Abstract
Background:
First pass effect (FPE) in mechanical thrombectomy is thought to be associated with good clinical outcomes. We performed this study to determine FPE rates as a function of thrombectomy technique and to compare clinical outcomes between patients with and without FPE.
Methods:
In July 2020, a literature search on FPE (defined as mTICI2c-3 after single pass) and modified FPE (mFPE, defined as TICI2b-3 after single pass) and mechanical thrombectomy for stroke was performed. Using random-effects meta-analysis, we evaluated following outcomes for both FPE and mFPE: overall rates, rates by thrombectomy technique, rates of good neurologic outcome (modified Rankin Scale (mRS) ≤2 at day 90), mortality, and sICH rate.
Results:
Sixty seven studies comprising 16,870 patients were included. Overall rates of FPE and mFPE were 28% and 45% respectively. Thrombectomy techniques shared a similar FPE (p=.17) and mFPE (p=.20) rates. Higher odds of good neurologic outcome were found when we compared FPE with non-FPE (56% vs 41%, OR 1.78) and mFPE with non-mFPE (57% vs 44%, OR 1.73). FPE had lower mortality rate (17% vs 25%, OR 0.62) than non-FPE. FPE and mFPE were not associated with lower sICH rate compared to non-FPE and non-mFPE (4% vs 18%, OR 0.41 for FPE; 5% vs 7%, OR 0.98 for mFPE).
Conclusions:
Our findings suggest that approximately one-third of patients achieve FPE and around half of patients achieve mFPE, with equivalent results throughout thrombectomy techniques.FPE and mFPE are associated with better clinical outcomes.
Keywords: First pass effect, modified first pass effect, thrombectomy, stroke, modified Rankin Scale
Introduction:
With mechanical thrombectomy (MT) becoming the standard of care for patients suffering from stroke due to large vessel occlusion (LVO), optimizing MT techniques to achieve better clinical outcomes has become increasingly important over the last couple of years. Previous studies have demonstrated the importance of minimizing delays to endovascular treatment and keeping thrombectomy procedural times less than 60 minutes (1). A shorter time to revascularization has been linked with better outcomes(2). Additionally, the number of passes to achieve successful angiographic outcomes has been suggested to affect clinical outcomes(3). Notably, first pass effect (FPE), first introduced by Zaidat, et al. and defined as complete revascularization of large vessel occlusion (mTICI 3) in a single thrombectomy pass, has been shown to be associated with better clinical outcomes compared to non-FPE (4). The impact of FPE on outcomes, as well as rates of FPE by thrombectomy device, is gaining widespread attention. FPE has become key index in evaluating the efficacy of new generation of devices in thrombectomy. Many studies have reported FPE is associated with better neurological outcome (mRS score 0–2 at 90 days) and lower mortality rate(5–7). We performed a systematic review and meta-analysis of studies providing data on FPE to assess overall rates and rates by type of thrombectomy technique, as well as to correlate clinical outcomes with presence or absence of FPE or mFPE.
Methods
Literature search and study selection
This study is reported in accordance with PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines. We performed a comprehensive literature search through July 2020. Several databases including PubMed, Ovid MEDLINE, and Ovid EMBASE were used to identify relevant articles. Keywords including first pass efficiency, first pass success, first pass revascularization, first pass recanalization, first pass effect, single pass success, first pass attempt, TICI-2b, TICI-2c, TICI-3, acute ischemic stroke, large vessel occlusion, thrombectomy were used in both ‘AND’ and ‘OR’ combinations. Identified studies were then further evaluated for inclusion in the meta-analysis. We searched the reference lists of included articles for additional papers. Inclusion criteria for studies in the analysis were the following: 1) acute ischemic stroke (AIS) patients with large vessel occlusion defined as occlusion of middle and anterior cerebral arteries, the vertebral, basilar and carotid terminus, as determined by MR angiography or, CT angiography, 2) retrospective or prospective articles or conference abstracts with at least ten patients, and 3) published in English. Exclusion criteria were the following: 1) studies with <10 patients, 2) animal/In-vitro studies only, and 3) case reports, letters, editorial comments, or review articles.
Two investigators independently reviewed the initial search results and selected relevant articles based on title and abstract for detailed review. In a case of duplication or overlapping study population (studies published on the same registry), studies with the largest patients’ population or the most amount of data relevant to our outcome were selected. The process of database search, study selection, data extraction, and final inclusion were reviewed in consensus with two investigators and was overseen by a board-certified interventional neuroradiologist.
Outcome variables
For the purpose of current study, we calculated the overall rate of FPE and mFPE (defined as achieving TICI 2b or greater after a single pass of device) and then correlated rates of FPE and mFPE with the type of thrombectomy technique (aspiration, stent-retriever, combination). We compared rates of clinical outcomes between FPE/non-FPE, mFPE/non-mFPE, FPE/ recanalized non-FPE, and mFPE/ recanalized non-mFPE. Recanalized non-FPE was defined as achieving mTICI 2c or higher on multiple passes and recanalized non-mFPE was considered as mTICI 2b or higher on multiple device passes The clinical outcomes we evaluated in this study were the good neurologic outcome, defined as an mRS of ≤2 at 90 days following MT, mortality rate, and symptomatic intracerebral hemorrhage (sICH) rate
Statistical analysis
Meta-analysis results were expressed as Odds Ratio (OR) for clinical outcomes and the rate for continuous outcomes with respective 95% Confidence Intervals (CIs). Random-effects meta-analysis was used for pooling across studies (8). The I2statistic was used to express the proportion of heterogeneity that is not attributable to chance (9). We explored the impact of publication bias by constructing funnel plots and checking for symmetry. Egger’s regression test was also used to evaluate publication bias. Meta-analysis was conducted using STATA version 14 (Stata Corp LP, College Station TX, USA).
Results
Literature search
A total of 151 articles were identified. After removing duplications, 87 were excluded based on abstract,title and full-text article assessment. A total of 67 articles reporting 16,870 patients were included for meta-analysis (Supplementary Table 1). A study selection flow diagram is provided in Figure 1.
Figure 1).
