Abstract
Disclosure of self-injurious thoughts and behaviors (SITBs) is critical to current treatment and prevention programs. Limited research has examined patterns of and barriers to SITB disclosure in adolescents. This work is critical given the limits of confidentiality in this population. Over 1,000 adolescents aged 13–17 with a history of mental health treatment and SITBs were recruited online. Participants reported their history with disclosing SITBs across a range of relationships, honesty in and barriers to disclosure to healthcare providers, and their experiences with breaches of confidentiality to parents/guardians. We examined relationships among these experiences and a range of outcomes, including perceived likelihood of future disclosure. Participants reported most frequent disclosure of all SITBs to friends, and more frequent disclosure of nonsuicidal self-injury compared to suicide ideation or attempts. Adolescents were most likely to disclose SITBs when directly asked by healthcare providers, though many participants reported continued SITB concealment. The most commonly endorsed barrier to disclosure was fear that the provider would tell a parent/guardian. Experiences with confidentiality breaches involving a non-collaborative breach were negatively associated with future disclosure, mental health symptoms, and adolescent-parent relationships. SITB disclosure is a cornerstone to their treatment and prevention. Better understanding of to whom and when, barriers, and the impact of disclosure experiences is critical. Our research suggests that most adolescents do not want their parents to know about their SITBs, and that fear of parent involvement prevents disclosure. Results have several implications for SITB assessment across physical and mental healthcare settings.
Keywords: adolescents, nonsuicidal self-injury, suicide ideation, suicide attempt, disclosure, therapy
Introduction
Suicide is a leading cause of death among youth in the United States; nearly 7,000 youth aged 10–24 died by suicide in the year 2018 alone (Center for Disease Control and Prevention [CDC], 2018). Even more common, approximately 4% of adolescents report a lifetime history of nonfatal suicidal behaviors (e.g., suicide attempts), 12% report suicide ideation and nearly 17% report nonsuicidal self-injury (NSSI; intentional self-harm enacted without suicidal intent; Nock et al., 2013; Swannell et al., 2014). These self-injurious thoughts and behaviors (SITBs) are associated with numerous negative outcomes including psychopathology, distress, interpersonal difficulties, and emotion dysregulation in adolescents (Mars et al., 2014; Wilkinson et al., 2018).
Given that suicide decedents often have recent contacts with both primary care (e.g., general medical setting; Luoma et al., 2002) and mental health providers (Appleby et al., 1999) leading up to their deaths, universal assessment of suicide ideation and related thoughts and behaviors are a critical part of suicide prevention across healthcare settings (Office of the Surgeon General & National Action Alliance for Suicide Prevention, 2012, 2021). Outside of the healthcare setting, suicide prevention initiatives often involve peers, friends, teachers, parents, and loved ones looking out for ‘warning signs’ and asking people whether they are thinking about suicide (e.g., Singer et al., 2019). Most of these critical assessments rely on a key factor: disclosure honesty and openness. Although disclosure is a necessary component of most suicide prevention programs, we know very little about adolescents’ experiences and decision making around SITB disclosure.
To help fill this gap in the literature, we sought to examine critical aspects of adolescent SITB disclosures across three distinct SITB subtypes: NSSI, suicidal ideation, and suicide attempts. This study has four primary aims: (1) characterize and compare adolescents’ choice and frequency of disclosure to key people in their lives; (2) examine adolescents’ honesty in disclosure to medical (e.g., pediatrician, primary care providers) and mental healthcare (e.g., therapists, psychiatrists, counselors) providers, including barriers to disclosure; (3) evaluate whether asking about SITBs is associated with a greater likelihood of disclosure across medical and mental health care settings; and (4) examine adolescents’ experiences with therapists breaching confidentiality, including impacts on mental health symptoms, relationships with parents/guardians and therapists, and future likelihood of disclosure.
Prior research examining SITB disclosure has primarily focused on suicide ideation disclosure among adults. This line of research shows that only around half of adults with suicide ideation and attempt histories choose to share their suicide ideation with others; those who share are substantially more likely to disclose to informal supports (e.g., friends and family) compared to formal supports (e.g., medical and mental healthcare professionals), and that they are more likely to share with family compared to friends. This is the case for adults across general (Encrenaz et al., 2012; Mérelle et al., 2018), psychiatric (e.g., Barnes et al., 2002), and mental health treatment seeking (Drum et al., 2009; Hom et al., 2017) samples. Moreover, there is some evidence that adults are more likely to disclose more ‘severe’ suicidal thoughts and behaviors than less ‘severe’ SITBs, with the greatest likelihood of disclosure of suicide attempts, followed by suicide plans, and suicidal ideation; this pattern was demonstrated across all categories of supports (e.g., close friends or family, health professionals, association or helplines, other; Encrenaz et al., 2012). Relatedly, research indicates that greater severity of suicidal ideation may be associated with greater disclosure across all categories of support (Calear & Batterham, 2019).
Research examining patterns of SITB disclosures in adolescents is scant. However, one such study examined suicide ideation disclosure in Swedish and Turkish high school students and found that, paralleling adults, just about half of students disclosed their suicide ideation to any support person. Unlike in adults, however, in this study the students reported lower rates of disclosure to parents (family) compared to friends (Eskin, 2003). In other words, limited prior work suggests that only about half of adolescents disclose their suicide ideation, and that their patterns of disclosure may differ from those observed in adults.
Few to no studies to date have directly compared rates and patterns across specific SITB disclosure in adults or adolescents. This gap is surprising, given that although NSSI is cross-sectionally and prospectively predictive of suicidal behavior (Ribeiro et al., 2016), NSSI is distinct in that it is typically engaged in more frequently and with a larger variation in methods, and commonly leaves tangible physical markings that can be difficult to conceal (Burke et al., 2020; Klonsky, May, & Glenn, 2013). That said, research specifically examining NSSI disclosures across adolescents and adults suggests some similar patterns to suicide ideation and attempts. A recent review by Simone & Hamza (2020), summarizing across nearly a dozen studies, found that rates of NSSI disclosure were near 50% in both adolescents and adults, although adults were more likely than adolescents to have disclosed their NSSI engagement. Moreover, results of this review demonstrated that both adolescents and adults were more likely to have disclosed NSSI to friends and romantic partners compared to family members. Thus, results of existing research suggests that rates of NSSI disclosure, and disclosure patterns (i.e., who adolescents tell) may be similar to disclosure of suicide ideation; yet, no studies to date have directly compared these disclosure patterns. The present exploratory study will begin to fill these gaps by characterizing patterns of SITB disclosure among adolescents living in the US. Specifically, we will examine and compare lifetime rates of disclosure across NSSI, suicide ideation, and suicide attempts as well as frequency of and differences in disclosure to key people in adolescents’ lives.
Disclosure of SITBs to healthcare professionals is critical given that healthcare professionals are often key players in suicide prevention, providing critical referrals when relevant. However, prior research shows that only a minority of adults share their SITBs with medical and mental health professionals (Calear & Batterham, 2019; Encrenaz et al., 2012), and that this disclosure may differ by healthcare provider specialty. Indeed, in a sample of undergraduates, participants reported more accurate suicide ideation disclosures to mental health professionals (i.e., therapist, psychiatrist, counselor), compared to medical doctors/physicians, when directly asked about suicidal ideation (Hom et al., 2017). Similarly, in a community sample of Australian adults, rates of suicidal ideation disclosure to psychologists and general practitioners were similar, but these disclosures were lower to other health professionals, psychiatrists, counselors, and social workers (Calear & Batterham, 2019). SITB disclosure patterns in adolescents remain understudied. However, insights from adolescent disclosure of other health risk behaviors suggests adolescents may be reticent to disclose to healthcare providers. Indeed, prior research indicates that most adolescents do not disclose engagement in other risky and stigmatized behaviors (e.g., drug/alcohol use) in medical settings (e.g., Santelli et al., 2019). The present study will examine rates of adolescents’ SITB disclosure honesty to healthcare professionals, and will examine whether disclosure honesty differs between healthcare provider types (i.e., medical [e.g., primary care providers, pediatricians] versus mental health providers [e.g., therapist, counselor, psychiatrists]), and across SITB types (i.e., NSSI, suicide ideation, suicide attempts).
