Abstract
Purpose
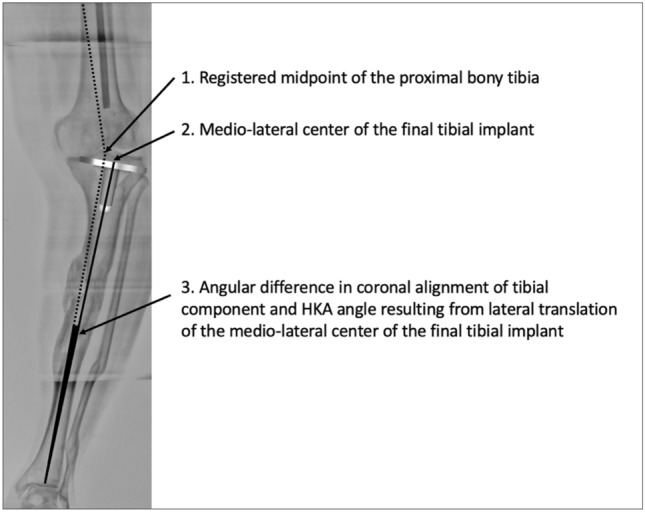
Placement of prosthetic components and limb alignment can be adversely impacted by errors in identification of registration points in digitally assisted knee arthroplasty. The purpose of this study was to trigonometrically analyze the impact on the accuracy of coronal tibial component and limb alignment of discrepancy between the registered midpoint of the proximal bony tibia vis-à-vis the radiographic medio-lateral center of the lateralized final tibial implant in certain varus-deformed knees.
Methods
We analyzed trigonometrically the angular difference in coronal alignment of tibial component and hip–knee–ankle angle resulting from lateral translation of the medio-lateral center of the final tibial implant, with respect to the initial registered midpoint of the proximal bony tibia. was calculated using the equation tan() = d/t, where d is the numerical distance between the registered point and the center of the final tibial tray position and t is the length of tibia distal to the resection.
Results
One degree of varus malpositioning of the tibial component and the limb can occur for every 6.3 mm of lateral translation of the tibial implant with respect to the midpoint of the proximal bony tibia of average reported length (372 mm). The magnitude of this error is inversely proportional to tibial length and the patient’s height.
Conclusions
Coronal malalignment of the tibial component and the limb is directly proportional to the amount of lateral translation of the tibial tray with respect to the registered midpoint of the proximal bony tibia and inversely proportional to the patient’s height. This may occur in cases with tibial extra-articular deformity, those undergoing reduction osteotomy, downsizing of the tray, or inadvertently during tibial preparation. The error can be avoided by initial registration of the tibial midpoint more laterally by templating, re-registering the new center of the resected tibial surface or osteotomy for extra-articular deformity.
Graphical Abstract
Keywords: Total knee arthroplasty, Computer-assisted knee arthroplasty, Robotic knee arthroplasty, Malalignment
Purpose
Placement of components and restoration of limb alignment can be adversely impacted by several factors that include the accuracy of bone cuts and achieving ligament balance [9, 15]. Navigation, robotics and patient-specific instrumented (PSI) can help improve positioning of the tibial tray, in particular [3, 6, 22]. However, the author has occasionally noted errors in overall alignment on final long-leg radiographs despite navigational data attesting to the accuracy of registration, correct bone cuts, extension gap balance, and intra-operative limb alignment (Fig. 1). Hence, an attempt was made to discover a possible cause of this observation.
Fig. 1.
