Abstract
CONTEXT
Racial/ethnic inequities are well documented in both maternal-infant health and substance use disorder treatment outcomes.
OBJECTIVE
To systematically review research on maternal-infant dyads affected by opioid use disorder (OUD) to evaluate for racial/ethnic disparities in health utilization or outcomes and critically assess the reporting and inclusion of race/ethnicity data.
DATA SOURCES
Peer-reviewed literature in MEDLINE, Embase, and Web of Science from 2000 to 2020.
STUDY SELECTION
Research reporting health utilization and outcomes data on dyads affected by OUD during pregnancy through the infant’s first birthday.
DATA EXTRACTION
We extracted data on race/ethnicity, study exposures/outcomes, how race/ethnicity data were analyzed, how authors discussed findings associated with race/ethnicity, and whether racism was mentioned as an explanation for findings.
RESULTS
Of 2023 articles reviewed, 152 quantitative and 17 qualitative studies were included. Among quantitative studies, 66% examined infant outcomes (n = 101). Three articles explicitly focused on evaluating racial/ethnic differences among dyads. Among quantitative studies, 112 mentioned race/ethnicity, 63 performed analyses assessing for differences between exposure groups, 27 identified racial/ethnic differences, 22 adjusted outcomes for race/ethnicity in multivariable analyses, and 11 presented adjusted models stratified by race/ethnicity. None of the qualitative studies addressed the role that race, ethnicity, or racism may have had on the presented themes.
CONCLUSIONS
Few studies were designed to evaluate racial/ethnic inequities among maternal-infant dyads affected by OUD. Data on race/ethnicity have been poorly reported in this literature. To achieve health equity across perinatal OUD, researchers should prioritize the inclusion of marginalized groups to better address the role that structural racism plays.
Over the past decade, the rate of deliveries affected by maternal opioid-related diagnoses in the United States more than doubled, from 3.5 cases per 1000 delivery hospitalizations in 2010 to 8.2 per 1000 deliveries in 2017.1 Along with an increase in the prevalence of maternal opioid use disorder (OUD), there has been an increase in neonatal abstinence syndrome (NAS), also referred to as neonatal opioid withdrawal syndrome (NOWS), rising from 4.0 to 7.3 cases per 1000 hospital births from 2010 to 2017.1 Untreated OUD during pregnancy has been associated with a lack of prenatal care, increased unscheduled health care utilization, increased risk of fetal growth restriction, fetal death, preterm labor, NOWS, and maternal mortality.2,3 During the same period, significant racial inequities in maternal-infant morbidity and mortality rates have persisted, with Black and Indigenous individuals having 4 to 5 times higher rates of mortality than White individuals, and the Black infant mortality rate was more than double that of White infants.4,5 Similarly, racial inequities have been noted in substance use disorder (SUD) treatment in both the pregnant and the general population, with non-White people being less likely to enter or complete substance use treatment programs, having less access to medications to treat OUD (MOUD), and having lower adherence.6–11 Even with these documented inequities across the perinatal continuum and within substance use treatment, and the significant growth in research exploring maternal and infant outcomes among maternal-infant dyads affected by OUD, a clear understanding of the inequities in health outcomes for dyads affected by OUD by race/ethnicity is lacking.
Objectives
In the setting of increased calls to deepen our understanding of the root causes of inequities and address structural racism within perinatal and SUD care12–15 and the dearth of medical research addressing the impact of racism,16 we designed this scoping review to (1) identify studies assessing for racial/ethnic inequities in outcomes and health care utilization metrics among dyads affected by OUD; (2) critically assess how the existing literature incorporates and analyzes parental or infant data on race/ethnicity; and (3) evaluate how studies addressed the role of structural determinants of health, specifically the identification of whether racism is acknowledged and discussed as a root cause for described differences. Finally, we provide recommendations for future research and health care guidelines to try to address existing health inequities in perinatal substance use care.
Methods
Eligibility Criteria, Information Sources, Search Strategy
We used a scoping review methodology because of our broad aim of assessing how a large set of heterogenous literature incorporated race/ethnicity data into their analyses and discussions.17 We developed our search strategy in consultation with a medical librarian who executed searches in Ovid MEDLINE, Embase, and Web of Science. Key words used were related to the concepts of opioid use, the peripartum period, and pregnancy outcomes; all databases were searched from inception to August 2020. The full MEDLINE search strategy is listed in Supplemental Table 4. Additionally, potentially relevant citations identified from reviewing literature from key citations or topics highly relevant to our review were identified through December 2020 and included. Citations were deduplicated using EndNote X8 and uploaded to Covidence systematic review software for screening.
Study Selection
Full-text articles were obtained if they had a clear focus on opioids and studied individuals during pregnancy or dyads up to 1 year after delivery. To further narrow the search, we chose to restrict our analysis to studies published after January 1, 2000, and inside the United States to limit studies to those related to the current US opioid epidemic. We included all studies related to OUD in pregnancy and postpartum, including the nonmedical use of prescription opioids. Studies focusing on the use of prescribed opioids during pregnancy (eg, chronic pain conditions, sickle cell disease) were believed to be outside the scope of the current study and were excluded. We excluded studies comparing outcomes of dyads affected by OUD with nonexposed dyads, as we believed these to represent significantly different study populations. We also excluded studies containing only descriptive data because we would not be able to address our third aim of evaluating how race/ethnicity was assessed with respect to outcomes reported. Editorials, case series, case reports, animal research, conference proceedings, non-English language, and cohort studies or pilot trials with <30 participants were excluded (given limited analyses with small sample sizes and problems of generalizability). Two reviewers independently reviewed all deduplicated titles and abstracts using Covidence systematic review software. Conflicts were resolved by consensus or by a third reviewer.
Data Extraction and Application of the Public Health Critical Race Framework (PHCRF)
We extracted study location, year, design, and reported race/ethnicity data. We classified studies based on the category of primary outcome assessed, including (1) prenatal/delivery, (2) maternal postpartum, (3) infant, and (4) outcomes crossing these multiple categories, but did not exclude any studies based on outcome studied. Types of outcomes studied by category are presented in Table 1. Each study was reviewed by a single extractor, with any areas of uncertainty reviewed by a second reviewer and discussed as a team to reach consensus.
TABLE 1.
