Abstract
Purpose
To investigate the impact of arthroscopic shoulder labral repair without shoulder instability on career longevity, game use, and performance in National Hockey League (NHL) athletes.
Methods
A retrospective review of all NHL players who underwent arthroscopic shoulder labral repair from 2004 to 2020 was performed. A 2:1 matched control group was used for comparison. Controls were matched by age, body mass index, position, and experience prior to the index year. Demographic characteristics, game use, and performance metrics were collected for all athletes. Statistical analysis examined game use and performance both at 1-year and 3-year follow-up compared with one season before injury.
Results
Twenty-nine players who underwent arthroscopic shoulder labral surgery returned to play (100%) and were matched with 55 control players. The operative cohort experienced shorter careers compared with controls (4.4 ± 3.1 vs 6.0 ± 3.6 seasons, P < .05). After one season, injured players experienced significant reductions in goals per 60 (0.6 ± 0.4 vs 0.8 ± 0.5, P = .013), points per 60 (1.5 ± 0.9 vs 2.0 ± 0.9, P = .001), and shooting percentage, (8.5 ± 5.8 vs 10.5 ± 5.2, P = .02) compared with the year prior. The reduction in goals (0.6 ± 0.4 vs 0.8 ± 0.5, P = .01) and shooting % (8.5 ± 4.7 vs 10.5 ± 5.2, P = .04) persisted at 3 years. Compared with controls, the surgical group experienced significant reductions at one season postindex in percentage of goals, assists, points per 60, and shooting percentage. Only the reduction in goals per 60 persisted at 3 seasons postindex.
Conclusions
Following return to play after arthroscopic shoulder labral repair, NHL players demonstrated reduced career longevity compared with healthy controls. Players exhibited significant reductions in game use and performance at one season after injury but returned closer to baseline after 3 seasons.
Level of Evidence
Level III; retrospective case control.
Ice hockey players have an elevated risk for upper-extremity injuries due to frequent contact and collisions.1, 2, 3, 4, 5 Shoulder injuries are among the most common upper extremity injuries among hockey players6 and comprise 10% to 12% of injuries in National Hockey League (NHL) players.7 These shoulder pathologies consist of acromioclavicular joint sprains, subluxations, dislocations, rotator cuff tears, and glenoid labral tears. Compared with recreational athletes, professional hockey players endure greater physical demands and are increasingly interested in returning to play quickly while also performing at an elite level. Shoulder injuries are not only physically debilitating for NHL players, but they also present a significant financial impact to the player. Donaldson et al.8 estimated that shoulder injuries in the NHL had one of the greatest mean costs in terms of salary lost per games missed. For those with symptomatic glenoid labral tears, these tears are debilitating to performance, and arthroscopic shoulder labral repair may facilitate faster return to the ice compared with nonoperative treatment.
Multiple studies have reported successful, sport-dependent return to play (RTP) after arthroscopic surgery for shoulder instability and labral tears in elite athletes.9, 10, 11, 12, 13, 14 Competitive ice hockey requires a dynamic range of motion and function of the shoulder for a variety of activities, including passing the puck, shooting, and giving or receiving hits. Swindell et al.15 examined a group of NHL players with shoulder instability and found that nonoperatively treated players experienced a significant reduction in points per game (P = .034) compared with those treated with operative stabilization. Conservatively managed players were more likely to have a recurrent shoulder instability event (14.3% vs 0% for conservative vs operative, respectively), ultimately leading to more games missed. These shoulder injuries in the NHL may be detrimental to performance and negatively impact participation. More information on these injuries may assist physicians in counseling NHL players about the timeline of rehabilitation as well as expected changes in career performance after surgery.
While few studies exist examining performance and career longevity after shoulder instability in NHL players, there is an even greater deficiency of studies specifically investigating arthroscopic shoulder labral repair outcomes.15, 16, 17, 18 The purpose of our study was to investigate the impact of arthroscopic shoulder labral repair without shoulder instability on career longevity, game use, and performance of NHL athletes. We hypothesized that NHL players who sustained shoulder labral tears and underwent arthroscopic repair would have reduced career longevity and performance.
