Abstract
We used the cottontail rabbit papillomavirus (CRPV) New Zealand White rabbit model to test a combination treatment of large established papillomas with intralesional cidofovir and DNA vaccination to cure sites and reduce recurrences. Intralesional 1% (wt/vol) (0.036 M) cidofovir treatment of rabbit papillomas led to elimination, or “cure,” of the papillomas over a 6- to 8-week treatment period (N. D. Christenson, M. D. Pickel, L. R. Budgeon, and J. W. Kreider, Antivir. Res. 48:131–142, 2000). However, recurrences at periods from 1 to 8 weeks after treatment cessation were observed at approximately 50% of cured sites. DNA vaccinations with CRPV E1, E2, E6, and E7 were initiated either after or at the time of intralesional treatments, and the recurrence rates were observed. When DNA vaccinations were started after intralesional cures, recurrence rates were similar to those of vector-vaccinated rabbits. A small proportion of recurrent sites subsequently regressed (4 out of 10, or 40%) in the vaccinated group versus no regression of recurrences in the vector-immunized group (0 out of 19, or 0%), indicating partial effectiveness. In contrast, when DNA vaccinations were conducted during intralesional treatments, a significant reduction of recurrences (from 10 out of 19, or 53%, of sites in vector-immunized rabbits to 3 out of 20, or 15%, of sites in viral-DNA-immunized rabbits) was observed. DNA vaccination without intralesional treatments had a minimal effect on preexisting papillomas. These data indicated that treatment with a combination of antiviral compounds and specific immune stimulation may lead to long-term cures of lesions without the ensuing problem of papilloma recurrence.
Treatment of persistent papillomas with intralesional and topical antiviral compounds and immunomodulators often leads to effective cure of treated lesions in clinical trials with human papillomavirus (HPV) disease (4, 5, 16, 56). However, recurrences are common after treatment cessation (5, 6, 16, 20, 56). The reasons for clinical recurrences are unclear, but possible mechanisms include (i) reinfection at adjacent sites, (ii) incomplete destruction of the entire area of active clinical disease, (iii) reactivation of subclinical HPV disease in wounded areas within and adjacent to treated sites, (iv) incomplete activation or induced anergy of antigen-specific cell-mediated immunity to HPV-infected papilloma cells, and (v) genetic factors associated with ineffective host immunity together with antigenic differences between variants of the same HPV type (2, 3, 9, 23, 31, 46, 47, 58).
There is strong evidence that host immunity to papillomavirus antigens can clear the bulk of HPV and animal papillomavirus infections (reviewed in references 22 and 39). Spontaneous regression of papillomas induced by cottontail rabbit papillomavirus (CRPV), rabbit oral papillomavirus, bovine papillomavirus type 4, and canine oral papillomavirus in rabbits, cattle, and beagles have been observed (8, 10, 12, 34, 38, 41). The regressions are associated with a heavy infiltrate of T cells of both CD4 and CD8 phenotypes (1, 33, 40), and regressions of all lesions occur systemically. Immunosuppression of animals during the periods of papilloma growth has been shown to prolong lesion persistence (29, 37, 48). HPV-infected lesion regression with an associated immune infiltrate and in situ detectable cytokines has been reported also (17, 57). The precise effector mechanisms leading to lesion destruction in these clinical infections, however, are unknown. Additional evidence for immune control of HPV infections includes the high incidence of active HPV disease in immunosuppressed patients (18, 19, 32, 35, 54).
Despite the strong evidence of multiple mechanisms of B-cell and T-cell immunity to papillomavirus antigens in hosts with papillomavirus infections (reviewed in references 22 and 39), persistent infections are common. Cervical cancer associated with HPV accounts for over 250,000 deaths of women worldwide (42). Thus, the bulk of persistent infections occurs in patients who are considered, in general, to be immunocompetent. Given this observation that persistent HPV infections can occur in immunocompetent individuals, it is clear that the viral immunity that develops during infection is often inadequate to clear clinical disease. Animal studies demonstrate clearly that protective cell-mediated immunity can be developed in individuals who would otherwise present with persistent disease upon infection (26, 30, 49, 52). These data suggest that induced immunity may deal effectively with residual disease and/or subclinical papillomavirus infections rather than with large clinically active lesions. A strategy that combines antiviral treatments to reduce clinical disease load with specific immune stimulations, therefore, represents a logical approach to the treatment of persistent HPV infections.
The goal of this study was to combine aspects of intralesional antiviral treatment of papillomas with immune activation to provide a long-lasting cure of persistent papillomavirus infections. We have used the CRPV rabbit system as a model for papilloma recurrence after lesion “cure” with intralesional cidofovir (15). Cidofovir was chosen as one of several compounds that could ablate CRPV-induced rabbit papillomas following intralesional or topical treatments (15). Recurrence rates from cured sites reached 50%, which is similar to rates of clinically treated HPV disease (5, 6, 16, 20, 56). The strategy was to cure large established papillomas by intralesional cidofovir and to include DNA vaccinations with CRPV viral genes to prevent recurrences. The data indicate that concurrent cidofovir treatment and DNA vaccinations lead to long-term cure of papillomas with a marked reduction in the incidence of recurrences.
MATERIALS AND METHODS
Viral infections.
Outbred New Zealand White rabbits of both sexes were purchased from Covance Research Products, Inc. (Denver, Pa.) and maintained in the animal facility of the Pennsylvania State University College of Medicine. All animal care and handling procedures were approved by the Institutional Animal Care and Use Committee of the Pennsylvania State University. Infection of rabbits with CRPV was conducted as previously described (13, 34). In brief, rabbits were lightly anesthetized with a mixture of ketamine-HCl (40 mg/kg of body weight) and xylazine (5 mg/kg), and their backs were shaved with electric clippers. Four 1- by 1-cm scarified sites on the back of each rabbit were produced by abrasion with a scalpel. Each scarified site received 50 μl of papilloma extract applied directly to the wound. The two anterior papillomas on each side of the mid-dorsum were induced with a 10−1 dilution of CRPV extract, whereas the two posterior papillomas were induced with a dilution of 10−2. Papillomas were allowed to develop without antiviral treatments for either 35 or 45 days after infection. All papillomas were measured weekly in three dimensions (length by width by height, in millimeters) beginning at 3 weeks after infection, and the geometric mean diameter (GMD) (in millimeters) was calculated.