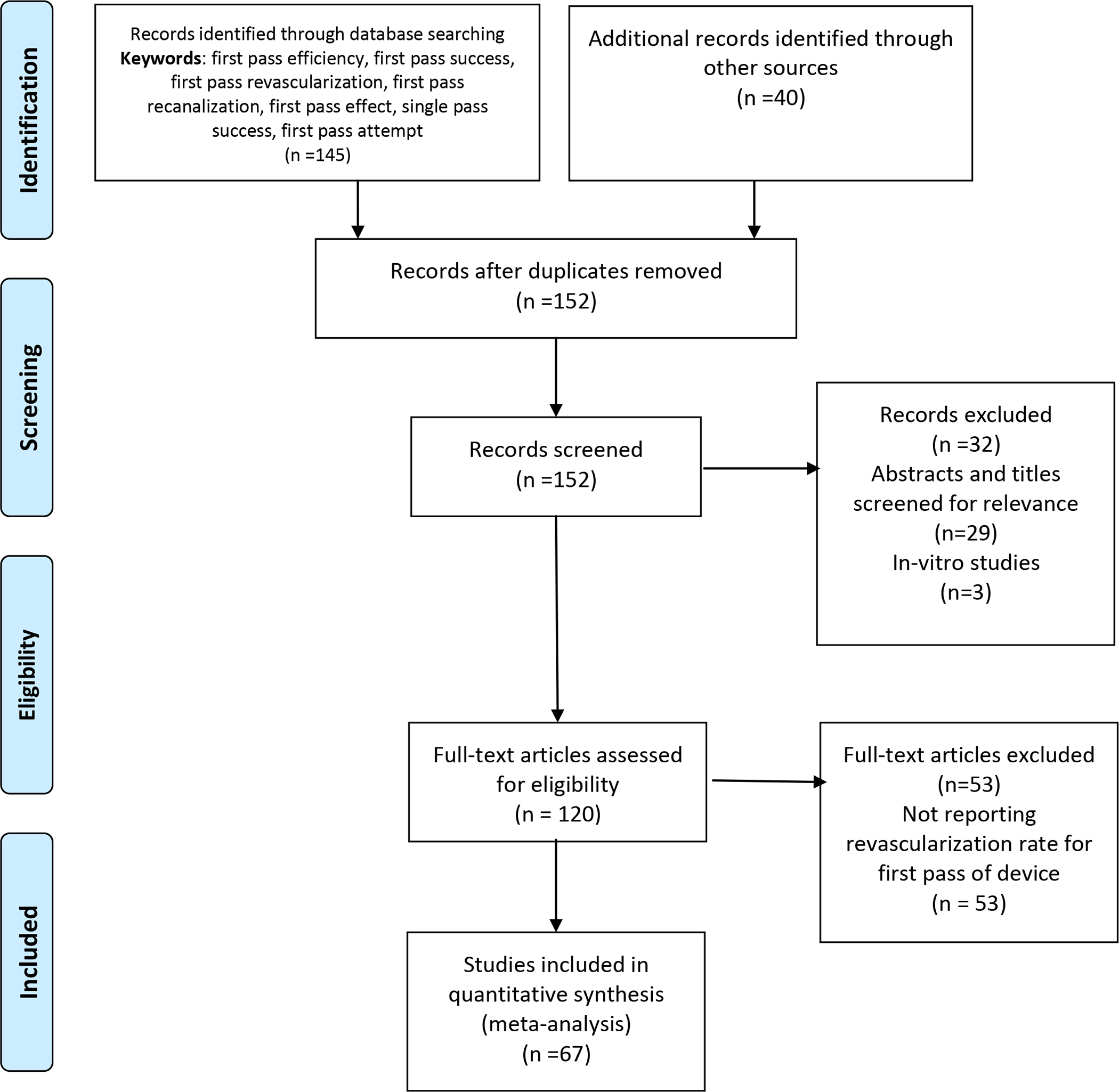
PRISMA flow diagram
All patients in the included studies were treated with direct aspiration, stent-retriever, or combination of stent-retriever/aspiration techniques. Twenty-six studies comprising 3708 patients were treated with aspiration alone (7, 10–34), while 34 studies including 6669 patients were stent-retriever technique alone (3–5, 7, 12, 15, 16, 18, 19, 22, 26–28, 30, 31, 35–53). Eight studies reported using combination of stent-retriever/aspiration for a total of 545 patients (12, 15, 18, 26, 31, 54–56). Eleven studies consisting of 5948 patients did not specify the technique that was used (6, 49, 57–63). Twenty-three studies which included 7299 patients provided direct comparative data between FPE and non-FPE (3–5, 7, 11, 16, 19, 26, 29, 33, 45, 53, 55, 59–68). Twelve studies provided additional data on mortality rate and complications (4, 7, 11, 16, 19, 50, 60–63, 65, 67, 68). moststudies were assessed as having a moderate risk of bias based on their non-randomized design. No studies were excluded for the high-risk of bias.
FPE Rate
As summarized in Figure 2 and Table 1, among 67 studies that reported mFPE and FPE rates, the overall rate was 28% (2440/ 9082) for FPE and 47% (5351/11689) for mFPE. FPE rate for aspiration, stent retriever, and combination technique was 29% (516/2147), 34% (1038/3312), and 26% (58/229) respectively. No statistically significant difference was noted when comparing FPE rate by thrombectomy techniques ((p=.17). mFPE rates were 48% (1653/3191) for aspiration, 48% (2211/4584) for stent retriever, and 58% (193/333) for combination technique. mFPE rate was not significantly different across thrombectomy techniques (p=.22, Supplementary Table 1).
Figure 2).