Methods
A retrospective review of all NHL athletes who underwent arthroscopic labrum repair from 2004 to 2020 was conducted. Individual player medical records were not available; therefore, consistent with previous literature, a public internet search using www.hockey-reference.com and www.nhl.com along with various news, team, and official NHL websites was performed.13,18, 19, 20, 21 All players identified were cross-referenced with a minimum of 2 sources to ensure accuracy of the injury and the date of surgery. Game statistics were evaluated to confirm missing data following surgical management. Players were excluded if the injury occurred outside of NHL participation, if they had a history of previous surgical management on the operative shoulder, had a history of ipsilateral shoulder instability, had a shoulder labrum debridement rather than a repair at the time of surgery, or if the player experienced concomitant injuries within 2 years before or after the index year.
The entire NHL season in which the surgery occurred, including the pre- and postseason, constituted the index year. If the injury occurred in the offseason and no game play was missed, the offseason was deemed as the index season. Player demographics, game use, and performance metrics were collected for 3 seasons before and after index injury. Player demographics (age, weight, body mass index [BMI], position, debut date, date of surgery, age at surgery, months until RTP) game use (seasons after RTP, games played per season, time on ice, average time on ice), and performance metrics (shots, goals, assists, points, goals per 60 games, assists per 60 games, points per 60 games, shooting percentage, Corsi percentage, Fenwick percentage, and shooting plus save percentage) were collected.
A 2:1 matched control cohort was created for comparison. Players were matched by age, position played, a BMI ±5, and ±2 years of experience before the surgery. The control index season was selected so that the player age and seasons of experience were similar between controls and those undergoing surgery. The index season for the healthy controls was matched within 5 years of the study group players’ index season. Comparisons between the surgical and matched control groups were performed for game use and performance metrics at 1-year postindex and 3 years postindex compared with 1 season preindex. Of note, 2 players did not have sufficient follow-up at 3 seasons postindex due to the recency of their surgery. In addition, relative baseline percentage of all metrics were calculated by dividing postindex season 1 or 3 by baseline preindex season 1. These relative percentages were used to compare short-term and long-term changes between operative and control players.
Statistical Analysis
All analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC). Categorical data are represented as percentages and counts; continuous data are represented as mean ± standard deviation. To evaluate categorical data, 2-group univariate comparisons were performed using the χ2 test for values greater than 5 and Fisher exact tests for values less than 5. Continuous variables were analyzed using 2-sample t-tests for normally distributed variables and Wilcoxon rank sum tests for non-normally distributed variables. Pre- and Post-data comparisons were performed using paired t tests when normally distributed. Differences were calculated as (post-pre). The association between time and RTP was calculated using Pearson correlation coefficient tests.
Results
Demographics and Return to Sport
All 29 of 29 (100%) NHL players who underwent arthroscopic shoulder surgery for labral tears successfully returned to sport. Of the 29 who underwent surgery, 16 players had surgery toward the end of the season in the months of April, May, or June. Table 1 contains the demographic comparison between the NHL players who underwent arthroscopic shoulder surgery and their healthy matched controls. These groups exhibited no difference in age (26 ± 3.9 vs 26.3 ± 3.6; P = .96) and position (6 centers, 6 defenseman, and 17 wings in the operative group, whereas the control group consisted of 12 centers, 10 defenseman, and 33 wings; P = .961). While groups significantly differed in BMI (P = .001), no differences were found in height (72.6 ± 2.3 vs 73.3 ± 2.0; P = .14) or weight (201.2 ± 20.2 vs 203.2 ± 21.3; P = .676) (Table 1). Following arthroscopic shoulder labral surgery, NHL players experienced a significant reduction in total seasons played (4.4 ± 3.1 vs 6.0 ± 3.6 seasons; P < .05) (Table 1).
Table 1.