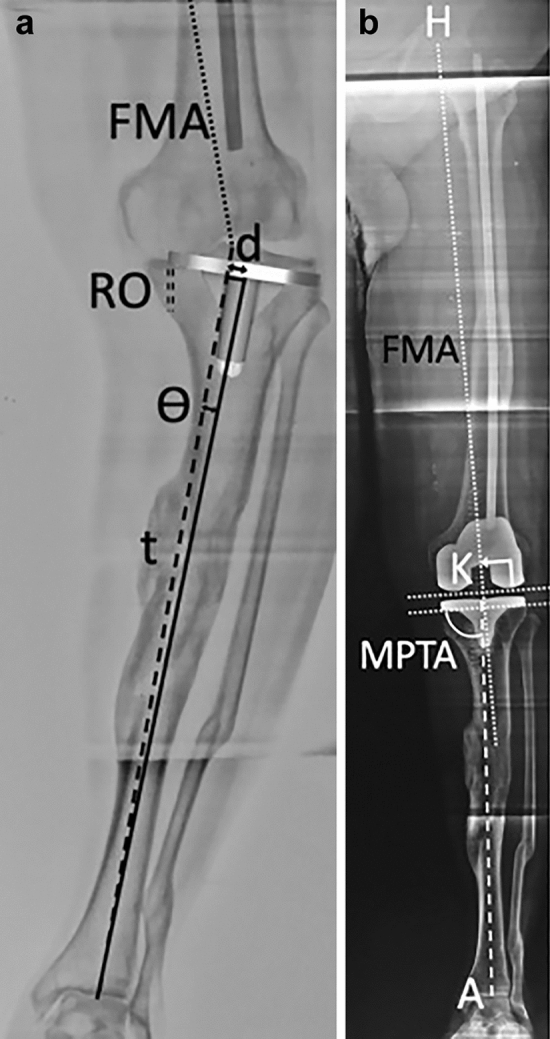
a Illustrates the trigonometric calculation of resultant error (). FMA represents the femoral mechanical axis (dotted line). TMA is the dashed line between initial registration point (midpoint between the tibial eminences) on upper tibia and center of ankle joint. The solid line connects the center of the tibial implant and the center of the ankle joint. ‘d’ equals the distance between the initial registration point and final center of tibial implant after reduction osteotomy (RO) indicated by a double dashed line. ‘t’ is the length of tibia distal to the tibial resection plane. b Shows the postoperative antero-posterior full-length radiograph where computer navigation settings were dialed in to restore mechanical alignment for both components (i.e., 90° to their respective mechanical axes in the coronal plane) and the limb. Tibial registration was at the midpoint between the tibial eminences. The dotted line shows the femoral component to be orthogonal to the FMA. However, both MPTA and HKA show the tibial component and limb to be in varus
Usually, the point registered as the center of the bony tibial plateau will coincide with the center of the final tibial implant. However, the two points may not be coincident in all patients. This may occur in patients with extra-articular deformity of the tibia due to developmental causes (metaphyseal tibia vara), proximal tibia osteotomy, malunited upper tibial fracture, osteomalacia, and Paget’s disease [13]. It may also occur in patients undergoing reduction osteotomy [14] to correct severe varus deformity where the posteromedial prominence of tibia is excised (Fig. 1). Other patients include those in whom the tibial tray is deliberately lateralized, downsized, and lateralized to maintain compatibility with the femoral component size, and also where the tray is inadvertently lateralized during tibial preparation.
Registration performed intra-operatively corresponds with the ‘recommended’ landmark of the midpoint between the tibial eminences [16]; this point can be measured on preoperative radiographs. However, this point is not available on postoperative radiographs (as the proximal tibia has been resected); the point used to measure hip–knee–ankle angle (HKA) is the medio-lateral center of the tibial implant. Likewise, no software for navigation or robotic-assisted TKA has this written into it for analysis. As these two points may not coincide in certain cases and neither a direct radiographic measurement nor a software-based calculation is possible, a trigonometric analysis needs to be used so as not to miss this potential source of error. A similar study has been reported using virtual modelling to determine the impact of variation of tibial tray rotation and posterior slope on coronal alignment [5]. The hypothesis of the present study was that if the registered midpoint of the proximal bony tibia does not coincide with the medio-lateral center of the final tibial implant it could result in inaccuracy in coronal tibial component and limb alignment.
Methods
We performed a trigonometric analysis of the resultant angular difference () in coronal alignment of tibial component and the limb resulting from lateral translation of the medio-lateral center of the final tibial implant with respect to the initial registered midpoint of the bony tibia. Radiographic measurements were made according to published methods [18]. Coronal limb alignment was measured as the HKA angle—the angle between femoral mechanical axis (line joining femoral head center to apex of the intercondylar notch) and the tibial mechanical axis, TMA (formed by the line joining the center of the tibial tray to the center of the ankle joint). Coronal alignment of the tibial component was measured as the MPTA—the medial angle between the tibial tray and the tibial mechanical axis (TMA). The recommended registration point for the proximal tibia during navigated TKA was the midpoint between the tibial intercondylar eminences [19].
