Abstract
Purpose
To compare magnetic resonance imaging (MRI) with magnetic resonance arthrogram (MRA) in the identification of hip capsular defects in patients who previously underwent hip arthroscopy.
Methods
Patients who underwent revision hip arthroscopy for capsular insufficiency by a single surgeon between March 2014 and December 2019 were identified by Current Procedural Terminology code. Patients with arthroscopically confirmed capsular defects treated surgically who underwent both MRI and MRA between their primary and revision surgeries were identified. Imaging studies were blinded, randomized, and distributed to two fellowship-trained musculoskeletal radiologists. Radiologists evaluated 14 components of different anatomic structures, including the presence of capsular defect and defect grading, over 2 months, with a 2-week washout period between 4 sets of reads to obtain 2 complete reads from each radiologist. Data were analyzed in R version 4.0.2.
Results
Two hundred thirty patients underwent revision hip arthroscopy between March 2014 and December 2019. Twelve patients had both an MRI and an MRA of the operated hip performed between their primary and revision surgeries. Time between primary and revision hip arthroscopy was 2.0 ± 1.5 years (R: .3-6.3). Time between MRI and MRA was .6 ± .6 years (R: .0-1.6). Sensitivity for detecting hip capsular defects was significantly higher for MRA than for MRI (87.5%, 95% CI: [68,96] vs 50%, 95% CI: [31,69], respectively; P = .008).
Conclusions
This retrospective review demonstrates that MRA has higher sensitivity than MRI in detecting surgically confirmed capsular defects. MRA may be more helpful in identifying capsular defects in patients presenting with hip instability symptoms who have had a previous hip arthroscopy.
Level of Evidence
Level IV, diagnostic case series.
Introduction
Hip instability as a cause of persistent pain and disability following hip arthroscopy is a subject of current controversy and interest. During hip arthroscopy, a capsulotomy is frequently performed to facilitate access to the hip joint. Various techniques have been described, including periportal, interportal, and T-type capsulotomies. Among hip arthroscopists, there is continued discussion regarding capsular management and the utility of routine capsular repair. Numerous capsular repair techniques have been described, and both cadaveric and clinical biomechanical studies demonstrate that capsular repair restores normal biomechanical capsular function.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11
In patients who previously underwent hip arthroscopy, symptoms of postsurgical capsular instability, such as pain with activities of daily living and exercise, must be differentiated from other hip pathologies.2 Concurrent pathologies may include primary or residual femoroacetabular impingement (FAI), chondrolabral pathology, adhesions, and acetabular dysplasia. The patient’s history, physical examination findings, and studies should be used to help make a diagnosis.2
Imaging evaluation of postsurgical capsular changes has been previously studied. One study comparing primary hip arthroscopy patients with repaired versus unrepaired capsulotomy demonstrated no significant difference in capsular appearance at 24 weeks postoperatively on magnetic resonance imaging (MRI).12 Another study demonstrated no significant difference in the number of capsular defects among asymptomatic versus symptomatic patients 1 year following primary hip arthroscopy, suggesting that imaging should be used to confirm clinical diagnoses. Still, another study demonstrated that all patients undergoing revision hip arthroscopy had capsular irregularities on magnetic resonance arthrogram (MRA).13
The purpose of this study was to compare MRI with MRA in the identification of hip capsular defects in patients who previously underwent hip arthroscopy. We hypothesized that MRA would be more sensitive than MRI for this purpose.
