Abstract
Background
Current research on activities of daily living (ADLs) disability has mostly focused on the analysis of demographic characteristics, while research on the microcharacteristics of individuals and the macroenvironment is relatively limited, and these studies solely concern the impact of air quality on individual health.
Methods
This study innovatively investigated the impact of air quality on ADL disability by matching micro data of individuals from the China Health and Retirement Longitudinal Study with data of urban environmental quality from 122 cities. In this study, an ordered panel logit model was adopted for the benchmark test, and the two-stage ordered probit model with IV was used for endogenous treatment.
Results
This innovative study investigated the impact of air quality on ADL disability by matching individual micro data from the China Health and Retirement Longitudinal Study with urban environmental quality data for 122 cities. The results showed that air quality significantly increased the probability of ADL disability. The positive and marginal effect of air quality on moderate and mild disability was higher. Generally, the marginal effect of air quality on residents’ health was negative. In terms of group heterogeneity, the ADL disability of individuals aged over 60 years, those in the high Gross Domestic Product (GDP) group, females, and those in the nonpilot long-term care insurance group was more affected by air quality, and the interaction between air quality and serious illness showed that the deterioration of air quality exacerbated the ADL disability caused by serious illness; that is, the moderating effect was significant.
Conclusions
According to the equilibrium condition of the individual health production function, the ADL disability caused by a 1% improvement in air quality is equivalent to the ADL disability caused by an 89.9652% reduction in serious illness, indicating that the effect of improved air quality is difficult to replace by any other method. Therefore, good air quality can not only reduce ADL disability directly but also reduce serious illness indirectly, which is equivalent to the reduction of ADL disability. This is called the health impact.
Keywords: Air quality, ADL disability, CHARLS, Pollutants, Ordered logit
Introduction
Since the beginning of the twenty-first century, the rapid development of China’s economy has been accompanied by a considerable increase in Gross Domestic Product (GDP). The per capita GDP reached 72,371 yuan in 2020 [1]. Consequently, the living standards of residents have also significantly improved. However, air pollution caused by economic development in all parts of China also increased, negatively impacting the health of the Chinese people. Outdoor air pollution was included in the list of carcinogens published by the International Agency for Research on Cancer of the World Health Organization in 2017 because dense particulate matter in the air can cause a significant impact on human health [2]. Both in China and globally, environmental protection is increasingly becoming a major issue for society as a whole. In 2017, Comrade Xi Jinping prioritized protecting the environment and maintaining harmony between man and nature in the 19th major report of the committee party [3]. Currently, it is necessary to adhere to the development concept of “Green mountains and green waters are golden mountains and silver mountains” and follow the basic state policy of conserving resources and protecting the environment. Individuals recognize that environmental protection is related to their fundamental wellbeing. Therefore, the study of air quality as it relates to environmental protection has important theoretical and practical significance.
Furthermore, from the perspective of China’s ageing population, disability has increasingly become a major livelihood problem. Existing research on the disabled population mostly focuses on the analysis of public and social policies or is conducted from a medical perspective. These studies include the analysis of the effectiveness of long-term care insurance (LTCI) for the disabled population [4, 5]; the analysis of the social characteristics of disabled people and their average life expectancy [6–8]; and the analysis of the internal physical changes that occur due to disability using the disability evaluation scale [9, 10].. On the other hand, from the perspective of air quality, the study of residents’ disability is rare. However, existing research has shown that changes in air quality have an important impact on human health. The change in individual health, especially the impact of serious illness, is usually the key factor or even the only direct factor for the impairment in activities of daily living (ADLs). Therefore, to address these gaps in the research, this study aimed to assess the impact of air quality on ADL disability in Chinese residents. The findings discussed here will provide evidence for prioritizing government programs to deal with the issues of ADL disability.
Literature review
There is abundant research concerning the impact of air pollution on health. From the macro perspective of health impact, Usmani et al. clearly gave the definition of air pollution, the motivation to study air pollution, and the impact and source of air pollution and climate change [11]. Han et al. provided a new measurement standard for evaluating global health inequality from the perspective of climate change and air pollution control efficiency (abbreviated as APCI) [12]. In general, air pollution is closely related to the national or regional average health level. If emission reduction efforts are shared by all countries, in all scenarios, the benefits of common health would far exceed the political costs [13]. Based on the exposure response function of epidemiology, it was revealed that the impact of future temperature changes on citizens’ health is more significant than the change in air pollutant concentration [14]. Among the environmental indicators, cultivated land is the indicator that shows the greatest impact on health and wealth in the next 10 years, while air pollution has the least impact on health and wealth for low-income countries [15]. However, it was found that environmental and air pollution impose a great threat on the health and wealth of residents in low-income countries. Moreover, there are significant differences in the effects of different pollutants. From the perspective of the impact pathway of pollution, NO2 and O3 are more important, and their AR (added health risk) decreases significantly in urban areas with crowded traffic, but no significant change in AR was found in other areas with low urbanization [16].
Among the research on individual health impacts, on the one hand, air pollution indeed has an impact on individual health [17–21]; on the other hand, it also affects potential medical consumption [22, 23]. In detail, (1) as one of the primary outcomes of the impact of air pollution, the death rate of respiratory diseases is increasing significantly [24], and this economic cost even exceeds the economic benefits. As a result, production efficiency decreased. For instance, based on the HAQI (health risk-based AQI), it was estimated that 20% of the population in the study area was exposed to polluted air. The total mortality rates caused by PM10, PM2.5, SO2, O3, NO2, and CO were 3.00, 1.02, 1.00, 4.22, 1.57, and 0.95%, respectively [25]. In addition, inhalable particles in air pollutants affect individual health mainly in two ways: one is the short-term effect on the human respiratory tract, which can cause respiratory tract infection, chronic obstructive pulmonary disease, lung cancer, and other respiratory diseases [26–29]; the other is the long-term impact on the respiratory tract that involves the triggering of the inflammatory cascade through local inflammatory factors, ultimately leading to a significant increase in the risk of cardiovascular and nervous system diseases [30–34]. As the research revealed, when PM10 and O3 in air pollutants increase by 10 μg/m3 and 10 ppb, the number of visitors to respiratory hospitals in 1 day will increase by 10.39 and 10.93%, respectively. This would bring about additional medical expenses of $67 million and $70 million, respectively [35]. Furthermore, the health effects of air pollution vary under different socioeconomic statuses. For example, self-rated air pollution has the greatest impact on the self-rated health of low socioeconomic groups, while with the improvement of socioeconomic status, the impact of self-rated air pollution on self-rated health decreases [36]. (2) Air pollution indirectly affects residents’ medical consumption. Sun et al. demonstrated that air pollution is also the main factor that influences residents’ expenditures on health management [37]. Theoretically, air pollution affects health mainly in two ways: first, the reduction in sleep time caused by ambient air pollution is not conducive to health; second, people spend more time on sedentary activities to avoid exposure to air pollution, which will indirectly lead to an increase in personal medical expenditure [38]. Additionally, from the empirical results, air pollution will lead to a significant increase in medical expenses, hospitalization expenses and extrabudgetary expenses [38]. For example, Liu et al. estimated age- and cause-specific premature deaths and quantified related health damage with the measurement of the age-adjusted value of statistical life (VSL). Their results suggest that while premature deaths fell as a result of China’s clean air actions, the health costs of air pollution remained high [39].
Most of the existing studies on residents’ ADLs are based on the micro viewpoints of individual disease risk. For example, in ADL disability assessment, based on the diagnosis rate of major diseases, individual disease risks are defined by establishing the relevant Disability Assessment Scale [5, 6]. However, even in countries or regions with long-term implementation of health care insurance, the impact of air pollution on residents’ ADL disability has rarely been investigated, neither in practice nor in theory. This also illustrates the major significance of this study. Current research in this field focuses on the factors that influence the population’s health via urban green spaces, the ecological environment and air quality. The findings from such studies show that the deterioration of the ecological environment negatively impacts human health. However, there are some gaps in the existing research. First, although there are relatively abundant studies on the impact of the ecological environment on individual health, the majority of these focus on direct health effects, ignoring the cumulative indirect effects of changes in environmental quality. Furthermore, these studies focus only on medical expenses. Second, in the measurement of air quality, the traditional air pollution index (API) or the concentration of a single pollutant are often used for testing. Although it is suitable to investigate the impact of a single pollutant, for estimates that are closer to the real-world impact, testing should include a comprehensive list of pollutants. Third, existing studies mainly focus on the impact of air quality on individual health without fully considering internal transmission mechanisms through which air quality affects health. To address these gaps, this study focused on the following points. First, we investigated the indirect impact of air pollution by assessing the decline in residents’ basic activities of daily living (ADLs). Second, sulfur dioxide (SO2), nitrogen dioxide (NO2) and inhalable particles (PM10) were included as proxy variables, and China Health and Retirement Longitudinal Study (CHARLS) data from 2015 and 2018 were matched with macro regional air quality data to construct panel data. Heterogeneity analysis and endogenous problem processing were used to ensure the reliability of the test results. The air quality index (AQI) was introduced to investigate the robustness of the results, considering the heterogeneity of a single air quality index and the overall impact. Third, by constructing the health production function, we investigated the substitution effect of air quality and serious illness on individual ADL disability and tested the transmission mechanism of air quality impacting individual ADL disability.
