Abstract
Background
The effect of time interval between injury and surgery on outcomes of Bankart repair surgery has not been published previously. The purpose of this study was to assess the effect of surgical delay on functional outcomes after arthroscopic Bankart repair.
Method
One hundred and five athletes who underwent arthroscopic Bankart repair ± remplissage were enrolled in the study. Patients were divided into 2 groups depending upon the injury to surgery time- < 12 months (n = 19), and ≥12 months (n = 86). Depending upon the number of episodes of dislocation, patients were further categorized into 2 groups- <10 episodes (n = 66) and ≥10 episodes (n = 39). All patients were assessed post-operatively for functional outcomes (Modified Rowe's score, Constant Murley score) and return to sports at a minimum of 2 years of follow-up.
Results
The mean injury to surgery time was 31.7 ± 23.1 months. The average number of episodes of dislocation before surgery were 10 (range 3–50). 49/105 (46.7%) patients returned to sports after a mean post-operative duration of 10.9 months. Athletes operated after a surgical delay of ≥12 months had inferior functional outcomes (Modified Rowe's score-89.5 ± 8.9 vs.77.4 ± 21.4; p = 0.02), lower rate of return to sports (14/19 vs. 35/86; p = 0.02) and higher mean time to return to sports (8.7 ± 1.9 vs. 11.5 ± 2.6; p < 0.05). Similarly, athletes who had ≥10 dislocations before surgery had inferior functional outcomes (Modified Rowe's score-84.5 ± 15.2 vs.72.9 ± 25.6; p = 0.004), lower rate of return to sports (37/66 vs. 12/39; p = 0.02) and higher mean time to return to sports (10.3 ± 2.4 vs. 12.6 ± 2.5; p < 0.05).
Conclusion
A delay in surgery (≥12 months) or dislocation episodes of ≥10 are associated with inferior functional outcomes, lower rate of return to sports and higher surgical failure rate.
Level of evidence
Level III; Prospective cohort study.
Keywords: Recurrent shoulder dislocation, Arthroscopic Bankart repair, Remplissage, Return to sports, Delay surgery
1. Introduction
Traumatic shoulder dislocation is a common injury in young male athletes involved in contact sports.1,2 This injury significantly affects athletes and can lead to temporary or permanent cessation of sports activities.3 Traumatic shoulder dislocations cause avulsion of the anterior-inferior glenoid labrum (Bankart lesion). Disruption of this labrum leads to shoulder instability. The incidence of recurrent shoulder dislocation following the first episode varies from 55.7% to 66.8%.4 Age (young males), glenoid bone loss, and engaging Hill Sach's lesion are risk factors for recurrent shoulder dislocations to occur.5
The gold standard treatment for recurrent shoulder dislocations is Bankart repair by way of shoulder arthroscopy.6 The timing of Bankart repair is controversial, as some authors suggest Bankart repair at the time of initial dislocation. After Bankart repair, a majority of patients are able to achieve good functional outcomes, yet not all the patients were able to achieve desired results. Therefore, it is important to identify various factors responsible for inferior functional outcomes after Bankart repair. In the present study, we hypothesize that the greater number of instability episodes and increased time interval between injury and surgery are associated with inferior functional outcomes.
2. Material and methods
The present study was a prospective cohort study conducted after the institutional ethical committee approval (IEC/2016/029). Written and informed consent was received from all the patients. A total of 105 athletes from different sports were enrolled in the study (Fig. 1). 47/105 players were professional players and 58/105 were recreational players. Inclusion criteria were male athletes aged between 18 and 40 years having multiple (>1) episodes of shoulder dislocations. The demographic details of all the patients are shown in Table 1.
Fig. 1.
Details of athletes involved in different sports.
Table 1.
Details of the study population.
| Mean age | 25.8±4.9 |
| Dominant: Non-dominant | 87:18 |
| Contact: Non-contact | 72:33 |
| Mean injury to surgery time (in months) | 31.7±23.1 |
| Average number of dislocation before surgery | 10 |
| Mean follow-up time | 31.8±8.6 |
All the patients were evaluated clinically (apprehension test, anterior drawer, and inferior laxity) and radiologically (X-ray, MRI, and CT scan). The patients with hyperlaxity, rotator cuff tears, SLAP lesions, glenoid bone loss, atraumatic multidirectional instabilities, revision surgery, or operated earlier for any shoulder problems were excluded from the study.
