Summary:
Neurons in the dorsolateral pontine reticular formation, in interaction with other brainstem and forebrain regions, generate the basic phenomena of rapid-eye-movement (REM) sleep. Non-REM sleep is the product of multiple control mechanisms in the forebrain and brainstem. Despite considerable progress in the identification of generation mechanisms, the functions of sleep remain a mystery. I hypothesize that REM sleep has a role in the regulation of receptor sensitivity in the central and peripheral nervous systems.
Keywords: Rapid-eye-movement sleep, Non-rapid-eye-movement sleep, Nucleus solitarius, Raphe, Locus ceruleus, Basal forebrain, Acetylcholine, Norepinephrine.
The purpose of this paper is to provide a general review of the current status of research on the neural control of sleep states. In order to put current research into perspective, it is helpful to recall the state of knowledge about sleep control that existed in the 1950s. At that time, sleep was thought to be a unitary process with varying levels of consciousness and corresponding changes in the relative proportion of high-voltage slow EEG waves in cortical recordings. The concept of a reticular formation in the core of the brainstem provided an anatomical substrate for the regulation of the sleep-wakefulness continuum. At minimal levels of activity in the reticular core, the maximal intensity of sleep, with its high-voltage EEG waves, was seen. Sensory inputs to the reticular core were thought to control its activity, thus providing an explanation for the arousing effects of sensory stimuli. However, this concept did not explain the fact that the complete removal of sensory inputs did not increase sleep or prevent sleep-wake cycles (Batsel, 1964). The discovery of rapid-eye-movement (REM) sleep (Aserinsky and Kleitman, 1953) further complicated this picture, since it soon became apparent that REM sleep was as different from non-REM (NREM) sleep as both stages of sleep were different from wakefulness. We now know that the control mechanisms for REM and NREM sleep are anatomically distinct. REM sleep is controlled by a relatively discrete system located in the pons, where NREM sleep is controlled by multiple systems, with crucial neuronal groups in the basal forebrain, hypothalamus, midbrain, pons, and medulla. Recent work has enabled the identification of the neuronal groups and neurotransmitter mechanisms involved in REM and NREM sleep control.
This paper reviews the basic phenomenology of REM and NREM sleep and describes the data relevant to the anatomical localization of the brain systems generating these states. Some speculations on the functional role of these states are then offered.
PHENOMENOLOGY OF NREM SLEEP
Traditionally, emphasis has been placed on the EEG correlates of sleep as a primary defining feature. Sleep onset is accompanied or followed by EEG spindle activity, depending on the defining criteria selected (Rechtschaffen and Kales, 1968; Ursin and Sterman, 1981). Spindles are high-voltage bursts of EEG activity in the 12–14-Hz range. Spindles become intermixed with 1–4-Hz slow waves as sleep progresses. In both humans and animals, the ratio of slow waves to spindles has been used to identify stages of NREM sleep. In cats, NREM sleep Stages 1 and 2 are scored, whereas in humans a subdivision into four NREM sleep stages has been made, with Stage 4 having the greatest proportion of slow waves.
Although EEG synchrony has been the most studied of NREM sleep signs, other physiological variables are equally characteristic and central to NREM sleep. Muscle tone is reduced, but not absent, in NREM sleep. Temperature and respiratory regulation are intact (Phillipson, 1978; Harper et al., 1988; Parmeggiani, 1988). Neuronal activity in the brainstem reticular formation is reduced from waking levels to the lowest levels that occur during the sleep–wake cycle (Siegel, 1979). In the cerebral cortex, unit discharge rates are also reduced in NREM sleep. There is a profound fall in blood flow, correlated with decreased glucose utilization in the brain. This blood flow decrease is present in all neocortical and some subcortical regions, consistent with the generalized decrease in unit discharge found in the brain (Kennedy et al., 1982; Ramm and Frost, 1986; Meyer et al., 1987). To summarize, NREM sleep is characterized by a widespread reduction in brain activity and energy usage correlated with EEG voltage increases and by a maintenance of autonomic regulation. However, there are a few very important exceptions to this general rule of reduced brain activity during NREM sleep, as described below.
WHERE IS NREM SLEEP GENERATED?
Extensive studies have led to the conclusion that NREM sleep generation involves interactions among several brainstem, diencephalic, and forebrain cell groups. A striking feature of the organization of NREM sleep mechanisms is that, whereas in the intact animal this entire network is involved, it is possible to see many of the signs of NREM sleep in either half of the brain after transections of the neuraxis. Thus, it appears that there are multiple generators for NREM sleep that can independently produce local aspects of this state in either brainstem or forebrain.
The most caudal region implicated in NREM sleep control is the region of the nucleus of the solitary tract. Low-frequency stimulation of this structure can produce short-latency sleep onset (Magnes et al., 1961). Stimulation of the baroreceptor afferents to this area can also produce rapid sleep onset with relatively short latency to REM sleep (Puizillout and Foutz, 1977). Cooling and obstruction of blood flow to the medulla is associated with arousal, as would be expected if one were inactivating a hypnogenic region (Berlucchi et al., 1964). A population of neurons in this area that is maximally active in NREM sleep has been identified (Eguchi and Satoh, 1980).
In NREM sleep, the role of the raphe system, the midline serotonergic system of the brainstem, remains unclear. Depletion of serotonin with the synthesis inhibitor P-chlorophenylalanine (PCPA) produces insomnia that can be rapidly reversed by injection of the serotonin precursor tryptophan (Pujol et al., 1971). Recent work has identified the anterior hypothalamus as perhaps the critical site for the action of serotonin in reversing PCPA insomnia (Jouvet et al., 1989). However, recording studies have found that raphe neurons discharge regularly in wakefulness, slowly in NREM sleep, and not at all in REM sleep (McGinty and Harper, 1976), not a pattern consistent with the depletion data indicating an active role for serotonin in inducing NREM sleep. One possible resolution to this discrepancy is to postulate that serotonin has some action in wakefulness that facilitates subsequent NREM sleep.
Shute and Lewis (1967) originated the concept of an ascending cholinergic activating system. This fit well with extensive data showing loss of behavioral responsiveness and EEG synchrony after damage to the midbrain reticular formation (Lindsley et al., 1949, 1950) and arousal after stimulation of this area. Recent work has helped identify the cellular components of this system, which originate in the pedunculopontine (PPN) and laterodorsal tegmental (LDT) nuclei of the dorsolateral pons (Jones and Beaudet, 1987; Vincent and Reiner, 1987; Shiromani et al., 1988). It has long been known that acetylcholine (ACh) release was maximal in states of desynchronized or low-voltage EEG, and minimal in NREM sleep (Kanai and Szerb, 1965; Celesia and Jasper, 1966). These data suggest that cholinergic neurons of the pons and midbrain produced the EEG desynchrony and associated arousal of waking and that their inactivity produced NREM sleep. A problem for the hypothesized role of the cholinergic ascending system in NREM sleep control is the lack of EEG changes after extensive cytotoxic lesion of these neurons. These lesions produce little increase in sleep and few EEG changes (Webster and Jones, 1988). Webster and Jones (1988) hypothesized that, although brainstem cholinergic systems may normally contribute to arousal, in the absence of brainstem cholinergic input, forebrain and noncholinergic brainstem systems are able to maintain EEG desynchrony and waking behavioral states. Recent work has indicated that brainstem ACh neurons do not have direct projections to cortex (Pare et al., 1988; Smith, 1988; Steriade et al., 1988). Therefore, changes in cortical ACh level must result from changes in the activity in diencephalic ACh containing neurons in the basal forebrain region, which may be under the control of brainstem systems.