Methods
Cohort Selection
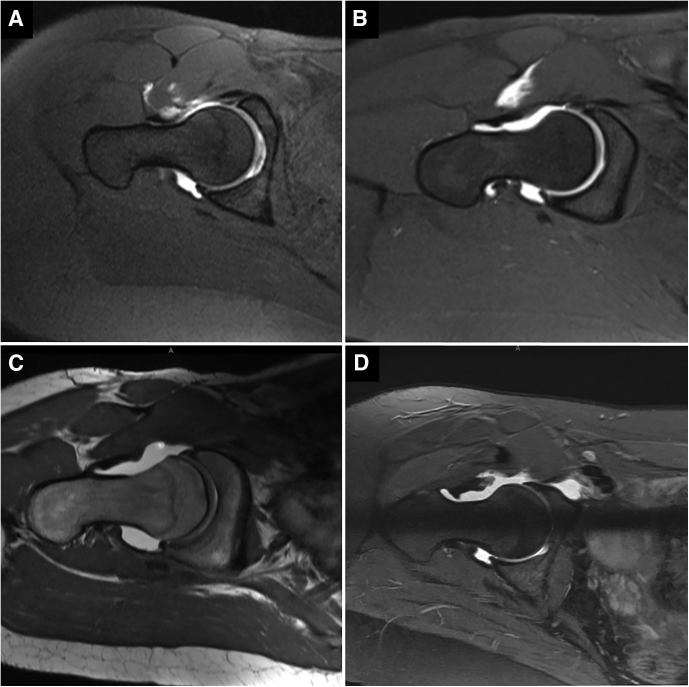
Following Institutional Review Board approval (IRB approval no. 55341), patients who underwent revision hip arthroscopy by a single surgeon (S.K.A.) between March 2014 and December 2019 were identified by Current Procedural Terminology (CPT) codes. Inclusion criteria were patients who underwent revision hip arthroscopy with a clinical diagnosis of hip instability, had an arthroscopically confirmed capsular defect, underwent surgical treatment for the capsular defect, and had both an MRI and MRA of the symptomatic hip obtained between the primary and revision surgeries. Presence of capsular defects was confirmed via operative note and arthroscopic imaging review for each patient (Fig 1). Electronic medical record review was performed to identify patients who had undergone both MRI and MRA of the operated hip after primary hip arthroscopy, but prior to revision hip arthroscopy. Once patients were identified, electronic medical record review was performed to collect demographic information.
Fig 1.
Arthroscopic image of a right hip from the anterolateral portal, superior view demonstrating a 2.5 × 2 cm capsular defect. CA, acetabular-sided capsule; CF, femoral-sided capsule; FH, femoral head.
MR Evaluation
All MRIs and MRAs were randomized and anonymized into four groups in PACS IntelliSpace (Philips, Amsterdam, Netherlands). Each group contained both MRIs and MRAs, but no group contained both scans from the same patient. Reads of the first two groups and the second two groups provided two complete sets of reads to facilitate analysis of intra-rater reliability. Two fellowship-trained musculoskeletal radiologists (H.A., A.M.C.) were recruited as readers to facilitate analysis of inter-rater reliability. Reads of each group of scans were 2 weeks apart, to allow for a washout period.
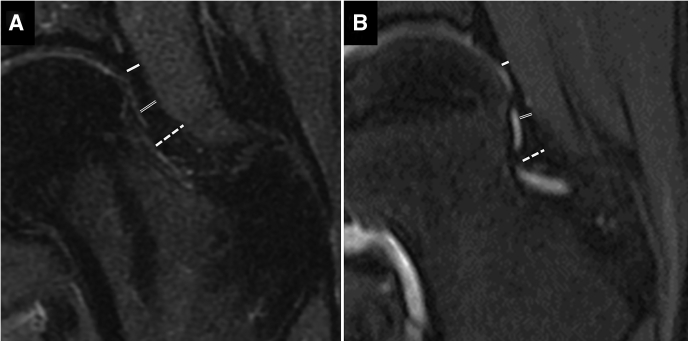
Readers were instructed to analyze 14 different components that are typically evaluated in a postoperative hip MRI and were blinded from the primary purpose of the study. Evaluation of multiple hip structures prevented readers from solely focusing on the capsule (Table 1). For each of these components, readers were asked to rate their diagnosis confidence on a scale of 1-4, with 1 being “not confident” and 4 being “very confident”. Capsular defects were graded using the scale described by O’Neill et al. (Fig 2).2 The presence of a capsular defect was then defined as a capsular grade greater than 0 and rated on a yes/no basis.
Table 1.
