Abstract
Background
Long course radiotherapy plus neoadjuvant chemotherapy followed by resection (total mesorectal excision, TME) has accepted widespread recognized in the treatment of locally advanced rectal cancer (LARC). Tislelizumab, an anti-PD1 humanized IgG4 monoclonal antibody, has been demonstrated with clinical activity and is approved for treating recurrent/refractory classical Hodgkin lymphoma and locally advanced/metastatic urothelial carcinoma in China. However, the safety and efficacy of long course (neoadjuvant chemoradiotherapy, NCRT) plus tislelizumab followed by TME for LARC is still uncertain.
Methods
This NCRT-PD1-LARC trial will be a prospective, multicenter and phase II clinical trial designed to evaluate the safety and efficacy of LARC patients treated with long course NCRT plus tislelizumab followed by TME. This trial will consecutively enroll 50 stage II/III LARC patients (cT3N0M0 and cT1-3N1-2M0) with the tumor distal location ≤ 7 cm from anal verge at 7 centers in China. The enrolled patients will receive long course radiotherapy (50 Gy/25 f, 2 Gy/f, 5 days/week) and three 21-day cycles capecitabine (1000 mg/m2, bid, po, day1-14) plus three 21-day cycles tislelizumab (200 mg, iv.gtt, day8), followed by TME 6–8 weeks after the end of radiotherapy. The primary efficacy endpoint will be the pathological complete response (pCR) rate, which is defined as absence of viable tumor cells in the primary tumor and lymph nodes.
Discussion
To our knowledge, this trial is the first multicenter clinical trial in China to assess the safety and efficacy of NCRT plus anti-PD1 therapy followed by TME to treat patients with LARC. NCRT followed by TME was recognized as the most recommended treatment against LARC while could not be completely satisfied in clinic. This study expects to provide a solid basis and encouraging outcomes for this promising combination of radiotherapy, chemotherapy and immunotherapy in LARC.
Trial registration
Name of the registry: ClinicalTrials.gov. Trial registration number: NCT04911517. Date of registration: 23 May 2021. URL of trial registry record: https://www.clinicaltrials.gov/ct2/show/NCT04911517?id=BFH-NCRTPD&draw=2&rank=1.
Background
Rectal cancer is one of the most common digestive malignant tumors in China [1, 2]. There are 253,000 new cases in China every year, accounting for 18.6% of the world [3]. With the improvement of lifestyle and living standard, the incidence rate of rectal cancer is still increasing by [4, 5]. Because of the insidious incidence and inapparent early clinical symptoms of rectal cancer, about 75% of the clinically diagnosed patients in China have been in the middle and late stage, some of them even lose the opportunity of surgery [6, 7]. Among them, low rectal cancer (the tumor distal location ≤ 7 cm from anal verge) accounted for most cases with poor quality of life because of the closer distance from the anus and lower anus preservation rate [8, 9].
At present, the standard treatment for the locally advanced rectal cancer (LARC) consisting of neoadjuvant chemoradiotherapy (NCRT) followed by total mesorectal excision (TME). Such therapeutic schedule not only can improve compliance to treatment and reduce toxicity, but also increase the rate of anus preservation and R0 resection to approach lower local recurrence rate [10, 11]. Therefore, the National Comprehensive Cancer Network (NCCN) guidelines preferred NCRT followed by TME for the treatment of LARC [12, 13]. However, the pathological complete response (pCR) rate of NCRT treating LARC patients is about 11%—15%, which is still expected to increase [14, 15]. Additionally, the overall survival (OS) rate of NCRT is not significantly higher than that of postoperative adjuvant chemotherapy according to some clinical trials [16, 17]. Consequently, novel treatment to improve the long-term survival rate of LARC is in the immediate needs.
The programmed cell death 1 (PD1) mediates immunosuppression by acting as a key immune-checkpoint receptor, while programmed cell death ligand 1 (PDL1) can engage PD1 resulting in anergy and apoptosis of T cells [18, 19] Inhibition of the interaction between PD1 and PDL1 can enhance T-cell responses further mediate antitumor activity. Based on DNA mutation pattern, colorectal cancer (CRC) consists of deficient mismatch repair (dMMR) and proficient mismatch repair (pMMR) [20, 21]. According to some clinical trials, PD-1/PD-L1 inhibitors could obtain good therapeutic effect in dMMR CRC patients and has been approved for treating dMMR CRC in clinic by the Food and Drug Administration (FDA) [22–24]. However, limited to lower proportion of dMMR (about 15%), the effectiveness of PD-1/PD-L1 inhibitors treating CRC especially LARC is still uncertain. Interestingly, radiotherapy was found to enlarge the anti-PD1/PDL1 treatment effect by promoting different links in the immune response such as activation and recruitment of T cells, promotion of dendritic cells maturation, antigen exposure and upregulation of major histocompatibility complex molecules [25, 26]. In addition, radiotherapy can also reduce tumor burden and reinvigorate exhausted T cells to strengthen the anti-PD1/PDL1 therapeutic efficacy [27, 28]. Therefore, the combination of anti-PD1 with NCRT might lead to improvement in local remission and survival in LARC.