Intralesional treatments with cidofovir.
Cidofovir (HPMPC) was obtained from Gilead Sciences, Foster City, Calif., in aqueous solution. A 1% (wt/vol) (0.036 M) cidofovir solution in saline was prepared for treatments. Two combination experiments with several treatment groups per experiment were conducted to assess therapeutic outcome, and a summary of the experimental designs is shown in Table 1. Each treatment group contained five rabbits per group, with four papillomas per rabbit. Intralesional delivery consisted of direct injection of a total of 100 μl of 1% (wt/vol) cidofovir per treatment into the base of each papilloma in two or three places, independent of papilloma size. Intralesional treatments were given three times per week for 7 to 8 weeks until most sites were cured. At this time point, cidofovir treatments were stopped but monitoring of all sites on a weekly basis was continued.
TABLE 1.
Design of experiments for combination treatments with intralesional cidofovir and DNA vaccinations
| Test group | Intralesional cidofovir | DNA vaccination(s) |
|---|---|---|
| Expt no. 1 | ||
| Group A | None | None |
| Group B | None | CRPV E1 + E2 + E6 (days 83, 120, 155) |
| Group C | 2 sites treated, from day 35 to 80 | CRPV E1 + E2 + E6 (day 120) |
| Group D | 2 sites treated, from day 35 to 80 | Vector alone (day 120) |
| Group E | 4 sites treated, from day 35 to 80 | CRPV E1 + E2 + E6 (days 83, 120, 155) |
| Group F | 4 sites treated, from day 35 to 80 | Vector alone (days 83, 120, 155) |
| Expt no. 2 | ||
| Group A | 4 sites treated, from day 45 to 100 | Vector alone (days 21, 35, 50, 120) |
| Group B | 4 sites treated, from day 45 to 100 | CRPV E1 + E2 (days 21, 35, 50, 120) |
| Group C | 4 sites treated, from day 45 to 100 | CRPV E6 + E7 (days 21, 35, 50, 120) |
| Group D | 4 sites treated, from day 45 to 100 | CRPV E1 + E2 + E6 + E7 (days 21, 35, 50, 120) |
DNA vaccinations.
DNA vaccinations were delivered intracutaneously by gene-gun-mediated particle bombardment as previously described (25). DNA expression constructs separately containing CRPV E1, E2, E6, and E7 and vector alone were delivered to shaved, depilated back skin and to the hairless skin of the inner ears. The expression constructs were prepared using the V1jns vector, which utilizes a cytomegalovirus promoter as previously described (25). All rabbits were anesthetized, and ears were temporarily plugged with cotton wool prior to gene gun vaccinations. Vaccinations consisted of approximately 10 μg of DNA per construct per treatment. In the first experiment, DNA vaccinations with E1, E2, and E6 were given on days 83, 120, and 155. E7 vaccination was not included with E1, E2, and E6 in this experiment because we had observed previously that E7 vaccination alone provided no protection against CRPV infection (25). In the second experiment, DNA vaccinations with E1, E2, E6, and E7 in several different combinations were given on days 21, 35, 50 and 120 (Table 1). The viral antigens chosen were based on our previous studies showing that combinations of E proteins provided the maximum protection prior to virus challenge (25, 27). The rationale for initiating vaccinations at an earlier time point in the second experiment was based on the data obtained from the first experiment, in which reductions in recurrences were not observed when vaccinations were initiated after intralesional treatments were stopped.
Cured sites and recurrences.
Sites cured by intralesional cidofovir treatments were operationally defined as a cure upon resolution of the treated lesion so that there was no clinically observable papillomas. A recurrence was defined as the reappearance of macroscopic papillomas at the primary treated site after a drug-treated cure had been achieved. A long-term cure was described as the resolution of the primary site (no macroscopically observable papillomas) and the lack of recurrence after a period of 8 to 10 weeks after intralesional cidofovir treatments had stopped. We observed that if a recurrence was obtained, then papilloma regrowth was seen from 1 to 8 weeks (usually 2 to 5 weeks) after intralesional treatments were stopped.
Statistical analyses.
Statistical analysis of mean papilloma size (GMD) over time was compared to the mean size of control-treated papillomas by using Student's t test. Statistical analyses and plots were prepared using the SigmaPlot 5.0 software program. Experimental data were presented as the mean (of GMD values) ± standard error of the mean (SEM) of papilloma sizes for each dose of compound plotted against time after CRPV infection. Frequencies of regressions of recurrent lesions were compared for vector-vaccinated versus viral gene-vaccinated rabbits using the Fisher exact probability test. Frequencies of recurrences were compared also with the Fisher exact probability test.
RESULTS
Intralesional cidofovir followed by DNA vaccination (experiment 1).
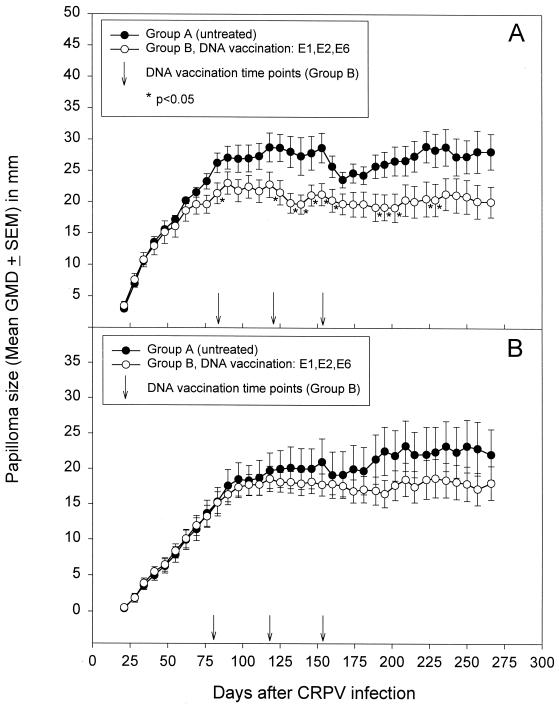
The first experiment (Table 1) was designed to test whether DNA vaccinations initiated after intralesional cidofovir cures could reduce recurrences or stimulate regressions of recurrences at a stage when the recurrent lesions were still small. Control groups A and B were included to demonstrate that DNA vaccinations alone were insufficient for complete cures of the large primary papillomas (Fig. 1). Papillomas initiated with a 10−1 dilution of CRPV extract reached a maximum mean GMD of between 20 and 25 mm at about 12 weeks after infection. Mean GMDs were slightly lower in the DNA vaccination group (group B) for several time points over the course of the entire experiment (Fig. 1A). In contrast, papillomas initiated with a 10−2 dilution of CRPV extract reached a maximum mean GMD of 20 mm at 14 weeks, and there was no significant difference between papilloma sizes of vaccinated versus nonvaccinated rabbits (Fig. 1B). These findings confirmed our previous observations that DNA vaccinations could not induce regressions of preexisting papillomas (24). The next two groups contained rabbits in which only the left two sites received intralesional cidofovir treatments. A single vaccination with CRPV E1 plus E2 plus E6 (group C) or vector alone (group D) was given on day 120. Cidofovir-cured sites totaled 6 out of 8 and 8 out of 10 for groups C and D, respectively. Recurrent sites which subsequently regressed included one out of two sites for the vaccinated group versus zero out of seven sites for the vector-only group (Table 2). Two rabbits (one from group C and one from group E) had to be euthanatized while the experimental treatments were ongoing, and data regarding the outcome of the treatments of the papillomas from these two rabbits were excluded from the analyses in Table 2.