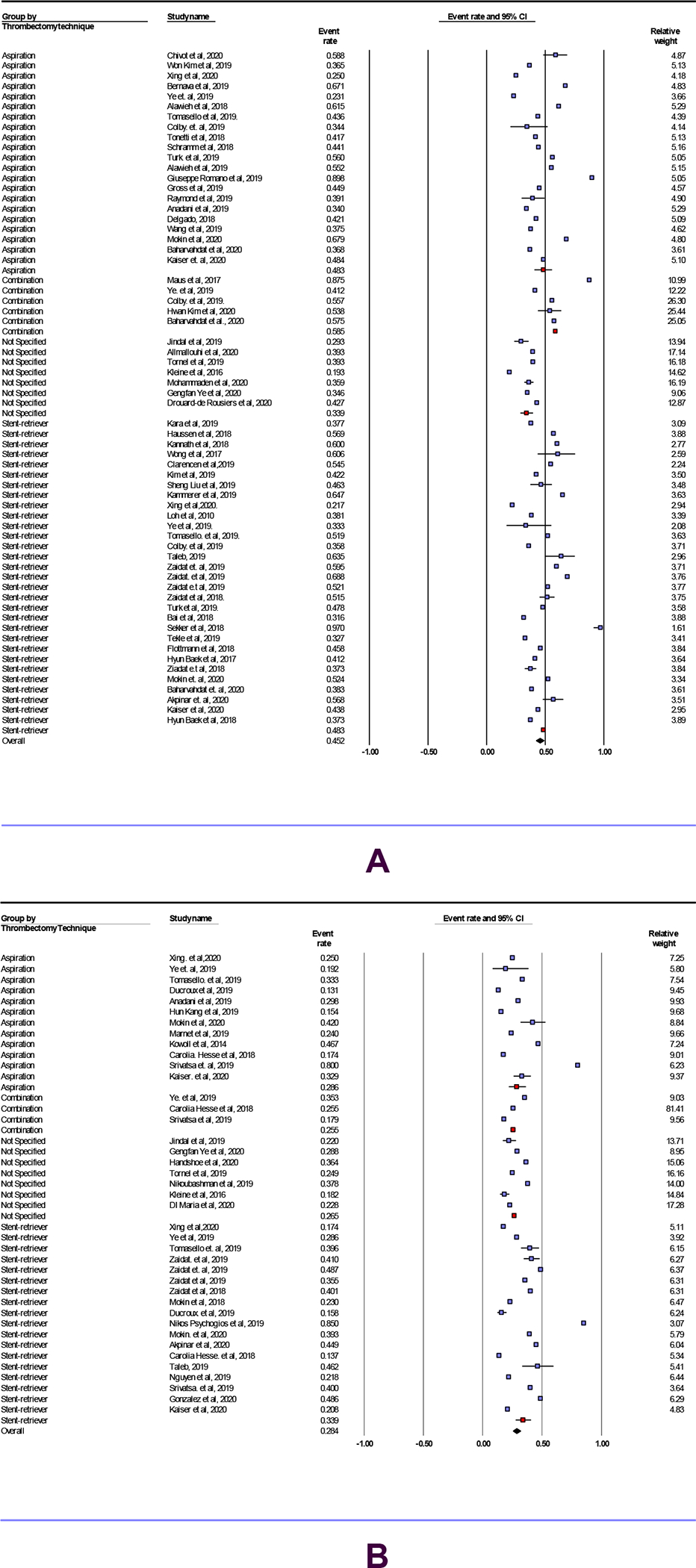
this forest plot compares mFPE (A) and FPE (B) rate between aspiration, stent-Retriever, Combination and, not specified groups.
TABLE 1.
FPE AND MFPE RATES
| THROMBECTOMY TECHNIQUE | Number of Studies (percentage) | FPE Rate ( 95% CI) | I2 heterogeneity | |
|---|---|---|---|---|
| ASPIRATION | 12 (30 %) | 29 (22–37)% | 90% | P-value |
| STENT RETRIEVER | 18 (45%) | 34 (28–40)% | 92% | 0.17 |
| COMBINATION | 3 (7.5%) | 26 (20–32)% | 0% | |
| NOT SPECIFIED | 7 (17.5%) | 27 (22–32)% | 87% | |
| OVERALL | 40 | 28 (26–32)% | 90% | |
| mFPE Rate ( 95% CI) | ||||
| ASPIRATION | 21 (34%) | 48% (40–55) | 93% | P-value |
| STENT RETRIEVER | 30 (48%) | 48% (44–53) | 90% | 0.20 |
| COMBINATION | 5 (8%) | 58% (48–68) | 66% | |
| NOT SPECIFIED | 7 (10%) | 34% (28–40) | 89% | |
| OVERALL | 63 | 45% (42–48) | 92% |
FPE: First pass effect; mFPE: modified first pass effect.
Clinical outcomes
Comparison of mFPE vs non-mFPE and FPE vs non-FPE
Findings are presented in Table 2. The rate of mRS 0–2 at 90 days was 56% (431/774) for FPE group compared with 41% (933/2285) for the non-FPE group (OR 1.78, 95% CI 1.50 to 2.11, p<0.01). Patients with mFPE had higher rate of mRS 0–2 at 90 days compared with non-mFPE patients (339 / 591 [57%] vs 402/ 91 [44%], OR 1.73, 95% CI 1.44 to 2.1, p<0.01; Figure 3). Compared to non-FPE group, patients with FPE had significantly lower mortality (129/771 [17%] vs 610/2457[25%]OR 0.62, 95% CI 0.50 to 0.76, p<0.01). sICH rate was not different between FPE and non-FPE group (28/651 [4%] vs 389/2118 [18%] 0.41 (0.09–1.93), OR 0.41, 95% CI 0.09 to 1.93, p= .26). The rate of mortality was (16%) 40/244 in the mFPE group and (21%) 132/634 for the non-mFPE group (OR 0.98, 95% CI 0.66 to 1.49, p= . 96) and the rate of sICH was 5% (13/245) (5%) vs 0.98(0.51 -1.88)for the mFPE group and 7% (47/670) for the non-mFPE group (OR 0.98, 95% CI 0.51 to 1.88, p= .95; Figure 4). (Supplementary Tables 2–4).
TABLE 2.
CLINICAL OUTCOMES
| Number Studies | Events/Total (percentage) | Odds ratio (CI 95%) | I2 heterogeneity | P-value | ||
|---|---|---|---|---|---|---|
| FPE | Non-FPE | FPE vs Non-FPE | ||||
| MRS(0–2) 90 DAYS | 6 | 431/774 (56%) | 933/2285(41%) | 1.78 (1.50–2.11) | 0 | <0.01 |
| SICH | 3 | 28/651 (4%) | 389/2118 (18%) | 0.41 (0.09–1.93) | 91 | 0.26 |
| MORTALITY | 5 | 129/771 (17%) | 610/2457(25%) | 0.62 (0.50–0.76) | 0 | <0.01 |
| mFPE | Non-mFPE | mFPE vs Non-FPE | ||||
| MRS(0–2) 90 DAYS | 7 | 339 / 591 (57%) | 402/ 917 (44%) | 1.73 (1.44–2.1) | 0.00 | <0.01 |
| SICH | 2 | 13 / 245 (5%) | 47 / 670 (7%) | 0.98(0.51 –1.88) | 0.00 | 0.95 |
| MORTALITY | 2 | 40 / 244(16%) | 132 / 634(21%) | 0.98 (0.66–1.49) | 0.00 | 0.95 |
FPE: First pass effect, mFPE: modified first pass effect, non-FPE: non-First pass effect, non-mFPE: non-modified first pass effect, mRS: modified Rankin Score, sICH: symptomatic intracranial hemorrhage.
Figure 3).