Outcomes Studied in the Literature Describing Dyads Affected by OUD by Category
| Outcome Category | Primary Outcomes Measured |
|---|---|
| Maternal | |
| Prenatal | Screening for OUD, prenatal toxicology testing, engagement and adherence with MOUD, nonprescribed and polysubstance use during pregnancy, unscheduled health care utilization, fetal growth restriction, delivery complications, serious maternal morbidity, peripartum pain management |
| Postpartum | Adherence with MOUD, recurring nonprescribed substance use, parental custody retention, maternal overdose, receipt of postpartum maternal care, postpartum contraception receipt, maternal morbidity and mortality, postpartum depression or mood disorders, community-based services engagement |
| Infant | Rooming-in, NAS severity including length of stay and need for pharmacologic treatment, receipt of maternal breastmilk, infant birth weight, preterm birth, head circumference, child welfare outcomes, early intervention engagement, hospital readmission rates |
| Multiple outcomes | Combination of any maternal and infant outcomes classified above that cross categories |
The PHCRF was adapted for public health practitioners from critical race theory, a construct developed to account for the influence of racism on outcomes and research processes within legal studies. PHCRF principles highlight the importance of race consciousness; race as a social construct rather than biological difference; the intersections of race with other characteristics, including gender; and the pervasiveness of racism, including in health care settings.18 We chose to use this framework for this scoping review to add methodological rigor to the process of broadly characterizing how researchers analyzed for inequities or documented race/ethnicity, as few studies explicitly set out to explore differences in outcomes by race/ethnicity. Previous research has successfully integrated this framework into structured reviews.19
First, to assess a measure of race consciousness, we determined if each study made any mention of race/ethnicity in any part of their methods, results, or discussion. Although race and ethnicity are distinct and important characteristics, given that they were often grouped in the research we analyzed, we used a composite variable to describe inclusion of race and/or ethnicity data. Second, we reviewed the studies’ methods to identify whether race was described as a social construct. Results were then scrutinized for statistical analyses that assessed for potential confounding or differences in exposure or primary outcome by race. Third, we extracted data on whether studies adjusted for race/ethnicity and stratified the primary outcome by race/ethnicity in multivariable modeling. Studies that presented exploratory analyses assessing multiple predictors that included outcome data by race/ethnicity were included in the group of studies that stratified by outcome. Finally, discussion sections were reviewed to identify how researchers interpreted the impact of differences by race/ethnicity and to determine if racism was discussed as a contributor to the outcomes studied. Qualitative studies were categorized separately and similarly reviewed independently to assess how race, ethnicity, or racism were reported in the themes that emerged.
A Note on Language
In this scoping review, we use the word maternal when describing birthing parents and individuals capable of pregnancy and delivery. We acknowledge the limitations of this approach because not all pregnant individuals and birthing parents identify as women. We use “Latinx” to describe individuals with ancestry from Latin American countries. Although many of the studies included in this review describe ethnicity of participants as “Hispanic,” we use “Latinx” to be as inclusive and specific as possible.
Results
Study Selection
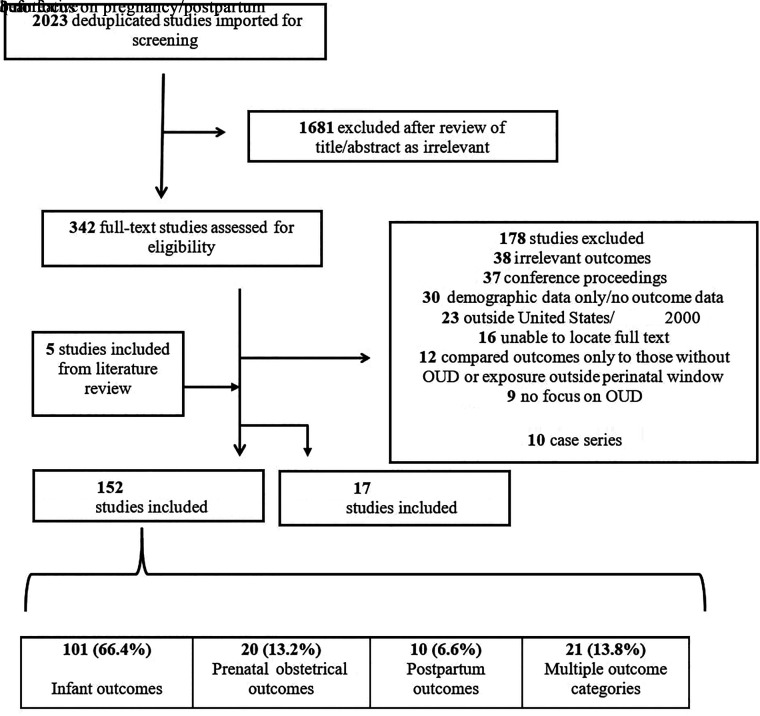
Our initial search yielded 2023 unduplicated articles. After reviewing all titles and abstracts, 342 met screening criteria. Five additional studies were identified from a review of citations or recently published literature. After full-text review, 152 quantitative studies and 17 qualitative studies were deemed eligible and included in the full analysis. Reasons for exclusion for the other 178 articles are shown Fig 1.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses review schematic: maternal-infant outcomes classification.
Study Characteristics
Summary characteristics of the included quantitative studies are shown in Table 2; all extracted data are shown in Supplemental Tables 5 and 6 for quantitative and qualitative studies, respectively. In the majority of the quantitative studies included, researchers examined infant outcomes (n = 101, 66.4%), followed by multiple (21, 13.8%), prenatal/obstetric (20, 13.2%), and postpartum (10, 6.6%) outcomes. Of studies that investigated multiple outcomes, 15 examined maternal prenatal and postpartum outcomes, whereas 6 examined maternal and infant outcomes. Seventy-two percent of studies were published between 2010 and 2020, and 65.8% included >100 participants. Retrospective cohort studies were the most common study type (67.1%).
TABLE 2.
Summary Characteristics of Included Quantitative Studies (n = 152)
| Study Characteristic | n (%) |
|---|---|
| Study year | |
| 1990–1999 | 2 (1.3) |
| 2000–2009 | 40 (26.3) |
| 2010–2020 | 110 (72.4) |
| No. of participants | |
| <50 | 14 (9.2) |
| 50–100 | 35 (23) |
| 100–200 | 39 (25.7) |
| >200 | 61 (40.1) |
| Unknown | 3 (2) |
| Study type | |
| Retrospective cohort | 102 (67.1) |
| Program evaluation | 15 (9.9) |
| Prospective cohort | 13 (8.6) |
| Randomized controlled trial | 9 (5.9) |
| Cross sectional | 7 (4.6) |
| Systematic review with meta-analysis | 4 (2.6) |
| Nonrandomized experimental study | 2 (1.3) |
| Primary outcome | |
| Infant | 101 (66.4) |
| Multiple | 21 (13.8) |
| Pregnancy/obstetrics | 20 (13.2) |
| Postpartum | 10 (6.6) |
Studies Aimed at Evaluating Racial/Ethnic Inequities
Only 3 articles had an explicit focus on the identification of racial/ethnic differences in maternal or infant outcomes among dyads affected by OUD, with mixed findings. Schiff et al9 (2020) and Peeler et al20 (2020) investigated associations between race/ethnicity and prenatal MOUD, finding in adjusted models that Black and Latinx individuals had significantly lower likelihood than White individuals of receiving any medications or consistently using medications. Parikh et al21 (2019) retrospectively examined associations between race and need for pharmacologic treatment within infants with NOWS. They found that Black infants in their cohort were less likely than White infants to require pharmacotherapy in unmatched data, whereas Peeler et al (2020) found no statistical association between NOWS severity and race/ethnicity.
