Abstract
The chronic nature of inflammatory bowel disease (IBD) creates a lifelong impact on the morbidity of children affected by the disease. The ability to confidently identify and characterize complications resulting from IBD in the pediatric patient is of critical importance. Magnetic resonance enterography (MRE) is especially valuable in the diagnostic assessment of IBD. However, precise elucidation of complications including strictures can be difficult with standard MRE sequences. The recent development of faster MRI pulse sequences provides rapid, real-time imaging of the intestinal tract. In this review, we describe how the addition of cine MRE confidently pinpoints areas of stricture, aids in lesion detection and diagnosis, and provides valuable information on intestinal motility.
Keywords: MR Enterography, CINE MRI, inflammatory bowel disease, IBD Complications, diagnosis, stricture, motility, steady state free precession
INTRODUCTION
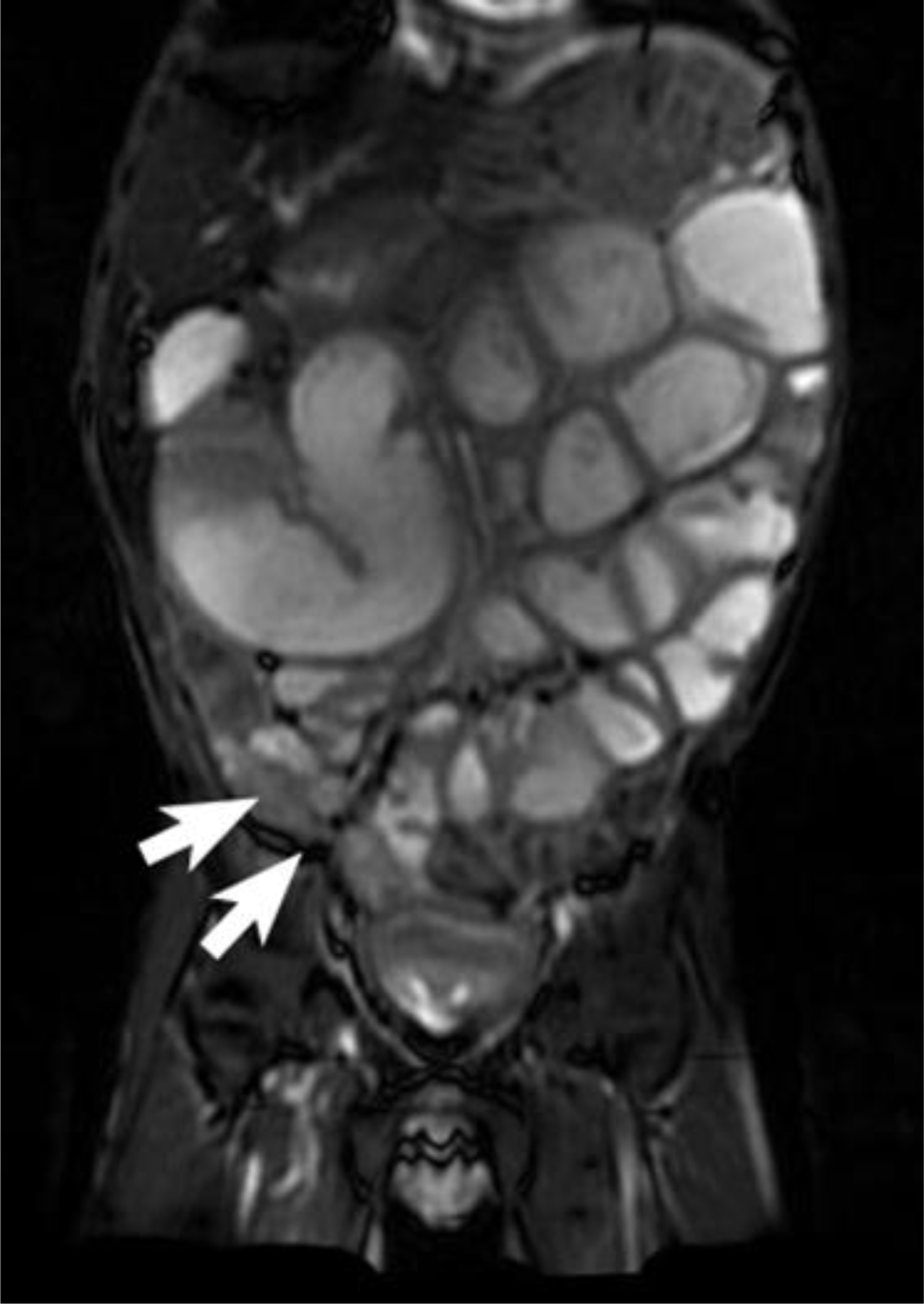
In the pediatric patient, IBD and resultant complications can be challenging to assess both from clinical and imaging perspectives. MRE offers substantial information on both intraluminal and extraluminal pathology without radiation exposure [1] [2] [FIGURE 1]. Imaging of strictures with standard MRE sequences can be challenging, since routine MRE captures images of the bowel frozen at one moment in time. This snapshot of the bowel makes it challenging to distinguish between a transient contracted segment during bowel peristalsis and a true stricture [FIGURE 2A and 2B]. However, the recent development of faster MRI pulse sequences provides a unique opportunity to provide more information.
