Abstract
Women, and specifically women of color, are underrepresented in clinical trials, limiting biological understanding and contributing to health inequities and social injustice. Analyses of barriers to inclusion suggest practical interventions that together create a roadmap of specific and actionable steps to increase diverse representation in research and sustainable change.
Women, and specifically women of color, are underrepresented in clinical trials, limiting biological understanding and contributing to health inequities and social injustice. Analyses of barriers to inclusion suggest practical interventions that together create a roadmap of specific and actionable steps to increase diverse representation in research and sustainable change.
Main text
Introduction
The safety, efficacy, and effectiveness of medicinal products depends upon the review and approval of planned clinical trials by impartial regulatory bodies including ethical review boards and health regulatory agencies. The practical adoption of study findings, however, depends upon the interpretation, communication, and strength of the results, and then upon the decisions and actions of healthcare practitioners and the public. Participation in clinical trials, therefore, should generally represent those affected by the disease or condition and for whom the intervention or product is intended, and that in turn depends upon the epidemiology of the condition or the intended use of the product. In the absence of appropriate epidemiological data relating to the incidence and severity of the condition being studied, participation should generally reflect the general population, with appropriate safeguards to protect vulnerable populations.
But what is representativeness, and how specific need one be? At one extreme, evaluating for every subgroup in a statistically meaningful way would require infinitely large clinical trials. At the other extreme, the concept of personalized medicine would imply that robust trials of specific subgroups are unnecessary, since every individual is unique. The practical compromise is to ensure that the evidence base for medicinal products is robust for major subgroups and that the collection of data for certain populations and for certain questions continues thereafter.
Historically, women have been underrepresented in clinical trials, but there has been a steady increase in the representation of women over the last several decades—in part a consequence of laws, regulations, policies, and guidance.1 However, in certain therapeutic areas, women remain underrepresented in, and underserved by, clinical trials despite efforts to mitigate the lack of inclusion, and that underrepresentation is significantly more acute for women of color. In this text, the term “women” is used to represent biological sex at birth. While many of the same issues discussed here apply to sexual orientation and gender identity, a topic deserving of thorough exploration, we are unable to consider these further in this short commentary. Here we examine factors that impact inclusion, biological and societal consequences of failing to correct underrepresentation, and multiple practical changes that can and should be introduced to advance inclusion.
Underrepresentation of women in clinical trials
The representation of women in clinical trials has increased over the years. In an effort to make demographic participation data more transparent, the US Food and Drug Administration (FDA) publishes Drug Trials Snapshots2 annually. Importantly, the data represent only participants that informed FDA approval of new drugs, and only for new molecular entities (NMEs) and biologics. Over the last 6 years, the percentage of women included in these trials has ranged from 40%–72% (Table 1). The data are only partially disambiguated and reported by therapeutic area (TA) (e.g., sex, race, and age are reported only for the top 3 or 4 TAs over the last 4 years). Further, while sex and race are reported, the interaction of sex and race are not, and thus the data cannot generally be analyzed by intersectional characteristics (e.g., sex by race). For example, the proportion of women is reported, the proportion of Black or African American people is reported, but the number of women who are Black or African American is not. The intersection of sex and race was only reported once in the 2015–2016 publication and, of women enrolled in global cardiovascular drug trials, only 3.2% were Black or African American. Latino and Hispanic ethnicity data are available beginning only in 2017, and data describing the intersection of sex and ethnicity are not reported. As the data are currently presented, it is not possible therefore to determine accurately the deficit in representation. Note, however, that the total percentage of participants (of which women comprise less than half) in oncology trials who were Black or African American over the years 2017–2020 ranged from 2% to 5%, and of Hispanic or Latino ethnicity from 4% to 6%. These numbers are in stark contrast to the demographics of the US population of which 12.1% are Black or African American and 18.7% are Hispanic or Latino, and the largest racial and ethnic minorities in the country, respectively.3 Not only are women underrepresented in certain therapeutic areas, but women of color are disproportionately excluded. In addition to FDA-regulated trials, numerous reports confirm the underrepresentation of women of diverse racial and ethnic backgrounds in post-approval trials, NIH-supported trials, comparative effectiveness trials, vaccine trials, and others.4, 5, 6, 7 An even more prevalent problem is the significant proportion of trials that fail to report race and ethnicity at all and, when reported, fail to analyze the data by demographic subgroup.