Reporting of Race/Ethnicity Data
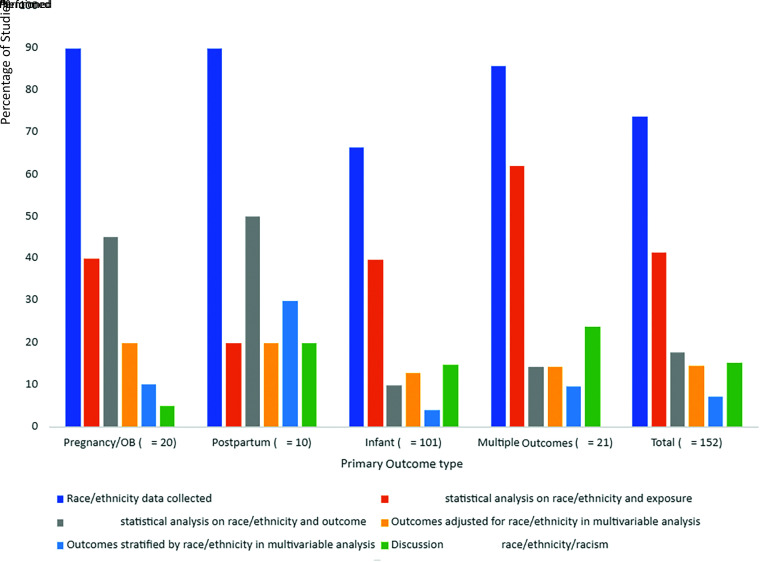
No studies explicitly defined race as a social construct in their study methods. In 112 (73.7%) of the 152 quantitative studies, researchers mentioned race/ethnicity or presented race/ethnicity data in some way, with 107 (70.4%) studies reporting the racial/ethnic breakdown of their study population. Only 66.3% of studies on infant outcomes mentioned or documented race/ethnicity data compared with studies assessing maternal outcomes (90% of prenatal outcome, 90% of postpartum outcome studies) (Fig 2). Prospective studies were more likely to report race/ethnicity data than retrospective studies (Supplemental Fig 3). Of the studies reporting race/ethnicity, 35 (32.7%) had >20% of participants who were non-White and/or Latinx.
FIGURE 2.
Study data collection and analyses of race/ethnicity by outcome categorization. OB, obstetrics.
A total of 63 of 152 studies (41.4%) performed statistical analyses to assess for potential differences between exposure groups based on race/ethnicity, 27 (17.8%) looked at differences by outcome, 22 (14.5%) adjusted outcomes for race/ethnicity in multivariable analyses, and 11 (7.2%) presented adjusted models stratified by race/ethnicity. These categories are presented by primary outcome type in Fig 2. Five studies found significant differences in exposure by race/ethnicity but did not adjust for race/ethnicity in multivariable analysis.22–26 Additionally, in 8 studies, race/ethnicity was included as a model covariate in the a priori analysis plan, even though no statistically significant racial/ethnic differences were identified by primary exposure.27–36
Studies Identifying Racial/Ethnic Differences
There were 9 quantitative studies that reported racial/ethnic differences in their primary outcomes (Table 3). In addition to the 3 studies described above,9,20,21 Scott et al37 (2020) found that Black infants were less likely than White infants to receive pharmacologic treatment of NOWS, yet this finding did not persist in multivariable modeling. Short et al36 (2016) looked at infant length of stay as a marker of NOWS severity and found that non-White maternal race was associated with an increased length of stay. Schiff et al38 (2018) explored characteristics associated with breastfeeding among dyads affected by OUD and found that maternal White race was negatively associated with breastfeeding initiation, but the association did not remain significant in adjusted analyses. Among studies looking at postpartum metrics, Krans et al39 (2018) identified in their study of postpartum contraceptive use patterns that Black and Latinx individuals with OUD were more likely to receive sterilization than other contraceptive methods. Patton et al35 (2019) investigated postpartum health care utilization among individuals with OUD and found that non-Latinx Black individuals were more likely to receive postpartum health care within the 300 days after delivery than non-Latinx White individuals. Finally, Lo-Ciganic et al40 (2019) evaluated both prenatal and postpartum buprenorphine treatment adherence and found that non-White race was a significant predictor of early treatment discontinuation.
TABLE 3.