Methods
Theoretical hypothesis: impact of air quality on health
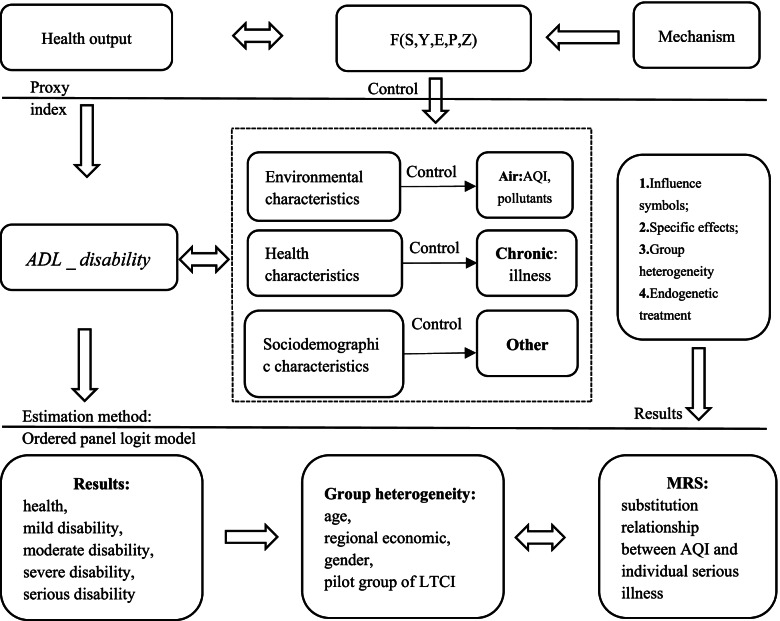
The health demand model was first proposed by Grossman [40], and the health production function, which is the core of the supply model, is derived from it. The health production function can be divided into macro and micro parts, which are interrelated. Among them, the microhealth production function emphasizes the relationship between family- or individual-level medical and health input and individual health output through macro policy intervention [41, 42]. The macrohealth production function considers the overall output effect of national health from the perspective of macroeconomics, government health expenditure, and medical insurance [43]. This study investigated air quality effects from a macro perspective by analysing the macro health production function. The theoretical mechanism of the impact of air pollution on residents’ health is shown in Fig. 1.
Fig. 1.
Theoretical mechanism of the impact of air pollution on Residents’ ADL disability
Based on Grossman’s health demand model, Filmer et al. [44] constructed a macro health production function model. Health needs are formed by the correlation between health and related factors that improve health. The core of the health production function is composed of output factors and health inputs. Due to the relevant hypothesis bias in the micro field, there is an estimation bias in the analysis of medical and health policy inputs and outputs using the perfect competition market model. Therefore, more nonendogenous factors must be explained. When health economists use the general production function theory, combined with health characteristics, they put forward that in the process of maintaining or improving health, the input and output of medical and health resources are included in the basic health production function. Therefore, the general health production function can be expressed as:
| 1 |
Equation (1) is the national health level at a certain time point, where S represents the input of social factors, Y is the input of economic variables, E is the input of educational variables, P is the input of medical and health policies and Z is the social health investment. However, the existing health production function does not consider the impact of the natural environment or air quality. Therefore, this study used individual ADL disability as a proxy for health variables and assumed that ADL disability is influenced by sociodemographic, regional environmental and individual health characteristics [45]. Here, sociodemographic characteristics include gender, age, household-registered marital status, etc. Regional environmental characteristics include regional financial expenditure, per capita GDP, population density, sunshine duration and rainfall. Individual health characteristics include serious illness, depression and self-reported health. Therefore, the health production function can be adjusted as follows:
| 2 |
In Eq. (2), ADL _ disability is calculated; R on the right side of the equation represents the regional environmental characteristics, H represents the individual health characteristics, and S represents the individuals’ sociodemographic characteristics. Based on existing research and the objectives of this study, air quality was considered the primary factor of ADL disability, while other influencing factors were taken as control variables. Therefore, Eq. (2) can be adjusted as follows:
| 3 |
The pilot for China’s LTCI showed that the most important cause of disability for most severely disabled persons was the occurrence of serious illness [5]. Therefore, this study considered the rate of serious illness (i.e., diagnosis rate of serious illness) as an important regulatory index to investigate the detrimental effect of air quality on individual ADL. The Chronic on the right of Eq. (3) is the serious illness rate. In addition, after controlling for other factors, we can further investigate the substitution relationship between air quality and serious illness, which can be derived from Eq. (3). When the individual ADL disability remains unchanged, it should be equal to 0, that is:
| 4 |
Then, the marginal substitution rate between air quality and residents’ serious illnesses can be:
| 5 |
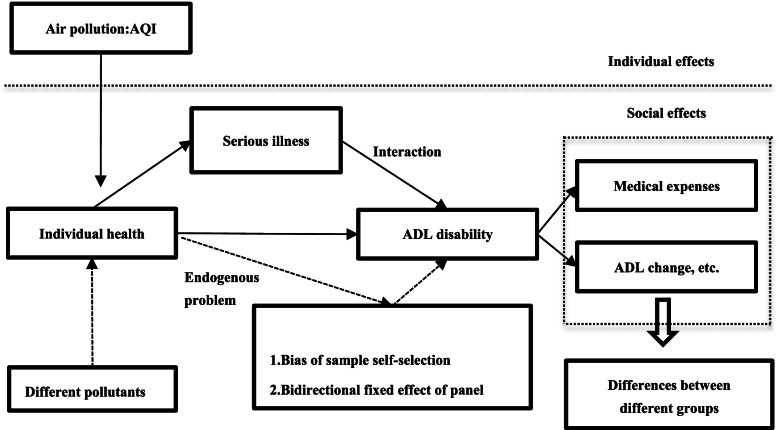
Equation (5) shows the substitution relationship between air quality and individual serious illness under the condition of constant ADL disability. Therefore, the reduction in individual serious illness by a one-unit improvement in air quality represents the health impact of air quality, which is measured by the changes in ADL disability due to air quality. The empirical method testing the impact of air pollution on residents’ health is shown in Fig. 2.
Fig. 2.
Effect of air pollution on the ADL disability of residents
Test model
Based on the above theoretical analyses of the health impact of air quality, this study further constructed an empirical test model. Considering that the core explanatory variable of this study was residents’ ADL disability, we classified ADL disability. Please refer to the definitions of core explanatory variables and classifications in the data section for specific explanations. This implied that the traditional OLS estimation would result in bias; therefore, the ordered panel logit model was selected for the test:
| 6 |
In Eq. (6), ADL _ disability represents the ADL disability of individual i living in city j in year t, which is the primary explained variable of this study; Airjt on the right side of the equation represents the air quality of city j in year t, which is another primary explanatory variable of this study. In this study, SO2, NO2, and PM10 in the API were selected as proxies of air quality, and the AQI was selected for the robustness test. In the data processing step, to avoid the influence of nondimensional values, logarithmic processing was used. Hijt represents individual health characteristics, including individual serious illness rate, self-reported health and physical pain. Rjt represents the environmental characteristics of j city in t year, including annual rainfall and annual sunshine duration. S indicates sociodemographic characteristics such as gender, age, marital status, etc. Since the panel logit model only provides the test results of random effects, to ensure reliable results, the individual effect, regional effect, and year effect were controlled simultaneously in the model, which were λi, δj and ηt in Eq. (6), respectively. εijt represents random error. Furthermore, the health production function of Eq. (6) is nonlinear; therefore, it satisfies the following conditions:
| 7 |
where ADL _ disabilityijt∗ is the unobservable continuous variable of ADL _ disabilityijt, which is the latent variable and satisfies the assumption of linearity. In Eq. (7), r0, r1, r2... denote the parameters to be estimated. To keep the ADL disability of residents unchanged, we can investigate how serious illness was impacted when air quality deteriorates. Based on the above analysis, the marginal substitution rate between air quality and serious illness can be adjusted to Eq. (8) based on Eq. (5), where |α/β| is the substitution rate between serious illness and air quality, as given below:
| 8 |
Considering the characteristics of the health production function, we should determine the substitution relationship between air quality and serious illness and how to improve air quality and reduce serious illness at the same time when the overall ADL disability is reduced. This is for determining the scale effect of the health production function and verifying the marginal effect of each variable in the real test, which will be discussed later.
