Abstract
Sporotrichosis is an important subcutaneous mycosis with high prevalence and threat to human and animal health worldwide. Sporothrix schenckii, Sporothrix brasiliensis, and Sporothrix globosa are the main etiological agents of this disease; and even though many efforts have been made recently to understand the Sporothrix-host interaction, little is known about S. globosa, an underestimated species. This organism shows the lowest virulence among the members of the Sporothrix pathogenic clade and represents an important pathogenic agent due to its global distribution. Here, we offer a review with all the known information about S. globosa, including its genome and proteomic information, and compare it with S. schenckii and S. brasiliensis, to explain the differences observed among these species, in terms of virulence, the host immune response, and the antifungal sensitivity. Also, we provide the gene prediction of some S. globosa putative virulence factors.
Keywords: antifungal drugs, fungal infection, host–fungus interplay, epidemiology, diagnosis, treatment
Introduction
Sporotrichosis is a human and animal fungal infection that affects the epidermis and subcutaneous tissues, having as etiological agent members of the Sporothrix genus.1–3 The classical infection route is the traumatic conidia implantation when interacting with decaying vegetal tissues, thus it is considered as a sapronosis.1 However, epidemic sporotrichosis outbreaks of domestic animals, in the last years, have revealed that the fungus can be transmitted by close contact between infected animals and human beings, and thus is now considered as a zoonosis too.4–6 The Sporothrix genus currently contains at least 51 species and phylogenetic analyses have grouped them within different clades, from which the pathogenic clade contains most of the sporotrichosis etiological agents: Sporothrix schenckii, Sporothrix brasiliensis, Sporothrix globosa, and Sporothrix luriei.7 The first three species are the most common ones associated with the disease, and S. schenckii was described and recognized as the causative agent of the disease more than a century ago, and thus it is currently the most studied species of the Sporothrix pathogenic clade.1,3 S. brasiliensis has attracted attention in recent years because of the zoonotic outbreaks in Brazil, and most recently in Argentina,1,8,9 affecting both domestic cats and human beings.8,10 In the case of S. globosa, the species has been recently associated with both sapronotic and zoonotic outbreaks in Asia, and to a lesser extent in some parts of America.11–13 This organism is the most underestimated and poorly study Sporothrix species; and thus far, no review papers dealing with both its basic and clinical aspects are available in the scientific literature. Therefore, in this review, we focused on highlighting the similarities and differences of S. globosa with other medically relevant Sporothrix species, in terms of basic biological aspects, clinical manifestations, diagnosis, and infection treatment.
Fundamental Aspects of Sporothrix globosa
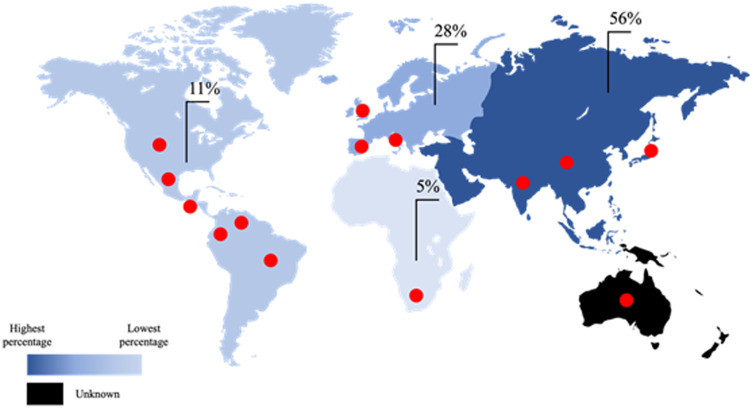
Although S. globosa is considered a cosmopolitan species, there are geographical areas where it is most frequently isolated, with a prevalence rate of 56% in Asia (China, India, and Japan), where it represents 99.3% of the total Sporothrix species in this region, 28% in Europe (Spain, Italy, and United Kingdom), 11% in America (Brazil, United States, Venezuela, Guatemala, Colombia, and Mexico), and 5% in Africa (South Africa) (Figure 1).13–18 It has also been reported that all the strains found in India so far belong to S. globosa, and it is the second main species found in Australia.19,20
Figure 1.
Geographic distribution of Sporothrix globosa isolates. This species is mainly found in Asia (China, India, and Japan), followed by Europe (Spain, Italy, and United Kingdom), America (Brazil, United States, Venezuela, Guatemala, Colombia, and Mexico), and Africa (South Africa). The red dots indicate the countries where S. globosa has been isolated.
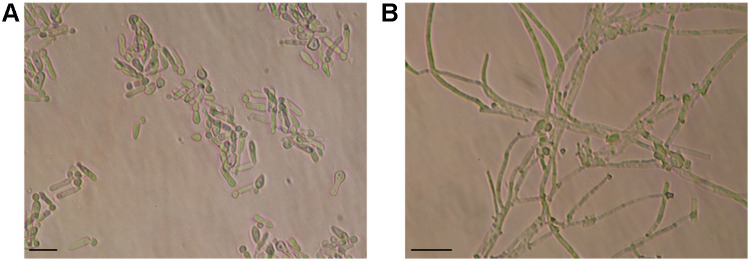
Like other medically relevant Sporothrix species, S. globosa is a thermodimorphic fungus that in vitro grows as conidium-producer hypha at 25°C, and this is regarded as the saprophytic phase found in the environment; while the yeast-like phase grows in vitro at 37°C and is considered the parasitic morphology found in the host tissues.1 S. schenckii, S. brasiliensis, and S. globosa have a similar conidial morphology when grown in the potato-dextrose-agar medium at 30°C, where terminal or intercalary on differentiated conidiophores conidiogenous cells are observed, and these may be of two kinds: sympodial conidia, which are usually hyaline to sub-hyaline, obovoidal and 2–5-µm-long by 1–3-µm-wide cells; and sessile conidia that are brown to dark brown, thick-walled, globose to subglobose, and 2.5–4-µm-long by 2–3.5-µm-wide cells (Figure 2).16,20,21 However, unlike S. schenckii and S. brasiliensis that display normal growth at temperatures up to 37°C, S. globosa has shown to decrease in growth rate as the temperature increases, as demonstrated by the mean colony diameter of 16–42 mm at 30°C, 3–15 mm at 35°C, and with very limited growth at 37 °C for most S. globosa isolates, with colony sizes ranging from 1.5 to 5.5 mm in diameter.13,16,18,22 The macroscopic morphologies of all three species, regardless of the culture medium, are also very similar, with creamy filamentous colonies, some of them darker to brown or black, oval or orbed with milky membranous edge and wrinkled surface.16,18 In the case of the fungal growth as yeast-like cells, S. globosa cultured in brain-heart-infusion at 37°C grows like elongated, cigar-shaped or globose hyaline budding yeast cells, measuring about 5–7 µm long and 1–3 µm wide (Figure 2), whereas colonies are moist, glabrous, and with a light brown color,20,23 similar to S. schenckii and S. brasiliensis grown under the same conditions.
Figure 2.
Microscopic morphology of Sporothrix globosa growing in the yeast–peptone–dextrose medium for 4 days. (A) Yeast-like cells growing at 35°C and pH 7.8, with the typical elongated cigar shape. (B) Mycelium growing at 28°C and pH 4.5, with globose conidia and branching septate hyphae. Scale bars = 10 µm.
Since S. globosa morphology is similar to other Sporothrix species, this phenotypical trait is useless for identification purposes. However, some biochemical parameters can help in species identification. One of them is the carbohydrate assimilation, such as sucrose, ribitol, and raffinose, which is different among the medically relevant Sporothrix species: S. globosa has positive assimilation to sucrose and ribitol, and negative assimilation to raffinose; S. schenckii has positive assimilation for the three sugars; and S. brasiliensis has negative assimilation to sucrose and raffinose, and positive assimilation to ribitol.16,20 These zymogram profiles are considered a tool for preliminary taxonomical identification, and molecular techniques are required for species confirmation, as discussed in the following sections.
The genome of two S. globosa strains has been sequenced and assembled, but not annotated. One strain was isolated from a facial lesion in Spain (CBS 120340) and the other was isolated from a Chinese patient with itraconazole-resistant sporotrichosis (SS01).24 Both strains had similar results, with an estimated genome size of 33,473,551 and 33,493,113 bp with a G+C content of 54.37%, 7760, and 7719 predicted genes, respectively, and a total of 126 putative tRNA genes decoding 20 standard amino acids.25 The mitochondrial genomes from the two strains were also very similar, consisting of a circular DNA of 26,288 and 26,672 bp, for CBS 1203740 and SS01, respectively, 44 unique genes subdivided in 24 tRNAs, 17 protein-coding genes, 2 rRNAs, and the rpnB gene that encodes for the RNA subunit of the RNaseP, a ribozyme responsible for tRNA maturation.26 In addition, both S. globosa mitochondrial genomes are similar and have synteny with S. schenckii ATCC MYA-4821 (26,572 bp), and are smaller than that of S. brasiliensis ATCC MYA-4823 (36,054 bp).27–29 Through in silico comparative genome analysis of the Sporothrix pathogenic species, it was found that S. schenckii, S. brasiliensis and S. globosa share 86–96% of genomic synteny, while the less virulent S. pallida species shares only 13%.30 In addition, it was observed that S. brasiliensis, S. globosa, S. pallida and S. schenckii have 8715, 8983, 9845 and 8719 genes, respectively, with a similarity of 80–100% among the most virulent species S. schenckii, S. brasiliensis and S. globosa, and only of 40% for S. pallida.30 When virulence associated genes were predicted using the pathogen–host interaction database, it was found that S. brasiliensis, S. schenckii, S. globosa, and S. pallida have a similar number of virulence genes in their genomes, with 1650, 1699, 1758 and 2020 genes, respectively, and most of these were cell wall associated genes, extracellular domains, stress response genes, iron acquisition genes, proteases and cell signalling molecules.30
Although the S. schenckii, S. brasiliensis, and S. globosa genome sequences are available, genomic, transcriptomic, and metabolomic comparative analyses are scarce and required to understand the molecular bases of the phenotypical differences shown by S. globosa. Sporothrix species have different levels of virulence and antifungal susceptibilities, which will be also further discussed, and these might be explained by molecular polymorphisms.31,32
S. schenckii undergoes recombination in nature, showing a high degree of genetic variability in its population, which has not been observed in S. brasiliensis, where the isolates from a feline outbreak are mainly clonal, conforming a homogenous population, which does not exclude the absence of sexual reproduction but does indicate the emergence of a successful genotype15,24,33 Regarding S. globosa, this species is also considered to have a low degree of genetic variation,15,24 but some molecular studies suggest the existence of a sexual state, since the MAT1-1 and MAT1-2 genes, which are essential for sexual reproduction, were found within this species genome.34 However, additional analyses of these genes are required to determine the teleomorphs existence. It is also suggested that S. globosa and S. brasiliensis are clonal offshoots that differentiated from a common ancestor shared with S. schenckii, a hypothesis generated by phylogenetic analyses and genetic diversity using the calmodulin encoding gene sequences.35 On the other hand, recent phylogenetic studies, discriminatory AFLP markers analysis and mating-type analysis from human, animal and environmental isolates suggest that S. schenckii, S. brasiliensis and S. globosa are closely related taxonomic entities with strong genetic introgression that come from a single ancestor,7,22,36 being S. brasiliensis and S. schenckii sister species from a clade that is sister to S. globosa.36
The S. schenckii and S. brasiliensis cell walls have been thoroughly studied and it is known that chitin is found in the inner layer, followed by β-1,3- and β-1,6-glucans surrounded by peptidorhamnomannan fibrils in the outer layer.26,37,38 The S. globosa cell wall composition is not well studied, but it has been reported that it shows lower rhamnose, mannose, and O- and N-linked glycans content than S. schenckii and S. brasiliensis, but similar levels of glucosamine.32 Moreover, it was also observed that even when S. globosa was grown under carbon and nitrogen limitation, the cell wall rhamnose, glucose, glucosamine, and mannose content did not change, at a difference of S. schenckii and S. brasiliensis, suggesting species-specific metabolic plasticity.39 In addition, S. globosa showed a higher β-1,3-glucan exposure at the cell surface,32,40 which might be an advantage for the host’s immunity.