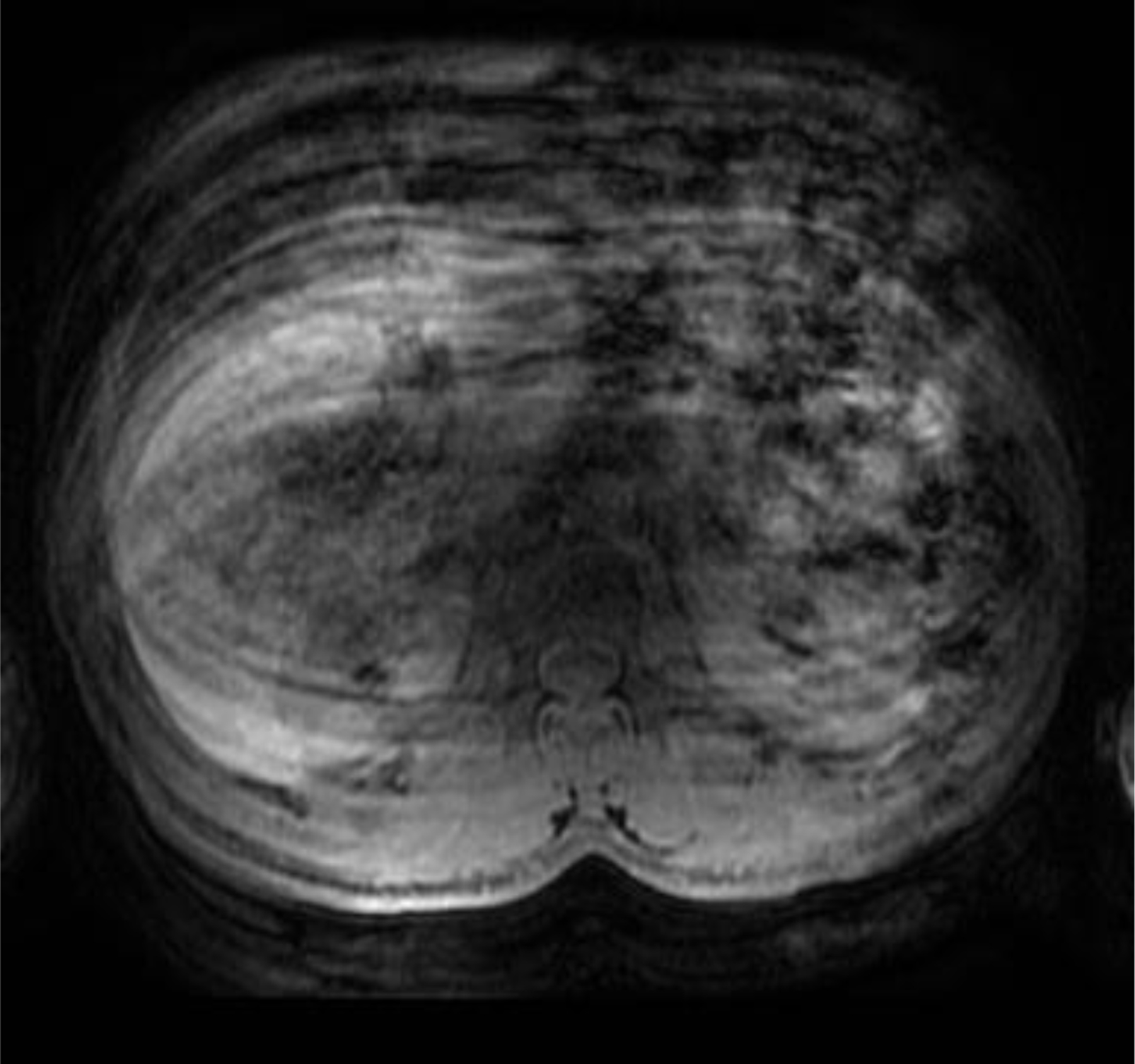
FIGURE 1:
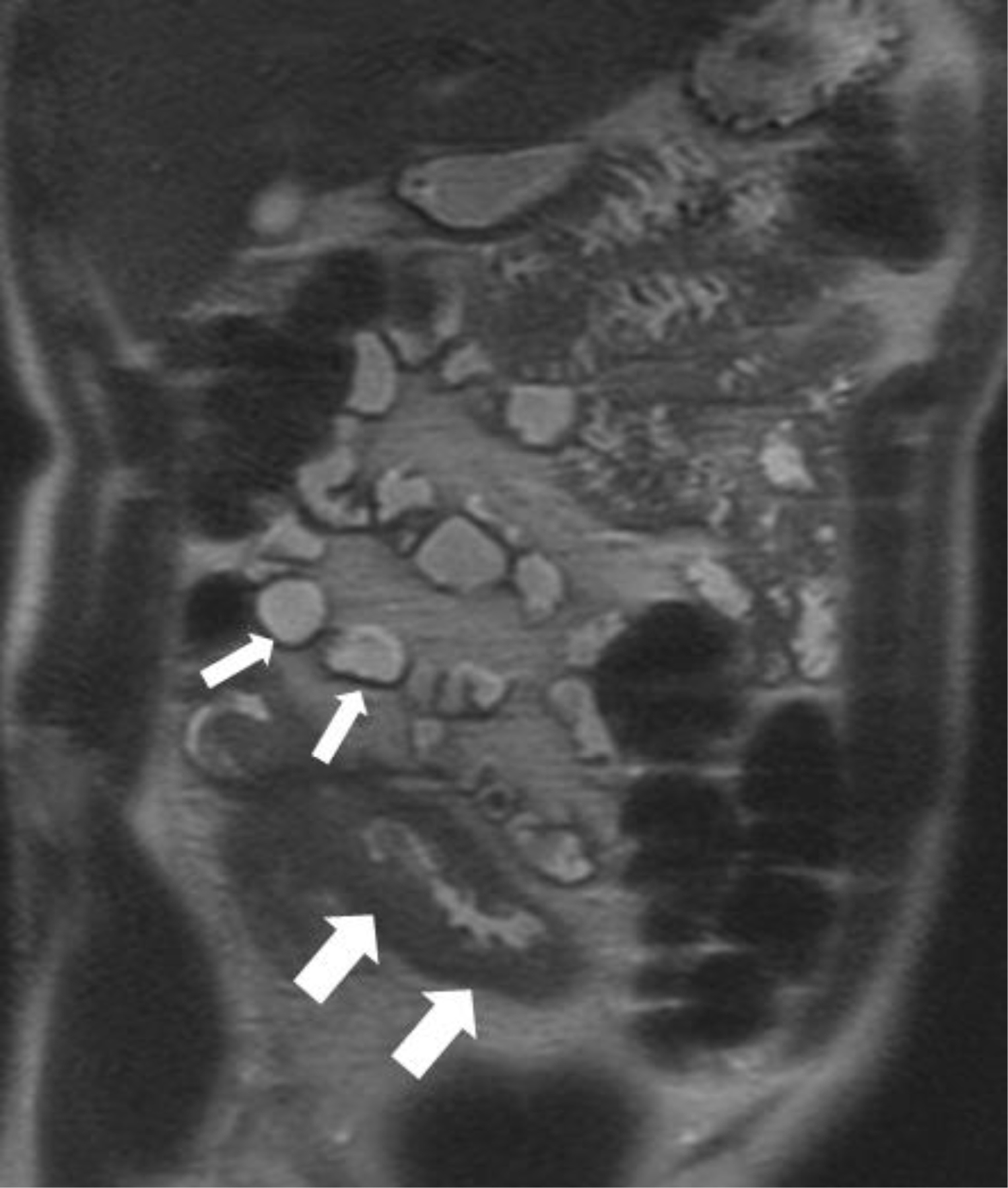
Coronal T2 weighted image in a patient with history of Crohn’s disease demonstrating marked thickening of the terminal ileum (thick white arrows). Normal, unaffected loops of intestine with normal wall thickness (thin white arrows) can also be seen.
