Abstract
Background
Disruption to everyday routine during the COVID-19 pandemic has resulted in considerable implications for global mental health. The inter- and intra-personal mechanisms by which disrupted routine can contribute to elevated depressive symptoms has not been well-explored. The present study aimed to examine how feelings of social (dis)connectedness and rumination, as a maladaptive coping strategy, could explain the association between disrupted well-being activities and depressive symptoms.
Methods
Participants (N = 496) ranging in age from 18 to 73 years (M = 28.73, SD = 10.93) completed an online survey within the first 3 months of the COVID-19 pandemic, which included measures of disruption to usual psychological and physical well-being activities, social connectedness, rumination, and depressive symptoms. Social connectedness and rumination were investigated as serial mediators of the association between disrupted well-being activities and depression using Hayes' PROCESS macro.
Results
39.5% of the sample reported clinically significant levels of depression. Disruption to well-being activities predicted higher depressive symptoms, and this was partially explained by feelings of social disconnectedness and subsequent rumination. Rumination, alone, was not a significant mediator between disrupted routine and depressive symptoms.
Limitations
The cross-sectional survey design does not preclude the possibility of bidirectional effects.
Conclusion
The social distancing public health measures to combat COVID-19 have contributed to widespread disrupted routine, and in turn, elevated symptoms of depression. Social disconnectedness plays a particularly important role in this association. Intervention strategies should consider social factors as a ‘social cure’ for mass, positive mental health promotion during COVID-19.
Keywords: COVID-19, Depression, Disrupted routine, Social connectedness, Rumination
1. Introduction
The COVID-19 pandemic has been a source of substantial stress, anxiety, and fear for many people (Lu et al., 2020), and while this undoubtedly stems from the disease itself, it can also come from (and be exacerbated by) the sequalae of events following disruption to daily life (Duan and Zhu, 2020; Xiong et al., 2020; Bo et al., 2020). In a bid to ‘flatten the curve’, ‘lockdowns’, and social/physical distancing measures have been implemented in many countries. Though necessary to reduce case numbers (Kontoangelos et al., 2020), this can have a deleterious effect on the mental health of the general population resulting from the broad disruption to work, home, and/or educational contexts (e.g., Zhang et al., 2020). Recent empirical research has demonstrated that COVID-19 is associated with poorer sleep quality, increased levels of depression, generalized anxiety (e.g., Huang and Zhao, 2020), PTSD symptoms (e.g., C. Wang et al., 2020; D. Wang et al., 2020), and stress (Xiao et al., 2020; for review see Vindegaard and Benros, 2020; Xiong et al., 2020). Notably, there has been a significant increase in the prevalence rates of depression, anxiety, and trauma symptoms during the COVID-19 pandemic compared to previous population studies (e.g., Hyland et al., 2020; Shevlin et al., 2020), with poorer mental health influenced by factors such as perceived risk, infection, and loss of income due to COVID-19 (Hyland et al., 2020).
Considering these additional COVID-specific risk factors, now, more than ever, there is a need for individuals to be able to engage in well-being activities to help manage symptoms of poorer mental health. Nonetheless, lockdowns and physical distancing restrictions present a barrier to engagement in typical, face-to-face social and well-being activities (Lades et al., 2020). Specifically, disruption to activities that are of physical (e.g., exercise; Giuntella et al., 2021) and psychological (e.g., support groups; Pelizza and Pupo, 2020) benefit, can further reinforce negative mental health states during COVID-19 as opportunities for effective symptom management become limited or, at best, altered from their typical face-to-face format. Worldwide step-counts have decreased since the declaration of the pandemic (Tison et al., 2020), with reduced physical activity correlated with poorer mental health (Maugeri et al., 2020). Likewise, poorer mental health can be explained by the lower levels of satisfaction with the fulfilment of basic psychological needs (autonomy, competence, relatedness) during lockdown (Cantarero et al., 2020). Mitigation of COVID-19 induced mental health concerns requires individual efforts in the initial instance, but research has called for mental health to be established as an international priority requiring government intervention (e.g., Holmes et al., 2020; Xiong et al., 2020). Given that COVID-19 presents an extraordinary context for rapidly increasing mental health concerns at a global level, it is critical to understand the mental health implications of such disruption to daily life, and the mechanisms by which this occurs and can be modified.
Human beings have a basic need for interpersonal contact; the lack of which can have a negative impact on mental and physical health (Coyle and Dugan, 2012). In recent months however, our typical social interactions with others have drastically changed due to the pandemic. Instead of attending a fitness class with others, the closure of, or limited access to, health centres has resulted in individuals exercising alone, or not at all. Friends and family cannot spend time together in person or receive support in ways that they typically would. Those attending support groups or therapy cannot engage in the typical face-to-face format. Increased interest in online solutions such as real-time videoconferencing has emerged in the context of the pandemic to facilitate continued access to structured physical activities (e.g., Schwartz et al., 2021), therapeutic (Simpson et al., 2020) and/or social support (Venville et al., 2021). Although addressing the increased demand for access despite physical distancing measures, for some this sudden and often forced shift from typical face-to-face well-being activities to online methods may not be a sufficient alternative. Such disruption to individuals' routine can increase feelings of isolation or a lack of connectedness and impede individuals' perception of belonging to a community/group; factors extensively shown to improve health (Haslam et al., 2015; Hawkley and Cacioppo, 2013; Saeri et al., 2018). Indeed, the social cure theory (Jetten et al., 2017) postulates that being socially connected to others as part of a group affords individuals access to resources (e.g., social identity, support, meaning, agency) that can promote better mental health. Disruption to our everyday activities has, at the very core, disrupted our social connections and the positive mental health effects that this can provide. In the current context, this sense of self-isolation is magnified as it is in accordance with the recommended physical distancing health guidelines to curb the transmission of COVID-19.
