With great interest, we read the recent article by Whebell and colleagues [1] and were appealed by the beneficial effect of extracorporeal membrane oxygenation (ECMO) on survival in patients affected by acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19). The gratifyingly low mortality rate in this ECMO cohort (25.8%) stands in remarkable contrast to other reports in COVID-19 patients [2]. Such excellent results are attributable to (1) very strict selection criteria to reduce candidate eligibility to those with the absolute best chances, resulting in cohort of young patients [46 (39–52) years] with isolated respiratory failure [Sequential Organ Failure Assessment (SOFA) 5 (4–7)] and little to no comorbidities [frailty scale 2 (1-2)]; (2) excellent clinical expertise provided by specialized ARDS/ECMO centers. However, analogous to the Cesar-trial [3] discussion 12 years ago, insights of the present study are similarly hampered by the unpredictable bias introduced through the comparison of highly experienced ARDS centers with peripheral, less experienced hospitals [4] making an assessment of the pure ECMO effect difficult to estimate.
From a more technical point, we were wondering if the matching strategy applied is indeed reasonable to answer the question of interest. In general, matching based on the propensity score attempts to eliminate the effect of any given selection bias that might have led to treatment assignment by correcting for all relevant observed confounders, thus leading to an unbiased treatment effect estimate. However, in this study, patients in both the intervention and control cohort were treated contemporarily in the same set of centers following a systematic clinical evaluation by the same set of physicians. Given that matching on all relevant observed confounders resulted in two almost identical cohorts at the time-point of ECMO evaluation, the question arises why some patients, given identical characteristics, received ECMO and the others did not. Only the presence of a major, treatment defining, unobserved confounder could explain this difference in treatment assignment, inevitably impeding unbiased causal treatment effect estimation (Fig. 1).
Fig. 1.
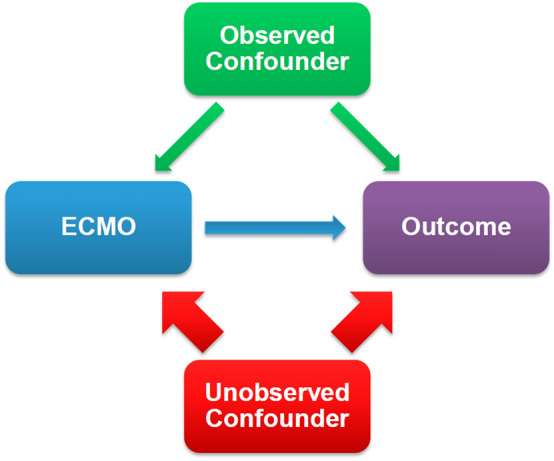
Directed acyclic graph depicting the causal effect of ECMO on patient outcome and the causal effect modulation by observed and unobserved confounders
Therefore, we are left pondering how the decision to withhold ECMO to some of these rather young COVID-19 patients with a fair probability of survival was reasoned. Was the limited availability of devices and/or beds in intensive care unit (ICU) on the specialized units the primary motivator for this decision? Having two almost identical cohorts in which solely the availability of resources led to therapeutic “stratification” would be of great interest from a scientific point of view. Indeed this kind of “randomization” would avoid many of the well-known difficulties and biases introduced by the high cross-over rates in randomized trials before [5].
Finally, this study underlines the ethical conundrum associated with ECMO withholding in ARDS patients with similar baseline characteristics, given (particularly in a pandemic) a setting of limited resource availability. How can we possibly argue for a restricted use of this potentially lifesaving organ-support modality in 2022, knowing the high chance of survival benefit associated with it in a rescue situation?
Declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Whebell S, Zhang J, Lewis R, Berry M, Ledot S, Retter A, Camporota L. Survival benefit of extracorporeal membrane oxygenation in severe COVID-19: a multi-centre-matched cohort study. Intensive Care Med. 2022 doi: 10.1007/s00134-022-06645-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbaro RP, MacLaren G, Boonstra PS, Combes A, Agerstrand C, Annich G, Diaz R, Fan E, Hryniewicz K, Lorusso R, Paden ML, Stead CM, Swol J, Iwashyna TJ, Slutsky AS, Brodie D. Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the international Extracorporeal Life Support Organization Registry. Lancet. 2021;398:1230–1238. doi: 10.1016/S0140-6736(21)01960-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, Hibbert CL, Truesdale A, Clemens F, Cooper N, Firmin RK, Elbourne D. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 4.Zwischenberger JB, Lynch JE. Will CESAR answer the adult ECMO debate? Lancet. 2009;374:1307–1308. doi: 10.1016/S0140-6736(09)61630-5. [DOI] [PubMed] [Google Scholar]
- 5.Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, Da Silva D, Zafrani L, Tirot P, Veber B, Maury E, Levy B, Cohen Y, Richard C, Kalfon P, Bouadma L, Mehdaoui H, Beduneau G, Lebreton G, Brochard L, Ferguson ND, Fan E, Slutsky AS, Brodie D, Mercat A. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]