Extensive work by Steriade and colleagues has identified thalamic generators as the source of spindle activity in NREM sleep (see Steriade, 1989, for review). He has shown that the nucleus reticularis, a nuclear shell surrounding much of the thalamus, is both necessary and sufficient for the generation of spindle activity in thalamic nuclei and in their cortical projection regions. The nucleus reticularis is in turn under the control of midbrain reticular elements, including those employing ACh as a transmitter.
Clinical observations and lesion studies led to the concept of a waking center in the posterior hypothalamus. Lesions and chemical inactivation of this area produced hypersomnia (von-Economo, 1918; Ranson, 1939; Nauta, 1946; Lin et al., 1989). Unit recording studies have found cells in this region that are “waking-active” (Vanni-Mercier, 1985).
This waking center may work reciprocally with a sleep center in the preoptic hypothalamic–basal forebrain region, the most rostral region shown to be critical in NREM sleep control. (The term basal forebrain is used to include the nucleus of the diagonal band, the substantia innominata, and lateral preoptic area.) Electrical stimulation of the basal forebrain has been shown to induce NREM sleep at short latency. Indeed, it is the only site at which high-frequency stimulation has been shown to induce sleep (Sterman and Clemente, 1962). Both electrolytic and chemical lesions of this area produce a profound insomnia, with a permanent reduction in NREM sleep time (McGinty and Sterman, 1968; Szymusiak and McGinty, 1986). The most definitive evidence for a normal role of this region in NREM sleep control is the discovery of a class of sleep-active neurons in the basal forebrain (Szymusiak and McGinty, 1986) and preoptic area (Kaitin, 1984). In contrast to the vast majority of brain neurons that reach their lowest discharge levels in NREM sleep, these cells are maximally active in NREM sleep. They have been shown to project to the cortex and to interact with midbrain regions (McGinty and Szymusiak, 1988). These neurons are thermosensitive, thus providing a basis for the facilitation of sleep by fever and possibly for a normal role of body temperature oscillations in sleep regulation.
WHAT IS REM SLEEP?
In intact, adult humans, REM sleep is identified by the simultaneous presence of a desynchronized (i.e., relatively low-voltage) cortical EEG, an absence of activity in the antigravity muscles (atonia), and periodic bursts of rapid eye movements. The rapid-eye-movement bursts are often accompanied by changes in respiration and by phasic muscle activity. In human infants and in many young animals, active sleep—the ontogenetic precursor of the REM sleep state—is not accompanied by tonic cortical EEG desynchrony or muscle atonia and must be identified by the phasic muscle twitches and eye movements that recur during the quiescent state.
Studies with deep electrodes have established that, whereas cortical EEG is highly desynchronized in the REM sleep state, hippocampal EEG is highly synchronized at a 4–10-Hz (theta) frequency. Hippocampal theta can also be observed in active waking, particularly during certain classes of movements, at times when neocortical EEG is maximally desynchronized (Vanderwolf and Robinson, 1981).
Another subcortically observed phenomenon that is characteristic of REM sleep is ponto-geniculo-occipital (PGO) spikes. These waves, which are generated in the pons (Jouvet, 1962), propagate rostrally through pathways in the vicinity of the brachium conjunctivum (Laurent and Guerrero, 1975; Sakai et al., 1976) and project through the lateral geniculate and other thalamic nuclei (Hobson et al., 1969) to the cortex. The PGO spikes are thought to be a pacemaker that drives many of the phasic events of REM sleep. Among the most significant of these phasic events are eye movements, changes in respiration (Orem, 1980), and changes in heart rate (Baust et al., 1972).
One phenomenon that is unique to REM sleep is the loss of activity in the antigravity musculature (Jouvet, 1962). Recordings of dorsal neck electromyography (EMG) in animals and submental EMG in humans are particularly useful in state classification. In most animals, only the diaphragm and extraocular muscles retain substantial tone during REM sleep. However, atonia is not complete in all animals. REM sleep neck muscle tone is well documented in the rabbit and bird, and is probably present in other animals and in particular muscle groups in a number of animals (Klein et al., 1964; Tradardi, 1966; Pivik et al., 1981). The muscle atonia of REM sleep may be interrupted by muscle twitches, which accompany bursts of PGO spikes and eye movements. During REM sleep, sympathetic tone is dramatically decreased (Baust et al., 1968; Reiner, 1986), contributing, along with disinhibition of the Edinger Westphal nucleus (Villablanca, 1966), to miosis of the pupil, changes in cardiovascular function, and other peripheral autonomic effects (Baust et al., 1971, 1972). Indeed, this reduction in sympathetic tone may be one of the most fundamental and functionally important aspects of this state.
All of the above-mentioned EEG, EMG, and autonomic phenomena can be readily explained in terms of changes in neuronal activity. Thus, the neocortical EEG desynchrony results from the asynchronous activity of thalamocortical projection neurons. The change in thalamic activity produces a change from synchronized rhythmic activity in adjacent cortical neurons, at approximately the frequency observed in surface electrodes, to a pattern of desynchronized activity with long bursts and pauses in unit discharge. Unit activity rate does not change in all cortical regions from NREM sleep to REM sleep, but the pattern changes dramatically (Evarts, 1964). During NREM sleep, the irregular, behavior-dependent, waking discharge patterns change to a regular burst pause pattern. The summed excitatory postsynaptic potentials (EPSPs) and inhibitory postsynaptic potentials (IPSPs) underlying this discharge produce the EEG spindles (Steriade and Llinas, 1988) and slowwaves of this state.
The loss of activity in antigravity muscles results from a cessation of discharge in the motoneurons supplying these muscles. Intracellular recordings have demonstratecl that this cessation results from a hyperpolarization of the motoneurons. This hyperpolarization occurs only in REM sleep and is thought to result from activity in brainstem cells projecting to motoneuron pools and inhibitory spinal interneurons (Chase and Morales, 1989).
WHERE IS REM SLEEP GENERATED?
