased cell death and weakened cytokine production. These changes in channel properties might be responsible for the less efficient release and lower level of induced cell damage of the Omicron variant (Figure 1J). We speculated that, in comparison with those of WT channels, the reduced potassium efflux and additional chloride influx mediated by T9I channels would cause less severe ionic dyshomeostasis, membrane disruption, and lysosome-related cell death.
Viruses may evolve to be less virulent to spare their hosts.5 Before the emergence of Omicron variants, the T9I mutation was found in the E proteins of other SARS-CoV-2 variants, including Alpha, Beta, Gamma, and Delta. The prevalence frequency of T9I in these variants was less than 0.20%. We speculated that the T9I mutation may have originated in these previous variants and been retained through evolutionary screening, perhaps due to the reduced virulence of the affected strains. Notably, in the most recently emerged Omicron XE strain, a BA.1/BA.2 recombinant, T9I was retained and is the only mutation identified in its E protein. However, we cannot exclude the possibility that the origin of T9I is just a coincidence, as may be the milder severity of Omicron.
One limitation of our study is the lack of evidence in the context of infection with this single-mutation SARS-CoV-2 strain in vivo, which can technically be achieved by generating a SARS-CoV-2 single mutant using reverse genetics. Considering the urgency of the COVID-19 pandemic and the lack of resources in P3 labs, we are very eager to share our discoveries. Overall, our study provides valuable insights into key features of the Omicron variant and critical information for the evolution of COVID-19.
Acknowledgments
We are grateful to the National Science Fund of Distinguished Young Scholars (81825021), the Fund of Youth Innovation Promotion Association (2019285), the National Natural Science Foundation of China (81773707, 92169202), the Lingang Lab (LG202101-01-04), the National Key Research and Development Program of China (2020YFC0842000), the project supported by the Shanghai Municipal Science and Technology Major Project (Grant Nos. 2018SHZDZX05, TZX022021002), and the Fund of Shanghai Science and Technology Innovation Action Plan (20ZR1474200).
Declaration of interests
The authors declare no competing interests.
Published Online: April 26, 2022
Contributor Information
Bingqing Xia, Email: xiabingqing@simm.ac.cn.
Zhaobing Gao, Email: zbgao@simm.ac.cn.
References
- 1.Shuai H., Chai Y., Yuen T.T.T., et al. Attenuated replication and pathogenicity of SARS-CoV-2 B.1.1.529 Omicron. Nature. 2022;603:693–699. doi: 10.1038/s41586-022-04442-5. [DOI] [PubMed] [Google Scholar]
- 2.Xia B., Shen X., He Y., et al. SARS-CoV-2 envelope protein causes acute respiratory distress syndrome (ARDS)-like pathological damages and constitutes an antiviral target. Cell Res. 2021;31:847–860. doi: 10.1038/s41422-021-00519-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mandala V.S., McKay M.J., Shcherbakov A.A., et al. Structure and drug binding of the SARS-CoV-2 envelope protein transmembrane domain in lipid bilayers. Nat. Struct. Mol. Biol. 2020;27:1202–1208. doi: 10.1038/s41594-020-00536-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghosh S., Dellibovi-Ragheb T.A., Kerviel A., et al. β-Coronaviruses use lysosomes for egress instead of the biosynthetic secretory pathway. Cell. 2020;183:1520–1535.e14. doi: 10.1016/j.cell.2020.10.039. e1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Markov P.V., Katzourakis A., Stilianakis N.I. Antigenic evolution will lead to new SARS-CoV-2 variants with unpredictable severity. Nat. Rev. Microbiol. 2022;20:251–252. doi: 10.1038/s41579-022-00722-z. [DOI] [PMC free article] [PubMed] [Google Scholar]