Abstract
Background
Substantial evidence indicates that dysbiosis of the gut microbial community is associated with colorectal neoplasia. This review aims to systematically summarise the microbial markers associated with colorectal neoplasia and to assess their predictive performance.
Methods
A comprehensive literature search of MEDLINE and EMBASE databases was performed to identify eligible studies. Observational studies exploring the associations between microbial biomarkers and colorectal neoplasia were included. We also included prediction studies that constructed models using microbial markers to predict CRC and adenomas. Risk of bias for included observational and prediction studies was assessed.
Results
Forty-five studies were included to assess the associations between microbial markers and colorectal neoplasia. Nine faecal microbiotas (i.e., Fusobacterium, Enterococcus, Porphyromonas, Salmonella, Pseudomonas, Peptostreptococcus, Actinomyces, Bifidobacterium and Roseburia), two oral pathogens (i.e., Treponema denticola and Prevotella intermedia) and serum antibody levels response to Streptococcus gallolyticus subspecies gallolyticus were found to be consistently associated with colorectal neoplasia. Thirty studies reported prediction models using microbial markers, and 83.3% of these models had acceptable-to-good discrimination (AUROC > 0.75). The results of predictive performance were promising, but most of the studies were limited to small number of cases (range: 9–485 cases) and lack of independent external validation (76.7%).
Conclusions
This review provides insight into the evidence supporting the association between different types of microbial species and their predictive value for colorectal neoplasia. Prediction models developed from case-control studies require further external validation in high-quality prospective studies. Further studies should assess the feasibility and impact of incorporating microbial biomarkers in CRC screening programme.
Subject terms: Prognostic markers, Microbiome
Introduction
Colorectal cancer (CRC) is the world’s third most common cancer and the second leading cause of cancer death [1]. It is reported that men have a higher risk of developing CRC compared to women, and women have up to 25% lower risk of CRC mortality than men [2]. Previous evidence suggests that this sex-specific difference could be attributed to the differential exposure to sex hormones, especially to oestrogen [3]. Elevated nuclear oestrogen receptor beta expression is independently associated with a better overall survival in female patients, revealing that the oestrogen receptor beta may be involved in underlying mechanisms in CRC [4].
Although substantial research has been conducted, a full understanding of the complex aetiology of CRC remains elusive, as well as the pathogenesis of progression. Increasing evidence is revealing that dysbiosis of the gut microbiome may be involved in the pathogenesis of CRC, which may lead to chronic metabolic and inflammatory changes and thus promote colorectal carcinogenesis [5–7]. For example, exposure to common prescription drugs (e.g., proton pump inhibitors and oral antibiotics) might influence the dysbiosis of gut microbiome and therefore contribute to the development of neoplastic lesions [8]. Apart from their potential for carcinogenesis, associations between gut bacteria and clinical outcomes of CRC have raised the possibility of using them as prognostic markers. Several molecular epidemiology studies have reported an inverse association between the tumour-associated Fusobacterium nucleatum and CRC survival [9, 10]. In addition, the gut microbiota may modulate the response to cancer therapy and susceptibility to toxic adverse effects, thereby affecting outcome, although there is only limited evidence for this [11, 12].
In recent years, many countries have introduced organized screening programme to increase early CRC detection followed by colonoscopy if needed [13]. Importantly, there is evidence that changes in the gut microbiome may occur during the early stages of colorectal carcinogenesis and can be used to identify individuals at risk. Changes in the microbiome over time might therefore be used as biomarkers for the early detection of colorectal neoplasia, and for improving screening strategies [14]. The interest is further encouraged by the fact that bacterial DNA can be successfully isolated from quantitative faecal immunochemical test (qFIT) cartridges [15] and used for risk prediction/stratification complementing existing qFIT screening programme. Microbial markers could be used as a complementary test for qFIT, especially among populations with borderline qFIT results. Therefore, a screening strategy that combines qFIT with microbial markers could optimise the existing programme and potentially reduce the number of unnecessary diagnostic colonoscopies [15]. Though it has been reported that proteomics could also be used as biomarkers for application in stool-based CRC screening, proteins identified for detection of colorectal adenomas are mainly makers of blood in the stool and therefore have limited complementary value to hemoglobin [16]. The independence of microbial markers to faecal hemoglobin reflects its potential in improving the current qFIT-based CRC screening strategies relative to protein markers [17].
In view of rapidly evolving in understanding the role of microbiota in benign and malignant colorectal neoplasia and their use as predictors for risk prediction/stratification, we set out to provide a comprehensive and current assessment of the literature. Here, we aimed to systematically review studies investigating associations between microbial markers and colorectal neoplasia and their application for risk prediction/stratification. We additionally conducted a comparative syntheses between the identified microbial markers and the predictors employed in risk prediction models to examine to what extent predictive models include the most influential factors.
Methods
Study design
This study was conceived and conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [18]. The study protocol was registered in PROSPERO (registration number: CRD42021227165).
Literature search and screening
We conducted a systematic literature search in MEDLINE and EMBASE databases (both through the OVID interface) from inception to December 1, 2020 to identify all relevant studies. No restrictions were applied for the literature searches. The detailed search syntax is presented in Supplementary Table S1. Title, abstract and full text were screened independently by two authors (L.Y. and G.Z.) based on the inclusion and exclusion criteria. Any disagreement was discussed with a senior investigator (L.W.). We also cross-checked the reference list of each eligible article for any additional studies.
Inclusion criteria
Studies were eligible for inclusion if they met the following predefined criteria: (i) observational studies exploring the associations between microbiota and colorectal neoplasia in population-based settings; (ii) studies developing or validating prediction models for colorectal neoplasia detection or prognostication (i.e., metastasis, recurrence or survival) using microbiota-related biomarkers. The exclusion criteria were as follows: (i) studies with very small sample size (n < 10) were excluded due to limited statistical power and low reliability of study findings; (ii) studies published in letter or abstract forms or with no full text available were excluded as they did not include enough data for our review; (iii) studies that investigated the efficiency of probiotics or therapeutic procedures of CRC or adenoma and prediction studies in which microbiome was not included as a predictor were excluded; (iv) animal, in vitro, and in vivo experiments were all excluded. When more than one study was conducted using the same sequencing data, we chose the study with the most comprehensive information.
Data extraction
For each included observational study, the following items were extracted: year of publication, study design, number of cases and controls, reason for colonoscopy, sample collection, antibiotic use prior to stool sample, microbiome detection method, database used for taxonomy assignment, storage temperature, microbial markers, and clinical outcome (incidence, prognosis, overall survival).
Quality assessment
The quality of observational studies was evaluated by using the Newcastle-Ottawa Scale (NOS) [19], which is designed to assess the quality of case-control studies. For risk prediction studies, we appraised each model using the checklist for critical appraisal and data extraction of systematic reviews of prediction modelling studies (CHARMS) [20]. According to this checklist, the risk of bias for each model was assessed following the criteria, which included five domains: participant selection, measurement and reporting of predictors, definition and measurement of the outcome, attrition (loss to follow-up), data analysis. For each domain, risk of bias was classified as ‘low’ if bias was unlikely, as ‘moderate’ if the criteria for low risk were not satisfied but no fatal flaws were present, or as ‘high’ if critical flaws were identified. Owning to the extensive heterogeneities among included studies, we did not conduct any quantitative analysis. Instead, we performed descriptive syntheses and reported the results narratively and thematically.
Results
Literature review and study characteristics
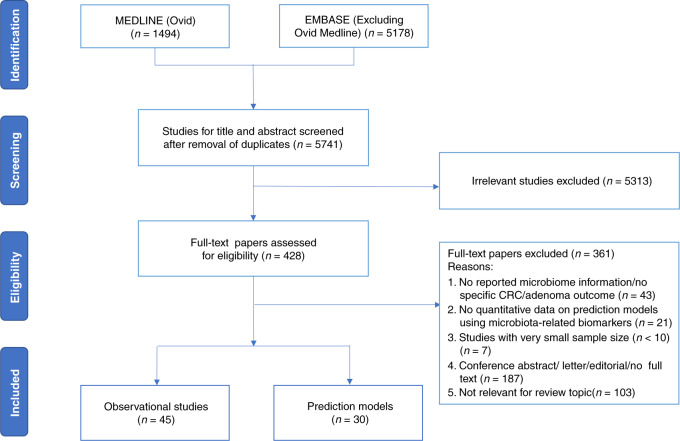
Overall, the literature search retrieved 5741 unique publications across the two databases. After parallel review, a total of 45 eligible observational studies [9, 15, 21–63] exploring the associations between microbiota and colorectal neoplasia risk in population screening settings and 30 studies [15, 29, 46, 50, 53, 54, 58, 59, 64–85] developing or validating prediction models for colorectal neoplasia detection or prognostication using microbial biomarkers were included. The detailed process of study selection is documented in Fig. 1. The characteristics of included studies are presented in Table 1 and Supplementary Table S2.