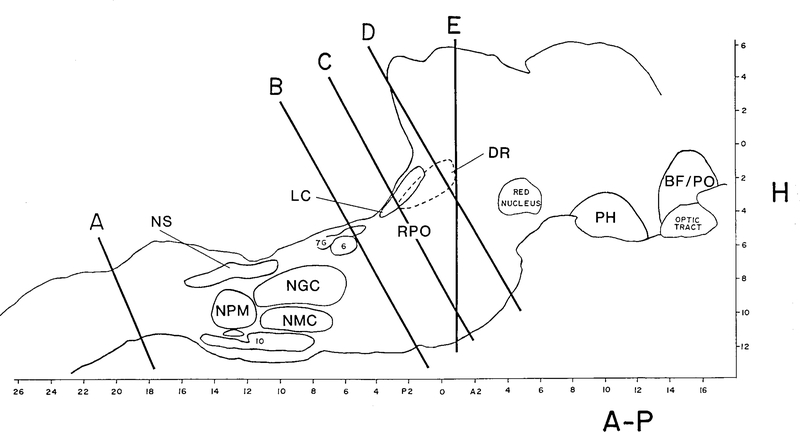
One can cut through the midbrain in the coronal plane, so as to separate the brainstem from the diencephalon and telencephalic structures. Animals with such lesions manifest a striking dissociation between polygraphically defined states in the forebrain and brainstem, i.e., by transecting the neuraxis, two independent generators of behavioral state are created, one rostral and one caudal to the transection. When transections are placed at levels D or E in Fig. 1, all the brainstem signs of REM sleep can be recorded caudal to the cut. Thus, atonia, rapid eye movements, and PGO spike bursts, as well as a REM sleep-like activation of reticular formation units, occur in a regular ultradian rhythm (Jouvet, 1962; Villablanca, 1966; Pompeiano and Hoshino, 1976).
FIG. 1.
Key cell groups studied in relation to sleep control are drawn on a sagittal outline of the cat brain. Abbreviations: BF/PO, basal forebrain/ preoptic region; PH, posterior hypothalamus; DR, dorsal raphe; RPO, nucleus reticularis pontis oralis; LC, locus ceruleus; 6, abducens nucleus; 7G, genu of the seventh nerve; NGC, nucleus gigantocellularis; NMC, nucleus magnocellularis; NPM, nucleus paramedianus; NS, nucleus solitarius.
The forebrain of animals with transections at levels D and E (Fig. 1) shows both synchronized and desynchronized states that alternate spontaneously (Villablanca, 1965). During desynchronized states, vertical pursuit eye movements and changes in pupil diameter can be evoked by external visual stimuli. The stereotyped pattern of spontaneous rapid eye movements with myosis that characterizes REM sleep is not present (Batini et al., 1958; Villablanca, 1965). Therefore, the desynchronized state seen in the rostral portion of these preparations closely resembles wakefulness.
Because of the presence of REM sleep caudal to midbrain transections and the absence of REM sleep signs rostral to such transections, one may conclude that structures rostral to the midbrain are not required for REM sleep and that structures caudal to the midbrain contain neurons that are sufficient to generate REM sleep.
Transection at the junction of the spinal cord and medulla (Fig. 1, level A) does not prevent all of the signs of REM sleep from occurring rostral to the cut (Adey et al., 1968; Puizillout et al., 1974). Thus, spinal mechanisms are not essential for the generation of REM sleep.
From the above we may conclude that structures caudal to the midbrain and rostral to the spinal cord are necessary for REM sleep.
We have carried this technique one step further by transecting between the medulla and pons and maintaining the animals for extended periods to allow the fullest possible recovery from the transection (Fig. 1B) (Siegel et al., 1986). As was the case with midbrain sections, the brain regions rostral and caudal to the cut produce independent, physiologically defined states. The medulla cycles regularly between an activated state and a quiescent state. The activated state is characterized by high levels of muscle tone identical to those seen in active waking and by accelerated respiration and heart rate. The quiescent state is characterized by lower levels of muscle tone, resembling those seen in NREM sleep, and slow regular respiration. Periods of muscle atonia are not seen after transections at the pontomedullary junction. Unit activity in the medial medulla of the medullary animal during the quiescent state resembles that seen in this region in NREM sleep, i.e., it is slow and regular. Thus, the respiratory regularity, the low level of muscle tone, the lack of eye movements, and the unit activity are similar to the conditions of NREM sleep. This indicates either that medullary regions, such as the nucleus of the solitary tract, are capable of generating the medullary signs of NREM sleep in the absence of rostral regions, or that the isolated medulla does not require any active hypnogenic influence to produce the physiological signs of NREM sleep. In the medullary cat, medial medullary unit activity during the activated state increases, as it does in waking in the intact animal. However, medial medullary neurons do not show the characteristic burst–pause discharge pattern seen in REM sleep. Therefore, the medulla and spinal cord, disconnected from rostral structures, show spontaneous variations in levels of arousal and NREM sleep-like states but do not show the medullary signs of REM sleep. Structures caudal to the pons are not sufficient to generate REM sleep.
A very different picture is seen in rostral structures after transection between the pons and medulla (Fig. 1, level B) (Siegel et al., 1984). Three states can be distinguished rostral to the transection. The first is an EEG-synchronized state without PGO spikes, resembling NREM sleep. Thus, both the medulla and forebrain show independent NREM sleep-like states after these transections. The second state is a desynchronized state without PGO spikes, resembling wakefulness. The third state is a desynchronized state with PGO spikes. The PGO activity occurs in irregular bursts and as isolated spikes in a manner very similar to that seen in REM sleep. Midbrain reticular units show irregular burst-pause patterns of discharge in conjunction with this third state, as they do in REM sleep (Siegel, 1985). There are, however, certain differences between this state and the REM sleep state seen in intact animals. In transected animals, the state may last for hours, compared to a maximum of 20–30 min in intact cats. Furthermore, while rapid eye movements often accompany the PGO bursts of this state, they may also be dissociated from them.
From the above one can see that when the pons is connected to midbrain and forebrain structures, most of the defining signs of REM sleep are seen in these rostral structures. When the pons is connected to the medulla and spinal cord, as in the midbrain decerebrate animal, most of the defining signs of REM sleep are seen in caudal structures. After all of these transections, NREM sleep-like states are seen on both sides of the transection.
One can then transect through the middle of the pons (Fig. 2, level C) and again ask the question, “Which side has REM sleep?” (Siegel et al., 1984, 1986). After this transection, the caudal pons and medulla shift between the aroused and quiescent states seen in the medullary animal (Siegel, 1985). No atonia or other signs of REM sleep are present. The rostral pons and forebrain show desynchronized, wakefulness-like states and synchronized NREM sleep-like states. The synchronized states may be accompanied by PGO spikes and PGO spike bursts, resembling those seen in NREM sleep and REM sleep transitions. However, midbrain unit activity is greatly decreased at these times, directly the opposite of the pattern seen in REM sleep in the intact animal. PGO spikes do not occur in the EEG-desynchronized state. Therefore, with this midpontine transection we have reached the limit of the transection technique. The major defining characteristics of the REM sleep state are absent on both sides of the transection, even in chronically maintained animals.
FIG. 2.
Coronal section of the feline pons shows the overlap of regions involved in REM sleep control. Coronal sections 3.1 and 4.0 mm caudal to stereotaxic zero. Abbreviations: BC, brachium conjunctivum; 5-M, motor nucleus of the trigeminal; PT, pyramidal tract. (Reproduced with permission from Siegel and Rogawski, 1988.)
Although the foregoing indicates that the pons is necessary for the generation of REM sleep-like states in both rostral and caudal structures, one may ask, “Is the pons in and of itself sufficient to generate the pontine aspects of REM sleep?” One can monitor REM sleep signs after transecting both rostral and caudal to the pons, producing an acute, isolated pons preparation (Matsuzaki, 1969) (Fig. 1, levels B and D). In this case, the pons continues to generate periodic episodes of rapid eye movements and PGO spikes in a pattern that, in the intact animal, is seen only in REM sleep. Neuronal activity has not been monitored in this preparation. However, the presence of PGO spikes and rapid eye movements in a REM sleep-like pattern is impressive evidence of pontine control of these basic aspects of REM sleep.
