INTRODUCTION
This article is the third in a dedicated series entitled ‘Spot the CLOT’, which aims to raise awareness of cancer-associated thrombosis (CAT) to improve patient and provider education, patient outcomes and, ultimately, reduce the burden of CAT. The first two articles, entitled ‘The significance of VTE in cancer: Introduction of the Spot the CLOT’ (Sardo et al., 2021) and ‘Spot the CLOT: What cancer patients want to know’ (Bayadinova et al., 2022) described CAT, the knowledge deficits of CAT in cancer patients, and strategies for raising awareness and educating patients diagnosed with cancer. The focus of this third article in the series is promoting awareness of CAT in healthcare providers. It will identify knowledge gaps among medical personnel, suggest tools for identifying patients at highest risk, and offer strategies and available resources for increasing awareness among providers.
GENERAL AWARENESS OF CAT IN HEALTHCARE PROVIDERS
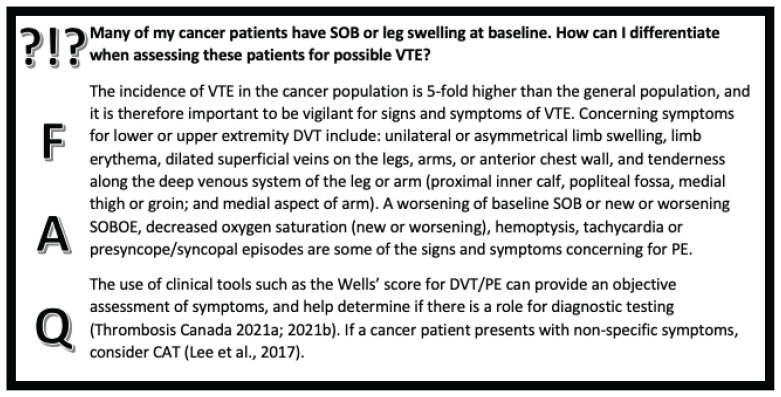
Despite the significant impact of CAT on patients and healthcare resources, there is a documented low awareness about CAT among healthcare providers (Baddeley et al., 2021; Noble et al., 2015). This may result in a delayed or missed diagnosis of venous thromboembolism (VTE), significantly impacting the cancer patient’s clinical course. Noble et al. (2015) described a significant knowledge deficit among physicians in the assessment and diagnosis of CAT. This knowledge deficit among healthcare providers was also noted by patients diagnosed with CAT because, despite presenting with classic signs and symptoms of VTE, other diagnoses were considered first (Noble et al., 2015). For example, a patient with unilateral leg swelling was continuously treated with escalating doses of diuretics with no improvement before a diagnosis of deep vein thrombosis (DVT) was considered. Similarly, a patient with shortness of breath and new onset chest pain was presumed to have pneumonia and was treated with antibiotics prior to the diagnosis of pulmonary embolism (PE) (Noble et al.,2015).
Similar knowledge deficits are evident in oncology nurses. A survey by Viale and Schwartz (2004), which evaluated the perceptions and knowledge of VTE in an outpatient cancer setting, was completed by 567 nurses. It is reassuring that the large majority (93%) of study participants agreed that DVT and/or PE were common, and potentially a serious complication in cancer patients. However, only 39% thought that a PE resulting from a DVT often causes death in cancer patients (Viale & Schwartz, 2004). More than half of the survey respondents did not think that cancer-associated thrombosis was underdiagnosed or undertreated (Viale & Schwartz, 2004). Furthermore, only 21% of the oncology nurses surveyed believed that nurses played an important role in the diagnoses of CAT, albeit a nurse practitioner was identified as the first contact for VTE concerns by an additional 19% (Viale & Schwartz, 2004). The lack of awareness that oncology nurses play an integral role in the diagnosis of CAT is concerning given the interdisciplinary team approach to cancer care, and the inherent trust that cancer patients place in their nurses.
The most common knowledge gaps identified by the oncology nurses who were surveyed included risk factors, prevention, and treatment of CAT (Viale & Schwartz, 2004). A more recent study by Lee et al. (2014) examined the perceived knowledge, as well as VTE assessment and prevention practices of inpatient nurses working in a variety of hospital settings, including oncology, medical, surgical, and critical care wards. The greatest barriers to nurses in carrying out VTE assessments were lack of time and lack of knowledge, each identified by 21% of respondents (Lee et al., 2014).