Demographic Characteristics of NHL Players who Underwent Arthroscopic Labral Repair Versus Matched Controls
| Response | Labrum (N = 29) | Control (N = 55) | P Value |
|---|---|---|---|
| Age | 26.7 ± 3.9 | 26.3 ± 3.6 | .96 |
| Height | 72.6 ± 2.3 | 73.3 ± 2.0 | .14 |
| Weight | 201.2 ± 20.2 | 203.2 ± 21.3 | .676 |
| BMI | 26.8 ± 1.6 | 24.9 ± 1.7 | .001 |
| Position | |||
| C | 6 (21%) | 12 (22%) | .961 |
| D | 6 (21%) | 10 (18%) | |
| W | 17 (59%) | 33 (60%) | |
| Handedness | |||
| Left | 15 (63%) | 19 (35%) | |
| Right | 9 (38%) | 36 (65%) | |
| RTP rate | 100% | 100% | |
| Seasons after RTP | 4.4 ± 3.1 | 6.0 ± 3.6 | <.05 |
NOTE. Age represented by years; height represented in inches; weight represented in pounds; seasons represented in years. Significant values are noted in bold, P ≤ .05.
BMI, body mass index; C, center; D, defenseman; NHL, National Hockey League; RTP, return to play; W, wing.
Acute Player Game Use and Performance: One-Year Pre-/Postindex Player Comparisons
Mean player game use and performance metrics pre- and postindex are illustrated in Table 2. In the first year of RTP, players who underwent arthroscopic shoulder labral surgery exhibited significant reductions in goals per 60 (0.6 ± 0.4 vs 0.8 ± 0.5; P = .013), points per 60 (1.5 ± 0.9 vs 2.0 ± 0.9, P = .001), and shooting percentage (8.5 ± 5.8 vs 10.5 ± 5.2, P = .02) compared with 1 season before injury. No significant differences were found for game use (games played [GP], time-on-ice [TOI]/GP), assists per 60, or advanced performance metrics (Corsi percentage, Fenwick percentage, and shooting plus save percentage) (Table 2).
Table 2.
Game Use and Performance One Year Before and After Labral Repair
| Time Point | Labrum (n = 29) | Control (n = 55) | |
|---|---|---|---|
| GP | Pre | 66.2 ± 20.9 | 62.1 ± 22.7 |
| Post | 56.6 ± 23.8 | 64.0 ± 25.9 | |
| P value | .36 | .51 | |
| TOI/GP | Pre | 16.5 ± 4.6 | 16.0 ± 4.3 |
| Post | 15.8 ± 4.7 | 16.5 ± 3.9 | |
| P value | .187 | .48 | |
| Goals per 60 | Pre | 0.8 ± 0.5 | 0.2 ± 0.2 |
| Post | 0.6 ± 0.4 | 0.2 ± 0.2 | |
| P value | .013 | .97 | |
| Assists per 60 | Pre | 1.1 ± 0.6 | 0.3 ± 0.2 |
| Post | 0.9 ± 0.5 | 0.3 ± 0.2 | |
| P value | .11 | .49 | |
| Points per 60 | Pre | 2.0 ± 0.9 | 0.5 ± 0.4 |
| Post | 1.5 ± 0.9 | 1.6 ± 7.8 | |
| P value | .001 | .65 | |
| Shooting percentage | Pre | 10.5 ± 5.2 | 9.6 ± 4.3 |
| Post | 8.5 ± 5.8 | 10.2 ± 5.9 | |
| P value | .02 | .74 | |
| Corsi percentage | Pre | 49.4 ± 3.9 | 49.9 ± 4.5 |
| Post | 49.6 ± 3.7 | 51.2 ± 4.3 | |
| P value | .68 | .09 | |
| Fenwick percentage | Pre | 49.5 ± 3.8 | 50.0 ± 4.2 |
| Post | 49.7 ± 3.8 | 51.1 ± 4.0 | |
| P value | .7 | .15 | |
| PDO | Pre | 99.9 ± 3.8 | 100.5 ± 4.8 |
| Post | 98.9 ± 3.8 | 100.5 ± 3.3 | |
| P value | .51 | .71 |
NOTE. Continuous variables are presented using adjusted mean ± standard error.
Significant P values (<.05) are indicated by bold text.
P values compare pre- vs post-values within the same group.
assists per 60, assists per 60 minutes; goals per 60, goals per 60 minutes; GP, games played; PDO, shooting plus save percentage; points per 60, points per 60 minutes; TOI/GP, time on ice per games played.