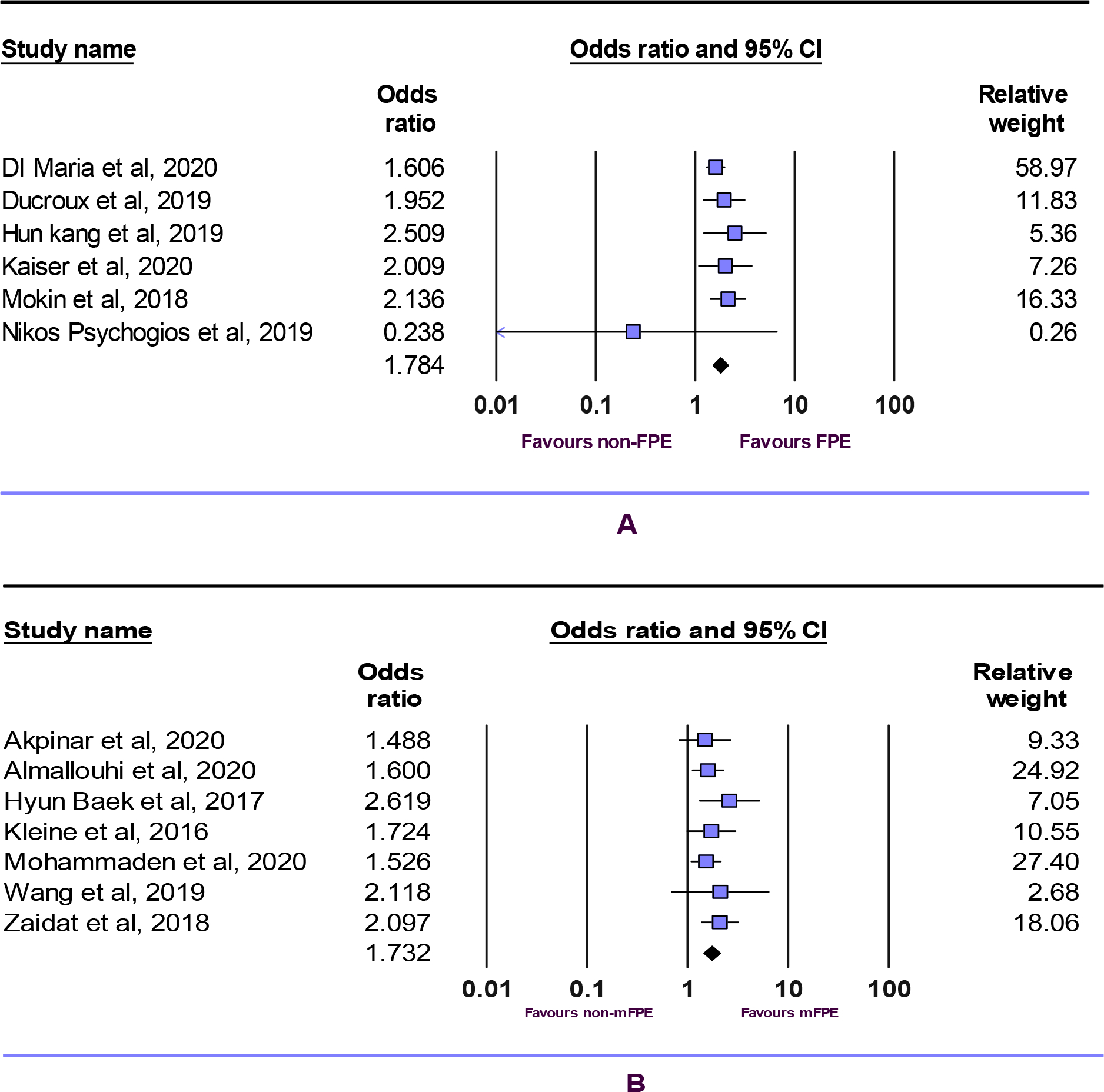
mRS (0–2) 90 days for FPE vs non-FPE (A), mFPE vs non-mFPE (B).
Figure 4).
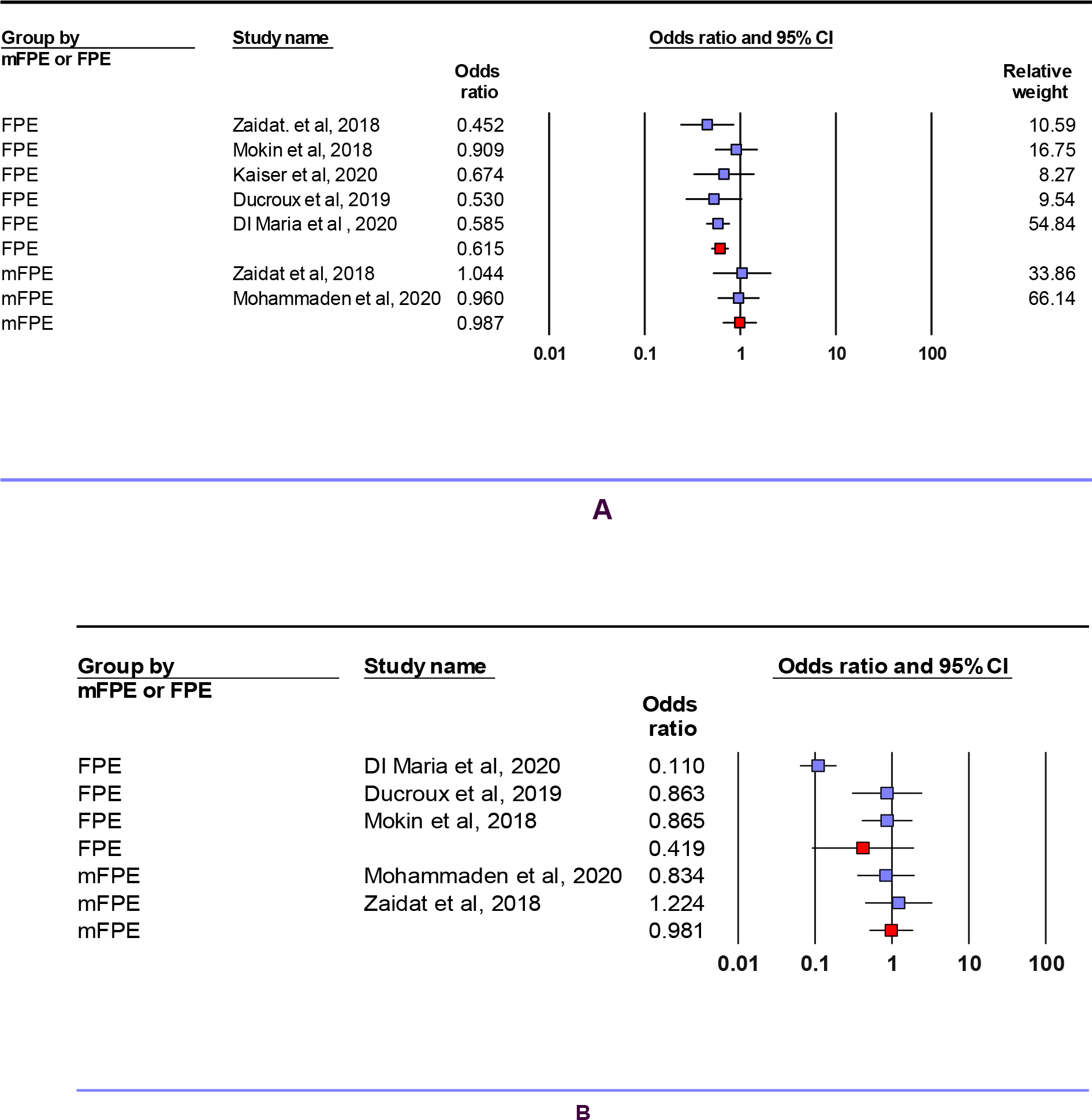
mortality at 90 days (A), sICH (B).