Social connectedness can act as a protective factor against the development of depressive symptoms (Cruwys et al., 2013) and, indeed, considerable research has highlighted the benefits of social connectedness for mental health (e.g., Lamblin et al., 2017; Williams and Galliher, 2006; Malaquias et al., 2015; Saeri et al., 2018). However, the converse, a lack of feeling socially connected, can equally account for poorer psychological well-being and increased depressive symptomatology (Santini et al., 2020). In particular, research has shown that feelings of social disconnectedness and isolation are linked to lower levels of self-rated physical health (Cornwell and Waite, 2009), higher levels of anxiety (Mehra et al., 2020), depression (Taylor et al., 2020) and overall poorer health (Miyawaki, 2015). Given the well-established impact of social connectedness on mental health, paralleled with the perceptions of social isolation during COVID-19 restrictions, social connectedness is one potential mechanism by which the association between disrupted activities and depression can be explained.
Without typical social connections, individuals may engage in other coping mechanisms to manage psychological distress. Response Style Theory (Nolen-Hoeksema, 1991) outlines that an individual's vulnerability for depression, the extent of the symptoms, and the duration can be determined by a ruminative style of thinking. This thinking style is mainly centred on the causes and consequences of one's psychological symptoms, and while this can be used as a meta-cognitive task to make sense of past events, there is a significant correlation to negative mental health (Rimes and Watkins, 2005; Lo et al., 2008). Thus, rumination can be considered a mechanism by which vulnerability for depression is heightened: an individual may engage in repetitive negative thinking that reinforces beliefs of loss of control, which can then deplete motivation to engage in activities to alleviate the depressive mood (Nolen-Hoeksema et al., 2008). Typically, rumination is a response to a stressful life event (e.g., Michl et al., 2013). COVID-19, in many respects, has introduced sudden stressors in social, work, education, and health contexts, bringing with it a likelihood for a ruminative response style in those who otherwise would not engage in ruminative processes (Ye et al., 2020). In fact, uncertainty is often a precursor that stimulates a ruminative style of thinking (e.g., Liao and Wei, 2011) and considering the uncertainty and change to daily routines within a COVID-19 context, increased use of rumination may account for poorer mental health outcomes. Without having supportive structures in place or maintaining feelings of connectedness to others which can reduce negative thought processes such as rumination (Puterman et al., 2010), it is plausible that the lack of social connectedness brought about by the disruption to daily routine, would contribute to the engagement of maladaptive coping mechanisms such as rumination, and in turn could have negative consequences for mental health.
As such, we aim to examine social connectedness and rumination as mediating factors underlying the association between disruption to well-being activities and mental health during COVID-19. This is a novel investigation into the mechanisms by which disruption caused by COVID-19 restrictions contributes to the well-reported elevated depressive symptoms (e.g., Hyland et al., 2020; Vindegaard and Benros, 2020). Based on the existing literature, we hypothesize that increased disruption to everyday routine across mental and physical well-being activities will be associated with decreased perceptions of social connectedness, which in turn will be linked to increased levels of rumination, which, finally, is associated with greater depressive symptoms.
2. Methods
2.1. Design
An online survey was programmed and disseminated using Qualtrics software to assess disruption to routine, social connectedness, rumination, and mental health in an Irish population. The survey, following a cross sectional, correlational design, was active for 4 weeks between April 8th, 2020 and May 11th, 2020, during which time Ireland was in the highest level of COVID-19 restrictions with a national lockdown. Depressive symptoms were included as the dependent variable, while the independent variable consisted of disruption to everyday well-being activities (physical and psychological). Social connectedness and rumination were examined as serial mediating variables within the model. This study received ethical approval from the Education and Health Sciences Ethics Committee at the University of Limerick (Ethical approval no.: 2020_04_16_EHS).
2.2. Participants
A total of 496 participants, ranging in age from 18 to 73 years old (M = 28.73, SD = 10.93) completed the survey. The sample consisted of predominantly Irish participants (n = 420; 84.7%) with 123 (24.8%) males and 372 (75.0%) females; in addition, 1 (0.2%) identified as ‘other’. See Table 1 for additional participant information. Participants were recruited via snowball sampling across a range of social media platforms including but not limited to Facebook and Instagram.
Table 1.
Descriptive statistics on participant characteristics.
| Variable | n (%) | M (SD) |
|---|---|---|
| Gender | ||
| Male | 123 (24.8%) | |
| Female | 372 (75%) | |
| Other | 1 (0.2%) | |
| Age | 28.73 (10.93) | |
| History of mental health conditions | ||
| Depression | 99 (20%) | |
| Generalized anxiety disorder | 65 (13.1%) | |
| Social anxiety | 47 (9.5%) | |
| Substance abuse disorder | 5 (1.0%) | |
| Obsessive compulsive disorder | 7 (1.4%) | |
| Eating disorder | 12 (2.4%) | |
| Other | 27 (5.4%) | |
| Not applicable | 213 (42.9%) | |
| Prefer not to say | 21 (4.2%) | |
| PHQ-9 | 8.97 (6.49) | |
| RRS-10 | 19.65 (6.40) | |
| Social connectedness pre-COVID-19 public health restrictions | 27.55 (6.05) | |
| Social connectedness post-COVID-19 public health restrictions | 19.53 (6.23) | |
| Disruption to well-being activities | 6.18 (2.27) |
Note. PHQ-9 = Patient Health Questionnaire; RRS-10 = Rumination Responses Scale.
2.3. Materials
2.3.1. Demographic questionnaire
A demographic questionnaire assessed participant characteristics including age, gender, and history of mental health conditions.
2.3.2. PHQ-9
The Patient Health Questionnaire-9 or PHQ-9 (Kroenke and Spitzer, 2002) was used to measure depressive symptoms. The PHQ-9 is a valid measurement tool within depression research (Kroenke, 2021). The PHQ-9 contains 9 questions (e.g., “Over the last two weeks how often have you been bothered by having little interest or pleasure in doing things”) which are used to measure symptoms of depression over a two-week period; assessed on a 4-point Likert scale ranging from 0 ‘not at all’ to 3 ‘nearly every day’. A severity (total) score was calculated by summing the total number of responses that indicated such events occurred ‘on several days’, ‘more than half the days’ or ‘nearly every day’. Higher scores indicated higher levels of depressive symptoms, ranging from 0 to 27., Clinical levels of depression were examined using the clinical cut-off score of ≥10, in line with Arroll et al. (2010) for the purpose of descriptive statistics only, however, the severity (continuous) score was used in the main analyses. Cronbach α analysis (α = 0.89) yielded high internal reliability for the current sample.