Fig. 1. PRISMA diagram.
Flowchart of the selection of studies.
Table 1.
Summarized characteristics of 45 eligible observational studies.
| Characteristics | Number of studies (%) |
|---|---|
| Participant region | |
| Europe | 10 (22.2) |
| Asia | 26 (57.8) |
| America | 8 (17.8) |
| Other | 1 (2.2) |
| Study design | |
| Prospective study | 20 (44.4) |
| Retrospective study | 25 (55.6) |
| Outcome | |
| Diagnosis | 36 (80.0) |
| Metastasis | 5 (11.1) |
| Survival | 4 (8.9) |
| Reason for colonoscopy | |
| Routine screening | 26 (57.8) |
| qFIT/gFOBT positive | 5 (11.1) |
| Symptoms + Screening | 5 (11.1) |
| Patients recruited at hospital | 9 (20.0) |
| Antibiotic use prior to sample | |
| Not in 1–4 weeks | 7 (15.6) |
| Not in 4–24 weeks | 18 (40.0) |
| At the time of baseline assessment | 3 (6.7) |
| Not mention | 17 (37.7) |
| Sample collection | |
| Faecal samples | 36 (70.0) |
| Tissue samples | 6 (13.3) |
| Oral samples | 1 (2.2) |
| Blood samples | 2 (4.4) |
| Database used for taxonomy assignment | |
| RDP | 15 (33.3) |
| Silva | 6 (13.3) |
| Greengenes | 5 (11.1) |
| Other | 5 (11.1) |
| Not mention | 14 (31.2) |
Microbiota markers related to colorectal neoplasia
There were 36 studies [15, 21–41, 46–54, 58–62] examining the microbiota differences for colorectal neoplasia risk, five [42, 43, 55, 56, 63] for CRC metastasis and four [9, 44, 45, 57] for CRC survival. Quality assessment using the NOS criteria classified 6.6% of included studies as low quality (NOS score: 0-5), 35.6% as moderate quality (NOS score: 6–7) and 57.8% as high quality (NOS score: 8–9). More details of the NOS assessment are presented in Supplementary Table S3.
We summarised the faecal microbial markers which were reported to be significantly different in abundance between case and control groups in at least two studies, and the results are presented in Table 2. Overall, bacteria from 18 genera belonging to five different phyla have been examined for their associations with colorectal neoplasia. At genus or species level, Fusobacterium (e.g., Fusobacterium nucleatum), Porphyromonas (e.g., Porphyromonas asaccharolytica), Peptostreptococcus (e.g., Peptostreptococcus stomatis) and Actinomyces were reported to be more abundant in CRC patients than healthy individuals in prospective studies [15, 22, 23, 25, 26, 29, 34, 36, 50, 52–54, 58, 59, 67, 75], and Enterococcus (e.g., Enterococcus faecalis), Salmonella (e.g., Escherichia coli) were reported in retrospective studies [27, 46, 49]. Bifidobacterium and Roseburia (e.g., Roseburia faecis) were consistently reported to be more abundant in healthy individuals than CRC patients [22, 23, 25, 26, 38, 39, 48, 51, 61, 62]. When comparing adenoma patients and healthy controls, Fusobacterium (e.g., Fusobacterium nucleatum) was consistently reported to be more abundant in adenoma patients with supporting evidence from at least two prospective studies [30, 58, 77, 81]. Conflicting evidence was reported for other identified microbial markers, including Bacteroides, Prevotella, Lactobacillus, Ruminococcus, Faecalibacterium, Clostridium, Streptococcus, Phascolarctobacterium and Salmonella.
Table 2.
Bacteria found in significantly different abundance in CRC, adenomas and controls in at least two studies.
| Bacteria taxonomic level | Reported to be more abundant in: | |||||
|---|---|---|---|---|---|---|
| Phylum | Order/Famliy | Genus | Species | CRC | Adenomas | Controls |
| Actinobacteria | [24] | [35] | [31] | |||
| Bifidobacteriaceae | Bifidobacterium | [22, 38, 39, 48, 61, 62] | ||||
| [Actinomycetaceae] | Actinomyces | [34, 36] | [35] | |||
| [Coriobacteriaceae] | Atopobium | [34] | [36] | |||
| Eggerthella lenta | [25, 51] | |||||
| Bacteroidetes | [21, 24, 26, 48, 49] | [31, 37] | [24, 26, 37, 47] | |||
| Porphyromonadaceae | Porphyromonas | [22, 26, 29] | [39] | |||
| Porphyromonas asaccharolytica | [15, 25, 50, 59] | |||||
| [Bacteroidaceae] | Bacteroides | [28, 29] | [23, 26] | |||
| Bacteroides fragilis | [34] | [30, 39] | [61] | |||
| [Prevotellaceae] | Prevotella | [28] | [23] | |||
| Firmicutes | [26, 29, 48] | [35] | [21, 24, 26, 31, 35, 37, 47] | |||
| Ruminococcaceae | Ruminococcus | [23, 38] | [29] | [48] | ||
| Faecalibacterium | Faecalibacterium prausnitzii | [43] | [69] | |||
| [Clostridiaceae] | Clostridium | [23] | [29] | |||
| Clostridium symbiosum | [52, 58, 69] | [58] | ||||
| Streptococcaceae | Streptococcus | [23, 26] | [35] | [24, 48] | ||
| [Lachnospiraceae] | Coprococcus | [50] | [53] | [53] | ||
| Lactobacillus | [28] | [39] | ||||
| Roseburia | [23, 26, 39] | |||||
| Roseburia faecis | [25, 51] | |||||
| [Enterococcaceae] | Enterococcus | [26, 32] | ||||
| Enterococcus faecalis | [46] | [30, 77] | ||||
| [Peptostreptococcaceae] | Peptostreptococcus | [22, 23, 26, 36] | ||||
| Peptostreptococcus stomatis | [15, 34, 52, 59] | |||||
| [Acidaminococcaceae] | Phascolarctobacterium | [29] | [35] | [38] | ||
| Fusobacteria | [29, 35, 38] | |||||
| [Fusobacteriaceae] | Fusobacterium | [22, 23, 32, 34, 36, 50, 54, 67] | [36] | |||
| Fusobacterium nucleatum | [15, 34, 43, 52–54, 58, 59, 75, 79] | [30, 58, 77, 81] | ||||
| Tenericutes | [26] | [35] | [35] | |||
| Alcaligenaceae | [22, 35] | [27] | ||||
| Enterobacteriaceae | Salmonella | [27, 46] | [36] | |||
| Escherichia coli | [43, 49] | |||||
| [Pseudomonadaceae] | Pseudomonas | [61] | [29] | |||
Bacteria in square brackets were not reported on this level and are there for reference.
The number represents the corresponding order of the sited reference in the manuscript.
We identified three studies looking for microbial markers related to colorectal neoplasia beyond faecal microbiota [24, 27, 33]. There were two population-based studies assessing the association of bacterial antibody levels with CRC risk in blood samples [27, 33]. In a prospective setting, a serological study demonstrated a positive association between antibody responses to Streptococcus gallolyticus subspecies gallolyticus (SGG) proteins and CRC risk using pre-diagnostic blood samples [33]. Another study found serum Salmonella antiflagellin antibody levels to be significantly higher in CRC cases and in all cases combined (CRC + polyps) comparing to controls without polyps [27]. Using oral rinse samples, a prospective study investigated the oral microbiome and found two oral pathogens, Treponema denticola and Prevotella intermedia, to be associated with subsequent risk of CRC [24].