Studies Quantitatively Revealing Differences in the Extent to Which Race/Ethnicity Is Associated With Study Outcome, Either in Bivariate Comparison or in Adjusted Models
| Authors | Year | Title | Primary Outcomes | What, if Any, Difference in Outcomes by Race/Ethnicity Was Found? | How Was Race, Racism, or Ethnicity Described in Discussion? |
|---|---|---|---|---|---|
| Infant outcomes | |||||
| Parikh et al (21) | 2019 | Racial Association and Pharmacotherapy in Neonatal Opioid Withdrawal Syndrome | Need for pharmacologic treatment of NOWS | Black infants less likely than White infants to require pharmacotherapy for NOWS in multivariable analysis. | Discussion was focused on potential genetic basis for difference in outcomes and potential that difference in outcomes may be due to differences in methadone dosing for pregnant individuals on the basis of race. |
| Scott et al (37) | 2020 | Factors Associated With the Need for pharmacological Management of Neonatal Opioid Withdrawal Syndrome | Need for pharmacologic treatment of NOWS | Black infants less likely to require pharmacotherapy compared with White infants in bivariate analysis; did not remain significant in multivariable model. | Authors discussed association of race with need for neonatal medication and suggested that limited racial/ethnic variability may be due to “the facility’s patient population rather than actual distribution of opioid use during pregnancy among races.” |
| Short et al (36) | 2016 | The Association Between Breastfeeding and Length Of Hospital Stay Among Infants Diagnosed With Neonatal Abstinence Syndrome: A Population-Based Study of In-Hospital Births | Infant length of stay | Race and ethnicity not significantly associated with breastfeeding status of infants with NAS in bivariate analysis, yet when race and ethnicity were included in multivariable analysis, P = .05 for infant length of stay. | Authors suggested that they may not have seen differences in race and ethnicity as factors given the homogeneity of the study population. |
| Prenatal/obstetrical outcomes | |||||
| Schiff et al (9) | 2020 | Assessment of Racial and Ethnic Disparities in the Use of Medication to Treat Opioid Use Disorder Among Pregnant Women in Massachusetts | Use of MOUD in year before delivery, type of medication used | Compared with White pregnant individuals, Black and Latinx pregnant individuals had lower likelihood of receiving, or consistently using, MOUD and lower likelihood of buprenorphine treatment compared with methadone in multivariable analysis. | Authors described differences in outcomes on the basis of race and ethnicity, including potential barriers to medication treatment and structural racism. |
| Postpartum maternal outcomes | |||||
| Krans et al (39) | 2018 | Postpartum Contraceptive Use and Interpregnancy Interval Among Women With Opioid Use Disorder | Contraception, interpregnancy interval | Compared with non-Latinx White women, Black and Latinx women were more likely to receive female sterilization than other forms of contraception. | Authors did not discuss outcomes related to race and ethnicity in discussion. |
| Patton et al (35) | 2019 | The Impact of Medicaid Expansion on Postpartum Health Care Utilization Among Pregnant Women With Opioid Use Disorder | Postpartum health care utilization | Non-Latinx Black women were more likely to receive postpartum health care within 300 d of delivery than non-Latinx White women. | Authors did not discuss outcomes related to race and ethnicity in discussion. |
| Schiff et al (38) | 2018 | Examination of Hospital, Maternal, and Infant Characteristics Associated With Breastfeeding Initiation and Continuation Among Opioid-Exposed Maternal-Infant Dyads | Breastfeeding initiation, continuation, exclusivity | Maternal White race negatively associated with breastfeeding initiation in unadjusted model but did not retain significance in adjusted models | Outcomes associated with race mentioned in the discussion. |
| Multiple outcome categories | |||||
| Lo-Ciganic et al (40) | 2019 | Adherence Trajectories of Buprenorphine Therapy Among Pregnant Women in a Large State Medicaid Program in the United States | Buprenorphine treatment adherence | Non-White race significant predictor of early discontinuation among early treatment responders in multivariable, multinomial logistic regression. | Authors concluded on the basis of the study findings that “factors were identified that could be used to target patients at high risk of late initiation or early buprenorphine discontinuation including…racial/ethnic minority groups.” |
| Peeler et al (20) | 2020 | Racial and Ethnic Disparities in Maternal and Infant Outcomes Among Opioid-Exposed Mother-Infant Dyads in Massachusetts (2017-2019) | Receipt of MOUD and early intervention referral, biological parental custody at discharge | Non-Hispanic Black women and Hispanic women were less likely to receive MOUD during pregnancy compared with non-Hispanic White women. | Authors attributed inequities in MOUD receipt by race and ethnicity to “socioeconomic differences, a lack of physicians trained to prescribe buprenorphine in communities of color, fear and stigma around the use of methadone and buprenorphine, and bias, discrimination, and racism within the substance use treatment system.” |
Mention and Interpretation of Race/Ethnicity in Discussion
Seventeen (11.2%) articles mentioned race/ethnicity in the discussion section, with a larger percentage of articles assessing postpartum maternal (20%) or multiple outcome categories (21.4%) compared with those that focused on prenatal/obstetric (8.7%) or infant outcomes (9%) (Fig 1). Eight of the studies that included race/ethnicity in the discussion merely noted that their samples were a homogenous, mostly White study population.36,41–47 Lawlor et al45 (2020) and Lopian et al44 (2019) discussed potential benefits of studies in primarily White populations, with Lawlor et al noting that the homogeneity decreased potential confounding in outcomes and Lopian et al stating that their primarily White study population reflected the general demographics of the opioid epidemic.
Two of the studies that mention race/ethnicity in the discussion, Lo-Ciganic et al40 (2019) and Schiff et al38 (2018), restated their findings with regard to race/ethnicity but did not further elaborate on these results, discuss potentially explanatory factors, or consider future research. Parikh et al21 (2019) hypothesized that the differences they found regarding need for pharmacologic treatment among infants may be due to biological differences in different groups experiencing withdrawal. Finally, Schiff et al9 (2020) and Peeler et al20 (2020) mentioned structural factors, including individual and institutional racism, that could be contributing to differences seen in MOUD.
Qualitative Studies
We identified 17 studies that used qualitative methodologies to analyze either focus group results or individual interviews with parent-infant dyads affected by OUD. Seven studies focused on the newborn hospitalization and maternal views on breastfeeding or rooming-in care, 5 focused on access to and experiences with substance use treatment and prenatal care, and 4 focused on parenting experiences and concerns, including experiences with child welfare systems and fetal loss. Among these 17 qualitative reports, 15 listed the racial/ethnic breakdown of participants, and 5 identified their predominately White non-Latinx samples as a limitation. Two studies note a majority or entirely Latinx study population. One of these, Cleveland et al49 (2016), described the lack of ethnic diversity in their entirely Latinx population as a limitation. None of the qualitative studies addressed the role that race or racism may have had on the themes that emerged from their analyses or describe probes used in focus groups or individual interviews to uncover factors potentially related to race or racism.