2.3.3. Disruption to well-being activities
Disruption to every day routine was measured across 2 domains: Psychological well-being and physical well-being. An overall ‘disruption to well-being activities’ variable was computed by averaging the score of both items: “In the past month, please indicate the extent to which your day-to-day routine has changed in the following areas (i) physical activities, (ii) activities to promote psychological wellbeing”. The extent to which their day-to-day routine was disrupted was assessed on a 10-point Likert scale measuring from 1 ‘Not changed at all’ to 10 ‘Changed extremely’. The higher a participant scored on this scale indicated a higher level of perceived disruption to well-being activities due to COVID-19. Cronbach's alpha for these two items was 0.54.
2.3.4. Social connectedness
An adapted version of the Social Connectedness Scale (Lee et al., 2001) was used to assess individuals' perceptions of connectedness to others and society. Six items from the scale were selected and then adapted to account for the COVID context at the time of data collection. Specifically, participants were asked to rate their perceptions of social connectedness in response to each item on a 6-point scale from ‘strongly disagree’ to ‘strongly agree’ considering two time points: pre- as well as post- COVID social and public health restrictions were introduced (e.g., “Current government guidelines around COVID-19 have resulted in people distancing themselves from family, friends, and other social activities that one might engage in. Please rate your agreement to the following questions regarding your experiences (prior to/ following) social distancing measures. - I was able to connect with other people”). Higher scores on the scale were indicative of higher levels of social connectedness. Reliability analyses indicated high internal reliability for both the pre- (α = 0.85) and post- (α = 0.81) measures.
2.3.5. Rumination
The Rumination Responses Scale (RRS; Treynor et al., 2003) measured rumination on a 10-item scale. This scale includes two subscales, brooding and reflection, however for the purpose of the current analyses, a total scale was calculated based on an average of both subscales. Participants were asked to report how often they felt or did each of the items, rating them on a 4-point Likert scale from 1 ‘almost never’ to 4 ‘almost always’. Sample items include “Write down what you are thinking and analyse it”, “Go someplace alone to think about your feelings”, “Think ‘What am I doing to deserve this?’”. Scores ranged from 10 to 40, with higher scores indicative of higher levels of ruminations. Previous research has highlighted this measure as a valid tool for analysing rumination (Schoofs et al., 2010). Cronbach's α for the current study is 0.87.
2.4. Procedure
All participants that took part in the study were recruited via snowball sampling methods. Links to the survey were distributed through social media platforms such as Facebook and Instagram. Survey completion took approximately 10–15 min. IBM's SPSS (Statistical Package for the Social Sciences) software was used to run statistical analysis on all recorded results.
2.5. Statistical analysis
Prior to analyses, the data was screened for outliers. From the initial sample of (N = 655), 159 participants were removed due to missing data leaving n = 496 within the main analysis. Preliminary correlation analyses and Analyses of Variance (ANOVA's) were conducted on confounding variables such as age, gender, and history of mental health conditions to examine their impact on disruption to well-being activities and depressive symptoms. The variables were selected as previous research has demonstrated their effect on depressive symptoms (e.g., Nolen-Hoeksema and Aldao, 2011; Glaesmer et al., 2011; Girgus and Yang, 2015; Piet and Hougaard, 2011). These variables were controlled for in the multiple regression analysis which examined the association between disruption to well-being activities and depressive symptoms. Following this, serial mediation analyses exploring social connectedness post-public health restrictions and rumination as potential mediators of the association between disrupted well-being activities and depressive symptoms was conducted using Hayes PROCESS Model 6 on IBM SPSS Version 26. Perceived social connectedness pre-COVID public health restrictions was also included as a covariate in the serial mediation analyses to account for change specific to the COVID-19 context. Mediation analyses were conducted using 5000 bootstrapped re-sampling with interpretation of the 95% bCI to determine significance of the mediational effect; if the range of the lower and upper 95% bCI crossed 0, the mediational effect was deemed non-significant. In all other analyses, the alpha level was set at 0.05.
3. Results
3.1. Descriptive statistics
Preliminary descriptive analyses showed that participants reported a mean depressive score of 8.94 (SD = 6.46) on the PHQ-9, corresponding to at least mild depressive symptoms (Kroenke and Spitzer, 2002). Using the clinical cut-off score of ≥10 (Arroll et al., 2010), 39.5% of the sample showed clinically significant levels of depression. Additionally, participants reported average levels of rumination (M = 19.66, SD = 6.41, Range = 10–40) similar to previous samples (e.g., Erdur-Baker and Bugay, 2010) while social connectedness scores post-social distancing (M = 19.44, SD = 6.18, Range = 6–36) were lower than average in comparison to other samples (e.g., Lee et al., 2001). Participants also reported moderately high levels of disruption to well-being activities (M = 6.14, SD = 2.27, Range = 1–10).
3.2. Preliminary analyses
3.2.1. Covariates
Preliminary analyses showed that age was negatively correlated with depressive symptoms (r = −0.26, p < .001) such that those who were younger reported higher levels of depression. Analyses of Variance also showed differences in levels of depression across genders (F (2, 495) = 6.50, p = .002) with those identifying as other (n = 1) reporting the highest level of depressive symptoms (M = 18.00) (though this should be interpreted with caution given the sample size of this group), followed by women (M = 9.50, SD = 6.45) and subsequently men (M = 7.28, SD = 6.35). Moreover, those with a previous history of mental health diagnoses reported higher levels of depressive symptoms (M = 11.22, SD = 6.62) in comparison to those who preferred not to say (M = 9.52, SD = 5.09) and those who reported no prior history (M = 6.15, SD = 5.26) (F (2, 495) = 41.92, p < .001). With respect to disrupted well-being activities, analyses revealed that the degree of disruption to such activities was similar irrespective of gender (F (2, 495) = 1.37, p = .26), history of mental health condition (F (2, 495) = 0.99, p = .37), or age (r = −0.02, p = .73).