Evaluated Components of MRI and MRA
| Anatomy | Evaluated Component | Response Options |
|---|---|---|
| Labrum | Tear Presence | Yes/No |
| Tear Location | Anterosuperior | |
| Posterosuperior | ||
| Posteroinferior | ||
| Acetabular cartilage | Severity | Normal/Partial/Full |
| Delamination | Yes/No | |
| Subchondral Edema | Yes/No | |
| Subchondral Cyst | Yes/No | |
| Femoral cartilage | Severity | Normal/Partial/Full |
| Delamination | Yes/No | |
| Subchondral Edema | Yes/No | |
| Subchondral Cyst | Yes/No | |
| Hip capsule | Defect presence | Yes/No |
| Grade∗ | Normal - 0 | |
| Redundancy -1 | ||
| Focal Rent - 2 | ||
| Gross extravasation - 3 | ||
| Osteoplasty | Completion | Yes/No |
| Intraarticular adhesions | Presence | Yes/No |
MRA, magnetic resonance arthrogram; MRI, magnetic resonance imaging.
As described by O’Neill et al.2
Fig 2.
Capsular grading in T1 axial oblique magnetic resonance arthrographic studies of four right hips as described by O’Neill et al.2 (A) Grade 0: normal capsular anatomy and volume. (B) Grade 1: intact continuous anterior capsule with increased capsular volume and redundancy. (C) Grade 2: focal capsular rent with increased contrast signal anteriorly indicating high capsular volume and a focal defect in the capsule. (D) Grade 3: highly irregular capsular contour and gross fluid extravasation.
Statistical Analysis
An a priori power analysis demonstrated that with 12 samples, there is 80% power to detect a 52% absolute decrease from 90% sensitivity using MRA and 38% sensitivity using MRI using a two-tailed paired t-test with a .05 significance level. Data were analyzed using R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). Times between primary and revision hip arthroscopy and between MRI and MRA were summarized as means ± SD and range (R). Sensitivities at detecting capsular defects were compared between MRI and MRA using a generalized estimating equation logistic regression. Sensitivity for detecting hip capsular defects using MRA vs. MRI were reported for each rater separately with 95% exact binomial confidence intervals (CIs). A generalized estimating equation (GEE) logistic regression model assumes an “exchangeable” correlation structure within subjects was used to compare sensitivity between MRA and MRI, adjusting for rater. From the same model, the average sensitivity of the two raters was estimated for each method (MRA and MRI) with 95% CIs. The average confidence of the two raters in the assessment of each of the 14 components was compared between MRA and MRI, using GEE linear models with 95% CIs.
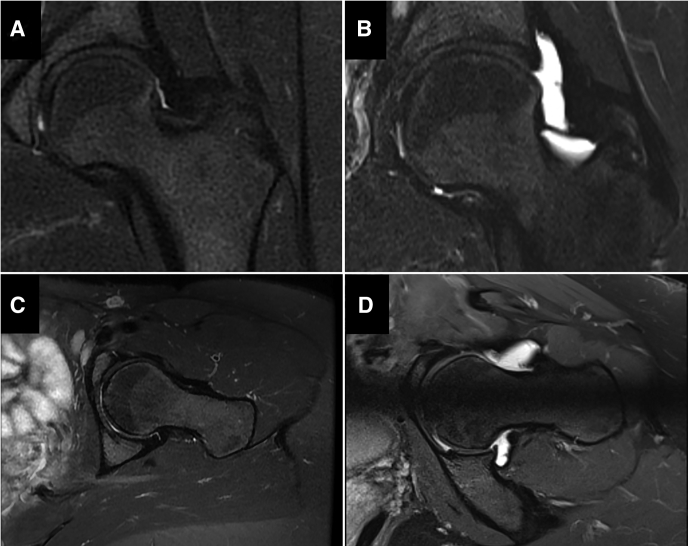
An intraclass correlation coefficient (ICC) with a 95% confidence interval was calculated to determine inter-rater reliability between the two sets of measurements. Similar to the methodology used by Strickland et al.,12 measurements consisted of proximal, middle, and distal capsular thickness performed on midcoronal T2 or proton density fat-saturated images; ICCs were reported as point estimates. Capsular thickness was defined proximally at the level of the labrum and distally through the thickness of the zona orbicularis, with middle defined as the capsular thickness at the midway point between the proximal and distal measurements (Fig 3). An ICC value greater than .9 was considered excellent, .75-.9 was considered good, .5-.75 was considered moderate, and less than .5 was considered poor.14
Fig 3.