Taking the consideration above, such NCRT-PD1-LARC phase II trial combines NCRT with tislelizumab, an anti-PD1 humanized IgG4 monoclonal antibody, to assess the safety and efficacy of this therapeutic plan for LARC patients.
Methods
Study design
This NCRT-PD1-LARC trial (Clinical trial number: NCT04911517) will be a prospective, multicenter, single-arm phase II clinical trial to evaluate the safety and efficacy of LARC patients treated with long course neoadjuvant chemoradiotherapy plus tislelizumab followed by TME.
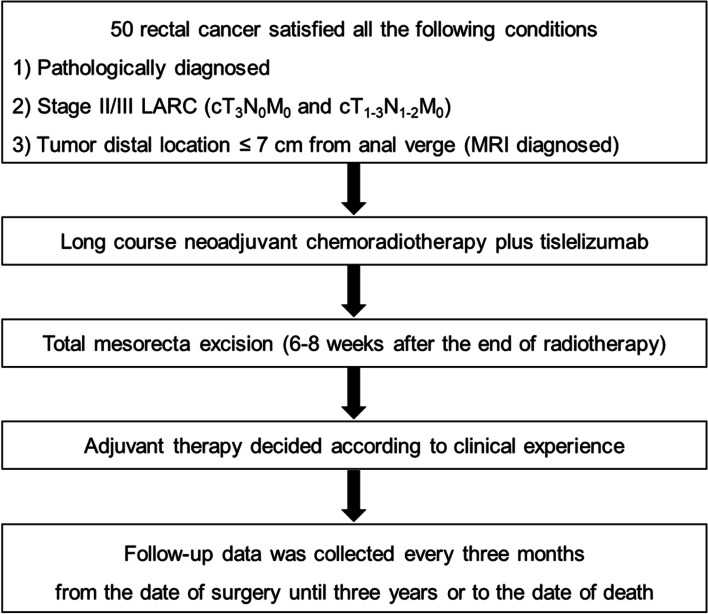
This trial will enroll 50 patients with pathologically diagnosed LARC at 7 centers in China. This study will be in progress abide by the principles of the Declaration of Helsinki. Ethics committee of Beijing Friendship Hospital, Capital Medical University has approved the study protocol on March 30, 2021 (Approval number: 2021-P2-110–01). All enrolled patients or their designated agents will sign the informed consent. Moreover, all enrolled patients will understand the significance, methods of the study and the obligation to cooperate with the follow-up. All clinical data for each patient will be collected during visits. The flow chart of this trial is illustrated in Fig. 1.
Fig. 1.
Study flow chart. (LARC, locally advanced rectal cancer; MRI, magnetic resonance imaging.)
Patient population
Consecutive patients aged ≥ 18 years who diagnosed as LARC (cT3N0M0 and cT1-3N1-2M0) with the tumor distal location ≤ 7 cm from anal verge (determined by MRI scan) will be eligible for inclusion in this study. The major exclusion criteria are congenital or acquired immune deficiency and present or previous active malignancies (except the diagnosis of rectal cancer this time). Detailed inclusion and exclusion criteria are shown in Table 1.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria: |
| 1. Patients have been fully aware of the content of this study and signed the informed consent voluntarily; |
| 2. Patients with rectal cancers must satisfied all the following conditions: |
| 1) Stage II/III LARC (cT1-3N1-2M0); |
| 2) Tumor distal location ≤ 7 cm from anal verge (MRI diagnosed); |
| 3. Patients regardless of gender with aged ≥ 18 years and ECOG score of 0 or 1; |
| 4. Physical and viscera function of patients can withstand major abdominal surgery; |
| 5. Patients are willing and able to follow the study protocol during the study; |
| 6. Patients give consent to the use of blood and pathological specimens for study; |
| 7. Within 28 days prior to enrolment, we must confirm a negative serological pregnancy test for child-bearing age women and they agree to use effective contraception for the duration of drug use and for 60 days after the last dose |
| Exclusion criteria: |
| 1. Patients have a present or previous active malignancy except the diagnosis of rectal cancer this time; |
| 2. Patients underwent major surgery within 4 weeks prior to study treatment; |
| 3. Patients have any condition affects the absorption of capecitabine through gastrointestinal tract; |
| 4. Patients have severe uncontrolled recurrent infections, or other severe uncontrolled concomitant diseases; |
| 5. Patients who are allergic to any of the ingredients under study; |
| 6. Patients with severe concomitant diseases with estimated survival ≤ 5 years; |
| 7. Patients with present or previous moderate or severe liver and kidney damage presently or previously; |
| 8. Patients have received other study medications or any immunotherapy currently or in the past; |
| 9. Patients preparing for or previously received organ or bone marrow transplant; |