Comparison of mFPE vs recanalized non-mFPE and FPE vs recanalized non-FPE
Patients with FPE had higher rate of mRS 0–2 at 90 days compared with recanalized non-FPE (323/524 [61%] vs 369/714 [51%], OR 1.75, 95% CI 1.37 to 2.25, p<0.01). The rate of mRS 0–2 at 90 days was 53% (387/734) for mFPE group compared with 42% (389/916) for the recanalized non-mFPE group (OR 1.6, 95% CI 1.31 to 1.96, p<0.01; supplementary Figure 1). The rate of sICH was 3.9% (9/233) in the FPE group and 3.8% (15/391) for the recanalized non-FPE group (OR 1.1, 95% CI 0.46 to 2.62, p= .82) and the rate of mortality was 11% (68/577) for the FPE group and 15% (105/681) for the recanalized non-FPE group (OR 0.53, 95% CI 0.37 to 0.75, p<0.01). sICH rate was not different between mFPE and the recanalized non-mFPE group (16/256 [6%] vs 25/316 [8%], OR 0.81, 95% CI 0.42 to 1.56, p= .54). Compared to recanalized non-mFPE group, patients with mFPE had significantly lower mortality (121/1043 [11%] vs 223/1331 [16%], OR 0.55, 95% CI 0.38 to 0.79, p<0.01; ; supplementary Figure 2) (Supplementary Tables 5–7).
Heterogeneity and publication bias
The I2 values were higher than 80% for FPE and mFPE rates, suggesting high heterogeneity. The I2 values were 0% for mRS(0–2) at 90 days indicating low heterogeneity (Table 2). The P-values for publication bias using Egger’s regression were higher than 0.05 for FPE rate, mFPE rate, and clinical outcomes, suggesting no bias.
Discussion
Our meta-analysis demonstrated a number of clinically relevant findings. First, as the literature stands, FPE and mFPE are achieved in only about one third and one-half of patients respectively. Notably, rates of both FPE and mFPE are fairly similar across thrombectomy techniques. Second, regarding clinical outcomes, patients in whom FPE or mFPE was achieved had statistically significant and clinically relevant improvements in the neurologic outcome as compared to those in whom these angiographic outcomes were not achieved. Also, the mortality rate was lower in the FPE group compared to the non-FPE group. Taken together, results of the current meta-analysis indicate that there is substantial room for improvement in the efficacy of all types of thrombectomy techniques with regard to FPE rate. Increasing the likelihood of successful revascularization on the first through development of new MT technique or newer devices would result in better outcomes for patients as FPE is associated with better clinical outcome.
Numerous, previous studies have focused on FPE (3–5, 7, 11, 16, 19, 26, 29, 33, 45, 55, 59–66). In general, rates of FPE and mFPE ranged from 13% to 85%, and 19% to 97% respectively. Furthermore, rates of FPE were noted to influence rates of good neurologic outcome. Zaidat, et al. (4), who introduced FPE as a key metric for the angiographic outcome, reported an FPE rate of 25% for 354 patients who were treated with stent-retriever (Solitaire FR) and they also showed that FPE is a predictor of good neurologic outcome (mRS score ≤2 at 30 days). In another study by Haussen, et al. authors noted a rate of 59% for mFPE (36). Also, in two studies in 2019, greater odds of achieving mRS 0–2 at 90 days were reported for both mFPE and FPE (11, 62). Our results provide clarity regarding the contemporary rates of FPE and mFPE, as well as confirm the strong relationship between FPE and good neurological outcome.
Conversely, results regarding the association of mortality and sICH rate with FPE and mFPE are inconsistent in the literature. In one study by Kang, et al., FPE was associated with higher odds of sICH (65) while five other articles reported lower odds of sICH (4, 7, 16, 60, 62). For mortality rate, only one article showed no correlation of mFPE with mortality rate, (4) whereas other articles mentioned positive correlation with either mFPE or FPE (4, 7, 11, 16, 19, 60–62). Our current study confirmed a lower mortality rate with FPE but not with mFPE, as well as the association between FPE and a reduction in the ‘other complications’ category.
Our study has limitations that need to be taken into consideration when interpreting our findings. First, we did not include assessments of other potential factors that might impact rates of FPE, including Symptom onset to reperfusion, location of occlusion, the size of aspiration catheter lumen(69), adjunctive devices such as balloon guiding catheters, imaging characteristics such as baseline ASPECTS (67), clot perviousness (22), better collateral grade (70), andclot surface phenotypenik(19), Further understanding of factors associated with FPE may influence choice of thrombectomy device and technique Included studies in our meta-analysis may suffer from biases such as ascertainment bias due tonot having core laboratory angiographic outcome adjustment or selection bias due to the retrospective nature of some studies and heterogeneous stroke population.
Conclusion
Our systematic review and meta-analysis demonstrated that patients with FPE or mFPE have better clinical outcomes compared with non-FPE or non-mFPE patients. Additionally, FPE rate is approximately thirty percent overall, and based on the current data available in the literature, existing endovascular techniques (aspiration, stent retriever, and combination) appear closely efficient in achieving successful revascularization on the first pass.
Supplementary Material
Funding:
This work was supported by the National Institutes of Health grant number (R01 NS105853)
Footnotes
Competing interests: None declared.
Patient consent for publication: Not required.
Research Ethics Approval: Not required
Data sharing statement: Data can be made available by contacting the corresponding author via email.