FIG. 1.
Sizes of CRPV-induced rabbit papillomas initiated with 10−1 (A) or 10−2 (B) dilutions of CRPV extract plotted against time (in days) after infection. Each point represent the mean ± SEM of GMDs for a total of 10 papillomas per group per virus dose. Groups included rabbits without treatment (group A) versus rabbits receiving three DNA vaccinations with CRPV E1 plus E2 plus E6 expression constructs. Between-group mean papilloma sizes were compared over time using Student's t test.
TABLE 2.
Experimental outcome of intralesional cidofovir followed by DNA vaccinations (experiment no. 1)
| Group | No. of sites cured by cidofovir treatment | No. of sites recurrent after intralesional cure | No. of recurrent sites that regressed |
|---|---|---|---|
| A (no treatment) | NAa | NA | NA |
| B (E1, E2, E6 vaccination) | NA | NA | NA |
| C (E1, E2, E6 vaccination) | 6/8 (75%) | 2/6 (33%) | 1/2 (50%) |
| D (vector vaccination) | 8/10 (80%) | 7/8 (88%) | 0/7 (0%) |
| E (E1, E2, E6 vaccination) | 19/23 (83%) | 8/19 (42%) | 3/8 (38%) |
| F (vector vaccination) | 29/30 (97%) | 12/29 (41%) | 0/12 (0%) |
| C + E | 25/31 (81%) | 10/25 (40%)b | 4/10 (40%)c |
| D + F | 37/40 (93%) | 19/37 (51%) | 0/19 (0%) |
NA, not available.
Comparison with groups D plus F yielded a P value of 0.443 (Fisher exact test).
Comparison with groups D plus F yielded a P value of 0.009 (Fisher exact test).
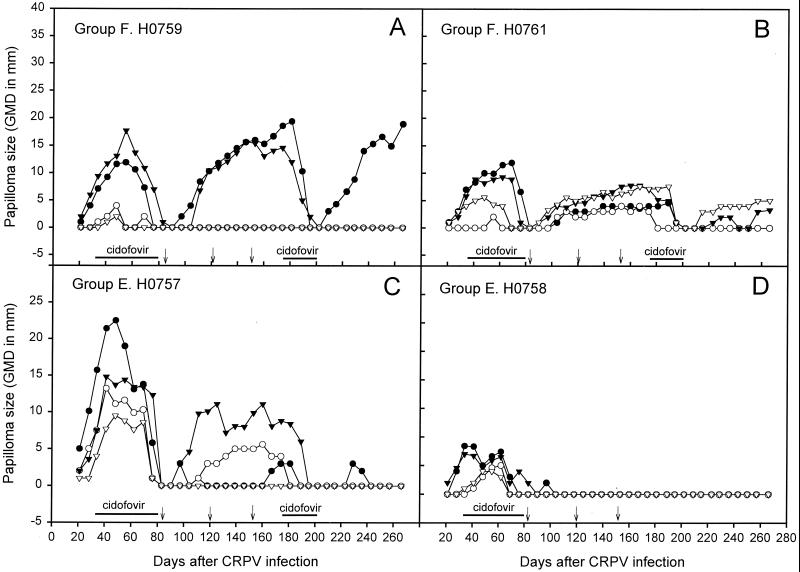
The final two groups (E and F) contained rabbits in which all four papillomas on each rabbit received intralesional cidofovir, followed by three DNA vaccinations, which were given on days 83, 120 and 155. Several rabbits in each group were treated at two separate time points with intralesional cidofovir in an attempt to cure recurrent sites. A total of 19 out of 23 (83%) papillomas were cured with intralesional cidofovir for group E rabbits which also received viral DNA vaccinations. Of the 19 cured sites, 8 out of 19 (42%) sites recurred, and 3 out of 8 (38%) of these recurrences subsequently regressed. For group F rabbits which received intralesional cidofovir and vaccinations with vector only, 29 out of 30 (97%) sites were cured by intralesional treatments and 12 out of 29 (41%) sites showed recurrences. All recurrent sites continued to grow without regression in these rabbits (Table 2). Several rabbits with recurrent papillomas in groups E and F were subjected to a second series of intralesional cidofovir treatments from days 175 to 200. These rabbits did not receive any further DNA vaccinations. Again, recurrences after intralesional cidofovir treatment were observed. Data from these additional intralesional treatments were added to the information in Table 2 for these two groups. Examples of papilloma growth rates of individual papillomas of selected rabbits from these two latter groups are shown in Fig. 2A to D.
FIG. 2.
Papilloma growth curves for individual rabbits infected at four sites as described in Materials and Methods section. Data from representative rabbits from group E (receiving cidofovir intralesional treatments and DNA vaccinations with CRPV E1 plus E2 plus E6) and group F (receiving cidofovir intralesional treatments and DNA vaccinations with vector alone) are plotted as papilloma size against time after infection with 10−1 (●, ▾) or 10−2 (○, ▿) dilutions of CRPV extract.