| 10. Patients who received immunosuppressive or systemic hormone therapy for immunosuppressive purposes within 1 month prior to the initiation of study therapy; |
| 11. Patients with congenital or acquired immune deficiency (such as HIV infection); |
| 12. If patients with a history of uncontrolled epilepsy, central nervous system disease or mental disorder, the investigator will determine whether the clinical severity prevents the signing of informed consent or affects the patient's oral medication compliance; |
| 13. Patients with other factors that may affect the study results or cause the study to be terminated midway, such as alcoholism, drug abuse, other serious diseases (including mental illness) requiring combined treatment and severe laboratory examination abnormalities |
| 14. Pregnant or lactating women |
LARC: locally advanced rectal cancer; MRI: magnetic resonance imaging; ECOG: Eastern Cooperative Oncology Group; HIV: human immunodeficiency virus
Therapeutic schedule
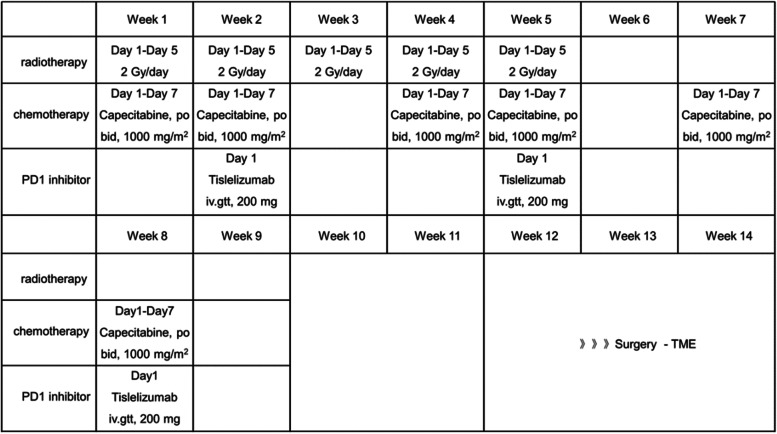
The enrolled patients will receive long course radiotherapy (50 Gy/25 f, 2 Gy/f, 5 days/week) in the first five weeks. As for chemotherapy and anti-PD1 therapy, the enrolled patients will be treated with three 21-day cycles capecitabine (1000 mg/m2, bid, po, day1-14) plus three 21-day cycles tislelizumab (200 mg, iv.gtt, day8) in the first nine weeks. Afterwards, patients will have two weeks of rest (week 10–11). While 6–8 weeks after the end of radiotherapy, patients will receive TME surgery to achieve the purpose of radical resection (week 12–14). Moreover, whether and how to use postoperative adjuvant chemotherapy will be determined according to clinical experience. The detailed therapeutic schedule and timeline is shown in Fig. 2.
Fig. 2.
Therapeutic timelines and schedule. (PD1, programmed cell death 1; TME, total mesorectal excision.)
Outcomes
The primary outcome of this NCRT-PD1-LARC trial is pCR rate. All the enrolled patients will receive TME surgery 6–8 weeks after the end of radiotherapy. The resected rectal specimens will be evaluated by the pathologists who are experienced on the rectal cancer diagnosis according to the 1997 Dworak grading system [29]. The pathological results will be classified into 5 grades, while grade 0–3 will be considered as non-pCR and grade 4 represent pCR. Such outcome will be measured after the surgery as soon as possible.
The secondary outcome including neoadjuvant rectal (NAR) score, objective response rate (ORR), R0 resection rate, anal preservation rate, 3-year local recurrence rate (LRR), 3-year disease free survival (DFS) and 3-year overall survival (OS). The NAR score is a predictive indicator of survival after preoperative chemoradiotherapy for rectal cancer, which will be calculated according to the following formula in Fig. 3 [30]. ORR is evaluated according to Response Evaluation Criteria in Solid Tumors (RECIST) v1.1 [31]. The ORR rate is the result of complete response (CR) rate plus partial response (PR) rate. During the surgical process, surgeons will evaluate the level of cancer resection, which will be classified as R0, R1, R2 resection. The R0 resection rate will be calculated right after the surgery. Surgeons will decide whether the anal can be preserved based on the rectal cancer and intraoperative situation during the surgery. The anal preservation rate is the percentage of patients who achieve anal preservation. Additionally, the 3-year LRR, 3-year DFS and 3-year OS will be calculated after the 3-year follow-up finished.
Fig. 3.
Calculation formula of the NAR score. (NAR, neoadjuvant rectal; pN, pathologic nodal stage; cT, clinical tumor stage; pT, pathologic tumor stage.)