Associations between microbial markers and CRC prognosis (e.g., metastasis and survival) were examined in nine studies [9, 42–45, 55–57, 63]. At genus or species levels, Fusobacterium nucleatum and Bacteroides fragilis were consistently reported to be associated with CRC metastasis [43, 56]. When comparing the differentially enriched microbial markers related to CRC survival, genera Bacteroides and Fusobacterium were consistently reported to be more abundant in CRC patients with poor survival outcomes [9, 44, 45, 57].
Multi-bacteria models for detection of colorectal neoplasia
For prediction models, 30 articles were identified describing 57 models, including seven external validation studies [50, 53, 66, 70, 71, 73, 74]. The detailed criteria and scores on risks of bias for each domain are presented in Supplementary Table S4–5 and Supplementary results. A summary of the study characteristics is presented in Table 3.
Table 3.
Multi-bacteria models for detection of colorectal cancer and adenomas.
| Author, year | Predictors | Sample examined (CRC/Adenomas/Controls) | Performance of AUROCs (CI) | Internal validation | External validation |
|---|---|---|---|---|---|
| Diagnosis/CRC vs HC | |||||
| Amitay, 2017 Germany | Fusobacterium nucleatum | 46/223/231 | 0.67 (0.59–0.76) | ||
| Fusobacterium nucleatum + age + sex | 46/223/231 | 0.75 (0.68–0.83) | |||
| Baxter, 2016 Canada + USA | 32 OTUs | 101/162/141 | 0.85 | ||
| 28 OTUs + qFIT | 101/162/141 | 0.83 | |||
| Gao, 2020 China | 18 genera | 100/110/332 | 0.86 (0.78–0.93) | Validation cohort | |
| 18 genera + qFIT | 100/110/332 | 0.99 (0.98–1.00) | |||
| Zackular, 2014 USA | 6 OTUs | 30/30/30 | 0.80 (0.69–0.91) | ||
| 6OTUs + age + race + BMI | 30/30/30 | 0.92 (0.86–0.99) | |||
| Coker, 2020 China | 9 species | 73/NA/92 | 0.82 (0.70–0.94) | Chinese Cohort C2 | |
| Alomair, 2018 Saudi Arabia | 11 genera | 29/NA/29 | 0.89 | ||
| Zhang, 2020 China | 5 oral microbiome OTUs | 161/NA/58 | 0.84 (0.77–0.90) | ||
| Arabameri, 2018 France | 22 species | 53/27/61 | 0.91 | American cohort & Austrian cohort | |
| 22 species + gFOBT | 53/27/61 | 0.92 | |||
| Liang, 2019 China | Fusobacterium nucleatum | 170/NA/200 | 0.87 (0.83–0.90) | Shanghai cohort II | |
| Fusobacterium nucleatum + qFIT | 170/NA/200 | 0.92 (0.82–0.96) | |||
| 4 bacteria | 170/NA/200 | 0.89 (0.85–0.92) | |||
| Baxter, 2016 Canada + USA | 34 OTUs | 120/198/172 | 0.85 | ||
| 23 OTUs + qFIT | 120/198/172 | 0.95 | |||
| Guo, 2018 China | Fusobacterium nucleatum | 215/NA/156 | 0.88 | Cohort II | |
| Fn/Fp+Fn/Bb | 215/NA/156 | 0.94 | |||
| Tarallo, 2019 Italy | bsRNA + bDNA + hsa-miRNAs | 29/27/24 | 0.87 | ||
| Flemer, 2017 Ireland | 16 faecal microbiota OTUs | 99/32/103 | 0.81 (0.73–0.81) | ||
| 16 oral microbiota OTUs | 99/32/103 | 0.90 (0.83–0.90) | |||
| 29 oral OTUs + 34 fecal OTUs | 99/32/103 | 0.94 (0.87–0.94) | |||
| Ai, 2017 China | 6 species | 42/47/52 | 0.94 | ||
| 6 species + gFOBT | 42/47/52 | 0.95 | French cohort | ||
| Ai, 2019 China | 9 genera | 53/42/61 | 0.93 | French cohort & Austria cohort | |
| Yachida, 2019 Japan | 29 species | 365/NA/251 | 0.73* | ||
| 55 species | 365/NA/251 | 0.83 | |||
| Zeller, 2014 France | 22 species | 53/42/61 | 0.84* | Denmark cohort & Spain cohort & Germany cohort | |
| 22 species + gFOBT | 53/42/61 | 0.87* | |||
| Kim, 2020 Korea | Collinsella + Solanum melongena | 32/NA/40 | 0.95 | ||
| Collinsella + Solanum melongena + leucine + oxalic acid | 32/NA/40 | 1.00 | |||
| Guven, 2019 Belgium | Streptococcus gallolyticus | 71/NA/77 | 0.84 (0.72–0.96) | ||
| Yu, 2017 China | 20 microbial gene markers | 74/NA/54 | 0.71 | Chinese Cohort C2 | Danish cohort & French cohort & Austrain cohort |
| Liang, 2020 China | 4 genera | 13/NA/22 | 0.83 | ||
| Shen, 2020 China | Firmicutes cluster1 (IVF group) | 30/NA/25 | 0.93 | ||
| Fusobacteria cluster | 30/NA/25 | 0.94 | |||
| Xie, 2017 China | Clostridium symbiosum + qFIT | 327/212/242 | 0.84* (0.77–0.89) | ||
| Clostridium symbiosum + Fusobacteria nucleatum + qFIT + CEA | 327/212/242 | 0.86* (0.79–0.91) | |||
| Clostridium symbiosum + Fusobacteria nucleatum + qFIT + CEA | 327/212/242 | 0.90 (0.87–0.93) | |||
| Wang, 2016 China | Fusobacterium nucleatum + CEA | 258/NA/200 | 0.85 | ||
| Diagnosis/Adenomas vs HC | |||||
| Gao, 2020 China | 18 genera | 100/110/332 | 0.62 (0.52–0.71) | Validation cohort | |
| 18 genera + qFIT | 100/110/332 | 0.72 (0.63–0.81) | |||
| Zackular, 2014 USA | 5 OTUs | 30/30/30 | 0.84 (0.74–0.94) | ||
| 5 OTUs + age + race + BMI | 30/30/30 | 0.90 (0.82–0.98) | |||
| Flemer, 2017 Ireland | 12 oral microbiota OTUs | 99/32/103 | 0.89 (0.80–0.89) | ||
| 12 oral OTUs + 16 faecal OTUs | 99/32/103 | 0.98 (0.95–0.98) | |||
| Baxter, 2016 Canada + USA | 22 OTUs | 120/198/172 | 0.67 | ||
| 23 OTUs + qFIT | 120/198/172 | 0.76 | |||
| Liu, 2020 China | Escherichia-Shigella + Acinetobacter | NA/22/19 | 0.81 | Validation cohort | |
| Escherichia-Shigella + Acinetobacter + BMI | NA/22/19 | 0.94 | |||
| Tarallo, 2019 Italy | bsRNA + bDNA + hsa-miRNAs | 29/27/24 | 0.47 | ||
| Zhang, 2020 China | 5 oral microbiome OTUs | NA/34/58 | 0.95 (0.91–0.99) | ||
| Goedert, 2015 China | 5 phyla + 7 genera | 2/20/24 | 0.77 | ||
| Wei, 2020 China | 2 species | 36/43/53 | 0.79 | ||
| Fusobacterium mortiferum + gFOBT | 36/43/53 | 0.47 | |||
| Prognostication | |||||
| Jin, 2019 China | 10 species | 161/NA/NA | 0.72 (0.59–0.88) | ||
| Li, 2019 China | 3 species | 37/NA/NA | 0.82 (0.69–0.96) | ||
| 3 species + age | 37/NA/NA | 0.91 (0.81–1.00) | |||
| Yu, 2019 China | 3 genera | 20/NA/NA | 0.79 (0.63–0.90) | ||
qFIT quantitative faecal immunochemical test, gFOBT guaiac faecal occult blood test, OTUs operational taxonomic units, AUROC area under the receiver operating characteristic curve, BMI body mass index, IVF intestinal lavage fluid, Fn Fusobacterium nucleatum, Fp Faecalibacterium prausnitzii, Bb Bifidobacterium.