The low rates of SITB disclosures to mental health providers among adults and college-aged students appears to be driven by numerous barriers, including concerns related to stigma, involuntary hospitalization, medication prescription, and fears of rejection or worrying one’s confidant (Hom, 2017; Fulginiti & Frey, 2019; Rosenrot & Lewis, 2018; Sheehan et al., 2019). Less research has examined barriers to SITB disclosure in adolescents; yet, numerous additional barriers discourage minors from disclosing (e.g., limited confidentiality that often does not extend to parent/guardians). In their study of Turkish and Swedish adolescents, Eskin (2003) found that beliefs they could not be helped, lack of close others, and fear of stigma-related judgments were key barriers to the disclosure of suicidal ideation to friends, family, and others. Research on the disclosure of other sensitive health risk behaviors demonstrates that lack of private (one-on-one) time with medical providers and unclear regulations around confidentiality impedes disclosure (e.g., Grilo et al., 2016). The present study will build on this work to examine barriers that impact teens’ SITB disclosure across both medical and mental healthcare providers. Such barriers are particularly important considering that these settings often act as gateways to suicide prevention services.
Another critical aspect of adolescent SITB disclosure to healthcare professionals is SITB risk assessment. SITB risk assessments are a key aspect of suicide prevention that typically involve direct questions assessing SITBs among people who enter medical and mental health settings. Despite preliminary support (Hom et al., 2017), it remains unclear whether asking directly about SITBs is associated with greater rates of disclosure, particularly among adolescents, or whether SITB disclosure when directly assessed varies across medical versus mental healthcare settings or across SITB type. The present study will test both whether asking about individual SITBs is associated with greater likelihood that they are disclosed, and whether this varies across medical and mental healthcare providers.
When people disclose SITBs, mental healthcare providers face the competing tensions of maintaining therapeutic rapport, ensuring youth safety, and upholding ethical mandates to breach confidentiality if a client is at imminent risk of harming themselves. These tensions are particularly complex when working with adolescents, as ethical guidelines require mental healthcare providers to breach confidentiality and share with parents/guardians when adolescents’ behaviors may result in ‘harmful outcomes’ (Rae, 2002). Decisions about what constitutes a ‘harmful outcome’ varies across providers’ value systems, training, and interpretation of research. Although standards exist for how and when to breach confidentiality in high and imminent risk scenarios (e.g., see Helms & Prinstein, 2014), pediatric psychologists vary widely in when they believe it ethical to breach confidentiality, often believing it ethical to do so in cases of low to moderate risk. For example, Rae and colleagues (2002) observed that pediatric psychologists found it “somewhat ethical” to breach confidentiality when an adolescent reported suicide ideation “once several months ago;” psychologists reported that it became increasingly ethical as the frequency of these thoughts increased (reaching “ethical under almost all circumstances” when daily for the past year). Pediatric psychologists reported finding it “ethical under many circumstances” to report when an adolescent reported a suicide attempt over a year ago, and it became nearly “unquestionably ethical” as the recency and frequency of suicide attempts increased. In other words: most pediatric psychologists find it ethical to breach confidentiality to share adolescent suicide ideation and attempts with a parent/guardian, particularly when the SITBs are more recent and frequent. Perceived ethicality of sharing NSSI among pediatric psychologists remains unstudied, but it may parallel suicide ideation, suicide attempts, and other health risk behaviors (e.g., risky sexual behaviors), wherein the ethicality varies across levels of frequency, intensity, and potential for serious harm (Rae et al., 2002).
Across other areas of study, there is evidence that adolescents may be less likely to disclose a risky behavior if they know their parent/guardian may be informed. For example, adolescents are less likely to seek out healthcare services (e.g., sexual health) if they are concerned their parents will find out about their visit (Cheng et al., 1993; Reddy, 2002). It is likely that such concerns extend to disclosure of SITBs. Indeed, Lothen-Kline and colleagues (2003) found that adolescents were 7% less likely to disclose suicidal thoughts in a research study when given a consent form stating that providers may need to reveal to parents/guardians or other professionals if adolescents report being ‘suicidal.’ Taken together, prior research provides indirect support that adolescents may be less likely to disclose SITBs to health providers if they think this information could be shared with a parent/guardian.
Given the potential for serious harm and even death, there are cases where parents/guardians likely need to be informed of adolescent SITBs. However, there is no standard on when or how this information should be shared, despite potentially widespread impacts. Thus, the fourth and final aim of this study is to test whether adolescents’ experiences with therapists breaching confidentiality are associated with their future SITB disclosure, trust and relationship with the therapist and parent(s), and mental health symptoms. Specifically, we will examine whether the way that therapists share this information (e.g., collaboratively or forcefully) with parents/guardians impacts these critical outcomes. Taken together, results from this study will provide crucial information about prevalence, characteristics, and barriers to SITB disclosure among adolescents.
Method
Participants
Participants were recruited online, using paid Instagram advertisements ($1,394 spent in total) targeting youth aged 13–17. Study advertisements highlighted that the confidential study would provide teenagers with the opportunity to share experiences in therapy. Those who clicked on our advertisement were directed to a brief screening survey, hosted on Qualtrics, assessing eligibility (i.e., aged 13–17, English speaking, living in the US, lifetime history of SITB engagement, lifetime history of mental health treatment) via relevant and filler items, unrelated to the inclusion criteria. Those who qualified for the study were invited to read the assent form. The assent form clarified study details, including that participation was entirely confidential and private, and that participation did not require parental consent. Participants then completed a brief quiz to ensure comprehension before being invited to start the study. Participants could then opt to start the study immediately, or to receive a link to the study survey via Qualtrics, depending on their preference. After completion of the study survey, participants were provided with electronic mental health resources and hotlines. All participants who completed the survey were entered into a lottery for one of 50 $25 gift cards to Amazon, Target, or iTunes. Research and recruitment procedures, including the study waiver of parental permission, were approved by the University of Denver Institutional Review Board (IRB). Several steps were taken to reduce the likelihood of fraudulent responders; for example, in Qualtrics, we selected the option to ‘prevent multiple submissions’ in both the screening survey and in the primary study survey. We also used the ‘bot detection,’ relevant ID ‘duplicate detection,’ and ‘fraud detection’ features within the primary survey. With these features, bot detection scores greater than .5, on a scale of 0–1, are deemed more likely to be a human; fraud detection scores below 30, on a scale from 0–100, indicate a response is likely not fraudulent; duplicate ID scores below 75, on a scale from 0–100, are unlikely to be duplicates, and duplicate ID scores of ‘FALSE’ indicate that a given participant is likely not duplicated.
In total, 2,100 people completed the screening survey; of those, 1,800 (86%) qualified for the study, read the study assent form, and agreed to participate; 1,706 began the study and 962 (56%) finished the full study. This rate of completion is likely related to the length of the survey, which took 45 minutes to complete on average. We excluded participants who completed the study twice, and who opened the study survey but did not complete any study measures regarding SITB disclosure (the first of which appeared 4 questions into the survey). We also excluded participants who were labeled by the Qualtrics bot, fraud, and duplicate detection methods to be fraudulent (n = 20). To maximize statistical power, all participants who answered questions about SITB disclosure were included in the study, even if they did not answer all study questions.
The final analytic sample size ranged from a maximum of 1,495 to a minimum of 945 adolescents. Participants ranged in age from 13–17, and the average age was 15.71 (standard deviation [SD] = 1.11). We assessed demographic characteristics toward the end of the survey; therefore, only 62% of the included sample responded to these items. Of those participants, regarding race/ethnicity, 591 (64%) participants identified as White/Caucasian, 161 (17.5%) as Hispanic/Latin American, 27 (3%) as Black/African American, 45 (5%) as Asian/Asian American/Pacific Islander, 79 (8.6%) as biracial or multiracial, and 19 (2%) as other, including Native American. Most participants (n=892; 95%) reported being assigned female sex at birth, and female gender (n=581; 62%). Substantial gender diversity was observed (i.e., 96 (10%) identified as gender nonbinary, 92 (10%) identified as gender queer, expansive, or other, 83 (9%) identified as transgender, 25 (3%) identified as cisgender boy/man, and 61 (7%) identified as questioning their gender. Additionally, only a minority of the sample identified as heterosexual/straight (n = 119; 13%); bisexual was the most commonly reported sexual orientation (n = 352; 39%).