Long-Term Player Game Use and Performance: One-Year Pre-/Three-Year Postindex Player Comparisons
When we analyzed game use and performance at 3 seasons postindex compared with season 1 preindex, players who underwent surgery experienced significant reductions in TOI/GP (15.8 ± 3.7 vs 16.5 ± 4.6, P = .04), goals per 60 (0.6 ± 0.4 vs 0.8 ± 0.5, P = .01), and shooting percentage (8.5 ± 4.7 vs 10.5 ± 5.2, P = .01). However, assists per 60 (1.0 ± 0.5 vs 1.1 ± 0.6, P = .12) and points per 60 (1.7 ± 0.8 vs 2.0 ± 0.9, P = .18) were no longer significantly different at 3 seasons postindex. Two players were not included in analysis at 3 seasons postindex due to the recency of surgery (Table 3).
Table 3.
Game Use and Performance One Year Before and Three Years After Labral Repair
| Time Point | Labrum (n = 27) | Control (n = 55) | |
|---|---|---|---|
| GP | Pre | 66.2 ± 20.9 | 62.1 ± 22.7 |
| Post | 55.3 ± 25.6 | 64.6 ± 20.4 | |
| P value | .07 | .53 | |
| TOI/GP | Pre | 16.5 ± 4.6 | 16.0 ± 4.3 |
| Post | 15.8 ± 3.7 | 16.5 ± 3.6 | |
| P value | .04 | .79 | |
| Goals per 60 | Pre | 0.8 ± 0.5 | 0.2 ± 0.2 |
| Post | 0.6 ± 0.4 | 0.2 ± 0.2 | |
| P value | .01 | .58 | |
| Assists per 60 | Pre | 1.1 ± 0.6 | 0.3 ± 0.2 |
| Post | 1.0 ± 0.5 | 0.3 ± 0.2 | |
| P value | .12 | .76 | |
| Points per 60 | Pre | 2.0 ± 0.9 | 0.5 ± 0.4 |
| Post | 1.7 ± 0.8 | 0.6 ± 0.4 | |
| P value | .18 | .66 | |
| Shooting percentage 1 y preindex | Pre | 10.5 ± 5.2 | 9.6 ± 4.3 |
| Post | 8.5 ± 4.7 | 9.2 ± 5.2 | |
| P value | .04 | .2 | |
| Corsi percentage | Pre | 49.4 ± 3.9 | 49.9 ± 4.5 |
| Post | 49.4 ± 3.7 | 51.7 ± 3.6 | |
| P value | .81 | .28 | |
| Fenwick percentage | Pre | 49.5 ± 3.8 | 50.0 ± 4.2 |
| Post | 49.2 ± 4.7 | 51.3 ± 4.0 | |
| P value | .96 | .5 | |
| PDO | Pre | 99.9 ± 3.8 | 100.5 ± 4.8 |
| Post | 100.0 ± 2.4 | 99.8 ± 3.0 | |
| P value | .72 | .11 |
NOTE. Continuous variables are presented using adjusted mean ± standard error.
P values with significance (≤.05) are indicated by bold text
P values compare pre vs post values within the same group.
assists per 60, assists per 60 minutes; goals per 60, goals per 60 minutes; GP, games played; PDO, shooting plus save percentage; points per 60, points per 60 minutes; TOI/GP, time on ice per games played.
