Abstract
Purpose
To review patient outcomes in the literature following arthroscopic partial meniscectomy (APM) in order to identify when patients report reaching subjective maximal improvement postoperatively.
Methods
A systematic review of the literature from January 2004 to August 2019 was conducted using PRISMA guidelines to identify articles evaluating patient-reported outcome measures (PROMs) up to a minimum of 6 months after APM in patients >18 years old. Studies were excluded if additional interventions were performed such as repairs, ligamentous reconstruction or repair, cartilaginous manipulation, or revision surgery. PROMs were pooled between studies at preoperative, 3 months, 6 months, 1 year, and 2 year time points. Weighted averages were used within a mixed model method in order to account for the differences in sample size and variance among studies. Significant improvements in PROMs at various time intervals were statistically analyzed using minimal clinically important difference.
Results
A total of 12 studies including 1663 patients who underwent APM were selected for the review. The pooled cohort consisted of 1033 (62%) males and 630 (38%) females. Significant improvements were demonstrated from preoperative scores to 3 months postoperatively in Knee Injury and Osteoarthritis Outcome Score subcategories, Lysholm, and visual analog scale scores while no differences were found for Tegner and International Knee Documentation Committee scores. Although statistically significant improvement in PROMs remained at all postoperative time points compared to preoperative scores, no significant differences were observed after 3 months postoperatively.
Conclusions
Patients undergoing APM had significant mean changes in legacy PROMs by 3 months postoperatively that exceeded given minimal clinically important difference values, without further clinically important improvement reported up to 2 years postoperatively.
Study design
Level III, systematic review.
Keywords: Meniscus, Meniscectomy, Meniscal tear, Arthroscopic, Knee, Maximal medical improvement, Patient-reported outcome measures
1. Introduction
Meniscal tears are one of the most common orthopedic injuries, with a reported prevalence of 61 cases per 100,00 people in the United States.1 The etiology of meniscal tears can vary widely and concomitant injuries are common. Athletes performing rapid accelerations/decelerations while changing direction may cause an excessive rotational force applied across the tibiofemoral joint resulting in acute meniscal tears. Alternatively, chronic or degenerative meniscal tears can result after years of degenerative pathology.2,3 For patients with persistent symptoms despite conservative treatments, arthroscopic partial meniscectomy (APM) can be a surgical option and is among the most commonly performed orthopedic surgeries.4,5 With an increasing rate of meniscal injuries in the general population, the number of APM has risen substantially over the last 25 years, with over half a million being performed a year.4,6
Patient outcomes following APMs have been extensively studied in the form of objective clinical findings as well as subjective patient-reported outcome measurements (PROMs).7, 8, 9, 10 These outcome measures allow physicians and researchers to quantify both objective and subjective progress during the recovery period after surgery to better elucidate clinical expectations. APM has been shown to result in significant improvements in objective clinical outcomes, such as range of motion, following surgery.11 Some commonly reported legacy PROMs in the literature include visual analog scale (VAS), Knee Injury and Osteoarthritis Outcome Score (KOOS), Tegner, International Knee Documentation Committee (IKDC), and Lysholm scores.7,9,12, 13, 14, 15 These PROMs enable patients to subjectively report their symptoms, activity, function, and whether they have returned to their preinjury baseline. Following APM, patients subjectively report improved function, pain, and quality of life when compared to a preoperative baseline.16,17 Compared to nonoperative treatment, patients’ short-term and long-term postoperative objective and subjective outcomes following APM have demonstrated success and satisfaction.7, 8, 9,13, 14, 15,18 Nevertheless, one disadvantage of the vast array of legacy PROMs reported in the literature is the lack of intuitive scoring systems and inability to standardize the scores, making it difficult for providers to compare and analyze outcomes. Even more so, achieving minimal clinically important differences (MCID) in these PROMs vary by scale, thereby making it difficult to understand the true improvement from surgical intervention as reported by patients. A concise summary of subjectively reported patient outcomes following APM is useful in guiding patient expectations through a common operative and postoperative course.
Orthopedic surgeons are performing APM for meniscal tears at increasing rates. Given that recent literature has demonstrated optimal outcomes for both operative and nonoperative management of meniscal tears, it is of paramount importance to use both objective and subjective outcomes in the clinic setting to help guide and monitor patient progress throughout the course of their treatment.19 Using PROMs enables physicians to understand when patients feel they are improving after an intervention, providing a tool physicians can utilize to educate patients on their course and help facilitate realistic timelines and expectations for their patients. The purpose of this study was to review patient outcomes in the literature following APM in order to identify when patients report reaching subjective maximal improvement postoperatively. Given previous literature on maximal subjective improvement following knee surgery, we hypothesized that patients would reach a maximal level of improvement at 6 months after an APM and would not demonstrate any improvements beyond this time point.20
2. Methods
2.1. Research framework
A systematic review was performed in accordance with the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).21
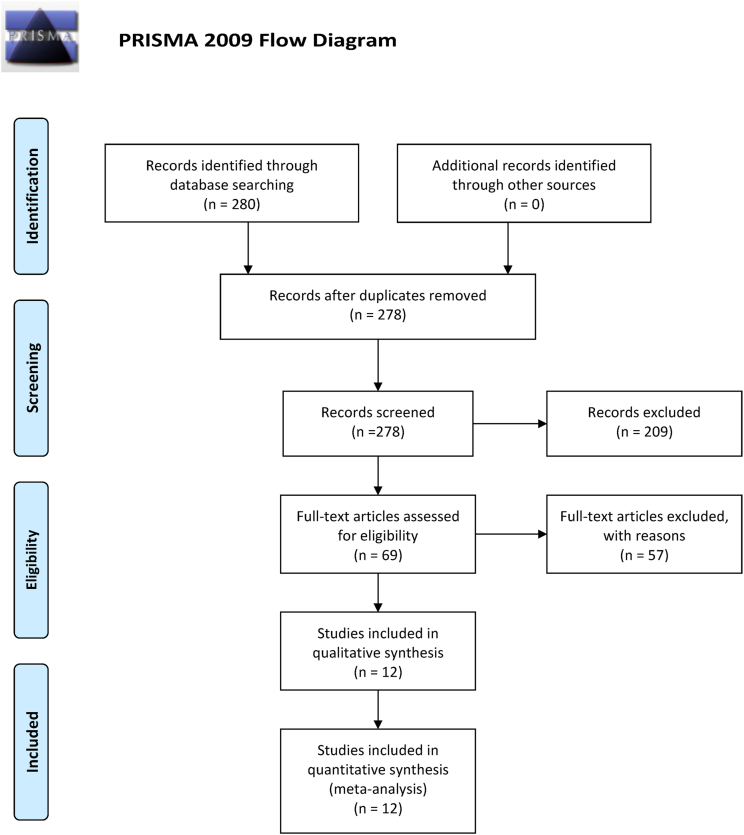
