Abstract
High-mobility group box 1 (HMGB1), a multifunctional nuclear protein, exists mainly within the nucleus of all mammal eukaryotic cells. It is actively secreted by the necrotic cells as a response to the inflammatory signaling pathway. HMGB1 binds to receptor ligands as RAGE, and TLR and becomes a pro-inflammatory cytokine with a robust capacity to trigger inflammatory response. It is a critical mediator of the pathogenesis of systemic inflammation in numerous inflammatory disorders. Release of HMGB1 is associated with different viral infections and strongly participates in the regulation of viral replication cycles. In COVID-19 era, high HMGB1 serum levels were observed in COVID-19 patients and linked with the disease severity, development of cytokine storm (CS), acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). SARS-CoV-2-induced cytolytic effect may encourage release of HMGB1 due to nuclear damage. Besides, HMGB1 activates release of pro-inflammatory cytokines from immune cells and up-regulation of angiotensin I-converting enzyme 2 (ACE2). Therefore, targeting of the HMGB1 pathway by anti-HMGB1 agents, such as heparin, resveratrol and metformin, may decrease COVID-19 severity. HMGB1 signaling pathway has noteworthy role in the pathogenesis of SARS-CoV-2 infections and linked with development of ALI and ARDS in COVID-19 patients. Different endogenous and exogenous agents may affect release and activation of HMGB1 pathway. Targeting of HMGB1-mediated TLR2/TLR4, RAGE and MAPK signaling, might be a new promising drug candidate against development of ALI and/or ARDS in severely affected COVID-19 patients.
Keywords: Anti-HMGB1 agents, High-mobility group box 1, SARS-CoV-2, COVID-19, Acute respiratory distress syndrome
Background
High-mobility group box 1 (HMGB1) is a nuclear protein that binds with DNA as a chromatin binding factor, and involved in DNA repair and control of replication process (Paudel et al. 2019). HMGB1 supports cell survival through activation of autophagy through interaction with anti-apoptotic protein (Tong et al. 2018). It is released from the cells during necrosis and as a response to the inflammatory signaling pathway (Shah et al. 2019; Alsousi and Igwe 2018). The intracellular HMGB1 is released out of cells through activation of nuclear factor kappa B (NF-κB) signaling pathway (Kim et al. 2018). Extracellular HMGB1 activates receptor for advanced glycation end-product (RAGE) and toll-like receptors (TLRs) (Yao et al. 2018). HMGB1 is secreted from immune cells like monocytes, macrophages and dendritic cells by specific secretory pathway as a cytokine mediator (Richard et al. 2017). Excess release of HMGB1 from activated immune cells mainly macrophages is associated with tissue damage as in ischemia, arthritis, endotoxemia and sepsis (Andersson et al. 2018). In addition, HMGB1 is translocated into the cytosol due to oxidative stress and high reactive oxygen species (ROS) (Tang et al. 2011). Various pathogens, like bacterial and viral infections may induce passive release of HMGB1 leading to release of pro-inflammatory cytokines and critical systemic inflammation (Wang et al. 2006).
High HMGB1 serum level has been reported in COVID-19 patients and linked with disease severity, development of cytokine storm (CS), acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) (Street 2020). Thus, the aim of the present perspective was to elucidate the potential role of HMGB1 in the pathogenesis of SARS-CoV-2 infection and to scrutinize anti-HMGB1 agents as possible new therapeutic modality in the management of COVID-19.
HMGB1 and respiratory viral infections
Induction of HMGB1 release is associated with different viral infections; Simpson et al. (2020) showed that acute bronchiolitis caused by respiratory syncytial virus (RSV) is correlated with high HMGB1 in the nasopharyngeal samples in children. RSV is regarded as the main cause of severe lower respiratory tract infections in children and linked with mortality in the elderly (Moriyama et al. 2020). RSV-mediated acute respiratory dysfunction is arbitrated to induction of oxidative stress and activation of HMGB1 pathway (Hosakote et al. 2016). During viral infections, HMGB1 has been shown to induce the phosphorylation of NF-κB and mitogen-activated protein kinase (MAPK) in the respiratory epithelial cells. Besides, HMGB1 activates release of pro-inflammatory cytokines from immune cells (Hosakote et al. 2016). Interestingly, viral molecules during respiratory infections activate pattern recognition receptors (PRRs) on the immune and lung epithelial cells that contribute to the augmentation and exacerbation of inflammation. Of interest, damage-associated molecular patterns (DAMPs) from necrotic cells like HMGB1 stimulate PRRs mainly RAGE and TLRs leading to induction of inflammatory cascade and disease exacerbation during respiratory viral infections (Hosakote et al. 2016). Indeed, binding of HMGB1 to the nucleoprotein of influenza virus in the infected cells enhances virus RNA-dependent polymerase activity and virus proliferation. Therefore, blocking binding of HMGB1 to the viral nucleoprotein might be a potential target in the management of influenza-induced complications (Moisy et al. 2012). As well, dengue virus mediates release of HMGB1 from monocytes and linked with the pathogenesis of endothelial injury as indicated by maintenance of the vascular barrier integrity after treatment with HMGB1 neutralizing antibody (Ong et al. 2012).
Previously, in SARS-CoV pandemic, HMGB1 was identified as a potential mediator in early severe local pulmonary inflammation and late critical systemic inflammation, and anti-HMGB1 antibody was used in the management of SARS pandemic (Chen et al. 2004). Therefore, HMGB1 is regarded as an imperative mediator in respiratory viral infections and their associated complications.
HMGB1 in acute lung injury
Acute lung injury (ALI) is a critical respiratory disorder characterized by severe lung inflammation and pulmonary vascular injury and/or permeability leading to hypoxemia and multi-organ damage (MOD) (Tsushima et al. 2009). ALI may be a consequence of different pathological conditions including, respiratory infection, trauma, aspiration, shock, and burns, it is associated with 40% mortality in intensive care unit (ICU) patients (Kellner et al. 2017). Various inflammatory cascades are involved in the pathogenesis of ALI and related interstitial pulmonary edema through cytokine release with consequent activation and recruitment of neutrophils and myeloperoxidase secretion. (Buesing et al. 2011). HMGB1 is a prognostic biomarker and potential target in ALI, because it reflects a degree of tissue inflammation as well as its potency in blocking inflammatory pathways. Further, HMGB1 is regarded as a late inflammatory mediator in the pathogenesis of ALI via induction of NF-κB signaling pathway, which further induces release of HMGB1 in a positive feedback loop (Ding et al. 2021).