Figure 1a depicts the method by which θ is measured. This is calculated using the numerical distance (d) between the registered point and the center of the final tibial tray position and the length of the tibia distal to the resection (t). The tangent of the angular difference between the preoperative and the postoperative TMA (angle ) in a right-angled triangle is the length of the side (d) opposite the angle divided by the length of the adjacent side (t). Thus tan() = d/t. From this, the resultant angular difference () can be calculated from trigonometry tables for any length of tibia.
All patients gave informed consent for surgery, for having their radiographs measured and analysed, and data from navigation software analysed. The study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. Institutional Ethics Committee approval was not warranted as the study was not a clinical study but a trigonometric analysis of data collected routinely.
Results
Using the equation tan() = d/t, one can compute the expected error. The expected errors for different amounts of lateral translation using a tibia of average length [1] as an example are shown in Table 1. For tibiae of any specific length, the error can be similarly calculated. In the example, we have used the average reported tibial length of the tibia which is 372 mm [1] and the length distal to the resection (t) is taken to be 364 mm, obtained by subtracting 8 mm of resected proximal tibia.
Table 1.
Trigonometric calculation of resultant error in medial proximal tibial angle (MPTA) and hip–knee–ankle axis (HKA) depending on distance between initial registration point on tibia and final lateralized center of tibial implant
| Distance between initial registration point on tibia and final center of tibial implant (mm) | Angular error in MPTA and HKA (in degrees) (°) |
|---|---|
| 6.2 | 1 |
| 12.5 | 2 |
| 18.8 | 3 |
| 25.1 | 4 |
| 31.4 | 5 |
The length of the tibia is 360 mm in this case
The greater the distance between the registered point and the center of the final tibial tray position, the greater will be the varus positioning of the tibial component and the limb. The shorter the patient, the greater will be the error, since a person’s height correlates with tibial length [4, 12]. As is calculated as a ratio of two lengths, it is independent of the magnification factor of radiographs.
Figures 2, 3 and 4 further serve to highlight this potential pitfall. They are full-length standing radiographs of a patient with a malunited proximal tibial fracture. In Fig. 2a, C1 represents the point on the tibial articular surface corresponding to the templated center of the tibial component equidistant from the medial and lateral resected tibial margins; the resection plane P1 is such that the resected lateral tibia is of an appropriate thickness and is perpendicular to the line from C1 to center of the ankle (the postoperative TMA). In Fig. 2b, C2 represents the proximal end of the tibial mechanical axis (TMA) corresponding to the midpoint between the tibial eminences. P2 is the resection plane perpendicular to the preoperative TMA. In patients with medial bone loss or obesity, a long-stemmed tibial component may be deployed and, when based off C1, the stem will be correctly centered in the canal (Fig. 3a). If the midpoint of the tibial component was to be centered on C2, the stem would impinge against the medial cortex (Fig. 3b) and the tibial component would necessarily have to be translated laterally (Fig. 3c). Similar would be the case for any other situation, deliberate or inadvertent, where the tibial component is laterally translated. In so doing, the registered center of the proximal tibia will no longer coincide with the final tibial tray center. The ‘final’ radiographs have been digitally manipulated (Fig. 4a, b) to show the tibial component aligned exactly parallel (assuming perfect extension balance) to the distal femoral resection line D which is orthogonal to the femoral mechanical axis FM. In Fig. 4a, where the tibial component positioning was templated and registered such that the tibial tray center would lie at C1, medial proximal tibial angle (MPTA) is 90° (angle V) and HKA is 180°. In Fig. 4b, the tibia was cut exactly perpendicular to the preoperative TMA, but the tibial component was translated laterally. The center of the tibial component is thus lateral to C2. When the tibial component is measured in relationship to the postoperative TMA, MPTA is in varus (angle Va). Likewise the HKA, also shows the limb to be in varus. Though classical mechanical alignment has been illustrated for simplicity, the same would apply to anatomical and kinematic alignment.
Fig. 2.