Ethical Considerations
This study received ethical approval from the University of Denver. We obtained participant assent and waived parental consent for the purposes of this research. Waivers of parental consent can be appropriate for online research in adolescents when the research cannot otherwise be carried out (parental consent is nearly impossible to verify online), when the study poses minimal risk to participants, when the waiver does not impact the rights or welfare of participants, and when participants are provided with additional information about the study after participating; each are relevant here. Consistent with best practices in online research involving SITBs (Smith et al., 2021), all participants were provided with access to electronic mental health resources and a self-guided safety plan (see https://osf.io/g6cha/) both after completing the study screener (regardless of qualification) and after completing the full study.
Measures
Screening survey.
We assessed participant eligibility using items from the Self-Injurious Thoughts and Behavior Interview-Revised (SITBI-R; Fox et al., 2020). Specifically, we used items from the SITBI-R to assess lifetime history of NSSI, suicide ideation, and suicide attempts. We also used single items to assess lifetime history of mental health treatment and age. Filler items were added to obscure inclusion criteria.
Demographics.
Demographic items were assessed at the end of the study survey. Items assessed age, race, ethnicity, gender, sexual orientation, and socioeconomic status, using the MacArthur Scale of Subjective Social Status–Youth Version (Goodman et al., 2001). Gender was assessed using a comprehensive measure, including a wide range of gender identities to better reflect youth gender identity (Thoma et al., 2019). Finally, in assessing sexual orientation, we allowed participants to select multiple sexual orientations in light of previous participant feedback that this was more reflective of their sexual identities.
History of SITB disclosure.
We used several items to assess SITB disclosure. We first determined SITB histories using items assessing NSSI, suicide ideation, and suicide attempts derived from the SITBI-R, which demonstrates strong psychometric properties for the assessment of each of these SITB across both in-person and online assessment formats (Fox et al., 2020).
When relevant participants were asked, “Have you ever told anyone about times where you [purposely hurt yourself without wanting to die/ had thoughts of killing yourself/ tried to kill yourself]?” Next, following this item, participants were asked to think about all of the times in their life that they engaged in a given SITB. Then, using a Likert-type scale including the options of never (0), rarely (1), sometimes (2), most times (3), every time (4), they were asked to select how frequently they have disclosed these behaviors. To clarify these instructions, participants were told: “Note, if you have engaged in [SITB listed] only ONCE, you should select “never” for anyone you did NOT tell about the event, and you should select “every time” for anyone that you DID tell about the event. Options included: parent/guardian, therapist (not including your psychiatrist), psychiatrist or doctor who prescribes your mental health medication, the ‘doctor you see for check-ups and physicals (termed pediatrician here for brevity), another adult that you trust, sibling, friend, acquaintance, someone you met online, and other. For the purposes of this study, and to maximize statistical power, we examined disclosures to friends, parents/guardians, therapists, psychiatrists, and pediatricians.
Future likelihood of SITB disclosure.
Participants were asked to report their likelihood of disclosing each SITB with their parent/guardian and with a therapist in the future on a scale from 0 (not at all) to 4 (extremely).
Provider SITB assessment and honesty.
To assess whether (1) medical doctors (e.g., pediatricians, defined as ‘doctor you see for check-ups and physicals’) and (2) mental health professionals/therapists (inclusive of therapists, psychiatrists, and other mental health providers worked with in mental health treatment) had directly assessed a given SITB, participants were asked whether the provider had ever asked them about each SITB, separately. Participants could answer yes, no, and don’t remember. In this study, only yes/no responses are considered. Next, to assess participant honesty in disclosures to a given provider, we adapted items from the Difficult Disclosures Survey (Blanchard and Farber, 2016). Specifically, participants were asked to “rate how honest you were” with their (1) pediatrician/medical providers and (2) therapists about each SITB, separately, on a scale ranging from 0 (not at all honest) to 4 (completely honest). N/A options were provided in instances when a participant had not yet engaged in a given SITB when meeting with their provider. Of note, participants were asked to rate their honesty in disclosure regardless of whether they were asked directly about these behavior(s) by their provider(s).
Barriers to disclosure.
We adapted items from Hom and colleagues’ (2017) to assess barriers to SITB disclosure to pediatricians and mental health professionals separately. Items were added to include barriers that may be particularly relevant to adolescents and not adults (e.g., telling parent/guardian) and to reflect additional forms of stigma (e.g., shame). All barriers assessed are included in Figure 2, and participants were asked to select each given barrier that applied to them.
Fig. 2:
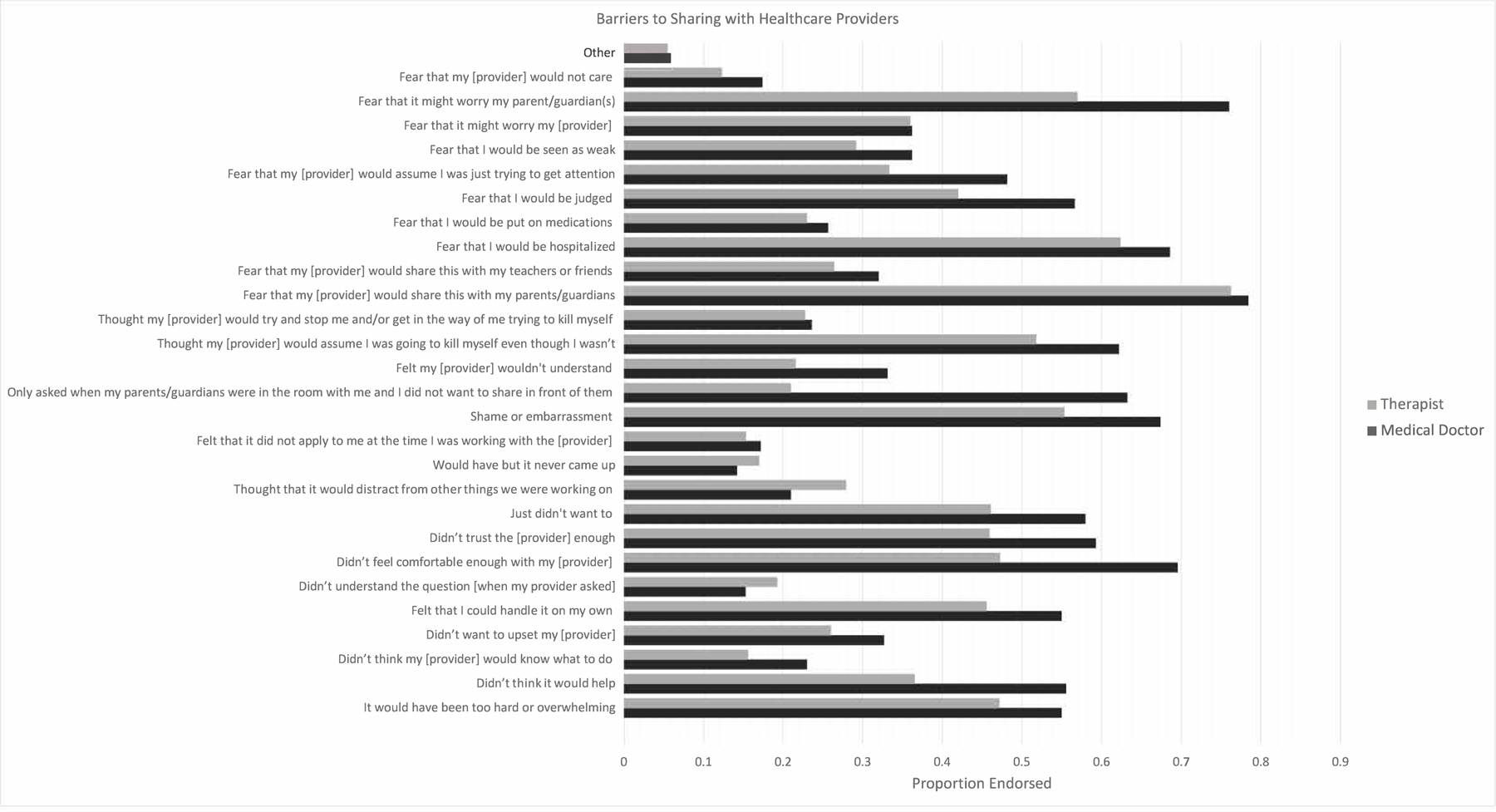
Barriers to disclosing to mental and medical healthcare providers
Impact of confidentiality breaches.