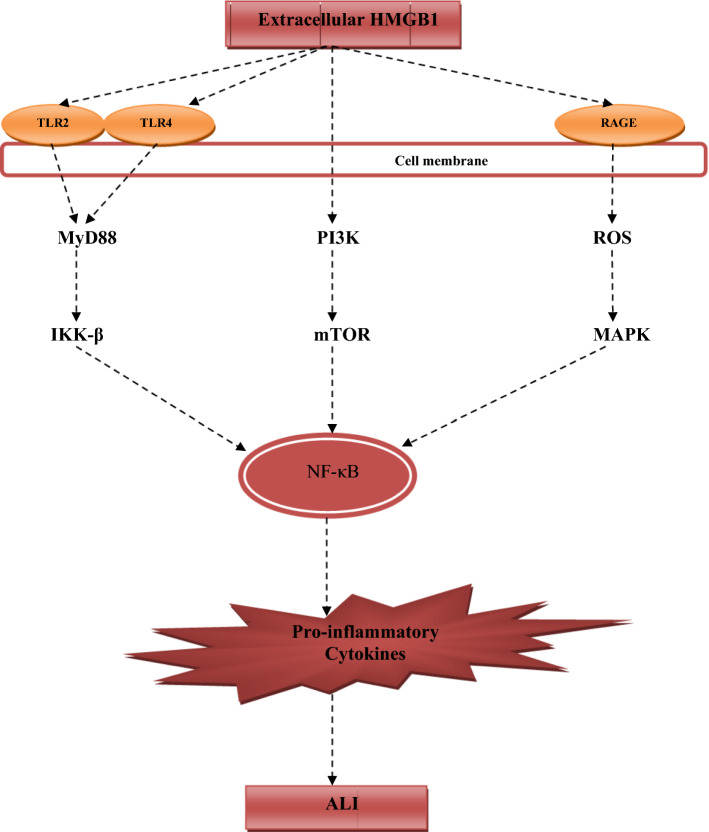
Initiation of ALI is started when extracellular HMGB1 activates cell membrane TLR2, TLR4 and RAGE receptors. Activation of RAGE receptors leads to triggering of ROS-dependent activation of MAPK pathway (Al-Kuraishy et al. 2021c; Jia et al. 2020). Though, activations of TLR2 and TLR4 by HMGB1 trigger activations of intracellular myeloid differentiation 88 (MyD88), which activates inhibitor of nuclear factor kappa B kinase (IKK-β) (Al-Kuraishy et al. 2021c). Both of IKK-β and MAPK stimulate NF-κB signaling pathway; however, extracellular HMGB1 may directly activate NF-κB through phosphatidyl-inositol 3 kinase (PI3K) and mammalian target of rapamycin (mTOR) independent of TLRs or RAGE receptors (Qu et al. 2019a). The interaction between HMGB1 and RAGE enhances the release of platelet derived growth factor (PDGF), transforming growth factor (TGF) and other fibrinogen mediators in the pulmonary tissue that result in ALI (Zou et al. 2018) (Fig. 1). Besides, HMGB1 may induce ALI through activation of autophagy, which causes release of inflammatory cytokines from neutrophils and macrophages, as well autophagy of epithelial and endothelial cells leading to release of chemokines and increased permeability, respectively (Qu et al. 2019a). Therefore, HMGB1 blood level might be a surrogate biomarker of ALI induced by different etiology.
Fig. 1.
Role of HMGB1 in the development of acute lung injury (ALI): extracellular high-mobility group box 1 (HMGB1) activates cell membrane TLR2, TLR4 and RAGE receptors. Activation of RAGE receptors leads to triggering of ROS-dependent activation of MAPK pathway. Though, activations of TLR2 and TLR4 by HMGB1 trigger activations of intracellular myeloid differentiation 88 (MyD88), which activates inhibitor of nuclear factor kappa B kinase (IKK-β). Both of IKK-β and mitogen-activated protein kinase (MAPK) stimulate NF-κB signaling pathway. However, extracellular HMGB1 may directly activate NF-κB through phosphatidyl-inositol 3 kinase (PI3K) and mammalian target of rapamycin (mTOR) independent of TLRs or RAGE receptors leading to release of pro-inflammatory cytokines that result in ALI
HMGB1 in COVID-19
SARS-CoV-2 is an enveloped positive sense RNA virus belongs to betacoronaviridiae, has high reproductive number and responsible for human respiratory infection. SARS-CoV-2 binds to the integral membrane protein named angiotensin-converting enzyme 2 (ACE2) by viral surface protein (SP) (Al-Kuraishy and Al-Gareeb 2020). This binding is facilitated by a cellular trypsin-like protease, trans-membrane protein serine 2 (TMPRSS2) (Alshahawey et al. 2020). The interaction between SARS-CoV-2 and ACE2 is associated with increasing in the vasoconstrictor angiotensin II (AngII) and reduction in the vasodilator Ang1-7 and Ang1-9 due to down-regulation of ACE2 (Al-Kuraishy et al. 2020c). SARS-CoV-2-induced deregulation of renin–angiotensin system (RAS) evokes notable disturbances in pulmonary hemodynamic and oxygen saturation (Al-Kuraishy et al. 2020b). SARS-CoV-2 mainly affects alveolar epithelial cell type II (AECII) leading to over-secretion of chemokines and inflammatory cytokines, such as IL-1β, IL-18, IL-6, and chemokine ligand 5 (CCL5) (Al-Kuraishy et al. 2020a). Besides, tumor necrosis factor alpha (TNF-α) and monocyte chemoattractant protein 1 (MCP-1) from activated macrophages augment AECII damage and may increase viral entry (Al-Kuraishy et al. 2021b). Therefore, exacerbation of immune response in SARS-CoV-2 infection may cause severe infection and cytokine storm with development of ALI and ARDS (Al-Kuraishy et al. 2021a).
Moreover, high pro-inflammatory cytokines with activation of NF-κB signaling pathway trigger the release of HMGB1 from monocytes and macrophages (Zou et al. 2020). As well, HMGB1 is also released from infected or necrotic non-immune cells (Klune et al. 2008). It has been proposed that SARS-CoV-2-induced cytolytic effect may encourage release of HMGB1 due to nuclear damage (Wyganowska-Swiatkowska et al. 2020). Of note, extracellular HMGB1 through activation of NF-κB signaling pathway provokes cytokine release and substantial neutrophil infiltrations into the lung with subsequent development of ALI and/or ARDS (Wyganowska-Swiatkowska et al. 2020).
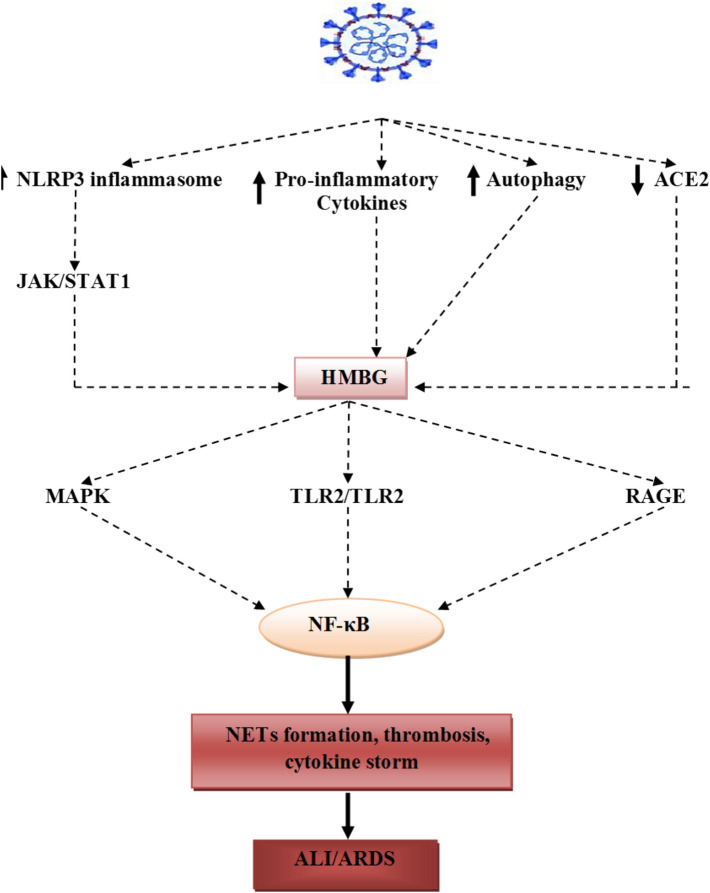
It has been shown that HMGB1-mediated autophagy is involved in in the pathogenesis of ALI in SARS-CoV-2 infection (Sun 2020). Yang and Shen (2020) illustrated that autophagy and endocytic pathway are incorporated in SARS-CoV-2 infections and linked with COVID-19 severity. In addition, over-expression of ACE2 is associated with lower release of HMGB1 (Qi et al. 2016), herein, down-regulation of ACE2 during SARS-CoV-2 infections may contribute into the release of HMGB1 and associated hyper-cytokinemia in ALI (Stilhano et al. 2020). Besides, SARS-CoV-2 may directly activate node-like receptor pyrin 3 (NLRP3) inflammasome, which through Janus kinase/signal transducer of transcription protein 1 (JAK/STAT1) triggers the release of HMGB1 from nucleus to the cytoplasm (Freeman and Swartz 2020). Therefore, inhibition of NLRP3 inflammasome and JAK/STAT1 signaling pathway may reduce release of HMGB1 and associated inflammatory reactions (Wang et al. 2017). Moreover, high circulating HMGB1 in diabetic patients predisposes them for high pro-inflammatory cytokine reactions and COVID-19 severity (Biscetti et al. 2019, Bloomgarden 2020). Indeed, the interaction between HMGB1 and RAGE receptors is mainly linked with development of ALI/ARDS in COVID-19 through injury of lung epithelial barriers and induction of endothelial permeability with development of pulmonary edema (Kerkeni and Gharbi 2020). Besides, soluble RAGE receptors are increased in the circulation of COVID-19 patients with ARDS (Chiappalupi et al. 2021).