Data
Individual ADL disability data
The individual micro data of this study were obtained from the CHARLS surveys of 2015 and 2018. The data that support the findings of this study are openly available at the following URL/DOI: http://charls.pku.edu.cn/. In this dataset, there were 12,520 participants from 2015 and 13,358 from 2018. By controlling for individual and time effects, as well as for sociodemographic characteristics of the population and the macro characteristics of the city, the reliability and accuracy of the estimated effect of air quality on individual ADLs were improved.
The core explanatory variable for the analysis was the ADL disability of residents, and the specific indicators were defined as follows: ADLs were determined based on the question “whether you have difficulties in dressing, bathing, eating, getting up and out of bed, going to the toilet, controlling defecation and defecation”. The score for this question was based on the selection of options from 1-no difficulty, 2-difficulty but still can be completed, 3-difficulty and need help, and 4-unable to complete. In total, six basic self-care ability indicators were used, and the total score ranged from 6 to 24. Based on the existing classification of disability, ADL disability was divided into five levels: serious disability, severe disability, moderate disability, mild disability, and healthy [6]. Through data processing, a total score of 6 was recorded as 5, which represented “healthy”; a score of 7–9 was defined as 4, indicating a mild disability; a score of 10–14 was recorded as 3, indicating moderate disability; a score of 15–20 was defined as 2, which indicated severe disability; and a score of 21–24 was 1, which indicated serious disability. Therefore, a higher ADL disability score indicated a lower degree of ADLs.
The statistics of the probability of ADL disability are presented in Table 1. As shown in Table 1, the rates of serious disability, severe disability and moderate disability increased from 2015 to 2018. The proportion of people with severe and mild ADL disability in the total population increased from 6.29 to 7.93%, but the proportion was still lower than that with mild disability. In addition, the proportion of the healthy population increased by a small degree during this period.
Table 1.
Probability statistics of ADL disability
| ADL disability | 2015 | 2018 | ||
|---|---|---|---|---|
| Relative frequency | Frequency (%) | Relative frequency | Frequency (%) | |
| Serious disability | 23 | 0.18 | 92 | 0.69 |
| Severe disability | 101 | 0.81 | 174 | 1.30 |
| Moderate disability | 664 | 5.30 | 794 | 5.94 |
| Mild disability | 2664 | 21.28 | 2482 | 18.58 |
| Healthy | 9068 | 72.43 | 9816 | 73.48 |
Air quality data
There are many measurement indicators of air pollution, such as the air quality index (AQI) and air pollution index (API). While the main pollutants in exhaust gas were mainly industrial emissions, the API indicator was not a comprehensive measure of air quality [46]. The AQI is a more comprehensive measure, and its data are released once an hour. Therefore, it is advantageous to use the annual average AQI value to investigate the impact of air quality on ADL disability [47].
Control variables
In addition to air quality, the main factors of ADL disability include sociodemographic characteristics and other factors. The definition and statistics of the control variables in this study are shown in Table 2, including the regional natural environment, economic environment, and individual and family characteristics.
Table 2.
Descriptive statistics of main variables
| Variable | Definition | 2015 (12520) | 2018 (13358) | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| ADL disability | 1 ~ 5; higher score indicated lower ADL disability | 4.651 | 0.513 | 4.636 | 0.595 |
| SO2 | SO2 content in air (μg /m3) | 27.53 | 17.96 | 16.26 | 10.58 |
| NO2 | NO2 content in air (μg /m3) | 32.74 | 11.62 | 39.23 | 15.93 |
| PM10 | PM10 content in air (μg /m3) | 94.38 | 40.94 | 89.74 | 40.32 |
| AQI | Dimensionless air quality; greater value indicated poorer quality | 85.76 | 25.79 | 72.14 | 16.55 |
| Fiscal expenditure | Total annual financial expenditure of the region (million yuan) | 544.9 | 729.6 | 688.0 | 1030 |
| Sunshine duration | Total sunshine duration in the whole year, (hour) | 1814 | 469.0 | 1903 | 354.4 |
| Rainfall | Annual total rainfall (mm) | 1067 | 624.8 | 997.3 | 441.2 |
| Per capita GDP | Annual regional GDP to population ratio, (yuan / person) | 49,467 | 34,418 | 56,468 | 35,992 |
| Population density | Annual area to population ratio (Person / m2) | 490.1 | 479.4 | 492.6 | 473.1 |
| Average temperature | Annual average temperature (centigrade) | 15.24 | 3.867 | 15.08 | 3.926 |
| GDP growth | Regional GDP growth compared with the previous year | 8.078 | 2.081 | 7.054 | 1.823 |
| Green space coverage | Ratio of green area to total area (in built up area) | 39.54 | 9.130 | 39.96 | 5.022 |
| Relative humidity | Percentage of water vapor pressure in air to saturated vapor pressure at the same temperature | 64.65 | 12.39 | 65.03 | 10.64 |
| Household register | Urban = 1, rural = 0 | 0.401 | 0.490 | 0.405 | 0.491 |
| Income | 1 ~ 5 respectively represent high income, middle-high-income, middle income, lower-middle-income and low income | 2.605 | 0.783 | 2.754 | 0.803 |
| Basic medical insurance | Enjoying basic medical insurance = 1, no = 0 | 0.945 | 0.137 | 0.971 | 0.168 |
| Marital status | Widowed = 1, no = 0 | 0.103 | 0.304 | 0.125 | 0.330 |
| Serious illness | Number of serious illnesses diagnosed; higher value indicates a greater number of illnesses | 0.0294 | 0.286 | 0.724 | 1.052 |
| Depression | 1–4; higher score indicates more severe depression | 2.468 | 0.740 | 2.275 | 0.783 |
| Self-reported health | 1 ~ 5; higher value indicates better health | 2.955 | 0.721 | 2.946 | 0.986 |
| Body disability | 0–5; higher score indicates more severe body disability | 0.154 | 0.444 | 0.145 | 0.445 |
| Physical pain | 1–5; higher score indicates more severe pain | 1.705 | 0.456 | 2.159 | 1.267 |
| Age | Actual age of the individual in the survey year | 59.14 | 10.32 | 58.74 | 10.32 |
| Gender | Male = 1, female = 0 | 0.478 | 0.500 | 0.474 | 0.499 |
| Education level | 1–11 respectively represent No formal education (illiterate),Did not finish primary school, Sishu/home school, Elementary school, Middle school, High school, Vocational school, Two−/Three-Year College/Associate degree, Four-Year College/Bachelor’s degree, Master’s degree, Doctoral degree/Ph.D. | 3.390 | 1.001 | 3.477 | 1.935 |
Abbreviations: ADL Activities of Daily Living, AQI Air Quality Index, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: Standard errors are in brackets; *** p < 0.01, ** p < 0.05, * p < 0.1. The model controls for both the year and individual effects to consider the influence of unobservable factors
Table 2 shows that the variation coefficients of ADL disability in 2015 and 2018 were 0.110 and 0.128, respectively. The degree of dispersion was small, and mild disability and health were the main parts. On the other hand, the variation coefficients of the concentrations of SO2, NO2 and PM10 were 0.652, 0.651, and 0.355 in 2015, respectively, and changed to 0.406, 0.434, and 0.449 in 2018. Thus, the variations in NO2 and PM2 were similar, while the dispersion of SO2 was relatively larger. The statistical values of the AQI in 2015 and 2018 were 85.76 and 72.14, respectively, which means that the air quality apparently improved in 2018.
Results
Benchmark regression
In the benchmark regression, the effects of different pollutant concentrations were tested, and the results are presented in Table 3. Models (1)–(3) are the results of the stepwise test of air pollutant concentration effects, controlled by individual and time effects, whereas Model (4) is based on the AQI. The results show that both SO2 and PM10 have significant and negative effects on ADL disability. The significance level of SO2 was low, whereas the results for the coefficient of PM10 were more robust. In other words, higher concentrations of SO2 and PM10 in the air have brought about a higher degree of ADL disability. These results demonstrate that an increased concentration of air pollutants aggravates the degree of ADL disability and that PM10 plays a more important role. The results of Model (4) show that air quality has a significant and negative impact on residents’ ADL disability; the worse the air quality is, the higher the degree of residents’ ADL disability. This result proves the robustness of the results of pollutant concentrations.