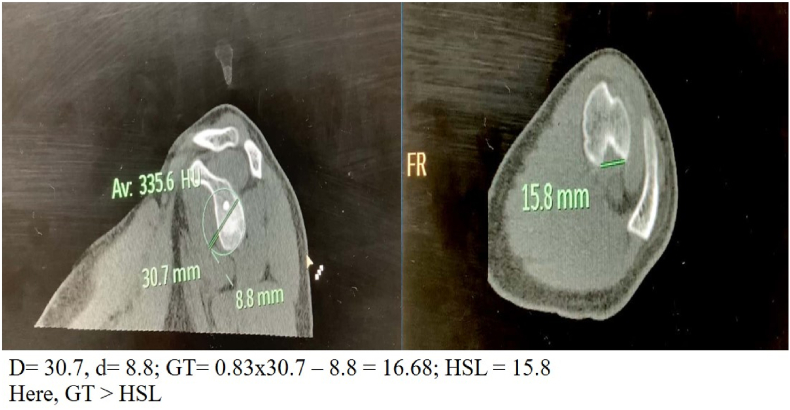
The functional assessment of all patients was done preoperatively and postoperatively using modified Rowe's score, Constant Murley score, and Tegner activity scale. Patients were also assessed using Instability Severity Index Score. The Hill-Sach's lesion was classified as ‘on-track’ or ‘off-track’ with the help of a 3D NCCT of the involved shoulder (as depicted in Fig. 2) using the “best-fit circle method” as described by E. Itoi.7 69/105 patients had “on-track” Hill-Sach's lesion and 36/105 patients had “off-track” Hill-Sach's lesion.
Fig. 2.
NCCT shoulder demonstrating “on track” Hill Sachs's lesion.
Patients were divided into 2 groups depending upon the injury to surgery time8- < 12 months (n = 19) and ≥12 months (n = 86). Depending upon the number of episodes of dislocation patients were further categorized into 2 groups- <10 episodes (n = 66) and ≥10 (n = 39).
All these patients underwent arthroscopic Bankart ± remplissage repair using suture anchors. Out of 105 patients, 36 patients underwent arthroscopic Bankart repair combined with remplissage and 69 patients underwent arthroscopic Bankart repair alone. All surgeries were performed by a single surgeon. All patients underwent similar rehabilitation protocol postoperatively. Patients were followed up for a minimum of 24 months. The final assessment was done at 24 months using Rowe's score and Constant Murley score. Incidence and timing to return to pre-injury level of sports were also documented.
3. Statistical analysis
Discrete categorical data were presented as percentage (%); continuous data were given as mean ± SD. The normality of quantitative data was checked by measures of Kolmogorov Smirnov tests of Normality. Comparisons for two groups (age, Modified Rowe's Score, Constant Murley Score) were made by the student t-test. Categorical variables were reported as counts and percentages. Group comparisons were made with the Chi-Square test (correlation between delay in surgery and number of patients returning to sports and number of dislocation). All statistical tests were two-sided and performed at a significance level of α = .05. The analysis was conducted using IBM SPSS STATISTICS (version 22.0).
4. Results
Overall, 49/105 (47%) athletes returned to the same level of sports, with a mean time to return to sports being 10.9 ± 2.7 months. The mean pre-operative ISIS score seen was 3.8 ± 2.2. Functional outcomes (Tegner activity, Modified Rowe's score, and Constant Murley score) were significantly improved after the Bankart repair ± remplissage surgery (Table 2).
Table 2.
Changes in functional outcome after the surgery.
| Before surgery | After surgery (2 years) | P-value | |
|---|---|---|---|
| Modified Rowe’s score | 33.3±14.1 | 82.9±13.2 | 0.0001 |
| Constant Murley score | 72.3±10.8 | 82.9±8.8 | 0.0001 |
| Tegner activity | 4.4±1 | 6.70±1.5 | 0.0001 |
It was observed that delay in surgery for ≥12 months was associated with significant increase in number of dislocation episodes and higher ISIS score. Athletes operated after ≥12 months of injury had inferior functional outcomes. These patients not only had a lower rate of return to sports but also took more time to return to pre-injury level of activity (Table 3). There was a significant increase in number of Hill Sach's lesion with increase in number of shoulder dislocation episodes. Inferior functional outcomes were also observed in athletes who had ≥10 episodes of dislocation as compared to athletes with <10 episodes of dislocation. Return to sports and time taken to return to sports was also inversely correlated with number of episodes of dislocation (Table 4).
Table 3.