Regarding HMGB1 serum level in COVID-19 patients and clinical outcomes, Chen et al. (2020) reported that critically patients in ICU have high circulating HMGB1, which correlated with poor clinical outcomes and high mortality. Severe COVID-19 infection is commonly associated with coagulopathy and thrombosis due to endothelial injury and development of CS (Ackermann et al. 2020). It has been reported that HMGB1 is regarded as a critical mediator of thrombosis through platelet activations, stimulation of inflammatory reactions, neutrophil recruitment, and induction of micro-thrombosis and formation of neutrophil extracellular traps (NETs) (Vogel et al. 2015). Therefore, HMGB1-induced thrombosis and CS are associated with development of ARDS in severe SARS-CoV-2 infections (Lupu et al. 2020). Herein, HMGB1 is regarded as the main player in SARS-CoV-2 infection in the initiation of hyper-cytokinemia, CS and immune-thrombosis that mediate development of ALI and ARDS (Fig. 2). Therefore, targeting of HMGB1 by conventional drugs or herbal medicine might be a potential therapeutic modality in the management of COVID-19.
Fig. 2.
SARS-CoV-2-induced ALI/ARDS: SARS-CoV-2 infection leads to activation release of extracellular high-mobility group box 1 (HMGB1) through down-regulation of ACE2, and activation of NLRP3 inflammasome, autophagy and TLR2/TLR4. HMGB1 activates TLR2, TLR4, RAGE receptors and mitogen-activated protein kinase (MAPK), provoke activation of NF-κB signaling pathway, which induces NETs formation, thrombosis and cytokine storm. These inflammatory mediators cause acute lung injury (ALI) and acute respiratory distress syndrome (ARDS)
Extracellular HMGB1 inhibitors
Different experimental, preclinical, and clinical studies illustrated that HMGB1 inhibitors reduced markedly the inflammatory conditions driven by HMGB1 in a broad set of inflammatory disease models (Yang et al. 2020). Therefore, we discussed some of HMGB1 antagonists, and how they could produce therapeutic effects through inhibition of HMGB1 pathway. It is noteworthy that these compounds are not HMGB1-specific, but they have the capacity to suppress HMGB1-triggered inflammation and other recognized bioactivities. Except for chloroquine and glycyrrhizin, the direct anti-viral effects of these compounds are not proven yet.
Statins
Statins are competitive inhibitors of 3-hydroxyl-3-methyl-glutaryrl Co-enzyme A (HMG-CoA) with cholesterol-lowering effect, used in the management of dyslipidemia and cardio-metabolic disorders (Kadhim et al. 2020). Statins also have significant anti-inflammatory, anti-thrombotic, and anti-platelet activities (Hussien et al. 2021). It has been shown that statins inhibit the interaction of HMGB1 with both TLR4 and RAGE receptors, in addition to inhibition of the expression of TLR4 and RAGE receptors in different inflammatory disorders (Yang et al. 2010). Therefore, statins could attenuate the effect of HMGB1 that is mediated by TLR4 and RAGE receptors. Kong et al. (2016) illustrated that statins suppress NLRP3 inflammasome via inhibition of TLR4/MyD88/NF-κB signaling pathway. Thus, statins may attenuate SARS-CoV-2 infection-induced pro-inflammatory cytokine reaction and COVID-19 mortality (Permana et al. 2021). However, meta-analyses of observational studies illustrated that COVID-19 patients who received statins therapy did not show marked decline in either hospital mortality or the COVID-19 severity (Scheen 2021). Nonetheless, statins therapy improves clinical outcomes in COVID-19 through modulation of cellular processes and inflammatory mediators, such as autophagy, NLPR3 inflammasome and up-regulation of ACE2, that collectively block release and activation of HMGB during SARS-CoV-2 infection (Rodrigues‐Diez et al. 2020).
Chloroquine
Chloroquine/hydroxychloroquine compounds have been reported to effectively abrogate the COVID-19 infection due to in vitro direct antiviral activities, decreased the spread of the virus and reduction of viral load (Al-Kuraishy and Al-Gareeb 2020). Hydroxychloroquine has potent anti-inflammatory effects through various mechanisms; one of these is inhibition release of HMGB from activated immune cells through inhibition of PH-dependent lysosomotropic effects (Zhang et al. 2020). As well, hydroxychloroquine assuages NETs formation-induced HMGB release in SARS-CoV-2 infection (Roldan et al. 2020). Indeed, hydroxychloroquine blocks autophagy and prevents release of HMGB (Zeh et al. 2020). Jansen et al. (2021), reported that hydroxychloroquine blocked the endosomal TLR signaling, with subsequent prevention of interferon activation and HMGB release in SARS-CoV-2 infection.
Thrombomodulin
Thrombomodulin is an integral membrane protein expressed in different cells mainly endothelial cell, monocyte and dendritic cells, it converts thrombin into an anticoagulant enzyme (Loghmani and Conway 2018). Thrombomodulin blocks and degrades free extracellular HMGB with the aid of proteolytic action of thrombin. Thus, recombinant thrombomodulin is used in the management of coagulopathy and inflammatory reactions in sepsis (Vincent et al. 2019). In COVID-19 era, pulmonary endothelial cell injury-induced thrombosis in severe infection is mediated through inhibition in the release of thrombomodulin (O'Sullivan et al. 2020). Hultstrom et al. (2021) illustrated that high circulating inflammatory angiopoitin-2 receptors in critical COVID-19 patients are associated thrombosis and development of ARDS through inhibition of thrombomodulin. Therefore, recombinant thrombomodulin might be effective in the management of COVID-19, through inhibition of HMGB-induced inflammation and thrombosis.
Haptoglobin
Haptoglobin is an acute-phase protein, binds free hemoglobin during intravascular hemolysis, and also inactivates extracellular HMGB at site of inflammation. Haptoglobin-HMGB1 complex activates macrophages for synthesis and release of anti-inflammatory IL-10, which, counteracted the action of excess pro-inflammatory cytokines during acute inflammatory conditions (Yang et al. 2017). However, in severe inflammatory process and when associated with bleeding at inflammatory site, the haptoglobin dissociated from HMGB-binding site, and attached free hemoglobin due to strong affinity of haptoglobin to the free hemoglobin (Devides et al. 2018). Therefore, inherited or acquired deficiency of haptoglobin is associated with exaggerated inflammatory reactions due to high unopposed free extracellular HMGB (Dahan et al. 2018). It has been observed that recombinant haptoglobin is effective in management of ALI, experimental pneumonia, trauma, and transfusion-mediated hemolysis (Remy et al. 2018). Therefore, recombinant haptoglobin therapy might be of interest in management of patients with severe COVID-19 due to its potential anti-inflammatory through blocking of HMGB-mediated thrombotic and inflammatory reactions.