Table 3.
Impact of air quality on ADL disability: Benchmark regression
| Variable | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| lnSO2 | − 0.0599*(0.0355) | |||
| lnNO2 | −0.0017(0.0533) | |||
| lnPM10 | − 0.1056**(0.0510) | |||
| lnAQI | − 0.1543**(0.0721) | |||
| Fiscal expenditure | − 0.0057(0.0276) | 0.0015(0.0273) | − 0.0027(0.0274) | − 0.0018(0.0271) |
| Sunshine duration | − 0.0204(0.0865) | − 0.0311(0.0861) | − 0.0364(0.0864) | −0.0219(0.0857) |
| Rainfall | 0.1173*(0.0620) | 0.1353**(0.0620) | 0.1015(0.0624) | 0.1232**(0.0611) |
| Per capita GDP | 0.0403(0.0330) | 0.0361(0.0357) | 0.0473(0.0334) | 0.0344(0.0328) |
| Population density | 0.0596***(0.023) | 0.0513**(0.0238) | 0.0744***(0.025) | 0.0666***(0.0237) |
| Average temperature | −0.4412***(0.093) | −0.4373***(0.093) | − 0.4503***(0.094) | − 0.4203***(0.0925) |
| GDP growth | 0.0139(0.0090) | 0.0159*(0.0090) | 0.0174*(0.0090) | 0.0173*(0.0089) |
| Green space coverage | 0.0007(0.0022) | 0.0007(0.0022) | 0.0005(0.0022) | 0.0004(0.0022) |
| Relative humidity | −0.0010(0.0029) | −0.0007(0.0029) | − 0.0014(0.0029) | −0.0017(0.0029) |
| Household register | 0.1030***(0.036) | 0.1015***(0.036) | 0.0968***(0.036) | 0.0701*(0.0358) |
| Income | −0.0190(0.0223) | −0.0186(0.0223) | − 0.0200(0.0223) | −0.0191(0.0222) |
| Basic medical insurance | 0.2187(0.1489) | 0.2232(0.1488) | 0.2269(0.1489) | 0.2268(0.1485) |
| Marital status | −0.1834**(0.072) | −0.1827**(0.072) | − 0.1837**(0.0721) | −0.2654***(0.0725) |
| Serious illness | 0.0486*(0.0271) | 0.0491*(0.0271) | 0.0506*(0.0271) | 0.0546**(0.0270) |
| Depression | 0.1194***(0.025) | 0.1183***(0.0251) | 0.1194***(0.025) | 0.1513***(0.0252) |
| Self-reported health | 0.0930***(0.020) | 0.0933***(0.0198) | 0.0937***(0.020) | 0.0866***(0.0197) |
| Body disability | −0.6474***(0.049) | −0.6473***(0.049) | − 0.6472***(0.049) | −0.6378***(0.0490) |
| Physical pain | −0.0369*(0.0215) | −0.0375*(0.0215) | − 0.0370*(0.0215) | −0.0415*(0.0215) |
| Age | −0.0017(0.0020) | −0.0017(0.0020) | − 0.0017(0.0020) | −0.3707***(0.0347) |
| Gender | −0.3703***(0.035) | −0.3705***(0.035) | − 0.3707***(0.035) | 0.0010(0.0020) |
| Education | −0.0350***(0.011) | −0.0350***(0.011) | − 0.0349***(0.011) | −0.0132(0.0110) |
| Individual / Year | Yes | Yes | Yes | Yes |
| |α/β| | 1.2325 | 0.0346 | 2.0870 | 2.8260 |
| sigma2_u | 1.7866***(0.119) | 1.7859***(0.119) | 1.7901***(0.119) | 1.7249***(0.1194) |
| Pseudo log likelihood | − 27,316.835 | − 27,318.331 | − 27,316.157 | − 27,260.191 |
| Observations | 26,218 | 26,218 | 26,218 | 26,218 |
Abbreviations: AQI Air Quality Index, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: Standard errors are in brackets; * p < 0.01, * p < 0.05, * p < 0.1. The pseudo log-likelihood value in the table is log pseudolikelihood
In terms of control variables, population density, annual rainfall and annual average temperature had significant effects on ADL disability. Population density and annual rainfall had positive effects: the higher the population density and annual rainfall were, the lower the degree of ADL disability. On the other hand, annual average temperature had negative effects: the higher the annual average temperature was, the higher the degree of ADL disability. Regarding individual characteristics, household registration, depression, self-reported health and serious illness had positive effects on ADL disability, but marital status, disability, physical pain, gender and education had significant and negative effects on ADL disability.
These results demonstrate that the concentration of air pollutants has a significant impact on ADL disability, and among the control variables, the basic health status of individuals is the primary factor affecting ADL disability. Moreover, by looking into the marginal substitution effect of air quality and serious illness, to maintain the level of ADL disability, the decrease in ADLs caused by a 1% increase in SO2, NO2, PM10 and the AQI needs to be compensated by a 1.2325, 0.0346, 2.087, and 2.826% reduction in the serious illness, respectively. The substitution relationship between air quality and other health variables can also be investigated; however, they were not of interest to this study.
Marginal effect analysis
Based on Table 3, the marginal effect of air quality on ADL disability can be further estimated, and the results are shown in Table 4. Because the ordered logit model can only provide limited information on the signs and significance of parameters, it is necessary to estimate the marginal effect of air quality on ADL disability. When all explanatory variables are at the mean value, the influence of the exogenous explanatory variables can be expressed as Eq. (9):
| 9 |
Table 4.
Marginal effect of air quality on ADL disability
| ADL disability | lnSO2 | lnNO2 | lnPM10 | lnAQI |
|---|---|---|---|---|
| Serious disability | 0.00003(0.00002) | 8.42e-07(0.00003) | 0.00005*(0.00003) | 0.00008*(0.00004) |
| Severe disability | 0.00013*(0.0001) | 3.77e-06(0.0001) | 0.0002**(0.0001) | 0.0003**(0.0002) |
| Moderate disability | 0.0012*(0.0007) | 0.00003(0.0010) | 0.0020**(0.0010) | 0.0030**(0.0014) |
| Mild disability | 0.0045*(0.0026) | 0.0001(0.0040) | 0.0079**(0.0038) | 0.0115**(0.0054) |
| Healthy | −0.0110*(0.0063) | − 0.0003(0.0098) | − 0.0194**(0.0094) | − 0.0284**(0.0133) |
Abbreviations: ADL Activities of Daily Living, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: The standard error is in brackets; *** p < 0.01, ** p < 0.05, * p < 0.1. The control variable results are not listed here
Table 4 shows the marginal effects of air quality on the ADL disability of residents. PM10 is the primary factor affecting ADL disability, and when the PM10 concentration is increased by 1 unit, the probability of serious disability, severe disability, moderate disability, mild disability and healthy status of residents is significantly increased by 0.005, 0.02, 0.20, 0.79 and 1.94%, respectively. The marginal effect of NO2 is very weak and nonsignificant. In comparison, when the SO2 concentration was increased by one unit, the increase in the probability of serious disability, moderate disability and mild disability was 0.013, 0.12 and 0.45%, respectively, whereas the health reduction probability was − 1.10%. From the test of the marginal effect of the AQI, the above results are robust. The marginal effect of the AQI on severe, mild severe, moderate and mild disability is positive, and the marginal effect of the AQI on moderate and mild disability is higher. If the AQI is increased by 1 unit, the probability of moderate and mild disability increases by 0.30 and 1.15%, respectively. Meanwhile, the marginal effect of the AQI on health reaches 2.84%, which means that a 1 unit increase in the AQI leads to a 2.84% decrease in the probability of residents’ health.
Analysis of group heterogeneity
To investigate the variations in the impact of air quality on ADL disability between different groups, analysis models were stratified according to age, regional economy (GDP), gender and LTCI policy pilot. These results are shown in Table 5.
Table 5.
