Abstract
Minoritized communities are underreached by biomedical interventions, such as the COVID-19 vaccine. This mixed-methods study identified factors associated with vaccine likelihood (VL) and uptake (VU) among 187 Latino sexual minority men (LSMM) in South Florida. Regression models with LASSO variable selection and Classification and Regression Trees (CART) assessed determinants of VL and VU while open-ended questions were evaluated using thematic content analysis. VL (range 1–7; M = 6.00, SD = 1.84) and VU (63.6%) was high. LASSO modeling identified being insured, worrying about others, fear of transmitting COVID-19, and financial stress as the most influential factors for VL; working remotely from home was important for VU. Time (weeks) since addition of COVID-19 vaccination-related questions (December 2nd, 2020) was associated with both outcomes across both modeling techniques. Convergence between data suggests capitalizing on altruistic motivations and improving accessibility to vaccine campaigns are valuable assets to increase LSMM’s vaccine confidence.
Keywords: COVID-19, Vaccine hesitancy, Sexual minority men, Latina/o/x, Mixed-methods
Introduction
Nearly 18 months into the COVID-19 pandemic, Hispanics/Latina/x/os1 (hereafter Latina/x/o) remain the most likely to experience severe COVID-19 morbidity, hospitalization, and mortality compared to all other racial/ethnic groups (Centers for Disease Control & Prevention, 2021; “Hispanic Americans Are Most Vulnerable to COVID-19,” 2021). All 42 states that include ethnicity data in COVID-19 data report infections among Latina/x/o people at two to four times their proportion of the overall population (“Hispanic Americans Are Most Vulnerable to COVID-19,” 2021), with Latina/x/o people nearly twice as likely as Black or Indigenous Americans – and 2.5 times more likely than White Americans – to become hospitalized with COVID-19. This increased burden is due to various factors, including overrepresentation in low wage “essential worker” positions that simultaneously offer high rates of exposure, poor health coverage and minimal sick leave, higher proportions of densely populated, multigenerational households (Lopez et al., 2021; McClure et al., 2020; Rodriguez-Diaz et al., 2020), and historical exclusion from comprehensive and equitable social and healthcare services (Lacayo, 2017). Furthermore, for Latina/x/o individuals whose identities are minoritized at multiple intersections (e.g., ethnicity, documentation status, sexual and gender minority statuses), these effects may be compounded due to intersecting inequities.
Latino sexual minority men (LSMM) may face additional structural, psychosocial, and health challenges associated with COVID-19, potentially attributable to minority stress. Minority Stress Theory posits that sexual orientation-related stigma is the fundamental cause underlying health disparities for lesbian, gay, bisexual, and other sexual minorities compared to their heterosexual counterparts (Meyer, 1995, 2003). Emerging evidence shows that LSMM experienced significant declines in mental health during the pandemic (Harkness et al., 2020), likely related to concomitant financial loss (Linnemayr et al., 2021) and its cascading effects to other determinants of health such as housing instability, social isolation, inadequate health care access, intimate partner violence, and substance misuse (Rhodes et al., 2021). Additionally, existing disparities worsened during COVID-19 when stay-at-home mandates reduced access to venues and organizations that provided affirming support to LSMM (Gonzales et al., 2020; Harkness, et al., 2021a, 2021b). Therefore, it is important to utilize an intersectional lens to understand the compounding effects of pandemic related stressors, as well as potential enablers or assets related to access to interventions, such as COVID-19 vaccines, that may lessen their burden.
Latina/x/os, and LSMM specifically, are often underreached by new biomedical prevention and treatment interventions. For example, influenza vaccine uptake among those identifying as Latina/x/o is lower (37.0%) than both Black (38.5%) and non-Latino White Americans (48.2%; Centers for Disease Control & Prevention, 2018). Data from August 2021 suggests that Latina/x/o-identifying individuals are significantly less likely to have received a COVID-19 vaccine dose than white Americans, increasing their already high risk of hospitalization and death (Ndugga et al., 2021). Possible reasons for this disparity have been investigated in Latina/x/o populations with reduced access to quality care, a historical and valid mistrust of the medical establishment (Suite et al., 2007), and individual vaccine ambivalence as potentially shaping uptake and intent to be vaccinated for COVID-19 (Sobo et al., 2021). However, this stands at odds with emerging research on LSMM vaccine attitudes and uptake among sexual and gender minorities broadly. In a diverse, bi-national survey of more than 7000 lesbian, gay, bisexual, and transgender (LGBT) people from June 2021, almost 70% of respondents (and 80% of Latina/x/o-identifying respondents) had already been vaccinated with 84% of non-vaccinated individuals reporting a desire to get vaccinated as soon as possible (Tegan & Sara Foundation, 2021).
As vaccination rates begin to stall and COVID-19 variants increase in frequency and virulence, additional research is needed to understand factors that may facilitate vaccine uptake among racial/ethnic and sexual minority populations. To understand COVID-19 vaccine attitudes and uptake among LSMM, we conducted a concurrent triangulation mixed methods study with a group of LSMM residing in South Florida—a majority-Latina/x/o area in a state that is currently a US epicenter of the fourth wave of COVID-19, driven by cases among the unvaccinated.
Methods
Participants and procedures
The present mixed-methods study is a secondary data analysis of a longitudinal cohort study (called “DÍMELO”; N = 290; Harkness, et al., 2021a, 2021b) examining access to behavioral and HIV prevention services among LSMM in South Florida. Self-report questions related to COVID-19 vaccine likelihood and uptake were collected via REDcap at the 8-month follow-up (8MFU) assessment (between December 2020 and July 2021), which included qualitative and quantitative questions assessed in English or Spanish. Eligible LSMM were recruited into the parent study through social and sexual networking platforms, word of mouth, and consent-to-contact databases. LSMM were eligible for the parent study if they identified as HIV-negative or unknown HIV status, age 18 to 60 years, Latino/Hispanic, gay, bisexual, or a man who has sex with men, and living in the greater Miami area. Participants were excluded if they were unable to provide consent or read or speak English or Spanish. The current study also excluded participants who did not complete the 8MFU assessment (n = 46), completed the 8MFU before the COVID-19 vaccine questions were added (n = 50), showed a pattern of inattentive responding (n = 2), or had incomplete data (n = 5), resulting in a final analytic sample of 187. Study procedures were IRB approved by [MASKED FOR REVIEW] and informed consent was obtained from all participants.
Measures
All measures were available in English and Spanish; participants could select which language the survey was presented in. Following established guidelines, measures not available in Spanish were translated by bilingual team members as follows: forward translation (English to Spanish), back translation (Spanish back to English), and an evaluation of the original and back-translated versions to ensure meaning was retained (Kurtines & Szapocznik, 1995).
Quantitative measures
Demographics
Demographic questions included age, financial stress, insurance, sexual orientation, nativity, citizenship, race/ethnicity, and employment.