A search of PubMed was performed on August 15, 2019, to include articles in the English language published from Jan 1, 2004 to August 15, 2019 with the following search terms: Lysholm, Tegner Activity Scale, SF-12, Knee Society Score, Cincinnati Rating System, Knee Injury and Osteoarthritis Outcome Score, KOOS, Patient Reported Outcomes Measurement Information, PROMIS, IKDC, International Knee Documentation Committee, Patient-Reported Outcomes, Patient-Reported Outcome Measur-, Outcome Measur-, Outcome Scores, Patient Reported Outcome Measures, and Patient Outcome Assessment. These were in combination with the medial subject headings partial and meniscectomies, meniscectomy, or meniscus/surgery, under the subheading of surgery. This search yielded 280 articles. Selection criteria included studies that reported clinical outcome scores after APM without additional treatments or interventions in adult patients >18 years of age at any time greater than 6 months after surgical intervention. The titles and abstracts of the resulting studies were reviewed by 6 independent reviewers. The full text of the article was reviewed if the abstract mentioned the collection of clinical outcome scores at least 6 months postoperatively in adult patients >18 years of age who underwent an APM without additional intervention, or if there was uncertainty about outcome reporting. The citations of included articles were also reviewed to identify articles that were missed by the initial query, none of which were found. Studies that met inclusion criteria and reported outcomes at an additional time point beyond 6 months were also included in this investigation (Fig. 1). A total of 209 articles were excluded if additional interventions were performed such as repairs, ligamentous reconstruction or repair, cartilaginous manipulation, revisions, if the patient was under 18 years of age, research conducted prior to 2000, follow-up and outcome reporting were less than 6 months postoperatively, or level of evidence was below level III, and articles that were meta-analyses or systematic reviews. Articles were excluded if data were not reported or if data were incomplete for outcome scores. Since performing our initial search from 2004 to 2019, additional relevant articles were published related to APM. However, these studies did not meet our inclusion criteria to be incorporated into our analysis due to limitations in incomplete outcomes of interest, limited time follow up < 6 months, and additional concomitant procedures.10,19,22, 23, 24
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of inclusion process. A total of 209 articles were excluded if additional interventions were performed such as repairs, ligamentous reconstruction or repair, cartilaginous manipulation, revisions, if the patient was under 18 years of age, research conducted prior to 2000, follow-up and outcome reporting were less than 6 months postoperatively, or level of evidence was below level III, and articles that were meta-analyses or systematic reviews. Articles were excluded if data were not reported or if data were incomplete for outcome scores.
2.2. Data extraction
Reviewers independently extracted data points from included articles. Data extraction included title, first author, date of publication, study design, study intervention, number of subjects, level of evidence, pathology of meniscal injury, arthroscopic grading of arthritis, and PROMs used and at which time points. Clinical outcome scores included KOOS, IKDC, Lysholm, Tegner Activity Scale, Western Ontario Meniscal Evaluation Tool, and VAS. Based on previous literature,20 a distribution-based method constructed from statistical characteristics of the obtained samples was used to calculate MCID for those outcome metrics that had a calculated MCID.20,25, 26, 27, 28 MCID were previously established for the IKDC (MCID = 9) and Lysholm (MCID = 10). An MCID was also established for each subscore of the KOOS: Pain (MCID = 6–6.1), Symptoms (MCID = 5–8.5), Activities of Daily Living (MCID = 7–8), Sports (MCID = 5.8), and Quality of Life (MCID = 7–7.2).20,29,30 In the case of multiple MCID previously reported for an individual PROM, the smallest MCID was used for analysis. For scores without an established MCID, statistical significance was used to analyze the change in outcome measures.
2.3. Data analysis
Clinical outcomes were evaluated at 5 time points: these include preoperatively, 3 months, 6 months, 1 year, and 2 years postoperatively. Reported means and standard deviations were collected and evaluated for all PROMs. Study medians were used in the place of means for studies that did not provide such values. If standard deviations were not provided but 95% confidence intervals were presented, the standard deviation was computed using the sample size and mean. Also, if only an interquartile range was reported, a standard of deviation was determined by assuming a normal distribution and dividing the interquartile range by 1.35. Risk of bias was evaluated using the validated Methodological Index for Non-randomized Studies (MINORS) instrument to rate the quality of investigations.31 The MINORS criteria is a 24-point scale for comparative studies and 16-point scale for non-comparative studies, with the score reported as a percentage of total possible points. A higher MINORS criteria score is indicative of a higher methodological quality of the given study.
2.4. Statistical analysis
Weighted averages were calculated and compared among different time points using mixed model methods. Within the mixed model method, the individual studies were considered the random effect and the time point was considered the fixed effect. When computing the weighted averages, inverse variance weights were used in these models which corresponds to studies with larger sample sizes and smaller variances receiving larger weights in the analysis. Comparisons were made using repeated-measures models, with results given as least squares (adjusted) means and standard errors, utilizing a Tukey-Kramer P value correction to adjust for multiple comparisons where appropriate. Statistical significance was set at P < 0.05. All analyses were performed using SAS Version 9.4 (SAS Institute Inc).