Effect of delay in surgery on outcomes of Bankart repair.
| Delay in surgery (in months) | Average number of dislocation | Mean ISIS | Engaging Hills Sach’s | Returned to sports | Duration of return to sports (in months) | Mean Modifies Rowes score | Mean constant Murley score |
|---|---|---|---|---|---|---|---|
| <12 (n=19) | 5.4±2.5 | 3.6±1.3 | 5 (26%) | 14 (74%) | 8.7±1.9 | 89.5±8.9 | 88±9.6 |
| >12 (n=84) | 10.5±4.6 | 5.1±2.01 | 31 (37%) | 35 (42%) | 11.5±2.6 | 77.4±21.4 | 76.2±21.1 |
| P-value | 0.0001 | 0.003 | 0.4 | 0.02 | 0.0001 | 0.02 | 0.01 |
Table 4.
Correlation between shoulder dislocation episodes and functional outcome of surgery.
| Number of episodes | Mean ISIS | Engaging Hills Sach’s | returned to sports | duration of return to sports (in months) | Mean Modifies Rowes score | Mean Constant Murley score |
|---|---|---|---|---|---|---|
| <10 (n=66) | 4.1±1.6 | 16 | 37(56%) | 10.3±2.4 | 84.5±15.2 | 82.8±17.4 |
| ≥10 (n=39) | 6.3±1.9 | 20 | 12 (31%) | 12.6±2.5 | 72.9±25.6 | 71.3±23.3 |
| 0.0001 | 0.006 | 0.02 | 0.0001 | 0.004 | 0.005 |
The mean age was 25.5 years in athletes who returned to sports after injury and 26.2 years in those who did not return to sports (n.s.). Return to sports among professional athletes was 66% (31/47) and in recreational athletes it was 31% (18/58). The recurrence rate in the present study was 3% (3/105) and all three patients had a surgical delay of ≥12 months. All three patients were involved in contact sports (2 Kabaddi players and 1 Wrestling player). Details of patients who underwent revision surgery are shown in Table 5.
Table 5.
Details of patients who had recurrence.
| Age | Time interval between injury and surgery (months) | Number of instability episodes before surgery | Hill Sach's lesion | |
|---|---|---|---|---|
| Case 1 | 23 | 22 | 10 | Non-engaging |
| Case 2 | 19 | 13 | 12 | Engaging |
| Case 3 | 22 | 14 | 9 | Engaging |
| Mean | 21.3 | 16.3 | 10.3 |
5. Discussion
The factors like age and nature of sporting activity can affects the outcomes after arthroscopic Bankart repair.10, 11, 12, 9 In the present study, it was observed that athletes who were operated after a surgical delay of ≥12 months had inferior functional outcomes, lower rate of return to sports and higher surgical failure risk. Inspite of good results of arthroscopic Bankart repair,13,14 many patients are still reluctant to go for surgery initially. Harris et al.15 in their systemic review study observed that the mean time interval between index injury and surgery was 3.5 years and the average number of instability episodes before surgery was 11.
In the present study, overall 47% of the patients returned to pre-injury level of sports with a mean time to return to sports being 10.9 months. Rate of return to sports in previously published studies varied from 40 to 90%.9,16, 17, 18, 19, 20 Low incidence of return to sports in the present study probably because of a long time interval between injury and surgery. Being out of the game for a long period had a bearing on the skills and activity level of athletes. This could be the probable reason for the low proportion of athletes being able to achieve their pre-injury activity level.
In the present study, it was observed that delay in surgery and higher number of instability episodes not only affect the rate of return to sports, but they also had impacted the timing of return to sports. Antonie et al. observed that athletes having >10 episodes of dislocation before the surgery took more time to return to sports as compared to athletes who had <10 episodes of instability.21
The surgical failure rate in the present study was 3%. In previous studies failure rate varied from 3.4 to 20%.16, 17, 18,22,23 Tyler et al. conducted a study on young athletes and observed athletes who were operated after the first episode of dislocation had low failure rate as compared to athletes who had multiple episodes of shoulder dislocation.24 The recent meta-analytic study also suggested that revision rates were low if surgery was done after the first episode of shoulder dislocation.25
In the present study, age of all three patients with recurrent instability after surgery was <24 years. Previous studies suggested that younger athletes are at higher risk of recurrent dislocations after surgery.22,23,26 Randelli et al. in their systemic review study observed that age <22 years, male gender, and a high number of pre-operative dislocations were associated with increased risk of surgical failure.23 Lee et al. in their study observed that patients who were operated after a delay of >6 months had higher chances of dislocation after arthroscopic Bankart repair as compared to those who were operated within 6 months of injury.27
This is a unique study as the impact of surgical delay and instability episodes on functional outcomes has not been studied previously. However, this study had some limitations as various possible factors (fear of re-injury, socio-economic status, engaged in another profession after index injury, etc.) affecting return to sports were not considered in this study.