Somatic symptoms
The 8-item Somatic Symptom Scale (SSS-8: (Gierk et al., 2014); α = 0.84) evaluates self-reported physical symptoms like “back pain” and “feeling tired or having low energy,” within the past 7 days. Items are rated using a 5-point Likert scale from 0 (not at all) to 4 (very much) and summed, with higher scores indicating greater somatic symptoms.
Pandemic stress
Items from the Pandemic Stress Index (Harkness et al., 2020), which evaluates the impact of COVID-19 in multiple domains, were used in the current analysis. The following binary items (yes or no) were included: “Previously tested for COVID-19,” “Isolating or quarantining yourself,” “No changes to my life or behavior,” “More anxiety,” “More depression,” “Fear of giving COVID-19 to someone else,” “Fear of getting COVID-19,” “Frustration or boredom,” “Confusion about what COVID-19 is, how to prevent it, or why social distancing/isolation/quarantines are needed,” “Feeling that I was contributing to the greater good by preventing myself or others from getting COVID-19,” “Being diagnosed with COVID-19,” “Loneliness,” “Worrying about friends, family, partners, etc.,” “A change in sexual activity,” “Working from home,” “Following media coverage related to COVID-19,” and “Stigma or discrimination from other people.” Additionally, an ordinal item from 1 (not at all) to 5 (extremely) was included: “How much is/did COVID-19 impact your day-to-day life?”.
Problem solving
The 11-item Problem-Solving Confidence (α = 0.87) subscale of the Problem-Solving Inventory (Heppner & Petersen, 1982) examined problem-solving confidence with items such as “Many problems I face are too complex for me to solve.” Items were assessed using a 6-point Likert scale ranging from 1 (strongly agree) to 6 (strongly disagree) and summed such that lower scores indicated greater problem-solving confidence.
Time since vaccine approval
Because participants completed their 8MFU survey assessments anytime from October 2020 to April 2021, we created a variable reflecting the time (measured in weeks) between when first COVID-19 vaccine questions were asked of participants on December 2nd, 2020, and the date each participant ended up completing the 8MFU. This date was not only chosen as a close parallel to the date in which the FDA authorized emergency use of the Pfizer/BioNTech COVID-19 vaccine on December 11th, 2020, but also allowed for individual differences in survey completion time and access to the vaccine.
COVID-19 vaccine likehood and uptake
Participants reported their likelihood of getting a COVID-19 vaccine using a 7-point Likert scale from 1 (not at all likely) to 7 (very likely; National Institutes of Health, 2021). They also reported their vaccine uptake, using an item designed based on the stages of change from the transtheoretical model (Prochaska & DiClemente, 1982). Participants indicated their stage of change with respect to vaccine uptake: “I am not planning to get the COVID-19 vaccine,” “I am considering getting the COVID-19 vaccine,” “I have scheduled an appointment to get the COVID-19 vaccine,” “I have already gotten the COVID-19 vaccine,” and “I have already received the COVID-19 vaccine and plan get future vaccines if needed.” This variable was dichotomized such that the first two stages (not getting/considering vaccine) were coded as “no” and the last three items (scheduled/received/will continue) were coded as “yes”.
Qualitative assessment
Based on how participants answered the COVID-19 uptake question, branching logic was used to invite participants to respond to an open-ended question further probing their reasons why they would or would not obtain a COVID-19 vaccine.
Analytic plan
Quantitative analysis
Although Florida first received doses of an FDA emergency authorized vaccine on December 30th, 2020, all people over the age of 18 were not eligible to access them until April 5th, 2021. Therefore, due to the fluid nature of the vaccine rollout process, all participants regardless of their vaccination status at the time of survey completion were included in the analytic samples for exploring both vaccine likelihood and uptake so to not risk losing valuable information.
All data were interrogated using numeric and graphical exploratory data analysis methods. Two modeling strategies were used, regression models with LASSO variable selection and Classification and Regression Trees (CART). Regression models provide estimates which indicate the direction of effects (i.e., increasing or decreasing vaccine likelihood and chances of uptake) and the size of effects (i.e., a small or large increase/decrease in vaccine likelihood and chance of uptake). LASSO methods shrink the size of effects to give results that are likely to be replicated. With LASSO, estimates for variables which do not predict an outcome will shrink to zero, indicating they do not strongly relate to the outcome. LASSO provides summaries of the relative importance of different predictors in a way that is less biased than traditional “p-values.”
Our second modeling strategy, CART, is a method that splits data into “homogenous” groups of people. CART models form upside-down “trees” with the top split being the best at classifying people into groups (e.g., LSMM who have been vaccinated vs. not). Then, within those subgroups CART finds additional splits. “Leaves,” at the bottom the tree, represent similar groups of people in terms of their outcome. Tracing from the top of the tree to the leaves identifies the profile of similar people in terms of their outcome. Regression/LASSO and CART methods both offer predictions for how future respondents may feel about vaccination based on known sociodemographic and behavioral predictors.
To judge the quality of the models, different sections of the data are used to train the models and then test the results. Here, models were trained on 70% of the data. LASSO models were tuned using a regular grid of 50 values and 50 bootstrap resamples. CART trees were tuned for both complexity () and tree depth across a regular grid of 5 levels, using tenfold cross-validation. For the seven-point likelihood of vaccination variable, performance was assessed using root mean squared error (RMSE). For the binary vaccine uptake variable, model quality was assessed using area under the ROC curve.
Analyses were conducted with R version 4.1.0 with the tidyverse (1.3.1), rUM (0.3.0), haven (2.4.3), and Table1 (1.4.2) packages used to preprocess, model, and summarize data (Balise & Odom, 2021; R Core Team, 2018; Rich, 2021; Wickham, 2021; Wickham et al., 2019). Modeling was conducted using tidymodels (0.1.3) using the rpart (4.1.15) and glmnet (4.1.2) engines and variable importance was assessed using the vip (0.3.2) package (Friedman et al., 2021; Greenwell et al., 2017; 2021; Kuhn & Wickham, 2021; Therneau et al., 2019).
Table 1.