3. Results
3.1. Study selection and study bias
The systematic review yielded 280 potential articles. Following the application of inclusion and exclusion criteria, 12 studies were included in the final analysis (Table 1).18,32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 MINORS (Methodological index for non-randomized studies) criteria was used to evaluate nonrandomized studies. Of the 12 studies, 4 were comparative studies and 2 were noncomparative studies. The mean MINORS criteria score for comparative studies was 20.75 (20–22) and 13.5 (13–14) for noncomparative studies.
Table 1.
Studies included in the final analysis.
| Author | Year | Journal | Study Design | Single vs. Multi-Center | Country | Level of Evidence |
|---|---|---|---|---|---|---|
| Haviv27 | 2016 | Arch Orthop Trauma Surg | Prospective cohort | Single | Israel | 2 |
| Herrlin28 | 2007 | KSSTA | RCT | Single | Sweden | 1 |
| Sihvonen29 | 2018 | Ann Rheum Dis | RCT | Multi | Finland | 1 |
| Roos30 | 2018 | BMJ Open | RCT | Multi | Denmark | 1 |
| Haviv31 | 2017 | J Knee Surg | Prospective cohort | Single | Israel | 3 |
| van de Graaf17 | 2018 | JAMA | RCT | Multi | Netherlands | 1 |
| Haviv32 | 2015 | Orthopedics | Prospective cohort | Single | Israel | 3 |
| Filardo33 | 2016 | AJSM | RCT | Single | Italy | 1 |
| Lizaur-Utrilla34 | 2019 | AJSM | Prospective cohort | Single | Spain | 2 |
| Thorlund35 | 2017 | BMJ | Prospective cohort | Multi | Denmark | 2 |
| Katz36 | 2013 | N Engl J Med | RCT | Multi | United States | 1 |
| Kise37 | 2018 | KSSTA | RCT | Single | Norway | 2 |
Randomized Controlled Trial (RCT); Knee Surg Sports Traumatol Arthrosc (KSSTA); Am J Sports Med (AJSM).
3.2. Study characteristics
A total of 1663 participants were included, 1033 (62%) were male and 630 (38%) were female. The mean age was 49.2 ± 6.3 years old. Participant demographics are demonstrated in Table 2.
Table 2.
Pooled patient characteristics and data of included studies.
| n (%) or Mean (SD) | |
|---|---|
| Levels of evidence (n = 12) | |
| 1 | 6 (50%) |
| 2 | 4 (33%) |
| 3 | 2 (67%) |
| Study design | |
| Prospective cohort | 5 (42%) |
| Randomized controlled trial | 7 (58%) |
| Center type | |
| Single | 7 (58%) |
| Multi-center | 5 (42%) |
| Age, year | 49.2 (6.3) |
| Sex | |
| Male | 1033 (62%) |
| Female | 630 (38%) |
| Body mass index, kg/m2 | 27.1 (1.4) |
| Tear pattern (n = 982) | |
| Longitudinal | 129 (13%) |
| Radial | 78 (8%) |
| Horizontal | 119 (12%) |
| Horizontal flap | 45 (5%) |
| Vertical flap | 155 (16%) |
| Complex | 394 (40%) |
| Bucket handle | 62 (6%) |
| Meniscal tear (n = 1203) | |
| Medial | 961 (80%) |
| Lateral | 210 (17%) |
| Both | 32 (3%) |
| Kl Grade (n = 694) | |
| 0 | 266 (38%) |
| 1 | 291 (42%) |
| 2 | 86 (12%) |
| 3 | 51 (7%) |
SD, standard deviation.
3.3. KOOS
Six studies were found to meet the inclusion criteria for analysis of KOOS scores.33,35,38, 39, 40,43,44 Among these 6 studies for KOOS, there were 9 individual groups of patients that had an APM that contributed results to the models. At the 6-month time point for all scores except pain, there was only 1 group that had measurements available at this time point. The weighted means and standard errors for the KOOS subscores at each of the 5 time points are depicted in Table 3A. The mean differences between the time points for these measures and the corresponding p-values are given in Table 3B.
Table 3A.
Weighted means and standard errors for KOOS scores.
| Pain |
Symptoms |
ADL |
Sports |
QOL |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Time | WM | SE | WM | SE | WM | SE | WM | SE | WM | SE |
| Preoperative | 56.77 | 2.47 | 57.37 | 3.36 | 67.39 | 2.50 | 32.12 | 3.38 | 41.58 | 2.00 |
| 2–3 months | 75.26 | 4.10 | 79.41 | 4.17 | 87.96 | 2.50 | 56.85 | 5.07 | 53.31 | 3.24 |
| 6 months∗ | 81.57 | 5.85 | 89.00 | 10.85 | 84.00 | 8.48 | 70.00 | 32.11 | 69.00 | 9.64 |
| 1 year | 76.93 | 4.13 | 74.95 | 6.12 | 82.11 | 4.23 | 50.80 | 7.03 | 57.98 | 3.97 |
| 2 years | 82.02 | 4.20 | 75.55 | 4.64 | 85.97 | 2.88 | 57.13 | 3.85 | 74.43 | 3.00 |
ADL, activities of daily living; KOOS, Knee Injury and Osteoarthritis Outcome Score; QOL, quality of life; SE, standard error; WM, weighted mean.
For all but the pain score, the results come from only one group of patients. This may lead to skewed means and large standard errors.
Table 3B.