*Early-stage detection of Colorectal Cancer.
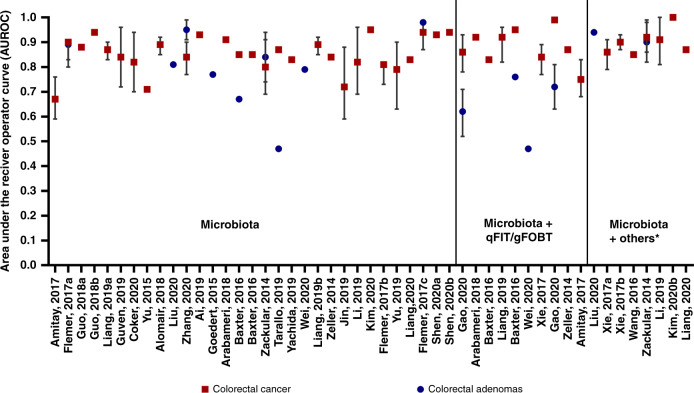
For CRC risk, prediction models were developed using different bacteria at different taxonomy levels, and discriminatory ability varied largely based on multiple markers. Five preditive [53, 54, 69, 74, 80] models including a single microbial marker achieved an AUROC ranging between 0.67–0.94. There were three studies [53, 54, 74] using single bacterium, Fusobacterium nucleatum, to distinguish CRC and healthy controls, reporting an AUROC of 0.87 (95%CI: 0.83–0.90), 0.67 and 0.88, respectively. In contrast, models using multiple bacterial species had relatively better performance as shown in Fig. 2. There were eight [15, 50, 53, 58, 59, 65, 71, 73] studies that combined faecal microbial markers plus qFIT/ guaiac faecal occult blood test (gFOBT) test result for CRC prediction. Generally, faecal microbial markers were shown to strengthen the accuracy of qFIT/gFOBT and improved the sensitivity and specificity of CRC prediction [50, 53, 59, 65, 71]. In addition, there was one study utilising Clostridium symbiosum and Fusobacteria nucleatum in combination with CEA, which achieved a good performance of 0.90 (95%CI: 0.87–0.93) for CRC discrimination [58].
Fig. 2. Model discrimination.
Relative discriminative performance of the AUROCs (Area under the receiver operator curves) ordered by number of variables included. (*: age, BMI, race, CEA).
Table 3 presents eight models based on multiple microbial markers to distinguish adenomas from healthy controls. Gao et al. [65] used only 18 different faecal genera and reported an AUROC of 0.86 (95%CI: 0.78–0.93) for CRC and 0.62 (95%CI: 0.52–0.71) for adenomas. Baxter et al. [15] developed two models, one containing 22 OTUs only and the other combining the OTUs with qFIT, and reported an AUROC of 0.67 and 0.76 for adenomas, respectively. Although combining microbial markers and qFIT improved the model performance, these models still had a lower sensitivity and specificity for adenoma prediction.
For prognostication of CRC, we identified three prediction studies [82–84]. One study by Li et al. [83] used three microbial markers to predict the anastomosis healing status in patients after CRC radical resection and reported an AUROC of 0.82 (95%CI: 0.69–0.96) for distinguishing the CRC patients that healed well compared to those that did not. Furthermore, there were two studies focusing on microbial prediction of adenomas recurrence in postoperative CRC patients. In one study [84], the microbiota signature of Parabacteroides, Streptococcus, and Ruminococcus showed an optimal discriminating performance of postoperative status with AUROC of 0.79 (95%CI: 0.63–0.90). Another study using 10 different species as predictors achieved an AUROC value of 0.72 (95%CI: 0.59–0.88) to distinguish postoperative patients with or without newly developed adenomas [82]. These results indicated that microbial makers may be clinically predictive for the prognostication of colorectal neoplasia.
Evidence was obtained by seven studies using external validation of multiple microbial models predicting colorectal neoplasia [50, 53, 66, 70, 71, 73, 74]. The model by Guo et al. which included three species markers reported an AUROC of 0.94 in a Chinese test population of 371 samples, and the same model was successfully validated in another independent Chinese cohort with an AUROC of 0.96 [74]. The prediction models developed by other five studies showed relatively lower discrimination in external validation populations. For instance, Arabameri et al. [73] used faecal metagenomes from 141 individuals attending routine CRC screening in a French cohort with an AUROC of 0.91, and the model was validated in independent American and Austrian cohorts, with lower AUROC values of 0.81 and 0.85, respectively. Liang et al. developed two models, one containing the Fusobacterium nucleatum and the other a combination of four bacteria, reporting AUROCs of 0.87 (95%CI: 0.83–0.90) and 0.89 (95%CI: 0.85–0.92), and received lower AUROCs of 0.68 (95%CI: 0.55–0.80) and 0.76 (95%CI: 0.64–0.87) in a smaller Chinese cohort that was used for external validation [53].
When comparing to microbial markers reported in association studies, four of the 18 genera, namely Fusobacterium (e.g., Fusobacterium nucleatum), Peptostreptococcus (e.g., Peptostreptococcus stomatis), Porphyromonas (e.g., Porphyromonas asaccharolytica) and Clostridium (Clostridium symbiosum), were commonly used predictors in prediction studies. Meanwhile, the Fusobacterium genus was also the most frequently used marker in CRC prognostic models.
Discussion
In total, 45 association studies and 30 prediction studies were included in this systematic review. The included studies followed different protocols in terms of study population selection, sample collection and storage, microbiome sequencing, and databases used for taxonomy assignment. A large number of parameters were used to describe the composition of microbiome at different taxonomic levels, making it difficult to synthesise studies using meta-analysis. We, therefore, systematically reviewed the methodology and results of the included studies and summarised the microbial markers associated with colorectal neoplasia and their application for the risk prediction.
Multiple-site microbiome for detection of colorectal neoplasia
We found seven faecal microbiota markers (e.g., Fusobacterium, Enterococcus, Porphyromonas, Salmonella, Pseudomonas, Peptostreptococcus and Actinomyces) at genus level that were consistently reported to be enriched in CRC patients, while two faecal microbial markers (Bifidobacterium and Roseburia) were consistently reported to be enriched in healthy controls. The reported bacterial differences between adenoma patients and healthy controls were not as consistent as with CRC. Of these, only Fusobacterium (e.g., Fusobacterium nucleatum) and Pseudomonas were consistently reported to be enriched in adenoma patients, indicating that these two bacteria species exhibited a progressive increase in abundance across the early to late stages of carcinogenesis. Apart from the faecal microbiome, there were also studies investigating IgG, indicating that serum antibody levels response to these specific bacteria were associated with CRC. Multiple studies indicated that CRC patients had higher levels of antibodies against Fusobacterium nucleatum when compared to healthy controls [85]. Furthermore, a positive association of CRC with serum antibody responses to SGG was observed in a nested case-control study, indicating CRC-related microbiota might induce specific humoral antibody and multiplex serology tests might be a new potential way for CRC detection. Oral microbiome composition was also investigated in related to CRC risk. Two oral pathogens, Treponema denticola and Prevotella intermedia, were associated with subsequent CRC risk. Findings from these studies implicated easier ways to obtain microbial markers related to CRC risk. In addition, these results raise the possibility that the oral microbiome may play an important role in CRC aetiology supporting the theory that the inflammation in gut could be driven by oral microbiota. Further studies with larger sample size are needed to confirm the identified associations and estimate the potential utilisation of the oral microbiota for CRC early detection or prevention.
Microbiome for prognostication of colorectal neoplasia
Apart from their potential for CRC diagnosis, associations identified between gut microbiota and clinical outcomes of CRC have raised the possibility of using them as prognostic markers. A number of studies have shown that Fusobacterium nucleatum and Bacteroides fragilis are associated with CRC prognosis, and the increased abundance of these two species indicates poor survival outcome for CRC patients [9, 44]. These findings highlight the potential of quantifying Fusobacterium nucleatum and Bacteroides fragilis in tumour tissue as prognostic markers, and indicate that reducing the abundance of these bacteria might improve prognosis and survival. Nevertheless, it should be noted that their association with prognostication could be confounded by other factors like clinicopathological parameters (e.g., TNM stage), and more validation studies are needed before these biomarkers could be used in the clinical context.