Intralesional cidofovir with concurrent DNA vaccination (experiment 2).
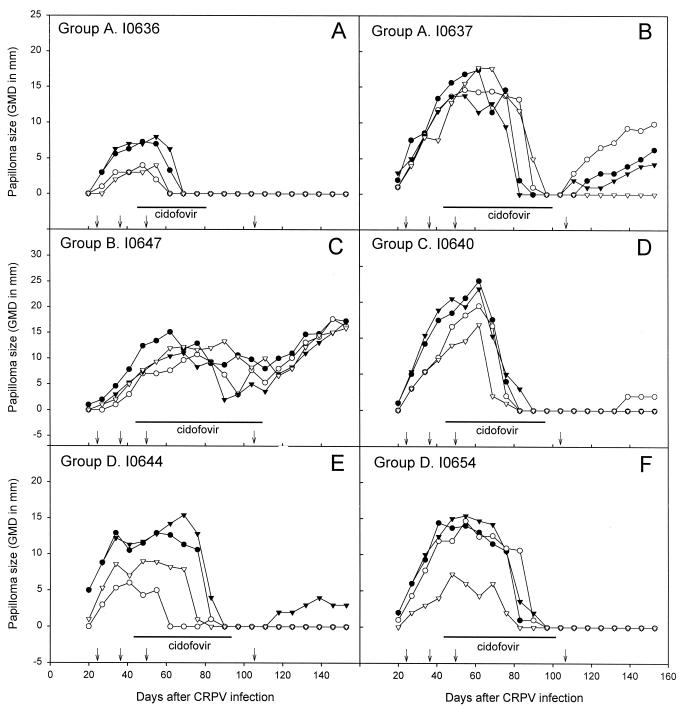
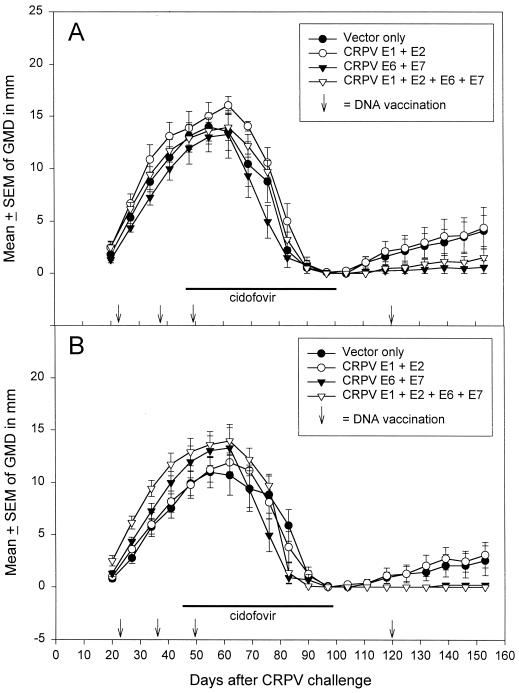
The second experiment was designed to determine whether recurrence rates could be reduced by beginning the DNA vaccinations at the time of intralesional cidofovir such that vaccine-induced antiviral immunity would be active systemically at the time of intralesional cures. Experimental groups were set up (Table 1) to include rabbits (five per group) vaccinated with CRPV E1 plus E2, CRPV E6 plus E7, all four CRPV genes, or vector alone. All papillomas were intralesionally treated with cidofovir until nearly all sites were cured. Of the 20 rabbits treated intralesionally, we observed one rabbit (in group B) in which none of the four papillomas were cured, despite extended cidofovir treatments (see Fig. 4C, rabbit I0647). Mean papilloma sizes of all cidofovir-cured papillomas for each group (papillomas that were not cured by cidofovir were excluded) were plotted over time for sites infected with high and low doses of CRPV (Fig. 3A and B, respectively). The mean size of the recurrent papillomas was greatest for vector-immunized rabbits and E1-plus-E2-immunized rabbits and lowest for the E6-plus-E7- and E1-plus-E2-plus-E6-plus-E7-immunized rabbits. Selected examples of individual rabbits for each of the four groups are shown in Fig. 4.
FIG. 4.
Papilloma growth curves for individual rabbits from experiment no. 2 infected at four sites as described in Materials and Methods. Data from representative rabbits from groups A, group B, group C, and group D are plotted as papilloma size against time after infection with 10−1 (●, ▾) or 10−2 (○, ▿) dilutions of CRPV extract. Intralesional treatment with cidofovir is marked as a solid line, and DNA vaccination time points are marked as arrows above the x axis.
FIG. 3.
Mean ± SEM of GMDs of papillomas cured by intralesional cidofovir starting from sites infected with 10−1 (A) or 10−2 (B) dilutions of CRPV extract. (A) The number of papillomas were 9 (vector alone), 8 (E1 plus E2), 10 (E6 plus E7), and 10 (all four genes). (B) The number of papillomas for the corresponding groups were 10, 8, 10, and 10. DNA vaccinations were given on days 21, 35, 50, and 120.
Intralesional cidofovir was able to achieve a long-term cure of all sites on one of the rabbits, which was vaccinated with vector alone (Fig. 4A, rabbit I0636). Several complete cures with cidofovir alone were also obtained in experiment no. 1 (data not shown), and these cures occurred particularly on those rabbits with smaller papillomas that grew slowly. Recurrences rates of cidofovir-cured sites in experiment no. 2 were 10 out of 19 in the vector-vaccinated rabbits versus 3 out of 20 in the rabbits vaccinated with either E6 plus E7 or all four viral genes (Table 3). In these two latter groups, the recurrences occurred on only two of the five rabbits such that three rabbits in each group were completely cured (Table 3). For rabbits receiving E1 plus E2 vaccinations, there were eight recurrent sites, confined to two rabbits.
TABLE 3.
Experimental outcome of intralesional cidofovir with concurrent DNA vaccinations (experiment no. 2)
| Group | No. of sites cured by cidofovir | No. of sites recurrent after intralesional cure | No. of recurrent sites that regressed | No. of rabbits with complete cures of four sites |
|---|---|---|---|---|
| A | 19/20 (95%) | 10/19 (53%) | 1/10 (10%) | 1/5 |
| B | 16/20 (80%) | 8/16 (50%)a | 0/8 (0%) | 2/5c |
| C | 20/20 (100%) | 3/20 (15%)b | 1/3 (33%) | 3/5 |
| D | 20/20 (100%) | 3/20 (15%)b | 0/3 (0%) | 3/5 |
Comparison with group A yielded a P value of 1.000 (Fisher exact test).