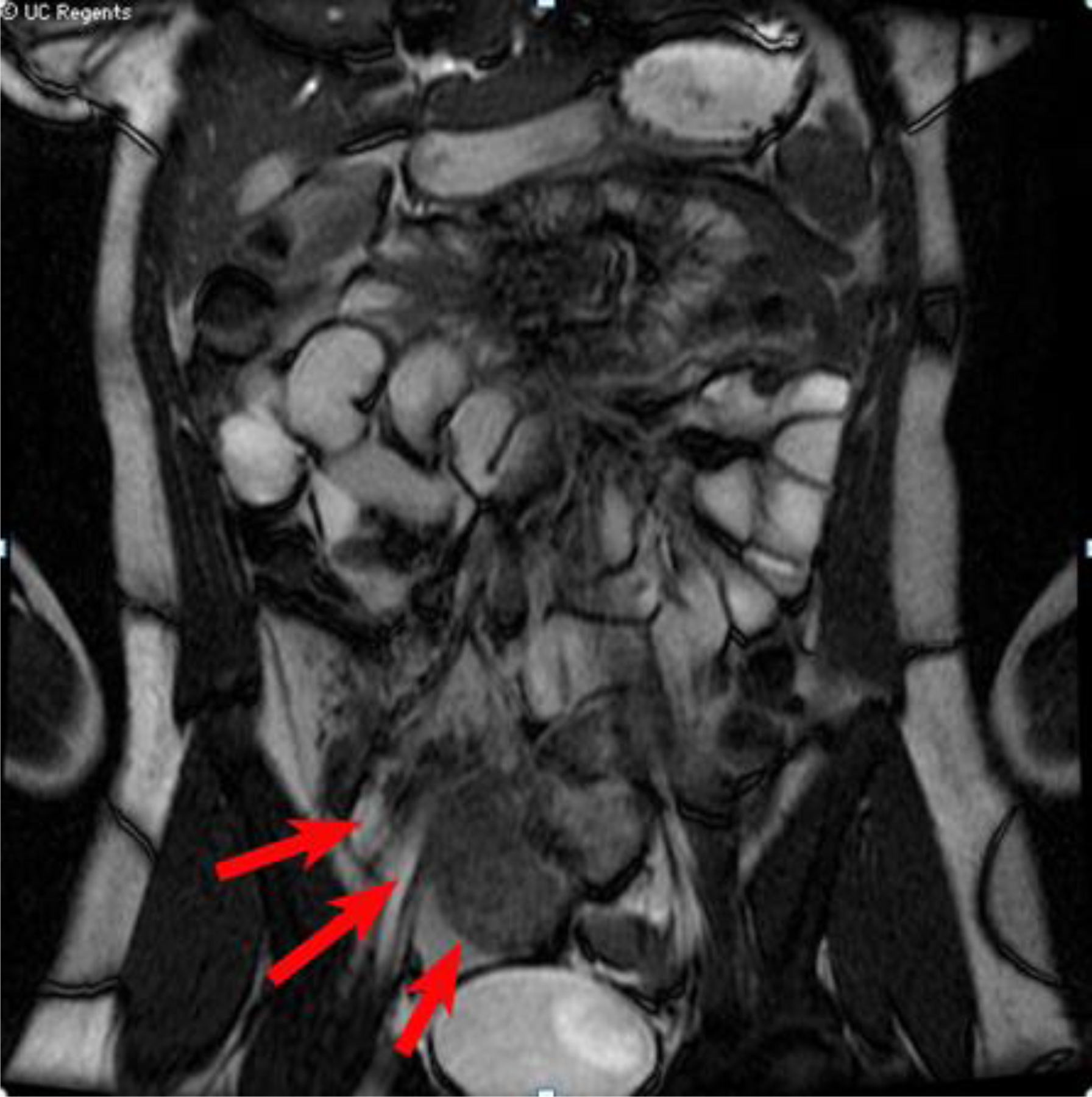
FIGURE 2A:

Coronal SSFP image from an MRE in a 15 year old patient with suspected Crohn’s disease. An area of narrowing is seen in the proximal jejunum (black arrows) and more distally in the proximal ileum (white arrows).