Diagnosis and prognostication of colorectal neoplasia prediction
Findings from observational studies pinpoint a potential core set of bacteria that could be used as predictive biomarkers for the detection of colorectal neoplasia. Thirty studies developed microbial prediction models for colorectal neoplasia. Faecal microbiome analysis discerned patients with CRC with varying levels of accuracy (with AUROC ranging from 0.71 to 0.95 in validation studies), but only seven of the identified models were validated in external populations. Several studies have utilised multiple bacterial species to distinguish CRC patients from healthy individuals, including three prospective studies [59, 74, 77] with large sample size (n > 300) achieving AUROCs of 0.85–0.94. The AUROCs reported in multiple predictor models for adenomas detection were lower than those for CRC discrimination. Combining the faecal microbiome data with other risk factors or results of screening qFIT/gFOBT tests increased the accuracy of discrimination for both CRC and adenomas. For instance, addition of faecal microbiota OTUs to qFIT or gFOBT testing improved the sensitivity for detection of CRC and advanced adenomas [15]. Findings from these predictive models indicated microbial markers have the potential to complement established tests such as gFOBT or qFIT as a non-invasive early detection tool for CRC and its precursors.
Synthesis of results and limitations
The absence of a gold-standard unified protocol leads to great heterogeneity in study design and methodology, which limits the validity, generalizability and comparability of results reported in the included studies. The main sources of bias stemmed from methodological limitations in study population selection, sample collection and data analysis. Several recent studies indicate that there are significant variations in the gut microbiome due to differences in ethnicity, geographic location, lifestyle, nutrition, and medication use across study populations [86–89]. The “core microbiota” could be influenced by the gut environment (e.g., intestinal immune system) and colorectal neoplasia may influence the microbial community composition in reverse [90], therefore, we could not infer a causal association between identified microbiota and colorectal neoplasia based on the current evidence. It is thought that the organization of bacterial communities into biofilms (higher-order spatial structures of bacterial species) may be necessary for bacteria-induced CRC initiation [91, 92]. A previous study by Li et al. demonstrated that poly-microbial biofilms might promote pro-carcinogenic activities that may partially underlie progression along the adenoma-CRC sequence [93]. Oral antibiotics may affect the microbiome composition [94], possibly leading to chronic inflammation and tumour progression [95, 96], and the pattern of use, formulations and dosages of the drugs may have changed over time, complicating the interpretation of results. Seventeen studies did not address antibiotics taken by the participants, and three studies only excluded participants taking antibiotics at the time of recruitment which did not give enough time for the gut microbial community to return to its normal composition. Only one study was based on a population-wide CRC screening programme using fresh stool samples collected within days for microbiome analysis [61]. The majority of included studies used frozen stool sample, which were stored for a few years before analysis, where collection methods, storage temperatures and duration before analysis of faecal samples varied widely and may have a differentiating effect on the results of microbiome analysis. Sex hormones status especially oestrogen receptor beta may be another factor affecting incidence and mortality of CRC [97, 98]. However, observational studies included in this systematic review did not report the association between microbiome and colorectal neoplasia by sex, and therefore we were unable to examine any sex differences. Additionally, the included studies used three different reference databases (i.e., Silva, Ribosomal Database Project (RDP), and Greengenes database) for taxonomic assignments, which may affect the accuracy and resolution of their findings.
The identified prediction studies used different microbial features to construct their models. It is unclear to what extent the heterogeneity among studies reflects the true differences in the ability to detect CRC based on different microbial patterns or whether it reflects variations in the technical aspects of studies. It should also be noted that prediction models developed from case-control studies were not validated externally in prospective studies. Limitations identified through the quality assessment of the included studies require cautious interpretation of the reported findings.
Conclusions
In summary, this systematic review provided a comprehensive overview of the microbial markers from multiple sites (faecal, oral and blood) for their associations with the risk of colorectal neoplasia, and summarised the evidence for applying these markers for colorectal neoplasia risk prediction and prognostication. Based on the currently published data, there is encouraging evidence that microbial markers from faecal, oral or blood specimens may be used to develop new, non-invasive and inexpensive tests that could complement the repertoire of current non-invasive CRC screening tools on their own or in combination with qFIT or gFOBT screening tests. However, current prediction models are mostly developed from case-control studies, which require further external validation in high-quality prospective studies. Future research should focus on developing unified documented and reproducible protocols for studying the human gut microbiome so that results can be more comparable and conclusions can be drawn on a larger basis. Other practical issues must be evaluated before microbiome analysis can be used in CRC screening, such as determination of cost effectiveness, affordability, and acceptability by patients and physicians, compared with established screening strategies. Collectively, these research advances have provided an unprecedented opportunity to move microbiota discoveries towards clinical applications, including prevention and treatment.
Supplementary information
Acknowledgements
Not applicable.
Author contributions
Lili Yu: Conceptualization, literature review, data extraction, writing-original draft. Gang Zhao: Conceptualization, data extraction, writing-review & editing. Xinxuan Li: Literature review, data extraction, writing-review & editing. Kleovoulos Kofonikolas: Literature review, data extraction. Xuan Zhou: Data extraction. Lijuan Wang: Data extraction. Yeting Hu: Data extraction. Yingshuang Zhu: Data extraction. Evropi Theodoratou: Conceptualization, supervision, writing-review & editing. Xue Li: Conceptualization, supervision, writing-review & editing. All authors read and approved the final submitted manuscript, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding information
XL is supported by the Natural Science Fund for Distinguished Young Scholars of Zhejiang Province (LR22H260001); ET is supported by a CRUK Career Development Fellowship (C31250/A22804); YSZ is supported by the National Natural Science Foundation of China (No. 82103905).
Data availability
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics approval and consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Lili Yu, Gang Zhao.
These authors jointly supervised this work: Evropi Theodoratou, Xue Li.
Supplementary information
The online version contains supplementary material available at 10.1038/s41416-022-01740-7.