In an attempt to further localize the neurons generating REM sleep, a number of investigators have removed portions of the pons within the region defined as critical by transection studies. The first comprehensive study of this problem (Carli and Zanchetti, 1965) found that lesions that destroyed the bulk of the nucleus reticularis pontis oralis (RPO)—the designation for the rostral pontine reticular formation—permanently eliminated REM sleep. Further studies have concluded that the lateral rather than the medial portion of RPO is critical (Sastre et al., 1981; Drucker-Colin and Pedraza, 1983; Friedman and Jones, 1984). This small region might be critical either because it contains the somas of cells involved in REM sleep generation or because major axonal pathways transverse it. A recent study attempted to distinguish between these possibilities by using the cytotoxin kainic acid to remove cells in this region while doing minimal damage to axonal tracts (Webster and Jones, 1988). It was found that these lesions disrupted REM sleep. To summarize, the lateral regions of the RPO (L2-L4 in the cat), ventral to the locus ceruleus, is the brain region most critical for REM sleep. This very small area comprising just a few cubic millimeters of tissue apparently recruits the massive change in brain neuronal activity that is REM sleep.
Pontine lesions can produce the syndrome of REM sleep without atonia (Jouvet and Delorme, 1965; Henley and Morrison, 1974). Animals with these lesions have relatively normal NREM sleep. During sleep they have periods of desynchronized EEG, rapid eye movements, miosis, and PGO spikes as seen in normal REM sleep. However, muscle tone is present throughout these periods. The critical lesions for producing this effect are much smaller than those required to block the REM sleep state. Depending on the exact placement of the lesion (Hendricks et al., 1982), the animal’s motor activity during this state will range from a slight raising of the head to elaborate displays of exploratory, aggressive, and other behaviors. The animal remains generally unresponsive to the environment during these displays and can be “awakened” by strong stimulation. This syndrome also occurs in humans (Mahowald and Schenck, 1989), although many of these patients do not have neurological signs indicating gross brainstem lesions.
A loss of muscle tone can be evoked by injection of the cholinergic agonist carbachol or the cholinesterase inhibitor physostigmine into the dorsal pons. The region where injection produces the most immediate and complete loss of tone corresponds very well with the region that, when lesioned, produces REM sleep without atonia. Depending on the exact injection site, carbachol may evoke only atonia of the skeletal muscles without other signs of REM sleep. The animal may demonstrate perception of the outside environment by visually tracking stimuli with its extraocular muscles (Mitler and Dement, 1974; Katayama et al., 1984). Larger injections or injections at other pontine sites can produce the full REM sleep pattern (George et al., 1964; Baxter, 1969; Amatruda et al., 1975; Van Dongen et al., 1978; Baghdoyan et al., 1984; Shiromani et al., 1986). Studies in the decerebrate cat have demonstrated that the pontine atonia region can be activated by glutamate as well as carbachol (Lai and Siegel, 1988). Non-N-methyl-D-aspartate receptors mediate the glutamate effect (Lai and Siegel, 1988), whereas muscarinic M2 receptors mediate the cholinergic effect (Moctezuma et al., 1989).
A second area in which stimulation can elicit atonia is the medial medulla. Magoun and Rhines (1946) first reported that electrical stimulation of this area in the decerebrate cat produces an immediate loss of muscle tone. Recent studies (Lai and Siegel, 1988) have shown that glutamate stimulation of the nucleus magnocellularis and cholinergic stimulation of the nucleus paramedianus of the medial medulla will produce atonia. We hypothesize that these two distinct areas within the medial medulla mediate the atonia triggered in REM sleep by pontine activation. Lesions of these medial medulla cell groups have recently been shown to produce REM sleep without atonia (Schenkel and Siegel, 1989), as do lesions of the dorsolateral pons. Thus, stimulation and lesion data indicate the essential role of both pontine and medial medullary regions in the suppression of muscle tone in REM sleep.
UNIT RECORDING STUDIES
REM Sleep-on cells
Guided by lesion, stimulation, and anatomical data, researchers have recorded from the pons in order to observe the activity of neuronal elements that might be involved in REM sleep generation. The lateral pontine reticular formation (Sakai, 1980) and medial medulla (Siegel, 1979; Sakai, 1980) contain a population of cells that discharges at a high rate throughout REM sleep and that has little or no activity in NREM sleep. In wakefulness, these cells are generally silent, even during vigorous movement; however, some are active during head lowering and related postural changes that involve reductions of tone in a number of muscles (Siegel et al., 1979). The pontine REM sleep-on cells are distributed throughout the lateral pontine region implicated by lesion studies in REM sleep control (Sakai, 1980; Shiromani et al., 1987). This distribution is significant, since it indicates that the critical lesion does not merely interrupt fibers of passage in the critical area, but also removes the somas of cells that are selectively active in REM sleep. Figure 2 summarizes the current state of our knowledge about the anatomical relation of pontine mechanisms responsible for REM sleep and carbachol atonia, REM sleep-on and REM sleep-off cells, and lesions blocking REM sleep.
A recent paper reports that REM sleep-on cells in this lateral region are not cholinergic (Shiromani et al., 1987), although it is likely that they are cholinoceptive. Aminergic neurons are also not present in this region. Thus, the transmitter employed by these cells remains unknown. The medullary REM sleep-on cells are located in an area receiving projections from the pontine REM sleep-on region (Sakai et al., 1979).
Noradrenergic Cells of the Locus Ceruleus Complex and Serotonergic Cells of the Raphe System
Cells in both of these regions have a similar discharge pattern during the sleep–wake cycle. During wakefulness, discharge is relatively regular, in contrast to the burst–pause discharge pattern seen in most medial reticular neurons. During the initial stages of NREM sleep, these cells slow slightly. During the transition to REM sleep (defined in the cat as the time at which PGO spikes begin appearing), discharge in both serotonergic and noradrenergic cells slows dramatically. During REM sleep, these cells have their lowest discharge rates, and many are completely silent (Hobson et al., 1975, 1983; McGinty and Harper, 1976; Aston-Jones and Bloom, 1981; Jacobs et al., 1981). The significance of these unit activity patterns for REM sleep control is unclear. The slowing of discharge in these cells in NREM sleep argues against the hypothesis that increased release of serotonin or norepinephrine triggers NREM sleep. The minimal discharge rate of these cells in REM sleep also argues against the hypothesis that they are required for REM sleep (Siegel and Rogawski, 1988). The complete absence of discharge in REM sleep does suggest that these cells may have a role in gating, inhibiting, or disinhibiting some aspect of REM sleep.