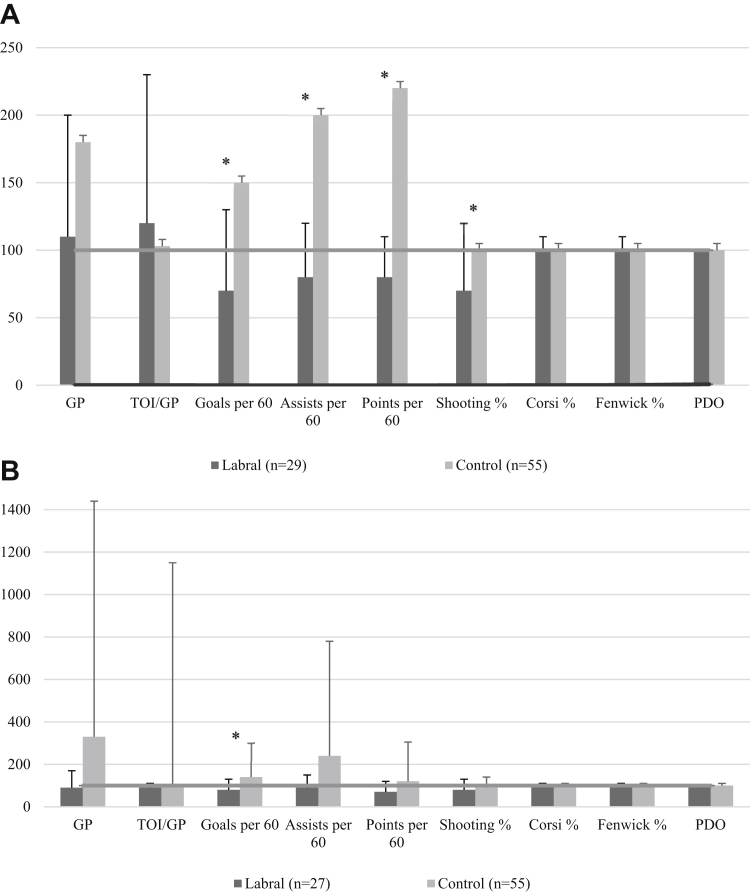
Relative Game Use and Performance: Percentage of Baseline Comparison (Operative Cohort Versus Controls)
The percentage of baseline game use and performance comparisons between operative and control players appears in Figure 1. At 1 season postindex, NHL athletes who underwent surgery demonstrated significant performance deteriorations with reduced goals per 60 (70 ± 60 vs 150 ± 170, P = .01), assists per 60 (80 ± 40 vs 200 ± 300, P = .02), points per 60 (80 ± 30 vs 220 ± 490, P < .05), and shooting percentage (70 ± 50 vs 100 ± 60, P = .04) compared with matched controls (Fig 1A). At 3 seasons postindex, the shoulder surgery group only sustained reductions in goals per 60 (80 ± 50 vs 140 ± 160, P = .03) compared with matched controls (Fig 1B).
Fig 1.
Relative percentage of game use and performance (A) 1 season and (B) 3 seasons following RTP from arthroscopic shoulder labral repair. Preindex baseline is represented by the horizontal line (100%) across all variables. Relative percentages below this line indicate that the postindex variable was less than baseline. ∗P ≤ .05: indicates significant differences between labral repair and control groups (assists per 60, assists per 60 minutes; goals per 60, goals per 60 minutes; GP, games played; PDO, shooting plus save percentage; points per 60, points per 60 minutes; RTP, return to play; TOI/GP, time on ice per games played.)
Discussion
The present study demonstrated that after arthroscopic shoulder labrum repair, 100% of NHL players successfully RTP; however, athletes participated in fewer seasons after injury compared with matched controls (4.4 ± 3.1 vs 6.0 ± 3.6 seasons; P < .05). NHL athletes experienced significant reductions in performance at 1 and 3 seasons postindex. Compared with matched controls, these players performed significantly worse at 1 season postindex with fewer goals, assists, points, and shooting percentage but only had a reduction in goals at 3 seasons postindex. These findings suggest that NHL players are significantly impacted by arthroscopic shoulder labrum repair in the acute setting but ultimately return closer to their baseline in the long term. However, career longevity appears to be reduced after surgery.