Discussion
Main Findings
In a scoping review of >2000 studies in the medical literature describing maternal and infant outcomes among dyads affected by OUD over 2 decades, only a few of the more than 150 included studies were designed to investigate how outcomes may differ by race/ethnicity. Furthermore, no studies specifically defined race as a social construct, not all studies presented race/ethnicity data, fewer than half assessed whether race/ethnicity could be a confounder in their analyses, less than fifteen percent adjusted for race/ethnicity in their multivariable models, less than ten percent stratified their outcome data by racial/ethnic group, and only two studies considered structural factors such as racism as a potential explanation for identified differences. An important, albeit insufficient, first step in being able to address inequities in outcomes requires researchers to accurately categorize and assess race/ethnicity in their studies; we found that this was addressed in the minority of studies, particularly those with a focus on infant outcomes.50 Most notably, none of these studies set out to understand the role that racism may play on the causal pathway toward increased substance use and worse perinatal outcomes, despite a growth in this literature in other areas of health.51
We found that a high proportion of the published literature studied a population that was either majority or entirely White. Although some authors acknowledged the lack of racial/ethnic diversity in their study population as a limitation, others viewed a more homogenous population as a strength. National prevalence data found that 77% of cases of OUD and 78% of opioid-related deaths occurred among non-Latinx White individuals in 2017,52 with non-Latinx Black individuals experiencing the greatest rise in overdose rate between 2015 and 2017.4,53 Despite the higher occurrence of OUD and NOWS among White and American Indian/Alaska Native populations,1,52,54 the overrepresentation of White participants in the studies included in our review was beyond the expected differences in the demographics of OUD and overdose prevalence among different racial groups. The way in which research participants are recruited and data are collected may reflect a long history of biomedical research that excluded marginalized groups from research and/or resulted in harm to groups of Black, Indigenous, and people of color (BIPOC) without proper consent for research.55 The challenges of recruiting a diverse sample are real, but the historic impact of scientific racism can be overcome with careful attention to trust and accurate information about the goals of research. Furthermore, prioritizing the diversity of participants included in research studies is necessary for research results to be of benefit to the whole population.56 To successfully bring communities affected by OUD and those with lived experience into the research process, diverse participants should be included in all stages of research, from project development and study design all the way to dissemination of results, to ensure diverse views throughout.57
With respect to the type of outcomes studied, the majority of studies included in our review focused on neonatal or infant outcomes, yet they were the least likely to include or analyze information about race/ethnicity in their study. We hypothesize that several factors could be contributing to this finding. First, infant race is often poorly described in birth records and may be incorrectly assigned on the basis of maternal race only.58 Second, the most commonly cited studies looking at NOWS prevalence over the past decade did not report infant race/ethnicity in their publications.59–61 Without national prevalence data documenting this variable, researchers may have been more likely to omit it themselves. However, given the significant racial/ethnic inequities that exist in other domains of child health,62,63 including in newborn and neonatal outcomes, we cannot fully explain through these hypotheses the omission of race/ethnicity characteristics.
When assessing differences in infant outcomes, we identified 3 studies that showed a lower rate of pharmacologic treatment of Black infants, with only 1 study’s findings persisting in adjusted models and 1 study finding no difference.20,21,37 Parikh et al21 concluded that these differences may be due to biological differences between races. Grossman et al64 and Clark and French15 critiqued this interpretation and highlighted how racial biases can affect a seemingly objective assessment of neonatal withdrawal. Similar to studies of both Black children and adults where inequities in pain management have been described,65,66 the findings of Parikh et al may actually reflect the variability in the scoring tool used, showing how symptoms of pain and discomfort could be assessed unequally by health care providers caring for Black infants because of conscious or implicit biases. Particularly, because the findings of a decreased need for pharmacologic treatment in non-White infants were not replicated in the adjusted models by Peeler et al20 and Scott et al,37 this study highlights the harms of using race as a proxy for risk factors, suggesting that although reporting race/ethnicity to document the health status of a population can be helpful, use of the social category of race or ethnicity to “produce biological attribution of causes” is dangerous.67,68 Furthermore, use of race in analyses as a measure of inherent risk results in an overfocus on risks in certain groups. Instead, we suggest that referring to race as a proxy for racism shifts the focus to potential points of intervention to promote health equity. In this review, we aimed to highlight the importance of assessing differences by race/ethnicity as a means to develop strategies to achieve equitable outcomes by groups, with the clear understanding that race is a social construct and is best used as a proxy for structural racism.
With respect to maternal treatment outcomes, we identified the presence of inequitable medication treatment receipt for pregnant people with OUD across multiple different studies, postpartum birth control receipt, and postpartum care utilization.9,20,40 None of the qualitative studies we identified that assessed barriers to prenatal and postpartum care highlighted the potential for participants’ race/ethnicity to affect care for BIPOC individuals. Qualitative research is well suited to explore the experiences of BIPOC individuals with OUD across the perinatal continuum, and future studies should prioritize the voices of BIPOC individuals to begin to address the root causes of medication treatment inequities. Furthermore, there is a need to identify factors contributing to both interpersonal racism and structural racism resulting in barriers to treatment receipt. Multidisciplinary collaboratives that bring together clinical, community, and public health stakeholders may be useful to examine barriers within health care, substance use treatment, and child welfare systems.69
Ghidei et al14 propose a framework for advancing inequities research in the field of perinatal health. They argue that although identification of inequities is important, equally important is the recognition that when “we study racial and ethnic disparities, race and ethnicity are so often mishandled, misreported, underreported, or wholly unreported.” Our scoping review highlighted an area of perinatal research that can benefit from a reckoning with how poorly race data have been incorporated to date. McLemore et al70 further highlight important suggestions when making decisions about race in research. First, investigators should include affected communities in exploring how race affects their lives. Second, community-based participatory methods, public health critical race praxis, and a reproductive justice framework can help facilitate a research process that is able to more deeply understand BIPOC individuals’ lives.71–74 Finally, when including race data, researchers must emphasize the role of racism, rather than race, as a risk factor for poor perinatal outcomes.75 Multidisciplinary teams of clinicians, perinatal quality collaboratives, policymakers, critical race scholars, and public health practitioners have an opportunity to work collectively to address racism by incorporating a more intentional approach to research, including race/ethnicity and the interpretation of its findings.
Limitations
There are important limitations to this research. First, by narrowly focusing on OUD and not including other SUDs, we acknowledge that this review contributes to the problem of prioritizing the impact of opioids, which have affected a majority White population. The response to the opioid epidemic, which has emphasized a national public health response,76 contrasts starkly with the response to the crack/cocaine epidemic in the 1980s, which tended to affect communities of color at a higher rate77 and was met with punitive carceral and child welfare responses.78 It will be important for future researchers to assess racial/ethnic inequities across the perinatal continuum for all types of SUDs. Second, as we highlighted, race/ethnicity data often are not collected in a systematic way; for example, data items that are assigned at hospital registration rather than self-reported can bias outcomes.70,79 Third, this review was limited to the current opioid epidemic in the United States, and thus, findings may not be generalizable to other countries with different historical and cultural contexts. Fourth, although our analysis prioritized race/ethnicity, other structural determinants of health, including socioeconomic status, education, immigration status, and health literacy, may not just be confounding factors affecting dyadic outcomes but actually factors that themselves are a result of structural racism. Future quantitative analysis could be strengthened by using a decomposition method to adjust for confounding effects of other factors while acknowledging their association with race and racism to better identify causal pathways between racism and inequitable health outcomes.80 Finally, we grouped race and ethnicity given that they were often linked together in the studies we assessed, but these are distinct factors, and the unique role of ethnicity is an important area for future study. A further appreciation of intersectionality demands attention to differences within arbitrary categories, such as geography, culture, history, and lived experience, to help prevent overgeneralization and inaccuracy in interpretation of results.