A study was also conducted among pharmacists in France, where 179 pharmacists completed a questionnaire assessing their understanding of the guidelines on the treatment of CAT and their application in practice (Rey et al., 2016). Only 4.5% of the respondents were aware of the existence of guidelines on the management of CAT (Rey et al., 2016). Forty-nine percent were able to identify the appropriate treatment strategy, and only 14% the proper treatment duration (Rey et al., 2016). Importantly, some of the learning needs that were self-identified in the group included general information about CAT and its management, the risk of recurrence, treatment duration, treatment side effects, and drug-drug and drug-food interactions (Rey et al., 2016).
An even more surprising finding was reported by Kakkar et al. (2020). The authors conducted a survey evaluating perceptions and clinical practices surrounding CAT, which was distributed to more than 5,000 oncologists worldwide who specifically treated patients with this diagnosis. Many of the answers on the survey were consistent with the current evidence based on CAT, which is not surprising, as the study participants likely encounter this diagnosis commonly in their practice. However, almost one-quarter of the respondents were not aware that the placement of a central venous catheter (CVC) increases the risk of VTE (Kakkar et al., 2020), although multiple studies have reported the incidence of upper extremity DVTs in patients with CVCs to be as high as 66% (Verso & Agnelli, 2016)! Similarly, Padbury et al. (2020) found that among 71 hematologists and oncologists, 25% and 45% were unable to correctly select direct oral anticoagulant therapy consistent with clinical guidelines for prophylaxis and treatment of CAT, respectively. And two-thirds of these participants rated their confidence in managing CAT between one and three on a five-point scale (five = high confidence) (Padbury et al., 2020). These findings demonstrate that there are knowledge deficits regarding CAT even among providers who treat patients with this diagnosis on a regular basis. It is somewhat reassuring that providers are aware and admit to knowledge gaps, suggestive of an opportunity and willingness for targeted CAT learning.
IDENTIFICATION OF HIGH RISK CANCER PATIENTS
Certain cancers predispose patients to a higher risk of developing CAT. The primary cancers with the highest rates of VTE include those of the pancreas, uterus, lung, stomach, kidneys, and brain (Abdol Razak et al., 2018). The type and stage of cancer, specifically the advanced cancer stage and cancer with metastatic disease, pose a higher risk for VTE. The initial three to six months after a cancer diagnosis represent the highest risk period (Abdol Razak et al., 2018; Falanga, 2009).
Specific cancer drugs or treatments may also predispose patients to VTE. Cancer-specific risk factors include chemotherapy, radiation therapy, use of CVCs, invasive procedures or surgeries, and hormone therapy. These cancer treatments, particularly those requiring hospitalization or imposing bedrest, all compound a patient’s risk of VTE (Abdol Razak et al., 2018; Pandhi et al., 2016). Some of the specific chemotherapy drugs that have been associated with an increased risk of endothelial injury and, therefore, thrombosis, are thalidomide, bevacizumab, and lenalidomide (Charalel & Vedantham, 2017).
TOOLS FOR RISK STRATIFICATION
Most cancer centres do not routinely screen for VTE risk. Reasons are likely multifactorial and may include limited resources in the outpatient setting, patients only having brief nursing encounters, and more recently, a trend towards virtual care (Hughes et al., 2022; Prip et al., 2018; Thorne et al., 2009). Depending on the practice environment, the nurse may be required to assess up to 30 patients in one working day with competing physical, diagnostic, psychosocial and prescriptive assessments expected at each visit. These may include measurement of vital signs, height and weight, venous access, Eastern Oncology Cooperative Group (ECOG) Status, Edmonton Symptom Assessment System (ESAS), medicine reconciliation updates, prescription renewal, and patient teaching (Azam et al., 2019; Green et al., 2017).