Capsular thickness measurements used in the calculation of intraclass correlation coefficients, similar to the methods used by Strickland et al.12 Capsular thickness was measured proximally at the level of the labrum (solid line); distally through the thickness of the zona orbicularis (dashed line), and at the midpoint between the proximal and distal measurements (double line). (A) Capsular thickness as measured on MRI in a left hip. (B) Capsular thickness as measured on MRA in a left hip.
Results
Cohort
Two hundred thirty patients who underwent revision hip arthroscopy between March 2014 and December 2019 were identified. Review of these 230 patients identified 12 patients who met inclusion criteria with arthroscopically confirmed capsular defects that had both a dedicated hip MRI and an MRA between the primary and revision surgeries. Demographics of patients who met inclusion criteria are detailed in Table 2. There were 10 females (83%) and 2 males (17%). Age at the time of revision hip arthroscopy was 30.3 ± 9.6 years. Time between primary and revision hip arthroscopy was 2.0 ± 1.5 years. Time between initial surgery and MRI was 1.4 ± 1.7 years. Time between initial surgery and MRA was 1.8 ± 1.6 years. Time between MRI and MRA was .6 ± .6 years.
Table 2.
Patient Demographics
| Variable | n = 12 |
|---|---|
| Age at revision surgery, years | 30.3 (9.6) |
| Range | 17.7, 48.0 |
| Sex, n (%) | |
| Female | 10 (83%) |
| Male | 2 (17%) |
| Time between index and revision surgeries, years | 2.0 (1.5) |
| Range | .3, 6.3 |
| Time between MRI and MRA, years | .6 (.6) |
| Range | .0, 1.6 |
Variables are reported as means (SD) unless otherwise specified. MRA, magnetic resonance arthrogram; MRI, magnetic resonance imaging.
MR Evaluation
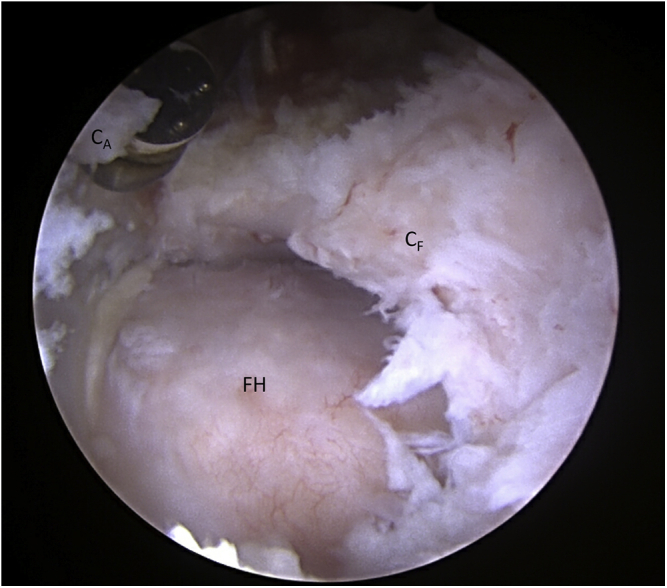
Sensitivity (rater average) for detecting hip capsular defects was higher for MRA than for MRI (87.5%, 95% CI: [68,96] vs 50%, 95% CI: [31,69], respectively; P = .008). MR appearance of capsular defects was modality dependent (Fig 4). Confidence ratings for both MRI and MRA for identification of capsular defects averaged 2.8 on a scale of 1-4, with 4 being the most confident. The differences between these ratings were not significant (P = .76).
Fig 4.
Comparison of MRI and MRA of the left hip in a 34-year-old female, demonstrating modality-dependent visualized differences in capsular appearance. MRI (A) and MRA coronal T2 sequences (B); MRI (C), and MRA oblique axial T2 sequences (D).
Reliability Analysis
ICCs for proximal and middle capsular thickness on MRI were .75 and .79, falling into the range of good. ICCs for distal capsular thickness on MRI and proximal, middle, and distal capsular thickness on MRA were .60, .66, .67, and .60, which fell into the moderate range.