We can summarize the present state of our knowledge about the localization of mechanisms generating REM sleep as follows. Transection studies have determined that the pons is sufficient to generate much of the phenomenology of REM sleep. Lesion studies have identified a small region in the lateral pontine tegmentum corresponding to lateral portions of the RPO and the region immediately ventral to the locus ceruleus, which is required for REM sleep. Unit recording studies have found a population of cells within this region that is selectively active in REM sleep. Whether this small region is sufficient for REM sleep generation, in the same sense that the suprachiasmatic nucleus is sufficient to generate a circadian signal (Kawamura and Inouye, 1979), is unknown. Nevertheless, it has become clear that much of the mechanism that drives this very complex behavioral state is localized to a very small portion of the brainstem. Having stated this, it should also be emphasized that, in the intact animal, many brain regions distant from the pons actively participate in the control of the REM sleep state. Obviously the phenomenology of REM sleep, such as muscle atonia, cortical desynchrony, rapid eye movements, alteration of sensory thresholds, and autonomic changes, require the recruitment of many brain systems. What is not always appreciated is the more subtle role of nonbrainstem systems in shaping REM sleep. Although the decerebrate animal has the basic brainstem physiology of REM sleep, closer inspection reveals substantial differences between the REM sleep of the isolated brainstem and the REM sleep of the intact animal. PGO spikes and associated eye movements in the decerebrate animal come in regular alternating clusters, distinct from the irregular pattern seen in the intact animal (Jouvet, 1962; Hoshino et al., 1976). Removal of the cerebellum, although not blocking REM sleep, alters the amplitude of PGO activity (Morrison and Bowker, 1975; Gadea-Ciria, 1976a). Lesions of the frontal cortex dramatically alter the amplitude and pattern of spiking (Gadea-Ciria, 1976b). The PGO spike drives the eye movements of REM sleep, which in humans are related to dream imagery (Dement and Kleitman, 1957; Roffwarg et al., 1962; Jacobs et al., 1972; Koulack, 1972). Therefore, one must not view the rest of the brain as merely as passive responder to a REM sleep state generated in the pons. Instead, present evidence suggests a dynamic interaction between forebrain and other systems in molding the structure and timing of PGO spikes, and in all likelihood the dream imagery of REM sleep.
WHAT IS THE FUNCTION OF REM SLEEP?
While our knowledge of mechanism has increased enormously over the last 20 years, the question of the function(s) of sleep remains in the realm of speculation, in stark contrast to that of other behavioral activities occupying substantially smaller amounts of time. Several long-standing theories have suggested that a primary function of NREM sleep may be to act as part of a system enforcing behavioral inactivity at inopportune times and facilitating metabolic energy conservation and thermoregulation (Zepelin and Rechtschaffen, 1974; Berger, 1975; Rechtschaffen et al., 1989). However, there is little consensus as to the function of REM sleep. We offer the following speculation.
The changes in brain unit activity during REM sleep should provide a clue to its function. In reviewing the neurophysiological findings on REM sleep, a seeming paradox emerges. There are two kinds of cells with unit activity changes unique to REM sleep: REM sleep-on and REM sleep-off cells. Convergent evidence from lesion and stimulation studies implicates the REM sleep-on cells of the lateral pontine reticular formation and medial medullary reticular formation in REM sleep generation. However, the dramatic cessation of activity in noradrenergic cells of the locus ceruleus, located immediately dorsal to the region critical for REM sleep, and in the serotonergic raphe system do not appear to be essential for REM sleep generation. We hypothesize that this cessation of activity may be significant for the function of REM sleep. Specifically, we propose that this periodic cessation of discharge prevents desensitization of norepinephrine and possibly 5-hydroxytoptamine receptors, which are continuously activated in wakefulness (Siegel and Rogawski, 1988; Siegel, 1989). Desensitization would reduce the effectiveness of these transmitters, which have the effect of increasing signal-to-noise ratio in neuronal information processing throughout the central nervous system. Therefore, the REM sleep-induced cessation of norepinephrine and serotonin release, by maintaining the optimal functioning of these receptors, would improve the organism’s ability to process information in wakefulness. One of the major features of REM sleep is the dramatic and complete loss of sympathetic tone. Like the cessation of locus ceruleus activity centrally, this loss of sympathetic activity would be expected to result in a reduction of norepinephrine release and up-regulation/prevention of desensitization of receptors peripherally. Thus, the receptor regulating role of REM sleep is hypothesized to operate peripherally as well as centrally. Indeed, the attenuation of sympathetic responsiveness centrally and peripherally may help account for the thermoregulatory disturbances that follow extended sleep deprivation (Bergmann et al., 1989; Rechtschaffen et al., 1989). By maintaining both central and peripheral receptor sensitivity within a narrow range, REM sleep would convey a distinct selective advantage.
Acknowledgment:
This work was supported by the Medical Research Service of the Veterans Administration, USPHS grants MH43811, NS 14610, and HL41370, and the American Narcolepsy Association.
REFERENCES
- Adey WR, Bors E, Porter RW. EEG sleep patterns after high cervical lesions in man. Arch Neurol 1968; 19:377–83. [DOI] [PubMed] [Google Scholar]
- Amatruda TT, Black DA, McCarley RW, Hobson JA, McKenna TM. Sleep cycle control and cholinergic mechanisms: differential effects of carbachol injections at pontine brainstem sites. Brain Res 1975;98:501–15. [DOI] [PubMed] [Google Scholar]
- Aserinsky E, Kleitman N. Regularly occurring periods of eye motility, and concomitant phenomena, during sleep. Science 1953;118:273–4. [DOI] [PubMed] [Google Scholar]