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.White A, Ironmonger L, Steele RJC, Ormiston-Smith N, Crawford C, Seims A. A review of sex-related differences in colorectal cancer incidence, screening uptake, routes to diagnosis, cancer stage and survival in the UK. BMC Cancer. 2018;18:906. doi: 10.1186/s12885-018-4786-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koo JH, Leong RW. Sex differences in epidemiological, clinical and pathological characteristics of colorectal cancer. J Gastroenterol Hepatol. 2010;25:33–42. doi: 10.1111/j.1440-1746.2009.05992.x. [DOI] [PubMed] [Google Scholar]
- 4.Topi G, Ehrnström R, Jirström K, Palmquist I, Lydrup ML, Sjölander A. Association of the oestrogen receptor beta with hormone status and prognosis in a cohort of female patients with colorectal cancer. Eur J Cancer. 2017;83:279–89. doi: 10.1016/j.ejca.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Nakatsu G, Li X, Zhou H, Sheng J, Wong SH, Wu WK, et al. Gut mucosal microbiome across stages of colorectal carcinogenesis. Nat Commun. 2015;6:8727. doi: 10.1038/ncomms9727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Narayanan V, Peppelenbosch MP, Konstantinov SR. Human fecal microbiome-based biomarkers for colorectal cancer. Cancer Prev Res (Philos) 2014;7:1108–11. doi: 10.1158/1940-6207.CAPR-14-0273. [DOI] [PubMed] [Google Scholar]
- 7.Castellarin M, Warren RL, Freeman JD, Dreolini L, Krzywinski M, Strauss J, et al. Fusobacterium nucleatum infection is prevalent in human colorectal carcinoma. Genome Res. 2012;22:299–306. doi: 10.1101/gr.126516.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bruno G, Zaccari P, Rocco G, Scalese G, Panetta C, Porowska B, et al. Proton pump inhibitors and dysbiosis: Current knowledge and aspects to be clarified. World J Gastroenterol. 2019;25:2706–19. doi: 10.3748/wjg.v25.i22.2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mima K, Nishihara R, Qian ZR, Cao Y, Sukawa Y, Nowak JA, et al. Fusobacterium nucleatum in colorectal carcinoma tissue and patient prognosis. Gut. 2016;65:1973–80. doi: 10.1136/gutjnl-2015-310101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haruki K, Kosumi K, Hamada T, Twombly TS, Väyrynen JP, Kim SA, et al. Association of autophagy status with amount of Fusobacterium nucleatum in colorectal cancer. J Pathol. 2020;250:397–408. doi: 10.1002/path.5381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Viaud S, Saccheri F, Mignot G, Yamazaki T, Daillère R, Hannani D, et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science. 2013;342:971–6. doi: 10.1126/science.1240537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerassy-Vainberg S, Blatt A, Danin-Poleg Y, Gershovich K, Sabo E, Nevelsky A, et al. Radiation induces proinflammatory dysbiosis: transmission of inflammatory susceptibility by host cytokine induction. Gut. 2018;67:97–107. doi: 10.1136/gutjnl-2017-313789. [DOI] [PubMed] [Google Scholar]
- 13.Toes-Zoutendijk E, Bonfrer JMG, Ramakers C, Thelen M, Spaander MCW, Dekker E, et al. Quality Monitoring of a FIT-Based Colorectal Cancer Screening Program. Clin Chem. 2019;65:419–26. doi: 10.1373/clinchem.2018.294041. [DOI] [PubMed] [Google Scholar]
- 14.Schloissnig S, Arumugam M, Sunagawa S, Mitreva M, Tap J, Zhu A, et al. Genomic variation landscape of the human gut microbiome. Nature. 2013;493:45–50. doi: 10.1038/nature11711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baxter NT, Ruffin MTT, Rogers MA, Schloss PD. Microbiota-based model improves the sensitivity of fecal immunochemical test for detecting colonic lesions. Genome Med. 2016;8:37. doi: 10.1186/s13073-016-0290-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Komor MA, Bosch LJ, Coupé VM, Rausch C, Pham TV, Piersma SR, et al. Proteins in stool as biomarkers for non-invasive detection of colorectal adenomas with high risk of progression. J Pathol. 2020;250:288–98. doi: 10.1002/path.5369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mariño-Crespo Ó, Cuevas-Álvarez E, Harding AL, Murdoch C, Fernández-Briera A, Gil-Martín E. Haptoglobin expression in human colorectal cancer. Histol Histopathol. 2019;34:953–63. doi: 10.14670/HH-18-100. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 20.Moons KG, de Groot JA, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. 2014;11:e1001744. doi: 10.1371/journal.pmed.1001744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen J, Hu S, Ji D, Gao Z, Wang H, Yang Y, et al. Hemolysin BL from novel Bacillus toyonensis BV-17 induces antitumor activity both in vitro and in vivo. Gut Microbes. 2020; 10.1080/19490976.2020.1782158:1-15. [DOI] [PMC free article] [PubMed]
- 22.Chen W, Liu F, Ling Z, Tong X, Xiang C. Human intestinal lumen and mucosa-associated microbiota in patients with colorectal cancer. PLoS ONE. 2012;7:e39743. [DOI] [PMC free article] [PubMed]
- 23.Wang X, Wang J, Rao B, Deng LI. Gut flora profiling and fecal metabolite composition of colorectal cancer patients and healthy individuals. Exp Therapeutic Med. 2017;13:2848–54. doi: 10.3892/etm.2017.4367. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Yang Y, Cai Q, Shu XO, Steinwandel MD, Blot WJ, Zheng W, et al. Prospective study of oral microbiome and colorectal cancer risk in low-income and African American populations. Int J Cancer. 2019;144:2381–9. doi: 10.1002/ijc.31941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y, Yu X, Yu E, Wang N, Cai Q, Shuai Q, et al. Changes in gut microbiota and plasma inflammatory factors across the stages of colorectal tumorigenesis: A case-control study. BMC Microbiol. 2018;18:92. [DOI] [PMC free article] [PubMed]
- 26.Wang T, Cai G, Qiu Y, Fei N, Zhang M, Pang X, et al. Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 2012;6:320–9. doi: 10.1038/ismej.2011.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kato I, Boleij A, Kortman GAM, Roelofs R, Djuric Z, Severson RK, et al. Partial associations of dietary iron, smoking and intestinal bacteria with colorectal cancer risk. Nutr Cancer. 2013;65:169–77. doi: 10.1080/01635581.2013.748922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sobhani I, Tap J, Roudot-Thoraval F, Roperch JP, Letulle S, Langella P, et al. Microbial dysbiosis in colorectal cancer (CRC) patients. PLoS ONE [Electron Resour] 2011;6:e16393. doi: 10.1371/journal.pone.0016393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zackular JP, Rogers MA, Ruffin MTT, Schloss PD. The human gut microbiome as a screening tool for colorectal cancer. Cancer Prev. Res. 2014;7:1112–21. doi: 10.1158/1940-6207.CAPR-14-0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rezasoltani S, Asadzadeh Aghdaei H, Dabiri H, Akhavan Sepahi A, Modarressi MH, Nazemalhosseini Mojarad E. The association between fecal microbiota and different types of colorectal polyp as precursors of colorectal cancer. Microb Pathog. 2018;124:244–9. doi: 10.1016/j.micpath.2018.08.035. [DOI] [PubMed] [Google Scholar]
- 31.Hale VL, Chen J, Johnson S, Harrington SC, Yab TC, Smyrk TC, et al. Shifts in the fecal microbiota associated with adenomatous polyps. Cancer Epidemiol Biomark Prev. 2017;26:85–94. doi: 10.1158/1055-9965.EPI-16-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang TW, Lee WH, Tu SJ, Huang WC, Chen HM, Sun TH, et al. Enterotype-based analysis of gut microbiota along the conventional adenoma-carcinoma colorectal cancer pathway. Sci Rep. 2019;9:10923. doi: 10.1038/s41598-019-45588-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Butt J, Jenab M, Willhauck-Fleckenstein M, Michel A, Pawlita M, Kyro C, et al. Prospective evaluation of antibody response to Streptococcus gallolyticus and risk of colorectal cancer. Int J Cancer. 2018;143:245–52. doi: 10.1002/ijc.31283. [DOI] [PubMed] [Google Scholar]
- 34.Kasai C, Sugimoto K, Moritani I, Tanaka J, Oya Y, Inoue H, et al. Comparison of human gut microbiota in control subjects and patients with colorectal carcinoma in adenoma: Terminal restriction fragment length polymorphism and next-generation sequencing analyses. Oncol Rep. 2016;35:325–33. doi: 10.3892/or.2015.4398. [DOI] [PubMed] [Google Scholar]