Heparin and heparinoid compounds
Heparin is an anticoagulant agent, acts through activation of endogenous anti-thrombin III, has high affinity to the extracellular HMGB (Li et al. 2015). Binding of heparin to the HMGB, reduces the ability of HMGB to activate RAGE receptors on the activated macrophages (Rouhiainen et al. 2018). Therefore, heparin mitigates inflammatory reactions that are induced through HMGB/RAGE receptors axis. On the other hand, heparinoid, which is low molecular weight heparin (LMWH), has anti-inflammatory effect with very low anti-coagulant activity has been used successfully in management of ALI through inhibition of neutrophil-mediated release of HMGB (Rasmuson et al. 2019; Utsunomiya et al. 2018). Therefore, heparin and other LMWH derivatives are effective in management of critical COVID-19 patients their antiviral and anti-inflammatory effects (Hippensteel et al. 2020).
Resveratrol
Resveratrol is a phytomedicine containing phenol molecule that has a protective function when produced from plants under stressful conditions (Salehi et al. 2018). Different studies reported that resveratrol has potent anti-inflammatory effects through suppression of HMGB-mediated signaling pathway, such as expression of TLR4, NF-κB, MyD88, during acute inflammatory disorders (de Sá Coutinho et al. 2018). (de Oliveira et al. 2019) confirmed that resveratrol was effective against lipopolysaccharide (LPS)-induced ALI through amelioration of inflammatory signaling mediators. Thus, resveratrol might be probable therapy in management of patients with COVID-19 through suppression of SARS-CoV-2-induced cytokine storm and development of ALI/ARDS (Hoang 2020). Also, resveratrol has potent in vitro antagonistic action against SARS-CoV-2 viral replication.
Glycyrrhizin
Glycyrrhizin is an herbal medicine derived from licorice roots, widely used in Chinese traditional medicine, has potent anti-inflammatory activities through inhibition of HMGB-mediated signaling pathway (Paudel et al. 2020). In addition, glycyrrhizin suppressed the viral replication of SARS-CoV, flaviviruses and H5N1 influenza (Wang et al. 2015). Besides, glycyrrhizin attenuates LPS-induced ALI through inhibition release of HMGB1 and other inflammatory mediators in experimental studies (Qu et al. 2019b). Recently, different preclinical and clinical studies highlighted the potential role of glycyrrhizin in COVID-19 through modulation of SARS-CoV-2 infectivity. It inhibits SARS-CoV-2 binding to the ACE2, alters viral lipid membrane, decreases the production of airway exudates, combats the SARS-CoV-associated secondary bacterial infection, and attenuates cellular inflammatory signaling with suppression of macrophage activity (Luo et al. 2020a; Gomaa and Abdel-Wadood 2021).
Dexmedetomidine and ketamine
Dexmedetomidine is an anxiolytic and sedative drug with sympatholytic effect, acts through activation of α-2 presynaptic adrenoceptor (Weerink et al. 2017). Also, dexmedetomidine inhibits release of pro-inflammatory cytokines via stimulation of cholinergic nicotinic receptor type 7 (7nAChR) (Xiang et al. 2014). It has been shown that dexmedetomidine attenuates LPS-induced ALI through inhibition of lung HMGB1-mediated TLR4/Nf-kB axis (Meng et al. 2018). Therefore, dexmedetomidine may reduce COVID-19 severity through different pathways including, inhibition of TLR4, release of HMGB1, NLRP3 inflammasome, NF-κB signaling and JAK/STAT signaling (Jain et al. 2021). Other 7nAChR agonists also have pulmo-protective effects through inhibition of lung macrophages and release of pro-inflammatory cytokines during SARS-CoV-2 infection (Jain et al. 2021). Dexmedetomidine is commonly used in combination with ketamine during anesthesia and ventilation support during mechanical ventilation (Luscri and Tobias 2006). Ketamine also inhibits release of HMGB1 and NETs formation during ALI (Akinosoglou et al. 2020). Further, ketamine has been shown to attenuate sepsis-induced ALI by down-regulating the HMGB1-RAGE pathway (Zhang et al. 2018). It was reported that ketamine protected against lung injury via down-regulation of the expressions of HMGB1 and TLR4 as well as the activity of myeloperoxidase in the inflamed lungs (Qin et al. 2015). Thereby, due to their potent anti-inflammatory effects, both ketamine and dexmedetomidine are more appropriate anesthetic agents in the management of ARDS in COVID-19 patients.
Metformin
Metformin is an insulin-sensitizing agent, used as first-line therapy in management of type 2 diabetes mellitus (T2DM) (Al-Kuraishy et al. 2020d; Al-Brakati et al. 2020; Othman et al. 2021b). Metformin has potent anti-inflammatory effect through activation of adenosine monophosphate protein kinase (AMPK) and inhibition of HMGB1 release (Al-Kuraishy et al. 2020d). Horiuchi et al. (2017) revealed that metformin directly inhibits HMGB1 acidic terminal part released from damaged cells in acute liver injury. Metformin therapy is associated with better clinical outcomes and low mortality in COVID-19 patients (Luo et al. 2020b). The case–control study of Al-Kuraishy et al. (2021a) illustrated that metformin therapy in COVID-19 patients with T2DM is linked with reduction of ALI and ischemic stroke, due to its potent anti-inflammatory effects.
Finally, this perspective highlighted the potential role of HMGB1 in the pathogenesis of SARS-CoV-2 infections and associated inflammatory reactions-induced-ALI/ARDS. Therefore, targeting of HMGB1 signaling pathway might be a new therapeutic modality in the management of COVID-19.
Salicylic acid
Salicylic acid (SA) is an organic compound, has antibacterial and antiseptic activity, used mainly in treatment of dermatological disorders like psoriasis, acne, and seborrheic dermatitis (Arif 2015). It has been reported that SA had ability to blocks the pro-inflammatory effect of HMGB1 at lower micromolar concentration to block the enzyme activity of COX-1 and COX-2 (Klessig et al. 2016). Of note, HMGB1 induces expression of COX-2 and other cytokine genes with propagation of inflammatory changes (Park et al. 2018). SA unlike acetylsalicylic acid (aspirin) which inhibits activity of COX-2, inhibits synthesis of COX-2 (Klessig et al. 2016; Othman et al. 2021a). Therefore, SA derivatives like acetylsalicylic acid could be effective in the management of COVID-19 by inhibiting HMGB1 and other inflammatory signaling pathways like NF-κB (Cacciapuoti and Cacciapuoti 2021). A cohort study involved 984 COVID-19 patients according to the use of acetylsalicylic acid before hospitalization, showed that COVID-19 patients with acetylsalicylic acid treatment had high survival rates compared to the non-user (Sisinni et al. 2021). These observations suggest the protective role acetylsalicylic acid against COVID-19 severity by reducing platelet activation and thrombotic complications.
Conclusion
HMGB1 signaling pathway has a noteworthy role in the pathogenesis of SARS-CoV-2 infections and linked with development of ALI and ARDS in COVID-19 patients. Different endogenous and exogenous agents may affect release and activation of HMGB1 pathway. Targeting of HMGB1-mediated TLR2/TLR4, RAGE and MAPK signaling, might be a new supporting line against development of ALI and/or ARDS in severely affected COVID-19 patients. Prospective and clinical trial studies are merited and reasonable to confirm the therapeutic benefit of anti-HMGB1 in managing of COVID-19.
Funding
No funding.
