Glenohumeral instability most commonly affects patients in their late teenage years.19 Anterior shoulder dislocations account for 97% of all shoulder dislocations1 and are usually caused by a forced abduction, external rotation, and hyperextension.16 Seizures are a common cause of shoulder dislocation and persistent glenohumeral instability.11 Although posterior shoulder dislocations are typically associated with seizures, anterior instability following an ictal episode is more common, and bilateral dislocations are possible.4
The patients presenting with an anterior dislocation usually present with acute pain, the arm held in abduction and external rotation, or an adducted arm at the side. There is often loss of the normal contour of the deltoid and prominence of the acromion posteriorly and laterally.8 The initial management of acute anterior shoulder dislocation in younger active patients remains controversial.14
Timely treatment of a dislocated shoulder is important, with reduction within 24 hours of the injury being essential to preserve the joint, requiring less sedation and fewer attempts at reduction.26 Failure to reduce a dislocated shoulder within 24 hours carries the risk that closed reduction will be difficult or even impossible to achieve safely. Dislocations that present subacutely (after 7-10 days) often require deep sedation and multiple relocation attempts and have been associated with brachial plexus and axillary artery injury.22,24 A glenohumeral dislocation that persists for multiple months can lead to osteopenia of the subchondral bone13 and collapse of the humeral head at the time of reduction, leading to poor long-term outcomes.9
Due to the COVID-19 pandemic, many patients have failed to seek medical care in a timely manner. Fear of the virus and the fact that many health care providers were exclusively doing virtual consultations are reasons that lead to worse outcomes documented across multiple specialties during the COVID-19 pandemic.18,20,23 Orthopedic surgery is the surgical field that has seen the highest proportion of its activities canceled or postponed due to the pandemic.6 This explains why waiting lists to see an orthopedic surgeon have significantly increased.21 Virtual consultations allow the physician to gather an adequate history but prevent the ability to perform significant portions of the physical examination which can be essential in establishing the correct diagnosis.
Shoulder dislocations are quite often easily diagnosed due to the clear symptoms, signs, and functional limitations associated with this pathology. A missed diagnosis of shoulder dislocation is rare, and the majority of these cases are associated with a clear traumatic event and are adequately managed.2,5,7 On the other hand, recurrent atraumatic dislocations are seen infrequently and have not been described adequately in the literature, for which there is no consensus on the best management method. We present a case of late presentation of locked anterior shoulder dislocation with an atraumatic cause during the time of COVID-19 and describe our primary and revision surgical strategies.
Case
A previously healthy 25-year-old man with no orthopedic history presented to the emergency room of our hospital with a four-month history of worsening left shoulder pain. The patient is known for cocaine and benzodiazepine use, takes no prescribed medication, and has no relevant past medical or surgical history. Four months prior to presenting to our emergency room, the patient woke up with acute pain in both shoulders and the sensation of severely limited movement in both of his shoulders. He was able to relocate the right shoulder by himself but not the left shoulder. He contacted his family doctor and was only able to get a telephone appointment due to the COVID-19 pandemic. After questioning, the physician concluded that the pain was likely muscular and recommended rotator cuff strengthening exercises. The patient proceeded to do some strengthening exercises he found on the internet. During the next 4 months, he was able to mobilize his right shoulder but complained of worsening left shoulder pain at rest and some range of motion limitation. He presented to our hospital four months after the initial onset of symptoms.
An X-ray of the shoulder was performed in the emergency room (Fig. 1), which showed a locked anterior dislocation of the left shoulder with a massive Hill-Sachs lesion of the humerus and a coracoid process fracture. On examination, the patient had 90 degrees of forward flexion, 80 degrees of abduction, and no external rotation. The good range of motion was likely due to scapulothoracic compensation and an enlarging Hill-Sach’s lesion. He had decreased strength and an intact neurovascular examination including full axillary nerve function. The right shoulder showed apprehension sign and was found to be positive on relocating test, suggesting an unstable shoulder that had previously dislocated.
Figure 1.

Antero-posterior view of the left shoulder on initial presentation showing an anterior dislocation and large Hill-Sachs fracture.
Due to the delay in presentation, closed reduction of the left shoulder was not deemed an option, and thus, we proceeded with left shoulder open reduction, fixation, and stabilization. The shoulder was stabilized using a Bristow procedure, and the massive Hill-Sachs lesion was treated with a hemi cap resurfacing hemiarthroplasty. In addition, a biceps tenodesis was performed. The postoperative films show adequate reduction of the glenohumeral joint (Fig. 2). Intraoperative mobilization demonstrated satisfactory shoulder stability. After the procedure, the patient was discharged home with a shoulder sling and instructions on the importance of maintaining the sling.
Figure 2.

Antero-posterior view of the left shoulder immediately after the primary surgery showing anatomical reduction and an adequately positioned hemi-cap button.
Two weeks following the surgery, the patient returned to the clinic for his follow-up appointment and described increasing left shoulder pain. He mentioned the possibility of receiving a small trauma to the shoulder in the last 2 weeks and admitted to not wearing the sling consistently. The physical examination showed a slightly restricted and painful range of motion and an intact distal neurovascular examination. The surgical wound showed good healing and no signs of infection. Plain films of the left shoulder showed a recurrent anterior shoulder dislocation with no signs of hardware failure or associated fractures (Fig. 3).