The proteome of these three main species has been studied, which may also explain the differences in virulence among them. From 247 proteins identified, 137 were found to be differentially expressed among the three species, and most of them were related to the carbohydrate and amino acid metabolism, and the stress response.41 Eight of the 10 enzymes involved in the glycolytic pathway (except phosphofructokinase-1 and phosphoglycerate mutase) were identified in S. schenckii, S. brasiliensis, and S. globosa, and seven of them (pyruvate kinase, fructose-bisphosphate aldolase, enolase, triosephosphate isomerase, glucose-6-phosphate isomerase, phosphoglycerate kinase, and glyceraldehyde 3 phosphate dehydrogenase) were upregulated in S. schenckii and S. globosa.41 In S. brasiliensis, three alcohol dehydrogenases were identified, while only two were found in S. schenckii and S. globosa.41 The enzyme pyruvate dehydrogenase E2 component dihydrolipoamide acetyltransferase, part of the pyruvate dehydrogenase complex, and the aconitate hydratase, malate dehydrogenase, citrate synthase, and fumarate hydratase, enzymes of the tricarboxylic acid cycle, were expressed by the three species, although with a higher abundance in S. schenckii and S. globosa. E1 and E2 proteins of the 2-oxoglutarate dehydrogenase complex were also found, but the first protein only in S. brasiliensis and the second in both S. brasiliensis and S. schenckii, while proteins such as thiamine biosynthetic enzyme, 6-phosphogluconate dehydrogenase, transaldolase, transketolase, and a UDP-N-acetylglucosamine pyrophosphorylase were found to be overexpressed in S. schenckii and S. globosa. On the other hand, glycosyl hydrolases like β-glucosidase, endo-1,3(4)-glucanase, and 1,3-β-glucosidase; the 4-hydroxyphenylpyruvate dioxygenase, metallopeptidase MepB, peptide-methionine (S)-S-oxide reductase, Xaa-Pro aminopeptidase, dipeptidyl-peptidase III, urease, and the trehalose synthase were found only or with higher abundance in S. brasiliensis.41 In the case of S. globosa, the three enzymes related to the lipid metabolism were downregulated, while the diphosphomevalonate decarboxylase was upregulated in S. brasiliensis and S. schenckii. The three Sporothrix species express enzymes involved in the oxidative stress response (catalase, superoxide dismutase, and peroxidase), but these were found upregulated in S. globosa.41 Finally, some heat shock proteins (chaperonin GroES, heat shock 70 kDa protein, molecular chaperone HtpG, and heat shock 70 kDa protein 18) were found to be downregulated in S. brasiliensis, but upregulated in S. schenckii and S. globosa.41 These proteomic differences suggest that S. brasiliensis metabolism is different from that of S. schenckii and S. globosa, which might explain the species-specific virulence.
Virulence Factors
Many Sporothrix spp. pathogenic aspects are unknown, and only a few virulence factors in S. schenckii and S. brasiliensis have been experimentally demonstrated. For S. globosa, the information in this regard is even more scarce, being this an opportunity area to expand our limited knowledge on this organism. In this section, the already known S. globosa virulence factors are discussed and others will be hypothesized, based on the genomic comparison with other Sporothrix species and with Candida albicans and Aspergillus fumigatus, two opportunistic fungal pathogens associated with high morbidity and mortality rates (Table 1).42
Table 1.
Genes Encoding for Putative Virulence Factors in Sporothrix globosa
| Putative Function | S. globosa Genomic Region | Best Hit | Similarity (%) | Coverage (%) | Ortholog in S. schenckii | Ortholog in S. brasiliensis |
|---|---|---|---|---|---|---|
| Dimorphism | ||||||
| Hyphal G cyclin 1 | Sequence ID: LVYW01000001.1 Range: 1,025,425 to 1,026,504 |
A. fumigatus G1/S-specific cyclin Cln1s | 67 | 87 | Yes | Yes |
| Cell wall synthesis | ||||||
| Chitin synthase | Sequence ID: LVYW01000005.1 Range: 1,866,742 to 1,869,543 |
A. fumigatus chitin synthase A | 73 | 95 | Yes | Yes |
| Sequence ID: LVYW01000004.1 Range: 3,601,706 to 3,604,024 |
A. fumigatus chitin synthase B | 83 | 75 | Yes | Yes | |
| Sequence ID: LVYW01000001.1 Range: 1,933,042 to 1,935,999 |
A. fumigatus chitin synthase F | 75 | 91 | Yes | Yes | |
| Sequence ID: LVYW01000004.1 Range: 659,665 to 662,220 |
A. fumigatus chitin synthase G | 77 | 97 | Yes | Yes | |
| β-1,3-Glucanosyltransferase | Sequence ID: LVYW01000002.1 Range: 622,419 to 627,869 |
A. fumigatus 1,3-β-glucan synthase catalytic subunit FksP | 85 | 94 | Yes | Yes |
| Dolichol phosphate synthase | Sequence ID: LVYW01000004.1 Range: 4,120,034 to 4,120,861 |
A. fumigatus dolichol phosphate mannosyl-transferase | 77 | 100 | Yes | Yes |
| Protein mannosyltransferase | Sequence ID: LVYW01000002.1 Range: 3,642,281 to 3,643,684 |
A. fumigatus protein O-mannosyl-transferase | 82 | 93 | Yes | Yes |
| Sequence ID: LVYW01000006.1 Range: 1,823,756 to 1,826,095 |
A. fumigatus protein mannosyl-transferase Pmt1 | 71 | 93 | Yes | Yes | |
| α-1,2-Mannosyltransferase | Sequence ID: LVYW01000005.1 Range: 2,631,677 to 2,632,711 |
A. fumigatus α-1,2-mannosyl-transferase (Kre2) | 81 | 80 | Yes | Yes |
| Sequence ID: LVYW01000001.1 Range: 1,590,849 to 1,591,889 |
A. fumigatus α-1,2-mannosyltransferase (Ktr4) | 77 | 87 | Yes | Yes | |
| Sequence ID: LVYW01000003.1 Range: 48,707 to 49,552 |
A. fumigatus α-1,2-mannosyl-transferase (Kre5) | 86 | 100 | Yes | Yes | |
| α-1,6-Mannosyltransferase | Sequence ID: LVYW01000002.1 Range: 3,966,407 to 3,967,531 |
A. fumigatus glycosyl-transferase Och1 | 65 | 82 | Yes | Yes |
| Sequence ID: LVYW01000005.1 Range: 2,421,530 to 2,422,483 |
A. fumigatus α1,6-mannosyl-transferase Mnn9 | 80 | 80 | Yes | Yes | |
| Thermotolerance | ||||||
| Suppresses thermotolerance and modulates capsule formation | Sequence ID: LVYW01000005.1 Range: 1,893,011 to 1,894,318 |
A. fumigatus cAMP-dependent protein kinase-like Sch9 | 86 | 99 | Yes | Yes |
|
Heat shock transcription factor |
Sequence ID: LVYW01000002.1 Range: 2,640,249 to 2,642,180 |
A. fumigatus heat shock transcription factor Hsf1 | 49 | 65 | Yes | Yes |
|
Heat shock-induced protein |
Sequence ID: LVYW01000005.1 Range: 1,292,334 to 1,294,616 |
A. fumigatus heat shock protein/chaperonin Hsp78 | 84 | 92 | Yes | Yes |
|
Invasin, member of Hsp70 |
Sequence ID: LVYW01000002.1 Range: 3,289,290 to 3,291,185 |
A. fumigatus molecular chaperone Hsp70 | 94 | 90 | Yes | Yes |
| Sequence ID: LVYW01000003.1 Range: 4,342,973 to 4,344,541 |
A. fumigatus Hsp70 chaperone BiP/Kar2 | 91 | 99 | Yes | Yes | |
| Sequence ID: LVYW01000003.1 Range: 1,590,876 to 1,592,192 |
A. fumigatus Hsp70 chaperone HscA | 88 | 99 | Yes | Yes | |
| Sequence ID: LVYW01000003.1 Range: 1,425,780 to 1,427,675 |
A. fumigatus mitochondrial Hsp70 chaperone (Ssc70) | 92 | 91 | Yes | Yes | |
| Sequence ID: LVYW01000001.1 Range: 3,575,451 to 3,577,520 |
A. fumigatus Hsp70 chaperone Hsp88 | 72 | 88 | Yes | Yes | |
| Sequence ID: LVYW01000006.1 Range: 1,235,654 to 1,237,159 |
A. fumigatus Hsp70 chaperone BiP | 68 | 91 | Yes | Yes | |
| Sequence ID: LVYW01000003.1 Range: 5,249,506 to 5,251,209 |
A. fumigatus Hsp70 family chaperone Lhs1/Orp150 | 70 | 71 | Yes | Yes | |
| Heat shock protein, mitochondrial chaperone (Hsp60) | Sequence ID: LVYW01000002.1 Range: 857,724 to 859,505 |
A. fumigatus antigenic mitochondrial protein Hsp60 | 87 | 96 | Yes | Yes |
| Heat shock protein involved in thermotolerance (Hsp90) | Sequence ID: LVYW01000005.1 Range: 880,214 to 881,443 |
A. fumigatus molecular chaperone and allergen Mod-E/Hsp90/Hsp1 | 94 | 87 | Yes | Yes |
| Adhesins | ||||||
| Cell wall integrity, adherence, and biofilm formation | Sequence ID: LVYW01000001.1 Range: 1,884,061 to 1,884,846 |
A. fumigatus cell wall glucanase Scw11 | 59 | 41 | Yes | Yes |
| Sequence ID: LVYW01000007.1 Range: 2,857,516 to 2,858,574 |
A. fumigatus cell wall glucanase | 61 | 95 | Yes | Yes | |
| Cell wall morphology, pH-dependent expression (Phr1) | Sequence ID: LVYW01000004.1 Range: 4,497,069 to 4,498,358 |
A. fumigatus β-1,3-glucanosyl-transferase | 69 | 78 | Yes | Yes |
| Sequence ID: LVYW01000001.1 Range: 86,737 to 87,795 |
A. fumigatus β-1,3-glucanosyl-transferase Gel1 | 76 | 78 | Yes | Yes | |
| Sequence ID: LVYW01000003.1 Range: 3,681,474 to 3,682,763 |
A. fumigatus β-1,3-glucanosyl-transferase Gel2 | 69 | 88 | Yes | Yes | |
| Biofilm formation | ||||||
| Transcription Factor (Ndt80) | Sequence ID: LVYW01000002.1 Range: 4,774,368 to 4,775,234 |
A. fumigatus NDT80/PhoG like DNA-binding family protein | 53 | 48 | Yes | Yes |
| Secreted hydrolases | ||||||
| Secreted aspartyl protease (Sap2) | Sequence ID: LVYW01000006.1 Range: 613,730 to 615,028 |
A. fumigatus aspartic-type endopeptidase OpsB | 69 | 88 | Yes | Yes |
| Sequence ID: LVYW01000006.1 Range: 2,678,211 to 2,679,401 |
C. albicans Sap8 | 47 | 81 | Yes | Yes | |
| Sequence ID: LVYW01000001.1 Range: 4,068,222 to 4,069,364 |
A. fumigatus aspartic endopeptidase Pep2 | 81 | 90 | Yes | Yes | |
| Sequence ID: LVYW01000005.1 Range: 1,785,032 to 1,786,228 |
A. fumigatus aspartic endopeptidase Ap1 | 63 | 88 | Yes | Yes | |
| Sequence ID: LVYW01000002.1 Range: 2,154,952 to 2,156,013 |
A. fumigatus aspartic-type endopeptidase CtsD | 57 | 75 | Yes | Yes | |
| Sequence ID: LVYW01000004.1 Range: 2,345,538 to 2,346,500 |
A. fumigatus extracellular aspartic endopeptidase | 66 | 77 | Yes | Yes | |
| Phospholipase | Sequence ID: LVYW01000001.1 Range: 4,901,960 to 4,903,879 |
A. fumigatus lysophospholipase Plb1 | 67 | 96 | Yes | Yes |
| Sequence ID: LVYW01000001.1 Range: 5,943,020 to 5,945,185 |
A. fumigatus phospholipase A2 PlaA | 63 | 87 | Yes | Yes | |
| Lipase | Sequence ID: LVYW01000002.1 Range: 2,894,403 to 2,895,689 |
A. fumigatus secretory lipase | 61 | 89 | Yes | Yes |
| Urease | Sequence ID: LVYW01000001.1 Range: 6,005,160 to 6,007,553 |
A. fumigatus Urease Ure | 84 | 87 | Yes | Yes |
| Melanin production | ||||||
| Polyketide synthase | Sequence ID: LVYW01000001.1 Range: 5,766,340 to 5,772,381 |
A. fumigatus conidial pigment polyketide synthase PksP/Alb1 | 60 | 94 | Yes | Yes |
| Phenoloxidase | Sequence ID: LVYW01000004.1 Range: 3,463,454 to 3,465,208 |
A. fumigatus ferrooxidoreduc-tase Fet3 | 67 | 96 | Yes | Yes |
| Sequence ID: LVYW01000001.1 Range: 5,252,734 to 5,254,242 |
A. fumigatus extracellular dihydrogeodin oxidase/laccase | 48 | 88 | Yes | Yes | |
| Sequence ID: LVYW01000003.1 Range: 3,378,591 to 3,380,357 |
A. fumigatus laccase TilA | 60 | 94 | Yes | Yes | |
| Nutrient uptake | ||||||
| GTPase | Sequence ID: LVYW01000001.1 Range: 2,496,580 to 2,497,089 |
A. fumigatus Rheb small monomeric GTPase RhbA | 89 | 100 | Yes | Yes |