Data availability
Enquiries about data availability should be directed to the authors.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinosoglou K, Gogos A, Papageorgiou C, Angelopoulos E, Gogos C. Ketamine in COVID-19 patients: thinking out of the box. J Med Virol. 2020;93:4069–4070. doi: 10.1002/jmv.26681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Brakati A, Albarakati AJA, Daabo HMA, Baty RS, Salem FEH, Habotta OA, Elmahallawy EK, Abdel-Mohsen DM, Taha H, Akabawy AMA, Kassab RB, Abdel Moneim AE, Amin HK. Neuromodulatory effects of green coffee bean extract against brain damage in male albino rats with experimentally induced diabetes. Metab Brain Dis. 2020;35:1175–1187. doi: 10.1007/s11011-020-00583-6. [DOI] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI. From SARS-CoV to nCoV-2019: ruction and argument. Arch Clin Infect Dis. 2020;15:e102624. doi: 10.5812/archcid.102624. [DOI] [Google Scholar]
- Al-Kuraishy H, Hussien N, Al-Naimi M, Al-Buhadily A, Al-Gareeb A, Lungnier C. Is ivermectin–azithromycin combination the next step for COVID-19? Biomed Biotechnol Res J (BBRJ) 2020;4:101–103. [Google Scholar]
- Al-Kuraishy H, Hussien N, Al-Naimi M, Al-Buhadily A, Al-Gareeb A, Lungnier C. Renin-Angiotensin system and fibrinolytic pathway in COVID-19: One-way skepticism. Biomed Biotechnol Res J (BBRJ) 2020;4:33–40. [Google Scholar]
- Al-Kuraishy HM, Sami OM, Hussain NR, Al-Gareeb AI. Metformin and/or vildagliptin mitigate type II diabetes mellitus induced-oxidative stress: the intriguing effect. J Adv Pharm Technol Res. 2020;11:142. doi: 10.4103/japtr.JAPTR_18_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Alblihed M, Cruz-Martins N, Batiha GE-S. COVID-19 and risk of acute ischemic stroke and acute lung injury in patients with type ii diabetes mellitus: the anti-inflammatory role of metformin. Front Med. 2021;8:110. doi: 10.3389/fmed.2021.644295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Faidah H, Al-Maiahy TJ, Cruz-Martins N, Batiha GE. The looming effects of estrogen in covid-19: a rocky rollout. Front Nutr. 2021;8:649128. doi: 10.3389/fnut.2021.649128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Qusty N, Cruz-Martins N, Batiha GE-S. Sequential doxycycline and colchicine combination therapy in Covid-19: the salutary effects. Pulm Pharmacol Ther. 2021;67:102008. doi: 10.1016/j.pupt.2021.102008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Niemi MS, Hussain NR, Al-Gareeb AI, Al-Harchan NA, Al-Kurashi AH. The potential role of renin angiotensin system RAS and dipeptidyl peptidase-4 (DPP-4) in COVID-19 navigating the uncharted. In: Kibel A, editor. Reninangiotensin system. London: IntechOpen; 2020. pp. 151–165. [Google Scholar]
- Alshahawey M, Raslan M, Sabri N. Sex-mediated effects of ACE2 and TMPRSS2 on the incidence and severity of COVID-19; the need for genetic implementation. Curr Res Transl Med. 2020;68:149–150. doi: 10.1016/j.retram.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsousi AA, Igwe OJ. Redox-active trace metal-induced release of high mobility group box 1 (HMGB1) and inflammatory cytokines in fibroblast-like synovial cells is Toll-like receptor 4 (TLR4) dependent. Biochim Biophys Acta. 2018;1864:3847–3858. doi: 10.1016/j.bbadis.2018.08.029. [DOI] [PubMed] [Google Scholar]
- Andersson U, Yang H, Harris H. High-mobility group box 1 protein (HMGB1) operates as an alarmin outside as well as inside cells. Semin Immunol. 2018;38:40–48. doi: 10.1016/j.smim.2018.02.011. [DOI] [PubMed] [Google Scholar]
- Arif T. Salicylic acid as a peeling agent: a comprehensive review. Clin Cosmet Investig Dermatol. 2015;8:455. doi: 10.2147/CCID.S84765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biscetti F, Rando MM, Nardella E, Cecchini AL, Pecorini G, Landolfi R, Flex A. High mobility group box-1 and diabetes mellitus complications: state of the art and future perspectives. Int J Mol Sci. 2019;20:6258. doi: 10.3390/ijms20246258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloomgarden ZT. Diabetes and COVID-19. J Diabetes. 2020;12:347–348. doi: 10.1111/1753-0407.13027. [DOI] [PubMed] [Google Scholar]
- Buesing KL, Densmore JC, Kaul S, Pritchard KA, Jr, Jarzembowski JA, Gourlay DM, Oldham KT. Endothelial microparticles induce inflammation in acute lung injury. J Surg Res. 2011;166:32–39. doi: 10.1016/j.jss.2010.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciapuoti F, Cacciapuoti F. Could low doses acetylsalicylic acid prevent thrombotic complications in COVID-19 patients? Clin Appl Thromb Hemost. 2021;27:10760296211014592. doi: 10.1177/10760296211014592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G, Chen D-Z, Li J, Czura CJ, Tracey KJ, Sama AE, Wang H. Pathogenic role of HMGB1 in SARS? Med Hypotheses. 2004;63:691–695. doi: 10.1016/j.mehy.2004.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Long X, Xu Q, Tan J, Wang G, Cao Y, Wei J, Luo H, Zhu H, Huang L, Meng F, Huang L, Wang N, Zhou X, Zhao L, Chen X, Mao Z, Chen C, Li Z, Sun Z, Zhao J, Wang D, Huang G, Wang W, Zhou J. Elevated serum levels of S100A8/A9 and HMGB1 at hospital admission are correlated with inferior clinical outcomes in COVID-19 patients. Cell Mol Immunol. 2020;17:992–994. doi: 10.1038/s41423-020-0492-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiappalupi S, Salvadori L, Vukasinovic A, Donato R, Sorci G, Riuzzi F. Targeting RAGE to prevent SARS-CoV-2-mediated multiple organ failure: hypotheses and perspectives. Life Sci. 2021;272:119251. doi: 10.1016/j.lfs.2021.119251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahan I, Thawho N, Farber E, Nakhoul N, Asleh R, Levy AP, Li YC, Ben-Izhak O, Nakhoul F. The iron-Klotho-VDR axis is a major determinant of proximal convoluted tubule injury in Haptoglobin 2–2 genotype diabetic nephropathy patients and mice. J Diabetes Res. 2018 doi: 10.1155/2018/7163652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Oliveira MTP, De Sá Coutinho D, De Souza ÉT, Guterres SS, Pohlmann AR, Silva PMR, Martins MA, Bernardi A. Orally delivered resveratrol-loaded lipid-core nanocapsules ameliorate LPS-induced acute lung injury via the ERK and PI3K/Akt pathways. Int J Nanomed. 2019;14:5215. doi: 10.2147/IJN.S200666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Sá Coutinho D, Pacheco MT, Frozza RL, Bernardi A. Anti-inflammatory effects of resveratrol: mechanistic insights. Int J Mol Sci. 2018;19:1812. doi: 10.3390/ijms19061812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devides AC, Romao-Veiga M, Matias ML, Ribeiro VR, Nunes PR, Gomes VJ, Fernandes MF, Borges VTM, Peracoli MTS, Peracoli JC. 127 Haptoglobin deficiency in the inflammatory process of preeclampsia. Pregnancy Hypertens. 2018;13:S81. doi: 10.1016/j.preghy.2018.08.239. [DOI] [Google Scholar]
- Ding X, Li S, Zhu L. Potential effects of HMGB1 on viral replication and virus infection-induced inflammatory responses: a promising therapeutic target for virus infection-induced inflammatory diseases. Cytokine Growth Factor Rev. 2021;62:54–61. doi: 10.1016/j.cytogfr.2021.08.003. [DOI] [PubMed] [Google Scholar]