KOOS scores in the postoperative time period.
| Pain |
Symptoms |
ADL |
Sports |
QOL |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time Comparisons | Mean difference | P-value | Mean difference | P-value | Mean difference | P-value | Mean difference | P-value | Mean difference | P-value | |
| Preoperative | 2–3 months | 18.49 | 0.008 | 22.04 | 0.014 | 20.57 | 0.004 | 24.73 | 0.015 | 14.73 | 0.018 |
| 6 months | 24.80 | 0.007 | 31.63 | 0.0049 | 16.61 | 0.133 | 37.88 | 0.305 | 27.42 | 0.049 | |
| 1 year | 20.16 | 0.005 | 17.58 | 0.065 | 14.72 | 0.040 | 18.68 | 0.074 | 16.40 | 0.021 | |
| 2 years | 25.25 | 0.002 | 18.40 | 0.032 | 18.31 | 0.008 | 25.01 | 0.008 | 32.85 | 0.0008 | |
| 2–3 months | 6 months | 6.31 | 0.410 | 9.59 | 0.455 | −3.96 | 0.676 | 13.15 | 0.706 | 12.69 | 0.280 |
| 1 year | 1.67 | 0.782 | −4.46 | 0.580 | −5.85 | 0.299 | −6.05 | 0.523 | 1.67 | 0.760 | |
| 2 years | 6.76 | 0.293 | −3.64 | 0.590 | −1.99 | 0.628 | 0.28 | 0.966 | 18.12 | 0.014 | |
| 6 months | 1 year | −4.64 | 0.541 | −14.05 | 0.322 | −1.89 | 0.851 | −19.20 | 0.590 | −11.02 | 0.350 |
| 2 years | 0.45 | 0.952 | −13.23 | 0.324 | 1.97 | 0.836 | −12.87 | 0.711 | 5.43 | 0.619 | |
| 1 year | 2 years | 5.09 | 0.420 | 0.82 | 0.920 | 3.86 | 0.492 | 6.33 | 0.473 | 16.45 | 0.029 |
ADL, activities of daily living; KOOS, Knee Injury and Osteoarthritis Outcome Score; QOL, quality of life.
Statistically significant values (p < 0.05) are in bold.
Statistically significant improvements were demonstrated from scores reported preoperatively to scores at 2–3 months in all KOOS subcategories. Among the KOOS subscores, Pain, Symptoms, Activities of Daily Living, and Sports did not demonstrate a significant improvement after 2–3 months (Table 3B). While changes from the preoperative time point were seen in scores at the 6-month, 1-year, and 2-years marks, only the Quality of Life subscore demonstrated statistically significant changes up to 2 years from other time points. It should be noted that the mean differences that were found to be statistically significant also exceeded the given MCID values in the literature.20,29,30
3.4. Lysholm
When evaluating Lysholm scores, 5 studies met the inclusion criteria.32, 33, 34,36,37 Across the 5 studies there were 7 individual groups of patients that underwent an APM. The weighted means and standard errors are presented in Table 4A and the mean differences with corresponding p-values in Table 4B. It was found that preoperative Lysholm scores were significantly lower than the 2-month, 1- and 2-year follow-ups. No significant improvement was seen relative to 2–3 months postoperatively indicating no significant improvement beyond 3 months postoperatively. The mean differences that were statistically significant did exceed the given MCID value values in the literature.20,29,30
Table 4A.
Weighted Means and Standard Errors for Lysholm, IKDC, Tegner and VAS scores.
| Lysholm |
IKDC |
Tegner |
VAS |
|||||
|---|---|---|---|---|---|---|---|---|
| Time | WM | SE | WM | SE | WM | SE | WM | SE |
| Preoperative | 64.85 | 1.18 | 49.31 | 6.23 | 3.04 | 0.36 | 6.22 | 0.42 |
| 2–3 months | 88.00∗ | 2.54 | 70.73 | 6.34 | 3.34† | 0.20 | 1.33‡ | 0.47 |
| 6 months | 84.00∗ | 4.33 | 75.93 | 6.00 | 4.15 | 0.38 | 1.31 | 0.62 |
| 1 year | 80.75 | 1.83 | 70.70∗ | 9.23 | 2.10∗ | 1.03 | ||
| 2 years | 80.60 | 2.03 | 71.50∗ | 7.50 | 2.28 | 0.37 | ||
IKDC, International Knee Documentation Committee; SE, standard error; VAS, visual analog scale; WM, weighted mean.
The results come from only one group of patients. This may lead to skewed means and large standard errors.
This reflects the time period of 1–2 months.
This reflects the time period of 1–3 months.
Table 4B.
Difference in Weighted Means between Time Points for Lysholm, IKDC, Tegner and VAS scores.
| Lysholm |
IKDC |
Tegner |
VAS |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Time Comparisons | MD | p-value | MD | p-value | MD | p-value | MD | p-value | |
| Preoperative | 2–3 months | 23.15 | 0.014 | 21.42 | 0.137 | 0.30∗ | 0.542 | −4.89† | <0.001 |
| 6 months | 19.15 | 0.050 | 26.32 | 0.091 | 1.14 | 0.167 | −4.91 | 0.001 | |
| 1 year | 15.90 | 0.018 | 21.39 | 0.194 | −4.12 | 0.013 | |||
| 2 years | 15.75 | 0.021 | 22.19 | 0.150 | −3.94 | <0.001 | |||
| 2–3 months | 6 months | −4.00 | 0.509 | 5.20 | 0.612 | 0.81∗ | 0.201 | −0.02† | 0.982 |
| 1 year | −7.25 | 0.146 | −0.03 | 0.997 | 0.77† | 0.526 | |||
| 2 years | −7.40 | 0.151 | 0.77 | 0.945 | 0.95† | 0.173 | |||
| 6 months | 1 year | −3.25 | 0.560 | −5.23 | 0.681 | 0.79 | 0.540 | ||
| 2 years | −3.40 | 0.551 | −4.43 | 0.690 | 1.57 | 0.236 | |||
| 1 year | 2 years | −0.15 | 0.963 | 0.80 | 0.952 | 0.18 | 0.876 | ||
IKDC, International Knee Documentation Committee; MD, mean difference; VAS, visual analog scale.
This reflects the time period of 1–2 months.
This reflects the time period of 1–3 months.