| Sequence ID: LVYW01000006.1 Range: 992,857 to 993,159 |
A. fumigatus RAS small monomeric GTPase Rsr1 | 86 | 72 | Yes | Yes | |
|
Ornithine monooxygenase |
Sequence ID: LVYW01000002.1 Range: 2,281,754 to 2,283,208 |
A. fumigatus L-ornithine N5-oxygenase SidA | 59 | 90 | Yes | Yes |
| Zinc homeostasis | Sequence ID: LVYW01000005.1 Range: 1,316,107 to 1,317,288 |
A. fumigatus high-affinity zinc ion transporter | 67 | 99 | Yes | Yes |
| Sequence ID: LVYW01000005.1 Range: 1,316,173 to 1,317,216 |
A. fumigatus plasma membrane low-affinity zinc ion transporter | 55 | 86 | Yes | Yes | |
| Sequence ID: LVYW01000002.1 Range 1: 1,172,630 to 1,173,124 |
A. fumigatus ZIP family zinc transporter | 83 | 71 | Yes | Yes | |
| Acetyl-CoA synthetase | Sequence ID: LVYW01000002.1 Range: 1,643,562 to 1,644,794 |
A. fumigatus acetyl-coenzyme A synthetase FacA | 88 | 92 | Yes | Yes |
| Serine/threonine kinase | Sequence ID: LVYW01000003.1 Range: 3,006,373 to 3,007,410 |
A. fumigatus carbon catabolite derepressing protein kinase Snf1 | 83 | 69 | Yes | Yes |
| Phosphoenolpyruvate carboxykinase | Sequence ID: LVYW01000003.1 Range 1: 1,604,482 to 1,605,645 |
A. fumigatus pyruvate kinase | 84 | 99 | Yes | Yes |
| Hexose kinase | Sequence ID: LVYW01000001.1 Range 1: 1,447,659 to 1,448,525 |
A. fumigatus hexokinase Kxk | 84 | 95 | Yes | Yes |
| Sequence ID: LVYW01000002.1 Range 1: 4,445,090 to 4,447,084 |
A. fumigatus hexokinase | 64 | 68 | Yes | Yes | |
| Sequence ID: LVYW01000005.1 Range 1: 443,537 to 444,583 |
A. fumigatus glucokinase | 68 | 82 | Yes | Yes | |
| Isocitrate lyase | Sequence ID: LVYW01000006.1 Range: 3,093,278 to 3,094,873 |
A. fumigatus isocitrate lyase AcuD | 83 | 98 | Yes | Yes |
| Sequence ID: LVYW01000005.1 Range: 2,780,931 to 2,782,532 |
C. albicans Isocitrate lyase 1 | 51 | 97 | Yes | Yes | |
| Malate synthase | Sequence ID: LVYW01000002.1 Range 1: 3,545,499 to 3,546,767 |
A. fumigatus malate synthase AcuE | 91 | 99 | Yes | Yes |
| Response to stress | ||||||
| Superoxide dismutase | Sequence ID: LVYW01000002.1 Range: 3,012,655 to 3,013,167 |
A. fumigatus Cu/Zn superoxide dismutase SOD1 | 78 | 97 | Yes | Yes |
| Sequence ID: LVYW01000003.1 Range: 2,047,916 to 2,048,404 |
A. fumigatus cytosolic Cu/Zn superoxide dismutase C. albicans SOD5 | 57 | 71 | Yes | Yes | |
| Catalase | Sequence ID: LVYW01000002.1 Range: 4,168,516 to 4,169,937 |
C. albicans catalase A | 74 | 97 | Yes | Yes |
| Sequence ID: LVYW01000004.1 Range: 3,095,593 to 3,097,812 |
A. fumigatus spore-specific catalase CatA | 71 | 97 | Yes | Yes | |
| Flavohemoglobin-related protein | Sequence ID: LVYW01000005.1 Range 1: 3,049,448 to 3,050,809 |
A. fumigatus flavohemoprotein | 56 | 98 | Yes | Yes |
| Serine/threonine phosphatase | Sequence ID: LVYW01000003.1 Range: 4,774,748 to 4,776,373 |
A. fumigatus calcineurin catalytic subunit CnaA | 85 | 96 | Yes | Yes |
| Thioredoxin | Sequence ID: LVYW01000001.1 Range: 5,596,040 to 5,597,059 |
A. fumigatus thioredoxin reductase Trr1/Trr2 | 77 | 82 | Yes | Yes |
| Sequence ID: LVYW01000001.1 Range: 1,734,081 to 1,734,710 |
A. fumigatus thioredoxin | 61 | 96 | Yes | Yes | |
| Toxins and secondary metabolites | ||||||
| Non-ribosomal peptide | Sequence ID: LVYW01000006.1 Range: 3,263,839 to 3,277,668 |
A. fumigatus nonribosomal siderophore peptide synthase SidC | 45 | 93 | Yes | Yes |
| C6 finger domain protein | Sequence ID: LVYW01000004.1 Range: 4,538,250 to 4,539,548 |
A. fumigatus C6 finger domain protein | 50 | 80 | Yes | Yes |
Virulence is defined as the pathogenicity degree of an organism, and it is determined by the ability to adhere, disseminate, and damage cells, tissues, organs, systems, or the whole organism.43 Some of these factors, already described in Sporothrix, include dimorphism, thermotolerance, the presence of melanin, secreted hydrolytic enzymes, and extracellular vesicles.44 S. brasiliensis and S. globosa are the members of the Sporothrix pathogenic clade with the highest and lowest virulence, respectively.45 In agreement with this observation, it was reported that different S. globosa strains were not capable of killing mice, in a murine model of experimental sporotrichosis, regardless of the inoculum size applied to animals; and the fungal burdens in spleen, lungs, liver, testicles, kidneys, and brain were considerably low in comparison with S. brasiliensis-infected animals.45 Additionally, some S. globosa strains have been reported as non-virulent.46,47 In one study, where 18 animals received subcutaneous and retroperitoneal S. globosa inoculums, none showed any symptoms and the inoculum site did not have any fungal growth after a 30-day observation period.46 Thus, it has been suggested that S. globosa causes mainly benign, fixed, or lymphocutaneous infections. However, it can spread to other organs such as the liver, kidneys, and brain, but to a lesser extent when compared with S. brasiliensis- and S. schenckii-caused infections.45 This low virulent phenotype could be mainly due to differences in the metabolism and cell wall structure, as already mentioned. The overexpression of enzymes involved in amino acids and lipids metabolism, and the upregulation of glycolytic enzymes and trehalose synthase in S. brasiliensis,41 suggest that this species has better nutrient exploitation during parasitism than S. globosa, better resistance to osmotic stress, and better cell wall remodeling, important factors for the infection that can contribute to fungal virulence. Moreover, the S. globosa cell wall, with its high levels of β-1,3-glucan exposed at the cell surface, is also a disadvantage when interacting with the host immunity.32,48 Furthermore, S. brasiliensis and S. schenckii tolerate growth at 37°C but S. globosa hardly grows above 35°C, with larger duplication times than the other two fungal species,16 and thus representing a handicap when adapting to grow within the host milieu.
Heat shock proteins are important factors for thermotolerance and mycelium-to-yeast transition, and six of them have been identified in S. globosa.41 Among them, an Hsp90 homolog is found, which has a key role in the resistance to heat stress in A. fumigatus.49 As a result, when this protein activity is inhibited in both S. schenckii and S. globosa, the transition from hypha to the yeast-like cells morphology is blocked.50 In S. schenckii, the Hsp90 interaction with the SsCmk1 enzyme, a Ca2+/calmodulin-dependent protein kinase, is necessary for thermotolerance, and molecular silencing of its encoding gene led to a phenotype similar to that observed when Hsp90 was inhibited with geldanamycin, ie, cells arrested in the filament morphology.50 Additionally, yeast two-hybrid assays suggested that SsCmk1 has a role in the fungus thermotolerance through its effects on Hsp90.50 The bioinformatics analysis of the S. globosa genome showed it contains one putative functional ortholog for both S. schenckii HSP90 and SsCMK1 (Table 2). It is worthy of mentioning that the bioinformatics predictions provided in Table 2 require experimental validation.
Table 2.
Prediction of Putative Virulence Factors in S. globosa, Based on S. schenckii and S. brasiliensis Known Virulence Factors
| Protein | Function | S. schenckii | S. brasiliensis | ||||
|---|---|---|---|---|---|---|---|
| E. value | Similarity (%) | Coverage (%) | E. value | Similarity (%) | Coverage (%) | ||
| Hsp90 | Thermotolerance | 0.0 | 99 | 100 | 0.0 | 99 | 100 |
| SsCMK1 | Thermotolerance | 0.0 | 90 | 99 | 0.0 | 91 | 100 |
| SsDRK1 | Morphological switching | 0.0 | 99 | 100 | 0.0 | 99 | 100 |
| PKC | Signal transduction | 0.0 | 85 | 98 | 0.0 | 93 | 92 |
| Gp70 | Adhesion | 0.0 | 90 | 100 | 0.0 | 91 | 100 |
| Enolase | Adhesion | 2e-176 | 97 | 100 | 2e-176 | 97 | 100 |
| Cell wall glucanase | Lysis of immune cells | 8e-170 | 86 | 98 | 2e-167 | 85 | 98 |
| SOD | Oxidative stress resistance | 0.0 | 89 | 100 | 8e-180 | 89 | 100 |
| Proteinase I | Hydrolysis of tissue | 0.0 | 92 | 99 | 0.0 | 97 | 96 |
| Proteinase II | Hydrolysis of tissue | 0.0 | 98 | 93 | 0.0 | 98 | 100 |
| Hsp60 | Adhesin | 0.0 | 95 | 96 | 0.0 | 95 | 91 |
| Pap1 | Adhesin | 3e-25 | 94 | 36 | 1e-25 | 96 | 31 |
Another protein kinase that participates in the S. schenckii morphological switch is the histidine kinase SsDrk1.51 This protein is important for the virulence of other pathogenic fungi, such as Blastomyces dermatitidis and Histoplasma capsulatum, as well as in S. schenckii, but unlike what has been seen in the typical histidine kinases, SsDrk1 is a soluble protein without a transmembrane domain.52 The SsDRK1 gene manipulation resulted in mutants with limited growth, which suggests a delay in asexual development; abnormalities in the plasma membrane and cell wall, such as short and abundant invaginations in the yeast morphology, and lack of the electron-dense zone in the cell wall surface; and abnormal sensitivity to cell wall perturbing agents, factors that suggest a defective cell wall components deposition, and thus, defective cell wall integrity.51 Moreover, the fungus’ ability to perform dimorphism and melanization was altered, as most of the cells displayed a conidium-like morphology.51 Finally, the SsDrk1-deficient strains had attenuated virulence in a murine model of cutaneous infection,51 which might be explained by (i) the defective cell wall, which makes the fungus more vulnerable to environmental stress, osmotic changes, and the immune recognition and response by the host; (ii) pigmentation decrease, since melanization is relevant in the cutaneous sporotrichosis pathogenesis, helping in granuloma formation, fungal dissemination, protecting the yeast-like cells against phagocytosis, and decreasing the efficacy of some treatments53–55; and (iii) decrease of dimorphism, a process that contributes to a rapid growth inside the host cells and slower fungal clearance from the tissues, by protecting the fungus from the immune response.51 A putative SsDRK1 ortholog is predicted to be part of the S. globose genome (Table 2).
The S. schenckii protein kinase C (PKC), an enzyme important in signal transduction, was also found to be related to the fungus dimorphism.56 The pkcSs-2 gene, which codes for the PKC, was found to be expressed at all intervals tested during the yeast to mycelium transition. A curious characteristic of this PKC is its ability to induce the morphological transition even at low calcium concentrations, which suggests the existence of two different mechanisms for dimorphism: a calcium-dependent pathway and a calcium-independent pathway.56,57 The S. globosa genome has a sequence very similar (85%) to that of S. schenckii pkcSs-2, being likely that similar dimorphism control occurs in this species (Table 2).