Comparison with group A yielded a P value of 0.019 (Fisher exact test).
One rabbit showed no cures with intralesional cidofovir.
Recurrence rates after intralesional cures.
The time to recurrence of cidofovir-cured papillomas was recorded for each group, and the data are summarized in Fig. 5. Recurrences ranged from 1 to 8 weeks after intralesional cure. In general, the recurrence rates were similar between vector-vaccinated and viral-gene-vaccinated rabbits for both experiments. A tendency to delayed recurrence for rabbits in groups C and D in experiment no. 2 was noted, although the sample size was small.
FIG. 5.
Time of recurrences after intralesional cidofovir cure of papillomas. Recurrences in selected groups from experiments no. 1 and 2 are shown (∗) and represent the time in weeks that macroscopic lesions were noticed at the cured sites. Frequencies of recurrences and the number of intralesional cures are numerically presented in Tables 2 and 3.
DISCUSSION
In this study, we combined intralesional antiviral treatments with viral DNA vaccinations to treat and cure large established CRPV-induced rabbit papillomas. The CRPV model proved to be an ideal system to test such an approach for the treatment of persistent papilloma infections. The CRPV strain that we use routinely is a progressive strain which produces large papillomas that persist with a very low frequency of spontaneous regressions (14, 45). In addition, we have observed that topical and intralesional cures lead to the phenomenon of papilloma recurrence at the rate of about 50% of cured sites (this report). This feature of the CRPV rabbit model is relevant to the situation observed for HPV disease treatment of patients with genital warts and laryngeal papillomas (4, 5, 16, 56). We have conducted experiments on outbred rabbits with DNA vaccinations and observed that preimmunizations could lead to protection against viral challenge (25) but that postinfection vaccinations were unable to cure established papillomas (reference 24 and this report). The outbred rabbits are thus immune competent, but natural and induced host immunity that develops during infection is insufficient to cure large papillomas. A combination approach including lesion ablation followed by specific antiviral immunizations to cure residual and/or subclinical disease is therefore a logical approach to the treatment of persistent papillomavirus infections.
When the two combination experiments were compared, the data indicated that late initiation of DNA vaccinations (experiment no. 1) had no impact on the frequency of recurrences but did affect the recurrent lesions, as evidenced by a small number of regressions. No regressions of recurrent sites were observed in the vector-only vaccinated rabbits (Table 2). In contrast, for rabbits receiving DNA vaccinations at the time of intralesional cidofovir treatments (experiment no. 2), there was a decrease in the incidence of recurrences (Table 3), but only one out of six recurrent sites subsequently regressed. These studies suggested that DNA vaccination-induced immunity to the viral antigens was insufficient for a complete cure of all recurrent sites in the second experiment. We have used DNA expression vectors that contain the cytomegalovirus promoter (14) to drive expression of the viral genes, and this promoter is susceptible to down-regulation in vivo during certain inflammatory responses which may occur during the boosting immunizations (11, 28, 43). Thus, expression constructs that utilize different promoters for the boosting vaccinations may induce a better therapeutic response.
One of 20 rabbits in experiment no. 2 received extended intralesional cidofovir treatment without being cured, although reductions were observed (Fig. 4C). Several rabbits in experiment no. 1 also had papillomas that were more resistant to cidofovir treatment. Other rabbits had papillomas that were easily cured by intralesional cidofovir (Fig. 4A). These observations indicated that there were considerable differences in response to cidofovir by papillomas on individual outbred rabbits.
An important observation in these experiments is that DNA vaccinations after papillomas had become established could not cure the primary sites. These observations indicated that there was a critical need for additional therapeutic treatment of existing lesions to achieve a more effective therapeutic outcome. A similar situation may occur in patients with persistent HPV infections. Current therapeutic approaches to HPV disease usually include either lesion ablation with antiviral compounds (4, 5, 16, 56) or viral antigen stimulations for the induction of antiviral immunity (7, 44, 51, 55, 59). The studies presented here with the CRPV rabbit model suggest that independent strategies may fail to cure persistent benign papillomas due to lesion recurrences (with antiviral compounds) and ineffective immunity (with viral antigen immunizations).
Earlier experiments with protective vaccinations using individual viral genes demonstrated no effect when E7 alone was used (14). In contrast, E1 had strong protective immunity and both E2 and E6 had moderate protective effects (27, 30, 49, 52). In those rabbits vaccinated with E1 plus E2 and in which complete protection was not obtained, lesions often regressed (27, 49). In the studies described here, postinfection vaccinations with E6 plus E7 showed an effective reduction of recurrences, whereas E1 plus E2 vaccinations were not as effective and there were no regressions of recurrences (Table 3). In addition, postinfection vaccinations alone were unable to cure existing papillomas (Fig. 1). These data indicate that there are differences in the antitumor (papilloma) immunity that is triggered in naive animals versus those bearing tumors (papillomas). Such differences in antitumor immunity have been observed in both humans and animals with tumor burden (reviewed in references 21, 36, 50 and 53).
In conclusion, combination antiviral treatment with DNA vaccinations has produced cures of large established CRPV-induced rabbit papillomas and reduced the incidence of lesion recurrence. Such a strategy may be effective in the treatment of persistent HPV disease.
ACKNOWLEDGMENTS
These studies were supported by Public Health Service grants AI85337 from the National Institutes of Allergy and Infectious Diseases and CA47622 from the National Cancer Institute, National Institutes of Health, and by the Jake Gittlen Memorial Golf Tournament.