3.2.2. Regression
Preliminary multiple regression analyses were conducted to examine the association between disruption to well-being activities (entered at Step 2 of the model) and depressive symptoms, controlling for age, gender, and history of mental health conditions (entered at Step 1). Results indicated that disruption to routine well-being activities was positively associated with depressive symptoms (β = 0.14, t = 3.64, p < .001, 95% CI [0.19, 0.64], R2 = 24.7) such that higher levels of reported disruption was associated with higher levels of depressive symptoms. See Table 2 for summary of regression statistics.
Table 2.
Summary of hierarchical regression model predicting depression symptoms (PHQ-9).
| Model | B | SE | β | t | Sig. | 95.0% confidence interval |
Adjusted R2 |
||
|---|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||||
| 1 | Constant | 14.61 | 1.43 | 10.21 | <0.001 | 11.80 | 17.42 | 0.19 | |
| Age | −0.16 | 0.02 | −0.27 | −6.68 | <0.001 | −0.20 | −0.11 | ||
| Gender | 2.42 | 0.59 | 0.16 | 4.70 | <0.001 | 1.25 | 3.59 | ||
| History of mental health conditions | −3.57 | 0.45 | −0.32 | −7.95 | <0.001 | −4.45 | −2.68 | ||
| 2 | Constant | 12.04 | 1.58 | 7.6 | <0.001 | 8.94 | 15.15 | 0.22 | |
| Age | −0.15 | 0.02 | −0.26 | −6.66 | <0.001 | −0.20 | −0.11 | ||
| Gender | 2.31 | 0.59 | 0.16 | 3.93 | <0.001 | 1.15 | 3.46 | ||
| History of mental health conditions | −3.47 | 0.44 | −0.31 | −7.82 | <0.001 | −4.35 | −2.60 | ||
| Disruption to well-being activities | 0.41 | 0.11 | 0.14 | 3.64 | <0.001 | 0.19 | 0.64 | ||
Dependent variable: PHQ9 (range 0–27) - Depression Score.
3.3. Main analyses.
3.3.1. Serial mediation
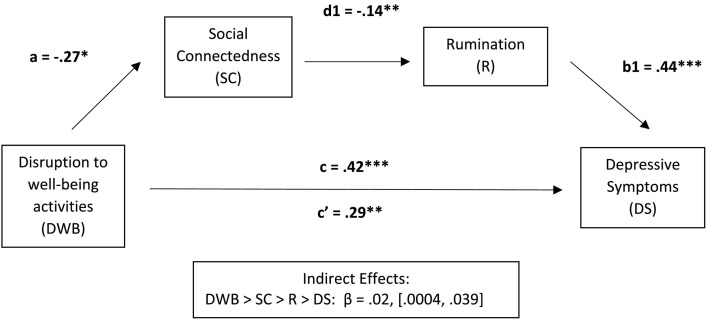
Serial mediation analyses were conducted using Hayes PROCESS v3.5 Model 6 to examine social connectedness and rumination as potential mediating variables explaining the association between disruption to well-being activities and depressive symptoms during the COVID-19 pandemic. Analyses included age, gender, social connectedness pre-public health restrictions, and a history of mental health condition as covariates. Results indicated a statistically significant serial mediation via social connectedness and rumination (β = 0.02, SE = 0.01, 95% bCI [0.0004, 0.0390]) such that disruption to well-being activities was negatively associated with social connectedness (β = −0.27, t = −2.22, p = .03, 95% bCI [−0.51, −0.03]) which, in turn, was negatively linked to rumination (β = −0.14, t = −3.35, p = .009, 95% bCI [−0.22, −0.06]), with rumination then positively associated with depressive symptoms (β = 0.44, t = 11.92, p < .001, 95% bCI [0.37, 0.51]) (see Fig. 1 ). In sum, this suggests that more disruption to individuals' well-being activities lead to lower levels of connectedness and then higher levels of rumination that subsequently results in more depressive symptoms.
Fig. 1.
Path diagram of serial mediation analyses between disruption to wellbeing activities and depressive symptoms, with perceived social connectedness post-COVID public health restrictions and rumination as mediators. Age, gender, history of mental health conditions, and social connectedness pre-COVID public health restrictions were included as covariates in the model.
Note: *p < .05; **p < .01; ***p < .001.
Results from the overall model also demonstrated a statistically significant simple indirect effect via social connectedness (β = 0.08, SE = 0.04, 95% bCI [0.003, 0.17]), but not via rumination (β = 0.03, SE = 0.04, 95% bCI [−0.07, 0.12].1
4. Discussion
The present study aimed to examine the effect of disruption to well-being activities during the COVID-19 pandemic on depressive symptoms, and the mechanisms by which this can occur. The results showed that greater disruption to an individual's well-being activities leads to more depressive symptoms and this association was serially mediated by social connectedness and rumination, although a direct effect was also maintained. When there was more disruption to an individuals' well-being activities (i.e., physical and psychological activities), individuals reported feeling less socially connected, which increased their levels of rumination, in turn contributing to increased depressive symptoms. When examining each mediator independently, only the pathway through social connectedness was significant. Lower social connectedness, and rumination resulting from such, is a potential mechanism that explains how disruption to well-being activities can have a negative effect on mental health.