FIGURE 2B:
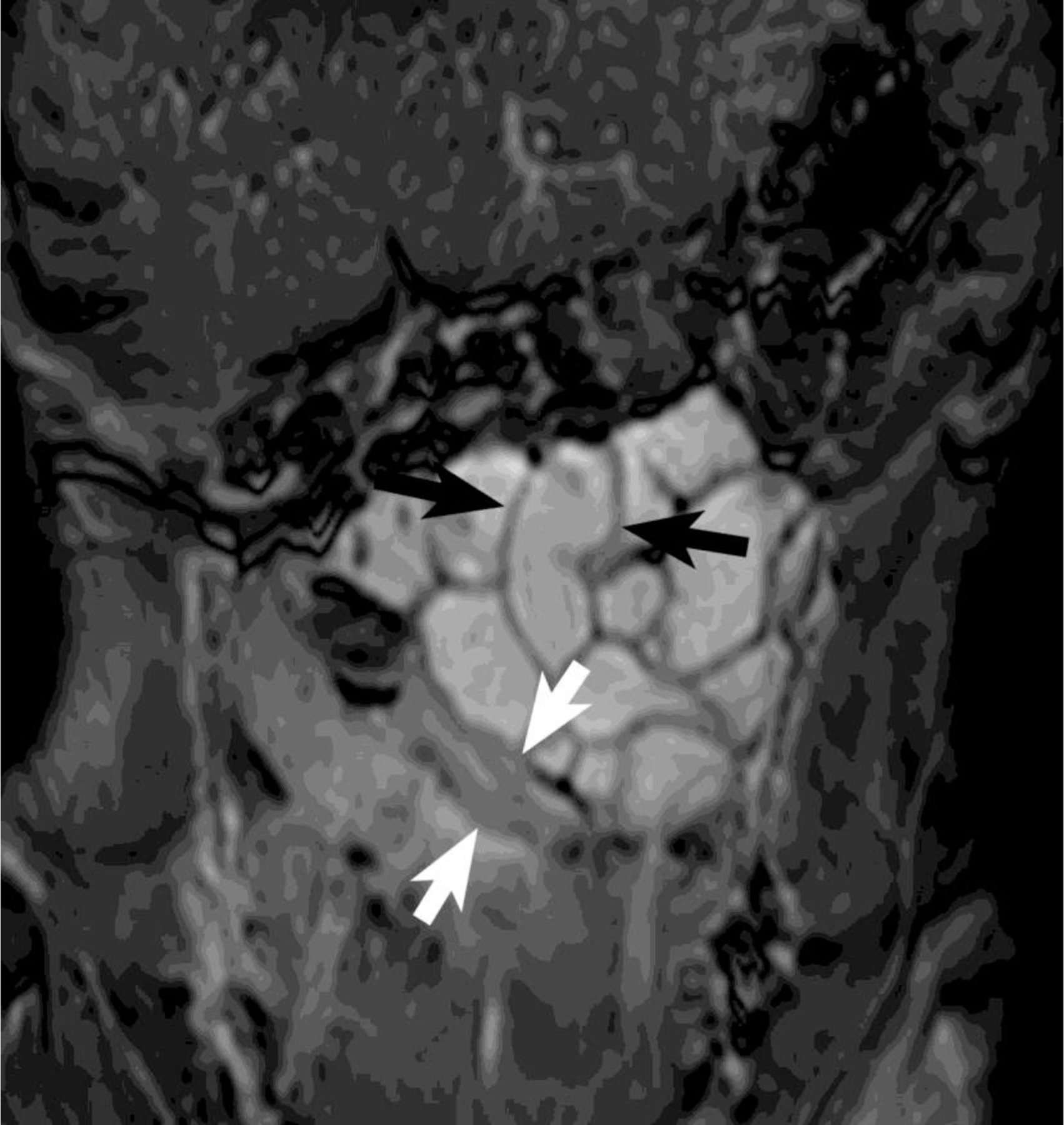
Coronal SSFP image (obtained seconds after image 2A). Prior area of narrowing in the proximal jejunum (black arrows) has opened. The more distal focus of narrowing, however, persists, compatible with a true stricture.
One type of faster MR imaging relies on steady state free precession (SSFP) to create a movie of cine images. SSFP sequences use a combination of balanced magnetic field gradients and radiofrequency excitation to acquire images rapidly with high spatial resolution and high signal-to-noise ratio. In addition to gastrointestinal imaging applications described here, SSFP is used for dynamic imaging of the cardiovascular system, angiographic imaging without intravenous contrast, and high resolution imaging of nerves within cerebrospinal fluid. SSFP requires high-performance MR hardware capable of rapidly applying gradients and radio frequency pulses. Most current MRI devices are capable of running this pulse sequence. The major limitations of this sequence are sensitivity to imperfections in the MRI magnetic field and flow within tissues. Additionally, SSFP has complicated T1- and T2- contrast and is not optimal for detecting subtle lesions in solid organs such as the liver [3].
Cine imaging confers the ability to observe the motion of intestinal segments over a relatively short period and in real-time [4]. Intestinal motility may be sampled at regular intervals over approximately 30 seconds [FIGURE 3]. Frame rates using cine imaging are typically around 10–20 images per second which is close to the frame rate of home movies at 30 frames per second.
FIGURE 3.
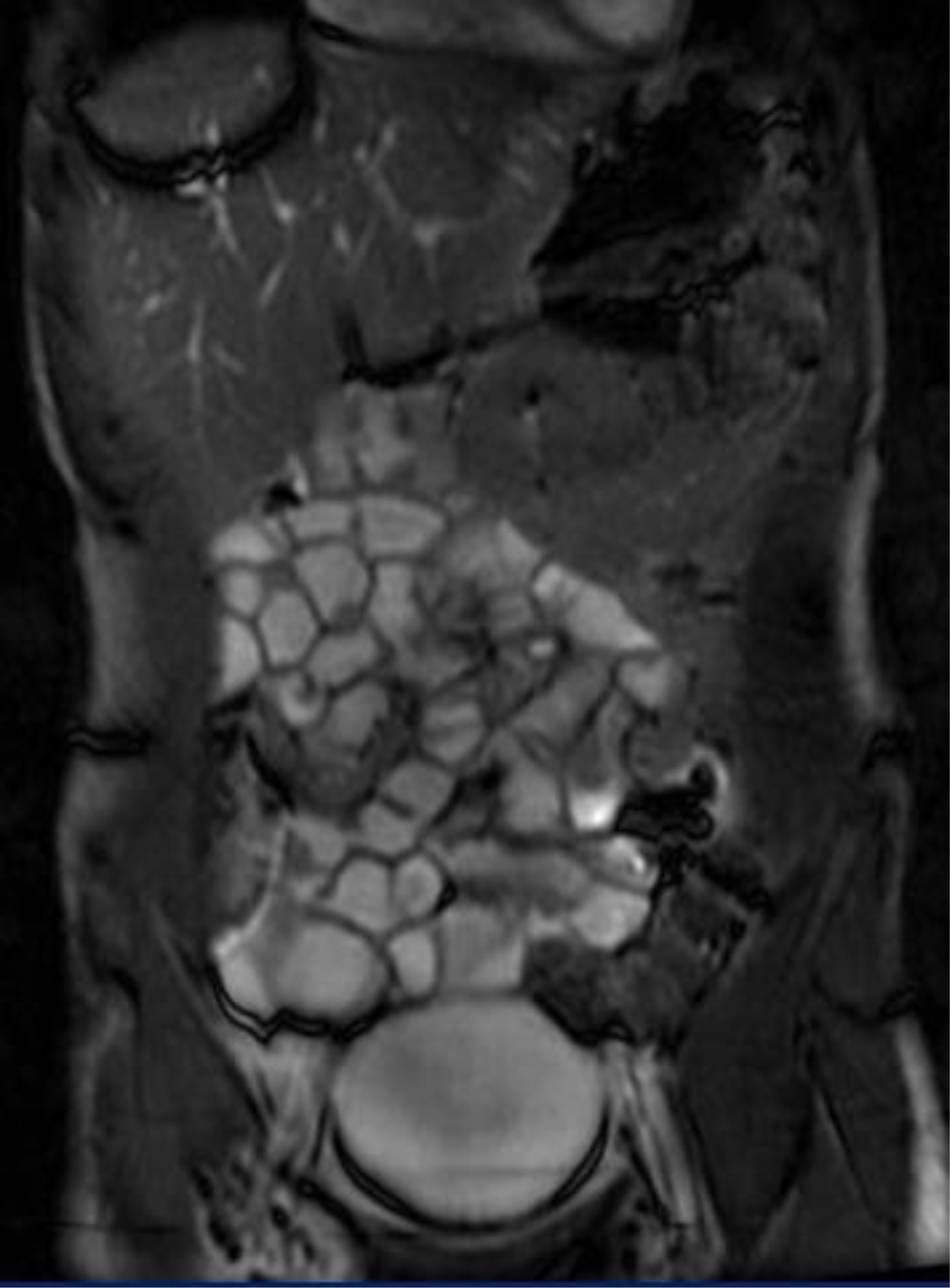
[STILL IMAGE PLACEHOLDER FOR CINE]: Coronal cine SSFP sequence in a patient referred for clinically suspected Crohn’s disease shows optimal opacification of the small intestine. Normal small intestinal motility is observed in the images of this patient.
Real-time imaging allows for confirmation of intestinal strictures, quantitative assessment of overall bowel motility [4, 5], and delineation of disease activity [6]. This review describes the potential utility of cine MRE with SSFP imaging for depicting bowel pathology in pediatric patients with IBD. Several cases are presented that illustrate the MRE technique of cine imaging and suggest clinical scenarios where cine imaging may provide additional information which may be helpful in the workup of patients with clinical suspicion for IBD.
TECHNIQUE