Several studies have shown successful RTP in elite athletes, after various arthroscopic shoulder procedures,9,11, 12, 13, 14 ranging from 70% to 100% depending on the sport. Few studies, however, explicitly focus on shoulder injuries in NHL athletes. Rangavajjula et al.22 retrospectively reviewed a cohort of 11 NHL players returning to play after arthroscopic labral repairs with an average follow-up of 19.4 months. On average, players RTP after 4.3 months and remain largely unaffected with no statistically significant differences in TOI or shots on goal per GP. Conclusions from their study were limited due to the small sample size, minimal performance variables, and absence of a control group. Lubbe et al.16 sought to compare RTP and performance outcomes between multiple upper- and lower-body injuries in NHL athletes. Among the 16 players who underwent shoulder instability surgery, 87.5% had RTP and no differences in GP or performance were found at seasons 1 and combined seasons 2/3 after surgery. For those 42 athletes undergoing shoulder arthroscopy for “noninstability” pathology, 95.2% had RTP and experienced significant reductions in games played at seasons 1 and 2/3 after surgery and a decline in performance only at season 1 but returned to baseline at seasons 2/3. Similar to previous results, our study found that NHL athletes suffer a drop in performance in the first season but largely returned to baseline except for a reduction in goals per 60 at 3 seasons when compared with matched controls. No differences in GP or time-on-ice/GP were found when compared with controls. In contrast to Lubbe et al.,16 our analysis excluded shoulder instability, specifically focusing on glenoid labral tears instead of a wide range of pathologies included in “noninstability” shoulder arthroscopy and provided a control group for comparison. After shoulder labral repair, professional hockey players demonstrate an acute decline in performance but are mostly able to return to baseline performance aside from a reduction in goals at longer term-follow-up.
Despite these relative successes in returning to competition at a high performing level after arthroscopic shoulder surgery, conflicting results of career longevity for NHL skaters exists in the literature. Lubbe et al.16 concluded that no differences in RTP or career length were found between injuries, although those with shoulder instability played 4 seasons postoperatively compared to 2.1 for noninstability shoulder injuries. Swindell et al.15 examined shoulder instability in a group of 57 NHL athletes and found a 98.5% RTP rate. Compared with matched controls, no differences in goals, assists, pointers per game, or postoperative seasons played (5.3 vs 4.8 seasons, P = .33) were found between cases and controls, suggesting that career longevity remained unaffected. Interestingly, when they compared operative versus nonoperatively managed injuries, recurrent instability occurred in 14.3% of conservatively managed players and 33.3% sustained season-ending injuries requiring surgeries. Players suffering a recurrent event played in significantly fewer total career games relative to those undergoing surgery initially for instability. Although these studies are not directly comparable due to the heterogeneity of procedures examined, our group uniquely identified that NHL players experience significantly shorter careers with 4.4 ± 3.1 vs 6.0 ± 3.6 seasons played after surgery compared with controls. Hockey players sustain a significant number of collisions from contact with sticks, pucks, boards, and other players. These traumatic blows to the shoulder predispose to shoulder injuries, with 76% to 86.5% of injuries attributed to mechanisms involving collision or contact with another player.1,2,4,23 In addition to the forces of body checking, various movements in hockey require full shoulder range of motion, from winding up for a slapshot to extending a stick for a poke check. While we cannot specifically comment on any alterations of the biomechanics of the shoulder, our results suggest that players score fewer goals at 3 seasons and career longevity is significantly affected by shoulder labral repair.
Athletes appear to perform differentially after arthroscopic shoulder procedures across professional sports. Higgins et al.17 found that Major Baseball League players had significantly lower RTP rates and longer recovery times compared with the National Football League (NFL), NHL, and National Basketball Association (NBA). Players in the NHL and NBA similarly performed worse in the first postoperative season but improved closer to baseline 2 seasons after surgery.17 Career longevity was the shortest in the Major Baseball League with 3.7 years, longest in the NBA with 5.8 years, and similar among NHL and NFL players who played for 4.7 and 4.8 years, respectively. Higgins et al.17 reported a similar trend in NHL performance and postoperative playing career lengths for NHL players as compared with the present study (4.4 vs 4.7 seasons). While NFL athletes endure a unique set of physical demands relative to the NHL, it is not surprising that the NFL athletes have similar postoperative playing careers. Previous literature has suggested that shoulder labrum tears may negatively impact football playing careers. Chambers et al.24 found that NFL athletes with a history of SLAP tears played in significantly fewer games (33.7 vs 48.3; P = .049) and had fewer game starts (19.6 vs 35.4; P = .036) relative to controls. For players in the NFL combine, history of previous shoulder instability had a significant effect on playing in the NFL for offensive and defensive linemen and shorter career lengths for defensive linemen.25 These high-impact collision sports, such as hockey and football, pose a significant risk for shoulder injuries, which may portend worse playing outcomes in the acute setting and shorter careers after surgery. Our findings, however, exhibit resilience of NHL hockey players with improved performance over additional seasons.