- 35.Peters BA, Dominianni C, Shapiro JA, Church TR, Wu J, Miller G, et al. The gut microbiota in conventional and serrated precursors of colorectal cancer. Microbiome. 2016;4:69. doi: 10.1186/s40168-016-0218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saito K, Koido S, Odamaki T, Kajihara M, Kato K, Horiuchi S, et al. Metagenomic analyses of the gut microbiota associated with colorectal adenoma. PLoS ONE. 2019;14:e0212406. [DOI] [PMC free article] [PubMed]
- 37.Liu W, Zhang R, Shu R, Yu J, Li H, Long H, et al. Study of the relationship between microbiome and colorectal cancer susceptibility using 16SrRNA Sequencing. BioMed Res. Int. 2020;2020:7828392. [DOI] [PMC free article] [PubMed]
- 38.Sarhadi V, Lahti L, Saberi F, Youssef O, Kokkola A, Karla T, et al. Gut microbiota and host gene mutations in colorectal cancer patients and controls of Iranian and finnish origin. Anticancer Res. 2020;40:1325–34. doi: 10.21873/anticanres.14074. [DOI] [PubMed] [Google Scholar]
- 39.Rezasoltani S, Ghanbari R, Looha MA, Mojarad EN, Yadegar A, Stewart D, et al. Expression of main toll-like receptors in patients with different types of colorectal polyps and their relationship with gut microbiota. Int J Mol Sci. 2020;21:1–10. doi: 10.3390/ijms21238968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Geravand M, Fallah P, Yaghoobi MH, Soleimanifar F, Farid M, Zinatizadeh N, et al. Investigation of enterococcus faecalis population in patients with polyp and colorectal cancer in comparison of healthy individuals. Arquivos de Gastroenterologia. 2019;56:141–5. doi: 10.1590/s0004-2803.201900000-28. [DOI] [PubMed] [Google Scholar]
- 41.Zinatizadeh N, Khalili F, Fallah P, Farid M, Geravand M, Yaslianifard S. Potential preventive effect of Lactobacillus acidophilus and Lactobacillus plantarum in patients with polyps or colorectal cancer. Arquivos de Gastroenterologia. 2018;55:407–11. doi: 10.1590/s0004-2803.201800000-87. [DOI] [PubMed] [Google Scholar]
- 42.Wu Y, Shi L, Li Q, Wu J, Peng W, Li H, et al. Microbiota Diversity in Human Colorectal Cancer Tissues Is Associated with Clinicopathological Features. Nutr Cancer. 2019;71:214–22. doi: 10.1080/01635581.2019.1578394. [DOI] [PubMed] [Google Scholar]
- 43.Hale VL, Jeraldo P, Chen J, Mundy M, Yao J, Priya S, et al. Distinct microbes, metabolites, and ecologies define the microbiome in deficient and proficient mismatch repair colorectal cancers. Genome Med. 2018;10:78. doi: 10.1186/s13073-018-0586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee JA, Yoo SY, Oh HJ, Jeong S, Cho NY, Kang GH, et al. Differential immune microenvironmental features of microsatellite-unstable colorectal cancers according to Fusobacterium nucleatum status. Cancer Immunology, Immunotherapy. 2020; 10.1007/s00262-020-02657-x. [DOI] [PMC free article] [PubMed]
- 45.Wei Z, Cao S, Liu S, Yao Z, Sun T, Li Y, et al. Could gut microbiota serve as prognostic biomarker associated with colorectal cancer patients’ survival? A pilot study on relevant mechanism. Oncotarget. 2016;7:46158–72. doi: 10.18632/oncotarget.10064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Goedert JJ, Gong Y, Hua X, Zhong H, He Y, Peng P, et al. Fecal microbiota characteristics of patients with colorectal adenoma detected by screening: a population-based study. EBioMedicine. 2015;2:597–603. doi: 10.1016/j.ebiom.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang Y, Misra BB, Liang L, Bi D, Weng W, Wu W, et al. Integrated microbiome and metabolome analysis reveals a novel interplay between commensal bacteria and metabolites in colorectal cancer. Theranostics. 2019;9:4101–14. doi: 10.7150/thno.35186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Feng Q, Liang S, Jia H, Stadlmayr A, Tang L, Lan Z, et al. Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat Commun 2015;6:6528. [DOI] [PubMed]
- 49.Grobbee EJ, Lam SY, Fuhler GM, Blakaj B, Konstantinov SR, Bruno MJ, et al. First steps towards combining faecal immunochemical testing with the gut microbiome in colorectal cancer screening. United European Gastroenterology. United European Gastroenterol J . 2020;8:293–302. doi: 10.1177/2050640619890732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zeller G, Tap J, Voigt AY, Sunagawa S, Kultima JR, Costea PI, et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol Syst Biol. 2014;10:766. [DOI] [PMC free article] [PubMed]
- 51.Chenard T, Malick M, Dube J, Masse E. The influence of blood on the human gut microbiome. BMC Microbiol. 2020;20:44. [DOI] [PMC free article] [PubMed]
- 52.Tunsjo HS, Gundersen G, Rangnes F, Noone JC, Endres A, Bemanian V. Detection of Fusobacterium nucleatum in stool and colonic tissues from Norwegian colorectal cancer patients. Eur J Clin Microbiol Infect Dis. 2019;38:1367–76. doi: 10.1007/s10096-019-03562-7. [DOI] [PubMed] [Google Scholar]
- 53.Liang Q, Chiu J, Chen Y, Huang Y, Higashimori A, Fang J, et al. Fecal Bacteria Act as Novel Biomarkers for Noninvasive Diagnosis of Colorectal Cancer. Clin Cancer Res. 2017;23:2061–70. doi: 10.1158/1078-0432.CCR-16-1599. [DOI] [PubMed] [Google Scholar]
- 54.Amitay EL, Werner S, Vital M, Pieper DH, Hofler D, Gierse IJ, et al. Fusobacterium and colorectal cancer: Causal factor or passenger? Results from a large colorectal cancer screening study. Carcinogenesis. 2017;38:781–8. doi: 10.1093/carcin/bgx053. [DOI] [PubMed] [Google Scholar]
- 55.Toychiev A, Abdujapparov S, Imamov A, Navruzov B, Davis N, Badalova N, et al. Intestinal helminths and protozoan infections in patients with colorectal cancer: prevalence and possible association with cancer pathogenesis. Parasitol Res. 2018;117:3715–23. doi: 10.1007/s00436-018-6070-9. [DOI] [PubMed] [Google Scholar]
- 56.Zhou Y, He H, Xu H, Li Y, Li Z, Du Y, et al. Association of oncogenic bacteria with colorectal cancer in South China. Oncotarget. 2016;7:80794–802. doi: 10.18632/oncotarget.13094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ge W, Hu H, Cai W, Xu J, Hu W, Weng X, et al. High-risk Stage III colon cancer patients identified by a novel five-gene mutational signature are characterized by upregulation of IL-23A and gut bacterial translocation of the tumor microenvironment. Int J Cancer. 2020;146:2027–35. doi: 10.1002/ijc.32775. [DOI] [PubMed] [Google Scholar]
- 58.Xie YH, Gao QY, Cai GX, Sun, Sun XM, Zou TH, et al. Fecal Clostridium symbiosum for noninvasive detection of early and advanced colorectal cancer: test and validation. Studies. 2017;1:32–40. doi: 10.1016/j.ebiom.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baxter NT, Koumpouras CC, Rogers MA, Ruffin MT, Schloss PD. DNA from fecal immunochemical test can replace stool for detection of colonic lesions using a microbiota-based model. Microbiome. 2016;4:59. doi: 10.1186/s40168-016-0205-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ocvirk S, Wilson AS, Posma JM, Li JV, Koller KR, Day GM, et al. A prospective cohort analysis of gut microbial co-metabolism in Alaska Native and rural African people at high and low risk of colorectal cancer. Am J Clin Nutr. 2020;111:406–19. doi: 10.1093/ajcn/nqz301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ohigashi S, Sudo K, Kobayashi D, Takahashi O, Takahashi T, Asahara T, et al. Changes of the intestinal microbiota, short chain fatty acids, and fecal pH in patients with colorectal cancer. Digestive Dis Sci. 2013;58:1717–26. doi: 10.1007/s10620-012-2526-4. [DOI] [PubMed] [Google Scholar]
- 62.Yusuf F, Ilyas S, Damanik HA, Fatchiyah F. Microbiota Composition, HSP70 and Caspase-3 Expression as Marker for Colorectal Cancer Patients in Aceh, Indonesia. Acta Med Indonesiana. 2016;48:289–99. [PubMed] [Google Scholar]
- 63.Han S, Wu W, Da M, Xu J, Zhuang J, Zhang L, et al. Adequate lymph node assessments and investigation of gut microorganisms and microbial metabolites in colorectal cancer. OncoTargets Ther. 2020;13:1893–906. doi: 10.2147/OTT.S242017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Coker OO, Wu WKK, Wong SH, Sung JJY, Yu J. Altered Gut Archaea Composition and Interaction With Bacteria Are Associated With Colorectal Cancer. Gastroenterology. 2020;159:1459. doi: 10.1053/j.gastro.2020.06.042. [DOI] [PubMed] [Google Scholar]