REFERENCES
- 1.Aiba S, Rokugo M, Tagami H. Immunohistologic analysis of the phenomenon of spontaneous regression of numerous flat warts. Cancer. 1986;58:1246–1251. doi: 10.1002/1097-0142(19860915)58:6<1246::aid-cncr2820580612>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 2.Apple R J, Becker T M, Wheeler C M, Erlich H A. Comparison of human leukocyte antigen DR-DQ disease associations found with cervical dysplasia and invasive cervical carcinoma. J Natl Cancer Inst. 1995;87:427–436. doi: 10.1093/jnci/87.6.427. [DOI] [PubMed] [Google Scholar]
- 3.Apple R J, Erlich H A, Klitz W, Manos M M, Becker T M, Wheeler C M. HLA DR-DQ associations with cervical carcinoma show papillomavirus-type specificity. Nat Genet. 1994;6:157–162. doi: 10.1038/ng0294-157. [DOI] [PubMed] [Google Scholar]
- 4.Auborn K J, Steinberg B M. Therapy of papillomavirus-induced lesion. In: Pfister H, editor. Papillomaviruses and human cancer. Boca Raton, Fla: CRC Press; 1990. pp. 203–224. [Google Scholar]
- 5.Baker G E, Tyring S K. Therapeutic approaches to papillomavirus infections. Dermatol Clin. 1997;15:331–340. doi: 10.1016/s0733-8635(05)70441-1. [DOI] [PubMed] [Google Scholar]
- 6.Beutner K R, Tyring S K, Trofatter K F, Jr, Douglas J M, Jr, Spruance S, Owens M L, Fox T L, Hougham A J, Schmitt K A. Imiquimod, a patient-applied immune-response modifier for treatment of external genital warts. Antimicrob Agents Chemother. 1998;42:789–794. doi: 10.1128/aac.42.4.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borysiewicz L K, Fiander A, Nimako M, Man S, Wilkinson G W, Westmoreland D, Evans A S, Adams M, Stacey S N, Boursnell M E, Rutherford E, Hickling J K, Inglis S C. A recombinant vaccinia virus encoding human papillomavirus types 16 and 18, E6 and E7 proteins as immunotherapy for cervical cancer. Lancet. 1996;347:1523–1527. doi: 10.1016/s0140-6736(96)90674-1. [DOI] [PubMed] [Google Scholar]
- 8.Campo M S, Moar M H, Jarrett W F H, Laird H M. Presence and expression of bovine papillomavirus type 4 in tumours of the alimentary canal of cattle and its possible role. A new papillomavirus associated with alimentary cancer in cattle. Nature. 1980;286:180–182. doi: 10.1038/286180a0. [DOI] [PubMed] [Google Scholar]
- 9.Carter J J, Koutsky L A, Wipf G C, Christensen N D, Lee S K, Kuypers J, Kiviat N, Galloway D A. The natural history of human papillomavirus type 16 capsid antibodies among a cohort of university women. J Infect Dis. 1996;174:927–936. doi: 10.1093/infdis/174.5.927. [DOI] [PubMed] [Google Scholar]
- 10.Chambers V C, Evans C A. Canine oral papillomatosis. I. Virus assay and observations of the various stages of the experimental infection. Cancer Res. 1959;19:1188–1195. [PubMed] [Google Scholar]
- 11.Cheeran M C, Hu S, Gekker G, Lokensgard J R. Decreased cytomegalovirus expression following proinflammatory cytokine treatment of primary human astrocytes. J Immunol. 2000;164:926–933. doi: 10.4049/jimmunol.164.2.926. [DOI] [PubMed] [Google Scholar]
- 12.Christensen N D, Han R, Kreider J W. Cottontail rabbit papillomavirus (CRPV) In: Ahmed R, Chen I, editors. Persistent viral infections. Sussex, England: John Wiley & Sons Ltd.; 2000. pp. 485–502. [Google Scholar]
- 13.Christensen N D, Kreider J W. Antibody-mediated neutralization in vivo of infectious papillomaviruses. J Virol. 1990;64:3151–3156. doi: 10.1128/jvi.64.7.3151-3156.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christensen N D, Kreider J W. Animal models of papillomavirus infections. In: Zak O, Sande M A, editors. Handbook of animal models of infection. London, England: Academic Press; 1999. pp. 1039–1047. [Google Scholar]
- 15.Christensen N D, Pickel M D, Budgeon L R, Kreider J W. In vivo anti-papillomavirus activity of nucleoside analogues including cidofovir on CRPV-induced rabbit papillomas. Antivir Res. 2000;48:131–142. doi: 10.1016/s0166-3542(00)00124-8. [DOI] [PubMed] [Google Scholar]
- 16.Cirelli R, Tyring S K. Interferons in human papillomavirus infections. Antivir Res. 1994;24:191–204. doi: 10.1016/0166-3542(94)90067-1. [DOI] [PubMed] [Google Scholar]
- 17.Clerici M, Merola M, Ferrario E, Trabattoni D, Villa M L, Stefanon B, Venzon D J, Shearer G M, DePalo G, Clerici E. Cytokine production patterns in cervical intraepithelial neoplasia: association with human papillomavirus infection. J Natl Cancer Inst. 1997;89:245–250. doi: 10.1093/jnci/89.3.245. [DOI] [PubMed] [Google Scholar]
- 18.Cooper K D, Androphy E J, Lowy D, Katz S I. Antigen presentation and T-cell activation in epidermodysplasia verruciformis. J Investig Dermatol. 1990;94:769–776. doi: 10.1111/1523-1747.ep12874631. [DOI] [PubMed] [Google Scholar]
- 19.Critchlow C W, Surawicz C M, Holmes K K, Kuypers J, Daling J R, Hawes S E, Goldbaum G M, Sayer J, Hurt C, Dunphy C, Kiviat N B. Prospective study of high grade anal squamous intraepithelial neoplasia in a cohort of homosexual men: influence of HIV infection, immunosuppression and human papillomavirus infection. AIDS. 1995;9:1255–1262. doi: 10.1097/00002030-199511000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Edwards L, Ferenczy A, Eron L, Baker D, Owens M L, Fox T L, Hougham A J, Schmitt K A. Self-administered topical 5% imiquimod cream for external anogenital warts. HPV Study Group. Human PapillomaVirus. Arch Dermatol. 1998;134:25–30. doi: 10.1001/archderm.134.1.25. [DOI] [PubMed] [Google Scholar]