We created a measure to assess adolescents’ experiences with therapists breaching confidentiality to share their SITB with parent/guardian(s). Across each SITB separately, participants were asked “Thinking about all of the times you talked about your [SITB behavior] during mental health treatment: After sharing these behaviors with your therapist, did they ever… (1) tell your parent/guardian(s) WITH your permission; (2) tell your parent/guardian(s) WITHOUT your permission; (3) help you to tell your parent/guardian(s) during session; (4) force you to tell your parent/guardian(s) during session”. Next, participants were asked to consider whether experiences with a therapist sharing their SITB(s) with a parent/guardian had a negative impact, no impact, or positive impact on key relationships, future therapy willingness, mental health symptoms, self-worth, and SITB urges (all items are listed in Figure 4).
Fig. 4:
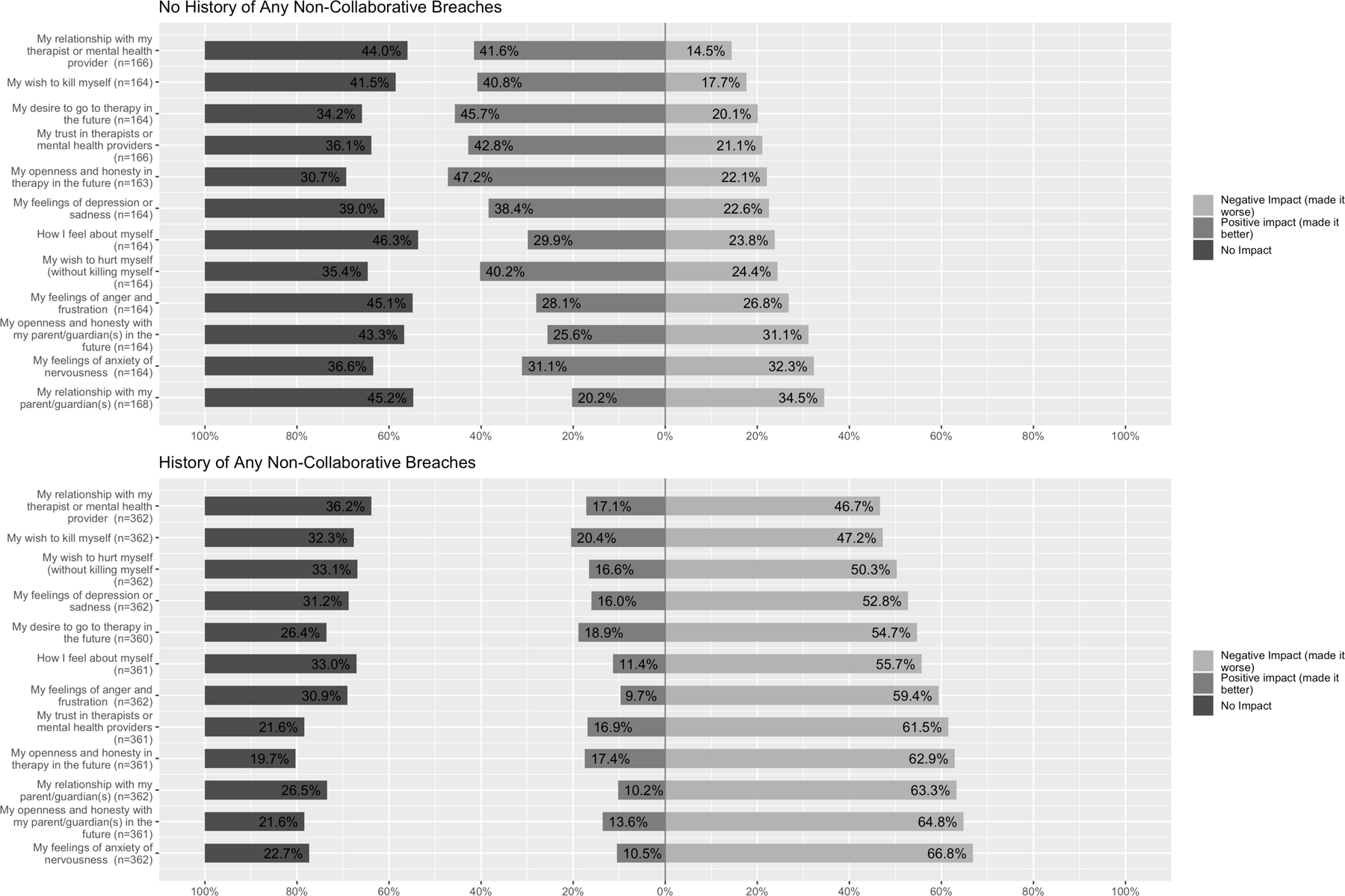
Therapy and parent outcomes after confidentiality breaches
Data Analysis
Aim 1: Characterize adolescents’ SITB disclosure to key people in their lives.
We first examined the percent of participants reporting a lifetime history of each primary SITB (i.e., NSSI, suicide ideation, suicide attempt). Next, using the item, “Have you ever told anyone about times where you [purposely hurt yourself without wanting to die/ had thoughts of killing yourself/ tried to kill yourself]?”, we examined the percent of participants reporting disclosure of each SITB, including only those participants with a history of a given behavior. Finally, we examined whether differences emerged in the frequency of disclosure of each SITB (NSSI, suicide ideation, suicide attempt) across key people in their lives (i.e., friends, parents, pediatricians, psychiatrists, therapists) using Fisher’s repeated measures one-way analysis of variance (ANOVA). Because more than two categories were examined, Student’s t-tests, using Holm corrections, were conducted to examine specific differences in the frequency of sharing across key people.
Aim 2: Examine teen honesty in disclosure to primary care and mental health care providers, including barriers to disclosure.
We used Fisher’s repeated measures ANOVA to examine whether differences emerged in participants’ self-reported disclosure honesty across provider type (mental health versus medical providers). To better understand rates of endorsements to these providers, we then shared the percentage of participants endorsing each of numerous key barriers to disclosure.
Aim 3: Test whether asking about SITBs is associated with greater rates of disclosure across medical care and mental health settings.
We assessed the frequency with which participants were explicitly asked about each SITB type across both medical care and mental health care providers. Next, we conducted McNemar’s χ2 tests to examine whether participants were more likely to disclose each SITB when they were explicitly asked about each behavior. This test was conducted separately for medical and mental health care providers.
Aim 4: Examine adolescents’ experiences with mental health providers breaching confidentiality, including whether such breaches are associated with adolescents’ mental health symptoms, relationships to their parents/guardians and providers, and future likelihood of disclosure.
We categorized participants into the following categories; those who reported (1) only non-collaborative breach experiences (i.e., telling a parent/guardian without the adolescents’ permission and/or forcing the teenager to tell their parent/guardian; n = 64), (2) only collaborative breaches (i.e., telling a parent/guardian with the adolescents’ permission and/or helping the teen to tell their parent/guardian; n = 155), (3) a mix of both non-collaborative and collaborative breaches (mixed breaches; n = 456), and (3) participants who denied any history of confidentiality breaches (n = 103). We used Welch’s one-way ANOVA to examine whether participants reporting different histories of therapist breaches reported (a) differences in the frequency of hiding, lying, or avoiding talking about their SITBs with a therapist because of bad experiences telling therapists in the past and (b) lower odds of disclosing SITBs to therapists in the future. Because more than two categories were examined, Games-Howell tests, using Holm corrections, were conducted to examine specific differences across categories of breaches.