Understanding the contributing factors that can lead to poorer mental health outcomes has been of importance both in an Irish context and across the globe, for decades. The COVID-19 pandemic, however, has provided an unprecedented situation where, not only detrimental physical health outcomes have been of grave concern, but also where the emotional distress associated with restrictive public health measures, lack of personal freedom, financial concerns, bereavement, among others, have exacerbated mental health issues, including depression. This poses a risk for the development of psychiatric illness across communicates on a mass level (Pfefferbaum and North, 2020). The adverse impact of lockdown, and the COVID-19 pandemic itself, on mental health has already been established, (Huang and Zhao, 2020; Vindegaard and Benros, 2020; C. Wang et al., 2020; D. Wang et al., 2020; Xiao et al., 2020; Xiong et al., 2020). Although the current study supports previous research that demonstrated the negative effect of low levels of social connectedness (Santini et al., 2020) and increased rumination (Rimes and Watkins, 2005; Lo et al., 2008) on mental health, our findings make a unique contribution to the ever-growing COVID literature by highlighting that these mechanisms explain, at least partially, how the disruption brought about by public health stay-at-home measures can impact mental health. Indeed, by demonstrating that more disruption to an individuals' well-being activities is linked to less perceived social connectedness and in turn, increased levels of rumination, it demonstrates that both inter-personal (social connectedness) and intra-personal (rumination) factors are of importance for mental health within a COVID context. This further adds to current evidence that a lack of socially relevant resources, such as lower levels of social support, can account for increased rumination which may subsequently increase the risk for the onset of mental health conditions (Thorsteinsson et al., 2013; Flynn et al., 2010; Mohr et al., 2004).
Despite this, it should be acknowledged that the results showed a significant simple effect via social connectedness alone, but not via rumination. This suggests that when assessed individually, rumination is not a significant mechanism by which disruption to routine is associated with depressive symptoms. Specifically, it indicates that disruption to well-being activities is not directly correlated with rumination, when controlling for self-perceived social connectedness. Instead, findings suggest that it is the lack of social connectedness that is brought about by the disruption to well-being activities that leads to increased rumination. As such, this highlights the value of a socially-based intervention in acting as a potential buffer for mitigating such negative effects on mental health. As lower levels of social connectedness is linked to higher levels of rumination, interventions that either directly or indirectly promote social connectedness could potentially reduce maladaptive coping mechanisms, and thus reduce depressive symptoms. For example, in response to stressful life events, stronger ingroup ties, a component of social identity, has been associated with less ruminative coping, consistent with the “social cure” perspective (Ysseldyk et al., 2018). Of course, this cross-sectional research cannot imply causal effects, however, it does provide a foundation for future research to explore group-based interventions as a means by which positive mental health outcomes can be supported. This is particularly relevant during a global, stressful event such as the COVID pandemic, and as we navigate the uncertainties of the post-COVID landscape.
While the outlook in Ireland, at least, is promising, particularly with the increased roll-out vaccination programmes, we are not yet in a ‘fully post-COVID’ world and mental health remains a priority in the current situation. The COVID-19 pandemic is a dynamic situation and the landscape has consistently moved in a nonlinear fashion through varying levels of heightened and lowered security over the last year. As we come out of lockdown and begin to ‘return to normality’ as public health restrictions ease, increased social interactions will occur as a form of naturalistic intervention. It would be expected that this would lead to increased feelings of connectedness and positively impact mental health, however, it may take considerable time for social interactions to return to pre-covid levels, if it ever does. It is plausible, however, that not all interactions will facilitate adaptive coping strategies, as the quality of support provision can determine the benefits or, alternatively, costs, to mental health. Afifi et al. (2013) observed that when poor social support was provided to individuals verbally ruminating, they reported increased anxiety, relationship dissatisfaction, and further rumination (brooding) following the conversation. Furthermore, social interaction may even facilitate ‘co-rumination’. In individuals self-reporting a recent major stressor that is of a psychological challenge, Horn and Maercker (2016) found that inter-personal emotion regulation, over and above the effect of intra-personal emotion regulation, accounted for symptoms of adjustment disorder and depression. Thus, group or socially based interventions that promote positive social interaction and support may provide mental health benefits as we enter an uncharted, post-COVID era.
Furthermore, the reopening of society brings with it a new type of disruption. Although the pandemic was originally a vast disruption to typical routine, people have adjusted to a new way of living; given the duration in which it has lasted. For many, it has allowed people to reassess what is most important, find meaning in life, and fosters individual as well as societal flourishing (Routledge and FioRito, 2021); but it is worth noting that the reopening of society is, in itself, another change. This type of disruption, however, may not necessarily present the same effects on social connectedness, rumination and depression, (i.e., this type of disruption could increase connectedness, and reduce rumination and depression), but this is an avenue for future research. Indeed, the current research provides a foundation for future research, and provides a better understanding of how disruption to well-being activities impact mental health, whether that is due to the COVID-19 pandemic or otherwise. Although conducted in the context of COVID-19, this research could serve as a foundation for understanding the processes impacting mental health, particularly in response to disruption to well-being activities across various contexts. As such, future research should aim to replicate these findings as restrictions begin to ease, and in a non-covid context.