There is a predominant antigenic glycoprotein named Gp70 described by several authors, which is found in the cell wall, extracellular space, and extracellular vesicles of all clinical Sporothrix species, including S. globosa (Table 2).47,58–60 This glycoprotein was predicted to be an enzyme with 3-carboxymuconate cyclase activity and was found to be the most immunogenic antigen in the S. brasiliensis, S. schenckii, and S. globosa cell wall.60 Additionally, the characterization by 2D-DIGE exposed that Gp70 presents several isoforms (that can range from 55 to 70 kDa), probably due to post-translational modifications, which are present in the clinical clade but absent in the non-pathogenic species.60 Amino acid modifications and glycosylation could be the possible post-translational modifications involved in isoforms production. Besides, Gp70 has low homology to proteins found in other pathogen and non-pathogen fungal species, and since is a shared molecule in the pathogenic clade, it can be used for sporotrichosis diagnosis.58,60 Gp70 is also an important vaccine candidate, due to the strong humoral response produced during the interaction with the host, which is backed up by several investigations.47,58,61–65 Due to its high immunogenicity, it was found that its expression is related to the virulence profile of the Sporothrix species and isolates since highly virulent S. brasiliensis isolates have a lower protein abundance when compared to S. schenckii low virulence strains.66
Some other cell wall and extracellular enzymes have been reported to be important for Sporothrix virulence. A cell wall glucanase, transported by extracellular vesicles, contributes to the fungal virulence by inducing host immunity evasion, due to cell wall remodeling.67 An enolase, a moonlighting protein in the cell wall with high antigenicity, has a possible role in the adhesion to the extracellular matrix, contributing to the fungal virulence;68 the superoxide dismutase, another cell wall protein, contributes to the growth and survival of the yeast under oxidative stress conditions, such as inside of macrophages;69 and, certain proteases, such as collagenase, gelatinase, and proteinase I and II, which hydrolyze human stratum corneum, type I collagen, and elastin,70,71 play an essential role in the host–fungus interaction, helping in the fungal invasion of cutaneous tissues and avoiding the immune response.72–74 However, these mentioned proteins have not been completely characterized in other Sporothrix species, but the S. globosa genome has sequences that encode for proteins with these enzyme activities.
Finally, a well-characterized polysaccharide found in the S. schenckii and S. brasiliensis yeast cell wall surface, the peptidorhamnomannan (PRM), influences macrophage function by inhibiting phagocytosis.75 This glycoconjugate is composed of a protein core (16%), modified with mannose (50%), rhamnose (33%), and galactose (1%).76 The identity of the proteins that belong to this complex was recently determined, and two of them were demonstrated to work as virulence factors, the chaperonin GroEL (Hsp60) and the Pap1 (peptidorhamnomannan-associated protein 1).77 It was demonstrated that both proteins are moonlighting proteins with adhesive properties on the S. schenckii cell wall, which allow fungal binding to the host extracellular matrix components.77 The Hsp60 is a highly conserved protein with intracellular chaperone activity, but on the S. schenckii surface binds to laminin, elastin, fibrinogen, and fibronectin.77 In addition, this protein participates in the fungal virulence, since the opsonization of the yeast-like cells with anti-recombinant Hsp60 antibodies and their subsequent use to challenge Galleria mellonella larva caused a decrease in the fungal ability to kill the host, probably due to increased fungal clearance by the larvae immune response.77 When the recombinant protein was inoculated in the larvae before the infection with S. schenckii, it stimulated immunological priming and increased the host survival.77 In the same line, Pap1, an uncharacterized protein, binds to laminin, elastin, fibrinogen, fibronectin, and type I and II collagen, and also participates in S. schenckii virulence. In similar experiments like those already described for Hsp60, Pap1 was also involved in fungal virulence.77 A BLAST search within the S. globosa genome found that both proteins are present in this pathogen, although Pap1 was found with a very low sequence coverage (Table 2), at the difference of what it was found in S. brasiliensis.77 This might suggest that this virulence factor is exclusive for the high virulence species of the Sporothrix clinical clade.
Recently, by comparing the A. fumigatus and C. albicans genomes with the S. schenckii genome sequence, putative factors were identified in this sporotrichosis etiological agent.78 The analysis suggested multiple proteins with putative functions that could serve as virulence factors in S. schenckii. Following the same strategy, we have searched for these putative virulence factors within the S. globosa genome (Table 1). The results suggest multiple proteins that could be involved in morphological switching, cell wall synthesis, thermotolerance, adhesion, biofilm formation, hydrolysis, melanin production, nutrition, response to stress conditions, and toxins and secondary metabolites production.
Immune Response Against Sporothrix globosa
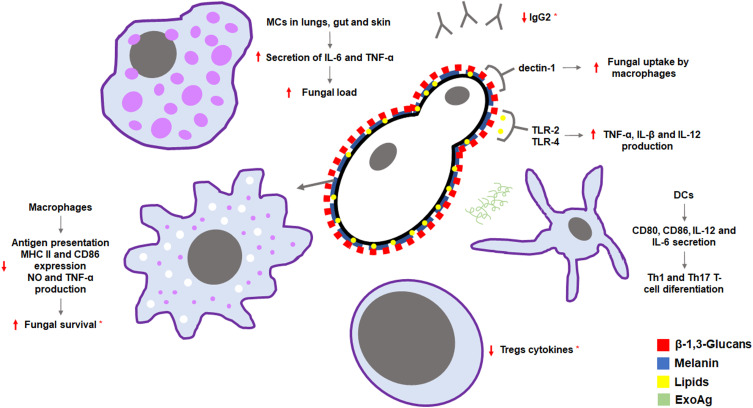
Even though the scientific community has made a significant effort trying to explain the host immune response against sporotrichosis, many details remain unclear regarding the S. globosa immune sensing, since most studies have been made in S. schenckii or S. brasiliensis (Figure 3).
Figure 3.
Immune response against Sporothrix globosa. Pathogen components trigger an innate immune response via dectin-1, TLR-2 and TLR-4 receptors, and macrophages and mast cells (MCs); an adaptative immune response via dendritic cells (DCs) and Tregs lymphocytes; and a humoral immune response by IgG antibodies. These responses have been observed in either Sporothrix schenckii or Sporothrix brasiliensis and are suggested for S. globosa, except those marked with*, which have already been demonstrated in S. globosa.
Innate Immune Response
As in viral and bacterial infections, the host reaction towards a fungal invader begins with the pathogen recognition by the innate immune system, a process in which pathogen-associated molecular patterns (PAMPs) and pattern recognition receptors (PRRs) are involved. PAMPs respond to evolutionary conserved molecular signatures of microorganisms, usually specific to the pathogen.79,80 In Sporothrix spp., the main PAMPs source is the cell wall, where PRM, melanin, glycoconjugates, chitin, and β-1,3- and β-1,6-glucans are found.1,26,37 On the other hand, PRRs, mainly expressed by antigen-presenting cells, such as macrophages and dendritic cells, are divided into four groups: Toll-like receptors (TLRs), nucleotide oligomerization domain (NOD)-like receptors, C-type lectin receptors (CLRs), and retinoic acid-inducible gene I (RIG-I)-like receptors (RLRs).79
Even though S. schenckii and S. brasiliensis cell wall components are very similar, their abundance varies and suggests a difference in the immune response against them, since chitin and β-glucans exposure on the fungal surface favors their binding to PRRs.37,81 It has been reported that dectin-1, a C-type lectin receptor, binds to C. albicans and A. fumigatus β-1,3-glucans, and this interaction triggers fungal uptake by murine and human macrophages.82 S. globosa has higher β-1,3-glucan levels at the cell surface than S. schenckii and S. brasiliensis, an observation that is regardless of the culture medium, while in S. brasiliensis and S. schenckii this depends on nutrients’ availability.32 This β-1,3-glucan exposure might explain the S. globosa’s lower virulence, due to a better recognition by the host.26,32
It has been demonstrated that TLR-2 and TLR-4 recognize the fungal lipid extracts and are relevant in sporotrichosis control, not only in S. schenckii infections but also in those caused by S. brasiliensis in mice; while in the human PBMCs-Sporothrix interaction, TLR-4 is dispensable, suggesting a host-dependent role for this PRR.26 TLR-2 has been linked to TNF-α and IL-β induction, whilst TLR-4 to TNF-α, IL-1β, and IL-12 production.83 In S. globosa, it is possible to suggest that similar PRRs are involved in its immune sensing.
Melanin plays structural and protective roles in dematiaceous fungi and has been related to the Sporothrix spp. dissemination to internal organs in different cases.84 It has been already demonstrated that S. schenckii melanin is involved in the antigen presentation inhibition by macrophages;54,85 and recent studies have confirmed that S. globosa melanin increases fungal survival during the infection.86 Twenty percent of mice infected with melanin-deficient S. globosa conidia developed spleen and kidney dissemination, while 80% of the animals infected with melanin producer conidia developed a lung infection and 100% developed liver, spleen, kidney, and testicle infections.86 Furthermore, results also showed a negative impact on MHC II and CD86 expression in murine macrophages, as well as in nitric oxide (NO) and TNF-α production, which are important in digestive macrophage functions.86 It is also known that conidia have a higher melanin content than yeast-like cells, and it has been suggested that accumulation of this component before yeast conversion delays the adaptative immunity induction.86
On the other hand, the role of mast cells (MCs) in the immune response has also been of special interest in the last years, as they are located in tissues at the interface with the environment (lungs, gut, skin). It has been reported that MCs may have a positive or negative immunoregulatory function within fungal infections; therefore, a recent study using MC-competent wild-type mice and an MC-deficient strain showed that infected mice with S. schenckii in the first group developed larger sporotrichosis lesions than mice of the second group.87 These observations are related to MCs proinflammatory cytokines IL-6 and TNF-α pronounced production due to S. schenckii stimulus.87 An earlier study also showed a correlation between MCs depletion and the decrease of fungal load in organs88 In addition, both groups showed decreased numbers of basophils, thus a contribution from these cells in the infection development may be suggested.87 According to this, there might be a dissimilar interaction between mast cells and S. globosa, as it is less virulent, and the host is more capable of controlling the infection. However, further investigation is needed.
Adaptative Immune Response
When activated, dendritic cells (DCs) PRRs recognize PAMPs and a signaling pathway gets triggered, causing the pathogen phagocytosis for subsequently MHC antigen presentation to naïve T-cells in secondary lymphoid tissues; thus, dendritic cells have been extensively studied in fungal infections and are considered to be a bridge between the innate and adaptative immune responses.89 Thus far, three signals are needed for T-cell activation: 1) DCs’ MHC presenting pathogen-derived peptides, 2) co-stimulatory molecules CD80 and CD86 expressed by DCs, and 3) DCs release of interleukins that promote T-cell differentiation.79
It has been demonstrated that DCs stimulation with S. schenckii yeast-like cells or a peptide-polysaccharide (Exoantigen or ExoAg) extracted from the supernatant of the fungal culture triggers the co-stimulatory molecules CD80 and CD86, and pro-inflammatory cytokines secretion, such as IL-12 and IL-6, that induce Th1 and Th17 T-cell differentiation, respectively.90,91 Th1 response has been considered critical to host defense against S. schenckii and S. brasiliensis infection since produces an increase in cytokines levels such as IFN-γ, which activates immune effector cells,83 while Th17 response is found crucial for optimal fungal clearance.92 Additionally, an enhanced Th1 response is reported when the fungal stimulus comes from a cutaneous infection and not from the visceral disease, being the latter responsible to induce a Th2 response.93 In contrast, recent studies have demonstrated a predominant Th2 response against S. globosa, while in systemic S. schenckii infected mice it was reported to begin in the later phase of infection.92 Moreover, studies in other pathogenic fungi, such as Cryptococcus neoformans, have shown that Th2 cells may inhibit Th1 and Th17 responses, prolonging fungal survival and inducing alternatively activated macrophages, which results in a worsened fungal infection.92 On the other hand, regulatory T-cells ratio is reported to be increased in S. schenckii infected mice at the early phase of infection, while in S. brasiliensis-infected mice, a long-lasting elevated regulatory T cells (Tregs) response is reported.92 S. globosa-infected patients have shown decreased Tregs cytokines, thus suggesting a dysfunction in the response of these immune cells.92 Furthermore, previous reports indicate that humoral immunity also participates in the antifungal response against S. schenckii and S. brasiliensis infection. In contrast, in the S. globosa infection, a positive correlation between Th2/Tregs and IgD-CD27-double-negative B cells (DN B) was found, whose role is still unclear, but it is believed that DN B cells might be exhausted memory B cells or a memory B cell precursor.92
Humoral Immunity
Although very little is known about humoral immunity when it comes to S. globosa infections in humans, its importance has been proven for the host defense against some other fungi, including C. neoformans, C. albicans, and Paracoccidioides brasiliensis.94 The antibodies role in fungal infections may involve mechanisms of protection such as fungal cells agglutination, interference with fungal attachment, phagocytosis enhancement by host effector cells, immunoregulatory molecules neutralization, and complement activation.63
Serum from patients with sporotrichosis infection have been positive for the immunoglobulin isotypes IgA, IgG, and IgM analyzed by ELISA against mycelial-phase exoantigens. In addition, cross-reactions with serum from healthy patients and patients with other infectious diseases such as histoplasmosis, tuberculosis, leishmaniasis, aspergillosis, paracoccidioidomycosis, and even cryptococcosis have been observed.95 IgM antibodies have had a higher number of cross-reactions, which may be due to their role in complement activation by the classical pathway in several mycotic diseases.95,96 On the other hand, IgA might be an important mechanism of defense as this immunoglobulin is predominantly present in mucosa.95 When the immune profile in circulation against S. globosa was investigated, a decreased level of IgG2 in patients of short and long-duration infection was observed, as well as in lymphocutaneous and fixed cutaneous forms.92 IgG2 antibodies are induced in the absence of T-cell help and in the presence of polysaccharide antigens,97 and their decreased levels found in S. globosa infection is thought to be associated with a decrease in B cells subsets, which are responsible for IgM and IgG secretion.92
Vaccine Against Sporothrix globosa
Antifungal treatments can lead to the rising of drug resistance, even when an intermittent dosage is given. Moreover, the use of these treatments may cause liver injury in risk patients such as children, pregnant women, and patients with liver disorders.33 Furthermore, in the case of S. globosa, it has been determined that this specie is less susceptible to most of the antifungals tested, such as amphotericin B, ketoconazole, posaconazole, and itraconazole;16 therefore, the generation of an effective prophylactic or therapeutical vaccine has gained great interest in the sporotrichosis treatment.