MRE is an increasingly important non-invasive diagnostic tool in the evaluation of patients with IBD [1, 2]. Once a dedicated protocol has been implemented, this radiation-free test is relatively straightforward to perform and interpret. For a standard MRE study, two types of contrast media are given to the patient: oral contrast to distend the small intestinal lumen and IV gadolinium contrast to depict signs of mucosal inflammation, fluid collections, and fistula tracts. We administer VoLumen (Bracco Diagnostics, Princeton, NJ) oral contrast with flavor crystal additives at 60 and 20 minutes prior to beginning the exam. Total amount of contrast is titrated by weight at 20 mL of oral contrast per kilogram. T1 and T2-weighted sequences in multiple imaging planes also provide information about the abdomino-pelvic viscera, lymph nodes, and abdominal vasculature. Patients also receive intravenous gadolinium for evaluation of areas of enhancement in active inflammation and to delineate abscess formation.
Incorporation of cine SSFP sequences into an MRE protocol requires additional considerations. The workflow is best optimized if this sequence performed as the final sequence of the examination, since the large volume of data obtained requires a substantial amount of computer processing and may prevent the acquisition of additional images until these data are processed (approximately 5–10 minutes). Some centers incorporate the administration of intravenous glucagon to attempt to reduce peristalsis and intestinal motion artifact. However, in our experience we have observed good performance without the need for this antiperistaltic agent. Cine sequences, therefore, should be obtained prior to the administration of glucagon in these protocols.
CONSIDERATIONS FOR 1.5 VS 3.0 TESLA IMAGING
The field strength of the MRI magnet will affect the rate at which images may be obtained and the magnitude of banding artifacts that potentially degrade image quality. For 1.5 Tesla (T) systems, the MRI technologist selects 5–7 representative coronal slices of the abdomen using the sagittal localizer image. Each slice is obtained over a 30 second period with a total of 50 images obtained over that time period (50 phases per location). Using newer 3.0T systems, it is possible to obtain up to 110 images per location over the same 30-second time period. An additional consideration for 3T imaging is the presence of “banding” artifact which is inherent to the SSFP sequence [FIGURE 4]. This artifact is more pronounced at 3T, particularly at air/soft tissue interfaces. In our experience, adequate small intestinal distention with oral contrast material mitigates this artifact.