Participant characteristics (N = 187)
| Demographic predictors | Mean (SD) or n (%) |
|---|---|
| Age (years) | 33.00 years (8.46) |
| Nativity | |
| U.S. born | 81 (43.3%) |
| Non-U.S. born | 106 (56.7%) |
| Preferred language | |
| Only Spanish | 35 (22.3%) |
| Only English | 77 (49.0%) |
| Both Spanish and English | 45 (28.7%) |
| How often in the past 12 months were you stressed for money? | |
| Always | 25 (13.4%) |
| Usually | 36 (19.3%) |
| Sometimes | 53 (28.3%) |
| Rarely | 35 (18.7%) |
| Never | 38 (20.3%) |
| Other | 5 (0.80%) |
| Has health insurance | 145 (77.4%) |
| Total problem-solving confidence (PSI) | 51.6 (9.83) |
| Total somatic symptoms severity (SSS-8) | 7.83 (5.93) |
| Total heritage culture score | 72.25 (16.23) |
| Total mainstream culture score | 67.38 (16.51) |
| COVID-19 behaviors | |
| Social distancing | 159 (85.0%) |
| Following COVID-19 media coverage | 114 (61.0%) |
| No change in behavior | 26 (13.9%) |
| Isolating/quarantining | 101 (54.0%) |
| Working from home | 84 (44.9%) |
| More anxiety | 108 (57.8%) |
| Frustration/boredom | 119 (63.6%) |
| Confusion about COVID-19 | 41 (21.9%) |
| Desire to contribute to the greater good | 79 (42.2%) |
| More depression | 84 (44.9%) |
| Prior COVID-19 diagnosis | 51 (27.3%) |
| Fear of getting COVID-19 | 127 (67.9%) |
| Fear of giving COVID-19 to somebody else | 107 (57.2%) |
| Loneliness | 89 (47.6%) |
| Change in sexual activity | 119 (63.6%) |
| Experienced stigma or discrimination | 38 (20.3%) |
| Worrying about others | 136 (72.7%) |
| Prior testing for COVID-19 | 167 (89.3%) |
| Change in sexual activity | 119 (63.6%) |
| How has COVID-19 impacted your day-to-day life? | |
| Not at all | 6 (3.2%) |
| A little | 43 (23.0%) |
| Much | 55 (29.4%) |
| Very much | 36 (19.3%) |
| Extremely | 47 (25.1%) |
| Vaccination factors | |
| Weeks since addition of COVID-19 vaccine-related questions (December 2nd, 2021) and completion of 8MFU | 17.8 (5.44) |
| Vaccine likelihood (range 1: extremely unlikely – 7: extremely likely) | 6.06 (1.79) |
| Which of the following applies to you regarding the COVID-19 vaccine? | |
| I am not planning to get the COVID-19 vaccine | 14 (7.5%) |
| I am considering getting the COVID-19 vaccine | 54 (28.9%) |
| I have scheduled an appointment to get a COVID-19 vaccine | 67 (35.8%) |
| I have already received the COVID-19 vaccine | 20 (10.7%) |
| I have already received the COVID-19 vaccine and will continue to get vaccines in the future | 32 (17.1%) |
Qualitative analysis
The last author developed a codebook of vaccine uptake barriers and facilitators using a mixed inductive and deductive approach. Codes were identified from a prior qualitative study on barriers to vaccination among a community sample of adults (Fisher et al., 2020), and then refined based on a preliminary review of the qualitative data from the current study. Following the development of the codebook, the last author trained the coding team (first, sixth, and seventh authors) to code the qualitative responses and iteratively revise the codebook based on emerging codes. The codebook was organized via a spreadsheet the coding team used to record codes. The sixth and seventh authors independently coded qualitative responses. The coding team, led by the first author, met weekly to review codes, iteratively revise the codebook, and establish consensus. Coding meetings allowed coders to discuss codebook interpretations and propose refinements to the codebook which ensured consistent and clear coding.
The coding team represented various levels of educational experience and included two undergraduate students, one graduate student in clinical psychology with a background in public health, and a faculty member with a background in psychology and public health. Coders were racially/ethnically diverse, either a self-identified sexual minority (first author) or LGBTQ + affirming and had a basic knowledge of Spanish. All participants had the chance to provide responses, yet only 164 participants provided some qualitative data, of which 151 were codable.
Mixed methods analysis
Triangulation was used to check the validity of our qualitative and quantitative data (Creswell, 2015). The first author, with feedback from the co-author team, identified areas of convergence and divergence between both types of data. Findings are illustrated in Fig. 5.
Fig. 5.
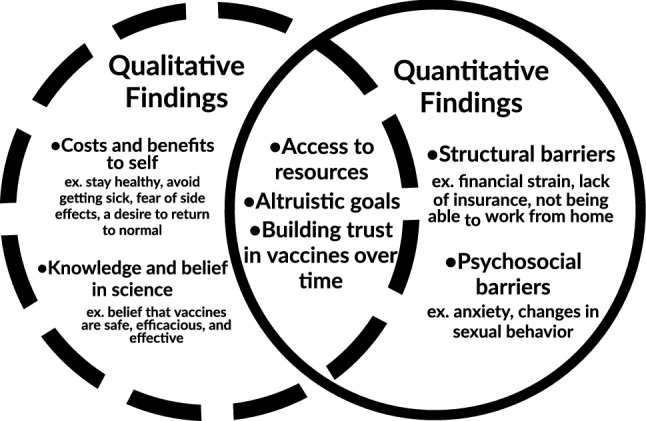
Convergence and Complementarity Between Qualitative and Quantitative Data. Convergent findings between the qualitative and quantitative data can be found in the center of the two circles. Complementary qualitative and quantitative findings can be found in the outer circles
Results
Participant characteristics
Table 1 contains complete demographic information for participants in this analysis (N = 187). Participants ranged in age from 19 to 60 years (M = 33.03, SD = 8.46). Most participants were born outside the United States (57%), had health insurance (78%), and reported financial stress sometimes, usually or always (61%). Most indicated a strong likelihood of obtaining a vaccine (M = 6.06, SD = 1.79) and 64% met our criteria for vaccine uptake (reported that they have scheduled/received/will continue to receive) a COVID-19 vaccine.
Quantitative findings
For each variable modeled (vaccine likelihood and uptake), we first present the LASSO results which informed variable selection, followed by ordinary linear regression analysis (for vaccine likelihood) and logistic regression (for vaccine uptake) and finally, the CART models which explore patterns within subgroups. Models related to the vaccine likelihood outcome are described first followed by models associated with the vaccine uptake outcome.
Outcome 1: vaccine likelihood
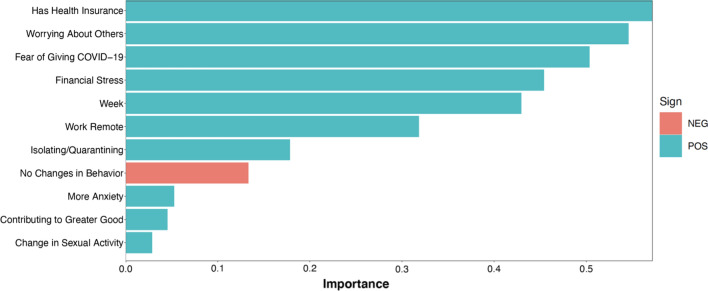
As shown in Fig. 1, 11 variables were determined by LASSO to be useful in predicting likelihood of vaccination. Although most of the selected variables (n = 10) were associated with increased vaccine likelihood, one led to decreased likelihood. As illustrated by the relatively long bars in Fig. 1, five variables including health insurance status, worrying about others, fear of giving COVID-19 to others, financial stress, and weeks since FDA emergency authorization approval were the most influential.
Fig. 1.