- Freeman TL, Swartz TH. Targeting the NLRP3 inflammasome in severe COVID-19. Front Immunol. 2020;11:1518. doi: 10.3389/fimmu.2020.01518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomaa AA, Abdel-Wadood YA. The potential of glycyrrhizin and licorice extract in combating COVID-19 and associated conditions. Phytomedicine Plus. 2021;1:100043–100043. doi: 10.1016/j.phyplu.2021.100043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hippensteel JA, Lariviere WB, Colbert JF, Langouët-Astrié CJ, Schmidt EP. Heparin as a therapy for COVID-19: current evidence and future possibilities. Am J Physiol Lung Cell Mol Physiol. 2020;319:L211–L217. doi: 10.1152/ajplung.00199.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang T. An approach of fatty acids and resveratrol in the prevention of COVID-19 severity. Phytother Res. 2020;35(2269):2273. doi: 10.1002/ptr.6956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horiuchi T, Sakata N, Narumi Y, Kimura T, Hayashi T, Nagano K, Liu K, Nishibori M, Tsukita S, Yamada T. Metformin directly binds the alarmin HMGB1 and inhibits its proinflammatory activity. J Biol Chem. 2017;292:8436–8446. doi: 10.1074/jbc.M116.769380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosakote YM, Brasier AR, Casola A, Garofalo RP, Kurosky A. Respiratory syncytial virus infection triggers epithelial HMGB1 release as a damage-associated molecular pattern promoting a monocytic inflammatory response. J Virol. 2016;90:9618–9631. doi: 10.1128/JVI.01279-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hultstrom M, Fromell K, Larsson A, Quaggin SE, Betsholtz C, Frithiof R, Lipcsey M, Jeansson M. Elevated Angiopoietin-2 inhibits thrombomodulin-mediated anticoagulation in critically ill COVID 19 patients. medRxiv. 2021;9:838. doi: 10.3390/biomedicines10061333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussien NR, Al-Niemi MS, Al-Kuraishy HM, Al-Gareeb AI. Statins and Covid-19: the neglected front of bidirectional effects. J Pak Med Assoc. 2021;71(Suppl. 8):S133–S136. [PubMed] [Google Scholar]
- Jain A, Lamperti M, Doyle DJ. Dexmedetomidine: another arrow in the quiver to fight COVID-19 in intensive care units. Br J Anaesth. 2021;126:e35. doi: 10.1016/j.bja.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen MA, Ciere LC, Moerland M. Hydroxychloroquine effects on TLR signalling: underexposed but unneglectable in COVID-19. J Immunol Res. 2021;2021:6659410. doi: 10.1155/2021/6659410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia L, Xue K, Liu J, Habotta OA, Hu L, Abdel Moneim AE. Anticolitic effect of berberine in rat experimental model: impact of PGE2/p38 MAPK pathways. Mediators Inflamm. 2020;2020:9419085. doi: 10.1155/2020/9419085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadhim SS, Al-Windy SA, Al-Nami MS, Al Kuraishy HM, Al Gareeb AI. Statins improve periodontal disease-induced inflammatory changes and associated lipid peroxidation in patients with dyslipidemia: two birds by one stone. J Int Oral Health. 2020;12:66. doi: 10.4103/jioh.jioh_194_19. [DOI] [Google Scholar]
- Kellner M, Noonepalle S, Lu Q, Srivastava A, Zemskov E, Black SM. ROS signaling in the pathogenesis of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) Adv Exp Med Biol. 2017;967:105–137. doi: 10.1007/978-3-319-63245-2_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerkeni M, Gharbi J. RAGE receptor: May be a potential inflammatory mediator for SARS-COV-2 infection? Med Hypotheses. 2020;144:109950. doi: 10.1016/j.mehy.2020.109950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Park J-C, Lee MH, Yang CE, Lee JH, Lee WJ. High-mobility group box 1 mediates fibroblast activity via RAGE-MAPK and NF-κB signaling in keloid scar formation. Int J Mol Sci. 2018;19:76. doi: 10.3390/ijms19010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klessig DF, Tian M, Choi HW. Multiple targets of salicylic acid and its derivatives in plants and animals. Front Immunol. 2016;7:206. doi: 10.3389/fimmu.2016.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klune JR, Dhupar R, Cardinal J, Billiar TR, Tsung A. HMGB1: endogenous danger signaling. Mol Med. 2008;14:476–484. doi: 10.2119/2008-00034.Klune. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong F, Ye B, Lin L, Cai X, Huang W, Huang Z. Atorvastatin suppresses NLRP3 inflammasome activation via TLR4/MyD88/NF-κB signaling in PMA-stimulated THP-1 monocytes. Biomed Pharmacother. 2016;82:167–172. doi: 10.1016/j.biopha.2016.04.043. [DOI] [PubMed] [Google Scholar]
- Li L, Ling Y, Huang M, Yin T, Gou S-M, Zhan N-Y, Xiong J-X, Wu H-S, Yang Z-Y, Wang C-Y. Heparin inhibits the inflammatory response induced by LPS and HMGB1 by blocking the binding of HMGB1 to the surface of macrophages. Cytokine. 2015;72:36–42. doi: 10.1016/j.cyto.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Loghmani H, Conway EM. Exploring traditional and nontraditional roles for thrombomodulin. Blood J Am Soc Hematol. 2018;132:148–158. doi: 10.1182/blood-2017-12-768994. [DOI] [PubMed] [Google Scholar]
- Luo P, Liu D, Li J. Pharmacological perspective: glycyrrhizin may be an efficacious therapeutic agent for COVID-19. Int J Antimicrob Agents. 2020;55:105995. doi: 10.1016/j.ijantimicag.2020.105995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo P, Qiu L, Liu Y, Liu X-L, Zheng J-L, Xue H-Y, Liu W-H, Liu D, Li J. Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am J Trop Med Hyg. 2020;103:69. doi: 10.4269/ajtmh.20-0375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lupu L, Palmer A, Huber-Lang M. Inflammation, thrombosis, and destruction: the three-headed cerberus of trauma- and SARS-CoV-2-induced ARDS. Front Immunol. 2020;11:584514. doi: 10.3389/fimmu.2020.584514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luscri N, Tobias JD. Monitored anesthesia care with a combination of ketamine and dexmedetomidine during magnetic resonance imaging in three children with trisomy 21 and obstructive sleep apnea. Pediatr Anesth. 2006;16:782–786. doi: 10.1111/j.1460-9592.2006.01857.x. [DOI] [PubMed] [Google Scholar]
- Meng L, Li L, Lu S, Li K, Su Z, Wang Y, Fan X, Li X, Zhao G. The protective effect of dexmedetomidine on LPS-induced acute lung injury through the HMGB1-mediated TLR4/NF-κB and PI3K/Akt/mTOR pathways. Mol Immunol. 2018;94:7–17. doi: 10.1016/j.molimm.2017.12.008. [DOI] [PubMed] [Google Scholar]