Albeit this study has provided novel insights into potential mechanisms by which the COVID-19 context has contributed to poorer mental health outcomes, it is not without limitations. Firstly, this study was conducted cross-sectionally so interpretation of the models warrants caution, as bidirectionality of the associations cannot be ruled out. As such, it is plausible that higher levels of rumination are associated with lower perceived social connectedness, and not vice versa as we have modelled. Thus, future research that incorporates longitudinal assessment of these variables will allow for stronger conclusions to be drawn on the proposed mediational pathways. Secondly, well-being activities are all-encompassing, which can introduce heterogeneity in operationalisation. Participants self-reported the disruption to their usual well-being activities in terms of how they typically promote physical and/or psychological health. Although not collected, consideration for the format of such activities, as either individual or group-based, may better elucidate the association between disruption to well-being activities and mental health via social connectedness in line with the social cure literature (Jetten et al., 2012). Indeed, the individual is closely integrated with the social, which has been brought to the forefront during public health measures to curb the spread of COVID-19. In fact, it may be that such measures have restricted the social identity resources of support, collective self-efficacy, and meaning afforded by group memberships as part of usual well-being activities. This requires further investigation. It is important to note that we do not advocate that this is the only potential mechanism by which disrupted routine may negatively impact mental health in COVID times or other, but it does support an accumulating body of literate of the pro-mental health benefits of social identity processes and associated group memberships (e.g., Jetten et al., 2017; Muldoon et al., 2019). Lastly, perceived social connectedness is likely distinct from tangible social connectedness, assessed in terms of the number of social contacts or interactions. Previous research has suggested that perceived social identity resources, such as social support, promote greater benefits than tangible resources (Ashida and Heaney, 2008). Thus, although an individual may be socially connected and/or maintain their social connections during COVID (e.g., through online interactions), it may not be perceived as such due to the requirement for physical social distancing as per public health measures. Therefore, an individual with more social interactions, could in fact, report feeling less socially connected than someone with fewer social interactions. As we controlled for pre-COVID self-reported levels of perceived social connectedness in our mediational analyses, we assessed the change in perceived social connectedness introduced by COVID-19 measures. As such, this is a particular strength of the current study as it accounts for the COVID-context, but equally the change in perceived connectedness may not directly map on to a change in social contacts/interactions. Indeed, 18% of the current sample reported no change or increased perceived social connectedness during COVID, relative to before the pandemic. It could be that the unity that comes with shared experiences during COVID fosters a greater sense of social connectedness (‘we are all in this together’) than that immediately afforded by direct, interpersonal relationships (Abrams et al., 2021). Future research should look to ascertain the nuances of how social connectedness (perceived, interpersonal or otherwise) is linked with mental health outcomes as this will be an important consideration in intervention approaches post-COVID where it is likely that a ‘new normal’ for social interactions remain.
In conclusion, the mental health effects of COVID-19 are an ever-increasing priority in the midst of an ongoing pandemic, but also for some time to come as we learn to re-engage with society post-pandemic. In a nationally representative sample, 39.5% of individuals reported clinical levels of depression evidencing the risk for mental health disorder onset in the current landscape. The magnitude of disruption to typical well-being activities resulting from pandemic public health measures predicted increased depressive symptoms; this was partially explained by the serial mediational pathway where lower levels of social connectedness in turn contributed to increased ruminative strategies, a known risk factor for depression. Interestingly, social connectedness was the driver of this association, over and above ruminative coping strategies, reinforcing the notion that interpersonal factors are as important a consideration as intrapersonal factors in supporting better mental health outcomes. Intervention strategies and approaches to remote working or education that can harness the potential of feeling socially connected, and the social resources afforded by this, offer much promise in terms of a “social cure” or “social prevention” for global mental health concerns as we cautiously emerge into a post-pandemic world.
CRediT authorship contribution statement
GMcM, EA & AD were involved in the conception of the research idea, design, survey development and recruitment. GMcM, EA, AD and KC contributed to the interpretation of the final analyses and preparation of the final manuscript.
Funding source
This project was not funded by any research body or organisation.
Conflict of interest
The authors have no conflict of interest to declare.
Acknowledgements
N/A.
Footnotes
To further assess the robustness of our proposed mediation pathways, a sensitivity analysis was conducted including mental health history as a moderator of all pathways using model 85 of Hayes PROCESS macro (controlling for age, gender, and social connectedness pre-COVID public health restrictions). No significant moderation of the direct effect of disruption to well-being activities on depressive symptoms (F(1, 468) = 0.18, p = .67), indirect effect via change in social connectedness (β = −0.03, SE = 0.09, 95% bCI[−0.21, 0.15]), indirect effect via rumination (β = 0.07, SE = 0.10, 95% bCI[−0.13, 0.26]), nor serial mediation (β = −0.01, SE = 0.02, 95% bCI[−0.04, 0.03]) was observed. Findings indicate that at-risk samples with a history of mental health conditions as well as individuals with no prior history experience an equivalent negative effect of disruption to their well-being activities, resulting in greater depressive symptoms through experiences of lower social connectedness and, in turn, higher rumination.
References
- Abrams D., Lalot F., Hogg M.A. Intergroup and intragroup dimensions of COVID-19: A social identity perspective on social fragmentation and unity. Group Processes & Intergroup Relations. 2021;24(2):201–209. doi: 10.1177/1368430220983440. [DOI] [Google Scholar]