Heterogeneity of ADL disability among different groups of residents affected by air quality
| Grouping | Indicators | lnSO2 | lnNO2 | lnPM10 | lnAQI | Observations |
|---|---|---|---|---|---|---|
| Age group | Under 60 years | 0.0170 (0.0452) | 0.0917 (0.0671) | −0.0078 (0.0653) | − 0.1352 (0.0921) | 15,526 |
| Over 60 years old | −0.1530*** (0.0567) | −0.1069 (0.0869) | − 0.2208*** (0.0801) | −0.1531 (0.1140) | 10,692 | |
| Regional economic status | Low GDP group | −0.0074 (0.0408) | 0.0112 (0.0576) | −0.0771 (0.0611) | −0.1275 (0.0896) | 18,952 |
| High GDP group | −0.2994*** (0.0907) | −0.1410 (0.1680) | − 0.3922*** (0.1316) | −0.2325 (0.1521) | 7266 | |
| Gender | Male | −0.0067 (0.0494) | 0.0739 (0.0739) | −0.0127 (0.0712) | −0.2606*** (0.0999) | 12,225 |
| Female | −0.1121** (0.0503) | −0.0696 (0.0753) | − 0.1812** (0.0720) | −0.0627 (0.1038) | 13,993 | |
| Long term insurance pilot | Pilot was launched | 0.3958 (6.8008) | −2.5769 (44.2767) | −0.3120 (5.3616) | −2.2673 (38.9568) | 419 |
| No pilot was conducted | −0.0597* (0.0358) | −0.0048 (0.0535) | − 0.1097** (0.0515) | −0.1475** (0.0727) | 25,799 |
Abbreviations: AQI Air Quality Index, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: Standard errors are in brackets; *** p < 0.01, ** p < 0.05, * p < 0.1. The control variable results are not listed here
Regarding age, we used the elderly population with higher ADL disability risk as the division reference; thus, those aged 60 years and above were divided from others. The results show that compared with the age group under 60 years, air quality has a significantly higher impact on ADL disability of residents over 60 years. SO2 and PM10 have a significant impact on the ADL disability of residents over 60 years. This indicates that under the same conditions, the probability of ADL disability in elderly individuals brought by air quality deterioration is higher than that of the nonelderly population. However, there was no significant difference in the effect of the AQI on ADL disability by age.
In terms of regional economy, we selected the regional economic aggregate as the grouping standard; that is, the regional GDP lower than the average GDP was the low economic group, whereas the regional GDP higher than the average GDP was assigned to the high economic group. The results showed that compared with the low economic group, air quality had a more significant and negative effect on ADL disability in the high economic group. This is probably because the areas with stronger economies tend to promote better quality of life. Areas of strong economic development also have higher population density and more urban automobile pollution and industrial pollution, thus resulting in a significantly higher impact of air quality on ADL disability. In the low-level economic development area, the situation is the opposite. However, there was no significant difference in the effect of the AQI on ADL disability of different regional economic groups.
Moreover, compared with male residents, air quality had a more significant impact on ADL disability in female residents. This is because the life expectancy of female residents is generally higher than that of male residents, and in daily life, female residents are mainly engaged in household activities. Therefore, females experience more ADL disability related to cooking fume inhalation at home than males. However, the impact of the AQI on ADL disability was more significant for male residents since in general, workers in the mining industry are mostly men. Therefore, the impact of outdoor air pollution is higher for males, which increases the probability of ADL disability.
For the LTCI pilot group, the dummy variable of the pilot policy was constructed according to the implementation time of the LTCI policy in 15 pilot cities in 2016, whereby the nontreatment group and treatment group were determined. The results show that compared with the pilot areas, the air quality in the nonpilot areas had a more significant impact on ADL disability; that is, the LTCI pilot reduced the risk of ADL disability caused by air quality and promoted the prevention or rehabilitation of ADL disability among residents.
Analysis of the interaction between air quality and serious illness
Among the individual characteristics that affect ADL disability, serious illness was the most important factor. Previous theoretical research on LTCI shows that the disabled population is mainly affected by serious illnesses such as cerebral haemorrhage and cerebral infarction. Therefore, it is of great theoretical significance to investigate the interaction between serious illnesses and air quality. The test results of the interaction items are presented in Table 6. The interaction terms of serious illness and SO2 and the interaction of serious illness and NO2 play a significant and positive role in ADL disability, and the serious disease rate has a significant and negative effect on ADL disability. However, from Table 3, which shows the estimation results for the models without interaction items, the impact of serious illness on ADL disability was significantly positive, which is contrary to reality and theory. The results for Model (4) in Table 6 also show that the interaction terms have a positive moderating effect but are not significant.
Table 6.
Estimation of the effects of the interaction between air quality and serious illness on ADL disability
| Variable | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| lnSO2 | −0.0882**(0.0367) | |||
| lnNO2 | −0.0538(0.0555) | |||
| lnPM10 | −0.1246**(0.0530) | |||
| lnAQI | −0.1548**(0.0724) | |||
| Serious illness | −0.2328*(0.1317) | −0.4058**(0.2038) | − 0.1697(0.2315) | 0.0126(0.0442) |
|
X × lnSO2/ X × lnNO2/ X × lnPM10/ X × lnAQI |
0.1043**(0.0478) | 0.1266**(0.0557) | 0.0496(0.0517) | 0.0225(0.0185) |
| Individual / Year | Yes | Yes | Yes | Yes |
| /sigma2_u | 1.7819***(0.1183) | 1.7848***(0.1186) | 1.7891***(0.1186) | 1.7806***(0.1183) |
| Pseudo log likelihood | −27,313.284 | −27,314.254 | − 27,315.495 | −27,315.248 |
| Observations | 26,218 | 26,218 | 26,218 | 26,218 |
Abbreviations: AQI Air Quality Index, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: Standard errors are in brackets; *** p < 0.01, ** p < 0.05, * p < 0.1. The control variable results are not listed here
X is the rate of serious illness
The estimation results of the interaction terms suggest that air quality aggravated ADL disability caused by serious illness, and the interaction terms of serious illness and the concentrations of SO2 and NO2 were the main factors in the positive promotion effect on ADL disability. The primary reason for this might be that the increase in air pollutants increases the probability of residents suffering from serious illness, thus aggravating the risk of ADL disability.
Extensive analysis
The effect of air quality on ADL disability has been analysed. Furthermore, to fix the problems of self-selection bias and missing variables in samples, we used control samples and considered two-way fixed effects in a more robust model.
Bias processing of the self-selection sample
Due to the environmental migration in the process of air pollution, the estimation results are likely biased. To reduce the estimation bias caused by environmental migration, in the sample processing step, a subsample test was conducted for the participants whose residence location and groups did not change. The results are given in Table 7. It becomes clear that SO2 had a negative impact on ADL disability at the 10% significance level, NO2 had a negative impact on ADL disability at the 5% significance level, and the AQI had a negative impact on ADL disability at the 10% significance level. Therefore, the findings of previous models were robust.
Table 7.
Effect of air quality on ADL disability of permanent residents
| Variable | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| lnSO2 | −0.0684*(0.0362) | |||
| lnNO2 | −0.0183(0.0544) | |||
| lnPM10 | −0.1307**(0.0521) | |||
| lnAQI | −0.1368*(0.0772) | |||
| Serious illness | 0.0563**(0.0279) | 0.0570**(0.0279) | 0.0586**(0.0279) | 0.0477(0.0291) |
| Depression | 0.1265***(0.0256) | 0.1255***(0.0256) | 0.1268***(0.0256) | 0.1261***(0.0267) |
| Self-reported health | 0.0850***(0.0203) | 0.0855***(0.0203) | 0.0860***(0.0203) | 0.0864***(0.0212) |
| Body disability | −0.6325***(0.0495) | −0.6323***(0.0495) | − 0.6324***(0.0495) | −0.6282***(0.0516) |
| Physical pain | −0.0342(0.0219) | −0.0349(0.0218) | − 0.0343(0.0219) | −0.0449**(0.0227) |
| Individual / Year | Yes | Yes | Yes | Yes |
| /sigma2_u | 1.7967***(0.1216) | 1.7962***(0.1216) | 1.8010***(0.1218) | 1.8027***(0.1296) |
| Pseudo log likelihood | −26,292.693 | −26,294.516 | −26,291.386 | −24,363.95 |
| Observations | 25,169 | 25,169 | 25,169 | 25,169 |
Abbreviations: AQI Air Quality Index, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: Standard errors are in brackets; *** p < 0.01, ** p < 0.05, * p < 0.1. The control variable results are not listed here
Treatment of bidirectional fixed effects of panel data
Although the above analysis synchronously controlled for the corresponding individual sociodemographic characteristics and urban environmental characteristics, missing variables might still exist and result in estimation bias. Therefore, we first used a two-way fixed effects model to address the endogeneity problem caused by missing variables. This was referred to by Liu and Hu [17], who viewed classified variables as continuous variables and employed a linear two-way fixed effects model. In this case, ADL disability was considered a continuous variable, and the test results for this model are presented in Table 8. As a result, SO2, NO2 and the AQI did not show a significant effect on ADL disability. The significance levels of SO2 and the AQI were decreased in the fixed effects model, but they were still significant at 15%. PM10 had a significant and negative effect on ADL disability at a significance level of 1%, and the significance of PM10 was higher than the results of the benchmark model. Therefore, air quality still had a significant impact on ADL disability in the panel two-way fixed effects model, which means that the result was robust.