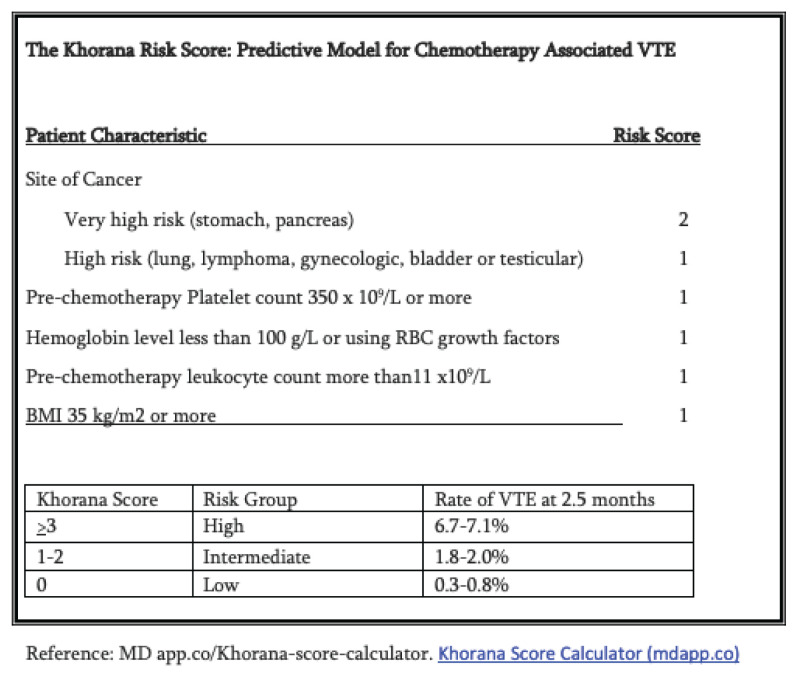
In order to include VTE risk assessment in routine clinical practice, assessment tools need to be valid, relevant and user friendly. Given that most CAT occurs in the outpatient setting, risk assessment tools may offer a strategy to determine VTE risk in outpatient oncology patients (Khorana et al., 2021). Objective assessment with the use of a tool can aid clinicians in overcoming limitations associated with subjective assessment alone. The original risk assessment model developed for identifying patients at risk for CAT was the 2008 Khorana Risk Score (KRS) (See Figure 1). This objective tool guides clinicians in identifying cancer patients at high VTE risk by isolating five predictive variables:
Figure 1.
Site of cancer (2 points for very high risk, 1 point for high risk)
Platelet count of 350 x 109/L or more (1 point)
Hb less than 100 g/L (10 g/dL) and/or use of erythropoiesis stimulating agents (1 point)
WBC of 11 x 109/L or more (1 point) and
BMI >35 (1 point)
A score of 2 or more on the KRS suggests significant VTE risk and may warrant close screening for symptoms typical of VTE (Khorana et al., 2008).
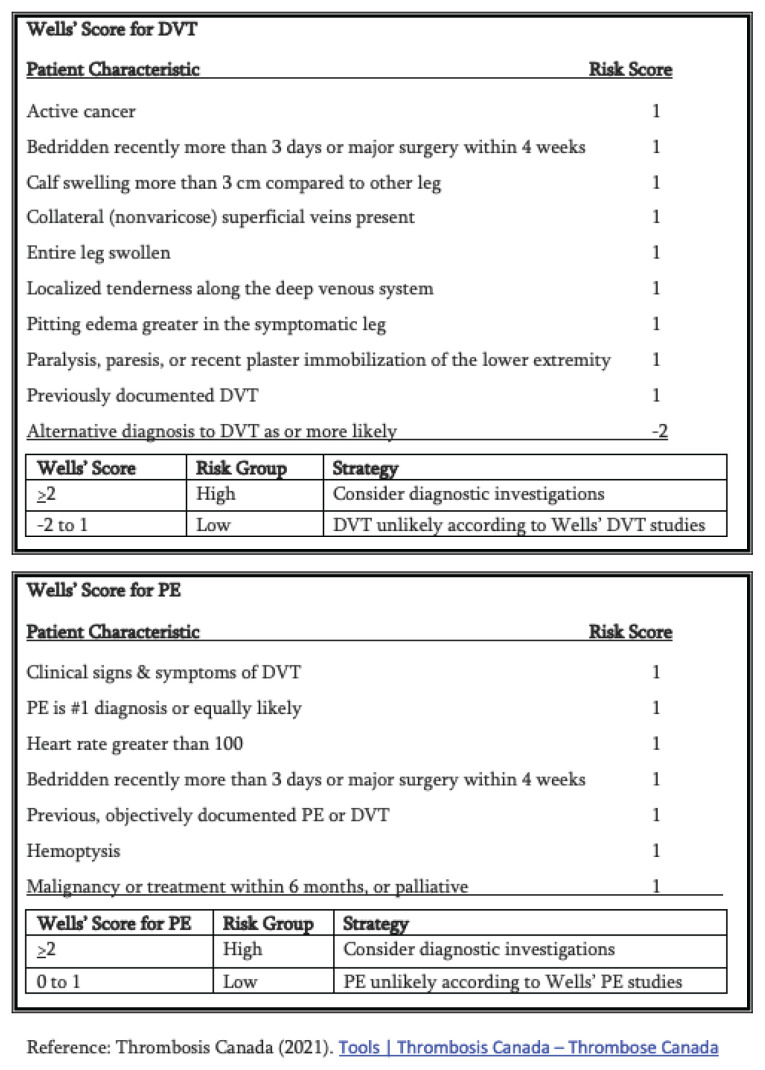
A second strategy to help determine VTE risk in the outpatient setting is the Wells’ score for DVT and PE (see Figure 2; Wells et al., 2000). The Wells’ score is a clinical assessment tool that incorporates both patient history (i.e., cancer or recent surgery) and clinical symptoms (i.e., tachycardia, tenderness along deep venous system of legs) into a risk score when VTE is suspected. A high Wells’ score suggests diagnostic assessment of symptoms including leg ultrasound or CTPA to rule out VTE disease (Wells et al., 2000). For centres with access to electronic medical records (EMRs), these risk assessment tools may be embedded into the nursing workflow sheets to allow for identification of high-risk patients. The ability to predict and screen for risk of VTE offers nurse clinicians added instruments in their toolkit for comprehensive oncology care.
Figure 2.