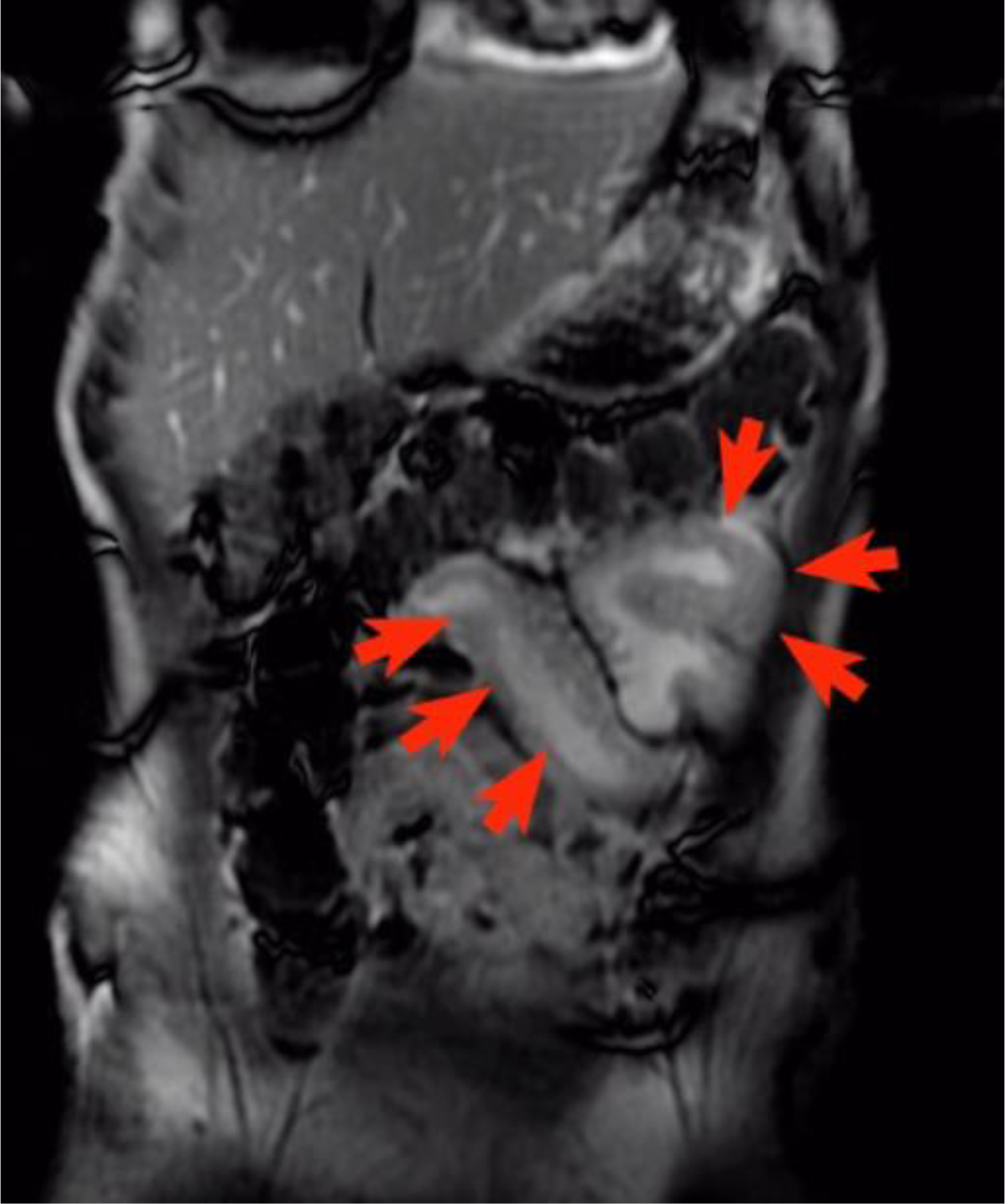
FIGURE 4:
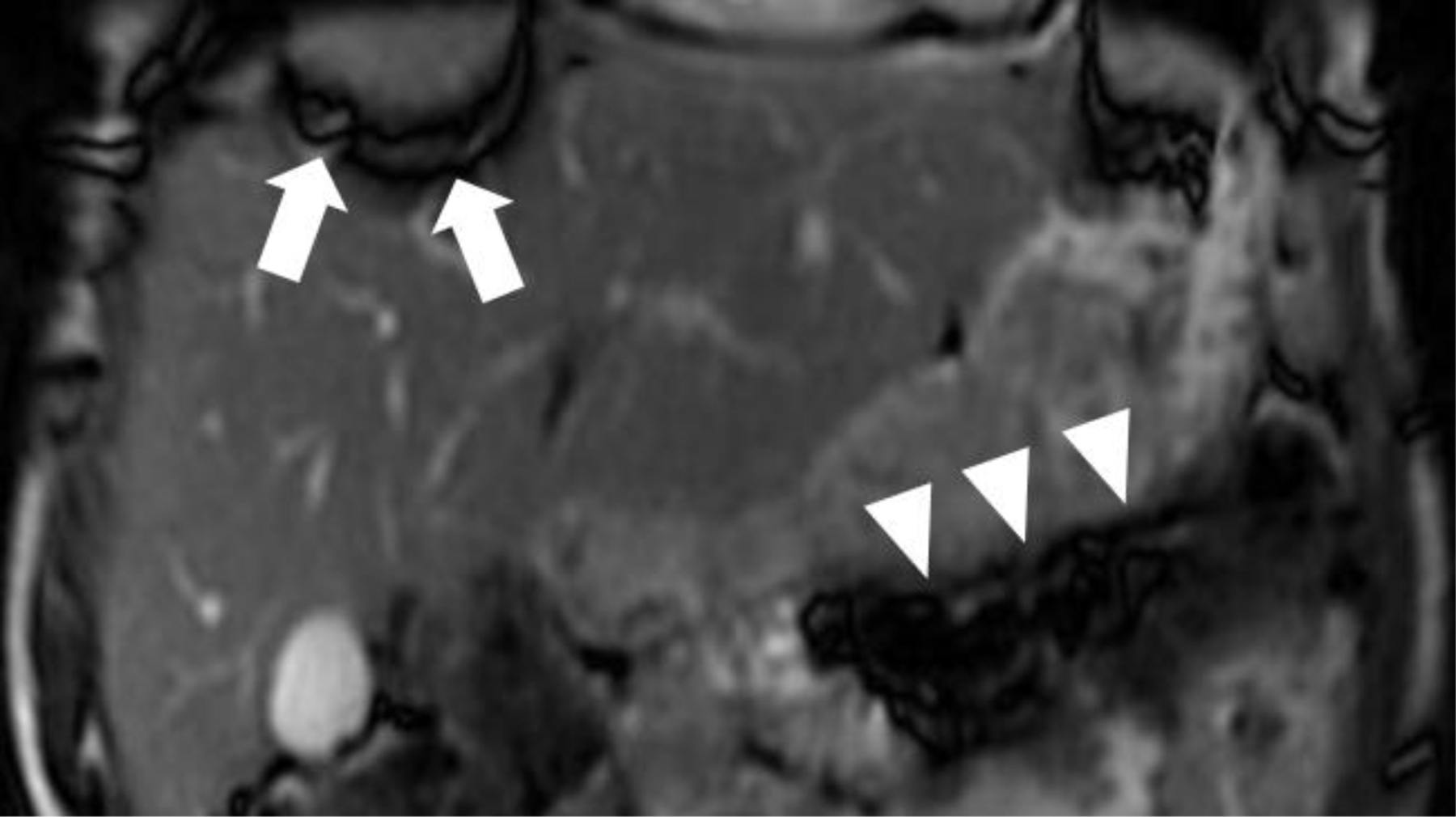
Coronal SSFP sequence obtained as part of an MR Enterography demonstrating “banding artifact” (dark coronal bands) along the periphery of the image (white arrows) and at air interfaces (white arrowheads). With cine SSFP at 3 Tesla, this artifact is amplified and must be accounted for when implementing this sequence.