Table 8.
Impact of air quality on ADL disability: Based on fixed effects
| Variable | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| lnSO2 | −0.0130(0.0095) | |||
| lnNO2 | −0.0238(0.0153) | |||
| lnPM10 | −0.0584***(0.0185) | |||
| lnAQI | 0.0002(0.0003) | |||
| Serious illness | −0.0157***(0.0054) | −0.0155***(0.0054) | − 0.0149***(0.0054) | −0.0155***(0.0054) |
| Depression | 0.0135**(0.0057) | 0.0134**(0.0057) | 0.0139**(0.0057) | 0.0134**(0.0057) |
| Self-reported health | −0.0071(0.0050) | −0.0070(0.0050) | − 0.0065(0.0050) | −0.0072(0.0050) |
| Body disability | −0.0651***(0.0119) | −0.0652***(0.0119) | − 0.0658***(0.0119) | −0.0649***(0.0119) |
| Physical pain | −0.0126***(0.0036) | −0.0129***(0.0036) | − 0.0128***(0.0036) | −0.0128***(0.0036) |
| Individual / Year | Yes | Yes | Yes | Yes |
| F Test | 5.87 | 5.89 | 6.26 | 5.81 |
| R2 | 0.0127 | 0.0127 | 0.0135 | 0.0126 |
| Observations | 26,218 | 26,218 | 26,218 | 26,218 |
Abbreviations: AQI Air Quality Index, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: Standard errors are in brackets; *** p < 0.01, ** p < 0.05, * p < 0.1. The control variable results are not listed here
Instrumental variables
We further adopted the instrumental variable method for endogenous processing. An ordered probit instrumental variable method was selected. According to previous studies, the abundance of regional mineral resources and the proportion of mining industry employees in the total population could be used as instrumental variables of air quality [17]. Therefore, we chose the proportion of mining industry employees in the total population as the proxy variable of regional mineral resources and constructed the two-stage method of IV for the ordered probit model. The results are given in Table 9.
Table 9.
Estimation results of the IV ordered probit model
| Variable | (1) | (2) | (3) | (4) | ||||
|---|---|---|---|---|---|---|---|---|
| First-stage lnSO2 |
Second-stage ADL | First-stage lnNO2 |
Second-stage ADL | First-stage lnPM10 |
Second-stage ADL | First-stage lnAQI |
Second-stage ADL | |
| Mineral endowment | 18.0074***(0.3361) |
6.4223*** (0.2497) |
7.9056*** (0.2517) |
1.8217*** (0.1610) |
||||
| lnSO2 | −0.2086*** | |||||||
| (0.0481) | ||||||||
| lnNO2 | −0.5079*** | |||||||
| (0.1249) | ||||||||
| lnPM10 | −0.4492*** | |||||||
| (0.1048) | ||||||||
| lnAQI | −1.8083*** | |||||||
| (0.3437) | ||||||||
| Serious illness | 0.0195* | 0.0192* | 0.0225** | 0.0201** | ||||
| (0.0106) | (0.0104) | (0.0105) | (0.0095) | |||||
| Depression | 0.0744*** | 0.0722*** | 0.0896*** | 0.0811*** | ||||
| (0.0106) | (0.0104) | (0.0106) | (0.0105) | |||||
| Self-reported health | 0.0366*** | 0.0360*** | 0.0331*** | 0.0295*** | ||||
| (0.0089) | (0.0087) | (0.0088) | (0.0080) | |||||
| Body disability | −0.3027*** | −0.2968*** | −0.2951*** | −0.2653*** | ||||
| (0.0163) | (0.0164) | (0.0163) | (0.0210) | |||||
| Physical pain | −0.0214** | −0.0210** | −0.0243*** | −0.0216*** | ||||
| (0.0084) | (0.0082) | (0.0083) | (0.0076) | |||||
| Individual / Year | YES | YES | YES | YES | ||||
| |α/β| | 10.6974 | 26.4531 | 19.9644 | 89.9652 | ||||
| First stage F value | 2870.47 | 661.23 | 976.54 | 128.13 | 128.13 | |||
| Adjust R2 | 0.0736 | 0.0180 | 0.0263 | 0.0035 | 0.0035 | |||
| Observations | 26,218 | 26,218 | 26,218 | 26,218 | 26,218 | 26,218 | 26,218 | 26,218 |
Abbreviations: AQI Air Quality Index, SO2 Sulfur Dioxide, NO2 Nitrogen Dioxide, PM10 Inhalable Particles
Note: Standard errors are in brackets; *** p < 0.01, ** p < 0.05, * p < 0.1. The control variable results are not listed here
From the results of the first-stage test in Models (1) to (3), mineral resources have a significant and positive effect on air quality. The validity test of instrumental variables shows that the F value in the first stage is significantly greater than 10, indicating that the problem of weak instrumental variables did not exist. In other words, the selection of instrumental variables was effective. The results of second-stage tests in Models (1) to (3) show that air quality had a significant and negative impact on residents’ ADL disability at the significance level of 1%, which further demonstrates that the results of this study are robust. The results for Model (4) suggest that the AQI still had a significant and negative effect on ADL disability. This further proves that poor air quality significantly aggravates ADL disability. In addition, it can be seen from Model (4) that to keep ADL disability unchanged, ADL disability caused by a 1% increase in the AQI requires an 89.9652% reduction in serious disease to compensate for ADL damage. This means that the reduction amount of ADL disability brought by a 1-unit improvement in air quality equals the amount caused by a 89.9652-unit decrease in severe illness.
Discussion
The air quality index at a certain time point is a comprehensive indicator of pollutant accumulation, which is also an accurate reflection of air pollution at a specific time point. Thus, this study takes the annual average value of the AQI in a region as the proxy index to reflect long-term air pollution. At the same time, a multidimensional measurement of ADL could be established by dividing the disability level into five levels: health, mild disability, moderate disability, severe disability and serious disability [6]. Based on this, this study empirically tests the impact of the AQI on residents’ ADL disability. The results demonstrate that air quality has a significant impact on residents’ ADL disability, which is mainly manifested by the health reduction effect and increasing effect on ADL disability. Compared with existing studies, this study breaks the mould by exploring the impact of the AQI on residents’ ADL disability from the perspective of air pollution and enriches the research perspective of the social cost of air pollution. In addition, this study uses the average value of the AQI as the proxy variable of air quality, which can empirically reflect the impact of long-term exposure to air pollution on residents’ ADL disability.
Most existing studies have investigated the impact of air pollution from the perspective of social risk cost. For example, several scholars have estimated the impact of air pollution on residents’ health outcomes [11–15]. The indicators of health include changes in individual health level or changes in the incidence of disease and the incidence rate of diseases in the whole region (such as lung cancer mortality or respiratory disease mortality per 10,000 people) [17–21], as well as the increase in the cost of treatment due to air pollution, which indicates the social cost of air pollution [22, 23]. Therefore, the reliability of the conclusions of this study is a further expansion of the scope of existing findings. First, this study not only investigated the direct health outcome of air pollution but also investigated the changing paths of residents’ health influenced by air pollution, for instance, by analysing the change in the prevalence of major diseases; thus, discussion of the changing path of residents’ ADL disability under the influence of air pollution could be extended. This study also empirically reveals the theoretical basis for the social governance of residents’ ADL disability and the optimization of long-term care insurance. Specifically, the findings of this study provide insights into environmental governance of residents with ADL disability [47–49]. For example, investigating the changes in the disability rate and factors of disability risk of local residents and the effective regulations of air pollution could be undertaken for environmental governance. In this study, this is mainly explained by investigating the impact of different pollutants on residents’ ADL disability. The results of this study clarify that the concentrations of SO2 and PM10 pollutants are the main elements affecting residents’ ADL disability. In addition, there are significant group differences in the impact of air quality on ADL disability. For example, air quality has a more significant impact on the ADL disability of elderly residents aged 60 and above, female residents, residents in regions with low economic levels, and residents in areas without pilot long-term insurance. Additionally, the negative effect of air pollution is stronger on these groups. These findings demonstrate that the health damage effect of air pollution can be effectively reduced after the implementation of effective social policy intervention. Furthermore, few studies or practices have calculated the cost of disability treatment caused by pollution or the cost borne by the entire society. This is also one of the main innovations of this study. Ultimately, we should not only realize the significant impact of air pollution on ADL disability but also consider the differences between different groups and take the most effective measures to control air pollution and reduce its long-term social cost, that is, the long-term care cost of treating disabled residents.