References
- 1.Spiotta AM, Vargas J, Turner R, Chaudry MI, Battenhouse H, Turk AS. The golden hour of stroke intervention: effect of thrombectomy procedural time in acute ischemic stroke on outcome. Journal of NeuroInterventional Surgery. 2014;6(7):511–6. [DOI] [PubMed] [Google Scholar]
- 2.Peretz S, Raphaeli G, Borenstein N, Leker RR, Brauner R, Horev A, et al. Effect of time from onset to endovascular therapy on outcomes: the National Acute Stroke Israeli (NASIS)-REVASC registry. Journal of NeuroInterventional Surgery. 2020;12(1):13–8. [DOI] [PubMed] [Google Scholar]
- 3.Flottmann F, Leischner H, Broocks G, Nawabi J, Bernhardt M, Faizy TD, et al. Recanalization rate per retrieval attempt in mechanical thrombectomy for acute ischemic stroke. Stroke. 2018;49(10):2523–5. [DOI] [PubMed] [Google Scholar]
- 4.Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke. 2018;49(3):660–6. [DOI] [PubMed] [Google Scholar]
- 5.Akpinar CK, Ozdemir AO, Gurkas E, Bilgic AB, Aykac O, Inanc Y, et al. Favorable first-pass recanalization rates with NeVa™ thrombectomy device in acute stroke patients: Initial clinical experience. Interventional Neuroradiology. 2020:1591019920938223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jindal G, Carvalho HDP, Wessell A, Le E, Naragum V, Miller TR, et al. Beyond the first pass: revascularization remains critical in stroke thrombectomy. Journal of neurointerventional surgery. 2019;11(11):1095–9. [DOI] [PubMed] [Google Scholar]
- 7.Mokin M, Primiani CT, Castonguay AC, Nogueira RG, Haussen DC, English JD, et al. First pass effect in patients treated with the Trevo stent-retriever: A TRACK registry study analysis. Frontiers in Neurology. 2020;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled clinical trials. 1986;7(3):177–88. [DOI] [PubMed] [Google Scholar]
- 9.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alawieh A, Chatterjee AR, Vargas J, Chaudry MI, Lena J, Turner R, et al. Lessons learned over more than 500 stroke thrombectomies using ADAPT with increasing aspiration catheter size. Neurosurgery. 2020;86(1):61–70. [DOI] [PubMed] [Google Scholar]
- 11.Anadani M, Alawieh A, Vargas J, Chatterjee AR, Turk A, Spiotta A. First attempt recanalization with ADAPT: rate, predictors, and outcome. Journal of NeuroInterventional Surgery. 2019;11(7):641–5. [DOI] [PubMed] [Google Scholar]
- 12.Baharvahdat H, Ooi YC, Khatibi K, Mejia LLP, Kaneko N, Nour M, et al. Increased Rate of Successful First Passage Recanalization During Mechanical Thrombectomy for M2 Occlusion. World neurosurgery. 2020;139:e792–e9. [DOI] [PubMed] [Google Scholar]
- 13.Bernava G, Rosi A, Boto J, Brina O, Kulcsar Z, Czarnetzki C, et al. Direct thromboaspiration efficacy for mechanical thrombectomy is related to the angle of interaction between the aspiration catheter and the clot. Journal of NeuroInterventional Surgery. 2020;12(4):396–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chivot C, Renier J, Deramond H, Bouzerar R, Yzet T. Direct aspiration for thrombectomy in ischemic stroke: Impact of dwell time. Interventional Neuroradiology. 2020;26(2):211–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colby GP, Baharvahdat H, Mowla A, Young R, Shwe Y, Jahan R, et al. Increased success of single-pass large vessel recanalization using a combined stentriever and aspiration technique: a single institution study. World neurosurgery. 2019;123:e747–e52. [DOI] [PubMed] [Google Scholar]
- 16.Ducroux C, Piotin M, Gory B, Labreuche J, Blanc R, Maacha MB, et al. First pass effect with contact aspiration and stent retrievers in the Aspiration versus Stent Retriever (ASTER) trial. Journal of neurointerventional surgery. 2020;12(4):386–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gross BA, Jadhav AP, Jovin TG, Jankowitz BT. Clinical Comparison of New Generation 0.071-inch and 0.072-inch Aspiration Catheters. World Neurosurgery. 2019;130:e463–e6. [DOI] [PubMed] [Google Scholar]
- 18.Hesse AC, Behme D, Kemmling A, Zapf A, Hokamp NG, Frischmuth I, et al. Comparing different thrombectomy techniques in five large-volume centers: a ‘real world’observational study. Journal of neurointerventional surgery. 2018;10(6):525–9. [DOI] [PubMed] [Google Scholar]
- 19.Kaiser D, Laske K, Winzer R, Hädrich K, Wahl H, Krukowski P, et al. Impact of thrombus surface on first pass reperfusion in contact aspiration and stent retriever thrombectomy. Journal of NeuroInterventional Surgery. 2020. [DOI] [PubMed] [Google Scholar]
- 20.Kowoll A, Weber A, Mpotsaris A, Behme D, Weber W. Direct aspiration first pass technique for the treatment of acute ischemic stroke: initial experience at a European stroke center. Journal of neurointerventional surgery. 2016;8(3):230–4. [DOI] [PubMed] [Google Scholar]
- 21.Marnat G, Barreau X, Detraz L, Bourcier R, Gory B, Sgreccia A, et al. First-line Sofia aspiration thrombectomy approach within the endovascular treatment of ischemic stroke multicentric registry: efficacy, safety, and predictive factors of success. American Journal of Neuroradiology. 2019;40(6):1006–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mokin M, Waqas M, Fifi J, De Leacy R, Fiorella D, Levy EI, et al. Clot perviousness is associated with first pass success of aspiration thrombectomy in the COMPASS trial. Journal of NeuroInterventional Surgery. 2020:neurintsurg-2020–016434. [DOI] [PubMed] [Google Scholar]
- 23.Raymond SB, Nasir-Moin M, Koch MJ, Rabinov JD, Leslie-Mazwi T, Patel AB. Initial experience with React 68 aspiration catheter. Interventional Neuroradiology. 2020;26(3):358–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Romano DG, Frauenfelder G, Casseri T, Piano M, Vinci S, Comai A, et al. Efficacy of ADAPT with large-bore reperfusion catheter in anterior circulation acute ischemic stroke: a multicentric Italian experience. La radiologia medica. 2020;125(1):57–65. [DOI] [PubMed] [Google Scholar]