Next, due to the relatively small number of participants reporting only non-collaborative breaches and because any non-collaborative breach may be harmful, we combined those who had experienced both only non-collaborative breaches and mixed breaches into a single group. We then examined the rates of endorsement of negative, positive, or neutral effects of times when a therapist shared their self-harming and/or suicidal thoughts and/or behaviors with their parents/guardians on several therapy related outcomes.
All analyses were conducted in R (Development Core Team, 2013); all statistical tests and figures were generated using ggstatsplot (Patil, 2021).
Results
Aim 1: Characterize adolescents’ SITB disclosure to key people in their lives.
Most of the sample reported a lifetime history of each SITB, with 98% reporting lifetime suicide ideation, 94% reporting lifetime NSSI, and 55% reporting lifetime suicide attempts. Moreover, 80% of participants with a history of NSSI, 78% of participants with a history of suicide ideation, and 73% of participants with a history of suicide attempt(s) reported disclosing these thoughts and behaviors to someone at some point in their lives.
Three ANOVAs demonstrated differences in frequency of NSSI disclosure (Ffisher (3.38, 3307.12) = 483.88, p < .001, partial omega squared = 0.23), suicide ideation disclosure (Ffisher (3.33, 3302.29) = 434.83, p < .001, partial omega squared = 0.20), and suicide attempt disclosure (Ffisher (3.39, 1833.48) = 184.45, p < .001, partial omega squared = 0.13), across key people (Supplemental Figure 1). Holm-corrected post-hoc tests revealed that patterns of disclosure were similar across SITBs; adolescents most frequently shared their NSSI, suicide ideation, and suicide attempts with their friends and least frequently with their pediatrician. Moreover, for both NSSI and suicide ideation, participants more frequently shared with their psychiatrists than their parents, although this difference was not statistically significant for suicide attempts.
Aim 2: Examine teen honesty in disclosure to medical care and mental health care providers, including barriers to disclosure.
Next, we examined participants’ reported honesty in their disclosure of each SITB to their mental health providers (e.g., therapists, counselors, psychiatrists) and to their medical providers (e.g., pediatricians, primary care providers) using Fisher’s repeated measures ANOVA (see Figure 1). There were significant differences in honesty of SITB disclosure to both therapists and pediatricians. In both cases, Holm corrected post-hoc tests demonstrated that participants were most honest in disclosing NSSI compared to both suicide ideation and attempts, and that they were also more honest in disclosing suicide ideation compared to suicide attempts to both types of providers.
Fig. 1:
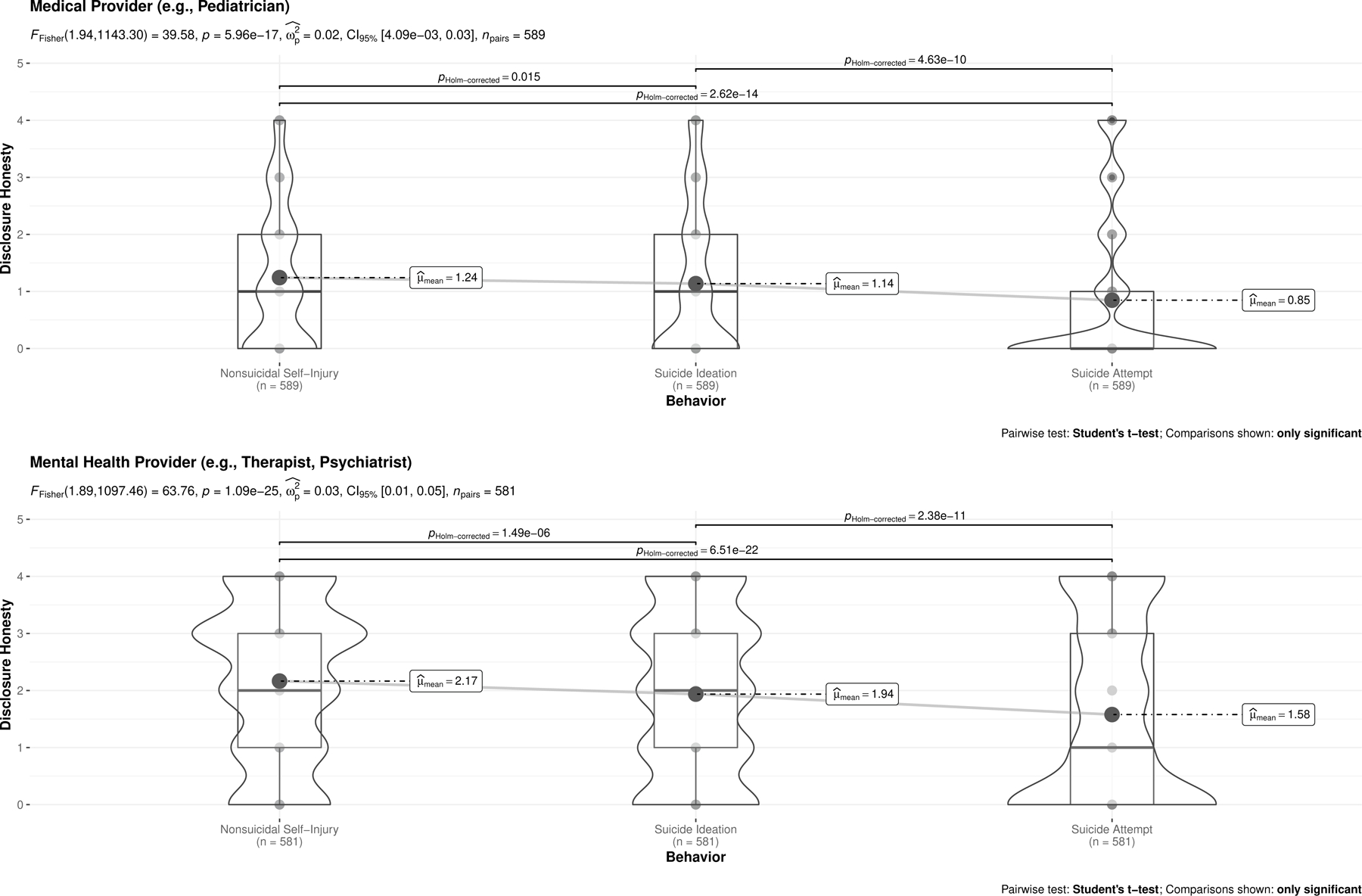
Nonsuicidal self-injury, suicide ideation, and suicide attempt disclosure honesty across medical and mental health providers
As noted in Figure 1, on average, participants reported being between a little bit and somewhat honest, at best, across SITBs to their medical doctor/pediatricians and therapists. Thus, we next examined participants reported barriers to honesty across both their therapists and pediatricians; frequency of endorsement of each barrier is plotted in Figure 2. Regarding barriers to honesty with therapists, the top 5 most commonly reported barriers were: worry that the therapist would share SITBs with their parents, worry about being hospitalized, fear of worrying their parents, shame/embarrassment, and fear that their therapist would assume their disclosure meant they were currently suicidal. Regarding barriers to honesty with pediatricians, the top 5 most commonly reported barriers were: worry that the provider would share SITBs with their parents, fear of worrying their parents, not feeling comfortable enough with the provider, worry about being hospitalized, and shame/embarrassment. Of note, approximately 60% also reported that they did not disclose because they did not want to share in front of their parent/guardian.
Aim 3: Test whether asking about SITBs increases disclosure across medical care and mental health settings.
McNemar’s χ2 test indicated that, across behaviors and providers, when participants were directly asked about NSSI, suicide ideation, and suicide attempts, they were also significantly more likely to disclose these thoughts and behaviors (all ps < .003, Cohen’s gs ranged from 0.12–0.44; see Supplemental Figure 2).