- 21.Forni G, Lollini P L, Musiani P, Colombo M P. Immunoprevention of cancer: is the time ripe? Cancer Res. 2000;60:2571–2575. [PubMed] [Google Scholar]
- 22.Frazer I H. Immunology of papillomavirus infection. Curr Opin Immunol. 1996;8:484–491. doi: 10.1016/s0952-7915(96)80035-5. [DOI] [PubMed] [Google Scholar]
- 23.Grassmann K, Wilczynski S P, Cook N, Rapp B, Iftner T. HPV-6 variants from malignant tumors with sequence alterations in the regulatory region do not reveal differences in the activities of the oncogene promoters but do contain amino acid exchanges in the E6 and E7 proteins. Virology. 1996;223:185–189. doi: 10.1006/viro.1996.0467. [DOI] [PubMed] [Google Scholar]
- 24.Han R, Cladel N M, Reed C A, Peng X, Budgeon L R, Pickel M D, Christensen N D. DNA vaccination prevents and/or delays carcinoma development of papillomavirus-induced skin papillomas on rabbits. J Virol. 2000;74:9712–9716. doi: 10.1128/jvi.74.20.9712-9716.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Han R, Cladel N M, Reed C A, Peng X, Christensen N D. Protection of rabbits from viral challenge by gene gun-based intracutaneous vaccination with a combination of cottontail rabbit papillomavirus E1, E2, E6, and E7 genes. J Virol. 1999;73:7039–7043. doi: 10.1128/jvi.73.8.7039-7043.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Han R, Reed C A, Cladel N M, Christensen N D. Intramuscular injection of plasmid DNA encoding cottontail rabbit papillomavirus E1, E2, E6 and E7 induces T cell-mediated but not humoral immune responses in rabbits. Vaccine. 1999;17:1558–1566. doi: 10.1016/s0264-410x(98)00356-9. [DOI] [PubMed] [Google Scholar]
- 27.Han R, Reed C A, Cladel N M, Christensen N D. Immunization of rabbits with cottontail rabbit papillomavirus E1 and E2 genes: protective immunity induced by gene gun-mediated intracutaneous delivery but not by intramuscular injection. Vaccine. 2000;18:2937–2944. doi: 10.1016/s0264-410x(00)00110-9. [DOI] [PubMed] [Google Scholar]
- 28.Harms J S, Oliveira S C, Splitter G A. Regulation of transgene expression in genetic immunization. Braz J Med Biol Res. 1999;32:155–162. doi: 10.1590/s0100-879x1999000200003. [DOI] [PubMed] [Google Scholar]
- 29.Harvey S B, Cladel N M, Budgeon L R, Welsh P A, Griffith J W, Lang C M, Christensen N D. Rabbit genital tissue is susceptible to infection by rabbit oral papillomavirus: an animal model of a genital tissue-targeting papillomavirus. J Virol. 1998;72:5239–5244. doi: 10.1128/jvi.72.6.5239-5244.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jensen E R, Selvakumar R, Shen H, Ahmed R, Wettstein F O, Miller J F. Recombinant Listeria monocytogenes vaccination eliminates papillomavirus-induced tumors and prevents papilloma formation from viral DNA. J Virol. 1997;71:8467–8474. doi: 10.1128/jvi.71.11.8467-8474.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kawase M, Orth G, Jablonska S, Blanchet-Bardon C, Rueda L A, Favre M. Variability and phylogeny of the L1 capsid protein gene of human papillomavirus type 5: contribution of clusters of nonsynonymous mutations and of a 30-nucleotide duplication. Virology. 1996;221:189–198. doi: 10.1006/viro.1996.0365. [DOI] [PubMed] [Google Scholar]
- 32.Kiviat N B, Critchlow C W, Holmes K K, Kuypers J, Sayer J, Dunphy C, Surawicz C, Kirby P, Wood R, Daling J R. Association of anal dysplasia and human papillomavirus with immunosuppression and HIV infection among homosexual men. AIDS. 1993;7:43–49. doi: 10.1097/00002030-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Knowles G, O'Neil B W, Campo M S. Phenotypical characterization of lymphocytes infiltrating regressing papillomas. J Virol. 1996;70:8451–8458. doi: 10.1128/jvi.70.12.8451-8458.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kreider J W, Bartlett G L. The Shope papilloma-carcinoma complex of rabbits: a model system of neoplastic progression and spontaneous regression. Adv Cancer Res. 1981;35:81–110. doi: 10.1016/s0065-230x(08)60909-4. [DOI] [PubMed] [Google Scholar]
- 35.Majewski S, Jablonska S, Orth G. Epidermodysplasia verruciformis. Immunological and nonimmunological surveillance mechanisms: role in tumor progression. Clin Dermatol. 1997;15:321–334. doi: 10.1016/s0738-081x(96)00169-1. [DOI] [PubMed] [Google Scholar]
- 36.Marincola F M, Jaffee E M, Hicklin D J, Ferrone S. Escape of human solid tumors from T-cell recognition: molecular mechanisms and functional significance. Adv Immunol. 2000;74:181–273. doi: 10.1016/s0065-2776(08)60911-6. [DOI] [PubMed] [Google Scholar]
- 37.McMichael H. Inhibition by methylprednisolone of regression of the Shope rabbit papilloma. J Natl Cancer Inst. 1967;39:55–65. [PubMed] [Google Scholar]
- 38.Nicholls P K, Klaunberg B A, Moore R A, Santos E B, Parry N R, Gough G W, Stanley M A. Naturally occurring, nonregressing canine oral papillomavirus infection: host immunity, virus characterization, and experimental infection. Virology. 1999;265:365–374. doi: 10.1006/viro.1999.0060. [DOI] [PubMed] [Google Scholar]
- 39.Nicholls P K, Stanley M A. The immunology of animal papillomaviruses. Vet Immunol Immunopathol. 2000;73:101–127. doi: 10.1016/s0165-2427(99)00165-8. [DOI] [PubMed] [Google Scholar]
- 40.Okabayashi M, Angell M G, Christensen N D, Kreider J W. Morphometric analysis and identification of infiltrating leucocytes in regressing and progressing Shope rabbit papillomas. Int J Cancer. 1991;49:919–923. doi: 10.1002/ijc.2910490620. [DOI] [PubMed] [Google Scholar]