Conclusions
In this scoping review, assessing 2 decades of perinatal OUD research utilizing the Public Health Critical Race Framework, we highlight a field of perinatal research that will benefit greatly from further attention to how researchers consider including, reporting, and using race/ethnicity data. To achieve equity, a greater emphasis on marginalized populations, regardless of the demographics of individuals with OUD, should be prioritized. As our country and medical and public health communities increasingly grapple with the impact of structural racism on health, there is an opportunity for perinatal OUD researchers to incorporate community-based participatory methods, public health critical race praxis, and a reproductive justice framework to help facilitate a research process that is able to more deeply understand BIPOC individuals’ experiences and to address treatment inequities.
Supplementary Material
Acknowledgments
We thank Catherine Reyes, MD, for assistance with shaping the study design and the future directions of this project and Lisa Liang Philpotts, BSN, MSLS, for expertise in creating the literature search for this review.
Glossary
- BIPOC
Black, indigenous, and people of color
- MOUD
medication to treat opioid use disorder
- NAS
neonatal abstinence syndrome
- NOWS
neonatal opioid withdrawal syndrome
- OUD
opioid use disorder
- PHCRF
Public Health Critical Race Framework
- SUD
substance use disorder
Footnotes
Dr Schiff conceptualized and designed the study, designed the data extraction instruments, developed the search strategy, drafted the initial manuscript, and reviewed and revised the manuscript; Ms Work designed the data extraction instruments, executed the search strategy, performed quantitative analyses and developed figures, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Hoeppner reviewed the statistical analyses, analyzed the data, and critically reviewed and revised all drafts of the manuscript; Dr Foley executed the search strategy, drafted the initial manuscript, and reviewed and revised the manuscript; Ms Applewhite executed the search strategy and assisted in study design, developing the search strategy, analyzing the data, and critically reviewing and revising all drafts of the manuscript; Drs Diop, Gupta, Peacock-Chambers, Vilsaint, Bernstein, and Bryant and Ms Goullaud assisted in the study design, developing the search strategy, analyzing the data, and critically reviewing and revising all drafts of the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: Funding from the National Institute on Drug Abuse (K23DA048169) was used to support this study through the primary author. Funded in part through a contract between the Massachusetts Health Policy Commission and the Neonatal Quality Improvement Collaborative of Massachusetts, with funding from a Substance Abuse and Mental Health Services Administration grant to the Massachusetts Department of Public Health, Bureau of Substance Addiction Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders. Funded by the National Institutes of Health (NIH).
In perinatal OUD research, race/ethnicity was underreported, few studies evaluated racial/ethnic differences, and no studies investigated the role of structural racism on health inequities.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2021-054961.
References
- 1. Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA. 2021;325(2):146–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Center for Substance Abuse Treatment . Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs. Treatment Improvement Protocol (TIP) Series 43. DHHS Publication No. (SMA) 05-4048. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005 [PubMed] [Google Scholar]
- 3. Mangla K, Hoffman MC, Trumpff C, O’Grady S, Monk C. Maternal self-harm deaths: an unrecognized and preventable outcome. Am J Obstet Gynecol. 2019;221(4):295–303 [DOI] [PubMed] [Google Scholar]
- 4. Petersen EE, Davis NL, Goodman D, et al. Racial/ethnic disparities in pregnancy-related deaths – United States, 2007-2016. MMWR Morb Mortal Wkly Rep. 2019;68(35):762–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ely DM, Driscoll AK. Infant Mortality in the United States, 2012: Data From the Period Linked Birth/Infant Death File (Report No. 10). Hyattsville, MD: Centers for Disease Control and Prevention; 2019 [PubMed] [Google Scholar]
- 6. Hansen HB, Siegel CE, Case BG, Bertollo DN, DiRocco D, Galanter M. Variation in use of buprenorphine and methadone treatment by racial, ethnic, and income characteristics of residential social areas in New York City. J Behav Health Serv Res. 2013;40(3):367–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76(9):979–981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hadland SE, Bagley SM, Rodean J, et al. Receipt of timely addiction treatment and association of early medication treatment with retention in care among youths with opioid use disorder. JAMA Pediatr. 2018;172(11):1029–1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schiff DM, Nielsen T, Hoeppner BB, et al. Assessment of racial and ethnic disparities in the use of medication to treat opioid use disorder among pregnant women in Massachusetts. JAMA Netw Open. 2020;3(5):e205734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schiff DM, Nielsen TC, Hoeppner BB, et al. Methadone and buprenorphine discontinuation among postpartum women with opioid use disorder. Am J Obstet Gynecol. 2021;225(4): 424.e1–424.e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goedel WC, Shapiro A, Cerdá M, Tsai JW, Hadland SE, Marshall BDL. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4):e203711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Crear-Perry J, Correa-de-Araujo R, Lewis Johnson T, McLemore MR, Neilson E, Wallace M. Social and Structural Determinants of Health Inequities in Maternal Health. J Womens Health (Larchmt). 2021;30(2):230–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kunins HV. Structural racism and the opioid overdose epidemic: the need for antiracist public health practice. J Public Health Manag Pract. 2020; 26(3):201–205 [DOI] [PubMed] [Google Scholar]
- 14. Ghidei L, Murray A, Singer J. Race, research, and women’s health: best practice guidelines for investigators. Obstet Gynecol. 2019;133(4):815–818 [DOI] [PubMed] [Google Scholar]
- 15. Clark RRS, French R. Conflating race and genetics among newborns with neonatal abstinence syndrome [published online ahead of print on October 4, 2021]. JAMA Pediatr. doi:https://doi.org/10.1001/jamapediatrics.2021. 3591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Krieger N, Boyd RW, De Maio F, Maybank M. Medicine’s privileged gatekeeps: producing harmful ignorance about racism and health. Health Affairs Blog. Available at: www.healthaffairs.org/do/10.1377/hblog20210415.305480/full