- 25.Schramm P, Navia P, Papa R, Zamarro J, Tomasello A, Weber W, et al. ADAPT technique with ACE68 and ACE64 reperfusion catheters in ischemic stroke treatment: results from the PROMISE study. Journal of neurointerventional surgery. 2019;11(3):226–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Srivatsa S, Duan Y, Sheppard JP, Pahwa S, Pace J, Zhou X, et al. Cerebral vessel anatomy as a predictor of first-pass effect in mechanical thrombectomy for emergent large-vessel occlusion. Journal of Neurosurgery. 2020;1(aop):1–9. [DOI] [PubMed] [Google Scholar]
- 27.Tomasello A, Ribò M, Gramegna LL, Melendez F, Rosati S, Moreu M, et al. Procedural approaches and angiographic signs predicting first-pass recanalization in patients treated with mechanical thrombectomy for acute ischaemic stroke. Interventional Neuroradiology. 2019;25(5):491–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turk AS III, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. The Lancet. 2019;393(10175):998–1008. [DOI] [PubMed] [Google Scholar]
- 29.Wang D, Shu H, Meng Y, Zhang H, Wang H, He S. Factors Promoting Futile Recanalization After Stent Retriever Thrombectomy for Stroke Affecting the Anterior Circulation: A Retrospective Analysis. World Neurosurgery. 2020;133:e576–e82. [DOI] [PubMed] [Google Scholar]
- 30.Xing PF, Yang PF, Li ZF, Zhang L, Shen HJ, Zhang YX, et al. Comparison of Aspiration versus Stent Retriever Thrombectomy as the Preferred Strategy for Patients with Acute Terminal Internal Carotid Artery Occlusion: A Propensity Score Matching Analysis. American Journal of Neuroradiology. 2020;41(3):469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ye G, Cao R, Lu J, Qi P, Chen J, Wang D. Association between thrombus density and reperfusion outcomes using different thrombectomy strategies: a single-center study and meta-analysis. Frontiers in Neurology. 2019;10:843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim Y-W, Hwang Y-H, Kim Y-S, Kang D-H. Frontline contact aspiration thrombectomy using SOFIA catheter for acute ischemic stroke: period-to-period comparison with Penumbra catheter. Acta Neurochirurgica. 2019;161(6):1197–204. [DOI] [PubMed] [Google Scholar]
- 33.Almandoz JED, Kayan Y, Wallace AN, Tarrel RM, Fease JL, Scholz JM, et al. Larger ACE 68 aspiration catheter increases first-pass efficacy of ADAPT technique. Journal of NeuroInterventional Surgery. 2019;11(2):141–6. [DOI] [PubMed] [Google Scholar]
- 34.Tonetti DA, Desai SM, Casillo S, Zussman BM, Brown MW, Jadhav AP, et al. Large-bore aspiration catheter selection does not influence reperfusion or outcome after manual aspiration thrombectomy. Journal of NeuroInterventional Surgery. 2019;11(7):637–40. [DOI] [PubMed] [Google Scholar]
- 35.Kara B, Selcuk HH, Salik AE, Zalov H, Yildiz O, Gul G, et al. Single-center experience with the Tigertriever device for the recanalization of large vessel occlusions in acute ischemic stroke. Journal of neurointerventional surgery. 2019;11(5):455–9. [DOI] [PubMed] [Google Scholar]
- 36.Haussen DC, Al-Bayati AR, Grossberg JA, Bouslama M, Barreira C, Bianchi N, et al. Longer stent retrievers enhance thrombectomy performance in acute stroke. Journal of NeuroInterventional Surgery. 2019;11(1):6–8. [DOI] [PubMed] [Google Scholar]
- 37.Bai Y, Pu J, Wang H, Yang D, Hao Y, Xu H, et al. Impact of Retriever Passes on Efficacy and Safety Outcomes of Acute Ischemic Stroke Treated with Mechanical Thrombectomy. Cardiovascular and interventional radiology. 2018;41(12):1909–16. [DOI] [PubMed] [Google Scholar]
- 38.Clarençon F, Baronnet F, Shotar E, Degos V, Rolla-Bigliani C, Bartolini B, et al. Should posterior cerebral artery occlusions be recanalized? Insights from the Trevo Registry. European Journal of Neurology. 2020;27(5):787–92. [DOI] [PubMed] [Google Scholar]
- 39.Kammerer S, de Rochemont RdM, Wagner M, You S-J, Tritt S, Mueller-Eschner M, et al. Efficacy of mechanical thrombectomy using stent retriever and balloon-guiding catheter. Cardiovascular and interventional radiology. 2018;41(5):699–705. [DOI] [PubMed] [Google Scholar]
- 40.Kannath SK, Rajan JE, Sylaja P, Sarma PS, Sukumaran S, Sreedharan SE, et al. Dwell time of stentriever influences complete revascularization and first-pass TICI 3 revascularization in acute large vessel occlusive stroke. World neurosurgery. 2018;110:169–73. [DOI] [PubMed] [Google Scholar]
- 41.Kim SH, Choi JH, Kang MJ, Cha JK, Kim DH, Nah HW, et al. Efficacy of Combining Proximal Balloon Guiding Catheter and Distal Access Catheter in Thrombectomy with Stent Retriever for Anterior Circulation Ischemic Stroke. Journal of Korean Neurosurgical Society. 2019;62(4):405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Z-S, Deng G, Zhou L-J, Sun Y, Zhang X-J, Kuang X-W, et al. Comparison of Micro-Clamping Stent-Retriever Thrombectomy with Conventional Stent-Retriever Thrombectomy in Intracranial Large Vessel Embolism. World Neurosurgery. 2018;116:e662–e9. [DOI] [PubMed] [Google Scholar]
- 43.Loh Y, Jahan R, McArthur D, Shi Z-S, Gonzalez N, Duckwiler G, et al. Recanalization rates decrease with increasing thrombectomy attempts. American Journal of Neuroradiology. 2010;31(5):935–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nguyen TN, Castonguay AC, Nogueira RG, Haussen DC, English JD, Satti SR, et al. Effect of balloon guide catheter on clinical outcomes and reperfusion in Trevo thrombectomy. Journal of NeuroInterventional Surgery. 2019;11(9):861. [DOI] [PubMed] [Google Scholar]
- 45.Psychogios M-N, Tsogkas I, Brehm A, Hesse A, McTaggart R, Goyal M, et al. Clot reduction prior to embolectomy: mSAVE as a first-line technique for large clots. PloS one. 2019;14(5):e0216258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seker F, Pfaff J, Wolf M, Ringleb PA, Nagel S, Schönenberger S, et al. Correlation of Thrombectomy Maneuver Count with Recanalization Success and Clinical Outcome in Patients with Ischemic Stroke. American Journal of Neuroradiology. 2017;38(7):1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Teleb MS. Endovascular Acute Ischemic Stroke Treatment with FlowGate Balloon Guide Catheter: A Single-Center Observational Study of FlowGate Balloon Guide Catheter Use. Interventional Neurology. 2018;7(6):327–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wong JHY, Do HM, Telischak NA, Moraff AM, Dodd RL, Marks MP, et al. Initial experience with SOFIA as an intermediate catheter in mechanical thrombectomy for acute ischemic stroke. Journal of NeuroInterventional Surgery. 2017;9(11):1103. [DOI] [PubMed] [Google Scholar]