LASSO modeling for vaccine likelihood. *Variable reflecting the time (measured in weeks) between addition of first COVID-19 vaccine questions (December 2, 2020) and the date the participant completed the 8MFU
To aid in the interpretation of the model, a traditional linear regression model was fit using the features selected by LASSO. Four features, low financial stress (b = 0.77, 95% CL: 0.19—1.36, p = 0.009), more weeks since initiation of vaccine related questions (beta = 0.62, 95% CL: 0.39—0.85, p < 0.001), having health insurance (beta = 0.59, 95% CL: 0.03—1.14, p = 0.038), and a fear of giving COVID-19 to others (beta = 0.57, 95% CL: 0.05—1.09, p = 0.031) were all statistically significantly associated with a greater likelihood for vaccination among LSMM using a cut point of p < 0.05.
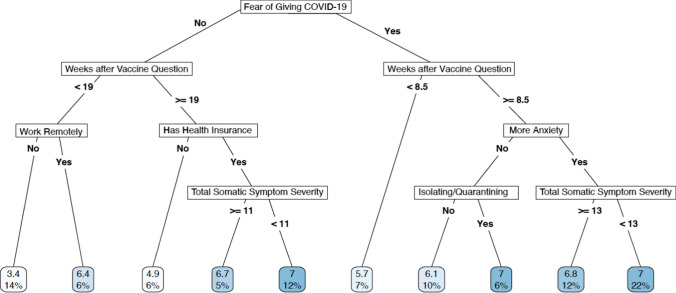
The regression tree shown in Fig. 2 identifies 7 variables as being important in predicting vaccine likelihood. Several variables were used repeatedly to make subgroups resulting in 9 different subsets of participants. The variable at the top of the tree, which can be interpreted as the feature that is best for predicting vaccine likelihood was fear of giving COVID-19 to someone else. Time since addition of COVID-19 related questions (December 2nd, 2020), as measured in weeks was the next most important variable. Many groups were predicted to have scores of “7” indicating that they reported being “very likely” to get an approved COVID-19 vaccine when it was available. However, CART also identified subgroups that were not likely to get vaccinated. For example, the 7% of participants who are in the right most branch of the tree consisted of LSMM who indicated they were “extremely likely” to get vaccinated (score of “7” on vaccine likelihood question). This group were fearful of giving COVID to others, completed their survey at or after early February (8.5 weeks after initiation of vaccine related questions), and had a total symptom severity score on the SSS-8 greater than or equal to 13 (high symptom severity).
Fig. 2.
CART Modeling for Vaccine Likelihood. The numbers located in the leaves of the tree (at the bottom of the page) represent both the predicted score (1–7) on the vaccine likelihood question as well as the proportion of the total analytic sample who fell into each of these distinct subgroups
Model evaluation using the testing data suggested that the LASSO model (RMSE: 1.9) was marginally better than the CART performance (RMSE: 2.2).
Outcome 2: vaccine uptake
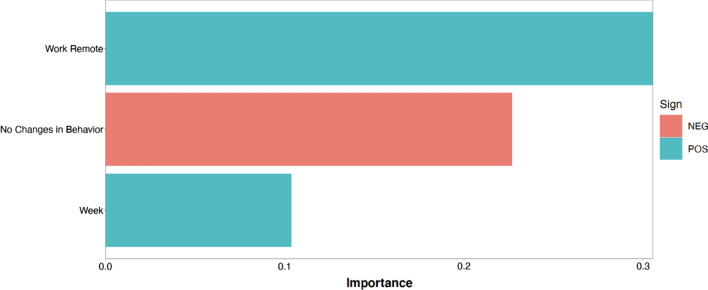
As shown in Fig. 3, three variables were determined by LASSO to be useful in predicting vaccine uptake. Two (working remotely and weeks since initiation of vaccine related questions) were associated with increased chance of vaccine uptake and one led to decreased probability (no change in behavior during COVID-19). As illustrated by the relatively long bar, the most influential variable was difference in time from when the COVID-19 vaccine questions were added to the assessment (December 1, 2020) to when a participant filled out their 8MFU survey.
Fig. 3.
LASSO Modeling for Vaccine Uptake. *Variable reflecting the time (measured in weeks) between addition of first COVID-19 vaccine questions (December 2, 2020) and the date the participant completed the 8MFU
When modeled using logistic regression, only two of the three features identified by LASSO were statistically significant at the p < 0.05 level. Participants who were working remotely were more than 3.5 times more likely to obtain a vaccine (b = 3.69, 95% CL: 1.8—7.96, p < 0.001) and vaccine uptake increased by almost 3 times the odds for each week that went by since addition of the COVID-19 vaccine questions (b = 2.92, 95% CL: 2.05—4.32, p < 0.001). These two variables identified as statistically significant in the logistic regression model maintained their predictive power in anticipating vaccine uptake among LSMM according to CART (Fig. 4). Additionally, problem-solving confidence was also identified by CART as being useful in predicting greater vaccine uptake.
Fig. 4.
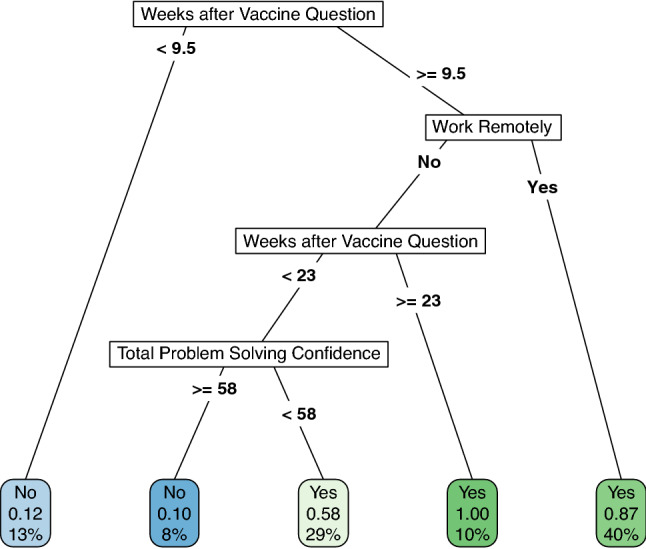
CART modeling for vaccine uptake. *The numbers located in the leaves of the tree (at the bottom of the page) represent both the predicted score (1–7) on the vaccine likelihood question as well as the proportion of the total analytic sample who fell into each of these distinct subgroups
The performance of the LASSO and CART models were comparable with an estimated area under of the receiver operating characteristic curve of 0.79 and an overall accuracy of 0.7.
Qualitative findings
24 codes reflecting facilitators and barriers to vaccine uptake were identified. Codes were organized within five themes: (1) costs and benefits to self, (2) degree of trust or mistrust, (3) altruistic goals, (4) knowledge or belief in science, and (5) general accessibility. Most themes consisted of both facilitator and barrier codes. Findings can be found in Table 2.
Table 2.