- 65.Gao R, Wang Z, Li H, Cao Z, Gao Z, Chen H, et al. Gut microbiota dysbiosis signature is associated with the colorectal carcinogenesis sequence and improves the diagnosis of colorectal lesions. J Gastroenterol Hepatol. 2020; 10.1111/jgh.15077. [DOI] [PubMed]
- 66.Yu J, Feng Q, Wong SH, Zhang D, Yi Liang Q, Qin Y, et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut. 2015;66:70–78. doi: 10.1136/gutjnl-2015-309800. [DOI] [PubMed] [Google Scholar]
- 67.Zhang S, Kong C, Yang Y, Cai S, Li X, Cai G, et al. Human oral microbiome dysbiosis as a novel non-invasive biomarker in detection of colorectal cancer. Theranostics. 2020;10:11595–606. doi: 10.7150/thno.49515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Flemer B, Warren RD, Barrett MP, Cisek K, Das A, Jeffery IB, et al. The oral microbiota in colorectal cancer is distinctive and predictive. Gut. 2018;67:1454–63. doi: 10.1136/gutjnl-2017-314814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guven DC, Dizdar O, Alp A, Akdogan Kittana FN, Karakoc D, Hamaloglu E, et al. Analysis of Fusobacterium nucleatum and Streptococcus gallolyticus in saliva of colorectal cancer patients. Biomark. 2019;13:725–35. doi: 10.2217/bmm-2019-0020. [DOI] [PubMed] [Google Scholar]
- 70.Ai D, Pan H, Li X, Gao Y, Liu G, Xia LC. Identifying gut microbiota associated with colorectal cancer using a zero-inflated lognormal model. Front Microbiol. 2019;10:826. [DOI] [PMC free article] [PubMed]
- 71.Ai L, Tian H, Chen Z, Chen H, Xu J, Fang JY. Systematic evaluation of supervised classifiers for fecal microbiota-based prediction of colorectal cancer. Oncotarget. 2017;8:9546–56. doi: 10.18632/oncotarget.14488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Alomair AO, Masoodi I, Alyamani EJ, Allehibi AA, Qutub AN, Alsayari KN, et al. Colonic mucosal microbiota in colorectal cancer: A single-center metagenomic study in Saudi Arabia. Gastroenterol Res Pract. 2018; 10.1155/2018/5284754. [DOI] [PMC free article] [PubMed]
- 73.Arabameri A, Asemani D, Teymourpour P. Detection of colorectal carcinoma based on microbiota analysis using generalized regression neural networks and nonlinear feature selection. IEEE/ACM Trans Comput Biol Bioinform. 2020;17:547–57. doi: 10.1109/TCBB.2018.2870124. [DOI] [PubMed] [Google Scholar]
- 74.Guo S, Li L, Xu B, Li M, Zeng Q, Xiao H, et al. A simple and novel fecal biomarker for colorectal cancer: ratio of fusobacterium nucleatum to probiotics populations, based on their antagonistic effect. Clin Chem. 2018;64:1327–37. doi: 10.1373/clinchem.2018.289728. [DOI] [PubMed] [Google Scholar]
- 75.Liu Y, Geng R, Liu L, Jin X, Yan W, Zhao F, et al. Gut Microbiota-based algorithms in the prediction of metachronous adenoma in colorectal cancer patients following surgery. Front Microbiol. 2020;11:1106. [DOI] [PMC free article] [PubMed]
- 76.Tarallo S, Ferrero G, Gallo G, Francavilla A, Clerico G, Luc AR, et al. Altered fecal small RNA profiles in colorectal cancer reflect gut microbiome composition in stool samples. mSystems. 2019;4:e00289-19. [DOI] [PMC free article] [PubMed]
- 77.Yachida S, Mizutani S, Shiroma H, Shiba S, Nakajima T, Sakamoto T, et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat Med. 2019;25:968–76. doi: 10.1038/s41591-019-0458-7. [DOI] [PubMed] [Google Scholar]
- 78.Kim DJ, Yang J, Seo H, Lee WH, Ho Lee D, Kym S, et al. Colorectal cancer diagnostic model utilizing metagenomic and metabolomic data of stool microbial extracellular vesicles. Sci Rep. 2020;10:2860. doi: 10.1038/s41598-020-59529-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liang S, Mao Y, Liao M, Xu Y, Chen Y, Huang X, et al. Gut microbiome associated with APC gene mutation in patients with intestinal adenomatous polyps. Int J Biol Sci. 2020;16:135–46. doi: 10.7150/ijbs.37399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shen W, Sun J, Yao F, Lin K, Yuan Y, Chen Y, et al. Microbiome in intestinal lavage fluid may be a better indicator in evaluating the risk of developing colorectal cancer compared with fecal samples. Transl Oncol. 2020;13:100772. [DOI] [PMC free article] [PubMed]
- 81.Wei PL, Hung CS, Kao YW, Lin YC, Lee CY, Chang TH, et al. Classification of changes in the fecal microbiota associated with colonic adenomatous polyps using a long-read sequencing platform. Genes. 2020;11:1–14. doi: 10.3390/genes11111374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jin Y, Liu Y, Zhao L, Zhao F, Feng J, Li S, et al. Gut microbiota in patients after surgical treatment for colorectal cancer. Environ Microbiol. 2019;21:772–83. doi: 10.1111/1462-2920.14498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li YD, He KX, Zhu WF. Correlation between invasive microbiota in margin-surrounding mucosa and anastomotic healing in patients with colorectal cancer. World J Gastrointest Oncol. 2019;11:717–28. doi: 10.4251/wjgo.v11.i9.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yu SY, Xie YH, Qiu YW, Chen YX, Fang JY. Moderate alteration to gut microbiota brought by colorectal adenoma resection. J Gastroenterol Hepatol (Aust) 2019;34:1758–65. doi: 10.1111/jgh.14735. [DOI] [PubMed] [Google Scholar]
- 85.Wang HF, Li LF, Guo SH, Zeng QY, Ning F, Liu WL, et al. Evaluation of antibody level against Fusobacterium nucleatum in the serological diagnosis of colorectal cancer. Sci Rep. 2016;6:33440. doi: 10.1038/srep33440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207-14. [DOI] [PMC free article] [PubMed]
- 87.Lloyd-Price J, Abu-Ali G, Huttenhower C. The healthy human microbiome. Genome Med. 2016;8:51. doi: 10.1186/s13073-016-0307-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Conlon MA, Bird AR. The impact of diet and lifestyle on gut microbiota and human health. Nutrients. 2014;7:17–44. doi: 10.3390/nu7010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mancabelli L, Milani C, Lugli GA, Turroni F, Ferrario C, van Sinderen D, et al. Meta-analysis of the human gut microbiome from urbanized and pre-agricultural populations. Environ Microbiol. 2017;19:1379–90. doi: 10.1111/1462-2920.13692. [DOI] [PubMed] [Google Scholar]
- 90.Janney A, Powrie F, Mann EH. Host-microbiota maladaptation in colorectal cancer. Nature. 2020;585:509–17. doi: 10.1038/s41586-020-2729-3. [DOI] [PubMed] [Google Scholar]
- 91.Dejea CM, Wick EC, Hechenbleikner EM, White JR, Mark Welch JL, Rossetti BJ, et al. Microbiota organization is a distinct feature of proximal colorectal cancers. Proc Natl Acad Sci USA. 2014;111:18321–6. doi: 10.1073/pnas.1406199111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Johnson CH, Dejea CM, Edler D, Hoang LT, Santidrian AF, Felding BH, et al. Metabolism links bacterial biofilms and colon carcinogenesis. Cell Metab. 2015;21:891–7. doi: 10.1016/j.cmet.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li S, Konstantinov SR, Smits R, Peppelenbosch MP. Bacterial biofilms in colorectal cancer initiation and progression. Trends Mol Med. 2017;23:18–30. doi: 10.1016/j.molmed.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 94.Wong SH, Yu J. Gut microbiota in colorectal cancer: mechanisms of action and clinical applications. Nat Rev Gastroenterol Hepatol. 2019;16:690–704. doi: 10.1038/s41575-019-0209-8. [DOI] [PubMed] [Google Scholar]
- 95.Francescone R, Hou V, Grivennikov SI. Microbiome, inflammation, and cancer. Cancer J. 2014;20:181–9. doi: 10.1097/PPO.0000000000000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Greer JB, O’Keefe SJ. Microbial induction of immunity, inflammation, and cancer. Front Physiol. 2011;1:168. doi: 10.3389/fphys.2010.00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rudolph A, Toth C, Hoffmeister M, Roth W, Herpel E, Jansen L, et al. Expression of oestrogen receptor β and prognosis of colorectal cancer. Br J Cancer. 2012;107:831–9. doi: 10.1038/bjc.2012.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Williams C, DiLeo A, Niv Y, Gustafsson J. Estrogen receptor beta as target for colorectal cancer prevention. Cancer Lett. 2016;372:48–56. doi: 10.1016/j.canlet.2015.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.