6. Conclusion
A delay in surgery (≥12 months) or dislocation episodes of ≥10 are associated with inferior functional outcomes, lower rate of return to sports and higher surgical failure rate.
Contributor Information
Ravi Gupta, Email: ravikgupta2000@yahoo.com.
Shrenuj Goel, Email: dr_shrenujgoel@yahoo.in.
Anil Kapoor, Email: anil88gmch@gmail.com.
Ashwani Soni, Email: asoniortho@gmail.com.
Gladson David Masih, Email: gladsondavid32@gmail.com.
Ravi Jethwa, Email: ravibj08@gmail.com.
References
- 1.Longo U.G., Huijsmans P.E., Maffulli N., Denaro V., De Beer J.F. Video analysis of the mechanisms of shoulder dislocation in four elite rugby players. J Orthop Sci. 2011;16(4):389–397. doi: 10.1007/s00776-011-0087-6. [DOI] [PubMed] [Google Scholar]
- 2.Zacchilli M.A., Owens B.D. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Jt Surg Am Vol. 2010;92(3):542–549. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 3.Fares M.Y., Fares J., Baydoun H., Fares Y. Prevalence and patterns of shoulder injuries in major league baseball. Physician Sportsmed. 2020;48(1):63–67. doi: 10.1080/00913847.2019.1629705. [DOI] [PubMed] [Google Scholar]
- 4.Robinson C.M., Howes J., Murdoch H., Will E., Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Jt Surg Am Vol. 2006;88(11):2326–2336. doi: 10.2106/JBJS.E.01327. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed I., Ashton F., Robinson C.M. Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability: functional outcomes and identification of risk factors for recurrence. J Bone Jt Surg Am Vol. 2012;94(14):1308–1315. doi: 10.2106/JBJS.J.01983. [DOI] [PubMed] [Google Scholar]
- 6.Castagna A., Garofalo R., Conti M., Flanagin B. Arthroscopic Bankart repair: have we finally reached a gold standard? Knee Surg Sports Traumatol Arthrosc. 2016;24(2):398–405. doi: 10.1007/s00167-015-3952-6. [DOI] [PubMed] [Google Scholar]
- 7.Di Giacomo G., Itoi E., Burkhart S.S. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy. 2014;30(1):90–98. doi: 10.1016/j.arthro.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Rees J.L., Shah A., Edwards K., et al. Treatment of first-time traumatic anterior shoulder dislocation: the UK TASH-D cohort study. Health Technol Assess. 2019;23(18):1–104. doi: 10.3310/hta23180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saper M.G., Milchteim C., Zondervan R.L., Andrews J.R., Ostrander R.V., 3rd Outcomes after arthroscopic Bankart repair in adolescent athletes participating in collision and contact sports. Orthop J Sports Med. 2017;5(3) doi: 10.1177/2325967117697950. 2325967117697950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Antunes J.P., Mendes A., Prado M.H., Moro O.P., Miro R.L. Arthroscopic Bankart repair for recurrent shoulder instability: a retrospective study of 86 cases. J Orthop. 2016;13(2):95–99. doi: 10.1016/j.jor.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watch G., Boileau P., Levigne C., Mandrino A., Neyret P., Donell S. Arthroscopic stabilization for recurrent anterior shoulder dislocation: results of 59 cases. Arthroscopy. 1995;11(2):173–179. doi: 10.1016/0749-8063(95)90063-2. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto N., Kijima H., Nagamoto H., et al. Outcome of Bankart repair in contact versus non-contact athletes. Orthop Traumatol Surg Res. 2015;101(4):415–419. doi: 10.1016/j.otsr.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Aboalata M., Plath J.E., Seppel G., Juretzko J., Vogt S., Imhoff A.B. Results of arthroscopic Bankart repair for anterior-inferior shoulder instability at 13-year follow-up. Am J Sports Med. 2017;45(4):782–787. doi: 10.1177/0363546516675145. [DOI] [PubMed] [Google Scholar]