Aim 4: Examine adolescents’ experiences with therapists breaching confidentiality, including whether this impacts their mental health symptoms, relationships to their parents/guardians and therapists, and their future likelihood of disclosure.
Welch’s F-tests revealed that history of different breach experiences were significantly related to subsequently hiding/lying about SITBs to a therapist, as well as likelihood of future SITB disclosure across all key SITB outcomes (see Figure 3). Holm-corrected post-hoc tests revealed that those with a history of only non-collaborative breaches were most likely to report subsequent hiding/lying, and they reported the lowest likelihood of sharing each SITB with a therapist in the future. Those with a history of mixed breach experiences were more likely than those with no breach experience to endorse hiding/lying about subsequent SITBs with a therapist; however, no differences emerged in their self-reported likelihood of disclosing any SITB to a therapist in the future.
Fig. 3:
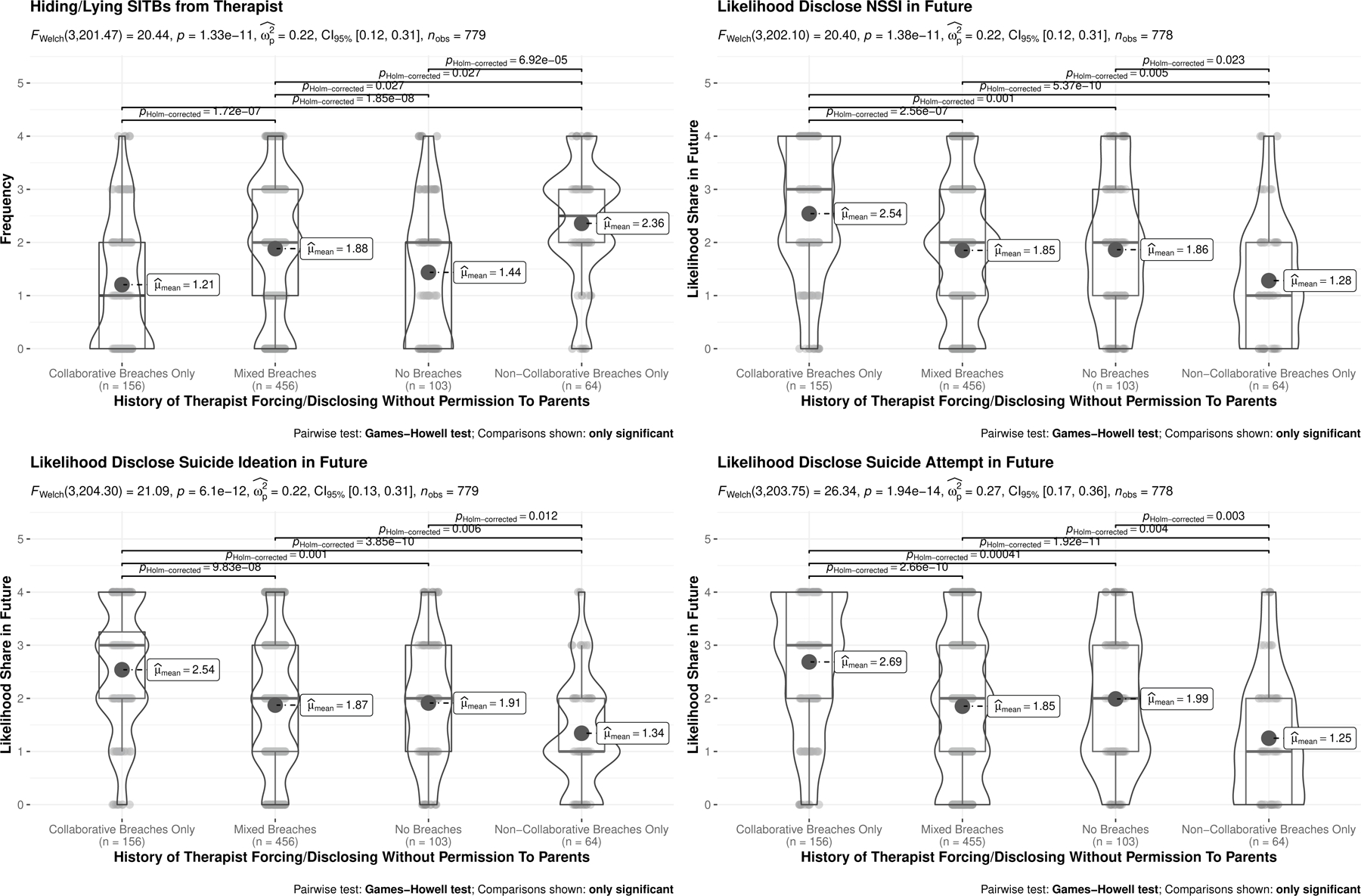
Relationship between type of confidentiality breach and likelihood of future disclosure
Differences in negative, positive, or neutral effects of different forms of confidentiality breaches on therapy-related outcomes are provided in Figure 4. Participants reporting any history of non-collaborative breach most commonly reported negative impacts on all outcomes, including relationship with their current therapist, their trust in mental health professionals more broadly, and their willingness to be honest with therapists in the future. Participants in this group also reported negative impacts on relationships with their parents and willingness to be honest with their parents in the future and negative impacts on mental health, involving exacerbated symptoms of depression, SITB urges, and decreased self-worth. In contrast, participants with only experiences of collaborative confidentiality breaches most commonly reported no impact on relationships with therapists or parents, and also no impact on mental health symptoms (including SITB urges). Instead, many of these participants reported positive impacts on their openness and honesty in therapy in the future and their desire to go to therapy in the future.
Discussion
SITB disclosure is a critical and necessary component of most existing suicide interventions; yet, patterns of adolescent disclosure remain unclear. This study examined to whom and how frequently adolescents disclose SITBs, whether direct querying about SITBs is related to adolescents’ disclosure, and self-reported honesty in and barriers to disclosures to physical and mental healthcare providers. We also examined experiences in which adolescents’ confidentiality was breached by a mental healthcare provider, and associations with key aspects of therapy, relationships, and self-reported future disclosure. Of note, all results are limited by the retrospective self-report design used, and should be interpreted in light of this limitation.
Adolescents with a history of mental health treatment reported overall high rates of disclosing SITBs to people in their lives. Across behaviors and consistent with some prior research (Eskin, 2003), participants report the greatest frequency of disclosure of all SITBs to their friends. Notably, participants reported higher frequency of disclosing NSSI compared to suicide ideation and attempt to specific people (friends, pediatricians, psychiatrists). Relatedly, when disclosing to therapists and medical doctors, participants also reported they were most honest when disclosing NSSI compared to both suicide ideation and attempts. This is the first study to our knowledge to compare rates of disclosure to specific people across NSSI, suicide ideation, and suicide attempts. Findings suggest that there may be something specific to NSSI, perhaps lower perceived risk of hospitalization or greater normalization of NSSI in adolescents, that may make it easier for adolescents to disclose. Alternatively, NSSI may, at times, be spotted on the body, potentially contributing to greater frequency of disclosure. Although some suicide attempts may not be concealable, especially those resulting in substantial physical damage and need for medical care, others are easier to conceal (e.g., minor overdose).
Several barriers to disclosure to healthcare providers were identified, including worry about the provider sharing with their parents, fear of worrying parents, worry about being hospitalized, lack of comfort with the provider, and feeling shame or embarrassment. Findings are promising in that they point to a range of clear provider behaviors that may directly mitigate barriers. Asking clearly and directly about SITBs, normalizing experiences of SITBs during adolescence, and delineating when and how confidentiality has to be breached and when hospitalization is necessary may help to reduce such barriers. Moreover, providing validation and plans for next steps in mental healthcare may be effective tools to reduce anxiety associated with disclosures. Of note, not all barriers were identical across provider type. For example, a barrier to disclosure endorsed by most adolescents for medical care providers (over 60%), yet less frequently for therapists (~15%), is that they did not want to share in front of parents, who were present for medical care visits. These findings emphasize the importance of asking sensitive questions of youth independently, as this may increase likelihood of openness and honesty.