- Aston-Jones G, Bloom FE. Activity of norepinephrine-containing locus coeruleus neurons in behaving rats anticipates fluctuations in the sleep-waking cycle. J Neurosci 1981;8:876–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baghdoyan HA, Rodrigo-Angula ML, McCarley RW, Hobson JA Site-specific enhancement and suppression of desynchronized sleep signs following cholinergic stimulation of three brainstem regions. Brain Res 1984;306:39–52. [DOI] [PubMed] [Google Scholar]
- Batini C, Moruzzi G, Palestini M, Rossi GF, Zanchetti A Persistent patterns of wakefulness in the pretrigeminal midpontine preparation. Science 1958;128:30–2. [DOI] [PubMed] [Google Scholar]
- Batsel HL. Spontaneous desynchronization in the chronic cat “cerveau isole.” Arch Ital Biol 1964; 102: 547–66. [PubMed] [Google Scholar]
- Baust W, Boehmke J, Blossfeld U. Somato-sympathetic reflexes during natural sleep and wakefulness in unrestrained cats. Exp Brain Res 1971;12:361–9. [DOI] [PubMed] [Google Scholar]
- Baust W, Holzbach E, Zechlin O. Phasic changes in heart rate and respiration correlated with PGO-spike activity during REM sleep. Pflugers Arch 1972;331:113–23. [DOI] [PubMed] [Google Scholar]
- Baust W, Weidinger H, Kirchner F. Sympathetic activity during natural sleep and arousal. Arch Ital Biol 1968;106:379–90. [PubMed] [Google Scholar]
- Baxter BL. Induction of both emotional behavior and a novel form of REM sleep by chemical stimulation applied to cat mesencephalon. Exp Neurol 1969;23:220–9. [DOI] [PubMed] [Google Scholar]
- Berger RJ. Bioenergetic functions of sleep and activity rhythms and their possible relevance to aging. Fed Proc 1975;34:97–102 [PubMed] [Google Scholar]
- Bergmann BM, Everson CA, Kushida CA, Fang VS, Leitch CA, Schoeller DA, Refetoff S, Rechtschaffen A Sleep deprivation in the rat: V. Energy use and mediation. Sleep 1989;12:31–41. [DOI] [PubMed] [Google Scholar]
- Berlucchi G, Maffei L, Moruzzi G, Strata P. EEG and behavioral effects elicited by cooling of medulla and pons. Arch Ital Biol 1964;102:372–92. [PubMed] [Google Scholar]
- Carli G, Zanchetti A. A study of pontine lesions suppressing deep sleep in the cat. Arch Ital Biol 1965; 103:751–88. [PubMed] [Google Scholar]
- Celesia GG, Jasper HH. Acetylcholine released from cerebral cortex in relation to state of activation. Neurology 1966;16:1053–63. [DOI] [PubMed] [Google Scholar]
- Chase MH, Morales FR. The control of motoneurons during sleep. In: Kryger MH, Roth T, Dement WC, eds. Principles and practices of sleep medicine. Philadelphia: Saunders, 1989:74–85. [Google Scholar]
- Dement W, Kleitman N. The relation of eye movements during sleep to dream activity: an objective method for the study of dreaming. J Exp Psychol 1957;53:339–46. [DOI] [PubMed] [Google Scholar]
- Drucker-Colin R, Pedraza JGB. Kainic acid lesions of gigantocellular tegmental field (FTG) neurons do not abolish REM sleep. Brain Res 1983;272:387–91. [DOI] [PubMed] [Google Scholar]
- Eguchi K, Satoh T. Convergence of sleep-wakefulness subsystems onto single neurons in the region of cat’s solitary tract nucleus. Arch Ital Biol 1980; 118:331–45. [PubMed] [Google Scholar]
- Evarts EV. Temporal patterns of discharge of pyramidal tract neurons during sleep and waking in the monkey. J Neurophysiol 1964;27:152–71 [DOI] [PubMed] [Google Scholar]
- Friedman L, Jones BE. Computer graphics analysis of sleep-wakefulness state changes after pontine lesions. Brain Res Bull 1984;13:53–8. [DOI] [PubMed] [Google Scholar]
- Gadea-Ciria M Cerebellar control of activity of the feline oculomotor system during paradoxical sleep. Exp Neurol 1976a;51:263–5. [DOI] [PubMed] [Google Scholar]
- Gadea-Ciria M Tele-encephalic versus cerebellar control upon ponto-gcniculo-occipital waves during paradoxical sleep in the cat. Experientia 1976b;32:889–90. [DOI] [PubMed] [Google Scholar]
- George R, Haslett WL, Jeden DJ. A cholinergic mechanism in the brainstem reticular formation: induction of paradoxical sleep. Int J Neuropharmacol 1964;3:541–52. [DOI] [PubMed] [Google Scholar]
- Harper RM, Frysinger RC, Zhang J, Trelease RB, Terreberry RR. Cardiac and respiratory interactions maintaining homeostasis during sleep. In: Lydic R, Biebuyck JF, eds. Clinical physiology of sleep. Bethesda: American Physiological Society, 1988:67–78 [Google Scholar]
- Hendricks JC, Morrison AR, Mann GL. Different behaviors during paradoxical sleep without atonia depend on pontine lesion site. Brain Res 1982;239:81–105. [DOI] [PubMed] [Google Scholar]
- Henley K, Morrison AR. A re-evaluation of the effects of lesions of the pontine tegmentum and locus coeruleus on phenomena of paradoxical sleep in the cat. Acta Neurobiol Exp 1974;34:215–32. [PubMed] [Google Scholar]
- Hobson JA, Alexander J, Frederickson CJ. The effect of lateral geniculate lesions on phasic electrical activity of the cortex during desynchronized sleep in the cat. Brain Res 1969;14:607–21. [DOI] [PubMed] [Google Scholar]
- Hobson JA, McCarley RW, Nelson JP. Location and spike-train characteristics of cells in anterodorsal pons having selective decreases in firing rate during desynchronized sleep. J Neurophysiol 1983;50: 770–83. [DOI] [PubMed] [Google Scholar]
- Hobson JA, McCarley RW, Wyzinski PW. Sleep cycle oscillation: reciprocal discharge by two brainstem neuronal groups. Science 1975;189:55–8. [DOI] [PubMed] [Google Scholar]
- Hoshino K, Pompeiano O, Magherini PC, Mergner T. Oscillatory activity of pontine neurons related to the regular occurrence of REM bursts in the decerebrate cat. Brain Res 1976;116: 125–30. [DOI] [PubMed] [Google Scholar]
- Jacobs BL, Heym J, Trulson ME. Behavioral and physiological correlates of brain serotonergic unit activity. J Physiol (Pans) 1981;77:431–6. [PubMed] [Google Scholar]
- Jacobs L, Feldman M, Bender MB. Are the eye movements of dreaming sleep related to the visual images of the dreams? Psychophysiology 1972;9:393–401. [DOI] [PubMed] [Google Scholar]
- Jones BE, Beaudet A Distribution of acetylcholine and catecholamine neurons in the cat brainstem: a choline acetyltransferase and tyrosine hydroxylase immunohistochemical study. J Comp Neurol 1987;261:15–32. [DOI] [PubMed] [Google Scholar]
- Jouvet M Recherches sur les structures nerveuses et les mechanismes responsables des differentes phases du sommeil physiologique. Arch Ital Biol 1962;100: 125–206. [PubMed] [Google Scholar]
- Jouvet M, Delorme F. Locus coeruleus et sommeil paradoxal. CR Soc Biol 1965;159:895–9. [Google Scholar]
- Jouvet M, Denoyer M, Kitahama K, Sallanon M. Slow wave sleep and indolamines: a hypothalamic target. In: Wauquier A, ed. Slow wave sleep: physiological, pathophysiological and functional aspects. New York: Raven Press, 1989:91–108. [Google Scholar]
- Kaitin KI. Preoptic area unit activity during sleep and wakefulness in the cat. Exp Neurol 1984;83:347–57. [DOI] [PubMed] [Google Scholar]