3.5. IKDC
Only 2 studies met inclusion criteria for the evaluation of IKDC scores.12,38 Among the 2 studies, there were 3 groups of patients who had an APM. Table 4A, Table 4BA and 4B demonstrate mean difference and progression of IKDC scores across 2-year follow-up. No statistically significant difference was seen between IKDC scores at any given time point.
3.5.1. Tegner
Two studies were included in the analysis of Tegner scores.33,38 Across both studies there was a total of 2 groups who underwent an APM. Table 4A, Table 4BA and 4B depict the mean difference and progression of reported scores up to 6 months postoperatively. There was no significant difference found between any time points.
3.6. VAS
A total of 5 studies were included in the analysis of VAS scores.7,8,13,15,16 Across all 5 studies there were 8 individual groups of patients who had an APM. Table 4A, Table 4BA and 4B depict the mean difference and progression of VAS scores spanning a 2-year follow up. Preoperative VAS scores were significantly lower than VAS scores at all postoperative time points (P < 0.01). No significant difference was seen beyond 3 months postoperatively.
4. Discussion
The present systematic review aimed to evaluate when patients report maximal subjective improvement following arthroscopic partial meniscectomy. This pooled analysis of 12 studies found that patients achieved clinically significant improvement by 3 months after APM, while incremental improvement in subsequent timepoints did not reach clinical significance thereafter. Specifically, the weighted means exceed the established MCID values in the literature for KOOS, Lysholm, and VAS scores at 3 months after APM compared to preoperatively, while no differences were found for IKDC and Tegner scores. However, additional clinically important differences were not found beyond 3 months after surgery for these legacy PROMs. These findings suggest that patients with meniscal tears experience the majority of reported subjective improvements within 3 months after APM.
For those with symptomatic meniscal tears, understanding time to symptomatic improvement after surgery is crucial to counseling patients and setting realistic expectations. Previous studies have identified that the majority of symptomatic improvements occur within the first 6 months of surgery.13,45,22,23,26 In a multi-center randomized control trial examining APM versus physical therapy alone, Katz et al. found no significant differences in improvement in pain or function between the 2 groups after 6 and 12 months.24 The majority of improvement occurred within 6 months of surgery. Beletsky and colleagues further attempted to answer this question of timing in a retrospective multivariate analysis.27 Their group identified 126 patients undergoing isolated APM and found that 73%–89.7% of patients achieved MCID for KOOS scores in a median 5.68–5.78 months. Factors independently associated with delays in achieving MCID included higher preoperative scores, medial sided and root tears while older patients, complex tears, or discoid meniscus required shorter times. Not surprisingly, those with pre-existing osteoarthritis were less likely to achieve clinically significant outcomes (66.2 vs. 77.4%) as were patients older than 50 years old with arthritis. While their results delineated important factors affecting time to achieving clinically significant outcomes, their time points were limited to preoperative and 6 months. The present pooled analysis enables evaluation of a larger sample size and reveals that maximal clinical benefit occurs earlier, within 2–3 months of surgery, without substantial improvement after this time period. This collective summary of the literature provides valuable information that will benefit physicians in counseling patients on expected course of recovery, specifically in the short-term postoperatively. Additionally, while this information helps providers establish a timeframe for improvement that may be used for comparison in future study interventions, it should be noted that commonly used legacy PROMs have varying results.
Disease specific PROMs vary in performance depending on the pathology and population studied. Multiple legacy PROMs have demonstrated favorable psychometric properties in terms of validity, reliability, and responsiveness for various knee pathologies, including meniscal tears. Those included in the present analysis have been studied extensively with regards to these properties, including KOOS,17, 18, 19, 20 IKDC,17 VAS, and Lysholm and Tegner activity scores.21, 22, 23 Van de Graaf and colleagues,23 sought to compare the properties of the IKDC and KOOS scores for those with meniscal tears. The KOOS tool demonstrated suboptimal performance relative to the IKDC in terms of internal consistency, measurement error, content validity, and the ability to measure true change. The KOOS tool exhibited significant floor and ceiling effects across its different domains. Their group ultimately recommended IKDC for assessing outcomes after APM. Interestingly in the present study, compared to preoperative scores, clinically important improvements were found for up to 2 years for almost all KOOS domains. However, the differences in the weighted means did not exceed the given MCID and therefore improvements were not observed at any time point for IKDC. These findings highlight the variability of PROM outcomes in patients with similar knee pathology and contrast the findings of van de Graaf and colleagues. It is noted this analysis includes a much larger pooled sample size of patients compared to the limited cohort of 75 patients in their study. Additionally, as suggested by the aforementioned studies, unseen floor and ceiling effects may account for undetected true clinical differences beyond 2–3 months in this analysis.
Similarly, Briggs et al. evaluated these same properties for the Lysholm knee score and Tegner activity scale in patients with meniscal tears.21 Both the Lysholm and Tegner scores revealed acceptable psychometric properties, however Lysholm showed unacceptable ceiling effects greater than 30% for the limp, instability, support, and locking domains of the score while the Tegner scale only had a moderate effect size for isolated meniscal lesions. Conversely, the present study demonstrated that Lysholm scores significant changes by 3 months postoperatively and plateaued thereafter, while Tegner scores did not reach clinical significant differences postoperatively. With such variability in performance of measures and evidence of validation,23 further studies are required to identify the ideal tool for capturing clinical progress in those with meniscal tears.