Direct assessment of SITBs was associated with greater rates of disclosure of NSSI, suicide ideation, and suicide attempts across healthcare settings. Although it is unclear from this study if disclosure occurred prior to questions about SITBs, findings are congruent with direct questions in medical settings increasing disclosure of other health risk behaviors (e.g., Grilo et al., 2016). Findings support the importance of directly assessing for SITBs in settings where adolescents receive healthcare services. Results complement research showing that screening for depression in primary care settings is an effective tool to identify and connect adolescents to mental health services (Forman-Hoffman & Viswanathan, 2018), and suggest that both selective and universal screening involving direct SITB assessment can help to identify youth at-risk for subsequent suicidal behavior (DeVylder et al., 2019). Fewer than half of adolescents with a suicide attempt history report receiving any contact with the mental healthcare system in the past year (Wu et al., 2010). Given that youth are more likely to have contact with pediatricians than mental health providers prior to SITB engagement (e.g., Rhodes et al., 2013), equipping pediatricians with tools to screen and refer youth may be particularly important for SITB prevention. More research is needed to test whether each SITB needs to be assessed separately in order to promote disclosure, or whether assessing one or two forms of SITBs increases odds of disclosure across forms.
Results also underscore the importance of disclosure experiences to healthcare providers. Nearly half (48%) of participants reported at least one experience in which a mental health provider either forced them to tell a parent/guardian about their SITB or told their parent/guardian without their permission. These non-collaborative breaches were associated with a host of negative outcomes, including poorer mental health outcomes, lowered trust in therapy, and lower likelihood of honest disclosures in the future. Although there are times where confidentiality breaches are needed (i.e., in cases of high and imminent risk), results highlight that these breaches may have considerable consequences that should be weighed. In cases of moderate risk, results highlight the importance of a collaborative approach to determine what information can be shared with a parent/guardian (e.g., see Helms & Prinstein, 2014). Specific training in responding to SITB disclosures is imperative for both pediatric physical and mental healthcare providers to help to decrease negative outcomes after SITB disclosure.
This work has several key clinical implications. Healthcare providers, including mental healthcare providers are often inadequately trained to assess and respond to SITB disclosures and risk (Gask et al., 2006; Schmitz et al., 2012; Sudak et al., 2007). More comprehensive training in SITB assessment, including appropriate responses to SITB disclosure in adolescents, is needed for both physical and mental healthcare providers. Training across these settings should include clear guidelines for the therapeutic assessment of SITBs in adolescents, which can help to decrease stigmatizing and unhelpful responses, including unnecessary breaches of confidentiality and hospitalizations, and increase the likelihood of future disclosures.
Critically, a large number of participants (between 20–45%) reported that they did not share their SITB histories with their pediatricians, and nearly ¼ (17–36%) reported that they did not share their SITB histories with mental health providers, even when directly asked about these behaviors. Although SITB assessment is a tool for suicide prevention, it cannot be the only tool. Alternative approaches to linking adolescents to mental health and crisis resources may be needed. Following Miller and colleagues (2010) who suggest providing adolescents with resources for intimate partner violence and abuse regardless of disclosure, we suggest that all healthcare providers should consider providing youth with brief psychoeducation about suicide and self-harm, along with crisis hotlines, textlines, and other electronic mental health resources. Such a step may help to normalize and de-stigmatize the experience of SITBs among youth. It would ensure that more adolescents in need get access to these potentially life-saving resources, even in the face of non-disclosure. Moreover, if adolescents are most likely to disclose to friends, peer-focused gatekeeper interventions may be important to further test and, eventually, invest in (King et al., 2009; Pfeiffer et al., 2019). Related to this issue: increasing rates of disclosure cannot be the only step in suicide prevention for youth; we must invest in creating and disseminating effective treatments for youth mental health across settings. Despite high rates of SITBs in adolescents, only a minority of SITB treatments have been tested this population to date (Fox, Huang, et al., 2020). This is a critical gap that must be addressed.
Results should be interpreted in light of study limitations. First, study completion took, on average, 45 minutes (after removing participants who took clear breaks across several days), and there was substantial attrition from study start to finish. Because demographic measures were assessed last, it was impossible to test whether key demographics (race/ethnicity, age, gender, socioeconomic status) impacted study completion. Given prior research showing these factors impact completion among other online teen samples (Thoma et al., 2019), we anticipate that results may overly represent the perspectives of white, female gender, and higher socioeconomic status adolescents. Second, although the sample is both gender and sexual orientation-diverse, a minority of participants identified as cisgender male, Black, and/or Indigenous. Future research is needed to assess whether results generalize to these and other populations. Third, all responses were based on retrospective self-report from a single perspective using novel items, and they did not assess the time course of disclosures. As such, the directionality of relationships observed remains unclear; for example, it is unclear whether providers’ asking about SITBs increased disclosure. Instead, it is possible that because a participant had engaged in and disclosed a SITB, their provider asked them follow-up questions about their SITBs. Future research assessing adolescent-therapist/psychiatrist/parent/friend dyads, and particularly assessing disclosure experiences and subsequent mental health outcomes across time, are needed. Fourth, most participants reported a history of a therapist engaging in both collaborative and non-collaborative breaches of confidentiality, with only a minority reporting exclusive non-collaborative breaches; future research with larger samples including greater heterogeneity in these experiences are needed to determine the stability of these findings. Finally, participants were recruited based on their history of both SITBs and mental health treatment, and most participants endorsed engaging in both NSSI and suicide ideation. Rates of disclosure may differ in a treatment naive sample, and a sample reporting fewer SITBs. Future research should consider extending this research in those directions. Youth denying prior mental health treatment may be particularly important to evaluate for SITB disclosure patterns and barriers in order to develop targeted interventions to increase help seeking and attainment.
The present study provides the first extensive overview of adolescents’ experiences with disclosing SITBs to key people in their lives, including parents, friends, and healthcare professionals. Unlike most studies on this topic, requirements for parental consent were waived, likely increasing participant willingness to participate and subsequent honesty in this study (as corroborated by Lothen-Kline et al., 2003). Results have key implications for healthcare providers to increase likelihood of adolescent SITB disclosure, and to better understand potential impacts of breaching confidentiality to parents on adolescent honesty, treatment, and longer-term likelihood of disclosure.