- Kanai T, Szerb JC. Mesencephalic reticular activating system and cortical acetylcholine output. Nature 1965;205:80. [DOI] [PubMed] [Google Scholar]
- Katayama Y, DeWitt DS, Becker DP, Hayes RL. Behavioral evidence for cholinoceptive pontine inhibitory area: descending control of spinal motor output and sensory input. Brain Res 1984;296: 241–62. [DOI] [PubMed] [Google Scholar]
- Kawamura H, Inouye ST. Circadian rhythm in a hypothalamic island containing the suprachiasmatic nucleus. In: Suda M, Hayaishi O, Nakagawa H, eds. Biological rhythms and their central mechanism. Amsterdam: North-Holland Biomedical Press, 1979:335–41. [Google Scholar]
- Kennedy C, Gillin JC, Mendelson W, Suda S, Miyaoka M, Ito M, Nakamura RK, Storch Fl. Local cerebral glucose utilization in non-rapid eye movement sleep. Nature 1982;297:325–7. [DOI] [PubMed] [Google Scholar]
- Klein M, Michel F, Jouvet M. Etude polygraphique du sommeil chez les oiseaux. CR Soc Biol 1964; 158: 99–103. [PubMed] [Google Scholar]
- Koulak D Rapid eye movements and visual imagery during sleep. Psychol Bull 1972;78:155–8. [DOI] [PubMed] [Google Scholar]
- Lai YY, Siegel JM. Medullary regions mediating atonia. J Neurosci 1988;8:4790–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent JP, Guerrero FA Reversible suppression of ponto-geniculo-occipital waves by localized cooling during paradoxical sleep in cats. Exp Neurol 1975;49:356–69. [DOI] [PubMed] [Google Scholar]
- Lin JS, Sakai K, Vanni-Mercier G, Jouvet M. A critical role of the posterior hypothalamus in the mechanisms of wakefulness determined by microinjection of muscimol in freely moving cats. Brain Res 1989;479:225–40 [DOI] [PubMed] [Google Scholar]
- Lindsley DB, Bowden JW, Magoun HW. Effect upon the EEG of acute injury to the brain stem activating system. Electroencephalogr Clin Neurophysiol 1949;1:475–86. [PubMed] [Google Scholar]
- Lindsley DB, Schreiner LH, Knowles WB, Magoun HW. Behavioral and EEG changes following chronic brain stem lesions in the cat. Electroencephalogr Clin Neurophysiol 1950;2:483–98. [DOI] [PubMed] [Google Scholar]
- Magnes J, Moruzzi G, Pompeiano O. Synchronization of the EEG produced by low-frequency electrical stimulation of the region of the solitary tract. Arch Ital Biol 1961;99:33–67. [Google Scholar]
- Magoun HW, Rhines R. An inhibitory mechanism in the bulbar reticular formation. .J Neurophysiol 1946;9:165–71. [DOI] [PubMed] [Google Scholar]
- Mahowald MW, Schenck CH. REM sleep behavior disorder, In: Kryger MH, Roth T, Dement WC, eds. Principles and practice of sleep medicine. Philadelphia: Saunders, 1989:389–401. [Google Scholar]
- Matsuzaki M Differential effects of sodium butyrate and physostigmine upon the activities of parasleep in acute brain stem preparations. Brain Res 1969;13:247–65- [DOI] [PubMed] [Google Scholar]
- McGinty DJ, Harper RM. Dorsal raphe neurons: depression of firing during sleep in cats. Brain Res 1976;101:569–75. [DOI] [PubMed] [Google Scholar]
- McGinty DJ, Sterman MB. Sleep suppression after basal forebrain lesions in the cat. Science 1968; 160: 1253–5. [DOI] [PubMed] [Google Scholar]
- McGinty D, Szymusiak R. Discharge of pedunculopontine area neurons related to PGO waves. Sleep Res 1988:17 [Google Scholar]
- Meyer J, Ishikawa Y, Hata T, Karacan I. Cerebral blood flow in normal and abnormal sleep and dreaming. Brain Cogn 1987;6:266–94. [DOI] [PubMed] [Google Scholar]
- Mitler MM, Dement WC. Cataplectic-like behavior in cats after micro-injection of carbachol in the pontine reticular formation. Brain Res 1974;68:335–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moctezuma JV, Gillin JC, Shiromani PJ. The effects of M1 and M2 muscarinic receptor agonists on REM sleep. Sleep Res 1989; 18:25. [DOI] [PubMed] [Google Scholar]
- Morrison AR, Bowker RM. The biological significance of PGO spikes in the sleeping cat. Acta Neurobiol Exp 1975;35:821–40. [PubMed] [Google Scholar]
- Nauta WJH. Hypothalamic regulation of sleep in rats: an experimental study. J Neurophysiol 1946;9: 285–316. [DOI] [PubMed] [Google Scholar]
- Orem J Neuronal mechanisms of respiration in REM sleep. Sleep 1980;3:251–67 [DOI] [PubMed] [Google Scholar]
- Pare D, Smith Y, Parent A, Steriade M. Projections of brainstem core cholinergic and non-cholinergic neurons of cat to intralaminar and reticular thalamic nuclei. Exp Brain Res 1988; 70:166–80. [DOI] [PubMed] [Google Scholar]
- Parmeggiani PL Thermoregulation during sleep from the viewpoint of homeostasis. In: Lydic R, Biebuyck JF, eds. Clinical physiology of sleep. Bethesda: American Physiological Society, 1988:159–69. [Google Scholar]
- Phillipson EA. Control of breathing during sleep. Am Rev Respr Dis 1978;118:909–39. [DOI] [PubMed] [Google Scholar]
- Pivik RT, Circar S, Braun C. Nuchal muscle tonus during sleep, wakefulness and tonic immobility in the rabbit. Physiol Behav 1981;26:13–20. [DOI] [PubMed] [Google Scholar]
- Pompeiano O, Hoshino K. Tonic inhibition of dorsal pontine neurons during the postural atonia produced by an anticholinesterase in the decerebrate cat. Arch Ital Biol 1976; 114:310–40. [PubMed] [Google Scholar]
- Puizillout JJ, Foutz AS. Characteristics of the experimental reflex sleep induced by vago-aortic nerve stimulation. Electroencephalogr Clin Neurophysiol 1977;42:552–63. [DOI] [PubMed] [Google Scholar]
- Puizillout JJ, Ternaux JP, Foutz AS, Fernandez G. Les stades de sommeil de la preparation “encephale isole”: I. Declenchement des pointes ponto-geniculo-occipitales et du sommeil phasique a ondes lentes. Role des noyaux du raphe. Electroencephalogr Clin Neurophysiol 1974;37:561–76. [DOI] [PubMed] [Google Scholar]
- Pujol JF, Buguet A, Froment JL, Jones B, Jouvet M. The central metabolism of serotonin in the cat during insomnia. A neurophysiological and biochemical study after administration of p-cholorphenylalanine or destruction of the raphe system. Brain Res 1971;29:195–212. [DOI] [PubMed] [Google Scholar]
- Ramm P, Frost BJ. Cerebral and local cerebral metabolism in the cat during slow wave and REM sleep. Brain Res 1986;365:112–24 [DOI] [PubMed] [Google Scholar]
- Ranson SW. Somnolence caused by hypothalamic lesion in the monkey. Arch Neurol Psychiatry 1939; 41:1–23. [Google Scholar]
- Rechtschaffen A, Bergmann BM, Everson CA, Kushida CA, Gilliand MA Sleep deprivation in the rat: X Integration and discussion of the findings. Sleep 1989;12:68–87. [PubMed] [Google Scholar]
- Rechtschaffen A, Kales AA manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Public Health Service. Washington, DC: U.S. Government Printing Office, 1968. [Google Scholar]