Adverse event
The adverse event management of this trail will strictly abide by the consensus recommendations from the Society for Immunotherapy of Cancer (SITC) toxicity management working group including dermatologic, gastroenterological, endocrine, pulmonary, rheumatologic, musculoskeletal, infusion reactions, cardiovascular, hematologic, renal, neurologic and ophthalmologic events [32]. The incidence of adverse event, management of immune-related adverse events and detailed reasons of withhold/permanently discontinue will be recorded.
Follow up
Follow-up data was collected by professional researchers through telephone and regular outpatient visits. The follow-up period was calculated every 3 months in the first postoperative year and every 6 months after the first postoperative year from the date of surgery until three years or to the date of death.
Quality control
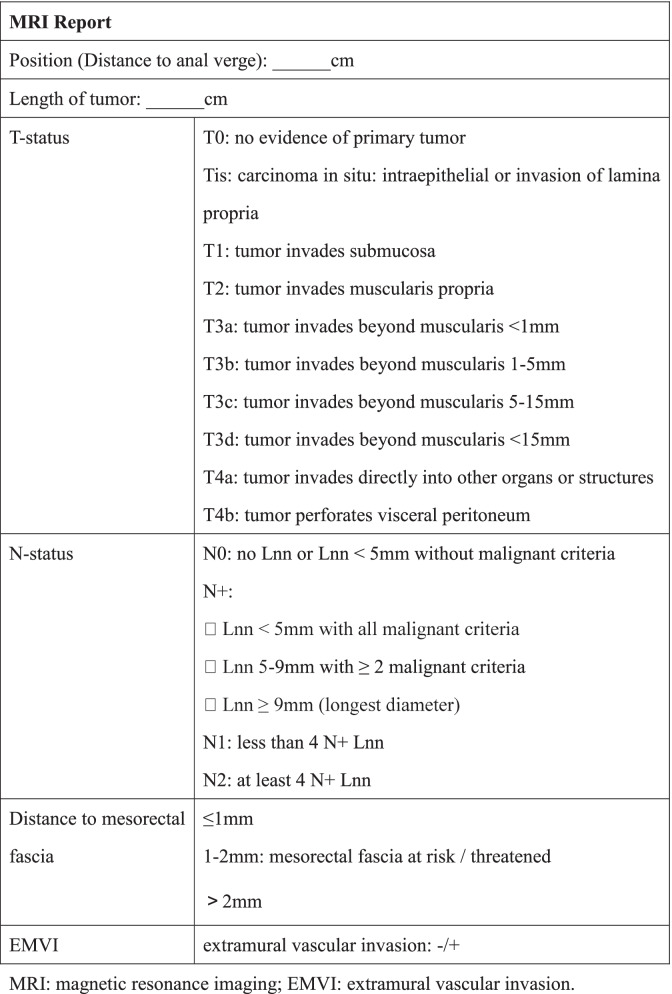
In order to ensure the accuracy of diagnosis of enrolled patients, all the MR images will be uploaded to the network data registration and read by two professional radiologists. Then they will issue the standardized report (Table 2).
Table 2.
Standardized MRI report
MRI magnetic resonance imaging, EMVI extramural vascular invasion
The operation is performed by experienced surgeons who should have at least 30 cases of TME experience. All the participating surgeons needs to submit unedited operative videos of at least 3 consecutive cases. Two independent reviewers will assess the surgical appearance. Additionally, the key steps of all operations should have operation records to query.
The fresh, unopened specimen will be sent to the pathologist and processed professionally after the operation. The site of the tumor will be sliced as thinly as possible (3-5 mm slices) including up to 2 cm above and below the tumor. We will collect all these slices of enrolled patients and submit them to a specific pathologist (Prof Guangyong Chen, one of the authors.) for a final report (Table 3). The standardized pathological report is made by us with reference to Standardized Pathology Report for Colorectal Cancer, 2nd Edition [33].
Table 3.
Standardized pathological report

DNA deoxyribo nucleic acid, MSI Microsatellite instability
The enrolled patients will be examined, treated and evaluated strictly according to this study protocol, while the obtained data will be recorded in the case report form. All forms must be completed, signed and dated by the person who filled in. The research supervisor will check the network database once a month to urge every center to complete the network data registration. If there is any missing data, the reason must be indicated. The follow-up will be completed by experienced professional follow-up personnel, while the collection of clinical data will be completed by gastrointestinal surgeons.
Sample size and statistical analysis
This study is designed as a multicenter, single-arm phase II clinical trial. The pCR rate of single preoperative NCRT is assumed to be about 15% according to previous studies [14, 15]. On the other hand, the expectant pCR rate in this trail will be 40%. The required sample size was calculated to be 50 patients with 80% power and 95% confidence intervals. Moreover, 10% loss of follow-up rate is also considered. Such sample size was calculated using PASS software (version 15).