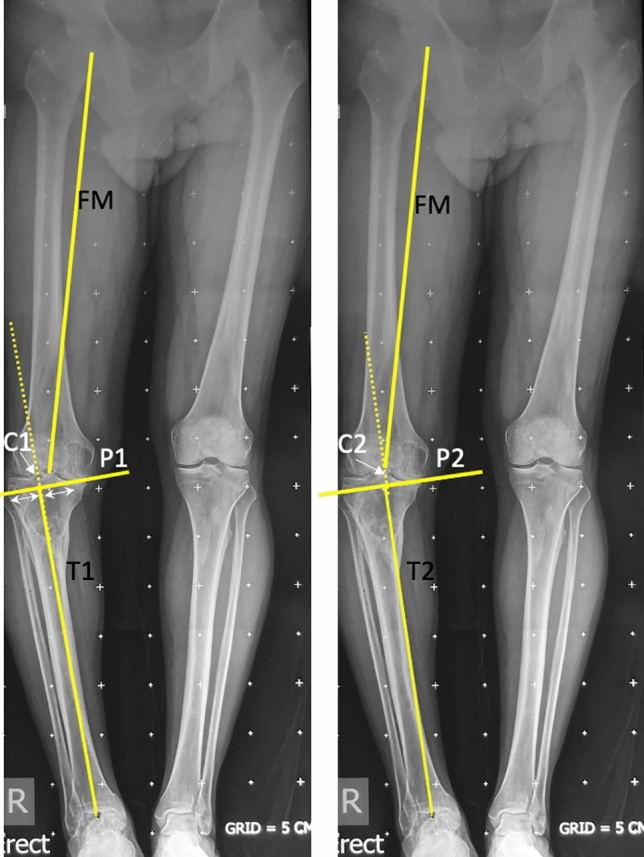
a (Left) Depicts a full-length standing radiograph of a patient with a malunited proximal tibial fracture. C1 represents the point on the tibial articular surface corresponding to the templated center of the final tibial component; the resection plane P1 is such that the resected lateral tibia is of an appropriate thickness and is perpendicular to the line from C1 to center of the ankle. b (Right) C2 represents the proximal end of the tibial mechanical axis MA corresponding to the midpoint between the tibial eminences. P2 is the resection plane perpendicular to MA
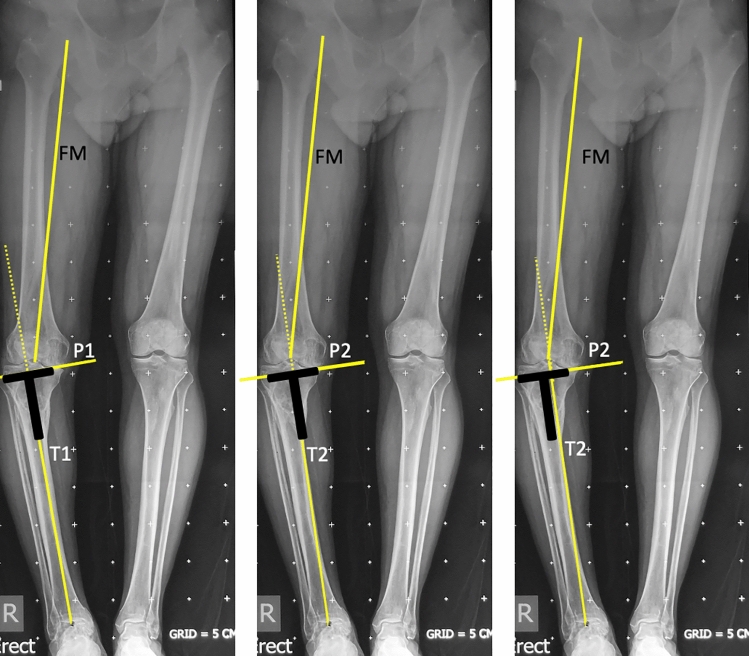
Fig. 3.
a (left): shows a stylized tibial component with stem extension that is correctly centered in the canal based on C1. b (center): shows that if the medio-lateral midpoint of the articular surface of the tibial component were to be centered on C2, the stem would impinge against the medial cortex and the tibial component would necessarily translate laterally to the position shown in Fig. 2c. c (right): shows correct lateral placement of the tibial component
Fig. 4.
