Abstract
Hymen imperforation is uncommon. Symptoms include primary amenorrhea, cyclical lower abdominal pain, and rarely a pelvic mass syndrome. Delayed discovery may lead to endometriosis and infertility. Pelvic ultrasound and nuclear magnetic resonance detect associated genito‐urinary malformations. Hymenectomy is the standard surgical treatment.
Keywords: genito‐urinary malformations, hematocolpos, hymen, ultrasound – MRI
Hymen imperforation is uncommon. Symptoms include primary amenorrhea, a bulging perineal mass, cyclical abdominal pain, and urinary retention or infections. Clinical awareness allows an opportune diagnosis, thus preventing complications.

1. INTRODUCTION
A 16‐year‐old female patient presented with amenorrhea, and cyclical abdominal pain. Secondary sexual characters were well‐developed, and a lower abdominal mass was palpable. Abdomino‐pelvic ultrasound revealed a complex fluid‐filled retrovesical mass. Pelvic MRI demonstrated a 150 × 95 × 95 mm hematocolpos, with no associated genito‐urinary or ano‐rectal malformations (Figure 1). A hematocolpos secondary to imperforate hymen was diagnosed.
FIGURE 1.
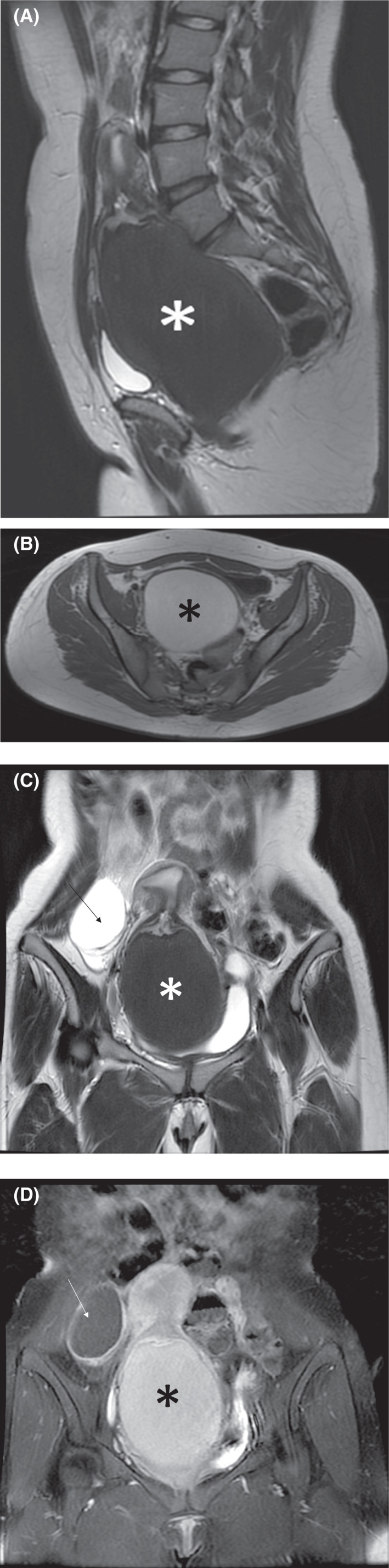
Pelvic MRI demonstrating hematocolpos secondary to imperforate hymen associated with an Orads 3 right ovarian cyst. Sagittal T2 (A) and axial T1 (B) images show T2 hyperintense (*) T1 hypointense (*) fluid distending the vaginal cavity but not involving the uterus measuring 150 × 95 × 95 mm. Coronal T2 (C) and T1 fat‐saturated and gadolinium‐enhanced (D) images show the hematocolpos (*) associated with a right ovarian cyst with smooth central septae and wall enhancement (Thin arrow) measuring 60 × 43 mm
Imperforate hymen is the most prevalent female genital tract obstructive congenital abnormality. The incidence varies between 0.01% and 0.05%. The hymen is a composite of vaginal and urogenital sinus epithelium. The imperforate hymen results from unsuccessful canalization of the vaginal plate and results in the entrapment of vaginal and uterine secretions.
Clinical presentations range from incidental, to primary amenorrhea, cyclical abdominal pain, lower abdominal mass with a protruding bluish hymen, urinary retention or infections, or acute renal injury. Diagnosis is made after menarche due to hematocolpos. 1
Retarded diagnosis complications include retrograde menstruation and ruptured hematosalpinx, endometriosis, pyocolpos, and infertility.
Given its rarity, imperforate hymen can be missed. A thorough physical examination is essential. Pelvic Ultrasound and MRI show hematometrocolpos thus confirming the diagnosis, and unmask associated malformations or complications. Hymenectomy is performed for drainage. 2 Timely diagnosis and management prevent complications and preserve future fertility.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
HR, HEN, and JEF contributed to conception, acquisition, analysis, interpretation of data, and drafted the manuscript. FZB, MJ, OZ, and MD critically revised the manuscript. All the authors have read and approved the final draft of the manuscript.
ETHICAL APPROVAL
Ethical approval is not required for de‐identified single case reports based on institutional policies.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
None.
Ramdani H, Benbrahim FZ, Jidal M, et al. Primary amenorrhea secondary to imperforate hymen. Clin Case Rep. 2022;10:e05786. doi: 10.1002/ccr3.5786
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
REFERENCES
- 1. Lui CT, Chan TWT, Fung HT, et al. A retrospective study on imperforate hymen and haematometrocolpos in a regional hospital. Hong Kong J Emerg Med. 2010;17:435‐440. [Google Scholar]
- 2. Ramareddy RS, Kumar A, Alladi A. Imperforate hymen: varied presentation, new associations, and management. J Indian Assoc Pediatr Surg. 2017;22(4):207‐210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.