Statistical analyses will be in progress using the SPSS software (version 22.0). All analyses were 2-tailed. The confidence interval was 5–95%. p-values < 0.05 were considered as statistically significant. Continuous variables will be presented as means ± standard deviation and analyzed using an unpaired t-test with Welch’s correction. Categorical variables will be presented as number and percentage and analyzed using chi-square test with Fisher’s exact test. The Kaplan–Meier method and log-rank test were used to calculate the DFS and OS.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Discussion
It is widely known that the incidence rate of LARC is increasing by in recent years. Limited to closer distance from the anus and lower anus preservation rate, this kind of patients have poor postoperative quality of life. NCRT followed by TME, the current recognized treatment recommended by NCCN, may achieve limited curative effect which cannot be completely satisfied in clinic. Therefore, this study expects to provide a solid basis and encouraging outcomes for this promising combination of radiotherapy, chemotherapy and immunotherapy in LARC.
PD-1/PD-L1 inhibitors can enhance T cell activation and prevent T cells from dysfunction and apoptosis, has become more efficient in the treatment of cancer [34]. Increasing evidence suggests that dMMR patients perform significant response to anti- PD-1/PD-L1 therapy in rectal cancer [35]. Encouragingly, PD-1/PD-L1 inhibitors has been approved for treating dMMR CRC in clinic by the FDA [22–24]. Nevertheless, the proportion of dMMR in LARC is about 15% and the effectiveness of PD-1/PD-L1 inhibitors in pMMR LARC is still indeterminate. Tislelizumab is an anti-PD1 monoclonal antibody which was specifically engineered to minimize Fcγ receptor binding on macrophages, for achieving abrogating antibody-dependent phagocytosis which is identified as a reason of T-cell clearance and further potential resistance to anti-PD1 therapy [36, 37]. Furthermore, tislelizumab has been approved for treating recurrent/refractory classical Hodgkin lymphoma and locally advanced/metastatic urothelial carcinoma in China. This study concentrates on the safety and efficacy of conventional therapy plus PD-1/PD-L1 inhibitors in all types of LARC patients, not limited in dMMR.
Increasing studies prove the superiority of NCRT in comparison to postoperative adjuvant chemotherapy, which adjust maximized treatment before surgery to acquire better compliance, fewer toxicity profiles, and superior pCR rates. Thereinto, long course radiotherapy (50 Gy/25 f, 2 Gy/f, 5 days/week) combine chemotherapy (capecitabine) is a more frequently chosen NCRT plan with fewer adverse events [38, 39]. Considering the combination of PD-1 inhibitors, such safer NCRT therapeutic plan might be appropriate. Ingeniously, it has been widely confirmed that radiotherapy combined with PD1/PDL1 inhibitors has synergistic antitumor effect. A phase I clinical trial (KEYNOTE-001) indicated that patients with advanced non-small cell lung cancer who had received radiotherapy before treating with Pembrolizumab, a PD-1 inhibitor, achieved longer progression-free survival and overall survival compared with those without radiotherapy [40]. Previous studies testified that radiotherapy up-regulate the expression of PD-L1 in tumor cells and macrophages, further reversed T cells depletion and apoptosis and make T cells immune response fully to fight tumor [41]. Moreover, the combination of radiotherapy and PD1/PDL1 inhibitors could induce the immune response of tumor antigen-specific T cells (CD8+ T cells), which enhanced the effector function of cytotoxic T lymphocyte (CTL) in tumor microenvironment to achieve more superior antitumor effect [42]. Consequently, the injection timing of tislelizumab was started form week 2 in order to achieve synergistic antitumor effect for better curative outcomes.
Inevitably, several limitations in this study need to be discussed. First, to explore the curative effect of the treatment strategy, we design this single-arm study. Though the single-arm design might provide a little weaker level of evidences owing to the lack of randomness and another control arm like NCRT group. A number of single-arm clinical studies on neoadjuvant therapy combined with immunotherapy are being conducted in order to assess clinical outcomes more quickly [43, 44]. However, there are so many patients suffering from advanced rectal cancer, it is very urgent to find out an effective treatment. Based on the number of visits at each research center, all the patients involved in this single-arm study will be operated and we can get the primary outcome in less than a year so that we can figure out how effective this treatment is quickly. If we get a satisfied result, we will carry out a further controlled trial (RCT) with more sites to evaluate the safety and efficacy of adding anti-PD1 therapy with NCRT to treat patients with LARC more credibly. Secondly, this study focuses only on Chinese LARC patients without other ethnic groups and its sample size is a little small. Moreover, different plan of chemotherapy and radiotherapy in NRCT might become a potential bias to calculate the sample size.
Conclusion
To our knowledge, this is the first multicenter clinical trial in China to assess the safety and efficacy of NCRT plus anti-PD1 therapy followed by TME to treat patients with LARC. Despite there are some limitations because of the design of the one-arm study, we can get the primary outcome more quickly and we hope that this study can provide us positive outcomes and further encourage phase III trials.