- 17. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(suppl 1):S30–S35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Doll KM, Snyder CR, Ford CL. Endometrial cancer disparities: a race-conscious critique of the literature. Am J Obstet Gynecol. 2018;218(5):474–482.e2 [DOI] [PubMed] [Google Scholar]
- 20. Peeler M, Gupta M, Melvin P, et al. Racial and ethnic disparities in maternal and infant outcomes among opioid-exposed mother-infant dyads in Massachusetts (2017-2019). Am J Public Health. 2020;110(12):1828–1836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Parikh A, Gopalakrishnan M, Azeem A, Booth A, El-Metwally D. Racial association and pharmacotherapy in neonatal opioid withdrawal syndrome. J Perinatol. 2019;39(10):1370–1376 [DOI] [PubMed] [Google Scholar]
- 22. Bell J, Towers CV, Hennessy MD, Heitzman C, Smith B, Chattin K. Detoxification from opiate drugs during pregnancy. Am J Obstet Gynecol. 2016;215(3):374.e1–374.e6 [DOI] [PubMed] [Google Scholar]
- 23. Garrison L, Leeman L, Savich RD, Gutierrez H, Rayburn WF, Bakhireva LN. Fetal growth outcomes in a cohort of polydrug- and opioid-dependent patients. J Reprod Med. 2016;61(7–8):311–319 [PMC free article] [PubMed] [Google Scholar]
- 24. Goodman D, Zagaria AB, Flanagan V, et al. Feasibility and acceptability of a checklist and learning collaborative to promote quality and safety in the perinatal care of women with opioid use disorders. J Midwifery Womens Health. 2019;64(1):104–111 [DOI] [PubMed] [Google Scholar]
- 25. Jancaitis B, Kelpin S, Masho S, May J, Haug NA, Svikis D. Factors associated with treatment retention in pregnant women with opioid use disorders prescribed methadone or electing non-pharmacological treatment. Women Health. 2020;60(1):1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jansson LM, Di Pietro JA, Elko A, Williams EL, Milio L, Velez M. Pregnancies exposed to methadone, methadone and other illicit substances, and poly-drugs without methadone: a comparison of fetal neurobehaviors and infant outcomes. Drug Alcohol Depend. 2012;122(3):213–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Almario CV, Seligman NS, Dysart KC, Berghella V, Baxter JK. Risk factors for preterm birth among opiate-addicted gravid women in a methadone treatment program. Am J Obstet Gynecol. 2009;201(3):326.e1–326.e6 [DOI] [PubMed] [Google Scholar]
- 28. Benningfield MM, Dietrich MS, Jones HE, et al. Opioid dependence during pregnancy: relationships of anxiety and depression symptoms to treatment outcomes. Addiction. 2012;107(suppl 1):74–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brogly SB, Hernández-Diaz S, Regan E, Fadli E, Hahn KA, Werler MM. Neonatal outcomes in a Medicaid population with opioid dependence. Am J Epidemiol. 2018;187(6):1153–1161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guille C, Simpson AN, Douglas E, et al. Treatment of opioid use disorder in pregnant women via telemedicine: a nonrandomized controlled trial. JAMA Netw Open. 2020;3(1):e1920177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Holbrook AM, Jones HE, Heil SH, et al. Induction of pregnant women onto opioid-agonist maintenance medication: an analysis of withdrawal symptoms and study retention. Drug Alcohol Depend. 2013;132(1-2):329–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Huybrechts KF, Bateman BT, Desai RJ, et al. Risk of neonatal drug withdrawal after intrauterine co-exposure to opioids and psychotropic medications: cohort study. BMJ. 2017;358:j3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lemon LS, Caritis SN, Venkataramanan R, Platt RW, Bodnar LM. Methadone versus buprenorphine for opioid use dependence and risk of neonatal abstinence syndrome. Epidemiology. 2018;29(2):261–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lemon LS, Naimi A, Caritis SN, Platt RW, Venkataramanan R, Bodnar LM. The role of preterm birth in the association between opioid maintenance therapy and neonatal abstinence syndrome. Paediatr Perinat Epidemiol. 2018;32(2):213–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Patton BP, Krans EE, Kim JY, Jarlenski M. The impact of Medicaid expansion on postpartum health care utilization among pregnant women with opioid use disorder. Subst Abus. 2019;40(3):371–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Short VL, Gannon M, Abatemarco DJ. The association between breastfeeding and length of hospital stay among infants diagnosed with neonatal abstinence syndrome: a population-based study of in-hospital births. Breastfeed Med. 2016;11(7):343–349 [DOI] [PubMed] [Google Scholar]
- 37. Scott LF, Guilfoy V, Duwve JM, Rawl SM. Factors associated with the need for pharmacological management of neonatal opioid withdrawal syndrome. Adv Neonatal Care. 2020;20(5):364–373 [DOI] [PubMed] [Google Scholar]
- 38. Schiff DM, Wachman EM, Philipp B, et al. Examination of hospital, maternal, and infant characteristics associated with breastfeeding initiation and continuation among opioid-exposed mother-infant dyads. Breastfeed Med. 2018;13(4):266–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Krans EE, Kim JY, James AE III, Kelley DK, Jarlenski M. Postpartum contraceptive use and interpregnancy interval among women with opioid use disorder. Drug Alcohol Depend. 2018;185:207–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lo-Ciganic WH, Donohue JM, Kim JY, et al. Adherence trajectories of buprenorphine therapy among pregnant women in a large state Medicaid program in the United States. Pharmacoepidemiol Drug Saf. 2019;28(1):80–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wilder C, Lewis D, Winhusen T. Medication assisted treatment discontinuation in pregnant and postpartum women with opioid use disorder. Drug Alcohol Depend. 2015;149:225–231 [DOI] [PubMed] [Google Scholar]
- 42. O’Connor AB, Uhler B, O’Brien LM, Knuppel K. Predictors of treatment retention in postpartum women prescribed buprenorphine during pregnancy. J Subst Abuse Treat. 2018;86:26–29 [DOI] [PubMed] [Google Scholar]
- 43. Nguyen L, Lander LR, O’Grady KE, et al. Treating women with opioid use disorder during pregnancy in Appalachia: Initial neonatal outcomes following buprenorphine + naloxone exposure. Am J Addict. 2018;27(2):92–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lopian KM, Chebolu E, Kulak JA, Kahn LS, Blondell RD. A retrospective analysis of treatment and retention outcomes of pregnant and/or parenting women with opioid use disorder. J Subst Abuse Treat. 2019;97:1–6 [DOI] [PubMed] [Google Scholar]
- 45. Lawlor ML, Shook LA, McQuerry K, et al. Care-by-parent model as a tool for reduction of neonatal opioid withdrawal syndrome in neonates exposed to buprenorphine maintenance therapy in-utero. J Matern Fetal Neonatal Med. 2020;33(16):2718–2722 [DOI] [PubMed] [Google Scholar]