Discussion
MRA resulted in significantly higher sensitivity than MRI in the identification of capsular defects. The ICCs suggest that MRI and MRA are moderately reliable ways to evaluate the hip capsule thickness in the setting of a previous hip arthroscopy. However, musculoskeletal radiologists did not report significant confidence differences in identifying capsular defects. Overall, our findings suggest MRA may be more appropriate than MRI in postoperative patients where capsular insufficiency and hip instability may be suspected. These findings are significant given evolving options for surgical management in the hip instability patient population.15, 16, 17, 18
Many studies examined the utility of MRA in the diagnosis of intra-articular hip lesions.19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 Several of these studies simultaneously evaluated the use of MRI in the diagnosis of intra-articular hip lesions and provided comparisons between the two.22,28,29,31 Byrd and Jones found in their study of 40 patients that MRA had higher sensitivity for the detection of labral tears and that sensitivity and specificity trended higher for MRA than MRI for the evaluation of labral tears, chondral damage, and ligamentum teres rupture, although these differences were not significant.22 Tian et al. evaluated the diagnostic performance of MRI and MRA in the diagnosis of acetabular labral tears in 34 patients and found that MRA was superior to MRI at 3-T.28 Magee et al. studied 3-T MRI versus 3-T MRA in the diagnosis of acetabular labral tears and chondral defects and concluded that sensitivity was comparable for MRI versus MRA in the detection of acetabular labral tears, but that MRA had higher sensitivity for the detection of acetabular chondral defects.29 Crespo Rodríguez et al. evaluated 3-T MRI versus 1.5-T MRA in the assessment of labral and articular cartilage lesions in patients with clinical suspicion of FAI and found similar diagnostic utility between the two studies.31 Overall, prior research has established MRA as being of equal or greater utility than MRI in the evaluation of intra-articular hip lesions.
Fewer studies have evaluated hip capsular imaging. Lurie et al. stated that MRI is the imaging modality of choice in the preoperative and postoperative assessments of patients undergoing hip arthroscopy, with specific focus on the labrum, capsule, and synovium.32 Most relevant to the current study, Strickland et al. performed a randomized controlled trial of 15 patients who underwent bilateral hip arthroscopy with one hip undergoing capsular repair and the other no capsular repair. MRI was performed at 6 and 24 weeks postoperatively and was analyzed by two musculoskeletal radiologists. They found that at 6 weeks postoperatively, there were more continuous, healed capsules in hips that underwent capsular repair, although at 24 weeks postoperatively, all discontinuous capsules at 6 weeks had demonstrated progression to healing.12 Kraeutler et al. continued this research in a multicenter randomized controlled trial and again demonstrated that repaired capsules healed at higher rates at 6 weeks postoperatively, although at 24 weeks postoperatively, this difference was normalized between the unrepaired and repaired groups. They concluded that capsular repair of small- to moderate-sized capsulotomy did not provide radiographic advantage following hip arthroscopy for FAI.33 Weber et al. evaluated 39 patients who underwent postoperative MRI following hip arthroscopy for FAI with routine capsular closure, and they found that 92.5% of repaired capsules remained closed at 1 year of follow-up.34 These studies suggest that capsular repair does not significantly impact capsular closure, as evaluated on a standard MRI.
Studies evaluating the hip capsule using MRA demonstrate more abnormal findings compared with studies using MRI. McCormick et al. evaluated 9 patients who underwent MRA following revision hip arthroscopy and found that all patients had postsurgical capsular irregularities, and 7 had capsular and iliofemoral defects.13 In symptomatic patients, O’Neill et al. characterized clinical and radiographic findings of capsular instability and devised a capsular grading system using MRA,2 as previously described and used in the present study. Magerkurth et al. demonstrated that hip joint laxity is associated with distinct findings on MR arthrography, including widening of the anterior hip joint recess and thinning of the adjacent joint capsule lateral to the zona orbicularis.35 Kim et al. evaluated imaging abnormalities in 17 asymptomatic and 17 symptomatic patients who underwent 1.5-T MR arthrography of the hip 1 year after undergoing arthroscopy for FAI, and counterintuitively found that capsular defects were more common in asymptomatic patients (77% vs 53%). These MRA studies demonstrate significantly more capsular defects and variations compared with the aforementioned MRI studies.