Acknowledgements
Participating centres: Beijing Chaoyang Hospital, Capital Medical University; Beijing Xuanwu Hospital, Capital Medical University; Tianjin Medical University General Hospital; Tianjin People's Hospital; Tianjin Medical University Cancer Institute and Hospital.
Abbreviations
- LARC
Locally advanced rectal cancer
- NCRT
Neoadjuvant chemoradiotherapy
- TME
Total mesorectal excision
- NCCN
National Comprehensive Cancer Network
- pCR
Pathological complete response
- OS
Overall survival
- PD1
Programmed cell death 1
- PDL1
Programmed cell death ligand 1
- CRC
Colorectal cancer
- dMMR
Deficient mismatch repair
- pMMR
Proficient mismatch repair
- FDA
Food and Drug Administration
- NAR
Neoadjuvant rectal
- ORR
Objective response rate
- LRR
Local recurrence rate
- OS
Overall survival
- DFS
Disease free survival
- RECIST
Response Evaluation Criteria in Solid Tumors
- CR
Complete response
- PR
Partial response
- SITC
Society for Immunotherapy of Cancer
- MRI
Magnetic resonance imaging
- ECOG
Eastern Cooperative Oncology Group
- HIV
Human immunodeficiency virus
- EMVI
Extramural vascular invasion
- DNA
Deoxyribo nucleic acid
- MSI
Microsatellite instability
Authors’ contributions
HY and ZZ initially conceived this study, provided the domain knowledge expertise reviewed the final protocol and are the principal investigators of this study; ZY, XZ and JZ designed the final study protocol, coordinated collaboration among investigators from all institutions, drew the diagrams and wrote the manuscript; JG, ZB, WD, GC, YA provided clinical input and perspectives for the protocol and helped revise the manuscript; YL and QW provided advice on statistical analysis and coordinated ethics approval; JH, AL, GL, YS and DK helped in the design of the final study protocol and are coordinating site investigators. All authors contributed to the development and implementation of this protocol. All authors read and approved the final manuscript.
Funding
This study is funded by China Association of Gerontology and Geriatrics. Additionally, the study protocol has undergone full external peer review by the funding body as part of the peer review process. The sponsor has positively evaluated the design of the study and will grant 36 months funding. This funding source had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.China Association of Gerontology and Geriatrics.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
This study will be conducted in compliance with the principles of the Declaration of Helsinki 2013 (www.wma.net). This study has been approved by Ethics committee of Beijing Friendship Hospital, Capital Medical University (Approval number: 2021-P2-110–01) and by the institutional review boards of all the participating centres (see the Acknowledgements section). The written informed consent of all participants was required prior to participation in the study. Participants will not be identified in any reports or publications.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhengyang Yang, Xiao Zhang and Jie Zhang contributed equally to this work.
Contributor Information
Hongwei Yao, Email: zhangzht@ccmu.edu.cn, Email: yaohongwei@ccmu.edu.cn.
Zhongtao Zhang, Email: zhangzht@ccmu.edu.cn, Email: yaohongwei@ccmu.edu.cn.
References
- 1.Sung JJY, Chiu H-M, Jung K-W, et al. Increasing Trend in Young-Onset Colorectal Cancer in Asia: More Cancers in Men and More Rectal Cancers. Am J Gastroenterol. 2019;114:322–329. doi: 10.14309/ajg.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 2.Chen WZ, Chen XD, Ma LL, et al. Impact of Visceral Obesity and Sarcopenia on Short-Term Outcomes After Colorectal Cancer Surgery. Dig Dis Sci. 2018;63:1620–1630. doi: 10.1007/s10620-018-5019-2. [DOI] [PubMed] [Google Scholar]
- 3.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 4.Lawler M, Alsina D, Adams RA, et al. Critical research gaps and recommendations to inform research prioritisation for more effective prevention and improved outcomes in colorectal cancer. Gut. 2018;67:179–193. doi: 10.1136/gutjnl-2017-315333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katsidzira L, Gangaidzo I, Thomson S, et al. The shifting epidemiology of colorectal cancer in sub-Saharan Africa. Lancet Gastroenterol Hepatol. 2017;2:377–383. doi: 10.1016/S2468-1253(16)30183-2. [DOI] [PubMed] [Google Scholar]