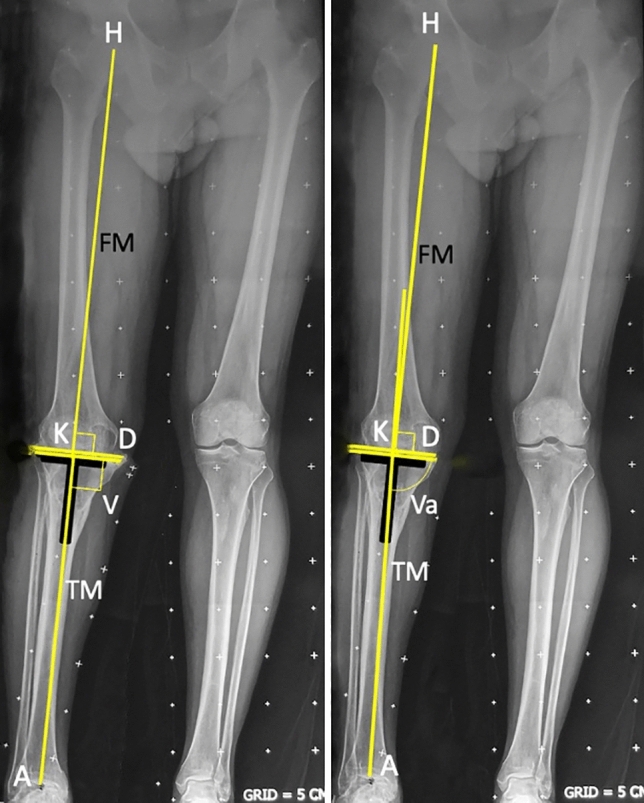
a (left): shows the tibial component aligned exactly parallel to the distal femoral resection line D which is orthogonal to the femoral mechanical axis FM; the tibial component positioning was templated and registered such that the tibial tray center was at C1. MPTA is 90° and HKA angle is 180°. b (right): shows the tibial component aligned exactly parallel to the distal femoral resection line; the tibia was cut exactly perpendicular to the preoperative MA, and the midpoint of the tibial component was translated lateral to point C2. The HKA angle and MPTA are in varus
Discussion
The most important finding of this study was that, for a tibia of average reported length, 1° of varus malpositioning of the tibial component and the limb can occur for every 6.3 mm of lateral translation of the tibial implant with respect to the registered midpoint of the proximal bony tibia; furthermore, the magnitude of this error is inversely proportional to tibial length and thus to the patient’s height [4, 12].
This varus ‘malpositioning’ is in reality a planning error. It is the outcome of using different landmarks: one at the beginning of surgery, and then another on postoperative radiographs. If the same landmarks were used on both occasions, this problem and error would be non-existent, which is the point that this study wishes to convey. The HKA and medial proximal tibial angle (MPTA) measured postoperatively utilize the center of the tibial implant [19]; the line representing the postoperative tibial axis connecting this point and the center of the ankle joint may thus be different from the one used intra-operatively (center of the bony tibia). It is in patients with tibial extra-articular deformity, those undergoing reduction osteotomy (Fig. 1a), downsizing of the tibia, or deliberate/inadvertent lateral translation of the tray during tibial preparation that this situation may arise (Fig. 1b). In cases with extra-articular deformity (EAD), another option to pre-empt this situation would be to perform a corrective osteotomy which may add complexity, and could be done as a prior procedure to correct EAD [13]. Lack of ligament balancing is another potential cause of malalignment [15], though this is not the topic of this study. Gap balancing (which is used by the author) rather that measured resection has been shown to reduce the number of outliers [8].
Studies using conventional instrumentation have recognized the problem of tibial deformity and have recommended different amounts of lateralization of the tibial cutting jig. These include 15 mm lateral placement [11], always using the lateral intercondylar eminence resulting in some valgus cuts [7], using Kennedy–White Zones 3 and 4 [17], and resecting more thickness of tibia [20]. Shao et al. [21] reported 15% outliers despite using the lateral intercondylar eminence.
The limitations of this study are that it is a trigonometric calculation. It is not a clinical study, but one aiming to alert surgeons of the possibility of an alignment error based on the author’s observations. The computer software does not permit analysis of the distance between an initial registration point and a new one that may supersede it at a later stage; hence no statistical analyses could be performed. The registration performed intra-operatively corresponds with the ‘recommended’ landmark of the midpoint between the tibial eminences; this point can be measured on preoperative radiographs. However, this point is not available on postoperative radiographs and may not coincide with the point used to measure HKA (medio-lateral center of the tibial implant) if implant is lateralized, thereby necessitating a trigonometric analysis. Also the cohort is not well-defined, nor have we stated inclusion and exclusion criteria, as the study alludes to a heterogenous group of cases in which this error is likely to be made. Further, there may be a concomitant rotational element to extra-articular deformities—not addressed in this study—which may need to be considered in the surgical technique. Lastly, the surgeon must also bear in mind that changes in posterior tibial slope, which are not evaluated in this study, may combine with tibial tray rotation leading to outliers in coronal alignment [5]. A recent virtual modelling study [5] has shown that coronal alignment of the tibial cut changes by 0.07° per degree of axial rotation and 0.22° per degree of posterior slope. There can be several other sources contributing to malalignment such as uneven cement mantle and incorrect ankle center registration.