Although mycelial components have been tested for vaccine design, Gp70 has been the most studied antigen for a long time, since Rodrigues et al, argued that the 70 kDa glycoprotein is the same molecule reported as exoantigen, cell-free antigen, and cell wall virulence factor for Sporothrix species, now identified as a 3-carboxymuconate cyclase.58,60 The importance of this antigen comes not only from its high immunoreactivity but also from its presence in species of the Sporothrix pathogenic clade, which may lead to a broad-spectrum vaccine against sporotrichosis.68 In 2017, Chen et al developed a successful Th1 and Th17 inducing vaccine against S. globosa, based on a Gp70 displaying recombinant phage (phage KR), whose safety has been approved by the Federal Drug Administration, USA.64 Furthermore, IgG antibodies against Gp70 produced in mice immunized with the recombinant phage were proved to protect the host during a lethal challenge of S. globosa, with an 80% of survival and a decreased fungal burden, demonstrating the antibodies efficiency as a treatment.98 These previous results show that the Gp70 displaying phage vaccine may function as an improvement in both protective cell-mediated and humoral immune responses, representing a new and potentially safe alternative for the treatment of the infection.
Monoclonal antibodies (mAb) such as IgG1 against S. schenckii Gp70, also known as mAbP6E7, have also shown an important role in decreasing fungal organ burden in infected mice. However, due to its origin, mAbP6E7 cannot be tested for human treatment. Humanized P6E7 (hP6E7) developed by genetic engineering technics also showed a similar antigen-binding capacity that promotes phagocytosis, which could be use for sporotrichosis treatment.63
Sporotrichosis Caused by Sporothrix globosa
Sporotrichosis is usually found as a subcutaneous mycosis, but other clinical forms have also been reported, such as mucosal, extracutaneous, or systemic and disseminated disease. The development of one clinical form or the other depends on diverse factors, such as the inoculum size, the infection route, strain virulence and thermal tolerance, and the host immunological status.45 When different S. schenckii isolates from different clinical forms were inoculated into healthy mice, to compare their virulence, it was observed that the strains isolated from disseminated sporotrichosis caused a severe disease, killing all of the subjects within 10 days, while the strains isolated from lymphocutaneous and fixed cutaneous forms, had mild and low virulence, respectively, both failing to cause death.99 Thus, proving that the same species can have different virulence profiles.
In terms of mortality, tissue damage, and fungal burden, S. brasiliensis has been reported as the most virulent species. When different inoculum concentrations and two different strains of S. brasiliensis, S. schenckii, S. globosa, Sporothrix mexicana, and Sporothrix albicans were intravenously inoculated in an immunocompetent murine model, high mortality was only observed for S. brasiliensis and S. schenckii, being S. brasiliensis the only species capable of killing mice with the lowest inoculum size.45 On the contrary, S. globosa presented low virulence in this model.45 These data have been confirmed in various studies using other models, such as Tenebrio molitor, where larvae were inoculated with different fungal doses to evaluate animal mortality, cytotoxicity and immunological parameters. These results, along with what has been observed in human clinical cases, have shown that S. globosa is associated with lesser host damage upon inoculation, with different clinical manifestations mainly limited to the skin (Table 3).23,62,100–103 Despite not being as virulent as S. brasiliensis and S. schenckii, infections caused by S. globosa have a broader distribution, as they have been found in Europe, America, and Asia, increasing its clinical significance.1
Table 3.
Clinical Manifestations and Treatments of Sporotrichosis Caused by S. globosa
| Patient | Clinical Manifestations | Risk Factor | Treatment | Outcome | Reference |
|---|---|---|---|---|---|
| 77-year-old woman (Brazil) | Verrucous lesion on the right dorsal hand with 12 ascending subcutaneous nodules on the arm, some of them fistulized | The patient handled plants, vegetable garden and soil, but did not remember local trauma | Itraconazole 100 mg/day for 5 months | Regression of all the lesions | de Oliveira et al 201023 |
| 70-year-old man (China) | Solitary, well-defined, painless, red plaque on the right forearm, with a central ulcer and yellow crusting | The patient was a greenhouse farmer with iatrogenic topical immunosuppression, and described a prior trauma with a wooden thorn | Itraconazole 200 mg/day for 4 months | Regression of the lesion | Gu et al 2020101 |
| 51-year-old man (China) | Suppurative wound and progressive subcutaneous nodules at the right arm, that became a verruca-like nodule | The patient was bitten by a stray cat | Itraconazole 200 mg/twice per day and terbinafine 250 mg/day for 1 month | Regression of the lesion | Liu et al 2020102 |
| 50-year-old woman (China) | Small mass on the right upper eyelid with rough keratinization, that often discharged purulent secretion | - | Resistant to amphotericin B, voriconazole, fluconazole, terbinafine and caspofungin Treated with itraconazole 0.2 g/twice per day for 3 months |
Regression of the lesion | Liu et al 2021103 |
| 66-year-old man (Brazil) | Scaly erythematous lesion that mimicked a sarcoid lesion with a well-demarcated ulcer in the middle of the left arm, without suppuration nor subcutaneous nodules or fistulization. | The patient was a farmer and was involved in rural activities, and described a prior trauma | Resistant to itraconazole Treated with a saturated solution of KI 1 g/day increased weekly by 1 g up to a maximum of 4 g/day for 6 months |
Regression of the lesion | Gompertz et al 2016100 |
| Mice with cutaneous infection | Soft subcutaneous lumps | - | Combination of itraconazole 60 mg/kg/day for 3 weeks, PDT at an irradiation energy density of 40 J/cm2 once every week for 3 weeks and methylene blue 2 mg/mL in the feet until they became dark blue | Reduction of the lesion and regression of the lesion in some mice at day 20 | Li et al 2019113 |
| Mice with disseminated infection | - | - | One day after infection, mice were treated once every 3 days with purified antibody against phage-KR | Increased in the survival rate (80%) | Chen et al 201998 |
The first report of S. globosa isolation in Brazil suggests that transmission of the fungus usually occurs by traumatic inoculation while working with soil.23 Nevertheless, the source of infection differs between species. The mycosis caused by S. schenckii presents a higher prevalence among patients who commonly interact with animals, particularly cats, and it is not gender-related,23 while a phylogeographic study showed that cats have never been associated as sources of sporotrichosis in S. globosa endemic areas.15 However, a cat-associated sporotrichosis case caused by S. globosa was found in China. A healthy 51-year-old man was bitten by a cat in his right hand, and developed an unhealing wound that progressed into multiple ascending subcutaneous nodules.102 Sporotrichosis diagnosis was confirmed by culture, and the species identification was performed by amplification and sequencing of the chitin synthase 1 gene, chs; the DNA topoisomerase II gene top2, the DNA polymerase α subunit B gene, and the DNA-directed RNA polymerase I and II subunits genes, suggesting that S. globosa can also cause cat bite-–associated sporotrichosis.102
Moreover, a dominance of female patients with confirmed S. globosa infection has been reported, although this gender difference might be related to higher exposure.11 In addition, systemic sporotrichosis is often associated with immunocompromised patients, although it is not the most common fungal form for this species,3 due to S. globosa inadequate grow at 37°C.1
S. globosa Identification
The importance of an efficient identification of the sporotrichosis etiological agent is due to the necessity of accurate and well-timed treatment. Clinical samples culture is the typical method for sporotrichosis diagnosis, but it is not enough to identify the causative agent at the species level.104 S. globosa is characterized by the production of both hyaline and sessile brown to dark brown conidia, as it has been reported on colonies grown on cornmeal agar at 37°C.11 The fungus on potato dextrose agar at 25°C grows as septate hyphae with terminal clavate obovoid structures.11 S. globosa growth on potato dextrose agar at 21 days shows a better development when the temperature rises from 20°C to 30°C but does not display an efficient growth when the temperature goes from 30°C to 37°C, which is related to the inability of the fungus to cause disseminated or systemic infections.21 Despite this, studies have reported S. globosa isolation and growth at 37°C,11,23 and it is hypothesized that this inconsistency may be related to the fungal genomic plasticity.
Molecular techniques are required to discern among clade members. Sequencing the calmodulin (CAL), beta-tubulin (BT) and translational elongation factor 1-alpha (TEF-1α) genes lead to S. globosa identification,20 and nowadays numerous methods for faster identification have been developed. Zhang et al established a novel real-time PCR method using the ITS (internal transcribed spacer) sequence for S. globosa identification, and its detection limit is the same as that of the species-specific PCR,105 in which primers are designed using representative orthologous genes. In addition, de Oliveira and collaborators evaluated T3B PCR fingerprinting to differentiate clinical Sporothrix strains at the species level. They obtained profiles that showed DNA fragments with different banding patterns, allowing a distinction between species, proposing a simpler, faster, and cheaper technique.106 Also, Rodrigues et al determined that rolling circle amplification and species-specific primers (CAL-Fw and CAL-Rv) may perform well for detecting Sporothrix DNA directly in complex environmental samples, expanding research on the distribution in nature, especially in endemic regions.107
For the diagnosis of sporotrichosis caused by S. globosa, a combination of microbiologic and molecular methods has been used, including pus or tissue culture; direct microscopic examination of tissue fragments with KOH; histopathological and microbiological examination of biopsy samples; hematoxylin and eosin, and periodic acid–Schiff (PAS) and Grocott stainings; partial sequencing of the nuclear CAL gene, the chs gene, the top2 gene, the DNA polymerase α subunit B, and the DNA-directed RNA polymerase I and II subunits.23,100,101
Therapy
Sporotrichosis treatment hinges on the clinical form, infection persistence, the patient’s health status, and the etiological agent.108 In addition, it has been reported that the development of the infection also depends on the strain virulence, as it was demonstrated using isolates from lymphocutaneous, fixed, and disseminated sporotrichosis, where mice inoculated with strains from the disseminated infection had an early onset of the mycosis, more severe lesions and died within the first 10 days of the infection.99,109 All of these factors should be taken into consideration to choose an accurate treatment.
Here are enlisted some antifungal drugs frequently used for treatment, according to the infection clinical form. For lymphocutaneous and fixed cases, potassium iodide (KI) is the treatment of choice in many developing countries, due to its high efficacy and low cost. However, it is not recommended for disseminated, extra-cutaneous cases, for immunocompromised patients, or during pregnancy.110
The Clinical Practice Guidelines for the Management of Sporotrichosis consider itraconazole as the drug of choice for sporotrichosis therapy, its use is recommended in lymphocutaneous, fixed, and disseminated infections.111 It presents fewer side effects than KI, a better cost–benefit relationship, and an easier administration.110 Yet, itraconazole presents multiple-drug interactions and is forbidden during pregnancy.112
Fluconazole can be used in lymphocutaneous cases, it is considered as the second line of therapy, and although it presents a modest efficacy, it is recommended when itraconazole cannot be tolerated. Similarly, terbinafine is highly recommended when itraconazole cannot be used, it presents low efficacy and can be used in patients with comorbidities due to its low drug interaction rate, which is lower than fluconazole and itraconazole.110
There are scarce reports for the treatment of sporotrichosis caused by S. globosa, but some cases have reported successful regression of the lesions with different treatment schemes in human patients, including itraconazole23,101,103 and KI100; and in murine models, such as treatment with photodynamic therapy and methylene blue,113 and phage-driven immunotherapy (Table 3).98
Nevertheless, reports that evaluate the correlation of treatment and the clinical form, are usually focused on infections caused by S. schenckii. Ottonelli-Stopiglia et al studied antifungal susceptibilities of the Sporothrix clinical clade and reported that there were no significant differences among species,114 which is not in agreement with other studies,44,45 that reported several differences in the susceptibility between species. Further work in this area is required to address this subject. However, here we described the antifungal susceptibility for S. globosa, regardless of the clinical form from where the isolates were obtained.