Despite the practical significance of the findings of this study, especially the results of the analysis, which have been proven valid after a series of robustness tests and endogenous treatments, this study still has some limitations. First, the sample of this study mainly comes from 122 cities in China, but the sample is limited to people over 45 years old and generally excludes those under 45 years old, which may affect the applicability and reliability of the conclusions to a certain extent. Second, as one of the most important purposes of this study, ADL disability caused by air pollution and the cost of disability treatment are the main focus of this study. However, due to the complexity of factors that cause disability and the indeterminacy of actual nursing costs, this study was not able to measure the social cost of ADL disability caused by current air pollution completely and accurately, which would also be an important direction for further research. By gradually fixing the above problems, we can further clarify the marginal effect and social cost of air pollution governance and theoretically provide important support for optimizing regional policy for disability prevention and long-term care service security. The main advantages of this study are that it not only explores the direction of the impact of the AQI on residents’ ADL disability but also investigates the specific effect of the AQI on residents’ ADL disability, in addition to the changing trend of the long-term ADL disability rate caused by the joint influences of the AQI and the rate of serious disease. Thus, the logical relationship and mutual effects between natural environmental factors (AQIs) and individual health characteristic factors (rate of serious disease) are entangled.
Conclusions
This study used tracking data from the CHARLS database from 2015 and 2018 to construct panel data for investigating the impact of air quality on ADL disability and its marginal effect. The results show that air quality has a significant impact on ADL disability, and the main impacts were from the concentrations of SO2 and PM10. Second, in terms of the marginal effect, the main effects of air quality on ADL disability appear to have a positive effect on disability increment, and it also shows that air quality plays a leading role in the negative effect of health. Moreover, it was revealed that air quality has a more significant impact on the ADL disability of residents aged 60 years and above, female residents, residents with poor economic status and residents in areas without LTCI. The results of the interaction between air quality and serious illness showed that air quality worsened the impact of serious illness on ADL disability. Finally, we confirmed the robustness of our findings by controlling subsamples and using two-way fixed effects and instrumental variables.
Our findings are also strongly relevant to policy decisions. First, social and economic development should be “environmentally friendly” and should not only consider the short-term increase in GDP but also consider the basic quality of life of local residents, especially the health of vulnerable groups such as the elderly population and those living in economically underdeveloped areas. Second, controlling air pollution should be prioritized. The impact of air quality on the natural environment of a country or region has been remarkable, and its impact on the health of individuals is also gradually being recognized. The increase in ADL disability caused by the increase in the incidence of individual serious illness influenced by air quality also indicates that the social cost of environmental pollution is increasing. Third, when investigating ADL disability in theory, we should not only pay attention to the causes of disability from the perspective of traditional medicine or socioeconomic environments but also note the influences of ecological environment changes and the negative impacts of changes in air quality. Therefore, intervention policies could be implemented to prevent ADL disability and improve quality of life.
Acknowledgements
The authors are very grateful for the financial support of National Natural Science Fund of China (71904167) and Dr. Wang Meng’s and Tiantian Hu help in research design, revising the article and polishing the language.
Abbreviations
- LTCI
Long-term Care Insurance
- CHARLS
China Health and Retirement Longitudinal Study
- AQI
Air Quality Index
- HAQI
Health Risk-based AQI
- API
Air Pollution Index
- PM2.5
Fine Particulate Matter
- PM10
Inhalable Particles
- O3
Ozone
- CO
Carbon Monoxide
- SO2
Sulfur Dioxide
- NO2
Nitrogen Dioxide
- GDP
Gross Domestic Product
Author’s contributions
H.L. drafted the manuscript and approved the version to be published,and carry out language retouching, modification. And he made a substantial contribution to the concept and design of the work, interpretation of data,and revised the article.
Funding
National Natural Science Fund of China (71904167).
Availability of data and materials
The data that support the findings of this study are openly available at the following URL/DOI: http://charls.pku.edu.cn/
Declarations
Ethics approval and consent to participate
We declare that all methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by Institutional Review Board at Peking University. And we confirmed that informed consent was obtained from all subjects or, if subjects are under 18, from a parent and/or legal guardian. The IRB approval number for the main household survey, including anthropometrics, is IRB00001052–11015; the IRB approval number for biomarker collection, was IRB00001052–11014.During the fieldwork, each respondent who agreed to participate in the survey was asked to sign two copies of the informed consent, and one copy was kept in the CHARLS office, which was also scanned and saved in PDF format.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nation Bureau of Statistics.(2021) Available from: http://www.mofcom.gov.cn/article/i/jyjl/l/202102/20210203038237.shtml. According to the preliminary statistics of GDP in 2020.
- 2.Olsson A, Schubauer-Berigan M, Schüz J. Strategies of the International Agency for Research on Cancer (IARC/WHO) to reduce the occupational cancer burden. Med Tr Prom Ekol. 2021;61(3):140–154. doi: 10.31089/1026-9428-2021-61-3-140-154. [DOI] [Google Scholar]
- 3.Xi Jinping's report at 19th CPC National Congress(2017) Available from: http://www.xinhuanet.com/english/download/Xi_Jinping's_report_at_19th_CPC_National_Congress.pdf
- 4.Chen L, Xu X. Effect evaluation of the long-term care insurance (ltci) system on the health care of the elderly: a review. J Multidiscip Healthc. 2020;13:863–875. doi: 10.2147/JMDH.S270454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu H. Formal and informal care: complementary or substitutes in care for elderly people? Empirical evidence from China. SAGE Open. 2020;11(2):1–16. doi: 10.1177/21582440211016413. [DOI] [Google Scholar]
- 6.Liu H. Research on disability grading based on icf functional framework: empirical evidence from Zhejiang province, China. Front Public Health. 2021;9:616180. doi: 10.3389/fpubh.2021.616180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li ZH, Lv YB, Kraus VB, Yin ZX, Shi XM. Trends in the incidence of activities of daily living disability among chinese elderly from 2002-2014. J Gerontol Ser A Biol Sci Med Sci. 2019;75(11):2113–2118. doi: 10.1093/gerona/glz221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Q, Granados J. Household heating associated with disability in activities of daily living among Chinese middle-aged and elderly: a longitudinal study. Environ Health Prev Med. 2020;25(1):49. doi: 10.1186/s12199-020-00882-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janca A, Kastrup M, Katschnig H, López-Ibor JJ, Mezzich JE, Sartorius N. The world health organization short disability assessment schedule (who das-s): a tool for the assessment of difficulties in selected areas of functioning of patients with mental disorders. Soc Psychiatry Psychiatr Epidemiol. 1996;31(6):349–354. doi: 10.1007/BF00783424. [DOI] [PubMed] [Google Scholar]
- 10.Habtamu K, Alem A, Medhin G, Fekadu A, Hanlon C. Validation of the world health organization disability assessment schedule in people with severe mental disorders in rural Ethiopia. Health Qual Life Outcomes. 2017;15(1):64. doi: 10.1186/s12955-017-0647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Usmani R, Saeed A, Abdullahi AM, Pillai TR, Hashem I. Air pollution and its health impacts in Malaysia: a review. Air Quality Atmosphere Health. 2020;13(4):1093–1118. doi: 10.1007/s11869-020-00867-x. [DOI] [Google Scholar]