Table 1.
Summary demographic data from FDA Drug Trial Snapshots
| Women (%) | Black/AA (%) | Asian (%) | White (%) | Other (%) | Age 65 or older (%) | |
|---|---|---|---|---|---|---|
| 2015 | 40 | 5 | 12 | 79 | 4 | 37 |
| 2016 | 48 | 7 | 11 | 79 | 7 | 21 |
| 2017 | 55 | 7 | 11 | 77 | 14 | 32 |
| 2018 | 56 | 11 | 10 | 69 | 14 | 15 |
| 2019 | 72 | 9 | 9 | 72 | 18 | 36 |
| 2020 | 56 | 8 | 6 | 75 | 11 | 30 |
Data are reproduced from the US FDA Drug Trial Snapshots reports that make available information about who participated in the clinical trials that informed the approval of either new molecular entities or biologic products in the given calendar year. The information is limited to the data available at the time of FDA approval and is not updated. Selected subpopulation demographic information from these trials is presented. AA, African American.
The absence of data and/or data disaggregated by subgroup results in the absence of knowledge for that population: drugs cannot be prescribed, devices cannot be used, and vaccines cannot be administered with certainty of safety or efficacy. Evidence suggests that the lack of data is meaningful: analysis by Ramamoorthy and colleagues has shown that, of new FDA-approved drugs, approximately 20% (2008–2013)8 and 10% (2014–2019)9 showed differences in exposure and/or response based on race, ethnicity, or pharmacogenetics that were sufficiently large to result in population-specific prescribing recommendations in certain cases. Subgroup differences reflect underlying biological differences, differences that are not caused by, but rather correlate with, race and ethnicity. Although sex is generally considered a biological variable,10 race and ethnicity are not; the underlying factors for racial and ethnic differences may relate to genetic diversity, co-morbidities, socioeconomic resources, housing, nutrition, or any number of other possibilities. It is with this knowledge that further studies must commence: why does drug, biologic, or vaccine response differ? What are the underlying biological factors that influence physiology? Subgroup differences are initial indicators for further investigation, not an end in themselves. The data to inform some of these potential factors are not routinely collected in clinical trials, nor are common data standards available, and any analysis is therefore blind to potential confounding variables and/or important correlations. In failing to ask these questions, not only do we forgo further scientific discovery, but we lose the opportunity to understand factors contributing to health equity.
Barriers to and approaches to increase participation of women
Barriers to research participation exist at structural, institutional, investigator, and participant levels and have been identified and reviewed (Box 1).6,11 What matters is not a detailed description of barriers, but rather the approaches and solutions that will ameliorate the challenges to participation. No single solution will be determinative, but each barrier needs to be addressed; a multiplicity of inclusive efforts is required, and all stakeholders in the clinical research enterprise have a role to play in that correction, with responsibility and accountability for their actions (Box 2).
Box 1. Selected barriers to clinical trial participation.
System and systemic barriers
Access
Education
Internet access, digital literacy, and access to technology
Healthcare practitioners uninformed of clinical trials or unwilling to refer
Provider attitudes and low referral patterns
Lack of outreach programs
Lack of incentives for participation
Participating centers not sited in appropriate geographic locations
Lack of community-based research programs
No regulatory standards to require inclusion or representation
Bias, racism
Mistrust
Trial design barriers
Lack of appropriate clinical trials
- Eligibility requirements
-
(1)Requirement to read, speak, or write English
-
(2)Exclusion of: older adults (e.g., >65 years) and children (<18 years); pregnant or lactating women; co-morbidities; cognitive or intellectual disabilities; physical disabilities; mental illness; polypharmacy; obese individuals; laboratory values normalized for white, not other, populations
-
(3)Inclusion of: requirement for health insurance coverage; requirement for internet access; requirement for certain personal information (e.g., social security number, immigration status); ability to provide consent
-
(1)
- Trial design
-
(1)Inflexibility in design (e.g., lack of adaptive features)
-
(2)Frequent data collection
-
(3)Requirements for in-person visits and at hospital or clinical site
-
(4)Inadequate consideration of decentralized and digital alternatives
-
(1)
- Trial recruitment
-
(1)Lack of health-literate and culturally and linguistically appropriate materials
-
(2)Recruitment in geographies of insufficient diversity
-
(3)Perception and discretion of investigators
-
(1)
Participant barriers
Lack of understanding of clinical trials
Language concordance between informational materials and participant
Health literacy of participant-facing materials
Age-appropriate materials (for children, the elderly)
Accessibility of materials and trial sites
Access to trials (e.g., education, information, location)
Expense and cost of participation
Lack of transportation
Time of participation
Loss of work
Childcare and eldercare responsibilities
Insurance requirements
Privacy and confidentiality concerns
Cultural and personal beliefs
Mistrust
Box 2. Considerations to promote inclusion in clinical trials.