- 14.Blonna D., Bellato E., Caranzano F., Assom M., Rossi R., Castoldi F. Arthroscopic Bankart repair versus open bristow-latarjet for shoulder instability: a matched-pair multicenter study focused on return to sport. Am J Sports Med. 2016;44(12):3198–3205. doi: 10.1177/0363546516658037. [DOI] [PubMed] [Google Scholar]
- 15.Harris J.D., Gupta A.K., Mall N.A., et al. Long-term outcomes after Bankart shoulder stabilization. Arthroscopy. 2013;29(5):920–933. doi: 10.1016/j.arthro.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Murphy A.I., Hurley E.T., Hurley D.J., Pauzenberger L., Mullett H. Long-term outcomes of the arthroscopic Bankart repair: a systematic review of studies at 10-year follow-up. J Shoulder Elbow Surg. 2019;28(11):2084–2089. doi: 10.1016/j.jse.2019.04.057. [DOI] [PubMed] [Google Scholar]
- 17.Milchteim C., Tucker S.A., Nye D.D., et al. Outcomes of Bankart repairs using modern arthroscopic technique in an athletic population. Arthroscopy. 2016;32(7):1263–1270. doi: 10.1016/j.arthro.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 18.Brilakis E., Avramidis G., Malahias M.-A., et al. Long-term outcome of arthroscopic remplissage in addition to the classic Bankart repair for the management of recurrent anterior shoulder instability with engaging Hill–Sachs lesions. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):305–313. doi: 10.1007/s00167-018-5261-3. [DOI] [PubMed] [Google Scholar]
- 19.Memon M., Kay J., Cadet E.R., Shahsavar S., Simunovic N., Ayeni O.R. Return to sport following arthroscopic Bankart repair: a systematic review. J Shoulder Elbow Surg. 2018;27(7):1342–1347. doi: 10.1016/j.jse.2018.02.044. [DOI] [PubMed] [Google Scholar]
- 20.Privitera D.M., Bisson L.J., Marzo J.M. Minimum 10-year follow-up of arthroscopic intra-articular Bankart repair using bioabsorbable tacks. Am J Sports Med. 2012;40(1):100–107. doi: 10.1177/0363546511425891. [DOI] [PubMed] [Google Scholar]
- 21.Gerometta A., Rosso C., Klouche S., Hardy P. Arthroscopic Bankart shoulder stabilization in athletes: return to sports and functional outcomes. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1877–1883. doi: 10.1007/s00167-014-2984-7. [DOI] [PubMed] [Google Scholar]
- 22.Flinkkila T., Knape R., Sirnio K., Ohtonen P., Leppilahti J. Long-term results of arthroscopic Bankart repair: minimum 10 years of follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):94–99. doi: 10.1007/s00167-017-4504-z. [DOI] [PubMed] [Google Scholar]
- 23.Randelli P., Ragone V., Carminati S., Cabitza P. Risk factors for recurrence after Bankart repair a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2129–2138. doi: 10.1007/s00167-012-2140-1. [DOI] [PubMed] [Google Scholar]
- 24.Marshall T., Vega J., Siqueira M., Cagle R., Gelber J.D., Saluan P. Outcomes after arthroscopic Bankart repair: patients with first-time versus recurrent dislocations. Am J Sports Med. 2017;45(8):1776–1782. doi: 10.1177/0363546517698692. [DOI] [PubMed] [Google Scholar]
- 25.Adam M., Attia A.K., Alhammoud A., Aldahamsheh O., Al Ateeq Al Dosari M., Ahmed G. Arthroscopic Bankart repair for the acute anterior shoulder dislocation: systematic review and meta-analysis. Int Orthop. 2018;42(10):2413–2422. doi: 10.1007/s00264-018-4046-0. [DOI] [PubMed] [Google Scholar]
- 26.Vermeulen A.E., Landman E.B.M., Veen E.J.D., Nienhuis S., Koorevaar C.T. Long-term clinical outcome of arthroscopic Bankart repair with suture anchors. J Shoulder Elbow Surg. 2019;28(5):e137–e143. doi: 10.1016/j.jse.2018.09.027. [DOI] [PubMed] [Google Scholar]
- 27.Lee J.H., Park I., Hyun H.S., Kim S.W., Shin S.J. Comparison of clinical outcomes and computed tomography analysis for tunnel diameter after arthroscopic Bankart repair with the all-suture anchor and the biodegradable suture anchor. Arthroscopy. 2019;35(5):1351–1358. doi: 10.1016/j.arthro.2018.12.011. [DOI] [PubMed] [Google Scholar]