Figure 3.

Antero-posterior view of the left shoulder showing redislocation of the shoulder without signs of hardware failure.
Following this new finding, the patient was indicated for a revision shoulder open reduction and Bristow procedure and an external fixator application. During the procedure, the surgeon noted that the subscapularis muscle appeared significantly medialized and torn as if the shoulder was subjected to a forceful movement such as trauma or seizure. The subscapularis was irreparable, and thus, a pectoralis major transfer was performed. The shoulder external fixator was applied by placing two self-tapping 5-mm Steinmann pins in the midshaft of the humerus anterolaterally, the clavicle anteriorly, and the acromion anterolaterally, which were then connected with 8-mm carbon fiber rods. After an extensive revision procedure, the patient was discharged with an external fixator for 6 weeks and a brace (Fig. 4). At the 6-week follow-up, the external fixator was removed and the shoulder had remained reduced.
Figure 4.
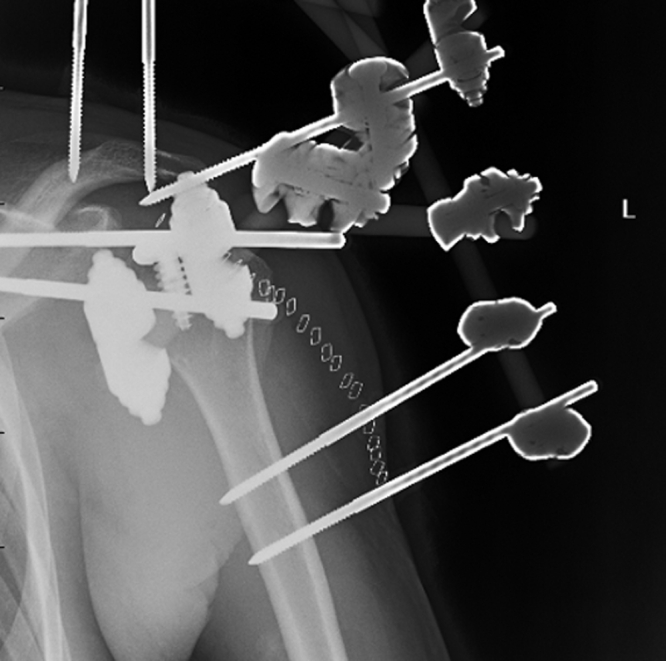
Postoperative x-ray showing the use of an external fixator to achieve and maintain reduction of the glenohumeral joint.
At one-year follow-up, the patient showed more than 100 degrees of active forward flexion and 90 degrees of abduction. After extensive physiotherapy, the patient had improved musculature of the deltoid and a painless and stable shoulder but persistent anterior deltoid atrophy. Plain films showed the shoulder remained reduced (Fig. 5), and the patient was happy with the result of the surgery and mentioned having no pain at rest. The patient has been advised to continue with physical therapy to try and improve his shoulder range of motion and strength.
Figure 5.

Antero-posterior view of the left shoulder at the patient’s one-year follow-up.
Discussion
This case of late presentation of locked anterior shoulder dislocation with an atraumatic cause during the time of COVID-19 in a young adult offers multiple discussion points. We will address the late presentation and thus diagnosis of dislocation and the surgical strategy used for the revision procedure. This patient initially consulted with his primary care doctor during the COVID-19 pandemic and was therefore only assessed via telemedicine. This missed diagnosis highlights the shortcomings of teleconsultations, more specifically the inability to proceed to an adequate physical examination virtually and the additional challenges posed by the virtual assessment of acute orthopedic pathologies.20
Chronic glenohumeral dislocations can present with minimal symptoms and be missed without adequate examination by a skilled clinician. This case presents delay in diagnosis and lack of treatment, which likely contributed to the increased risk of recurrence and worsening of the Hill-Sachs lesion. Prolonged delay to surgical fixation contributed to difficulty of the procedure due to the presence of scar tissue along with the absence of the subscapularis muscle which posed an additional challenge. Although rare, missed shoulder dislocations are associated with unsatisfactory long-term functional outcome. Due to the challenging nature of the procedure and the inherent glenohumeral instability,5 reduced long-term range of motion of the shoulder and a high incidence of postoperative pain are common complications.2,5,7 Some authors have recommended using the acromiohumeral transfixing pins for stability when using an open reduction technique for chronic dislocations.10,17 The Bristow procedure has been shown to be safe and effective15 and to have a rate of recurrent dislocation and revision surgery of 2.9%.12 The most common reason for failure of the Bristow procedure is graft nonunion.27
External fixators of the shoulder are used in cases of complex proximal humeral fractures, allowing shoulder stability with a minimally invasive technique3,28; they have been used for treating a floating shoulder,25 but to our knowledge, they are rarely used in cases of shoulder dislocation. The decision to use an external fixator during the revision procedure was based on the fact that the intraoperative glenohumeral reduction was very difficult to achieve and to maintain. Additionally, extensive scar tissue and significant trauma to the subscapularis muscle were identified. Finally, as seen following the primary surgery, the patient’s adherence to immobilization instructions was insufficient, and the patient was deemed unreliable in that regard.