Regulators, funders, editors, and oversight bodies
Require reporting of sex, race, ethnicity and sex by race and ethnicity
Require reporting of screening, enrollment, retention, completion, and any disproportionality
Require comparison of demographics of clinical trial population to epidemiology of disease by demographic
- Develop common data standards for collection and reporting of
-
(1)Gender identity and sexual orientation
-
(2)Social determinants of health
-
(1)
Sponsors and institutions
Early and authentic engagement with community and others
Recruit, train, and support a diverse workforce
Plan for inclusion in trial time and cost/budget
Navigate differing regulatory expectations and proactively plan for appropriate representation
Investigators and their study teams
Help define scientific utility of inclusion
Refine eligibility criteria to those scientifically or ethically justified
Provide accurate site feasibility assessments
Plan for adequate staffing and time
Develop subgroup-informed recruitment and retention strategies
Provide cultural competence and implicit bias training for all staff
Use best available data standards
Standardize data collection and reporting to the extent possible
Utilize best practices in conduct
Deploy decentralized and hybrid trials
Provide transparent data analyses plans
Participants, patient advocacy groups, and public
Improve awareness
Seek access
Request that study design and research procedures be less burdensome
Provide input on logistics of trial conduct
Address mistrust
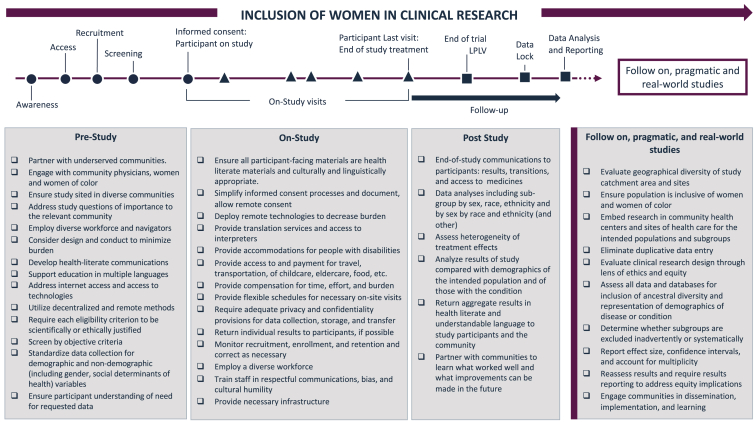
Addressing each barrier substantively, from developing the study question to conduct, analysis, and reporting, to post-approval studies (e.g., observational studies, comparative effectiveness research, pragmatic and simple trials, social and behavioral research, real world data studies) is important (Figure 1). In this way, clinical trial sponsors and trialists—and others—can focus on each step of a clinical trial to develop a more comprehensive assessment and solution set to challenges, disaggregated by subgroup. Women often carry the dual burden of family caretaker and economic contributor; efforts should therefore focus on how to reduce the additional burden participation in clinical trials may impose. Thus, for instance, an effort to recruit and retain Latina women might include attention to the challenges they face specifically. For example, if visits to the trial sites are required, arrangements and payment for travel, transportation, food, eldercare, childcare, and other incidental expenses should be provided. Payment must be prompt and include compensation for time and burden. Clinic hours of operation outside of the typical workday and school day, typically early evening and weekend hours, are considerate of inflexible work schedules and childcare responsibilities. Attention should also be given to the geographic location of the trial sites; an understanding of how the community receives trusted information (thus informing educational information and invitations to participate); engagement with local institutions of faith, gathering places, and networks; and, importantly, translation of all participant-facing materials into Spanish. Translations should be vetted by members of the community to ensure linguistic nuances and cultural humility. Remote technologies that are offered or utilized must be available in Spanish as should instructions for use. If participation is dependent on technologies, not only should internet access be provided but data plans paid for, smartphones provided, and tech support offered in Spanish. Members of the workforce and the research team, and specifically those individuals who will be interacting with participants and their caregivers should be bilingual if possible and, if not, interpreters should be provided. When available, aggregate and/or individual results should be health literate and translated into Spanish and offered in preferred formats (e.g., email, text, letter, etc.) for communication. Of course, this example is neither prescriptive nor complete: engagement with community members will inform additional approaches to increase participation.