- Afifi T., Afifi W., Merrill A.F., Denes A., Davis S. “You need to stop talking about this!”: verbal rumination and the costs of social support. Hum. Commun. Res. 2013;39(4):395–421. doi: 10.1111/hcre.12012. [DOI] [Google Scholar]
- Arroll B., Goodyear-Smith F., Crengle S., Gunn J., Kerse N., Fishman T., Hatcher S.… Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann. Fam. Med. 2010;8(4):348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashida S., Heaney C.A. Differential associations of social support and social connectedness with structural features of social networks and the health status of older adults. J. Aging Health. 2008;20(7):872–893. doi: 10.1177/0898264308324626. [DOI] [PubMed] [Google Scholar]
- Bo H.X., Li W., Yang Y., Wang Y.U., Zhang Q., Cheung T., Xiang Y.T.… Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020;51(6):1052–1053. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantarero K., van Tilburg W.A., Smoktunowicz E. Affirming basic psychological needs promotes mental well-being during the COVID-19 outbreak. Soc. Psychol. Personal. Sci. 2020;12(5):821–828. doi:10.1177%2F1948550620942708. [Google Scholar]
- Cornwell E.Y., Waite L.J. Social disconnectedness, perceived isolation, and health among older adults. J. Health Soc. Behav. 2009;50(1):31–48. doi: 10.1177/002214650905000103. 10.1177%2F002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle C.E., Dugan E. Social isolation, loneliness and health among older adults. J. Aging Health. 2012;24(8):1346–1363. doi: 10.1177/0898264312460275. [DOI] [PubMed] [Google Scholar]
- Cruwys T., Dingle G.A., Haslam C., Haslam S.A., Jetten J., Morton T.A. Social group memberships protect against future depression, alleviate depression symptoms and prevent depression relapse. Soc. Sci. Med. 2013;98:179–186. doi: 10.1016/j.socscimed.2013.09.013. [DOI] [PubMed] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdur-Baker Ö., Bugay A. The short version of ruminative response scale: reliability, validity and its relation to psychological symptoms. Procedia Soc. Behav. Sci. 2010;5:2178–2181. doi: 10.1016/j.sbspro.2010.07.433. [DOI] [Google Scholar]
- Flynn M., Kecmanovic J., Alloy L.B. An examination of integrated cognitive-interpersonal vulnerability to depression: the role of rumination, perceived social support, and interpersonal stress generation. Cogn. Ther. Res. 2010;34(5):456–466. doi: 10.1007/s10608-010-9300-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girgus J.S., Yang K. Gender and depression. Curr. Opin. Psychol. 2015;4:53–60. doi: 10.1016/j.copsyc.2015.01.019. [DOI] [Google Scholar]
- Giuntella O., Hyde K., Saccardo S., Sadoff S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. 2021;118(9) doi: 10.1073/pnas.2016632118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaesmer H., Riedel-Heller S., Braehler E., Spangenberg L., Luppa M. Age- and gender-specific prevalence and risk factors for depressive symptoms in the elderly: a population-based study. Int. Psychogeriatr. 2011;23(8):1294–1300. doi: 10.1017/s1041610211000780. [DOI] [PubMed] [Google Scholar]
- Haslam C., Cruwys T., Haslam S.A., Jetten J. Social connectedness and health. Ency. Geropsychol. 2015;2015 doi: 10.1007/978-981-287-080-3_46-2. 46-1. [DOI] [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Human Bonding: The Science of Affectional Ties. 2013. Social connectedness and health; pp. 343–364. [DOI] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn A.B., Maercker A. Intra-and interpersonal emotion regulation and adjustment symptoms in couples: The role of co-brooding and co-reappraisal. BMC Psychology. 2016;4(1):1–11. doi: 10.1186/s40359-016-0159-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Vallières F.… Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020;142(3):249–256. doi: 10.1111/acps.13219. [DOI] [PubMed] [Google Scholar]
- Jetten J., Haslam C., Alexander S.H. Psychology press; 2012. The Social Cure: Identity, Health and Well-being. [Google Scholar]
- Jetten J., Haslam S.A., Cruwys T., Greenaway K.H., Haslam C., Steffens N.K. Advancing the social identity approach to health and well-being: progressing the social cure research agenda. Eur. J. Soc. 2017;47(7):789–802. doi: 10.1002/ejsp.2333. [DOI] [Google Scholar]
- Kontoangelos K., Economou M., Papageorgiou C. Mental health effects of COVID-19 pandemia: a review of clinical and psychological traits. Psychiatry Investig. 2020;17(6):491. doi: 10.30773/pi.2020.0161. 10.30773%2Fpi.2020.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K. PHQ-9: global uptake of a depression scale. World Psychiatry. 2021;20(1):135. doi: 10.1002/wps.20821. 10.1002%2Fwps.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 2002;32(9):509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Lades L.K., Laffan K., Daly M., Delaney L. Daily emotional well-being during the COVID-19 pandemic. Br. J. Health Psychol. 2020;25(4):902–911. doi: 10.1111/bjhp.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamblin M., Murawski C., Whittle S., Fornito A. Social connectedness, mental health and the adolescent brain. Neurosci. Biobehav. Rev. 2017;80:57–68. doi: 10.1016/j.neubiorev.2017.05.010. [DOI] [PubMed] [Google Scholar]
- Lee R.M., Draper M., Lee S. Social connectedness, dysfunctional interpersonal behaviors, and psychological distress: testing a mediator model. J. Couns. Psychol. 2001;48(3):310. https://psycnet.apa.org/doi/10.1037/0022-0167.48.3.310 [Google Scholar]
- Liao K.Y.H., Wei M. Intolerance of uncertainty, depression, and anxiety: the moderating and mediating roles of rumination. J. Clin. Psychol. 2011;67(12):1220–1239. doi: 10.1002/jclp.20846. [DOI] [PubMed] [Google Scholar]
- Lo C.S., Ho S.M., Hollon S.D. The effects of rumination and negative cognitive styles on depression: a mediation analysis. Behav. Res. Ther. 2008;46(4):487–495. doi: 10.1016/j.brat.2008.01.013. [DOI] [PubMed] [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malaquias S., Crespo C., Francisco R. How do adolescents benefit from family rituals? Links to social connectedness, depression and anxiety. J. Child Fam. Stud. 2015;24(10):3009–3017. doi: 10.1007/s10826-014-0104-4. [DOI] [Google Scholar]