- 49.Ye G, Gao Q, Qi P, Wang J, Hu S, Chen K, et al. The role of diabetes mellitus on the thrombus composition in patients with acute ischemic stroke. Interventional Neuroradiology. 2020;26(3):329–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zaidat OO, Bozorgchami H, Ribó M, Saver JL, Mattle HP, Chapot R, et al. Primary results of the multicenter ARISE II study (Analysis of Revascularization in Ischemic Stroke With EmboTrap). Stroke. 2018;49(5):1107–15. [DOI] [PubMed] [Google Scholar]
- 51.Zaidat OO, Haussen DC, Hassan AE, Jadhav AP, Mehta BP, Mokin M, et al. Impact of stent retriever size on clinical and angiographic outcomes in the STRATIS stroke thrombectomy registry. Stroke. 2019;50(2):441–7. [DOI] [PubMed] [Google Scholar]
- 52.Tekle WG, Hassan AE, Jadhav AP, Haussen DC, Budzik RF, Bonafe A, et al. Impact of Periprocedural and Technical Factors and Patient Characteristics on Revascularization and Outcome in the DAWN Trial. Stroke. 2020;51(1):247–53. [DOI] [PubMed] [Google Scholar]
- 53.Baek J-H, Kim BM, Heo JH, Nam HS, Kim YD, Park H, et al. Number of stent retriever passes associated with futile recanalization in acute stroke. Stroke. 2018;49(9):2088–95. [DOI] [PubMed] [Google Scholar]
- 54.Maus V, Behme D, Kabbasch C, Borggrefe J, Tsogkas I, Nikoubashman O, et al. Maximizing first-pass complete reperfusion with SAVE. Clinical neuroradiology. 2018;28(3):327–38. [DOI] [PubMed] [Google Scholar]
- 55.Kim SH, Lee H, Kim SB, Kim ST, Baek JW, Heo YJ, et al. Hybrid mechanical thrombectomy for acute ischemic stroke using an intermediate aspiration catheter and Trevo stent simultaneously. Journal of Clinical Neuroscience. 2020. [DOI] [PubMed] [Google Scholar]
- 56.Gonzalez AV, Goerlich D, Buerke B, Muennich N, Sauerland C, Rusche T, et al. Predictors of Successful First-Pass Thrombectomy with a Balloon Guide Catheter: Results of a Decision Tree Analysis. Translational Stroke Research. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Almallouhi E, Al Kasab S, Alawieh A, Chalhoub RM, Anadani M, Arthur A, et al. Abstract WP3: Predictors and Outcomes of Successful First Pass in Neurothrombectomy-Insights From the STAR Collaboration. Stroke. 2020;51(Suppl_1):AWP3–AWP. [Google Scholar]
- 58.Handshoe LS, Mulpur B, Andrapalliyal N, Uchino K, Hussain M. Abstract WP7: Early Neurological Improvement With First Pass Effect is More Common in Early Window Endovascular Intervention for Emergent Large Vessel Occlusion. Stroke. 2020;51(Suppl_1):AWP7–AWP. [Google Scholar]
- 59.Kleine JF, Wunderlich S, Zimmer C, Kaesmacher J. Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. Journal of neurointerventional surgery. 2017;9(2):117–21. [DOI] [PubMed] [Google Scholar]
- 60.Mohammaden M, Pisani L, Perry da Camara C, Bousalma M, Al bayati A, Haussen DC, et al. Abstract WP502: Predictors Of First Pass Reperfusion In Anterior Circulation Large Vessel Occlusion Stroke. Stroke. 2020;51(Suppl_1):AWP502–AWP. [Google Scholar]
- 61.Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, et al. True first-pass effect: first-pass complete reperfusion improves clinical outcome in thrombectomy stroke patients. Stroke. 2019;50(8):2140–6. [DOI] [PubMed] [Google Scholar]
- 62.García-Tornel Á, Requena M, Rubiera M, Muchada M, Pagola J, Rodriguez-Luna D, et al. When to Stop: Detrimental Effect of Device Passes in Acute Ischemic Stroke Secondary to Large Vessel Occlusion. Stroke. 2019;50(7):1781–8. [DOI] [PubMed] [Google Scholar]
- 63.Di Maria F, Kyheng M, Consoli A, Desilles J-P, Gory B, Richard S, et al. Identifying the predictors of first-pass effect and its influence on clinical outcome in the setting of endovascular thrombectomy for acute ischemic stroke: Results from a multicentric prospective registry. International Journal of Stroke. 2020:1747493020923051. [DOI] [PubMed] [Google Scholar]
- 64.Wessell A, Carvalho H, Le E, Cannarsa G, Kole M, Stokum J, et al. A Critical Assessment of the Golden Hour and the Impact of Procedural Timing in Stroke Thrombectomy. American Journal of Neuroradiology. 2020;41(5):822–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kang D-H, Kim BM, Heo JH, Nam HS, Kim YD, Hwang YH, et al. Effects of first pass recanalization on outcomes of contact aspiration thrombectomy. Journal of NeuroInterventional Surgery. 2020;12(5):466–70. [DOI] [PubMed] [Google Scholar]
- 66.Baek J-H, Yoo J, Song D, Kim YD, Nam HS, Kim BM, et al. Predictive value of thrombus volume for recanalization in stent retriever thrombectomy. Scientific reports. 2017;7(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mohammaden MH, Haussen DC, Pisani L, Al-Bayati AR, da Camara CP, Bhatt N, et al. Baseline ASPECTS and hypoperfusion intensity ratio influence the impact of first pass reperfusion on functional outcomes. Journal of NeuroInterventional Surgery. 2020. [DOI] [PubMed] [Google Scholar]
- 68.Drouard-de Rousiers E, Lucas L, Richard S, Consoli A, Mazighi M, Labreuche J, et al. Impact of Reperfusion for Nonagenarians Treated by Mechanical Thrombectomy: Insights From the ETIS Registry. Stroke. 2019;50(11):3164–9. [DOI] [PubMed] [Google Scholar]
- 69.Fitzgerald S, Ryan D, Mullins L, Thornton J, Nogueira R. E-018 A novel 8fr aspiration catheter significantly increases the first pass effect in comparison with industry standard 6fr devices in an in-vitro human vasculature model. British Medical Journal Publishing Group; 2020. [Google Scholar]
- 70.Jadhav A, Zaidat O, Desai S, Nogueira R, Mueller-Kronast N, Jovin T, et al. O-001 Predictors of the first pass effect with neurothrombectomy for acute ischemic stroke. Journal of NeuroInterventional Surgery. 2019;11(Suppl 1):A1–A. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