- 6.Zhu J, Liu A, Sun X, et al. Multicenter, Randomized, Phase III Trial of Neoadjuvant Chemoradiation With Capecitabine and Irinotecan Guided by UGT1A1 Status in Patients With Locally Advanced Rectal Cancer. J Clin Oncol. 2020;38:4231–4239. doi: 10.1200/JCO.20.01932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen Z, Bu Z, Li A, et al. Multicenter study of surgical and oncologic outcomes of extra-levator versus conventional abdominoperineal excision for lower rectal cancer. Eur J Surg Oncol. 2020;46:115–122. doi: 10.1016/j.ejso.2019.08.017. [DOI] [PubMed] [Google Scholar]
- 8.Hata T, Takahashi H, Sakai D, et al. Neoadjuvant CapeOx therapy followed by sphincter-preserving surgery for lower rectal cancer. Surg Today. 2017;47:1372–1377. doi: 10.1007/s00595-017-1527-5. [DOI] [PubMed] [Google Scholar]
- 9.Yang Z, Chunhua G, Huayan Y, et al. Anatomical basis for the choice of laparoscopic surgery for low rectal cancer through the pelvic imaging data-a cohort study. World J Surg Oncol. 2018;16:199. doi: 10.1186/s12957-018-1498-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shamseddine A, Zeidan YH, El Husseini Z, et al. Efficacy and safety-in analysis of short-course radiation followed by mFOLFOX-6 plus avelumab for locally advanced rectal adenocarcinoma. Radiat Oncol. 2020;15:233. doi: 10.1186/s13014-020-01673-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731–1740. doi: 10.1056/NEJMoa040694. [DOI] [PubMed] [Google Scholar]
- 12.Provenzale D, Gupta S, Ahnen DJ, et al. Genetic/Familial High-Risk Assessment: Colorectal Version 1.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2016;;4:1010–30. doi: 10.6004/jnccn.2016.0108. [DOI] [PubMed] [Google Scholar]
- 13.Willett CG. Management of Locoregional Rectal Cancer. J Natl Compr Canc Netw. 2018;16:617–619. doi: 10.6004/jnccn.2018.0037. [DOI] [PubMed] [Google Scholar]
- 14.Bosset JF, Calais G, Mineur L, et al. Enhanced tumorocidal effect of chemotherapy with preoperative radiotherapy for rectal cancer: preliminary results–EORTC 22921. J Clin Oncol. 2005;23:5620–5627. doi: 10.1200/JCO.2005.02.113. [DOI] [PubMed] [Google Scholar]
- 15.Gerard JP, Conroy T, Bonnetain F, et al. Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3–4 rectal cancers: results of FFCD 9203. J Clin Oncol. 2006;24:4620–4625. doi: 10.1200/JCO.2006.06.7629. [DOI] [PubMed] [Google Scholar]
- 16.Bosset JF, Collette L, Calais G, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006;355:1114–1123. doi: 10.1056/NEJMoa060829. [DOI] [PubMed] [Google Scholar]
- 17.Wu F, Zhou C, Wu B, et al. Adding Adjuvants to Fluoropyrimidine-based Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Cancer: An Option Worthy of Serious Consideration. J Cancer. 2021;12:417–427. doi: 10.7150/jca.48337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ganesh K, Stadler ZK, Cercek A, et al. Immunotherapy in colorectal cancer: rationale, challenges and potential. Nat Rev Gastroenterol Hepatol. 2019;16:361–375. doi: 10.1038/s41575-019-0126-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taieb J, Shi Q, Pederson L, et al. Prognosis of microsatellite instability and/or mismatch repair deficiency stage III colon cancer patients after disease recurrence following adjuvant treatment: results of an ACCENT pooled analysis of seven studies. Ann Oncol. 2019;30:1466–1471. doi: 10.1093/annonc/mdz208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chalabi M, Fanchi LF, Dijkstra KK, et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med. 2020;26:566–576. doi: 10.1038/s41591-020-0805-8. [DOI] [PubMed] [Google Scholar]
- 22.Dekker E, Tanis PJ, Vleugels JLA, et al. Colorectal cancer. Lancet. 2019;394:1467–1480. doi: 10.1016/S0140-6736(19)32319-0. [DOI] [PubMed] [Google Scholar]
- 23.Overman MJ, Lonardi S, Wong KYM, et al. Durable Clinical Benefit With Nivolumab Plus Ipilimumab in DNA Mismatch Repair-Deficient/Microsatellite Instability-High Metastatic Colorectal Cancer. J Clin Oncol. 2018;36:773–779. doi: 10.1200/JCO.2017.76.9901. [DOI] [PubMed] [Google Scholar]
- 24.Overman MJ, McDermott R, Leach JL, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol. 2017;18:1182–1191. doi: 10.1016/S1470-2045(17)30422-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao Y, Li W, Wang Z, et al. Potential and unsolved problems of anti-PD-1/PD-L1 therapy combined with radiotherapy. Tumori . 2020;107(4):282–291. doi: 10.1177/0300891620940382. [DOI] [PubMed] [Google Scholar]