- 46. Krans EE, Bobby S, England M, et al. The Pregnancy Recovery Center: A women-centered treatment program for pregnant and postpartum women with opioid use disorder. Addict Behav. 2018;86:124–129 [DOI] [PubMed] [Google Scholar]
- 47. Gopalan P, Moses-Kolko E, Valpey R, Shenai N, Smith E. Benzodiazepine withdrawal in pregnant women with opioid use disorders: an observational study of current clinical practices at a tertiary obstetrical hospital. Gen Hosp Psychiatry. 2019;57:29–33 [DOI] [PubMed] [Google Scholar]
- 48. McGlothen KS, Cleveland LM, Gill SL. “I’m doing the best that I can for her”: infant-feeding decisions of mothers receiving medication-assisted treatment for an opioid use disorder. J Hum Lact. 2018;34(3):535–542 [DOI] [PubMed] [Google Scholar]
- 49. Cleveland LM, Bonugli RJ, McGlothen KS. The mothering experiences of women with substance use disorders. ANS Adv Nurs Sci. 2016;39(2):119–129 [DOI] [PubMed] [Google Scholar]
- 50. Howell EA, Brown H, Brumley J, et al. Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle. Obstet Gynecol. 2018;131(5):770–782 [DOI] [PubMed] [Google Scholar]
- 51. Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Orgera K, Tolbert J. The opioid epidemic and Medicaid’s role in facilitating access to treatment. Kaiser Family Foundation; 2019. Available at: www.kff.org/medicaid/issue-brief/the-opioid- epidemic-and-medicaids-role-in- facilitating-access-to-treatment
- 53. Substance Abuse and Mental Health Services Administration . The Opioid Crisis and the Black/African American Population: An Urgent Issue. Publication No. PEP20-05-02-001. Rockville, MD: Office of Behavioral Health Equity; 2020 [Google Scholar]
- 54. Centers for Disease Control and Prevention . Wide-Ranging Online Data for Epidemiologic Research (WONDER). Atlanta, GA: National Center for Health Statistics; 2016 [Google Scholar]
- 55. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463 [DOI] [PubMed] [Google Scholar]
- 56. NIH Central Resource for Grant and Funding Information . Inclusion of women and minorities as participants in research involving human subjects, 2019. Available at: grants.nih.gov/policy/inclusion/women-and-minorities.htm
- 57. Cacari-Stone L, Wallerstein N, Garcia AP, Minkler M. The promise of community-based participatory research for health equity: a conceptual model for bridging evidence with policy. Am J Public Health. 2014;104(9):1615–1623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Mason LR, Nam Y, Kim Y. Validity of infant race/ethnicity from birth certificates in the context of U.S. demographic change. Health Serv Res. 2014;49(1):249–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307(18):1934–1940 [DOI] [PubMed] [Google Scholar]
- 60. Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW. Incidence and costs of neonatal abstinence syndrome among infants with Medicaid: 2004-2014. Pediatrics. 2018;141(4):e20173520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ko JY, Patrick SW, Tong VT, Patel R, Lind JN, Barfield WD. Incidence of neonatal abstinence syndrome - 28 states, 1999-2013. MMWR Morb Mortal Wkly Rep. 2016;65(31):799–802 [DOI] [PubMed] [Google Scholar]
- 62. Sigurdson K, Mitchell B, Liu J, et al. Racial/ethnic disparities in neonatal intensive care: a systematic review. Pediatrics. 2019;144(2):e20183114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Greenwood BN, Hardeman RR, Huang L, Sojourner A. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci U S A. 2020;117(35):21194–21200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Grossman MR, Berkwitt AK, Osborn RR. Racial association and pharmacotherapy in neonatal opioid withdrawal syndrome: thinking beyond genetics. J Perinatol. 2020;40(4):689–690 [DOI] [PubMed] [Google Scholar]
- 65. Goyal MK, Johnson TJ, Chamberlain JM, et al. ; Pediatric Emergency Care Applied Research Network (PECARN) . Racial and ethnic differences in emergency department pain management of children with fractures. Pediatrics. 2020;145(5):e20193370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr. 2015;169(11):996–1002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Braun L, Fausto-Sterling A, Fullwiley D, et al. Racial categories in medical practice: how useful are they? PLoS Med. 2007;4(9):e271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Helms JE, Jernigan M, Mascher J. The meaning of race in psychology and how to change it: a methodological perspective. Am Psychol. 2005;60(1):27–36 [DOI] [PubMed] [Google Scholar]
- 69. Nordstrom BR, Saunders EC, McLeman B, et al. Using a learning collaborative strategy with office-based practices to increase access and improve quality of care for patients with opioid use disorders. J Addict Med. 2016;10(2):117–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. McLemore MR, Asiodu I, Crear-Perry J, et al. Race, research, and women’s health: best practice guidelines for investigators. Obstet Gynecol. 2019;134(2):422–423 [DOI] [PubMed] [Google Scholar]
- 71. Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71(8):1390–1398 [DOI] [PubMed] [Google Scholar]
- 72. Franck LS, McLemore MR, Cooper N, et al. A novel method for involving women of color at high risk for preterm birth in research priority setting. J Vis Exp. 2018;(131):56220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Taylor J, Novoa C, Hamm K, Phadke S. Eliminating Racial Disparities in Maternal and Infant Mortality. Washington, DC: Center for American Progress; 2019 [Google Scholar]
- 74. Sister Song . Reproductive justice. Available at: www.sistersong.net/reproductive-justice
- 75. Hardeman RR, Murphy KA, Karbeah J, Kozhimannil KB. Naming institutionalized racism in the public health literature: a systematic literature review. Public Health Rep. 2018;133(3):240–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Comprehensive Addiction and Recovery Act of 2016. Pub. L. No. 114-198 130 Stat 695.
- 77. Shiels MS, Freedman ND, Thomas D, Berrington de Gonzalez A. Trends in U.S. drug overdose deaths in non- Hispanic Black, Hispanic, and non- Hispanic white persons, 2000-2015. Ann Intern Med. 2018;168(6):453–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Substance Abuse and Mental Health Services Administration . Results From the 2018 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Center for Behavioral Health Statistics and Quality; 2019 [Google Scholar]
- 79. Boehmer U, Kressin NR, Berlowitz DR, Christiansen CL, Kazis LE, Jones JA. Self-reported vs administrative race/ethnicity data and study results. Am J Public Health. 2002;92(9):1471–1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Jackson JW, VanderWeele TJ. Decomposition analysis to identify intervention targets for reducing disparities. Epidemiology. 2018; 29(6):825–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.