- 12.Han C, Xu R, Zhang Y, Yu W, Guo Y. Air pollution control efficacy and health impacts: a global observational study from 2000 to 2016. Environ Pollut. 2021;287:117211. doi: 10.1016/j.envpol.2021.117211. [DOI] [PubMed] [Google Scholar]
- 13.Markandya A, Sampedro J, Smith SJ, Dingenen RV, Pizarro-Irizar C, Arto I, et al. Health co-benefits from air pollution and mitigation costs of the Paris agreement: a modelling study. Lancet Planet Health. 2018;2(3):e126–e133. doi: 10.1016/S2542-5196(18)30029-9. [DOI] [PubMed] [Google Scholar]
- 14.José RS, Pérez JL, Pérez L, Barras R. Effects of climate change on the health of citizens modelling urban weather and air pollution. Energy. 2018;165:53–62. doi: 10.1016/j.energy.2018.09.088. [DOI] [Google Scholar]
- 15.Xiang Z, Azam M, Islam T, Zaman K. Environment and air pollution like gun and bullet for low income countries: war for better health and wealth. Environ Sci Pollut Res. 2020;23(4):3641–3657. doi: 10.1007/s11356-015-5591-3. [DOI] [PubMed] [Google Scholar]
- 16.Msha B, Hcfa B, Pkkla C, Akhla D. Combined effects of increased o 3 and reduced no 2 concentrations on short-term air pollution health risks in Hong Kong. Environ Pollut. 2021;270:116280. doi: 10.1016/j.envpol.2020.116280. [DOI] [PubMed] [Google Scholar]
- 17.Guo Y, Teixeira JP, Ryti N. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381(8):705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X, Chen X, Zhang XB. The impact of exposure to air pollution on cognitive performance. Proc Natl Acad Sci. 2018;115(37):201809474. doi: 10.1073/pnas.1809474115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xue T, Zhu T, Zheng Y, et al. Author correction: declines in mental health associated with air pollution and temperature variability in China. Nat Commun. 2019;10(1):1–3. doi: 10.1038/s41467-019-11660-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morris GP, Beck SA, Hanlon P, Robertson R. Getting strategic about the environment and health. Public Health. 2006;120(10):889–903. doi: 10.1016/j.puhe.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 21.Kunzli N, Medina S, Kaiser R, Quenel P, Horak F, Studnicka M. Assessment of deaths attributable to air pollution: should we use risk estimates based on time series or on cohort studies? Am J Epidemiol. 2017;11:1050–1055. doi: 10.1093/aje/154.10.974. [DOI] [PubMed] [Google Scholar]
- 22.Di Q, Wang Y, Zanobetti A, Wang Y, Schwartz JD. Air pollution and mortality in the medicare population. N Engl J Med. 2017;376(26):2513–2522. doi: 10.1056/NEJMoa1702747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Song C, Wu L, Xie Y, He J, Chen X, Wang T, et al. Air pollution in China: status and spatiotemporal variations. Environ Pollut. 2017;227(aug.):334–347. doi: 10.1016/j.envpol.2017.04.075. [DOI] [PubMed] [Google Scholar]
- 24.Halkos G, Argyropoulou G. Modeling energy and air pollution health damaging: a two-stage DEA approach. Air Qual Atmosphere Health. 2021;14(8):1221–1231. doi: 10.1007/s11869-021-01012-y. [DOI] [Google Scholar]
- 25.Luo H, Guan Q, Lin J, Wang Q, Wang N. Air pollution characteristics and human health risks in key cities of Northwest China. J Environ Manag. 2020;269:110791. doi: 10.1016/j.jenvman.2020.110791. [DOI] [PubMed] [Google Scholar]
- 26.Camarinho R, Garcia PV, Rodrigues AS. Chronic exposure to volcanogenic air pollution as cause of lung injury. Environ Pollut. 2013;181(10):24–30. doi: 10.1016/j.envpol.2013.05.052. [DOI] [PubMed] [Google Scholar]
- 27.Berend N. Contribution of air pollution to COPD and small airway dysfunction. Respirology. 2016;21(2):237–244. doi: 10.1111/resp.12644. [DOI] [PubMed] [Google Scholar]
- 28.Bowatte G, Lodge CJ, Knibbs LD, et al. Traffic-related air pollution exposure is associated with allergic sensitization, asthma, and poor lung function in middle age. J Allergy Clin Immunol. 2017;139(1):122–129. doi: 10.1016/j.jaci.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Schultz ES, Litonjua AA, Erik M. Effects of long-term exposure to traffic-related air pollution on lung function in children. Curr Allergy Asthma Rep. 2017;17(6):41. doi: 10.1007/s11882-017-0709-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alderete TL, Habre R, Toledo-Corral CM, et al. Longitudinal associations between ambient air pollution with insulin sensitivity, β-cell function, and adiposity in Los Angeles Latino children. Diabetes. 2017;66(7):1789–1796. doi: 10.2337/db16-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bourdrel T, Bind MA, Béjot B, et al. Cardiovascular effects of air pollution. Arch Cardiovasc Dis. 2017;110(11):634–642. doi: 10.1016/j.acvd.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cacciottolo M, Wang X, Driscoll I, et al. Particulate air pollutants, APOE alleles and their contributions to cognitive impairment in older women and to Amyloidogenesis in experimental models. Translational. Psychiatry. 2017;7(1):e1022. doi: 10.1038/tp.2016.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Munzel T, Gori T, Al-Kindi S, et al. Effects of gaseous and solid constituents of air pollution on endothelial function. Eur Heart J. 2018;39(38):3543–3550. doi: 10.1093/eurheartj/ehy481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toledo-Corral CM, Alderete TL, Habre R, et al. Effects of air pollution exposure on glucose metabolism in Los Angeles minority children. Pediatric. Obesity. 2018;13(1):54–62. doi: 10.1111/ijpo.12188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim MJ. Air pollution, health, and avoidance behavior: evidence from South Korea. Environ Resour\ Econ. 2021;79(10):63–91. doi: 10.1007/s10640-021-00553-1. [DOI] [Google Scholar]
- 36.Jiao K, Xu M, Liu M. Health status and air pollution related socioeconomic concerns in urban China. Int J Equity Health. 2018;17(1):18. doi: 10.1186/s12939-018-0719-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liao, L.P. , Du M.Z., & Chen ZF. (2021). Air pollution, health care use and medical costs: evidence from China - ScienceDirect. Energy Econ, 95:105132. https://doi.org/10.1016/j.eneco.2021.105132
- 38.Sun H, Leng Z, Zhao H, Ni S, Huang C. The impact of air pollution on urban residents' health expenditure: spatial evidence from Yangtze river delta, China. Air Qual Atmosphere Health. 2020;14:343–350. doi: 10.1007/s11869-020-00939-y. [DOI] [Google Scholar]
- 39.Liu J, Yin H, Tang X, Zhu T, Yi HH. Transition in air pollution, disease burden and health cost in China: a comparative study of long-term and short-term exposure. Environ Pollut. 2021;277:116770. doi: 10.1016/j.envpol.2021.116770. [DOI] [PubMed] [Google Scholar]
- 40.Grossman M. On the concept of health capital and the demand for health. Journal of political. Economics. 1972;80(2):223–255. doi: 10.2307/1830580. [DOI] [Google Scholar]
- 41.Muller C. A health production function for quasi-autarkic agricultural households in Rwanda. Eur J Dev Res. 2001;13(1):87–105. doi: 10.1080/09578810108426782. [DOI] [Google Scholar]
- 42.Bichaka F, Paulos G. Estimating a health production function for sub-Saharan Africa (SSA) Appl Econ. 2005;37(2):155–164. doi: 10.1080/00036840412331313521. [DOI] [Google Scholar]
- 43.Thornton J. Estimating a health production function for the US: some new evidence. Appl Econ. 2002;34(1):59–62. doi: 10.1080/00036840010025650. [DOI] [Google Scholar]
- 44.Filmer D, Pritchett L. The impact of public spending on health: does money matter? Soc Sci Med. 1999;49(10):1309–1323. doi: 10.1016/S0277-9536(99)00150-1. [DOI] [PubMed] [Google Scholar]
- 45.Liu H, Hu T. Evaluating the long-term care insurance policy from medical expenses and health security equity perspective: evidence from China. Arch Public Health. 2022;2022:80,3. doi: 10.1186/s13690-021-00761-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tian Y, Jiang Y, Liu Q, Xu D, Zhao S, He L, et al. Temporal and spatial trends in air quality in Beijing. Landscape Urban Plann. 2019;185:35–43. doi: 10.1016/j.landurbplan.2019.01.006. [DOI] [Google Scholar]
- 47.Liu H. Health depreciation effect and medical cost effect of air pollution:based on multidimensional health perspective. Air Qual Atmosphere Health. 2022;3:1–16. doi: 10.1007/s11869-022-01189-w. [DOI] [Google Scholar]
- 48.Liu H, Hu T. How does air quality affect residents’ life satisfaction? Evidence based on multiperiod follow-up survey data of 122 cities in China. Environ Sci Pollut Res. 2021;28:61047–61060. doi: 10.1007/s11356-021-15022-x. [DOI] [PubMed] [Google Scholar]
- 49.Liu H, Hu T, Wang M. Impact of air pollution on residents’ medical expenses: a study based on the survey data of 122 cities in China. Front Public Health. 2021;9:743087. doi: 10.3389/fpubh.2021.743087. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available at the following URL/DOI: http://charls.pku.edu.cn/