Facilitator ( +) and barrier (-) codes grouped by thematic domain with example quotes
| Thematic Domains | Barriers/Facilitators^ | n (%) | Example Quotation |
|---|---|---|---|
| Costs and benefits to self | 118 (78.1%) | ||
| Side effect concerns (-) | 11 (9.3%) | “It’s new and unknown side effects” (34 years old, thinking about getting vaccinated) | |
| Vaccination not a priority (-) | 1 (0.8%) | “Not a priority right now” (29 years old, thinking about getting vaccinated) | |
| Member of a high-risk group ( +) | 3 (2.5%) | “I'm a survivor who, five months later, is STILL dealing with the damage this virus caused” (29 years old, received the vaccine) | |
| Desire to return to normal ( +) | 10 (8.5%) | “Because it helps life get back to normal” (23 years old, planning on getting vaccinated) | |
| Personal protection – desire to stay healthy or avoid getting sick ( +) | 106 (89.8%) | “Protection against COVID-19 and reduction of severe illness and/or death” (37 years old, planning on getting vaccinated) | |
| Required/able to access vaccine through work ( +) | 9 (7.6%) | “I am a healthcare worker, and I believe in them.” (23 years old, received the vaccine) | |
| Peer pressure/societal expectations ( +) | 1 (0.8%) | “To conform” (56 years old, received the vaccine) | |
| Altruistic goals | 25 (15.9%) | ||
| Help the community (e.g., achieve herd immunity) ( +) | 4 (16.0%) | “For the greater good of the community” (30 years old, planning on getting vaccinated) | |
| Prevent transmission to others ( +) | 21 (84.0%) | “I would get if for peace of mind and to be safe around others, knowing I wouldn't be able to transmit it to loved ones” (31 years old, thinking about getting vaccinated) | |
| Knowledge and belief in science | 19 (12.6%) | ||
| Belief that vaccine is effective/efficacious/safe ( +) | 14 (73.7%) | “I trust science & doctors and I believe it is the right thing to do” (26 years old, planning to get the vaccine) | |
| Vaccine efficacy concerns (-) | 1 (5.3%) | “Having to continue receiving the vaccine routinely, unknown side effects” (24 years old, considering getting vaccinated) | |
| General misconceptions or misinformation about vaccines (-) | 1 (5.3%) | “Because of the number of fatalities for it reported by the CDC” (57 years old, not planning to get the vaccine) | |
| Belief in science and research ( +) | 3 (15.8%) | “Research results” (53 years old, considering getting vaccinated) | |
| Degree of trust or mistrust | 10 (6.6%) | ||
| Lack of trust in vaccine development and testing process (-) | 5 (50.0%) | “Don’t feel comfortable with the amount of time it took to clear the vaccine through trials” (32 years old, not planning to get the vaccine) | |
| Lack of trust in government/CDC (-) | 1 (10.0%) | “Because I think COVID-19 is a made-up virus from the government to produce vaccines to fuck up the people” (24 years old, not planning to get the vaccine) | |
| Don’t believe in, want, or feel comfortable with vaccines (-) | 4 (40.0%) | “Not interested” (33 years old, not planning to get the vaccine) | |
| Accessibility | 4 (2.6%) | ||
| Lack of access (-) | 2 (50%) | “Because I am not a citizen or a permanent resident so I do not know if I even could” (19 years old, considering getting the vaccine) | |
| Overall ease of access ( +) | 2 (50%) | “Just because I could” (21 years old, received the vaccine) | |
Themes and subthemes are not mutually exclusive
^ ( +) denotes facilitator codes while (-) identifies barrier codes
Qualitative findings (N = 151)
Costs and benefits to self
LSMM’s vaccine uptake was dependent on their evaluation of the costs vs. benefits they perceived because of getting the vaccine. Participants described personal benefits such as staying healthy, avoiding illness, returning to pre-pandemic life, wanting protection from COVID-19 due to being part of a “high risk” group, and being able to meet work requirements (e.g., vaccination required for return to work). In contrast, some perceived a lack of benefit (i.e., perceiving vaccination to not be a priority) and were therefore less likely to be vaccinated. Although most cited personal benefits that motivated vaccination, some discussed the personal cost of side effects as a deterrent to vaccination.
Altruistic goals
In the scientific literature, altruism is often defined as the process by which an individual engages with certain behaviors outside of their own interest for the sole purpose to help another achieve some form of benefit (Rushton, 1982), with altruistic motivations being an extension of this concept reflecting an individual’s interest in engaging with a behavior to help another. For many LSMM in our study, altruistic motivations such as preventing COVID-19 transmission to others, contributing to herd immunity, and a general desire to keep their community safe facilitated their vaccine uptake contributed to COVID-19 vaccine uptake.
Knowledge and belief in vaccines
Participants who lacked belief in or knowledge about vaccines were hesitant to receive a COVID-19 vaccine. LSMM cited concerns about whether approved COVID-19 vaccines could keep them protected from infection as well as misinformation about the vaccines.
Degree of trust or mistrust
LSMM’s vaccine uptake was influenced by their degree of trust or mistrust in the vaccine development and dissemination process. LSMM’s belief in science and vaccines more broadly facilitated their uptake of the COVID-19 vaccine. In contrast, barriers to vaccination for LSMM included a lack of confidence in either the vaccine development/testing process or the government/relevant governmental institutions (e.g., CDC). Addition barriers included being were uncomfortable with, not believing in, or not being interested in receiving the COVID-19 vaccine.
Accessibility
Although rare, LSMM identified vaccine accessibility issues as a barrier. Vaccine uptake was low for participants who reported that vaccine was hard to access compared to participants who sought out the vaccine for no reason other than its availability.
Mixed methods findings
Figure 5 outlines the areas of convergence and complementarity between the quantitative and qualitative data. Convergence between the two data sources predominately highlighted how psychosocial factors at the individual and community levels (e.g., altruistic motivations) were influential in improving LSMM’s likelihood and uptake of COVID-19 vaccines. Specifically, participants identified a desire to prevent COVID-19 transmission to others and help their community as primary drivers for vaccination qualitatively—a theme which was mirrored in the quantitative data with found that factors such as worrying about others, wanting to contribute to the greater good, and fear of giving COVID-19 to others were predictors for COVID-19 vaccine likelihood and uptake.
In addition to specific areas of convergence, significant complementarity between qualitative and quantitative data was also observed. Although issues related to access were identified in both the qualitative and quantitative data as potential facilitators and barriers to vaccine uptake among LSMM, the specific indicators identified diverged between the two data sources. Factors such as not having insurance, being financially strained, and not being able to work from home during the pandemic were identified by the quantitative data as barriers to vaccination, whereas being required to get vaccinated through work, being in a high-risk group, and having general accessibility to the vaccine were mentioned in participant open-ended responses as facilitators for vaccination. Additionally, time and its relationship to vaccine accessibility and feeling comfortable with the vaccines was a theme identified by LSMM across data types in unique ways. In the open-ended responses, some participants reported varying levels of mistrust in relation to the vaccine development and dissemination process resulting in a lower likelihood and uptake of the vaccine. These findings supported quantitative trends suggesting that for participants who completed their assessments later in the study period were more likely to express a higher likelihood in and uptake of the COVID-19 vaccine.