- Reiner PB. Correlational analysis of central noradrenergic neuronal activity and sympathetic tone in behaving cats. Brain Res 1986;378:86–96. [DOI] [PubMed] [Google Scholar]
- Roffwarg HP, Dement WC, Muzio JN, Fisher C. Dream imagery: relationship to rapid eye movements of sleep. Arch Gen Psychiatry 1962;1:235–58. [DOI] [PubMed] [Google Scholar]
- Sakai F, Meyer JS, Karajan I, Yamaguchi F, Yamamoto M. Narcolepsy: regional cerebral blood flow during sleep and wakefulness. Neurology 1979;29:61–7. [DOI] [PubMed] [Google Scholar]
- Sakai K Some anatomical and physiological properties of ponto-mesencephalic tegmental neurons with special reference to the PGO waves and postural atonia during paradoxical sleep in the cat. In: Hobson JA, Brazier MA, eds. The reticular formation revisited. New York: Raven Press, 1980: 427–47. [Google Scholar]
- Sakai K, Petitjean F, Jouvct M. Effects of ponto-mesencephalic lesions and electrical stimulation upon PGO waves and EMPs in unancsthetized cats. Electroencephalogr Clin Neurophysiol 1976;41:49–63. [DOI] [PubMed] [Google Scholar]
- Sastre JP, Sakai K, Jouvet M. Are the gigantocellular tegmental field neurons responsible for paradoxical sleep? Brain Res 1981;229:147–61. [DOI] [PubMed] [Google Scholar]
- Schenkel E, Siegel JM. REM sleep without atonia after lesions of the medial medulla. Neurosci Lett 1989; 98:159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiromani PJ, Armstrong DM, Berkowitz A, Jeste DV, Gillin JC. Distribution of choline acetyltransferase immunoreactive somata in the feline brainstem: implications for REM sleep generation. Sleep 1988;11:1–16 [DOI] [PubMed] [Google Scholar]
- Shiromani PJ, Armstrong DM, Bruce G, Hersh LB, Groves PJ, Gillin C. Relation of pontine choline acetyltransferase immunoreactive neurons with cells which increase discharge during REM sleep. Brain Res Bull 1987;18:447–55 [DOI] [PubMed] [Google Scholar]
- Shiromani P, Siegel JM, Tomaszewski KS, McGinty DJ. Alterations in blood pressure and REM sleep after pontine carbachol microinfusion. Exp Neurol 1986;91:285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shute CCD, Lewis PR. The ascending cholinergic reticular system: neocortical, olfactory and subcortical projections. Brain 1967;90:497–520. [DOI] [PubMed] [Google Scholar]
- Siegel JM. Behavioral functions of the reticular formation. Brain Res Rev 1979;1:69–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JM. Pontomedullary interactions in the generation of REM sleep. In: McGinty DJ, Drucker-Colin R, Morrison A, Parmeggiani PL, eds. Brain mechanisms of sleep. New York: Raven Press, 1985:157–74. [Google Scholar]
- Siegel JM. Brainstem mechanisms generating REM sleep. In: Kryger MK, ed, Principles and practice of sleep medicine. Philadelphia: Saunders, 1989:104–20. [Google Scholar]
- Siegel JM, Nienhuis R, Tomaszewski KS. REM sleep signs rostral to chronic transections at the pontomedullary junction. Neurosci Lett 1984;45:241–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JM, Rogawski MA. A function for REM sleep: regulation of noradrenergic receptor sensitivity. Brain Res Rev 1988;13:213–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JM, Tomaszewski KS, Nienhuis R.. Behavioral states in the chronic medullary and mid-pontine cat. Electroencephalogr Clin Neurophysiol 1986;63:274–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JM, Wheeler RL, McGinty DJ. Activity of medullary reticular formation neurons in the unrestrained cat during waking and sleep. Brain Res 1979; 179:49–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith OA. Sleep and other behavioral states reflected in cardiovascular response patterns. In: Lydic R, Biebuyck JF, eds. Clinical physiology of sleep. Bethesda: American Physiological Society, 1988:53–65. [Google Scholar]
- Steriade M Brain electrical activity and sensory processing during waking and sleep states. In: Kryger MH, Roth T, Dement WC, eds. Principles and practice of sleep medicine. Philadelphia: Saunders, 1989: 86–103. [Google Scholar]
- Steriade M, Llinas RR. The functional states of the thalamus and the associated neuronal interplay. Physiol Rev 1988;68:649–742 [DOI] [PubMed] [Google Scholar]
- Steriade M, Pare D, Parent A, Smith Y. Projections of cholinergic and non-cholinergic neurons of the brainstem core to relay and associational thalamic nuclei in the cat and macaque monkey. Neuroscience 1988;25:69–86 [DOI] [PubMed] [Google Scholar]
- Sterman MB, Clemente CD. Forebrain inhibitory mechanisms: sleep patterns induced by basal forebrain stimulation in the behaving cat. Exp Neurol 1962;6:103–17 [DOI] [PubMed] [Google Scholar]
- Szymusiak R, McGinty DJ. Sleep-related neuronal discharge in the basal forebrain of cats. Brain Res 1986;370:82–92 [DOI] [PubMed] [Google Scholar]
- Tradardi V Sleep in the pigeon. Arch Ital Biol 1966;104:516–21. [PubMed] [Google Scholar]
- Ursin R, Sterman MB. An manual for standardized scoring ofsleep and waking states in the adult cat. Brain Information Service/Brain Research Institute. Los Angeles: University of California, 1981. [Google Scholar]
- Van Dongen PAM, Broekkamp CLE, Cools AR. Atonia after carbachol microinjections near the locus coeruleus in cats. Phannacol Biochem Behav 1978;8:527–32. [DOI] [PubMed] [Google Scholar]
- Vanderwolf CH, Robinson TE. Reticulo-cortical activity and behavior: a critique of the arousal theory and a new synthesis. Behav Brain Sci 1981;4:459–514. [Google Scholar]
- Vanni-Mercier G, Sakay K, Salvert D, Jouvet M. Waking-state specific neurons in the posterior hypothalamus of cat. In: Koella WP, Ruther E, Schulz H, eds. Sleep. New York: Gustav Fisher Verlag, 1985:238–40. [Google Scholar]
- Villablanca J The electrocorticogram in the chronic cerveau isole cat. Electroencephalogr Clin Neurophysiol 1965;19:576–86 [DOI] [PubMed] [Google Scholar]
- Villablanca J Behavioral and polygraphic study of “sleep” and “wakefulness” in chronic deccrebrate cats. Electroencephalogr Clin Neurophysiol 1966;21:562–77. [DOI] [PubMed] [Google Scholar]
- Vincent SR, Reiner PB. The immunohistochemical localization of choline acetyltransferase in the cat brain. Brain Res Bull 1987;18:371–415 [DOI] [PubMed] [Google Scholar]
- von-Economo C Die encephalitis lethargica. Wien: Deuticke, 1918. [Google Scholar]
- Webster HH, Jones BE. Neurotoxic lesions of the dorsolateral pontomescncephalic tegmentum-cholinergic cell area in the cat. Il. Effects upon sleep-waking states. Brain Res 1988;458:285–302. [DOI] [PubMed] [Google Scholar]
- Zepelin H, Rechtschaffen A Mammalian sleep, longevity and energy metabolism. Brain Behav Evol 1974;10:425–70. [DOI] [PubMed] [Google Scholar]