In this study, the fellowship-trained musculoskeletal radiologists were more accurate in the identification of capsular defects using MRA, although they rated their confidence similarly between the two modalities. Several aforementioned MRI-based capsular imaging studies demonstrated adequate capsular healing with and without capsular repair following primary hip arthroscopy.12,33,34 The noncongruence between diagnostic accuracy and confidence for MRI demonstrated in the present study highlights that MRI is considered by musculoskeletal radiologists to be a reliable imaging modality for the detection of capsular defects, despite its apparent shortcomings in capsular visualization.
In the current study, the use of MRA resulted in significantly increased sensitivity for the detection of hip capsular defects compared with MRI. These findings suggest that apparent capsular healing as visualized on MRI may not be an adequate imaging study for the visualization of all capsular defects and that MRA may be more appropriate than MRI for patients presenting with symptoms of iatrogenic hip instability to evaluate for capsular defects. In suspected postarthroscopy hip instability, clinical history and presentation are often sufficient for diagnosis. To confirm the presence of capsular defects and evaluate for other causes of postarthroscopy hip pain, the authors of the present study recommend the use of MRA over MRI prior to revision hip arthroscopy.
Limitations
There are several limitations to this study. First, this study only evaluated patients with known capsular defects, preventing the calculation of specificity for both MRI and MRA. Second, because this study was performed retrospectively, patients did not have both MRI and MRA performed on the same date, and patients may have developed a capsular defect in between their studies. However, 11 of 12 patients underwent MRI prior to their MRA, and all patients had a similar presentation consistent with postarthroscopic hip instability. Future research should compare capsular defect identification using MRI, MRA, and intraoperative visualization within a restricted timeframe. Third, the sample size in this study is limited to 12 due to the strict inclusion criteria. In order to evaluate the ability to visualize a capsular defect on MR imaging, the study inclusion criteria needed to focus on patients that had both an MRI and an MRA following the primary surgery, along with an arthroscopic confirmed capsular defect on the revision surgery. Because of the small sample size, inter-rater reliability as assessed by ICCs was moderate to good. Still, a statistically significant difference in sensitivity of detection of capsular defects between MRI and MRA was observed. Fourth, the limited number of patients undergoing revision hip arthroscopy who underwent both MRI and MRA compared with the number of patients who only underwent one or zero advanced imaging modalities could introduce bias. Finally, while most patients underwent imaging studies at the authors’ institution, some imaging was obtained from outside hospitals. MRI machines and obtained image sequences were, therefore, not standardized among all patients.
Conclusions
This retrospective review demonstrates that MRA has higher sensitivity than MRI in detecting surgically confirmed capsular defects. MRA may be more helpful in identifying capsular defects in patients presenting with hip instability symptoms, who have had a previous hip arthroscopy.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: H.A. reports being a minority shareholder in Elucent Medical. A.M.C. reports personal fees from Biocompatibles, Inc., outside the submitted work. S.K.A. reports personal fees from Stryker Corporation, Smith & Nephew, and Active Medical LLC, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Abrams G.D., Hart M.A., Takami K., et al. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015;31:1511–1517. doi: 10.1016/j.arthro.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 2.O’Neill D.C., Mortensen A.J., Cannamela P.C., Aoki S.K. Clinical and radiographic presentation of capsular iatrogenic hip instability after previous hip arthroscopy. Am J Sports Med. 2020;48:2927–2932. doi: 10.1177/0363546520949821. [DOI] [PubMed] [Google Scholar]