- Moisy D, Avilov SV, Jacob Y, Laoide BM, Ge X, Baudin F, Naffakh N, Jestin J-L. HMGB1 protein binds to influenza virus nucleoprotein and promotes viral replication. J Virol. 2012;86:9122–9133. doi: 10.1128/JVI.00789-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol. 2020;7:83–101. doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- O’Sullivan JM, MC Gonagle D, Ward SE, Preston RJ, O’Donnell JS. Endothelial cells orchestrate COVID-19 coagulopathy. Lancet Haematol. 2020;7:e553–e555. doi: 10.1016/S2352-3026(20)30215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong SP, Lee LM, Leong YF, Ng ML, Chu JJ. Dengue virus infection mediates HMGB1 release from monocytes involving PCAF acetylase complex and induces vascular leakage in endothelial cells. PLoS One. 2012;7 :e41932. doi: 10.1371/journal.pone.0041932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Othman MS, Al-Bagawi AH, Obeidat ST, Fareid MA, Habotta OA, Moneim AEA. Antitumor activity of zinc nanoparticles synthesized with berberine on human epithelial colorectal adenocarcinoma (Caco-2) cells through acting on Cox-2/NF-kB and p53 pathways. Anticancer Agents Med Chem. 2021;22(2002):2010. doi: 10.2174/1871520621666211004115839. [DOI] [PubMed] [Google Scholar]
- Othman MS, Khaled AM, Al-Bagawi AH, Fareid MA, Ghany RA, Habotta OA, Moneim AEA. Hepatorenal protective efficacy of flavonoids from Ocimum basilicum extract in diabetic albino rats: a focus on hypoglycemic, antioxidant, anti-inflammatory and anti-apoptotic activities. Biomed Pharmacother. 2021;144:112287. doi: 10.1016/j.biopha.2021.112287. [DOI] [PubMed] [Google Scholar]
- Park EJ, Kim YM, Kim HJ, Chang KC. Luteolin activates ERK1/2 – and Ca2+-dependent HO-1 induction that reduces LPS-induced HMGB1, iNOS/NO, and COX-2 expression in RAW264. 7 cells and mitigates acute lung injury of endotoxin mice. Inflamm Res. 2018;67:445–453. doi: 10.1007/s00011-018-1137-8. [DOI] [PubMed] [Google Scholar]
- Paudel YN, Angelopoulou E, Piperi C, Balasubramaniam VR, Othman I, Shaikh MF. Enlightening the role of high mobility group box 1 (HMGB1) in inflammation: updates on receptor signalling. Eur J pharmacol. 2019;858:172487. doi: 10.1016/j.ejphar.2019.172487. [DOI] [PubMed] [Google Scholar]
- Paudel YN, Angelopoulou E, Semple B, Piperi C, Othman I, Shaikh MF. Potential neuroprotective effect of the HMGB1 inhibitor glycyrrhizin in neurological disorders. ACS Chem Neurosci. 2020;11:485–500. doi: 10.1021/acschemneuro.9b00640. [DOI] [PubMed] [Google Scholar]
- Permana H, Huang I, Purwiga A, Kusumawardhani NY, Sihite TA, Martanto E, Wisaksana R, Soetedjo NNM. In-hospital use of statins is associated with a reduced risk of mortality in coronavirus-2019 (COVID-19): systematic review and meta-analysis. Pharmacol Rep. 2021;73(769):780. doi: 10.1007/s43440-021-00233-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi YF, Zhang J, Wang L, Shenoy V, Krause E, Oh SP, Pepine CJ, Katovich MJ, Raizada MK. Angiotensin-converting enzyme 2 inhibits high-mobility group box 1 and attenuates cardiac dysfunction post-myocardial ischemia. J Mol Med (Berl) 2016;94:37–49. doi: 10.1007/s00109-015-1356-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin M-Z, Gu Q-H, Tao J, Song X-Y, Gan G-S, Luo Z-B, Li B-X. Ketamine effect on HMGB1 and TLR4 expression in rats with acute lung injury. Int J Clin Exp Pathol. 2015;8:12943. [PMC free article] [PubMed] [Google Scholar]
- Qu L, Chen C, Chen Y, Li Y, Tang F, Huang H, He W, Zhang R, Shen L. High-mobility group box 1 (HMGB1) and autophagy in acute lung injury (ALI): a review. Med Sci Monit: Int Med J Exp Clin Res. 2019;25:1828–1837. doi: 10.12659/MSM.912867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu L, Chen C, He W, Chen Y, Li Y, Wen Y, Zhou S, Jiang Y, Yang X, Zhang R, Shen L. Glycyrrhizic acid ameliorates LPS-induced acute lung injury by regulating autophagy through the PI3K/AKT/mTOR pathway. Am J Transl Res. 2019;11:2042–2055. [PMC free article] [PubMed] [Google Scholar]
- Rasmuson J, Kenne E, Wahlgren M, Soehnlein O, Lindbom L. Heparinoid sevuparin inhibits Streptococcus-induced vascular leak through neutralizing neutrophil-derived proteins. FASEB J. 2019;33:10443–10452. doi: 10.1096/fj.201900627R. [DOI] [PubMed] [Google Scholar]
- Remy KE, Cortés-Puch I, Solomon SB, Sun J, Pockros BM, Feng J, Lertora JJ, Hantgan RR, Liu X, Perlegas A. Haptoglobin improves shock, lung injury, and survival in canine pneumonia. JCI insight. 2018;3:e123013. doi: 10.1172/jci.insight.123013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard SA, Sackey M, Su Z, Xu H. Pivotal neuroinflammatory and therapeutic role of high mobility group box 1 in ischemic stroke. Biosci Rep. 2017;37:BSR20171104. doi: 10.1042/BSR20171104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues-Diez RR, Tejera-Muñoz A, Marquez-Exposito L, Rayego-Mateos S, Santos Sanchez L, Marchant V, Tejedor Santamaria L, Ramos AM, Ortiz A, Egido J. Statins: could an old friend help in the fight against COVID-19? Br J Pharmacol. 2020;177:4873–4886. doi: 10.1111/bph.15166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roldan EQ, Biasiotto G, Magro P, Zanella I. The possible mechanisms of action of 4-aminoquinolines (chloroquine/hydroxychloroquine) against Sars-Cov-2 infection (COVID-19): a role for iron homeostasis? Pharmacol Res. 2020;158:104904. doi: 10.1016/j.phrs.2020.104904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouhiainen A, Nykänen N-P, Kuja-Panula J, Vanttola P, Huttunen HJ, Rauvala H. Inhibition of Homophilic interactions and ligand binding of the receptor for advanced glycation end products by heparin and heparin-related carbohydrate structures. Medicines. 2018;5:79. doi: 10.3390/medicines5030079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehi B, Mishra AP, Nigam M, Sener B, Kilic M, Sharifi-Rad M, Fokou PVT, Martins N, Sharifi-Rad J. Resveratrol: a double-edged sword in health benefits. Biomedicines. 2018;6:91. doi: 10.3390/biomedicines6030091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheen AJ. Statins and clinical outcomes with COVID-19: meta-analyses of observational studies. Diabetes Metab. 2021;47:101220. doi: 10.1016/j.diabet.2020.101220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah BS, Burt KG, Jacobsen T, Fernandes TD, Alipui DO, Weber KT, Levine M, Chavan SS, Yang H, Tracey KJ. High mobility group box-1 induces pro-inflammatory signaling in human nucleus pulposus cells via toll-like receptor 4-dependent pathway. J Orthop Res. 2019;37:220–231. doi: 10.1002/jor.24154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson J, Loh Z, Ullah MA, Lynch JP, Werder RB, Collinson N, Zhang V, Dondelinger Y, Bertrand MJ, Everard ML. Respiratory syncytial virus infection promotes necroptosis and HMGB1 release by airway epithelial cells. Am J Respir Crit Care Med. 2020;201:1358–1371. doi: 10.1164/rccm.201906-1149OC. [DOI] [PubMed] [Google Scholar]