Limitations
There are several limitations inherent to this study. The retrospective design is subject to information bias. Publicly available sources may report inaccurate information in terms of shoulder pathology, surgery performed, and concurrent injuries. Sports reporters may not understand the nuances of shoulder pathology and type of procedures offered, leading to misclassification of injury and procedure type in our study. Selection bias may exist for more prominent athletes, with increased attention paid to more prominent players, therefore skewing which injuries are reported and causing underreporting of lesser-known player injuries. Additional injuries after the index injury may not have been reported as well, which could have confounded the role shoulder labral repair factored into outcomes. While our methods of acquiring data are consistent with previous literature, we are unable to access official medical records or a centralized injury database and therefore were unable to completely rule out concomitant injuries or sequelae. Furthermore, the reported performance scores may not accurately represent a player’s role on a team. Certain players in the NHL, for example, serve as enforcers, penalty killers, or faceoff specialists rather than goal scorers. Finally, although we narrowed our study to address only glenoid labral tears and excluded shoulder instability, we were unable to comment on specific labral tear locations and types that may factor into repair strategy and outcome.
Conclusions
Following RTP after arthroscopic shoulder labral repair, NHL players demonstrated reduced career longevity compared with healthy controls. Players exhibited significant reductions in game use and performance at 1 season after injury but returned closer to baseline after 3 seasons.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Molsa J., Kujala U., Myllynen P., Torstila I., Airaksinen O. Injuries to the upper extremity in ice hockey: Analysis of a series of 760 injuries. Am J Sports Med. 2003;31:751–757. doi: 10.1177/03635465030310051901. [DOI] [PubMed] [Google Scholar]
- 2.Trojan J.D., Meyer L.E., Edgar C.M., Brown S.M., Mulcahey M.K. Epidemiology of shoulder instability injuries in collision collegiate sports from 2009 to 2014. Arthroscopy. 2020;36:36–43. doi: 10.1016/j.arthro.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Morrissey P.J., Maier S.P., 2nd, Zhou J.J., et al. Epidemiology and trends of adult ice hockey injuries presenting to United States emergency departments: A ten-year analysis from 2007-2016. J Orthop. 2020;22:231–236. doi: 10.1016/j.jor.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melvin P.R., Souza S., Mead R.N., Smith C., Mulcahey M.K. Epidemiology of upper extremity injuries in NCAA men's and women's ice hockey. Am J Sports Med. 2018;46:2521–2529. doi: 10.1177/0363546518781338. [DOI] [PubMed] [Google Scholar]
- 5.Gil J.A., Goodman A.D., DeFroda S.F., Owens B.D. Characteristics of operative shoulder injuries in the national collegiate athletic association, 2009-2010 through 2013-2014. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118790764. 2325967118790764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tuominen M., Stuart M.J., Aubry M., Kannus P., Parkkari J. Injuries in men's international ice hockey: A 7-year study of the International Ice Hockey Federation Adult World Championship Tournaments and Olympic Winter Games. Br J Sports Med. 2015;49:30–36. doi: 10.1136/bjsports-2014-093688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berube E.R., Lopez C.D., Trofa D.P., Popkin C.A. A systematic review of the orthopedic literature involving National Hockey League Players. Open Access J Sports Med. 2020;11:145–160. doi: 10.2147/OAJSM.S263260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donaldson L., Li B., Cusimano M.D. Economic burden of time lost due to injury in NHL hockey players. Inj Prev. 2014;20:347–349. doi: 10.1136/injuryprev-2013-041016. [DOI] [PubMed] [Google Scholar]