Discussion
This mixed-methods study is the first to explore psychosocial and structural factors related to COVID-19 vaccination among LSMM. Key factors associated with greater vaccine likelihood for LSMM included low financial stress, more time since addition of COVID-19 related questions and parallel FDA emergency authorization of a COVID-19 vaccine, being insured, expressing concern about transmitting COVID-19 to others, experiencing COVID-19 anxiety, and having high somatic symptoms (i.e., above 13). Vaccine uptake was also strongly predicted by more time since addition of COVID-19 related questions and parallel FDA emergency authorization of a COVID-19 vaccine as well as working from home. Convergent quantitative and qualitative data highlighted trust, altruism, and vaccine accessibility. Additionally, findings suggest strong interest in and uptake of COVID-19 vaccines among LSMM, highlighting the heterogeneity of racial/ethnic minorities in terms of vaccine hesitancy versus confidence (Funk & Tyson, 2020) and confirming data suggesting COVID-19 vaccination interest and uptake among Latina/o/x LGBTQ + individuals are high (~ 80%; Tegan & Sara Foundation, 2021). This is important as we continue as a field to move away from considering Latinos and or sexual minority populations as homogenous and appreciate the nuances between these groups as it relates to both confidence in and hesitancy towards new health promotion interventions like the COVID-19 vaccine.
As the US enters its fourth major COVID-19 wave with ongoing health disparities among Latina/o/xs and sexual minorities (Smith, 2021), innovation is needed to increase vaccination rates. Although our findings suggest high COVID-19 vaccine interest and uptake, improving financial opportunities and knowledge about vaccine development may further serve as enablers and assets for improving interest in and uptake of COVID-19 vaccines among LSMM who remain hesitant. For LSMM who expressed lower vaccine likelihood and actual vaccine uptake, structural factors such as financial stress, lack of insurance, misinformation about vaccines, and lack of access were all barriers to obtaining COVID-19 vaccines, whereas confidence in one’s problem-solving abilities served as a facilitator. Subgroups of LSMM with financial stress, no insurance, and other structural barriers to vaccination, may have felt the effects of these barriers more intensely due to policies (e.g., stringent Medicaid expansion for low-income communities) that have systematically made it more challenging for minoritized groups to access biomedical prevention services (Galvan et al., 2017), and undermined their trust in medicine and public health (Goldstein & Sedacca, 2021). Future vaccination programming should consider how local, state, and federal policies that disenfranchise marginalized communities may contribute to COVID-19 vaccine hesitancy and promote problem solving skills that enables self-efficacy for individuals as they navigate structural barriers to vaccination.
COVID-19 vaccination campaigns tailored to LSMM may benefit from continuing to leverage altruistic goals related to Latina/o/x cultural values and the altruistic strengths of sexual minority communities. For LSMM, cultural factors such as familismo (loyalty to family), personalismo (mutual sharing), and respeto (respect) contribute to their own psychological functioning (De Santis et al., 2019), and also their willingness to seek out certain health services (Bermúdez et al., 2010; Caballero, 2011) to protect their families, friends, and communities. Similarly, the fact that many sexual minority men have ties with not only their families of origin, but also families of “choice” composed of other sexual minority folk suggests that COVID-19 vaccination campaigns could harness peer influence and community wide fellowship among these “created” families to promote vaccination vaccine related knowledge dissemination among LSMM. Leveraging the relational strengths of sexual minority communities is exemplified by the fact that the CDC’s understanding of COVID-19 Delta variant breakthrough cases was supported by the conscientious nature of sexual minority communities in Provincetown, Massachusetts who banded together by sharing COVID-19 statuses, engaging in contact tracing, and promoting vaccination with a universal desire to keep people safe (Simmons-Duffin, 2021).
Finally, it is important to recognize that uptake of new biomedical interventions is not immediate. Accordingly, vaccination campaigns should incorporate an appreciation of the time it takes to build trust and confidence in taking a new vaccine. LSMM who participated later in the study were more likely to have signed up for or received the COVID-19 vaccine. Although this may be in part due to universal vaccine eligibility on April 5th, 2021, it is possible that as participants knew more vaccinated people and heard more positive messages about vaccination, their trust grew, which in turn increased their interest in and uptake of the vaccine. Similarly, the observed dips in interest and uptake of vaccines during certain timepoints in our study points to the possibility that critical events/situations (e.g., FDA pausing roll-out of the Johnson & Johnson vaccine due to blood clots) may occur that could affect trends of interest and uptake of vaccines.
This study is not without limitations. Although the qualitative data facilitated a deeper understanding of the barriers and facilitators to LSMM’s vaccine uptake, responses were brief, and some so sparse that they were uninterpretable. Despite the parent’s study longitudinal design, the COVID-19 vaccine data were cross-sectional, preventing examination of changes over time and the extent to which vaccine intentions translated to uptake. This is important because when we began assessing vaccine uptake, some LSMM were not yet “eligible” based on local and national guidance. The full adult population was officially eligible for the COVID-19 vaccine in April 2021, which is why we included those with a scheduled appointment as having taken up the vaccine and included everyone, regardless of their vaccination status, in the analytic sample for our first outcome exploring vaccine likelihood among LSMM. By doing this, we reduced the potential for validity concerns through the introduction of systematic bias in our analysis of likelihood for vaccination and gained richer insights through our CART modeling procedures which are dependent on larger analytic sample sizes. Now that everyone is eligible for a COVID-19 vaccine and accessibility of COVID-19 vaccination has improved overall, researchers should repeat this study among a larger sample of unvaccinated people now to better tease out additional facilitators and barriers for COVID-19 vaccination uptake among LSMM.
Overall, this study possesses several strengths and innovations. First, the findings are compelling because of the convergence between the qualitative and quantitative data. Relatedly, we used innovative quantitative methods that are recommended for enhancing the replicability of findings (Kuhn & Johnson, 2018). Second, this study assessed a identified a variety of multilevel barriers and facilitators to vaccination and points to modifiable factors to target in vaccine uptake interventions for LSMM. Third, this study focused on LSMM – a population at the intersection of two minoritized groups and disproportionally affected by COVID-19 health disparities—offering a unique insight on the experiences of a population that is often overlooked in biomedical research. Finally, this study was conducted in South Florida, the epicenter of the fourth wave of COVID-19 in the US (Bella & Kornfield, 2021), making the findings even more poignant.
Acknowledgements
We would like to thank Annette Yates and Michaela Larson for their assistance with this project. We also thank every participant in the study and the many community members and partners who shared information about the study to prospective participants.
Author contributions
Conceptualization (EW, NM, MJBR, AH), Formal Analysis (EW, RB, CM, BC, AH), Funding Acquisition (AH, SAS), Investigation (EW, DM, CM, BC, AH), Methodology (EW, RB, AH), Project Administration (EW,AH, DM), Writing – Original Draft (EW, RB, NM, MJBR, CM, AH), Writing – Review & Editing (EW, RB, NM, MJBR, DM, CM, BC, SAS, AH), Visualization (EW, RB).