INTERVENTIONS FOR INCREASING AWARENESS OF CAT
Implementation of Risk Stratification in EMRs
Incorporating risk stratification tools into EMRs could be an effective strategy in increasing awareness of CAT, and alerting providers to consider objective investigations for patients at high risk for VTE. Kunapareddy et al. (2019), for example, implemented the KRS into the EMRs of ambulatory cancer patients. An alert was displayed for patients with a high KRS to each clinician opening the patient’s chart. Providers had the options of ignoring the alert, ordering a lower-extremity ultrasound, or repeating the risk stratification at a later date (Kunapareddy et al., 2019). Twelve and a half percent of the patients screened with ultrasound, as suggested by the high-risk alert, had a confirmed diagnosis of VTE. An additional 8.3% of the patients who were not screened with ultrasound presented with a symptomatic DVT and 4.5% with a PE within 90 days (Kunapareddy et al., 2019). Of the non-screened patients with confirmed DVT, 30.8% also had concomitant PE (Kunapareddy et al., 2019). These findings suggest that provider alerts may aid in the early identification of CAT and potentially prevent PEs if DVTs are identified and treated earlier.
Another study by Ades et al. (2017) that also implemented the KRS and Protecht score (another risk stratification tool by Verso et al., 2012) into the EMRs of ambulatory cancer patients with provider alerts for high-risk patients. Patient education on the topic of CAT increased from less than 5% before implementation to 84% during implementation, and an impressive 95% 15 months post implementation (Ades et al., 2017). All high-risk patients were offered a referral to a hematologist for the consideration of VTE prophylaxis and, ultimately, 86% of these patients were prescribed pharmacologic prophylaxis (Ades et al., 2017). This study demonstrates the significant impact that clinician alerts can have on raising provider awareness of CAT, improving patient education, and increasing considerations for VTE prophylaxis when appropriate.