This potentially avoidable cause of error has not been previously highlighted in techniques requiring registration of the tibial center. Surgeons and engineers involved in planning of digitally assisted TKA oblivious to this error will continue to be surprised to find inaccuracies on measuring the final tibial component placement and limb alignment despite precise cuts [2, 10, 15, 23]. This may be wrongly attributed to the computer or robotic software, cutting errors, or radiographic measurement errors.
A couple of degrees of varus error on the tibial side along with tray malrotation and incorrect tibial slope or a couple of degrees of additional varus on the femoral side, deliberate or accidental, may be additive and a harbinger of implant failure [24]. Even if the error is not substantial in most cases, it can be avoided by initial registration of the tibial midpoint more laterally by careful templating. The distance to be lateralized is half the medio-lateral width of the reduction osteotomy/osteophyte being excised, or half the width of the uncovered medial tibial surface resulting from lateralization or downsizing the tibial tray. If the computer or robotic system software permits (as most systems do), surgeons can re-register the center of the bony tibia to the correct center of the trial tibial implant, and verify tibial component and limb alignment, so that this avoidable cause of error can be mitigated.
Conclusions
The magnitude of coronal malalignment of the tibial component and the limb is directly proportional to the amount of lateral translation of the tibial tray with respect to the midpoint of the registered proximal bony tibia and inversely proportional to the patient’s height. The error can be avoided by initial registration of the tibial midpoint more laterally by careful templating, re-registering the new center of the resected tibial surface, or osteotomy for extra-articular deformity.
Author contributions
AM analyzed and interpreted the patient data, contributed in writing the manuscript, read and approved the final manuscript.
Funding
No funds, grants, or other support was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The author has no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval and consent to participate
Not required, as it is a trigonometric analysis of radiographic measurements.
Consent for publication
Consent for publication was obtained from all patients to publish their data in any form (including any individual details, images or videos).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Attada P, Ravindranadh G, Kumari K. Anthropometric measurement of maximum tibia length in south Indian population. Anatomical Sciences. 2018;15:57–64. [Google Scholar]
- 2.Bae DK, Song SJ, Heo DB, Tak DH. Does the severity of preoperative varus deformity influence postoperative alignment in both conventional and computer-assisted total knee arthroplasty? Knee Surgery, Sports Traumatology Arthroscopy. 2013;21:2248–2254. doi: 10.1007/s00167-012-2263-4. [DOI] [PubMed] [Google Scholar]
- 3.Bäthis H, Perlick L, Tingart M, Lüring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. The Journal of Bone and Joint Surgery. 2004;B86:682–687. doi: 10.1302/0301-620X.86B5.14927. [DOI] [PubMed] [Google Scholar]
- 4.Chavan SK, Chavan KD, Mumbre SS, Makhani CS. Stature and percutaneus tibial length: A correlational study in Maharashtrian population. Journal of Indian Academy of Forensic Medicine and Pathology. 2009;2(3):334–337. [Google Scholar]
- 5.Dima D, Huang P, Suryanarayan P, Rosen A, Dima DD. Tibial tray rotation and posterior slope increase risk for outliers in coronal alignment: A virtual modelling investigation. Bone Joint Journal. 2020;102:43–48. doi: 10.1302/0301-620X.102B6.BJJ-2019-1533.R1. [DOI] [PubMed] [Google Scholar]
- 6.Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK. Meta-analysis of navigation vs conventional total knee arthroplasty. Journal of Arthroplasty. 2012;27:1177–1182. doi: 10.1016/j.arth.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 7.Kim SM, Kim KW, Cha SM, Han KY. Proximal tibial resection in varus-deformed tibiae during total knee arthroplasty: An in vitro study using sawbone model. International Orthopaedics. 2015;39:429–434. doi: 10.1007/s00264-014-2485-9. [DOI] [PubMed] [Google Scholar]