ORAL CONTRAST
Addition of flavor crystals to the oral contrast material has greatly improved patient compliance with contrast intake. Furthermore, routine right lateral decubitus positioning of patients 10 minutes prior to the start of the exam has aided in opacification of more proximal small intestinal loops, documented by cine SSFP [7], and allows for optimal jejunal assessment [FIGURE 5].
FIGURE 5.

[STILL IMAGE PLACEHOLDER FOR CINE]: Coronal cine SSFP sequence from and MRE performed in a teenage patient with clinically suspected Crohn’s disease. Right lateral decubitus positioning prior to scanning combined with the use of cine SSFP imaging allows for improved evaluation of jejunal loops (white arrows).
AGE LIMITATION
Consideration must be made to the age of the child and the ability tolerate the MR exam without sedation or anesthesia, as this can be a limiting factor in performing MRE. At our institution, very few toddlers in the 2–5 year age range are evaluated with MRE, most likely due to the age distribution of IBD and the added requirement of sedation / anesthesia to complete the examination. When MRE is necessary, the preference of our anesthesiologists is to perform the study without the use of oral contrast material.
In general, it is at age six years old and above when we begin to contemplate having the child undergo the examination without anesthesia. Some children younger than six are able to hold still long enough without anesthesia and some older that six are still unable to hold still and need anesthesia. These patients are evaluated on a case-by-case basis.
In these youngest patients, we employ a combination of pre-exam preparation with our Child Life specialists and allow the child to watch a movie during the examination using MRI compatible video goggles in order to maximize the child’s ability to tolerate the exam and cooperate with the examination. Using this strategy, patients as young as 4 years of age, have successfully completed MRE examinations, without sedation/anesthesia.
It should be noted that when the child cannot hold still or breath-hold, the cine sequence is actually an added benefit. The cine images are always obtained without the need for a breath-hold; instead the cine images are routinely acquired during normal breathing. The cine image capture is impervious to motion artifact during respiration since each “still frame” of the cine is acquired very rapidly - in under a second for each still frame.
FINDINGS
Lesion Detection
Assessment of inflammation can be challenging, as post contrast imaging requires the patient to cooperate with a succession of breath-holds, each lasting 15–20 seconds. Breath-hold imaging prevents a substantial amount of motion artifact and provides excellent depiction of lesion location and activity/acuity on the post-gadolinium enhanced portion of the examination. The technique for IV contrast enhanced imaging relies on T1 spoiled gradient echo sequences, which are very motion sensitive. The sensitivity to motion of these sequences means image quality can easily become motion degraded [FIGURE 6]. In our experience, cine imaging can sometimes help reveal lesions that may be masked if the patient is unable to cooperate with breath-holds.
FIGURE 6:
Axial 3D T1 SPGR image of the abdomen with severe respiratory motion artifact in a patient unable to cooperate with breath holding.
While not its primary purpose, cine SSFP, may also improve lesion detection in patients with Crohn’s disease, compared with standard sequences [8]. Inflamed bowel segments tend to demonstrate hypomotility compared to normal bowel [FIGURES 7 AND 8]. While cine SSFP alone cannot completely characterize affected intestinal segments, a decrease in motility of specific bowel segments on cine imaging may provide a valuable clue indicating potential areas of inflammation. Thus, decreased segmental motility may serve as a marker for abnormal intestinal segments. In our practice, this sequence serves as an additional “safety net” to detect subtle areas of inflamed intestine not seen on initial review of the static MRE sequences.
FIGURE 7.

[STILL IMAGE PLACEHOLDER FOR CINE]: Coronal SSFP sequence demonstrating hypoperistalsis of the inflamed terminal ileum (red arrows). Compare with normal peristalsis of uninflamed normal bowel (white arrows).
FIGURE 8.
[STILL IMAGE PLACEHOLDER FOR CINE]: Coronal SSFP sequence in a pediatric patient with acute right lower quadrant pain and a history of Crohn’s disease demonstrating inflamed distal ileal segment (red arrows)
Stricture Assessment
Stricture formation is an unfortunately common complication in Crohn’s disease that proves particularly challenging. Accurate characterization can aid in the determination of surgical versus medical management. A significant value of real time cine SSFP imaging is the ability to non-invasively and selectively interrogate suspected diseased segments with intestinal narrowing. Utilizing MRE with cine SSFP sequences, suspected strictures are identified on the standard static sequences and are observed real time. A suspected stricture remains closed and fixed, while transient peristalsis is easily demonstrated to resolve. This lack of motion is important to detect since disease activity appears to correlate with the degree of peristalsis in the terminal ileum [6]. Strictures resulting from acute inflammation often demonstrate decreased but not entirely absent peristalsis [FIGURE 9], while chronic, fibrostenotic strictures will typically remain fixed [FIGURE 10]. However, further work is needed to further clarify the ability of cine SSFP to distinguish these entities. Use of alternative methods such as capsule endoscopy (CE) in this setting can result in retention of the capsule proximal to the area of narrowing that may require surgical retrieval [9]. Capsule retention, which is the most common complication of CE [9], can also lead to intestinal obstruction and perforation [10–12]. Particularly in cases with a high degree of suspicion for stricture, cine SSFP MRE can provide a safe non-invasive means of assessment, without the concern for complications that exist with more invasive methods.
FIGURE 9.
[STILL IMAGE PLACEHOLDER FOR CINE]: 14 year old male with a 4-month history of worsening periumbilical, cramping and stabbing abdominal pain, bloody stools, and non-compliance with mesalamine maintenance therapy. Cine images from a free breathing SSFP sequence were obtained over 3.5 minutes with four sequential coronal slices acquired with 110 dynamic phases per slice (30s/slice, 272ms/phase). Inflamed bowel is depicted as thickened and narrowed loops of ileum with decreased peristalsis (red arrows), in contrast with normal-appearing bowel loops elsewhere (yellow arrows).