- Maugeri G., Castrogiovanni P., Battaglia G., Pippi R., D'Agata V., Palma A., Musumeci G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. 2020;6(6) doi: 10.1016/j.heliyon.2020.e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehra A., Rani S., Sahoo S., Parveen S., Singh A.P., Chakrabarti S., Grover S. A crisis for elderly with mental disorders: relapse of symptoms due to heightened anxiety due to COVID-19. Asian. J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102114. 10.1016%2Fj.ajp.2020.102114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michl L.C., McLaughlin K.A., Shepherd K., Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: longitudinal evidence in early adolescents and adults. J. Abnorm. Psychol. 2013;122(2):339. doi: 10.1037/a0031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyawaki C.E. Association of social isolation and health across different racial and ethnic groups of older Americans. Aging Soc. 2015;35(10):2201. doi: 10.1017/S0144686X14000890. 10.1017%2FS0144686X14000890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D.C., Classen C., Barrera M. The relationship between social support, depression and treatment for depression in people with multiple sclerosis. Psychol. Med. 2004;34(3):533–541. doi: 10.1017/s0033291703001235. [DOI] [PubMed] [Google Scholar]
- Muldoon O.T., Haslam S.A., Haslam C., Cruwys T., Kearns M., Jetten J. The social psychology of responses to trauma: social identity pathways associated with divergent traumatic responses. Eur. Rev. Soc. Psychol. 2019;30(1):311–348. doi: 10.1080/10463283.2020.1711628. [DOI] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. J. Abnorm. Psychol. 1991;100(4):569. doi: 10.1037/0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., Aldao A. Gender and age differences in emotion regulation strategies and their relationship to depressive symptoms. Pers. Individ. 2011;51(6):704–708. doi: 10.1016/j.paid.2011.06.012. [DOI] [Google Scholar]
- Nolen-Hoeksema S., Wisco B.E., Lyubomirsky S. Rethinking rumination. Perspect. Psychol. Sci. 2008;3(5):400–424. doi: 10.1111/j.1745-6924.2008.00088.x. 10.1111%2Fj.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Pelizza L., Pupo S. COVID-19 epidemic and public mental health care in Italy: ethical considerations. Soc. Psychiatry Psychiatr. Epidemiol. 2020;55(8):1093–1094. doi: 10.1016/j.schres.2020.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Piet J., Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin. Psychol. Rev. 2011;31(6):1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Puterman E., DeLongis A., Pomaki G. Protecting us from ourselves: social support as a buffer of trait and state rumination. J. Soc. Clin. Psychol. 2010;29(7):797–820. doi: 10.1521/jscp.2010.29.7.797. [DOI] [Google Scholar]
- Rimes K.A., Watkins E. The effects of self-focused rumination on global negative self-judgements in depression. Behav. Res. Ther. 2005;43(12):1673–1681. doi: 10.1016/j.brat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Routledge C., FioRito T.A. Why meaning in life matters for societal flourishing. Front. Psychol. 2021;11:3925. doi: 10.3389/fpsyg.2020.601899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeri A.K., Cruwys T., Barlow F.K., Stronge S., Sibley C.G. Social connectedness improves public mental health: investigating bidirectional relationships in the New Zealand attitudes and values survey. Aust. N. Z. J. Psychiatry. 2018;52(4):365–374. doi: 10.1177/0004867417723990. 10.1177%2F0004867417723990. [DOI] [PubMed] [Google Scholar]
- Santini Z.I., Jose P.E., Cornwell E.Y., Koyanagi A., Nielsen L., Hinrichsen C., Koushede V.… Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1) doi: 10.1016/S2468-2667(19)30230-0. e62-e70. [DOI] [PubMed] [Google Scholar]
- Schoofs H., Hermans D., Raes F. Brooding and reflection as subtypes of rumination: evidence from confirmatory factor analysis in nonclinical samples using the dutch ruminative response scale. J. Psychopathol. Behav. Assess. 2010;32(4):609–617. doi: 10.1007/s10862-010-9182-9. [DOI] [Google Scholar]
- Schwartz H., Har-Nir I., Wenhoda T., Halperin I. Staying physically active during the COVID-19 quarantine: exploring the feasibility of live, online, group training sessions among older adults. TBM. 2021;11(2):314–322. doi: 10.1093/tbm/ibaa141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin M., McBride O., Murphy J., Miller J.G., Hartman T.K., Levita L., Bentall R.P.… Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych. Open. 2020;6(6) doi: 10.1192/bjo.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson S., Richardson L., Pietrabissa G., Castelnuovo G., Reid C. Videotherapy and therapeutic alliance in the age of COVID-19. Clin. Psychol. Psychother. 2020;28(2):409–421. doi: 10.1002/cpp.2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor C.T., Pearlstein S.L., Stein M.B. A tale of two systems: testing a positive and negative valence systems framework to understand social disconnection across anxiety and depressive disorders. J. Affect. Disord. 2020;266:207–214. doi: 10.1016/j.jad.2020.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsteinsson E.B., Ryan S.M., Sveinbjornsdottir S. The mediating effects of social support and coping on the stress-depression relationship in rural and urban adolescents. Open J. Depress. 2013;02(01):1–6. doi: 10.4236/ojd.2013.21001. [DOI] [Google Scholar]
- Tison G.H., Avram R., Kuhar P., Abreau S., Marcus G.M., Pletcher M.J., Olgin J.E. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann. Intern. Med. 2020;173(9):767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treynor W., Gonzalez R., Nolen-Hoeksema S. Rumination reconsidered: a psychometric analysis. Cogn. Ther. Res. 2003;27(3):247–259. doi: 10.1023/A:1023910315561. [DOI] [Google Scholar]
- Venville A., O’Connor S., Roeschlein H., Ennals P., McLoughlan G., Thomas N. Mental health service user and worker experiences of psychosocial support via telehealth through the COVID-19 pandemic: qualitative study. JMIR Ment. Health. 2021;8(8) doi: 10.2196/29671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Ho C.… A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Peng Z.… Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K.L., Galliher R.V. Predicting depression and self–esteem from social connectedness, support, and competence. J. Soc. Clin. Psychol. 2006;25(8):855–874. doi: 10.1521/jscp.2006.25.8.855. [DOI] [Google Scholar]
- Xiao S., Luo D., Xiao Y. Survivors of COVID-19 are at high risk of posttraumatic stress disorder. Global Health Research and Policy. 2020;5(1):1–3. doi: 10.1186/s41256-020-00155-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M., Gill H., Phan L., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye B., Wu D., Im H., Liu M., Wang X., Yang Q. Stressors of COVID-19 and stress consequences: The mediating role of rumination and the moderating role of psychological support. Child. Youth Serv. Rev. 2020;118:105466. doi: 10.1016/j.childyouth.2020.105466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ysseldyk R., McQuaid R.J., McInnis O.A., Anisman H., Matheson K. The ties that bind: Ingroup ties are linked with diminished inflammatory immune responses and fewer mental health symptoms through less rumination. PLoS ONE. 2018;13(4) doi: 10.1371/journal.pone.0195237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S.X., Wang Y., Rauch A., Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]