Educational Strategies
A recent mixed-methods study by Baddeley et al. (2021) examined the impact of the implementation of a brief patient education video on CAT into clinical practice at a regional cancer centre. Key informant interviews were conducted with nine outpatient chemotherapy nurses to determine the impact of the video. One of the findings was that nurses considered CAT a low priority topic for patient education in those starting systemic anticancer therapy. There were three reasons identified behind this finding. The first is the nursing knowledge deficit regarding CAT. Despite knowing that patients are at a higher risk of thrombosis given their cancer diagnosis, most nurses were not aware of the reasons behind the higher risk, and were unable to quantify this risk (Baddeley et al., 2021). The second reason was that nurses prioritized educating patients on topics they thought were most important, including sepsis. In order to avoid overwhelming patients with information, CAT was often not discussed (Baddeley et al., 2021). Finally, CAT is often not mentioned in printed patient educational materials, or if mentioned, it appears at the end of this literature. Many nurses follow the educational materials when educating patients, and CAT therefore often gets missed (Baddeley et al., 2021). The video had a significant impact not only on the nurses’ knowledge, but also the prioritization of patient education regarding CAT. Many nurses were surprised at the magnitude of the risk of CAT, as well as its impact on morbidity and mortality (Baddeley et al., 2021). The implementation of the video resulted in nursing practice change where they started consistently including CAT into patient education sessions, as well as updating the patient literature to reflect the significance and seriousness of CAT.
Another study by Padbury et al. (2020) evaluated the impact on hematologists and oncologists of an educational session in a video format comprised of a roundtable discussion by CAT experts. The study assessed the participants’ knowledge and confidence in the management of CAT. Of the 71 participants, 27% demonstrated an improvement in the ability to identify appropriate thromboprophylaxis and treatment of CAT, and importantly, 44% of providers had an increase in their confidence in the management of CAT (Padbury et al., 2020).
Most nurses surveyed expressed preference for online education about VTE (Viale & Schwartz, 2004).
Resources for Healthcare Providers
There is a growing awareness of the need to address the barriers to recognizing and treating CAT (Monreal et al., 2019). Education to promote awareness, prevention, diagnosis, and treatment of CAT is imperative. The following websites are committed to providing evidence-based information and offer clinician resources on CAT.
Thrombosis Canada (https://thrombosiscanada.ca)
Thrombosis Canada is a Canadian charity with membership consisting of some of the top international thrombosis researchers without commercial bias. Their website has exceptional educational resources, treatment guidelines, and clinical tools for healthcare professionals to optimize CAT care, improve clinical outcomes, and prevent CAT mortality. There is a section dedicated specifically for increasing the awareness of CAT, providing customizable posters, patient education videos, and an accredited provider education program available at https://thrombosiscanada.ca/recognizing-cancer-associated-thrombosis/
In addition, a treatment algorithm for CAT, e-learning modules, patient resource library, and accredited educational programs are available at https://thrombosiscanada.ca/resourcepage/resources-2/, https://thrombosiscanada.ca/cancer-associated-thrombosis-patient-resource-library/et https://thrombosiscanada.ca/catguidelines2020/
International Society of Thrombosis and Haemostasis (https://www.isth.org/)
The International Society of Thrombosis and Haemostasis (ISTH) is an international organization consisting of some of the world experts in the fields of thrombosis and hematology. The ISTH Academy offers an accredited course, entitled ‘Cancer-Associated Thrombosis’, available at: https://academy.isth.org/isth/2019/cancer-associated-thrombosis/286356/session.speakers.html
CONCLUSION
VTE is a common and serious complication in cancer patients, being the leading cause of morbidity and second leading cause of mortality (Noble et al., 2015). Despite its significance, however, the awareness of CAT is low not only in patients and caregivers, but also, concerningly, healthcare providers. Some studies have shown that healthcare provider education is effective in increasing the awareness of CAT. Some of the self-identified learning gaps include the general overview of CAT, including its risk factors and prevention strategies, as well as treatment recommendations, including specific drugs, duration of treatment, and drug interactions. This third article in the ‘Spot the CLOT’ series offers resources for increasing provider awareness of CAT with the goal of more effective prevention strategies, more timely diagnosis and, ultimately, reducing the burden of this disease.
ACKNOWLEDGEMENT
The authors would like to thank LEO Pharma for encouragement to write a series on this important topic. Disseminated education can help increase awareness of VTE in the cancer population. LEO Pharma did not contribute or influence intellectual content, however, did support the CONJ for translation services.