Figure 1.
Practical approaches, by study phase, for inclusion of women in clinical research
For each study phase, a model checklist of actionable steps for the inclusion of women, and underrepresented subgroups of women, is presented. The study phases are divided into three parts: pre-study, on-study, and follow-up. In addition, considerations for post-approval trials (e.g., observational studies, comparative effectiveness research, platform or master trials, pragmatic or simple trials, trials utilizing real world data) are shown. The list is neither exhaustive nor prescriptive; considerations will vary by disease or condition, intended participant population, geographic, resources, and other factors.
Beyond clinical trials
No clinical trial portfolio can be sufficiently powered to allow robust statistical analysis of all subgroup differences. Further, for safety reasons, clinical trials may have restrictive eligibility criteria such that the study population differs from the affected real-world population that is or will be subject to the intervention. And differences between the contexts of clinical trials and real-world experiences are known—the duration of exposure is often shorter, and compliance with interventions (e.g., taking a medication on schedule for as long as intended) is often greater in clinical trials than when prescribed for clinical care. Rare safety events can often only be identified by observational data or submitted reports after a product is in wide and sometimes prolonged use, not from the limited numbers of participants, regardless of their demographic distribution, in clinical trials. Thus, diversity and inclusion of underrepresented populations of women are necessary in post-approval clinical research.
Optimally, “real-world” data would reflect the diversity of the general population, those with the condition or disease, or those who receive the intervention. But attention to the collection and analysis of data remains paramount. First, real-world data are often collected during clinical care visits or for billing or other purposes and are therefore not of the same “quality” as data intentionally collected within the strict parameters of clinical trials. Second, real-world data, including data extracted from electronic medical records, often suffer from a high degree of “missingness” that must be accounted for, and methods to do so differ. Third, data definitions may differ across systems and sites, and even by their use or context. Fourth, sample size should be based on disease-specific epidemiological data; standardized analyses and reporting of the data that include estimated effect size of and confidence intervals for each subgroup, tests of interaction, and accounts for multiplicity of analyses should be required. Finally, the representativeness of the data informing any analysis is an important criterion for its use. Data from insurance claims, for instance, may well underrepresent immigrant populations or those who are economically disadvantaged, leading to conclusions that are not generalizable. While analysis of real-world data might inform heterogeneity of treatment effect for subgroups (e.g., underrepresented populations), its limitations must be appreciated.
As the research community takes on the challenge of understanding the biology and social and political implications of diverse populations, it is important to measure those factors that might inform important health correlates. As mentioned, the fact that social determinants of health are rarely captured in clinical trials and not systematically collected in health care settings presents a significant barrier to progress. An immediate recommendation is to develop common data standards for social determinants of health that are likely to correlate with outcomes—factors such as economic stability, education, nutrition, housing, and others—coupled with an educational campaign to explain to the public why these data are necessary and to what use they will be put. Further, ways of asking for the data that are socially and culturally appropriate, and standardized, must be developed. Community and public engagement in this activity will be helpful to uncover methods of ascertaining accurate data. Protections against misuse, including sanctions where necessary, must be introduced. Importantly, information shared by the public for the benefit of understanding the diagnosis, treatment, and prevention of disease, addressing health equity, and/or preserving and protecting public health should not be used for other purposes (e.g., employment, insurability, deportation, taxation). Individuals should be asked to share their data only when there is safety and trust in the use of those data.