Furthermore, the findings of the present analysis must be interpreted based on the specific inclusion and exclusion criteria applied. The majority of studies featured in this analysis were from a relatively homogenous patient population that excluded severe forms of osteoarthritis or presence altogether, most concomitant procedures, and typically included middle-aged patients with irreparable meniscus tears. Franovic et al. retrospectively reviewed patients undergoing arthroscopic meniscal surgery and found that PROMIS-PF, PI, and D significantly improved after 3 months.10 Individuals with preoperative PROMIS-PF scores below 34.9 led to an 82% probability of achieving MCID, as well as PROMIS-PI above 67.5 (86% probability), and PROMIS-D cutoff of 58.9% (60% probability). Their study only included outcomes up to 3 months, which excluded them from our present analysis, and excluded all patients <40 years old, concomitant surgeries, and did not report on tear morphology. Previous literature, however, has demonstrated that features of the tear morphology and pathology of the knee factor into recovery timelines.7,24 Gowd et al. established MCID, substantial clinical benefit, and patient-acceptable symptom state for patients undergoing APM.28 Their group found that tear morphology such as degenerative, medial sided, and root tears were less likely to achieve meaningful outcomes in 2 or more scores. Similarly, multiple studies have reported preoperative factors such as complex tears, meniscal extrusions, larger meniscus excisions, and femoral condyle lesions portending worse outcomes 1–5 years after APM.11,29,30 Taking account of tear morphology, cartilage defects, osteoarthritis severity, additional injuries present in the knee preoperatively, patient age, and activity level are all important considerations that may significantly impact the course of recovery. Our results specifically offer insight into the timeline to recovery for patients with isolated meniscal tears without severe osteoarthritis who underwent APM, but given the inherent nature of a pooled systematic review, it was not possible to account for all potential confounding factors.
4.1. Limitations
A variety of limitations in our study must be acknowledged. MCID are established within specific patient populations. Amongst the included studies, heterogeneity in patients exists across studies and may affect the application of previously published MCIDs. To combat this, we included strict inclusion criteria that only featured patients undergoing isolated partial meniscectomy without concomitant procedures. To date, our study features the largest analysis of outcomes of at least 6 months after APM. Additionally, a mix of prospective randomized control trials and retrospective studies were analyzed, therefore limiting the overall level of evidence of this systematic review. Retrospective studies are inherently biased in patient reporting, selection, and outcomes studied. Certain PROM scores were also unavailable for various time points postoperatively, such as the Tegner activity scale, and not all PROMs were utilized in each study. This missing information may be one explanation why significance was not found for Tegner scores or IKDC at any timepoint due to limited reporting in the studies meeting inclusion criteria. We are unable to comment on the effect of previous activity level, comorbidities, nor results of athletic populations as the included studies may not generalize to all populations. Further collection of these variables in future studies will be valuable in counseling additional patient populations suffering meniscal injuries. It would have been ideal to summarize the MCID rates across the studies. However, this information was not available within the included studies and hence the mean differences were interpreted with respect to given MCID values.
5. Conclusions
Patients undergoing arthroscopic partial meniscectomy had significant mean changes in legacy PROMs by 3 months postoperatively that exceeded given minimal clinically important difference values, without further clinically important improvement reported up to 2 years postoperatively.
Author contributions
All authors met with the librarian, Stephanie Stebens, who assisted with performing a literature review under PRISMA guidelines. All authors agreed on final inclusion and exclusion criteria to be applied to the literature. MT, AC, and GR carried out the initial literature assessment of the abstracts and created the data extraction tool. JP, LK MA, and SD provided oversight and reviewed all selected abstracts as well as reading full texts to finalize which manuscripts were included. KO is the attending physician who reviewed the literature review protocol, the articles included and database extraction tool for final approval. All authors contributed towards:
-
•
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
-
•
Drafting the work or revising it critically for important intellectual content; AND
-
•
Final approval of the version to be published; AND
-
•
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
•
Interpreting the statistical analysis results provided by Dr. Lonni Schultz, PhD.
All authors contributed towards drafting the manuscript and multiple revisions of the manuscript. KO approved each step of the study, reviewed the literature cited and statistical analysis requested, revised each draft of the manuscript, and provided mentorship throughout the course of the study. All authors read and approved the final manuscript.
Social medial handles
Twitter: @JoshCastleMD; @Lafi_KhalilMD; @HenryFordNews; @DoctorOkoro.
Instagram: @jcas30; @lafi.s.khalil; @muhammad.j.abbas; @DoctorOkoro; @henryfordhealthsystem
Institutional Review Board: This project did not require institutional review board approval.
Declaration of competing interest
K.R.O. has received grant support from Arthrex; education payments from Arthrex, Medwest, and Smith & Nephew; consulting fees from Endo Pharmaceuticals and Smith & Nephew; nonconsulting fees from Arthrex; and hospitality payments from Stryker, Wright Medical, and Zimmer Biomet. All other authors have no financial disclosures.
Acknowledgements
The authors would like to acknowledge Stephanie Stebens, MLIS, AHIP for her assistance in literature review and methodological processes and by Dr. Lonni Schultz, PhD for providing and interpreting the statistical analysis.
Contributor Information
Joshua P. Castle, Email: Joshua.p.castle@gmail.com.
Lafi S. Khalil, Email: lskhalil@gmail.com.
Muhammad J. Abbas, Email: fh1408@wayne.com.
Stephanie DeBolle, Email: sadebolle@gmail.com.
Marissa Tandron, Email: marissatandron@gmail.com.
Austin G. Cross, Email: austingcross@gmail.com.
Guillermo A. Rodriguez, Email: guillermo0390@gmail.com.
Kelechi R. Okoroha, Email: krokoroha@gmail.com.