There is disagreement about whether the drug sensitivity tests for S. globosa should be performed using yeast or mycelial phase.115 Various reports used the yeast-like cells116 according to the statement that these cells are the infective form, but still, the results obtained from using different growth phases of this morphology are considerably different.115
Bao and collaborators compared the antifungal sensitivity of S. globosa yeast and mycelial phases. They found that all the studied clinical isolates were highly sensitive to itraconazole and insensitive to fluconazole. However, they also reported differences in the minimum inhibitory concentration (MIC) between the mycelial and yeast phases, which were significant for itraconazole, voriconazole, posaconazole, 5-fluorouracil, and echinocandins. The reasons for this variation in antifungal susceptibility in vitro are still unclear.115
A study that tested in vitro antifungal susceptibility of 80 S. globosa isolates showed that the sensitivity is dependent on the incubation temperature and growth phase. The in vitro susceptibility profile of the nine drugs tested demonstrated that as the incubation temperature of the microplates increased, MICs were significantly decreased, except for amphotericin B and terbinafine.117 Additionally, terbinafine was the most active agent, regardless of incubation temperature or growth phase; however, it is not recommended as a first-line treatment for cutaneous sporotrichosis. All isolates tested were resistant to voriconazole.117
Amphotericin B is suggested for life-threatening cases.104 High MIC values are reported against S. globosa mycelial and yeast phases, and there were no significant differences between them.115
Drug resistance and complications during antifungal therapy are major concerns, especially in patients with liver disorders, children, and pregnant women. Different alternatives are being developed, such as photodynamic therapy (PDT). Li et al evaluated the in vitro and in vivo S. globosa susceptibility to photodynamic inactivation using methylene blue as a photosensitizer and LED as the light source. PDT-methylene blue could effectively inhibit sporotrichosis in vivo, and this method also shows the advantage of avoiding the adverse side effects caused by drugs (Table 3).113
Concluding Remarks
Although the first sporotrichosis case was reported more than a century ago, it was until 2007 that the etiological agents of this mycosis were identified, and even more recently their genomes were sequenced and made available.24,28 Therefore, the current vision we have about the clinically relevant Sporothrix species can be considered recent and limited.
Many efforts to understand the Sporothrix-host interaction have been made, but these have focused on S. schenckii and S. brasiliensis. However, to fully understand sporotrichosis, all the causative agents should be studied at the same level. So far, S. globosa genetic modification has not been reported, like in S. schenckii, and the availability of the genome sequences opens the possibility to generate mutant strains and to produce recombinant proteins to start characterizing the virulence factors of this fungal species. Although the genome is not annotated, the information that we already know about S. schenckii and S. brasiliensis paves the way to start analyzing the mechanisms behind S. globosa virulence and antifungal sensibility. For example, the contribution of some virulence factors already confirmed in S. schenckii and S. brasiliensis, such as SsCmk1, SsDrk1, Gp70, and proteins of the PRM, can be evaluated in S. globosa to establish whether they have similar functions to those reported in other Sporothrix species, or perform species-specific tasks, adding evidence that helps us to better understand the phenotypes displayed by these organisms.
Also, a deeper insight into the immune response against S. globosa could contribute to the knowledge of the host–fungus interaction. For this, the composition of the S. globosa cell wall needs to be fully evaluated, to explain the differences observed in the recognition by the host immune response of the three Sporothrix species. Moreover, it is important to determine the immune receptors that recognize this species and the role of different immune cells when interacting with S. globosa cells.
The antifungal drug resistance observed in S. globosa highlights the importance of prompt identification of the sporotrichosis etiological agent, to provide a suitable treatment to control the infection.
In conclusion, S. globosa is a well-known etiological agent of sporotrichosis, but there is an opportunity area in the study of its biological and clinical aspects. Therefore, further molecular, genetic, immunological, epidemiological, and clinical studies of this organism will positively impact the diagnosis and treatment of this infection.
Acknowledgments
This work was supported by Consejo Nacional de Ciencia y Tecnología (ref. FC 2015-02-834 and CF-2019-6380), and Red Temática Glicociencia en Salud (CONACYT-México).
Author Contributions
All authors made a significant contribution to the work reported, in the conception, design, execution, acquisition of data, analysis, and interpretation, critically reviewed the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare no conflict of interest.
References
- 1.Lopes-Bezerra LM, Mora-Montes HM, Zhang Y, et al. Sporotrichosis between 1898 and 2017: the evolution of knowledge on a changeable disease and on emerging etiological agents. Med Mycol. 2018;56(suppl_1):126–143. doi: 10.1093/mmy/myx103 [DOI] [PubMed] [Google Scholar]
- 2.Mora-Montes HM, Dantas Ada S, Trujillo-Esquivel E, de Souza Baptista AR, Lopes-Bezerra LM. Current progress in the biology of members of the Sporothrix schenckii complex following the genomic era. FEMS Yeast Res. 2015;15(6):fov065. doi: 10.1093/femsyr/fov065 [DOI] [PubMed] [Google Scholar]
- 3.López-Romero E, Reyes-Montes Mdel R, Pérez-Torres A, et al. Sporothrix schenckii complex and sporotrichosis, an emerging health problem. Future Microbiol. 2011;6(1):85–102. doi: 10.2217/fmb.10.157 [DOI] [PubMed] [Google Scholar]
- 4.Rossow JA, Queiroz-Telles F, Caceres DH, et al. A one health approach to combatting Sporothrix brasiliensis: narrative review of an emerging zoonotic fungal pathogen in South America. J Fungi. 2020;6(4):247. doi: 10.3390/jof6040247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han HS, Kano R. Feline sporotrichosis in Asia. Braz J Microbiol. 2020;52:125–134. doi: 10.1007/s42770-020-00274-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodrigues AM, Della Terra PP, Gremião ID, Pereira SA, Orofino-Costa R, de Camargo ZP. The threat of emerging and re-emerging pathogenic Sporothrix species. Mycopathologia. 2020;185(5):813–842. doi: 10.1007/s11046-020-00425-0 [DOI] [PubMed] [Google Scholar]
- 7.de Beer ZW, Duong TA, Wingfield MJ. The divorce of Sporothrix and Ophiostoma: solution to a problematic relationship. Stud Mycol. 2016;83:165–191. doi: 10.1016/j.simyco.2016.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodrigues AM, de Hoog GS, de Camargo ZP. Sporothrix species causing outbreaks in animals and humans driven by animal-animal transmission. PLoS Pathog. 2016;12(7):e1005638. doi: 10.1371/journal.ppat.1005638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Etchecopaz AN, Lanza N, Toscanini MA, et al. Sporotrichosis caused by Sporothrix brasiliensis in Argentina: case report, molecular identification and in vitro susceptibility pattern to antifungal drugs. J Mycol Med. 2020;30(1):100908. doi: 10.1016/j.mycmed.2019.100908 [DOI] [PubMed] [Google Scholar]
- 10.Gremião ID, Miranda LH, Reis EG, Rodrigues AM, Pereira SA. Zoonotic epidemic of sporotrichosis: cat to human transmission. PLoS Pathog. 2017;13(1):e1006077. doi: 10.1371/journal.ppat.1006077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moussa TAA, Kadasa NMS, Al Zahrani HS, et al. Origin and distribution of Sporothrix globosa causing sapronoses in Asia. J Med Microbiol. 2017;66(5):560–569. doi: 10.1099/jmm.0.000451 [DOI] [PubMed] [Google Scholar]
- 12.Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, Mochizuki T, Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015;53(1):3–14. doi: 10.1093/mmy/myu062 [DOI] [PubMed] [Google Scholar]
- 13.Camacho E, León-Navarro I, Rodríguez-Brito S, Mendoza M, Niño-Vega GA. Molecular epidemiology of human sporotrichosis in Venezuela reveals high frequency of Sporothrix globosa. BMC Infect Dis. 2015;15:94. doi: 10.1186/s12879-015-0839-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou X, Rodrigues AM, Feng P, de Hoog GS. Global ITS diversity in the Sporothrix schenckii complex. Fungal Divers. 2014;66(1):153–165. [Google Scholar]
- 15.Zhang Y, Hagen F, Stielow B, et al. Phylogeography and evolutionary patterns in Sporothrix spanning more than 14 000 human and animal case reports. Persoonia. 2015;35:1–20. doi: 10.3767/003158515X687416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marimon R, Cano J, Gené J, Sutton DA, Kawasaki M, Guarro J. Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol. 2007;45(10):3198–3206. doi: 10.1128/JCM.00808-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madrid H, Cano J, Gene J, Bonifaz A, Toriello C, Guarro J. Sporothrix globosa, a pathogenic fungus with widespread geographical distribution. Rev Iberoam Micol. 2009;26(3):218–222. doi: 10.1016/j.riam.2009.02.005 [DOI] [PubMed] [Google Scholar]
- 18.Zhao L, Cui Y, Zhen Y, et al. Genetic variation of Sporothrix globosa isolates from diverse geographic and clinical origins in China. Emerg Microbes Infect. 2017;6(10):e88. doi: 10.1038/emi.2017.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.New D, Beukers AG, Kidd SE, et al. Identification of multiple species and subpopulations among Australian clinical Sporothrix isolates using whole genome sequencing. Med Mycol. 2019;57(7):905–908. doi: 10.1093/mmy/myy126 [DOI] [PubMed] [Google Scholar]
- 20.Rudramurthy SM, Shankarnarayan SA, Hemashetter BM, et al. Phenotypic and molecular characterisation of Sporothrix globosa of diverse origin from India. Braz J Microbiol. 2021;52(1):91–100. doi: 10.1007/s42770-020-00346-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruz R, Vieille P, Oschilewski D. Aislamiento ambiental de Sporothrix globosa en relación a un caso de esporotricosis linfo-cutánea. Rev chil infectol. 2012;29:401–405. doi: 10.4067/S0716-10182012000400006 [DOI] [PubMed] [Google Scholar]
- 22.Rodrigues AM, de Hoog S, de Camargo ZP. Emergence of pathogenicity in the Sporothrix schenckii complex. Med Mycol. 2013;51(4):405–412. doi: 10.3109/13693786.2012.719648 [DOI] [PubMed] [Google Scholar]
- 23.de Oliveira MM, de Almeida-paes R, de Medeiros Muniz M, de Lima Barros MB, Galhardo MC, Zancope-Oliveira RM. Sporotrichosis caused by Sporothrix globosa in Rio De Janeiro, brazil: case report. Mycopathologia. 2010;169(5):359–363. doi: 10.1007/s11046-010-9276-7 [DOI] [PubMed] [Google Scholar]
- 24.Huang L, Gao W, Giosa D, et al. Whole-genome sequencing and in silico analysis of two strains of Sporothrix globosa. Genome Biol Evol. 2016;8(11):3292–3296. doi: 10.1093/gbe/evw230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fernandes KSS, Mathews HL, Bezerra LML. Differences in virulence of Sporothrix schenckii conidia related to culture conditions and cell-wall components. J Med Microbiol. 1999;48(2):195–203. doi: 10.1099/00222615-48-2-195 [DOI] [PubMed] [Google Scholar]