- Sisinni A, Rossi L, Battista A, Poletti E, Battista F, Battista RA, Malagoli A, Biagi A, Zanni A, Sticozzi C. Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: the ASA-CARE study. Int J Cardiol. 2021;344:240–245. doi: 10.1016/j.ijcard.2021.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stilhano RS, Costa AJ, Nishino MS, Shams S, Bartolomeo CS, Breithaupt-Faloppa AC, Silva EA, Ramirez AL, Prado CM, Ureshino RP. SARS-CoV-2 and the possible connection to ERs, ACE2, and RAGE: Focus on susceptibility factors. FASEB J: Off Publ Fed Am Soc for Exp Biol. 2020;34:14103–14119. doi: 10.1096/fj.202001394RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street ME. HMGB1: a possible crucial therapeutic target for COVID-19? Horm Res Paediatr. 2020;93:73–7. doi: 10.1159/000508291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun J. The hypothesis that SARS-CoV-2 affects male reproductive ability by regulating autophagy. Med Hypotheses. 2020;143:110083. doi: 10.1016/j.mehy.2020.110083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang D, KanG R, Zeh HJ, III, Lotze MT. High-mobility group box 1, oxidative stress, and disease. Antioxid Redox Signal. 2011;14:1315–1335. doi: 10.1089/ars.2010.3356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S, Zhang L, Joseph J, Jiang X. Celastrol pretreatment attenuates rat myocardial ischemia/reperfusion injury by inhibiting high mobility group box 1 protein expression via the PI3K/Akt pathway. Biochem Biophys Res Commun. 2018;497:843–849. doi: 10.1016/j.bbrc.2018.02.121. [DOI] [PubMed] [Google Scholar]
- Tsushima K, King LS, Aggarwal NR, de Gorordo A, D'Alessio FR, Kubo K. Acute lung injury review. Intern Med. 2009;48:621–630. doi: 10.2169/internalmedicine.48.1741. [DOI] [PubMed] [Google Scholar]
- Utsunomiya R, Dai X, Murakami M, Masuda K, Okazaki H, Tsuda T, Mori H, Shiraishi K, Tohyama M, Sayama K. Heparinoid suppresses Der p-induced IL-1β production by inhibiting ERK and p38 MAPK pathways in keratinocytes. Exp Dermatol. 2018;27:981–988. doi: 10.1111/exd.13685. [DOI] [PubMed] [Google Scholar]
- Vincent J-L, Francois B, Zabolotskikh I, Daga MK, Lascarrou J-B, Kirov MY, Pettilä V, Wittebole X, Meziani F, Mercier E. Effect of a recombinant human soluble thrombomodulin on mortality in patients with sepsis-associated coagulopathy: the SCARLET randomized clinical trial. JAMA. 2019;321:1993–2002. doi: 10.1001/jama.2019.5358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel S, Bodenstein R, Chen Q, Feil S, Feil R, Rheinlaender J, Schäffer TE, Bohn E, Frick JS, Borst O, Münzer P, Walker B, Markel J, Csanyi G, Pagano PJ, Loughran P, Jessup ME, Watkins SC, Bullock GC, Sperry JL, Zuckerbraun BS, Billiar TR, Lotze MT, Gawaz M, Neal MD. Platelet-derived HMGB1 is a critical mediator of thrombosis. J Clin Invest. 2015;125:4638–4654. doi: 10.1172/JCI81660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Ward MF, Fan X-G, Sama AE, Li W. Potential role of high mobility group box 1 in viral infectious diseases. Viral Immunol. 2006;19:3–9. doi: 10.1089/vim.2006.19.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Yang R, Yuan B, Liu Y, Liu C. The antiviral and antimicrobial activities of licorice, a widely-used Chinese herb. Acta Pharm Sin B. 2015;5:310–315. doi: 10.1016/j.apsb.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Han Z, Fan Y, Zhang J, Chen K, Gao L, Zeng H, Cao J, Wang C. MicroRNA-9 inhibits NLRP3 inflammasome activation in human atherosclerosis inflammation cell models through the JAK1/STAT signaling pathway. Cell Physiol Biochem. 2017;41:1555–1571. doi: 10.1159/000470822. [DOI] [PubMed] [Google Scholar]
- Weerink MA, Struys MM, Hannivoort LN, Barends CR, Absalom AR, Colin P. Clinical pharmacokinetics and pharmacodynamics of dexmedetomidine. Clin Pharmacokinet. 2017;56:893–913. doi: 10.1007/s40262-017-0507-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyganowska-Swiatkowska M, Nohawica M, Grocholewicz K, Nowak G. Influence of herbal medicines on HMGB1 release, SARS-CoV-2 viral attachment, acute respiratory failure, and sepsis. A literature review. Int J Mol Sci. 2020;21:4639. doi: 10.3390/ijms21134639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang H, Hu B, Li Z, Li J. Dexmedetomidine controls systemic cytokine levels through the cholinergic anti-inflammatory pathway. Inflammation. 2014;37:1763–1770. doi: 10.1007/s10753-014-9906-1. [DOI] [PubMed] [Google Scholar]
- Yang N, Shen H-M. Targeting the endocytic pathway and autophagy process as a novel therapeutic strategy in COVID-19. Int J Biol Sci. 2020;16:1724–1731. doi: 10.7150/ijbs.45498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Huang C, Yang J, Jiang H, Ding J. Statins attenuate high mobility group box-1 protein induced vascular endothelial activation: a key role for TLR4/NF-κB signaling pathway. Mol Cell Biochem. 2010;345:189–195. doi: 10.1007/s11010-010-0572-9. [DOI] [PubMed] [Google Scholar]
- Yang H, Wang H, Wang Y, Addorisio M, Li J, Postiglione MJ, Chavan SS, Al-Abed Y, Antoine DJ, Andersson U. Expression of concern: the haptoglobin beta subunit sequesters HMGB 1 toxicity in sterile and infectious inflammation. J Intern Med. 2017;282:76–93. doi: 10.1111/joim.12619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Wang H, Andersson U. Targeting inflammation driven by HMGB1. Front Immunol. 2020;11:484. doi: 10.3389/fimmu.2020.00484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao D, Wang S, Wang M, Lu W. Renoprotection of dapagliflozin in human renal proximal tubular cells via the inhibition of the high mobility group box 1-receptor for advanced glycation end products-nuclear factor-κB signaling pathway. Mol Med Rep. 2018;18:3625–3630. doi: 10.3892/mmr.2018.9393. [DOI] [PubMed] [Google Scholar]
- Zeh HJ, Bahary N, Boone BA, Singhi AD, Miller-Ocuin JL, Normolle DP, Zureikat AH, Hogg ME, Bartlett DL, Lee KK. A randomized phase II preoperative study of autophagy inhibition with high-dose hydroxychloroquine and gemcitabine/nab-paclitaxel in pancreatic cancer patients. Clin Cancer Res. 2020;26:3126–3134. doi: 10.1158/1078-0432.CCR-19-4042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Zhang M, Wang C, Shen A. Ketamine alleviates LPS induced lung injury by inhibiting HMGB1-RAGE level. Eur Rev Med Pharmacol Sci. 2018;22:1830–1836. doi: 10.26355/eurrev_201803_14603. [DOI] [PubMed] [Google Scholar]
- Zhang S, Zhang Q, Wang F, Guo X, Liu T, Zhao Y, Gu B, Chen H, Li Y. Hydroxychloroquine inhibiting neutrophil extracellular trap formation alleviates hepatic ischemia/reperfusion injury by blocking TLR9 in mice. Clin Immunol. 2020;216:108461. doi: 10.1016/j.clim.2020.108461. [DOI] [PubMed] [Google Scholar]
- Zou W, He F, Liu S, Pu J, Hu J, Sheng Q, Zhu T, Zhu T, Li B, Ran P. PM2.5 induced the expression of fibrogenic mediators via HMGB1-RAGE signaling in human airway epithelial cells. Can Respir J. 2018;2018:1817398. doi: 10.1155/2018/1817398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou H, Yin J, Zhang Z, Xiang H, Wang J, Zhu D, Xu X, Cao Y. Destruction in maternal–fetal interface of URSA patients via the increase of the HMGB1-RAGE/TLR2/TLR4-NF-κB signaling pathway. Life Sci. 2020;250:117543. doi: 10.1016/j.lfs.2020.117543. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Enquiries about data availability should be directed to the authors.