REFERENCES
- Abdol Razak NB, Jones G, Bhandari M, Berndt MC, Metharom P. Cancer-associated thrombosis: An overview of mechanisms, risk factors, and treatment. Cancers. 2018;10:380. doi: 10.3390/cancers10100380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ades S, Gilchrist S, Holm A, Libby K, Cushman M, Douce D, Holmes CE. Venous thromboembolism prevention in the ambulatory cancer clinic (VTE-PACC): A systems-based, personalized, multidisciplinary program to increase venous thromboembolism (VTE) risk assessment, education and anticoagulant prophylaxis in cancer outpatients initiating therapy. Blood. 2017;130(Suppl 1):217. doi: 10.1182/blood.V130.Suppl_1.217.217. [DOI] [Google Scholar]
- Azam F, Latif M, Farooq A, Tirmazy S, AlShahrani S, Bashir S, Bukhari N. Performance status assessment by using ECOG (Eastern cooperative oncology group) score for cancer patients by oncology healthcare professionals. Case Reports in Oncology. 2019;12(3):728–736. doi: 10.1159/000503095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baddeley E, Torrens-Burton A, Newman A, Nelson A, Pease N, Nelson R, Noble S. A mixed-methods study to evaluate a patient-designed tool to reduce harm from cancer-associated thrombosis: The EMPOWER study. Research and Practice in Thrombosis and Haemostasis. 2021;5(5):e12545. doi: 10.1002/rth2.12545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayadinova JA, Sardo LA, Higgins-Nogareda V, Scott J, MacKinnon B. « Prévenir la thrombose »: Ce que veulent savoir les patients atteints de cancer. Revue canadienne de soins infirmiers en oncologie, 2022;32(1):151–156. [PMC free article] [PubMed] [Google Scholar]
- Charalel RA, Vedantham S. Deep vein thrombosis interventions in cancer patients. Seminars in Interventional Radiology. 2017;34(1):50–53. doi: 10.1055/s-0036-1597763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falanga A. The incidence and risk of venous thromboembolism associated with cancer and nonsurgical cancer treatment. Cancer Investigation. 2009;27:105–119. doi: 10.1080/07357900802563028. [DOI] [PubMed] [Google Scholar]
- Green E, Yuen D, Chasen M, Amernic H, Shabestari O, Brundage M, Krzyzanowska M, Klinger C, Ismail Z, Pereira J. Oncology nurses’ attitudes toward the Edmonton symptom assessment system: Results from a large cancer care Ontario study. Oncology Nursing Forum. 2017;44(1):116–125. doi: 10.1188/17.ONF.116-125. [DOI] [PubMed] [Google Scholar]
- Hughes L, Petrella A, Phillips N, Taylor RM. Virtual care and the impact of COVID-19 on nursing: A single centre evaluation. Journal of Advanced Nursing. 2022;78(2):498–509. doi: 10.1111/jan.15050. https://doi.org.libaccess.lib.mcmaster.ca/10.1111/jan.15050 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakkar AK, Bauersachs R, Falanga A, Wong J, Kayani G, Kahney A, Hughes R, Levine M. Fundamental Research in Oncology and Thrombosis 2 (FRONTLINE 2): A follow-up survey. The Oncologist. 2020;25(7):e1091–e1097. doi: 10.1634/theoncologist.2019-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francie CW. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood. 2008;111(10):4902–4907. doi: 10.1182/blood-2007-10-116327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khorana AA, DeSancho MT, Liebman H, Rosovsky R, Connors JM, Zwicker J. Prediction and prevention of cancer-associated thromboembolism. Oncologist. 2021;26(1):e2–e7. doi: 10.1002/onco.13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunapareddy G, Switzer B, Jain P, Conces M, Chen YW, Patel B, Patel S, Pinnamaneni P, Pohlman B, Angelini DE, McCrae KR, Khorana AA. Implementation of an electronic medical record tool for early detection of deep vein thrombosis in the ambulatory oncology setting. Research and Practice in Thrombosis and Haemostasis. 2019;3(2):226–233. doi: 10.1002/rth2.12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A, Carrier M, Bouzianne A, Carignan M, DeCarolis M, Fournier C, Habert J, Kavan P, Smith R. Recognizing cancer-associated thrombosis: Provider education program PPT. Thrombosis Canada. 2017 https://thrombosiscanada.ca/recognizingcancer-associated-thrombosis/ [Google Scholar]