- 26.Martinez-Alvarez JA, Perez-Garcia LA, Mellado-Mojica E, et al. Sporothrix schenckii sensu stricto and Sporothrix brasiliensis are differentially recognized by human peripheral blood mononuclear cells. Front Microbiol. 2017;8:843. doi: 10.3389/fmicb.2017.00843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garcia-Carnero LC, Clavijo-Giraldo DM, Gomez-Gaviria M, et al. Early virulence predictors during the Candida species-Galleria mellonella Interaction. J Fungi. 2020;6(3):152. doi: 10.3390/jof6030152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teixeira MM, de Almeida LG, Kubitschek-Barreira P, et al. Comparative genomics of the major fungal agents of human and animal sporotrichosis: Sporothrix schenckii and Sporothrix brasiliensis. BMC Genomics. 2014;15:943. doi: 10.1186/1471-2164-15-943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.D’Alessandro E, Giosa D, Huang L, et al. Draft genome sequence of the dimorphic fungus Sporothrix pallida, a nonpathogenic species belonging to Sporothrix, a genus containing agents of human and feline sporotrichosis. Genome Announc. 2016;4(2):e00184–00116. doi: 10.1128/genomeA.00184-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prakash H, Karuppiah P, A Al-Dhabi N, et al. Comparative genomics of Sporothrix species and identification of putative pathogenic-gene determinants. Future Microbiol. 2020;15:1465–1481. doi: 10.2217/fmb-2019-0302 [DOI] [PubMed] [Google Scholar]
- 31.Mesa-Arango AC, Del Rocío Reyes-Montes M, Pérez-Mejía A, et al. Phenotyping and genotyping of Sporothrix schenckii isolates according to geographic origin and clinical form of sporotrichosis. J Clin Microbiol. 2002;40(8):3004–3011. doi: 10.1128/JCM.40.8.3004-3011.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lozoya-Perez NE, Clavijo-Giraldo DM, Martinez-Duncker I, et al. Influences of the culturing media in the virulence and cell wall of Sporothrix schenckii, Sporothrix brasiliensis, and Sporothrix globosa. J Fungi. 2020;6(4):323. doi: 10.3390/jof6040323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rodrigues AM, de Hoog G, Zhang Y, de Camargo ZP. Emerging sporotrichosis is driven by clonal and recombinant Sporothrix species. Emerg Microbes Infect. 2014;3(5):e32. doi: 10.1038/emi.2014.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kano R, Anzawa K, Mochizuki T, et al. Sporothrix schenckii (sensu strict S. globosa) mating type 1-2 (MAT1-2) gene. J Dermatol. 2013;40(9):726–730. doi: 10.1111/1346-8138.12226 [DOI] [PubMed] [Google Scholar]
- 35.Rangel-Gamboa L, Martínez-Hernandez F, Maravilla P, Arenas-Guzmán R, Flisser A. Update of phylogenetic and genetic diversity of Sporothrix schenckii sensu lato. Med Mycol. 2016;54(3):248–255. doi: 10.1093/mmy/myv096 [DOI] [PubMed] [Google Scholar]
- 36.de Carvalho JA, Beale MA, Hagen F, et al. Trends in the molecular epidemiology and population genetics of emerging Sporothrix species. Stud Mycol. 2021;100:100129. doi: 10.1016/j.simyco.2021.100129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lopes-Bezerra LM, Walker LA, Nino-Vega G, et al. Cell walls of the dimorphic fungal pathogens Sporothrix schenckii and Sporothrix brasiliensis exhibit bilaminate structures and sloughing of extensive and intact layers. PLoS Negl Trop Dis. 2018;12(3):e0006169. doi: 10.1371/journal.pntd.0006169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Villalobos-Duno HL, Barreto LA, Alvarez-Aular Á, et al. Comparison of cell wall polysaccharide composition and structure between strains of Sporothrix schenckii and Sporothrix brasiliensis. Front Microbiol. 2021;12:726958. doi: 10.3389/fmicb.2021.726958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lozoya-Perez NE, Casas-Flores S, Martinez-Alvarez JA, et al. Generation of Sporothrix schenckii mutants expressing the green fluorescent protein suitable for the study of host-fungus interactions. Fungal Biol. 2018;122(10):1023–1030. doi: 10.1016/j.funbio.2018.07.004 [DOI] [PubMed] [Google Scholar]
- 40.Clavijo-Giraldo DM, Matinez-Alvarez JA, Lopes-Bezerra LM, et al. Analysis of Sporothrix schenckii sensu stricto and Sporothrix brasiliensis virulence in Galleria mellonella. J Microbiol Methods. 2016;122:73–77. doi: 10.1016/j.mimet.2016.01.014 [DOI] [PubMed] [Google Scholar]
- 41.Silva-Bailão MG, de Sousa Lima P, Evangelista de Oliveira MM, et al. Comparative proteomics in the three major human pathogenic species of the genus Sporothrix. Microbes Infect. 2020;23. doi: 10.1016/j.micinf.2020.09.008 [DOI] [PubMed] [Google Scholar]
- 42.Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv113. doi: 10.1126/scitranslmed.3004404 [DOI] [PubMed] [Google Scholar]
- 43.Casadevall A, Pirofski LA, Fischetti VA. Host-pathogen interactions: redefining the basic concepts of virulence and pathogenicity. Infect Immun. 1999;67(8):3703–3713. doi: 10.1128/IAI.67.8.3703-3713.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garcia-Carnero LC, Perez-Garcia LA, Martinez-Alvarez JA, Reyes-Martinez JE, Mora-Montes HM. Current trends to control fungal pathogens: exploiting our knowledge in the host-pathogen interaction. Infect Drug Resist. 2018;11:903–913. doi: 10.2147/IDR.S170337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arrillaga-Moncrieff I, Capilla J, Mayayo E, et al. Different virulence levels of the species of Sporothrix in a murine model. Clin Microbiol Infect. 2009;15(7):651–655. doi: 10.1111/j.1469-0691.2009.02824.x [DOI] [PubMed] [Google Scholar]
- 46.Cruz Choappa R, Pérez Gaete S, Rodríguez Badilla V, Vieille Oyarzo P, Opazo Sanchez H. Virulence of Sporothrix globosa in murine models. Rev Argent Microbiol. 2016;48(3):196–199. doi: 10.1016/j.ram.2016.04.007 [DOI] [PubMed] [Google Scholar]
- 47.Della Terra PP, Rodrigues AM, Fernandes GF, Nishikaku AS, Burger E, de Camargo ZP. Exploring virulence and immunogenicity in the emerging pathogen Sporothrix brasiliensis. PLoS Negl Trop Dis. 2017;11(8):e0005903–e0005903. doi: 10.1371/journal.pntd.0005903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gow NA, Netea MG, Munro CA, et al. Immune recognition of Candida albicans beta-glucan by dectin-1. J Infect Dis. 2007;196(10):1565–1571. doi: 10.1086/523110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Csermely P, Schnaider T, So″ti C, Prohászka Z, Nardai G. The 90-kDa molecular chaperone family: structure, function, and clinical applications. a comprehensive review. Pharmacol Ther. 1998;79(2):129–168. doi: 10.1016/s0163-7258(98)00013-8 [DOI] [PubMed] [Google Scholar]
- 50.Rodriguez-Caban J, Gonzalez-Velazquez W, Perez-Sanchez L, Gonzalez-Mendez R, Rodriguez-del Valle N. Calcium/calmodulin kinase1 and its relation to thermotolerance and HSP90 in Sporothrix schenckii: an RNAi and yeast two-hybrid study. BMC Microbiol. 2011;11:162. doi: 10.1186/1471-2180-11-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang Z, Hou B, Wu YZ, Wang Y, Liu X, Han S. Two‑component histidine kinase DRK1 is required for pathogenesis in Sporothrix schenckii. Mol Med Rep. 2018;17(1):721–728. doi: 10.3892/mmr.2017.8005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hou B, Zhang Z, Zheng F, Liu X. Molecular cloning, characterization and differential expression of DRK1 in Sporothrix schenckii. Int J Mol Med. 2013;31(1):99–104. doi: 10.3892/ijmm.2012.1193 [DOI] [PubMed] [Google Scholar]
- 53.Jacobson ES. Pathogenic roles for fungal melanins. Clin Microbiol Rev. 2000;13(4):708–717. doi: 10.1128/CMR.13.4.708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Romero-Martinez R, Wheeler M, Guerrero-Plata A, Rico G, Torres-Guerrero H. Biosynthesis and functions of melanin in Sporothrix schenckii. Infect Immun. 2000;68(6):3696–3703. doi: 10.1128/IAI.68.6.3696-3703.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mario DA, Santos RC, Denardi LB, Vaucher Rde A, Santurio JM, Alves SH. Interference of melanin in the susceptibility profile of Sporothrix species to amphotericin B. Rev Iberoam Micol. 2016;33(1):21–25. doi: 10.1016/j.riam.2015.03.001 [DOI] [PubMed] [Google Scholar]
- 56.Aquino-Piñero E, Rodríguez-del Valle N. Characterization of a protein kinase C gene in Sporothrix schenckii and its expression during the yeast-to-mycelium transition. Med Mycol. 2002;40(2):185–199. doi: 10.1080/mmy.40.2.185.199 [DOI] [PubMed] [Google Scholar]
- 57.Serrano S, Valle N. Calcium uptake and efflux during the yeast to mycelium transition in Sporothrix schenckii. Mycopathologia. 1990;112(1):1–9. doi: 10.1007/BF01795170 [DOI] [PubMed] [Google Scholar]
- 58.Martinez-Alvarez JA, Garcia-Carnero LC, Kubitschek-Barreira PH, et al. Analysis of some immunogenic properties of the recombinant Sporothrix schenckii Gp70 expressed in Escherichia coli. Future Microbiol. 2019;14:397–410. doi: 10.2217/fmb-2018-0295 [DOI] [PubMed] [Google Scholar]
- 59.Ruiz-Baca E, Toriello C, Perez-Torres A, Sabanero-Lopez M, Villagomez-Castro JC, Lopez-Romero E. Isolation and some properties of a glycoprotein of 70 kDa (Gp70) from the cell wall of Sporothrix schenckii involved in fungal adherence to dermal extracellular matrix. Med Mycol. 2009;47(2):185–196. doi: 10.1080/13693780802165789 [DOI] [PubMed] [Google Scholar]
- 60.Rodrigues AM, Kubitschek-Barreira PH, Fernandes GF, de Almeida SR, Lopes-Bezerra LM, de Camargo ZP. Immunoproteomic analysis reveals a convergent humoral response signature in the Sporothrix schenckii complex. J Proteomics. 2015;115:8–22. doi: 10.1016/j.jprot.2014.11.013 [DOI] [PubMed] [Google Scholar]
- 61.de Almeida JRF, Jannuzzi GP, Kaihami GH, Breda LCD, Ferreira KS, de Almeida SR. An immunoproteomic approach revealing peptides from Sporothrix brasiliensis that induce a cellular immune response in subcutaneous sporotrichosis. Sci Rep. 2018;8(1):4192. doi: 10.1038/s41598-018-22709-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lozoya-Pérez NE, García-Carnero LC, Martínez-álvarez JA, Martínez-Duncker I, Mora-Montes HM. Tenebrio molitor as an alternative model to analyze the Sporothrix species virulence. Infect Drug Resist. 2021;14:2059–2072. doi: 10.2147/IDR.S312553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.de Almeida JR, Santiago KL, Kaihami GH, Maranhão AQ, de Macedo Brígido M, de Almeida SR. The efficacy of humanized antibody against the Sporothrix antigen, gp70, in promoting phagocytosis and reducing disease burden. Front Microbiol. 2017;8:345. doi: 10.3389/fmicb.2017.00345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen F, Jiang R, Wang Y, et al. Recombinant phage elicits protective immune response against systemic S. globosa infection in mouse model. Sci Rep. 2017;7:42024. doi: 10.1038/srep42024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Almeida JR, Kaihami GH, Jannuzzi GP, de Almeida SR. Therapeutic vaccine using a monoclonal antibody against a 70-kDa glycoprotein in mice infected with highly virulent Sporothrix schenckii and Sporothrix brasiliensis. Med Mycol. 2015;53(1):42–50. doi: 10.1093/mmy/myu049 [DOI] [PubMed] [Google Scholar]
- 66.Castro RA, Kubitschek-Barreira PH, Teixeira PA, et al. Differences in cell morphometry, cell wall topography and gp70 expression correlate with the virulence of Sporothrix brasiliensis clinical isolates. PLoS One. 2013;8(10):e75656. doi: 10.1371/journal.pone.0075656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rossato L, Moreno LF, Jamalian A, et al. Proteins potentially involved in immune evasion strategies in Sporothrix brasiliensis elucidated by ultra-high-resolution mass spectrometry. mSphere. 2018;3(3):e00514–00517. doi: 10.1128/mSphere.00514-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Portuondo DL, Dores-Silva PR, Ferreira LS, et al. Immunization with recombinant enolase of Sporothrix spp. (rSsEno) confers effective protection against sporotrichosis in mice. Sci Rep. 2019;9(1):17179. doi: 10.1038/s41598-019-53135-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Téllez MD, Batista-Duharte A, Portuondo D, Quinello C, Bonne-Hernández R, Carlos IZ. Sporothrix schenckii complex biology: environment and fungal pathogenicity. Microbiology. 2014;160(Pt 11):2352–2365. doi: 10.1099/mic.0.081794-0 [DOI] [PubMed] [Google Scholar]