- 3.Philippon M.J., Trindade C.A.C., Goldsmith M.T., et al. Biomechanical assessment of hip capsular repair and reconstruction procedures using a 6 degrees of freedom robotic system. Am J Sports Med. 2017;45:1745–1754. doi: 10.1177/0363546517697956. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz-Declet V., Mu B., Chen A.W., et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34:303–318. doi: 10.1016/j.arthro.2017.06.030. [DOI] [PubMed] [Google Scholar]
- 5.Khair M.M., Grzybowski J.S., Kuhns B.D., Wuerz T.H., Shewman E., Nho S.J. The effect of capsulotomy and capsular repair on hip distraction: A cadaveric investigation. Arthroscopy. 2017;33:559–565. doi: 10.1016/j.arthro.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Wuerz T.H., Song S.H., Grzybowski J.S., et al. Capsulotomy size affects hip joint kinematic stability. Arthroscopy. 2016;32:1571–1580. doi: 10.1016/j.arthro.2016.01.049. [DOI] [PubMed] [Google Scholar]
- 7.Wylie J.D., Beckmann J.T., Maak T.G., Aoki S.K. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44:39–45. doi: 10.1177/0363546515608162. [DOI] [PubMed] [Google Scholar]
- 8.Bolia I.K., Fagotti L., Briggs K.K., Philippon M.J. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthroscopy. 2019;35:1828–1834. doi: 10.1016/j.arthro.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 9.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: A comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 10.Larson C.M., Ross J.R., Stone R.M., et al. Arthroscopic management of dysplastic hip deformities: Predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2015;44:447–453. doi: 10.1177/0363546515613068. [DOI] [PubMed] [Google Scholar]
- 11.Riff A.J., Kunze K.N., Movassaghi K., et al. Systematic review of hip arthroscopy for femoroacetabular impingement: The importance of labral repair and capsular closure. Arthroscopy. 2019;35:646–656.e3. doi: 10.1016/j.arthro.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Strickland C.D., Kraeutler M.J., Brick M.J., et al. MRI evaluation of repaired versus unrepaired interportal capsulotomy in simultaneous bilateral hip arthroscopy: A double-blind, randomized controlled trial. JBJS. 2018;100:91–98. doi: 10.2106/JBJS.17.00365. [DOI] [PubMed] [Google Scholar]
- 13.McCormick F., Slikker W., Harris J.D., et al. Evidence of capsular defect following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2013;22:902–905. doi: 10.1007/s00167-013-2591-z. [DOI] [PubMed] [Google Scholar]
- 14.Koo T.K., Li M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Featherall J., Tomasevich K.M., O’Neill D.C., Mortensen A.J., Aoki S.K. Arthroscopic hip capsule reconstruction for anterior hip capsule insufficiency in the revision setting. Arthrosc Tech. 2021;10:e1339–e1344. doi: 10.1016/j.eats.2021.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trindade C.A.C., Sawyer G.A., Fukui K., Briggs K.K., Philippon M.J. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4:e71–e74. doi: 10.1016/j.eats.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kurz A.Z., Memon M., Williams D., Ayeni O.R. Anterior capsule reconstruction of the native hip: A technique guide. Arthrosc Tech. 2019;8:e1247–e1253. doi: 10.1016/j.eats.2019.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mei-Dan O., Garabekyan T., McConkey M., Pascual-Garrido C. Arthroscopic anterior capsular reconstruction of the hip for recurrent instability. Arthrosc Tech. 2015;4:711–715. doi: 10.1016/j.eats.2015.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Czerny C., Hofmann S., Urban M., et al. MR arthrography of the adult acetabular capsular-labral complex: Correlation with surgery and anatomy. Am J Roentgenol. 1999;173:345–349. doi: 10.2214/ajr.173.2.10430132. [DOI] [PubMed] [Google Scholar]
- 20.Schmid M.R., Nötzli H.P., Zanetti M., Wyss T.F., Hodler J. Cartilage lesions in the hip: Diagnostic effectiveness of MR arthrography. Radiology. 2003;226:382–386. doi: 10.1148/radiol.2262020019. [DOI] [PubMed] [Google Scholar]
- 21.Keeney J.A., Peelle M.W., Jackson J., Rubin D., Maloney W.J., Clohisy J.C. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;429:163–169. doi: 10.1097/01.blo.0000150125.34906.7d. [DOI] [PubMed] [Google Scholar]