Funding
Data collection for this study was supported by P30AI073961 (Pahwa) and U54MD002266 (Behar-Zusman). Additional research support was provided by P30MH116867 (Safren). Some of the author time was supported by K24DA040489 (Safren) and K23MD015690 (Harkness). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data availability
The data that support the findings of this study are available within the article and/or its supplementary materials. All other data are available from the corresponding author, EW, upon reasonable request.
Code availability
All code for data cleaning and analysis is available upon request from EW.
Declarations
Conflict of interest
Dr. Safren receives royalties from Oxford University Press, Guilford Publications, and Springer/Humana press for books on cognitive behavioral therapy. Elliott R. Weinstein, Raymond Balise, Nicholas Metheny, Maria Jose Baeza Robba, Daniel Mayo, Cassandra Michel, Bill Chan and Audrey Harkness have no other conflict of interest to disclose.
Ethical approval
All study procedures were approved by the University of Miami’s Institutional Review Board consistent with guidelines on research with human subjects. This study did not include any research on animals.
Consent to participate
Singed informed consent for study protocols was obtained from all participants using informed consent procedures approved by the University of Miami’s Institutional Review Board.
Consent for publication
Singed informed consent regarding publishing of participants’ de-identified data was obtained from all participants.
Footnotes
Following guidance from Dr. del Río-Gonzalez (2021), we use Latina/x/o to describe the overall community and specifically include men, women, and non-binary individuals, whereas we refer to individuals of a specific gender with the corresponding gendered term.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Elliott R. Weinstein, Email: erw73@miami.edu
Raymond Balise, Email: balise@miami.edu.
Nicholas Metheny, Email: nick.metheny@miami.edu.
Maria Jose Baeza Robba, Email: mxb2129@miami.edu.
Daniel Mayo, Email: mayo.f.daniel@gmail.com.
Cassandra Michel, Email: cxm1494@miami.edu.
Bill Chan, Email: bchan1711@gmail.com.
Steven A. Safren, Email: ssafren@miami.edu
Audrey Harkness, Email: aharkness@miami.edu.
References
- Balise, R., & Odom, G. (2021). rUM: R Templates from the University of Miami (0.3.0) [Computer software]. https://CRAN.R-project.org/package=rUM
- Bella, T. & Kornfield, M. (2021, August 1). Florida breaks record for new coronavirus cases as surge of infections rips through state. Washington Post. Retrieved August 30, 2021, from https://www.washingtonpost.com/nation/2021/08/01/florida-highest-coronavirus-cases-record/
- Bermúdez J, Kirkpatrick D, Hecker L, Torres-Robles C. Describing Latinos families and their help-seeking attitudes: Challenging the family therapy literature. Contemporary Family Therapy. 2010;32:155–172. doi: 10.1007/s10591-009-9110-x. [DOI] [Google Scholar]
- Caballero AE. Understanding the Hispanic/Latino patient. The American Journal of Medicine. 2011;124:S10–15. doi: 10.1016/j.amjmed.2011.07.018. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Vaccination coverage among US adults, NHIS, 2016. https://www.cdc.gov/vaccines/imz-managers/coverage/adultvaxview/pubs-resources/NHIS-2016.html
- Centers for Disease Control and Prevention. (2021, August 18). Joint statement from HHS public health and medical experts on COVID-19 booster shots. https://www.cdc.gov/media/releases/2021/s0818-covid-19-booster-shots.html
- Creswell, J. W. (2015). Revisiting mixed methods and advancing scientific practices. The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry. 10.1093/oxfordhb/9780199933624.013.39
- De Santis JP, Gattamorta KA, Valdes B, Sanchez M, Provencio-Vasquez E. The relationship of Hispanic cultural factors and sexual behaviors of Hispanic men who have sex with men. Sexuality & Culture. 2019;23:292–309. doi: 10.1007/s12119-018-9557-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Río-González AM. To Latinx or not to Latinx: A question of gender inclusivity versus gender neutrality. American Journal of Public Health. 2021;111:1018–1021. doi: 10.2105/AJPH.2021.306238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, K. A., Bloomstone, S. J., Walder, J., Crawford, S., Fouayzi, H., & Mazor, K. M. (2020). Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Annals of Internal Medicine,173(12), 964–973. 10.7326/M20-3569 [DOI] [PMC free article] [PubMed]
- Friedman, J., Hastie, T., Tibshirani, R., Narasimhan, B., Tay, K., Simon, N., & Qian, J. (2021). glmnet: Lasso and Elastic-Net Regularized Generalized Linear Models (4.1–2) [Computer software]. https://CRAN.R-project.org/package=glmnet
- Funk, C., & Tyson, A. (2020, December 3). Intent to get a COVID-19 vaccine rises to 60% as confidence in research and development process increases. Pew Research Center Science & Society. https://www.pewresearch.org/science/2020/12/03/intent-to-get-a-covid-19-vaccine-rises-to-60-as-confidence-in-research-and-development-process-increases/
- Galvan FH, Bogart LM, Klein DJ, Wagner GJ, Chen Y-T. Medical mistrust as a key mediator in the association between perceived discrimination and adherence to antiretroviral therapy among HIV-positive Latino men. Journal of Behavioral Medicine. 2017;40:784–793. doi: 10.1007/s10865-017-9843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierk B, Kohlmann S, Kroenke K, Spangenberg L, Zenger M, Brähler E, Löwe B. The somatic symptom scale-8 (SSS-8): A brief measure of somatic symptom burden. JAMA Internal Medicine. 2014;174:399–407. doi: 10.1001/jamainternmed.2013.12179. [DOI] [PubMed] [Google Scholar]
- Goldstein, J., & Sedacca, M. (2021, August 12). Why only 28 percent of young black New Yorkers are vaccinated. The New York Times. https://www.nytimes.com/2021/08/12/nyregion/covid-vaccine-black-young-new-yorkers.html
- Gonzales G, Loret de Mola E, Gavulic KA, McKay T, Purcell C. Mental health needs among lesbian, gay, bisexual, and transgender college students during the COVID-19 pandemic. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2020;67:645–648. doi: 10.1016/j.jadohealth.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwell, B., Boehkme, B., & Gray, B. (2021). Vip: Variable importance plots [R]. koalaverse. https://github.com/koalaverse/vip (Original work published 2017)
- Harkness A, Behar-Zusman V, Safren SA. Understanding the impact of COVID-19 on Latino sexual minority men in a US HIV hot spot. AIDS and Behavior. 2020 doi: 10.1007/s10461-020-02862-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness, A., Weinstein, E. R., Atuluru, P., Hernandex Altamirano, D., Vidal, R., Rodriguez-Diaz, C., & Safren, S. A. (In Press). Latino sexual minority men’s intersectional minority stress, general stress, and coping during COVID-19: A rapid qualitative study. [DOI] [PMC free article] [PubMed]