- 70.Tsuboi R, Sanada T, Takamori K, Ogawa H. Isolation and properties of extracellular proteinases from Sporothrix schenckii. J Bacteriol. 1987;169(9):4104–4109. doi: 10.1128/jb.169.9.4104-4109.1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hogan LH, Klein BS, Levitz SM. Virulence factors of medically important fungi. Clin Microbiol Rev. 1996;9(4):469–488. doi: 10.1128/CMR.9.4.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Da Rosa D, Gezuele E, Calegari L, Goñi F. Excretion-secretion products and proteases from live Sporothrix schenckii yeast phase: immunological detection and cleavage of human IgG. Rev Inst Med Trop Sao Paulo. 2009;51(1):1–7. doi: 10.1590/S0036-46652009000100001 [DOI] [PubMed] [Google Scholar]
- 73.Lima OC, Bezerra LML. Identification of a concanavalin A-binding antigen of the cell surface of Sporothrix schenckii. J Med Vet Mycol. 1997;35(3):167–172. doi: 10.1080/02681219780001101 [DOI] [PubMed] [Google Scholar]
- 74.Sandoval-Bernal G, Barbosa-Sabanero G, Shibayama M, Perez-Torres A, Tsutsumi V, Sabanero M. Cell wall glycoproteins participate in the adhesion of Sporothrix schenckii to epithelial cells. Mycopathologia. 2011;171(4):251–259. doi: 10.1007/s11046-010-9372-8 [DOI] [PubMed] [Google Scholar]
- 75.Oda LM, Kubelka CF, Alviano CS, Travassos LR. Ingestion of yeast forms of Sporothrix schenckii by mouse peritoneal macrophages. Infect Immun. 1983;39(2):497–504. doi: 10.1128/iai.39.2.497-504.1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lloyd KO, Bitoon MA. Isolation and purification of a peptido-rhamnomannan from the yeast form of Sporothrix schenckii. Structural and immunochemical studies. J Immunol. 1971;107(3):663–671. [PubMed] [Google Scholar]
- 77.García-Carnero LC, Salinas-Marín R, Lozoya-Pérez NE, et al. The heat shock protein 60 and Pap1 participate in the Sporothrix schenckii-host interaction. J Fungi. 2021;7(11):960. doi: 10.3390/jof7110960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tamez-Castrellon AK, Romeo O, Garcia-Carnero LC, Lozoya-Perez NE, Mora-Montes HM. Virulence factors in Sporothrix schenckii, one of the causative agents of sporotrichosis. Curr Protein Pept Sci. 2020;21(3):295–312. doi: 10.2174/1389203720666191007103004 [DOI] [PubMed] [Google Scholar]
- 79.Joffre O, Nolte MA, Spörri R, Reis e Sousa C. Inflammatory signals in dendritic cell activation and the induction of adaptive immunity. Immunol Rev. 2009;227(1):234–247. doi: 10.1111/j.1600-065X.2008.00718.x [DOI] [PubMed] [Google Scholar]
- 80.Almeida S. Therapeutic monoclonal antibody for sporotrichosis. Front Microbiol. 2012;3:409. doi: 10.3389/fmicb.2012.00409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fernandes GF, Dos Santos PO, Rodrigues AM, Sasaki AA, Burger E, de Camargo ZP. Characterization of virulence profile, protein secretion and immunogenicity of different Sporothrix schenckii sensu stricto isolates compared with S. globosa and S. brasiliensis species. Virulence. 2013;4(3):241–249. doi: 10.4161/viru.23112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Drummond RA, Brown GD. The role of Dectin-1 in the host defence against fungal infections. Curr Opin Microbiol. 2011;14(4):392–399. doi: 10.1016/j.mib.2011.07.001 [DOI] [PubMed] [Google Scholar]
- 83.Martinez-Alvarez JA, Perez-Garcia LA, Flores-Carreon A, Mora-Montes HM. The immune response against Candida spp. and Sporothrix schenckii. Rev Iberoam Micol. 2014;31(1):62–66. doi: 10.1016/j.riam.2013.09.015 [DOI] [PubMed] [Google Scholar]
- 84.Almeida-Paes R, de Oliveira LC, Oliveira MME, Gutierrez-Galhardo MC, Nosanchuk JD, Zancopé-Oliveira RM. Phenotypic characteristics associated with virulence of clinical isolates from the Sporothrix complex. Biomed Res Int. 2015;2015:212308. doi: 10.1155/2015/212308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Madrid IM, Xavier MO, Mattei AS, et al. Role of melanin in the pathogenesis of cutaneous sporotrichosis. Microbes Infect. 2010;12(2):162–165. doi: 10.1016/j.micinf.2009.10.004 [DOI] [PubMed] [Google Scholar]
- 86.Song Y, Yao L, Zhen Y, et al. Sporothrix globosa melanin inhibits antigen presentation by macrophages and enhances deep organ dissemination. Braz J Microbiol. 2021;52(1):19–31. doi: 10.1007/s42770-020-00345-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jiao Q, Luo Y, Scheffel J, et al. Skin mast cells contribute to Sporothrix schenckii infection. Front Immunol. 2020;11:469. doi: 10.3389/fimmu.2020.00469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Romo-Lozano Y, Hernández-Hernández F, Salinas E. Mast cell activation by conidia of Sporothrix schenckii: role in the severity of infection. Scand J Immunol. 2012;76(1):11–20. doi: 10.1111/j.1365-3083.2012.02706.x [DOI] [PubMed] [Google Scholar]
- 89.Cambi A, Netea MG, Mora-Montes HM, et al. Dendritic cell interaction with Candida albicans critically depends on N-linked mannan. J Biol Chem. 2008;283(29):20590–20599. doi: 10.1074/jbc.M709334200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Verdan FF, Faleiros JC, Ferreira LS, et al. Dendritic cell are able to differentially recognize Sporothrix schenckii antigens and promote Th1/Th17 response in vitro. Immunobiology. 2012;217(8):788–794. doi: 10.1016/j.imbio.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 91.Kusuhara M, Qian H, Li X, et al. Mouse bone marrow-derived dendritic cells can phagocytize the Sporothrix schenckii, and mature and activate the immune response by secreting interleukin-12 and presenting antigens to T lymphocytes. J Dermatol. 2014;41(5):386–392. doi: 10.1111/1346-8138.12472 [DOI] [PubMed] [Google Scholar]
- 92.Zu J, Yao L, Song Y, et al. Th2 Biased immunity with altered B cell profiles in circulation of patients with sporotrichosis caused by Sporothrix globosa. Front Immunol. 2020;11:570888. doi: 10.3389/fimmu.2020.570888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Uenotsuchi T, Takeuchi S, Matsuda T, et al. Differential induction of Th1-prone immunity by human dendritic cells activated with Sporothrix schenckii of cutaneous and visceral origins to determine their different virulence. Int Immunol. 2006;18(12):1637–1646. doi: 10.1093/intimm/dxl097 [DOI] [PubMed] [Google Scholar]
- 94.Nascimento RC, Almeida SR. Humoral immune response against soluble and fractionate antigens in experimental sporotrichosis. FEMS Immunol Med Microbiol. 2005;43(2):241–247. doi: 10.1016/j.femsim.2004.08.004 [DOI] [PubMed] [Google Scholar]
- 95.Almeida-Paes R, Pimenta MA, Monteiro PC, Nosanchuk JD, Zancopé-Oliveira RM. Immunoglobulins G, M, and A against Sporothrix schenckii exoantigens in patients with sporotrichosis before and during treatment with itraconazole. Clin Vaccine Immunol. 2007;14(9):1149–1157. doi: 10.1128/CVI.00149-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kozel TR. Activation of the complement system by pathogenic fungi. Clin Microbiol Rev. 1996;9(1):34–46. doi: 10.1128/CMR.9.1.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vidarsson G, Dekkers G, Rispens T. IgG subclasses and allotypes: from structure to effector functions. Front Immunol. 2014;5:520. doi: 10.3389/fimmu.2014.00520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chen F, Jiang R, Dong S, Yan B. Efficient treatment of Sporothrix globosa infection using the antibody elicited by recombinant phage nanofibers. Front Pharmacol. 2019;10:160. doi: 10.3389/fphar.2019.00160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kong X, Xiao T, Lin J, Wang Y, Chen HD. Relationships among genotypes, virulence and clinical forms of Sporothrix schenckii infection. Clin Microbiol Infect. 2006;12(11):1077–1081. doi: 10.1111/j.1469-0691.2006.01519.x [DOI] [PubMed] [Google Scholar]
- 100.Fischman Gompertz O, Rodrigues AM, Fernandes GF, Bentubo HDL, de Camargo ZP, Petri V. Atypical clinical presentation of sporotrichosis caused by Sporothrix globosa resistant to itraconazole. Am J Trop Med Hyg. 2016;94(6):1218–1222. doi: 10.4269/ajtmh.15-0267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gu A, Zhang X, Ma F, Nie Z, Sybren de Hoog G, Zhang Y. Fixed cutaneous sporotrichosis in a patient with numerous fungal elements. Med Mycol Case Rep. 2020;29:32–34. doi: 10.1016/j.mmcr.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Liu Y, Liu L, Kang M, Zong Z. An unhealing wound and subcutaneous nodules due to Sporothrix globosa after a cat bite. PLoS Negl Trop Dis. 2020;14(12):e0008859. doi: 10.1371/journal.pntd.0008859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liu F, Liu Y, Yuan N, et al. Fixed cutaneous sporotrichosis due to Sporothrix globosa. Clin Cosmet Investig Dermatol. 2021;14:91–96. doi: 10.2147/CCID.S288259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Orofino-Costa R, Macedo PM, Rodrigues AM, Bernardes-Engemann AR. Sporotrichosis: an update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. An Bras Dermatol. 2017;92(5):606–620. doi: 10.1590/abd1806-4841.2017279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang M, Li F, Gong J, Yang X, Zhang J, Zhao F. Development and evaluation of a real-time polymerase chain reaction for fast diagnosis of sporotrichosis caused by Sporothrix globosa. Med Mycol. 2020;58(1):61–65. doi: 10.1093/mmy/myz029 [DOI] [PubMed] [Google Scholar]
- 106.de Oliveira MME, Sampaio P, Almeida-Paes R, Pais C, Gutierrez-Galhardo MC, Zancope-Oliveira RM. Rapid identification of Sporothrix species by T3B fingerprinting. J Clin Microbiol. 2012;50(6):2159–2162. doi: 10.1128/JCM.00450-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rodrigues AM, Najafzadeh MJ, de Hoog GS, de Camargo ZP. Rapid identification of emerging human-pathogenic Sporothrix species with rolling circle amplification. Front Microbiol. 2015;6:1385. doi: 10.3389/fmicb.2015.01385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lopes-Bezerra LM, Mora-Montes HM, Bonifaz A. Sporothrix and sporotrichosis. In: Mora-Montes HM, Lopes-Bezerra LM, editors. Current Progress in Medical Mycology. Vol. 1. Switzerland: Springer, Cham; 2017:309–331. [Google Scholar]
- 109.Brito MM, Conceição-Silva F, Morgado FN, et al. Comparison of virulence of different Sporothrix schenckii clinical isolates using experimental murine model. Med Mycol. 2007;45(8):721–729. doi: 10.1080/13693780701625131 [DOI] [PubMed] [Google Scholar]
- 110.Bonifaz A, Vázquez-González D. Diagnosis and treatment of lymphocutaneous sporotrichosis: what are the options? Curr Fungal Infect Rep. 2013;7(3):252–259. doi: 10.1007/s12281-013-0140-3 [DOI] [Google Scholar]
- 111.de Lima Barros MB, Schubach AO, de Vasconcellos Carvalhaes de Oliveira R, Martins EB, Teixeira JL, Wanke B. Treatment of cutaneous sporotrichosis with itraconazole-study of 645 patients. Clin Infect Dis. 2011;52(12):e200–e206. doi: 10.1093/cid/cir245 [DOI] [PubMed] [Google Scholar]
- 112.Barros MB, de Almeida Paes R, Schubach AO. Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev. 2011;24(4):633–654. doi: 10.1128/CMR.00007-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Li J, Zhu M, An L, Chen F, Zhang X. Fungicidal efficacy of photodynamic therapy using methylene blue against Sporothrix globosa in vitro and in vivo. Eur J Dermatol. 2019;29(2):160–166. doi: 10.1684/ejd.2019.3527 [DOI] [PubMed] [Google Scholar]
- 114.Ottonelli Stopiglia CD, Magagnin CM, Castrillón MR, et al. Antifungal susceptibilities and identification of species of the Sporothrix schenckii complex isolated in Brazil. Med Mycol. 2014;52(1):56–64. doi: 10.3109/13693786.2013.818726 [DOI] [PubMed] [Google Scholar]
- 115.Bao F, Pan Q, Wang Z, Liu H, Zhang F. Susceptibility testing of clinical isolates of Sporothrix globosa in Shandong, China. Mycoses. 2020;63(11):1191–1194. doi: 10.1111/myc.13141 [DOI] [PubMed] [Google Scholar]
- 116.Li J, Zhan P, Jiang Q, et al. Prevalence and antifungal susceptibility of Sporothrix species in Jiangxi, central China. Med Mycol. 2019;57(8):954–961. doi: 10.1093/mmy/myy163 [DOI] [PubMed] [Google Scholar]
- 117.Song Y, Li S, Shi Y, et al. In vitro antifungal susceptibility of Sporothrix globosa isolates from Jilin Province, northeastern China: comparison of yeast and mycelial phases. Braz J Microbiol. 2021;52(1):81–90. doi: 10.1007/s42770-020-00316-y [DOI] [PMC free article] [PubMed] [Google Scholar]