- Lee J-A, Grochow D, Drake D, Johnson L, Reed P, van Servellen G. Evaluation of hospital nurses’ perceived knowledge and practices of venous thromboembolism assessment and prevention. Journal of Vascular Nursing. 2014;31(1):18–24. doi: 10.1016/j.jvn.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Monreal M, Calleja Hernandez MA, Easaw JC, Elalamy I, Young A, Bang Jespersen L, Balthazar-Christensen V, Domecq G, Manzanera J, Bachman M, Kendall V, Borget I, Matzdorf A. Cancer-associated thrombosis (CAT), a neglected cause of cancer death: Actions needed to increase health outcomes and reduce mortality: Report summarizing the findings of an Expert Steering Group meeting in Belgium. 2019 https://ecpc.org/wp-content/uploads/2019/08/ECPCWhite-Paper-Cancer-Associated-Thrombosis-1.pdf. [Google Scholar]
- Noble S, Prout H, Nelson A. Patients’ experiences of living with cancer-associated thrombosis: The PELICAN study. Patient Preference and Adherence. 2015;9:337–345. doi: 10.2147/PPA.S79373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padbury C, Harris M, LaCouture M, Spyropolous J. Success of online CME at improving knowledge and confidence around guideline-directed management of cancer-associated thrombosis. Blood. 2020;136(Suppl 1):13. doi: 10.1182/blood-2020-137153. [DOI] [Google Scholar]
- Pandhi MB, Desai KR, Ryu RK, Lewandowski RJ. The role of inferior vena cava filters in cancer patients. Seminars in Interventional Radiology, 2016;33(2):71–74. doi: 10.1055/s-0036-1581090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prip A, Moller K, Nielsen D, Jarden M, Olsen M, Danielsen A. The patient-healthcare professional relationship and communication in the oncology outpatient setting: A systematic review. Cancer Nursing. 2018;41(5):E11–E22. doi: 10.1097/NCC.0000000000000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey JB, Jovenin N, Kreit P, Sicard J, Parent D, Hettler D, Nguyen P, Ducrocq JL. Venous thromboembolism: What pharmacists know? What do they need? Journal of Oncology Pharmacy Practice: Official Publication of the International Society of Oncology Pharmacy Practitioners. 2016;22(1):135–141. doi: 10.1177/1078155214560639. [DOI] [PubMed] [Google Scholar]
- Sardo LA, Bayadinova JA, Jenkins S, Penton L. Importance de la thromboembolie veineuse liée au cancer: Premier article de la série « Prévenir la thrombose ». Revue canadienne de soins infirmiers en oncologie, 2021;31(4):504–507. [PMC free article] [PubMed] [Google Scholar]
- Thorne SE, Hislop TG, Stajduhar K, Oglov V. Time-related communication skills from the cancer patient perspective. Psycho-Oncology. 2009;18:500–507. doi: 10.1002/pon.1418. [DOI] [PubMed] [Google Scholar]
- Thrombosis Canada. Wells’ criteria for pulmonary embolism/PE. 2021a https://thrombosiscanada.ca/tools/?calc=wellsPE . [Google Scholar]
- Thrombosis Canada. Wells’ criteria for deep vein thrombosis/DVT. 2021b https://thrombosiscanada.ca/tools/?calc=wellsDVT . [Google Scholar]
- Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. Journal of Clinical Oncology. 2016;21(19):3665–3675. doi: 10.1200/JCO.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Verso M, Agnelli G, Barni S, Gasparini G, LaBianca R. A modified Khorana risk assessment score for venous thromboembolism in cancer patients receiving chemotherapy: The Protecht score. Internal and Emergency Medicine. 2012;7(3):291–292. doi: 10.1007/s11739-012-0784-y. [DOI] [PubMed] [Google Scholar]
- Viale PH, Schwartz RN. Venous thromboembolism in patients with cancer part I: Survey of oncology nurses’ attitudes and treatment practices for ambulatory settings. Clinical Journal of Oncology Nursing. 2004;8(5):455–461. doi: 10.1188/04.CJON.455-461. [DOI] [PubMed] [Google Scholar]
- Wells PS, Anderson DR, Ginsberg J. Assessment of deep vein thrombosis or pulmonary embolism by the combined use of clinical model and noninvasive diagnostic tests. Seminars in Thrombosis and Hemostasis. 2000;26(6):643–656. doi: 10.1055/s-2000-13219. [DOI] [PubMed] [Google Scholar]