- 22.Byrd J.W.T., Jones K.S. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668–1674. doi: 10.1177/0363546504266480. [DOI] [PubMed] [Google Scholar]
- 23.Chan Y.-S., Lien L.-C., Hsu H.-L., et al. Evaluating hip labral tears using magnetic resonance arthrography: A prospective study comparing hip arthroscopy and magnetic resonance arthrography diagnosis. Arthroscopy. 2005;21 doi: 10.1016/j.arthro.2005.07.007. 1250. e1-1250.e8. [DOI] [PubMed] [Google Scholar]
- 24.Freedman B.A., Potter B.K., Dinauer P.A., Giuliani J.R., Kuklo T.R., Murphy K.P. Prognostic value of magnetic resonance arthrography for Czerny stage II and III acetabular labral tears. Arthroscopy. 2006;22:742–747. doi: 10.1016/j.arthro.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 25.Toomayan G.A., Holman W.R., Major N.M., Kozlowicz S.M., Vail T.P. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. Am J Roentgenol. 2006;186:449–453. doi: 10.2214/AJR.04.1809. [DOI] [PubMed] [Google Scholar]
- 26.Studler U., Kalberer F., Leunig M., et al. MR arthrography of the hip: Differentiation between an anterior sublabral recess as a normal variant and a labral tear. Radiology. 2008;249:947–954. doi: 10.1148/radiol.2492080137. [DOI] [PubMed] [Google Scholar]
- 27.Ziegert A.J., Blankenbaker D.G., De Smet A.A., Keene J.S., Shinki K., Fine J.P. Comparison of standard hip MR arthrographic imaging planes and sequences for detection of arthroscopically proven labral tear. AJR Am J Roentgenol. 2009;192:1397–1400. doi: 10.2214/AJR.08.1609. [DOI] [PubMed] [Google Scholar]
- 28.Tian C.-Y., Wang J.-Q., Zheng Z.-Z., Ren A.-H.3. 0T conventional hip MR and hip MR arthrography for the acetabular labral tears confirmed by arthroscopy. Eur J Radiol. 2014;83:1822–1827. doi: 10.1016/j.ejrad.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 29.Magee T. Comparison of 3.0-T MR vs 3.0-T MR arthrography of the hip for detection of acetabular labral tears and chondral defects in the same patient population. Br J Radiol. 2015;88:20140817. doi: 10.1259/bjr.20140817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crespo Rodríguez A.M., de Lucas Villarrubia J.C., Pastrana Ledesma M.A., Millán Santos I., Padrón M. Diagnosis of lesions of the acetabular labrum, of the labral–chondral transition zone, and of the cartilage in femoroacetabular impingement: Correlation between direct magnetic resonance arthrography and hip arthroscopy. Radiología. 2015;57:131–141. doi: 10.1016/j.rx.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Crespo-Rodríguez A.M., De Lucas-Villarrubia J.C., Pastrana-Ledesma M., Hualde-Juvera A., Méndez-Alonso S., Padron M. The diagnostic performance of non-contrast 3-Tesla magnetic resonance imaging (3-T MRI) versus 1.5-Tesla magnetic resonance arthrography (1.5-T MRA) in femoro-acetabular impingement. Eur J Radiol. 2017;88:109–116. doi: 10.1016/j.ejrad.2016.12.031. [DOI] [PubMed] [Google Scholar]
- 32.Lurie B., Gold S.L., Potter H.G. In: Hip joint restoration: Worldwide advances in arthroscopy, arthroplasty, osteotomy and joint preservation surgery. McCarthy J.C., Noble P.C., Villar R.N., editors. Springer; New York: 2017. Magnetic resonance imaging of the hip labrum, capsule, and synovium; pp. 231–245. [Google Scholar]
- 33.Kraeutler M.J., Strickland C.D., Brick M.J., et al. A multicenter, double-blind, randomized controlled trial comparing magnetic resonance imaging evaluation of repaired versus unrepaired interportal capsulotomy in patients undergoing hip arthroscopy for femoroacetabular impingement. J Hip Preserv Surg. 2018;5:349–356. doi: 10.1093/jhps/hny045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weber A.E., Kuhns B.D., Cvetanovich G.L., et al. Does the hip capsule remain closed after hip arthroscopy with routine capsular closure for femoroacetabular impingement? A magnetic resonance imaging analysis in symptomatic postoperative patients. Arthroscopy. 2017;33:108–115. doi: 10.1016/j.arthro.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 35.Magerkurth O., Jacobson J.A., Morag Y., Caoili E., Fessell D., Sekiya J.K. Capsular laxity of the hip: Findings at magnetic resonance arthrography. Arthroscopy. 2013;29:1615–1622. doi: 10.1016/j.arthro.2013.07.261. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.