- Harkness, A., Weinstein, E. R., Atuluru, P., Mayo, D., Vidal, R., Rodriguez-Diaz, C., & Safren, S. A. (2021a). Latinx sexual minority men’s access to HIV and behavioral health services during COVID-19: Barriers, facilitators, and implications for innovation. Journal of the Association of Nurses in AIDS Care. [DOI] [PMC free article] [PubMed]
- Harkness A, Weinstein ER, Mayo D, Rodriguez-Diaz C, Safren SA. Latinx sexual minority men’s behavioral, psychosocial, and medical experiences during COVID-19: Differences across immigration statuses. Annals of LGBTQ Public and Population Health. 2021 doi: 10.1891/LGBTQ-2020-0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heppner P, Petersen C. The development and implications of a personal problem-solving inventory. Journal of Counseling Psychology. 1982;29:66–75. doi: 10.1037/0022-0167.29.1.66. [DOI] [Google Scholar]
- Hispanic americans are most vulnerable to COVID-19. (2021, June 5). The Economist. https://www.economist.com/united-states/2021/06/05/hispanic-americans-are-most-vulnerable-to-covid-19
- Kuhn M, Johnson K. Applied predictive modeling. Springer; 2018. [Google Scholar]
- Kuhn, M., & Wickham, H. (2021). Tidymodels: Easily install and load the “tidymodels” packages (0.1.3) [Computer software]. https://CRAN.R-project.org/package=tidymodels
- Kurtines WM, Szapocznik J. Cultural competence in assessing Hispanic youths and families: Challenges in the assessment of treatment needs and treatment evaluation for Hispanic drug-abusing adolescents. NIDA Research Monograph. 1995;156:172–189. [PubMed] [Google Scholar]
- Lacayo CO. Perpetual inferiority: Whites’ racial ideology toward Latinos. Sociology of Race and Ethnicity. 2017;3:566–579. doi: 10.1177/2332649217698165. [DOI] [Google Scholar]
- Linnemayr S, Mayo-Wilson LJ, Saya U, Wagner Z, MacCarthy S, Walukaga S, Nakubulwa S, Karamagi Y. HIV care experiences during the COVID-19 pandemic: Mixed-methods telephone interviews with clinic-enrolled HIV-infected adults in Uganda. AIDS and Behavior. 2021;25:28–39. doi: 10.1007/s10461-020-03032-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez L, III, Hart LH, III, Katz MH. Racial and Ethnic Health Disparities Related to COVID-19. JAMA. 2021;325:719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- Mayo, D. (In Press). “We know you’re gay but we don’t talk about it”: Conceptualizing the nuances of cultural experiences of Latino sexual minority men.
- McClure ES, Vasudevan P, Bailey Z, Patel S, Robinson WR. Racial capitalism within public health-How occupational settings drive COVID-19 disparities. American Journal of Epidemiology. 2020;189(11):1244–1253. doi: 10.1093/aje/kwaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. Journal of Health and Social Behavior. 1995;36:38–56. doi: 10.2307/2137286. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2021). Community engaged research alliance against COVID-19 disparities common survey []. RTI International.
- Ndugga, N., Hill, L., Artiga, S., & Parker, N. (2021, August 18). Latest data on COVID-19 vaccinations by race/ethnicity. KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/
- Prochaska JO, DiClemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy Theory, Research & Practice. 1982;19:276–288. doi: 10.1037/h0088437. [DOI] [Google Scholar]
- R Core Team. (2018). R: A language and enviroment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/
- Rhodes SD, Mann-Jackson L, Alonzo J, Garcia M, Tanner AE, Smart BD, Horridge DN, Van Dam CN, Wilkin AM. A rapid qualitative assessment of the impact of the COVID-19 pandemic on a racially/ethnically diverse sample of gay, bisexual, and other men who have sex with men living with HIV in the US south. AIDS and Behavior. 2021;25:58–67. doi: 10.1007/s10461-020-03014-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich, B. (2021). table1: Tables of descriptive statistics in HTML [R]. https://github.com/benjaminrich/table1 (Original work published 2017)
- Rodriguez-Diaz CE, Guilamo-Ramos V, Mena L, Hall E, Honermann B, Crowley JS, Baral S, Prado GJ, Marzan-Rodriguez M, Beyrer C, Sullivan PS, Millett GA. Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics. Annals of Epidemiology. 2020 doi: 10.1016/j.annepidem.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushton JP. Altruism and Society: A Social Learning Perspective. Ethics. 1982;92:425–446. doi: 10.1086/292353. [DOI] [Google Scholar]
- Simmons-Duffin, S. (2021). How a gay community helped the CDC spot a COVID outbreak—And learn more about Delta. http://www.capradio.org/news/npr/story?storyid=1025553638
- Smith, C. H. (2021, August 19). Harris County’s Latino community remains underinsured and unvaccinated. Houston Public Media. https://www.houstonpublicmedia.org/articles/news/health-science/2021/08/19/406269/texas-latino-community-remains-underinsured-and-unvaccinated/
- Sobo, E., Schow, D., & McClure, S. (2021, July 8). Black and Latino communities often have low vaccination rates – But blaming vaccine hesitancy misses the mark. PBS NewsHour. https://www.pbs.org/newshour/health/black-and-latino-communities-often-have-low-vaccination-rates-but-blaming-vaccine-hesitancy-misses-the-mark
- Suite DH, La Bril R, Primm A, Harrison-Ross P. Beyond misdiagnosis, misunderstanding and mistrust: Relevance of the historical perspective in the medical and mental health treatment of people of color. Journal of the National Medical Association. 2007;99:879–885. [PMC free article] [PubMed] [Google Scholar]
- Tegan and Sara Foundation. (2021). It’s for us: COVID-19 vaccination and the LGBTQ+ communitiy. https://static1.squarespace.com/static/582601b4440243fc471a91d0/t/60c76c654a25e73bb1fc850d/1623682153103/It%27s+For+US-+COVID-19+Vaccination+and+the+LGBTQ%2B+Community.pdf
- Therneau, T., Atkinson, B., & Ripley, B. (2019). rpart: Recursive Partitioning and Regression Trees (4.1–15) [Computer software]. https://CRAN.R-project.org/package=rpart
- Wickham, H. (2021). Tidyverse: Easily install and load the “tidyverse” (1.3.1) [Computer software]. https://CRAN.R-project.org/package=tidyverse
- Wickham H, Averick M, Bryan J, Chang W, McGowan LD, François R, Grolemund G, Hayes A, Henry L, Hester J, Kuhn M, Pedersen TL, Miller E, Bache SM, Müller K, Ooms J, Robinson D, Seidel DP, Spinu V, Yutani H. Welcome to the tidyverse. Journal of Open Source Software. 2019;4:1686. doi: 10.21105/joss.01686. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available within the article and/or its supplementary materials. All other data are available from the corresponding author, EW, upon reasonable request.
All code for data cleaning and analysis is available upon request from EW.