- 9.Beyzadeoglu T., Circi E. Superior labrum anterior posterior lesions and associated injuries: Return to play in elite athletes. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115577359. 2325967115577359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ricchetti E.T., Weidner Z., Lawrence J.T., Sennett B.J., Huffman G.R. Glenoid labral repair in Major League Baseball pitchers. Int J Sports Med. 2010;31:265–270. doi: 10.1055/s-0030-1247596. [DOI] [PubMed] [Google Scholar]
- 11.Robins R.J., Daruwalla J.H., Gamradt S.C., et al. Return to play after shoulder instability surgery in National Collegiate Athletic Association Division I intercollegiate football athletes. Am J Sports Med. 2017;45:2329–2335. doi: 10.1177/0363546517705635. [DOI] [PubMed] [Google Scholar]
- 12.Okoroha K.R., Taylor K.A., Marshall N.E., et al. Return to play after shoulder instability in National Football League athletes. J Shoulder Elbow Surg. 2018;27:17–22. doi: 10.1016/j.jse.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 13.Khalil L.S., Jildeh T.R., Abbas M.J., et al. Career longevity and performance after shoulder instability in National Football League athletes. Arthroscopy. 2021;37:1437–1445. doi: 10.1016/j.arthro.2020.12.225. [DOI] [PubMed] [Google Scholar]
- 14.Lu Y., Okoroha K.R., Patel B.H., et al. Return to play and performance after shoulder instability in National Basketball Association athletes. J Shoulder Elbow Surg. 2020;29:50–57. doi: 10.1016/j.jse.2019.05.035. [DOI] [PubMed] [Google Scholar]
- 15.Swindell H.W., McCormick K.L., Tedesco L.J., et al. Shoulder instability, performance, and return to play in National Hockey League players. JSES Int. 2020;4:786–791. doi: 10.1016/j.jseint.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubbe R.J., Freshman R.D., Singh G., et al. Performance outcomes and return-to-sport rate of National Hockey League athletes vary after common orthopedic surgical procedures. Clin J Sport Med. 2021;31:57–62. doi: 10.1097/JSM.0000000000000696. [DOI] [PubMed] [Google Scholar]
- 17.Higgins M.J., DeFroda S., Yang D.S., Brown S.M., Mulcahey M.K. Professional athlete return to play and performance after shoulder arthroscopy varies by sport. Arthrosc Sports Med Rehabil. 2021;3:e391–e397. doi: 10.1016/j.asmr.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khalil L.S., Jildeh T.R., Tramer J.S., et al. Effect of Achilles tendon rupture on player performance and longevity in National Basketball Association players. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120966041. 2325967120966041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jildeh T.R., Meta F., Young J., Page B., Okoroha K.R. Concussion in National Football League athletes is not associated with increased risk of acute, noncontact lower extremity musculoskeletal injury. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211003491. 23259671211003491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khalil L.S., Matar R.N., Rahman T., et al. Effect of workload After ACL reconstruction on rerupture rates in NBA players. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120964467. 2325967120964467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marshall N.E., Jildeh T.R., Okoroha K.R., et al. Performance, return to play, and career longevity after ulnar collateral ligament reconstruction in professional catchers. Arthroscopy. 2018;34:1809–1815. doi: 10.1016/j.arthro.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Rangavajjula A., Hyatt A., Raneses E., McCrossin J., Cohen S., DeLuca P. Return to play after treatment of shoulder labral tears in professional hockey players. Phys Sportsmed. 2016;44:119–125. doi: 10.1080/00913847.2016.1168688. [DOI] [PubMed] [Google Scholar]
- 23.Owens B.D., Agel J., Mountcastle S.B., Cameron K.L., Nelson B.J. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37:1750–1754. doi: 10.1177/0363546509334591. [DOI] [PubMed] [Google Scholar]
- 24.Chambers C.C., Lynch T.S., Gibbs D.B., et al. Superior labrum anterior-posterior tears in the National Football League. Am J Sports Med. 2017;45:167–172. doi: 10.1177/0363546516673350. [DOI] [PubMed] [Google Scholar]
- 25.Brophy R.H., Lyman S., Chehab E.L., Barnes R.P., Rodeo S.A., Warren R.F. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37:768–775. doi: 10.1177/0363546508329542. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.