References
- 1.Raj M.A., Bubnis M.A. StatPearls Publishing; Island, FL: 2021. Knee Meniscal Tears. StatPearls. Treasure. NBK431067. [PubMed] [Google Scholar]
- 2.Kurzweil P.R., Cannon W.D., DeHaven K.E. Meniscus repair and replacement. Sports Med Arthrosc Rev. 2018;26:160–164. doi: 10.1097/JSA.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 3.Wilson P.L., Wyatt C.W., Romero J., Sabatino M.J., Ellis H.B. Incidence, presentation, and treatment of pediatric and adolescent meniscal root injuries. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118803888. 2325967118803888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van de Graaf V.A., Wolterbeek N., Mutsaerts E.L., et al. Arthroscopic partial meniscectomy or conservative treatment for nonobstructive meniscal tears: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2016;32:1855–1865. doi: 10.1016/j.arthro.2016.05.036. the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, e1854. [DOI] [PubMed] [Google Scholar]
- 5.Baker B.E., Peckham A.C., Pupparo F., Sanborn J.C. Review of meniscal injury and associated sports. Am J Sports Med. 1985;13:1–4. doi: 10.1177/036354658501300101. [DOI] [PubMed] [Google Scholar]
- 6.Kim S., Bosque J., Meehan J.P., Jamali A., Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Jt Surg Am Vol. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 7.Beletsky A., Gowd A.K., Liu J.N., et al. Time to achievement of clinically significant outcomes after isolated arthroscopic partial meniscectomy: a multivariate analysis. Arthrosc Sports Med Rehabil. 2020;2:e723–e733. doi: 10.1016/j.asmr.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noorduyn J.C.A., Glastra van Loon T., van de Graaf V.A., et al. Functional outcomes of arthroscopic partial meniscectomy versus physical therapy for degenerative meniscal tears using a patient-specific score: a randomized controlled trial. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120954392. 2325967120954392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gowd A.K., Lalehzarian S.P., Liu J.N., et al. Factors associated with clinically significant patient-reported outcomes after primary arthroscopic partial meniscectomy. Arthroscopy. 2019;35:1567–1575. doi: 10.1016/j.arthro.2018.12.014. the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, e1563. [DOI] [PubMed] [Google Scholar]
- 10.Franovic S., Kuhlmann N.A., Pietroski A., et al. Preoperative patient-centric predictors of postoperative outcomes in patients undergoing arthroscopic meniscectomy. Arthroscopy. 2021;37:964–971. doi: 10.1016/j.arthro.2020.10.042. [DOI] [PubMed] [Google Scholar]
- 11.Koch M., Memmel C., Zeman F., et al. Early functional rehabilitation after meniscus surgery: are currently used orthopedic rehabilitation standards up to date? Rehabil Res Pract. 2020;2020:3989535. doi: 10.1155/2020/3989535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van de Graaf V.A., Wolterbeek N., Scholtes V.A., Mutsaerts E.L., Poolman R.W. Reliability and validity of the IKDC, KOOS, and WOMAC for patients with meniscal injuries. Am J Sports Med. 2014;42:1408–1416. doi: 10.1177/0363546514524698. [DOI] [PubMed] [Google Scholar]
- 13.Briggs K.K., Kocher M.S., Rodkey W.G., Steadman J.R. Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Joint Surg Am. 2006;88:698–705. doi: 10.2106/JBJS.E.00339. [DOI] [PubMed] [Google Scholar]
- 14.Yim J.H., Seon J.K., Song E.K., et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41:1565–1570. doi: 10.1177/0363546513488518. [DOI] [PubMed] [Google Scholar]
- 15.Sofu H., Oner A., Camurcu Y., Gursu S., Ucpunar H., Sahin V. Predictors of the clinical outcome after arthroscopic partial meniscectomy for acute trauma-related symptomatic medial meniscal tear in patients more than 60 years of age. Arthroscopy. 2016;32:1125–1132. doi: 10.1016/j.arthro.2015.11.040. the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. [DOI] [PubMed] [Google Scholar]
- 16.Bernholt D., Wright R.W., Matava M.J., Brophy R.H., Bogunovic L., Smith M.V. Patient Reported Outcomes Measurement Information System scores are responsive to early changes in patient outcomes following arthroscopic partial meniscectomy. Arthroscopy. 2018;34:1113–1117. doi: 10.1016/j.arthro.2017.10.047. the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. [DOI] [PubMed] [Google Scholar]
- 17.Paxton E.S., Stock M.V., Brophy R.H. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. [DOI] [PubMed] [Google Scholar]
- 18.van de Graaf V.A., Noorduyn J.C.A., Willigenburg N.W., et al. Effect of early surgery vs physical therapy on knee function among patients with nonobstructive meniscal tears: the ESCAPE Randomized Clinical Trial. JAMA. 2018;320:1328–1337. doi: 10.1001/jama.2018.13308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katz J.N., Shrestha S., Losina E., et al. Five-year outcome of operative and nonoperative management of meniscal tear in persons older than forty-five years. Arthritis Rheumatol. 2020;72:273–281. doi: 10.1002/art.41082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agarwalla A., Puzzitiello R.N., Liu J.N., et al. Timeline for maximal subjective outcome improvement after anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47:2501–2509. doi: 10.1177/0363546518803365. [DOI] [PubMed] [Google Scholar]
- 21.Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Okoroha K.R., Lu Y., Nwachukwu B.U., et al. How should we define clinically significant improvement on patient-reported outcomes measurement information system test for patients undergoing knee meniscal surgery? Arthroscopy. 2020;36:241–250. doi: 10.1016/j.arthro.2019.07.036. [DOI] [PubMed] [Google Scholar]
- 23.Bloise C., Fong B., Jeffers K., et al. Predictors of disparities in patient-reported outcomes before and after arthroscopic meniscectomy. J Knee Surg. 2022 doi: 10.1055/s-0042-1743229. [DOI] [PubMed] [Google Scholar]
- 24.Bisson L.J., Kluczynski M.A., Wind W.M., et al. Better outcomes but No difference in joint space narrowing at five years among patients without unstable chondral lesions versus those with unstable chondral lesions (Left In Situ) at the time of arthroscopic partial meniscectomy. Arthroscopy. 2022;38:936–944. doi: 10.1016/j.arthro.2021.06.030. [DOI] [PubMed] [Google Scholar]