Supplementary Material
References
- Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K, Kiernan K, Davies S, Bickley H, & Parsons R (1999). Suicide within 12 months of contact with mental health services: National clinical survey. BMJ, 318(7193), 1235–1239. 10.1136/bmj.318.7193.1235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes LS, Ikeda RM, & Kresnow M (2002). Help-Seeking Behavior Prior to Nearly Lethal Suicide Attempts. Suicide and Life-Threatening Behavior, 32(s1), 68–75. 10.1521/suli.32.1.5.68.24217 [DOI] [PubMed] [Google Scholar]
- Burke TA, Ammerman BA, Hamilton JL, Stange JP, & Piccirillo M (2020). Nonsuicidal self-injury scar concealment from the self and others. Journal of psychiatric research, 130, 313–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calear AL, & Batterham PJ (2019). Suicidal ideation disclosure: Patterns, correlates and outcome. Psychiatry research, 278, 1–6. [DOI] [PubMed] [Google Scholar]
- Cheng TL, Savageau JA, Sattler AL, & DeWitt TG (1993). Confidentiality in Health Care: A Survey of Knowledge, Perceptions, and Attitudes Among High School Students. JAMA, 269(11), 1404–1407. 10.1001/jama.1993.03500110072038 [DOI] [PubMed] [Google Scholar]
- Drum DJ, Brownson C, Burton Denmark A., & Smith SE (2009). New data on the nature of suicidal crises in college students: Shifting the paradigm. Professional Psychology: Research and Practice, 40(3), 213–222. 10.1037/a0014465 [DOI] [Google Scholar]
- Encrenaz G, Kovess-Masféty V, Gilbert F, Galéra C, Lagarde E, Mishara B, & Messiah A (2012). Lifetime risk of suicidal behaviors and communication to a health professional about suicidal ideation. Results from a large survey of the French adult population. Crisis, 33(3), 127–136. 10.1027/0227-5910/a000113 [DOI] [PubMed] [Google Scholar]
- Eskin M (2003). A cross-cultural investigation of the communication of suicidal intent in Swedish and Turkish adolescents. Scandinavian Journal of Psychology, 44(1), 1–6. 10.1111/1467-9450.t01-1-00314 [DOI] [PubMed] [Google Scholar]
- Forman-Hoffman VL, & Viswanathan M (2018). Screening for Depression in Pediatric Primary Care. Current Psychiatry Reports, 20(8), 62. 10.1007/s11920-018-0926-7 [DOI] [PubMed] [Google Scholar]
- Fox KR, Choukas-Bradley S, Salk RH, Marshal MP, & Thoma BC (2020). Mental health among sexual and gender minority adolescents: Examining interactions with race and ethnicity. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulginiti A, & Frey LM (2019). Exploring suicide-related disclosure motivation and the impact on mechanisms linked to suicide. Death studies, 43(9), 562–569. [DOI] [PubMed] [Google Scholar]
- Gask L, Dixon C, Morriss R, Appleby L, & Green G (2006). Evaluating STORM skills training for managing people at risk of suicide. Journal of Advanced Nursing, 54(6), 739–750. 10.1111/j.1365-2648.2006.03875.x [DOI] [PubMed] [Google Scholar]
- Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, & Colditz GA (2001). Adolescents’ Perceptions of Social Status: Development and Evaluation of a New Indicator. PEDIATRICS, 108(2), e31–e31. 10.1542/peds.108.2.e31 [DOI] [PubMed] [Google Scholar]
- Grilo SA, Catallozzi M, Santelli JS, Yan H, Song X, Heitel J, … & Klein JD (2019). Confidentiality discussions and private time with a health-care provider for youth, United States, 2016. Journal of Adolescent Health, 64(3), 311–318. [DOI] [PubMed] [Google Scholar]
- Hom MA, Stanley IH, Podlogar MC, & Joiner TE (2017). “Are You Having Thoughts of Suicide?” Examining Experiences With Disclosing and Denying Suicidal Ideation. Journal of Clinical Psychology, 73(10), 1382–1392. 10.1002/jclp.22440 [DOI] [PubMed] [Google Scholar]
- King CA, Klaus N, Kramer A, Venkataraman S, Quinlan P, & Gillespie B (2009). The Youth-Nominated Support Team-Version II for suicidal adolescents: A randomized controlled intervention trial. Journal of Consulting and Clinical Psychology, 77(5), 880–893. 10.1037/a0016552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, May AM, & Glenn CR (2013). The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. Journal of abnormal psychology, 122(1), 231. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, & Pearson JL (2002). Contact With Mental Health and Primary Care Providers Before Suicide: A Review of the Evidence. The American Journal of Psychiatry, 159(6), 909–916. 10.1176/appi.ajp.159.6.909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars B, Heron J, Crane C, Hawton K, Kidger J, Lewis G, Macleod J, Tilling K, & Gunnell D (2014). Differences in risk factors for self-harm with and without suicidal intent: Findings from the ALSPAC cohort. Journal of Affective Disorders, 168, 407–414. 10.1016/j.jad.2014.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mérelle S, Foppen E, Gilissen R, Mokkenstorm J, Cluitmans R, & Van Ballegooijen W (2018). Characteristics Associated with Non-Disclosure of Suicidal Ideation in Adults. International Journal of Environmental Research and Public Health, 15(5), 943. 10.3390/ijerph15050943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Prevalence, Correlates, and Treatment of Lifetime Suicidal Behavior Among Adolescents: Results From the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300. 10.1001/2013.jamapsychiatry.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Surgeon General (US), & National Action Alliance for Suicide Prevention (US). (2012). 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action: A Report of the U.S. Surgeon General and of the National Action Alliance for Suicide Prevention. US Department of Health & Human Services (US). http://www.ncbi.nlm.nih.gov/books/NBK109917/ [PubMed] [Google Scholar]
- Pfeiffer PN, King C, Ilgen M, Ganoczy D, Clive R, Garlick J, Abraham K, Kim HM, Vega E, Ahmedani B, & Valenstein M (2019). Development and pilot study of a suicide prevention intervention delivered by peer support specialists. Psychological Services, 16(3), 360–371. 10.1037/ser0000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rae WA (2002). Adolescent Health Risk Behavior: When Do Pediatric Psychologists Break Confidentiality? Journal of Pediatric Psychology, 27(6), 541–549. 10.1093/jpepsy/27.6.541 [DOI] [PubMed] [Google Scholar]
- Reddy DM (2002). Effect of Mandatory Parental Notification on Adolescent Girls’ Use of Sexual Health Care Services. JAMA, 288(6), 710. 10.1001/jama.288.6.710 [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, & Nock MK (2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychological medicine, 46(2), 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenrot SA, & Lewis SP (2020). Barriers and responses to the disclosure of non-suicidal self-injury: A thematic analysis. Counselling Psychology Quarterly, 33(2), 121–141. [Google Scholar]
- Schmitz WM, Allen MH, Feldman BN, Gutin NJ, Jahn DR, Kleespies PM, Quinnett P, & Simpson S (2012). Preventing Suicide through Improved Training in Suicide Risk Assessment and Care: An American Association of Suicidology Task Force Report Addressing Serious Gaps in U.S. Mental Health Training. Suicide and Life-Threatening Behavior, 42(3), 292–304. 10.1111/j.1943-278X.2012.00090.x [DOI] [PubMed] [Google Scholar]
- Sheehan L, Oexle N, Armas SA, Wan HT, Bushman M, Glover L, & Lewy SA (2019). Benefits and risks of suicide disclosure. Social Science & Medicine, 223, 16–23. [DOI] [PubMed] [Google Scholar]
- Simone AC, & Hamza CA (2020). Examining the disclosure of nonsuicidal self-injury to informal and formal sources: a review of the literature. Clinical psychology review, 101907. [DOI] [PubMed] [Google Scholar]
- Singer JB, Erbacher TA, & Rosen P (2019). School-Based Suicide Prevention: A Framework for Evidence-Based Practice. School Mental Health, 11(1), 54–71. 10.1007/s12310-018-9245-8 [DOI] [Google Scholar]
- Smith DM, Lipson SM, Wang SB, & Fox KR (2021). Online methods in adolescent self-injury research: challenges and recommendations. Journal of Clinical Child & Adolescent Psychology, 1–12. [DOI] [PubMed] [Google Scholar]
- Sudak D, Roy A, Sudak H, Lipschitz A, Maltsberger J, & Hendin H (2007). Deficiencies in Suicide Training in Primary Care Specialties: A Survey of Training Directors. Academic Psychiatry, 31(5), 345–349. 10.1176/appi.ap.31.5.345 [DOI] [PubMed] [Google Scholar]
- Swannell SV, Martin GE, Page A, Hasking P, & St John NJ (2014). Prevalence of Nonsuicidal Self-Injury in Nonclinical Samples: Systematic Review, Meta-Analysis and Meta-Regression. Suicide and Life-Threatening Behavior, 44(3), 273–303. 10.1111/sltb.12070 [DOI] [PubMed] [Google Scholar]
- Thoma BC, Salk RH, Choukas-Bradley S, Goldstein TR, Levine MD, & Marshal MP (2019). Suicidality Disparities Between Transgender and Cisgender Adolescents. Pediatrics, 144(5), e20191183. 10.1542/peds.2019-1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson PO, Qiu T, Neufeld S, Jones PB, & Goodyer IM (2018). Sporadic and recurrent non-suicidal self-injury before age 14 and incident onset of psychiatric disorders by 17 years: Prospective cohort study. The British Journal of Psychiatry, 212(4), 222–226. 10.1192/bjp.2017.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