FIGURE 10:

[STILL IMAGE PLACEHOLDER FOR CINE]: Coronal cine SSFP sequence from MRE in a teenage female patient with abdominal pain and distention and previous history of abdominal surgery for Crohn’s disease. Red arrows demonstrate a focal, non-peristalsing segment that was found to be related to a post-surgical adhesion.
Evaluation of Intestinal Motility
Small bowel follow-through (SBFT) has long been applied to non-invasively assess small intestinal motility. The use of ionizing radiation with SBFT, however, must be taken into account given the lifetime of imaging that is projected for pediatric patients with IBD. Cine SSFP MRE offers new potential for non-radiation real time assessment of bowel motility. Clinically challenging cases such as intestinal pseudo-obstruction can be interrogated extensively without use of ionizing radiation [FIGURE 11], as also documented in a recent report from Ohkubo et al. [13]. Infiltration of the intestine by diffuse abdominal processes such as lymphangiomatosis can be documented, and the degree of compromise in intestinal peristalsis can be assessed [FIGURE 12]. In addition to the subjective interpretation of cine SSFP, objective quantification has been studied. Measurement of change in luminal caliber has been employed to quantitatively determine amplitude and frequency of bowel contractions to characterize and quantify intestinal function [4] and characterize disease-related abnormalities [5]. Further investigation is needed in the practical clinical utilization of this quantitative application.
FIGURE 11.
[STILL IMAGE PLACEHOLDER FOR CINE]: Coronal SSFP sequence demonstrating peristalsing, non-dilated bowel (white arrows) in a 9 year old male patient with chronic idiopathic intestinal pseudo-obstruction syndrome.
FIGURE 12.

[STILL IMAGE PLACEHOLDER FOR CINE]: 6 year old male with prior history of extensive intraabdominal lymphangioma. Coronal SSFP image shows thickened infiltrated, but peristalsing bowel loops (red arrows).
CONCLUSION
Cine imaging obtained during MRE provides additional and useful information on abnormal segmental intestinal motility and may enhance the detection and characterization of intestinal lesions related to IBD when compared with standard/static MR imaging. Information provided with cine SSFP imaging complements the valuable information provided by standard MRE sequences. Compared with other methods of evaluating the small intestine such as CT or fluoroscopy, MRE with cine SSFP sequences provides real time information without the use of ionizing radiation. Small intestinal strictures can be assessed without concern for obstruction proximal to the stricture that exists with capsule endoscopy. In addition, both intraluminal and extraluminal information is obtained with MRE.
The benefits of cine imaging complement a standard MRE protocol and provide a very comprehensive, non-radiation method of evaluating the gastrointestinal tract. This is especially important in patients with suspected or with diagnosed Crohn’s disease. Cine imaging may be performed over a relatively short period without much additional effort or time investment compared with routine MRE examination. While considerations must be made for younger patients and their ability to tolerate MRI, this examination can be performed in many children using a combination of Child Life support and technologies designed to help children tolerate lying still in the MRI scanner, such as MRI compatible video goggles. Cine imaging of the intestinal tract is a state of the art technique that should be considered either as a complement or possibly even a standard component of routine MRE.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Leyendecker JR, Bloomfeld RS, DiSantis DJ, et al. MR enterography in the management of patients with Crohn disease. Radiographics 2009;29(6):1827–46. [DOI] [PubMed] [Google Scholar]
- 2.Masselli G, Gualdi G. MR imaging of the small bowel. Radiology 2012;264(2):333–48. [DOI] [PubMed] [Google Scholar]
- 3.Scheffler K, Lehnhardt S. Principles and applications of balanced SSFP techniques. Eur Radiol 2003;13(11):2409–18. [DOI] [PubMed] [Google Scholar]
- 4.Wakamiya M, Furukawa A, Kanasaki S, et al. Assessment of small bowel motility function with cine-MRI using balanced steady-state free precession sequence. Journal of magnetic resonance imaging : JMRI 2011;33(5):1235–40. [DOI] [PubMed] [Google Scholar]
- 5.Odille F, Menys A, Ahmed A, et al. Quantitative assessment of small bowel motility by nonrigid registration of dynamic MR images. Magn Reson Med 2012;68(3):783–93. [DOI] [PubMed] [Google Scholar]
- 6.Menys A, Atkinson D, Odille F, et al. Quantified terminal ileal motility during MR enterography as a potential biomarker of Crohn’s disease activity: a preliminary study. Eur Radiol 2012;22(11):2494–501. [DOI] [PubMed] [Google Scholar]
- 7.Torkzad MR, Vargas R, Tanaka C, et al. Value of cine MRI for better visualization of the proximal small bowel in normal individuals. Eur Radiol 2007;17(11):2964–8. [DOI] [PubMed] [Google Scholar]
- 8.Froehlich JM, Waldherr C, Stoupis C, et al. MR motility imaging in Crohn’s disease improves lesion detection compared with standard MR imaging. Eur Radiol 2010;20(8):1945–51. [DOI] [PubMed] [Google Scholar]
- 9.Liao Z, Gao R, Xu C, et al. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc 2010;71(2):280–6. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez Carro P, Picazo Yuste J, Fernandez Diez S, et al. Intestinal perforation due to retained wireless capsule endoscope. Endoscopy 2005;37(7):684. [DOI] [PubMed] [Google Scholar]
- 11.Lin OS, Brandabur JJ, Schembre DB, et al. Acute symptomatic small bowel obstruction due to capsule impaction. Gastrointest Endosc 2007;65(4):725–8. [DOI] [PubMed] [Google Scholar]
- 12.Repici A, Barbon V, De Angelis C, et al. Acute small-bowel perforation secondary to capsule endoscopy. Gastrointest Endosc 2008;67(1):180–3. [DOI] [PubMed] [Google Scholar]
- 13.Ohkubo H, Kessoku T, Fuyuki A, et al. Assessment of Small Bowel Motility in Patients With Chronic Intestinal Pseudo-Obstruction Using Cine-MRI. Am J Gastroenterol 2013. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