- 25.Nwachukwu B.U., Chang B., Voleti P.B., et al. Preoperative short form health survey score is predictive of return to play and minimal clinically important difference at a minimum 2-year follow-up after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2784–2790. doi: 10.1177/0363546517714472. [DOI] [PubMed] [Google Scholar]
- 26.Rai S.K., Yazdany J., Fortin P.R., Aviña-Zubieta J.A. Approaches for estimating minimal clinically important differences in systemic lupus erythematosus. Arthritis Res Ther. 2015;17:143. doi: 10.1186/s13075-015-0658-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Darrith B., Khalil L.S., Franovic S., et al. Preoperative patient-reported outcomes measurement information system global health scores predict patients achieving the minimal clinically important difference in the early postoperative time period after total knee arthroplasty. J Am Acad Orthop Surg. 2021 doi: 10.5435/JAAOS-D-20-01288. [DOI] [PubMed] [Google Scholar]
- 28.Khalil L.S., Darrith B., Franovic S., Davis J.J., Weir R.M., Banka T.R. Patient-reported outcomes measurement information system (PROMIS) global health short forms demonstrate responsiveness in patients undergoing knee arthroplasty. J Arthroplasty. 2020;35:1540–1544. doi: 10.1016/j.arth.2020.01.032. [DOI] [PubMed] [Google Scholar]
- 29.Paradowski P.T., Witoński D., Kęska R., Roos E.M. Cross-cultural translation and measurement properties of the Polish version of the Knee injury and Osteoarthritis Outcome Score (KOOS) following anterior cruciate ligament reconstruction. Health Qual Life Outcome. 2013;11:107. doi: 10.1186/1477-7525-11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Collins N.J., Misra D., Felson D.T., Crossley K.M., Roos E.M. Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS-PS), knee outcome survey activities of daily living scale (KOS-ADL), Lysholm knee scoring scale, Oxford knee score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), activity rating scale (ARS), and Tegner activity score (TAS) Arthritis Care Res. 2011;63(Suppl 11):S208–S228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 32.Haviv B., Bronak S., Kosashvili Y., Thein R. Arthroscopic meniscectomy of traumatic versus atraumatic tears in middle aged patients: is there a difference? Arch Orthop Trauma Surg. 2016;136:1297–1301. doi: 10.1007/s00402-016-2504-y. [DOI] [PubMed] [Google Scholar]
- 33.Herrlin S., Hallander M., Wange P., Weidenhielm L., Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15:393–401. doi: 10.1007/s00167-006-0243-2. [DOI] [PubMed] [Google Scholar]
- 34.Sihvonen R., Paavola M., Malmivaara A., et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369:2515–2524. doi: 10.1056/NEJMoa1305189. [DOI] [PubMed] [Google Scholar]
- 35.Roos E.M., Hare K.B., Nielsen S.M., Christensen R., Lohmander L.S. Better outcome from arthroscopic partial meniscectomy than skin incisions only? A sham-controlled randomised trial in patients aged 35-55 years with knee pain and an MRI-verified meniscal tear. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-019461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haviv B., Bronak S., Kosashvili Y., Thein R. Does timing of arthroscopic partial meniscectomy in stable knees matter? J Knee Surg. 2017;30:47–50. doi: 10.1055/s-0036-1579668. [DOI] [PubMed] [Google Scholar]
- 37.Haviv B., Bronak S., Kosashvili Y., Thein R. Gender effect on the outcome of partial medial meniscectomy. Orthopedics. 2015;38:e925–928. doi: 10.3928/01477447-20151002-61. [DOI] [PubMed] [Google Scholar]
- 38.Filardo G., Di Matteo B., Tentoni F., et al. No effects of early viscosupplementation after arthroscopic partial meniscectomy: a randomized controlled trial. Am J Sports Med. 2016;44:3119–3125. doi: 10.1177/0363546516660070. [DOI] [PubMed] [Google Scholar]
- 39.Lizaur-Utrilla A., Miralles-Munoz F.A., Gonzalez-Parreno S., Lopez-Prats F.A. Outcomes and patient satisfaction with arthroscopic partial meniscectomy for degenerative and traumatic tears in middle-aged patients with No or mild osteoarthritis. Am J Sports Med. 2019;47:2412–2419. doi: 10.1177/0363546519857589. [DOI] [PubMed] [Google Scholar]
- 40.Thorlund J.B., Englund M., Christensen R., et al. Patient reported outcomes in patients undergoing arthroscopic partial meniscectomy for traumatic or degenerative meniscal tears: comparative prospective cohort study. BMJ. 2017;356:j356. doi: 10.1136/bmj.j356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Katz J.N., Losina E. Surgery versus physical therapy for meniscal tear and osteoarthritis. N Engl J Med. 2013;369:677–678. doi: 10.1056/NEJMc1307177. [DOI] [PubMed] [Google Scholar]
- 42.Kise N.J., Roos E.M., Stensrud S., Engebretsen L., Risberg M.A. The 6-m timed hop test is a prognostic factor for outcomes in patients with meniscal tears treated with exercise therapy or arthroscopic partial meniscectomy: a secondary, exploratory analysis of the Odense-Oslo meniscectomy versus exercise (OMEX) trial. Knee Surg Sports Traumatol Arthrosc. 2019;27:2478–2487. doi: 10.1007/s00167-018-5241-7. [DOI] [PubMed] [Google Scholar]
- 43.Katz J.N., Meredith D.S., Lang P., et al. Associations among preoperative MRI features and functional status following arthroscopic partial meniscectomy. Osteoarthritis Cartilage. 2006;14:418–422. doi: 10.1016/j.joca.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 44.Kise N.J., Aga C., Engebretsen L., Roos E.M., Tariq R., Risberg M.A. Complex tears, extrusion, and larger excision are prognostic factors for worse outcomes 1 and 2 Years after arthroscopic partial meniscectomy for degenerative meniscal tears: a secondary explorative study of the surgically treated group from the Odense-Oslo meniscectomy versus exercise (OMEX) trial. Am J Sports Med. 2019;47:2402–2411. doi: 10.1177/0363546519858602. [DOI] [PubMed] [Google Scholar]
- 45.Wang L., Lin Q., Qi X., Chen D., Xia C., Song X. Predictive factors associated with short-term clinical outcomes and time to return to activity after arthroscopic partial meniscectomy in nonathletes. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671221080787. 23259671221080787. [DOI] [PMC free article] [PubMed] [Google Scholar]