- 26.Tang H, Liang Y, Anders RA, et al. PD-L1 on host cells is essential for PD-L1 blockade-mediated tumor regression. J Clin Invest. 2018;128:580–588. doi: 10.1172/JCI96061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang AC, Postow MA, Orlowski RJ, et al. T-cell invigoration to tumour burden ratio associated with anti-PD-1 response. Nature. 2017;545:60–65. doi: 10.1038/nature22079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kong Y, Ma Y, Zhao X, et al. Optimizing the Treatment Schedule of Radiotherapy Combined With Anti-PD-1/PD-L1 Immunotherapy in Metastatic Cancers. Front Oncol. 2021;11:638873. doi: 10.3389/fonc.2021.638873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.von Moos R, Koeberle D, Schacher S, et al. Neoadjuvant radiotherapy combined with capecitabine and sorafenib in patients with advanced KRAS-mutated rectal cancer: A phase I/II trial (SAKK 41/08) Eur J Cancer. 2018;89:82–89. doi: 10.1016/j.ejca.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Imam I, Hammarstrom K, Sjoblom T, et al. Neoadjuvant rectal (NAR) score: Value evaluating the efficacy of neoadjuvant therapy and prognostic significance after surgery? Radiother Oncol. 2021;157:70–77. doi: 10.1016/j.radonc.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 31.Hodi FS, Hwu WJ, Kefford R, et al. Evaluation of Immune-Related Response Criteria and RECIST v1.1 in Patients With Advanced Melanoma Treated With Pembrolizumab. J Clin Oncol. 2016;34:1510–7. doi: 10.1200/JCO.2015.64.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puzanov I, Diab A, Abdallah K, et al. Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer. 2017;5:95. doi: 10.1186/s40425-017-0300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim B-h, Kim JM, Kang GH, et al. Standardized Pathology Report for Colorectal Cancer, 2nd Edition. J Pathol Transl Med. 2020;54(1):1–19. doi: 10.4132/jptm.2019.09.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu SY, Wu YL. Tislelizumab: an investigational anti-PD-1 antibody for the treatment of advanced non-small cell lung cancer (NSCLC) Expert Opin Investig Drugs. 2020;29:1355–1364. doi: 10.1080/13543784.2020.1833857. [DOI] [PubMed] [Google Scholar]
- 35.Zhang J, Cai J, Deng Y, et al. Complete response in patients with locally advanced rectal cancer after neoadjuvant treatment with nivolumab. Oncoimmunology. 2019;8:e1663108. doi: 10.1080/2162402X.2019.1663108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Q, Dong Y, Pan Y, et al. Case Report: Clinical Responses to Tislelizumab as a First-Line Therapy for Primary Hepatocellular Carcinoma With B-Cell Indolent Lymphoma. Front Immunol. 2021;12:634559. doi: 10.3389/fimmu.2021.634559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J, Lu S, Yu X, et al. Tislelizumab Plus Chemotherapy vs Chemotherapy Alone as First-line Treatment for Advanced Squamous Non-Small-Cell Lung Cancer: A Phase 3 Randomized Clinical Trial. JAMA Oncol. 2021;7:709–717. doi: 10.1001/jamaoncol.2021.0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ayez N, Alberda WJ, Burger JW, et al. Is restaging with chest and abdominal CT scan after neoadjuvant chemoradiotherapy for locally advanced rectal cancer necessary? Ann Surg Oncol. 2013;20:155–160. doi: 10.1245/s10434-012-2537-6. [DOI] [PubMed] [Google Scholar]
- 39.Raldow AC, Chen AB, Russell M, et al. Cost-effectiveness of Short-Course Radiation Therapy vs Long-Course Chemoradiation for Locally Advanced Rectal Cancer. JAMA Netw Open. 2019;2:e192249. doi: 10.1001/jamanetworkopen.2019.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shaverdian N, Lisberg AE, Bornazyan K, et al. Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: a secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol. 2017;18:895–903. doi: 10.1016/S1470-2045(17)30380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Derer A, Frey B, Fietkau R, et al. Immune-modulating properties of ionizing radiation: rationale for the treatment of cancer by combination radiotherapy and immune checkpoint inhibitors. Cancer Immunol Immunother. 2016;65:779–786. doi: 10.1007/s00262-015-1771-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deng L, Liang H, Burnette B, et al. Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice. J Clin Invest. 2014;124:687–695. doi: 10.1172/JCI67313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu Y, Han G, Li H, et al. Camrelizumab combined with FOLFOX as neoadjuvant therapy for resectable locally advanced gastric and gastroesophageal junction adenocarcinoma. J Clin Oncol. 2020;38(15_suppl):4536–36.
- 44.Lin ZY, Cai M, Zhang P, et al. Short-course radiotherapy and subsequent CAPOX plus camrelizumab followed by delayed surgery for locally advanced rectal cancer:Short-term results of a phase II trial. J Clin Oncol. 2021;39(3):63–63. doi: 10.1200/JCO.2021.39.3_suppl.63. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.