- 41.Parsons R J, Kidd J G. A virus causing oral papillomatosis in rabbits. Proc Soc Exp Biol Med. 1936;35:441–443. [Google Scholar]
- 42.Pisani P, Parkin D M, Ferlay J. Estimates of the worldwide mortality from eighteen major cancers in 1985. Implications for prevention and projections of future burden. Int J Cancer. 1993;55:891–903. doi: 10.1002/ijc.2910550604. [DOI] [PubMed] [Google Scholar]
- 43.Qin L, Ding Y, Pahud D R, Chang E, Imperiale M J, Bromberg J S. Promoter attenuation in gene therapy: interferon-gamma and tumor necrosis factor-alpha inhibit transgene expression. Hum Gene Ther. 1997;8:2019–2029. doi: 10.1089/hum.1997.8.17-2019. [DOI] [PubMed] [Google Scholar]
- 44.Ressing M E, van Driel W J, Brandt R M, Kenter G G, de Jong J H, Bauknecht T, Fleuren G J, Hoogerhout P, Offringa R, Sette A, Celis E, Grey H, Trimbos B J, Kast W M, Melief C J. Detection of T helper responses, but not of human papillomavirus-specific cytotoxic T lymphocyte responses, after peptide vaccination of patients with cervical carcinoma. J Immunother. 2000;23:255–266. doi: 10.1097/00002371-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Salmon J, Ramoz N, Cassonnet P, Orth G, Breitburd F. A cottontail rabbit papillomavirus strain (CRPVb) with strikingly divergent E6 and E7 oncoproteins: an insight in the evolution of papillomaviruses. Virology. 1997;235:228–234. doi: 10.1006/viro.1997.8680. [DOI] [PubMed] [Google Scholar]
- 46.Sastre-Garau X, Loste M N, Vincent-Salomon A, Favre M, Mouret E, dela Rochefordiere A, Durand J C, Tartour E, Lepage V, Charron D. Decreased frequency of HLA-DRB1 ∗ 13 alleles in French women with HPV-positive carcinoma of the cervix. Int J Cancer. 1996;67:159–164. doi: 10.1002/(SICI)1097-0215(19960621)69:3<159::AID-IJC1>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 47.Schneider A, Kirchhoff T, Meinhardt G, Gissmann L. Repeated evaluation of human papillomavirus 16 status in cervical swabs of young women with a history of normal Papanicolaou smears. Obstet Gynecol. 1992;79:683–688. [PubMed] [Google Scholar]
- 48.Seibel W, Sundberg J P, Lesko L J, Sauk J J, McCleary L B, Hassell T M. Cutaneous papillomatous hyperplasia in cyclosporine-A treated beagles. J Investig Dermatol. 1989;93:224–230. doi: 10.1111/1523-1747.ep12277577. [DOI] [PubMed] [Google Scholar]
- 49.Selvakumar R, Borenstein L A, Lin Y L, Ahmed R, Wettstein F O. Immunization with nonstructural proteins E1 and E2 of cottontail rabbit papillomavirus stimulates regression of virus-induced papillomas. J Virol. 1995;69:602–605. doi: 10.1128/jvi.69.1.602-605.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sinkovics J G, Horvath J C. Vaccination against human cancers. Int J Oncol. 2000;16:81–96. doi: 10.3892/ijo.16.1.81. [DOI] [PubMed] [Google Scholar]
- 51.Steller M A, Gurski K J, Murakami M, Daniel R W, Shah K V, Celis E, Sette A, Trimble E L, Park R C, Marincola F M. Cell-mediated immunological responses in cervical and vaginal cancer patients immunized with a lipidated epitope of human papillomavirus type 16 E7. Clin Cancer Res. 1998;4:2103–2109. [PubMed] [Google Scholar]
- 52.Sundaram P, Tigelaar R E, Xiao W, Brandsma J L. Intracutaneous vaccination of rabbits with the E6 gene of cottontail rabbit papillomavirus provides partial protection against virus challenge. Vaccine. 1998;16:613–623. doi: 10.1016/s0264-410x(97)84510-0. [DOI] [PubMed] [Google Scholar]
- 53.Tagawa M. Cytokine therapy for cancer. Curr Pharm Des. 2000;6:681–699. doi: 10.2174/1381612003400597. [DOI] [PubMed] [Google Scholar]
- 54.Tieben L M, Berkhout R J, Smits H L, Bouwes Bavinck J N, Vermeer B J, Bruijn J A, Van der Woude F J, ter Schegget J. Detection of epidermodysplasia verruciformis-like human papillomavirus types in malignant and premalignant skin lesions of renal transplant recipients. Br J Dermatol. 1994;131:226–230. doi: 10.1111/j.1365-2133.1994.tb08496.x. [DOI] [PubMed] [Google Scholar]
- 55.van Driel W J, Ressing M E, Kenter G G, Brandt R M, Krul E J, van Rossum A B, Schuuring E, Offringa R, Bauknecht T, Tamm-Hermelink A, van Dam P A, Fleuren G J, Kast W M, Melief C J, Trimbos J B. Vaccination with HPV16 peptides of patients with advanced cervical carcinoma: clinical evaluation of a phase I-II trial. Eur J Cancer. 1999;35:946–952. doi: 10.1016/s0959-8049(99)00048-9. [DOI] [PubMed] [Google Scholar]
- 56.Wilson W R, Hashemiyoon R, Hawrych A. Intralesional cidofovir for recurrent laryngeal papillomas: preliminary report. Ear Nose Throat J. 2000;79:236–240. [PubMed] [Google Scholar]
- 57.Wu T C, Kurman R J. Analysis of cytokine profiles in patients with human papillomavirus-associated neoplasms. J Natl Cancer Inst. 1997;89:185–187. doi: 10.1093/jnci/89.3.185. [DOI] [PubMed] [Google Scholar]
- 58.Xi L F, Demers G W, Koutsky L A, Kiviat N B, Kuypers J, Watts D H, Holmes K K, Galloway D A. Analysis of human papillomavirus type 16 variants indicates establishment of persistent infection. J Infect Dis. 1995;172:747–755. doi: 10.1093/infdis/172.3.747. [DOI] [PubMed] [Google Scholar]
- 59.Zhang L F, Zhou J, Chen S, Cai L L, Bao Q Y, Zheng F Y, Lu J Q, Padmanabha J, Hengst K, Malcolm K, Frazer I H. HPV6b virus like particles are potent immunogens without adjuvant in man. Vaccine. 2000;18:1051–1058. doi: 10.1016/s0264-410x(99)00351-5. [DOI] [PubMed] [Google Scholar]