- 8.Li S, Luo X, Wang P, Sun H, Wang K, Sun X. Clinical outcomes of gap balancing vs measured resection in Total Knee Arthroplasty : A systematic review and meta-analysis involving 2259 subjects. Journal of Arthroplasty. 2018;33(8):2684–2693. doi: 10.1016/j.arth.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 9.MacDessi SJ, Wood JA, Diwan AD, Harris IA. Surgeon-defined assessment is a poor predictor of knee balance in total knee arthroplasty: A prospective, multicenter study. Knee Surgery, Sports Traumatology, Arthrosc. 2021;29:498–506. doi: 10.1007/s00167-020-05925-6. [DOI] [PubMed] [Google Scholar]
- 10.Marchand R, Sodhi N, Khlopas A, Sultan A, Higuera CA, Stearns KL, Mont MA. Coronal correction for severe deformity using robotic-assisted total knee arthroplasty. The Journal of Knee Surgery. 2018;31:2–5. doi: 10.1055/s-0037-1608840. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda S, Mizu-uchi H, Miura H, Nagamine R, Urabe K, Iwamoto Y. Tibial shaft axis does not always serve as a correct coronal landmark in total knee arthroplasty for varus knees. Journal of Arthroplasty. 2003;18:56–62. doi: 10.1054/arth.2003.50002. [DOI] [PubMed] [Google Scholar]
- 12.Mehta AA, Mehta AA, Gabhije VM, Verma S. Correlation of percutaneous tibial length with body height and estimation of stature in living central India population. International Journal of Anatomy and Research. 2015;3(2):1159–1161. doi: 10.16965/ijar.2015.187. [DOI] [Google Scholar]
- 13.Mullaji A, Shetty GM. Computer-assisted total knee arthroplasty for arthritis with extra-articular deformity. Journal of Arthroplasty. 2009;24:1164–1169. doi: 10.1016/j.arth.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Mullaji AB, Shetty GM. Correction of varus deformity during TKA with reduction osteotomy knee. Clinical Orthopaedics Related Research. 2014;472:126–132. doi: 10.1007/s11999-013-3077-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mullaji AB, Shetty GM, Lingaraju AP, Bhayde S. Which factors increase risk of malalignment of the hip-knee-ankle axis in TKA? Clinical Orthopaedics Related Research. 2013;471:134–141. doi: 10.1007/s11999-012-2520-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.No authors listed. (2015) No Title. Knee ver 3.1 Software User Guide Revision 1.1 Brainlab AG Germany
- 17.Palanisami D, Jagdishbhai CP, Manohar M, Ramesh P, Natesan R, Shanmuganathan R. Improving the accuracy of tibial component placement during total knee replacement in varus knees with tibial bowing: A prospective randomised controlled study. The Knee. 2019;26:1088–1095. doi: 10.1016/j.knee.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Paley D. What is alignment and malalignment. In: Thienpont E, editor. Improving accuracy in knee arthroplasty. Jaypee Brothers Medical Publishers; 2012. pp. 1–17. [Google Scholar]
- 19.Park A, Stambough JB, Nunley RM, Barrack RL, Nam D. The inadequacy of short knee radiographs in evaluating coronal alignment after total knee arthroplasty. Journal of Arthroplasty. 2016;31(4):878–882. doi: 10.1016/j.arth.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 20.Saibaba B, Dhillon MS, Chouhan DK, Kanojia RK, Prakash M, Bachhal V. Significant incidence of extra-articular tibia vara affects radiological outcome of total knee arthroplasty. Knee Surg Related Research. 2015;27:173–180. doi: 10.5792/ksrr.2015.27.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shao H, Chen C, Scholl D, Faizan A, Chen AF. Tibial shaft anatomy differs between Caucasians and East Asian individuals. Knee Surgery, Sports Traumatology, Arthrosc. 2018;26:2758–2765. doi: 10.1007/s00167-017-4724-2. [DOI] [PubMed] [Google Scholar]
- 22.Tandogan RN, Kort NP, Ercin E, et al. Computer-assisted surgery and patient-specific instrumentation improve the accuracy of tibial baseplate rotation in total knee arthroplasty compared to conventional instrumentation: A systematic review and meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy. 2021 doi: 10.1007/s00167-021-06495-x. [DOI] [PubMed] [Google Scholar]
- 23.Thienpont E, Schwab PE, Fennema P. Efficacy of patient-specific instruments in total knee arthroplasty. Journal of Bone and Joint Surgery. American Volume. 2017;99:521–530. doi: 10.2106/JBJS.16.00496. [DOI] [PubMed] [Google Scholar]
- 24.Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. Journal of Biomechanics. 2005;38:349–355. doi: 10.1016/j.jbiomech.2004.02.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.