In addition to those actions that sponsors, investigators, institutions, and sites may take, others in the clinical trial ecosystem can advance the inclusion of women and specifically women of color. All clinical research results should be reported with demographic information that allows analysis of data by sex, race, and ethnicity, among other factors (e.g., social determinants of health), and with the intersection of sex by race and ethnicity. In addition, screening, recruitment, and retention data should be included, and disproportionate failures to complete should be reported. These data should be presented with what is known about the epidemiological demographics of the condition being studied. Journal editors, funders, and federal agencies should require such reporting. Federal agencies need to acquire, analyze, and report epidemiological demographic (and non-demographic) data with attention not only to the condition or disease, but with other relevant data such as stage of disease. Review committees for funding, policy committees, and standards development bodies must include representatives of the relevant community so that individuals with relevant lived experience can speak directly, for themselves, and for their community and not through an intermediary; such service should be compensated appropriately to allow those individuals to dedicate the time and attention required.
Community partnership, collaboration, and consultation are necessary to ensure that the questions asked are relevant and resonant with, or driven by, community members. Investment in clinical research infrastructure in the community should be coupled with investment in education and innovation, and with training of a diverse workforce. Directing efforts and resources to support the inclusion of underrepresented women in research will strengthen both the generalizability of research findings and their direct application to improvement in health outcomes and health equity.
Acknowledgments
Author contributions
Conceptualization: B.E.B., L.G.M., H.R.A., and S.A.W.; Writing – original draft: B.E.B.; Writing – review and editing: B.E.B., L.G.M., H.R.A., and S.A.W.
Declaration of interests
The authors declare no competing interests.
References
- 1.National Institutes of Health. (1993). NIH Revitalization Act of 1993 Public Law 103-43.
- 2.US Food and Drug Administration Drug Trial Snapshots. https://www.fda.gov/drugs/drug-approvals-and-databases/drug-trials-snapshots
- 3.United States Census Bureau Population. https://www.census.gov/topics/population.html
- 4.Dawson S., Campbell S.M., Giles S.J., Morris R.L., Cheraghi-Sohi S. Black and minority ethnic group involvement in health and social care research: A systematic review. Health Expect. 2018;21:3–22. doi: 10.1111/hex.12597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flores L.E., Frontera W.R., Andrasik M.P., Del Rio C., Mondríguez-González A., Price S.A., Krantz E.M., Pergam S.A., Silver J.K. Assessment of the inclusion of racial/ethnic minority, female, and older individuals in vaccine clinical trials. JAMA Netw. Open. 2021;4:e2037640. doi: 10.1001/jamanetworkopen.2020.37640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan D., Sze S., Minhas J.S., Bangash M.N., Pareek N., Divall P., Williams C.M., Oggioni M.R., Squire I.B., Nellums L.B., et al. The impact of ethnicity on clinical outcomes in COVID-19: A systematic review. EClinicalMedicine. 2020;23:100404. doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clark L.T., Watkins L., Piña I.L., Elmer M., Akinboboye O., Gorham M., Jamerson B., McCullough C., Pierre C., Polis A.B., et al. Increasing diversity in clinical trials: overcoming critical barriers. Curr. Probl. Cardiol. 2019;44:148–172. doi: 10.1016/j.cpcardiol.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Ramamoorthy A., Pacanowski M.A., Bull J., Zhang L. Racial/ethnic differences in drug disposition and response: review of recently approved drugs. Clin. Pharmacol. Ther. 2015;97:263–273. doi: 10.1002/cpt.61. [DOI] [PubMed] [Google Scholar]
- 9.Ramamoorthy A., Knepper T.C., Merenda C., Mendoza M., McLeod H.L., Bull J., Zhang L., Pacanowski M. Demographic composition of select oncologic new molecular entities approved by the FDA between 2008 and 2017. Clin. Pharmacol. Ther. 2018;104:940–948. doi: 10.1002/cpt.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute of Health Office of Research on Women’s Health. NIH Policy on Sex as a Biological Variable. https://orwh.od.nih.gov/sex-gender/nih-policy-sex-biological-variable
- 11.Bierer B.E., White S.A., Meloney L.G., Ahmed H.R., Strauss D.H., Clark L.T. Achieving diversity, inclusion, and equity in clinical research, version 1.0. Multi-Regional Clinical Trials Center of Brigham and Women’s Hospital and Harvard. 2020. https://mrctcenter.org/diversity-in-clinical-trials/