It remains unclear if a trauma, seizure, or other event caused the redislocation following the surgery. However, the patient’s age, delay to examination by a physician, and severity of the pathology mandated a comprehensive surgical plan. Poor patient adherence to postoperative immobilization, increased time to surgical management, and baseline hypermobility were important contributing factors leading to failure of the primary open reduction and fixation.
Conclusion
This case report shows a complication associated with reduced access to health care during the times of COVID-19 and how this delay can lead to worsening pathology, more challenging surgery, and lower success rate of treatments undergone. Additionally, we showed a unique and successful method of providing shoulder stability and maintaining reduction in a chronic atraumatic and recurrent shoulder dislocation in a young patient with poor compliance.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
This study has been exempted from institutional review board review by the McGill University Institutional Review Board.
References
- 1.Abrams R., Akbarnia H. 2020. Shoulder Dislocations Overview. [PubMed] [Google Scholar]
- 2.Ahmad K., Bin Ayaz S., Bin Khalil H., Matee S. Bilateral spontaneous anterior shoulder dislocation: A missed orthopedic injury mistaken as proximal neuropathy. Chin J Traumatol. 2017;20:370–372. doi: 10.1016/j.cjtee.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blonna D., Assom M., Bellato E., Pisanu G., Greco V., Marmotti A., et al. Outcomes of 188 Proximal Humeral Fractures Treated with a Dedicated External Fixator with Follow-up Ranging from 2 to 12 Years. J Bone Joint Surg Am. 2019;101:1654–1661. doi: 10.2106/jbjs.18.00734. [DOI] [PubMed] [Google Scholar]
- 4.Bühler M., Gerber C. Shoulder instability related to epileptic seizures. J Shoulder Elbow Surg. 2002;11:339–344. doi: 10.1067/mse.2002.124524. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhary D., Joshi D., Jain V., Mohindra M., Mehta N. A six months old neglected anterior shoulder dislocation managed by closed reduction and Latarjet procedure. Chin J Traumatol. 2016;19:295–297. doi: 10.1016/j.cjtee.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collaborative C., Nepogodiev D., Omar O.M., Glasbey J.C., Li E., Simoes J.F.F., et al. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2022;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cuffolo G., Coomber R., Burtt S., Gray J. 2014. Case Report: Posterior shoulder dislocation while lifting weights: a missed diagnosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cutts S., Prempeh M., Drew S. Anterior Shoulder Dislocation. Ann R Coll Surg Engl. 2009;91:2–7. doi: 10.1308/003588409X359123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flatow E., Miller S., Neer C. Chronic anterior dislocation of the shoulder. J Shoulder Elbow Surg. 1993;2:2–10. doi: 10.1016/S1058-2746(09)80131-6. [DOI] [PubMed] [Google Scholar]
- 10.Goga I. Chronic shoulder dislocations. J Shoulder Elbow Surg. 2003;12:446–450. doi: 10.1016/s1058-2746(03)00088-0. [DOI] [PubMed] [Google Scholar]
- 11.Goudie E.B., Murray I.R., Robinson C.M. Instability of the shoulder following seizures. J Bone Joint Surg Br. 2012;94:721–728. doi: 10.1302/0301-620X.94B6.28259. [DOI] [PubMed] [Google Scholar]
- 12.Griesser M., Harris J., McCoy B., Hussain W., Jones M., Bishop J., et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg. 2013;22:286–292. doi: 10.1016/j.jse.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Jerosch J., Riemer R., Schoppe R. Asymptomatic chronic anterior posttraumatic dislocation in a young male patient. J Shoulder Elbow Surg. 1999;8:492–494. doi: 10.1016/s1058-2746(99)90082-4. [DOI] [PubMed] [Google Scholar]
- 14.Kane P., Shawn M.B., Dodson C.C., Freedman K.B. Approach to the treatment of primary anterior shoulder dislocation: A review. Phys Sportsmed. 2015;43:54–64. doi: 10.1080/00913847.2015.1001713. [DOI] [PubMed] [Google Scholar]
- 15.Khawaja K., Mohib Y., Khan D.M., Juman N., Habib A., P H. Functional outcomes of modified Bristow procedure in recurrent shoulder dislocation. J Pak Med Assoc. 2021;71:2448–2450. doi: 10.47391/JPMA.05-608. [DOI] [PubMed] [Google Scholar]
- 16.Kirkley A., Werstine R., Ratjek A., Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21:55–63. doi: 10.1016/j.arthro.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 17.Mansat P., Guity M., Mansat M., Bellumore Y., Rongières M., Bonnevialle P. [Chronic anterior shoulder dislocation treated by open reduction sparing the humeral head] Rev Chir Orthop Reparatrice Appar Mot. 2003;89:19–26. [Article in French] [PubMed] [Google Scholar]
- 18.Masroor S. Collateral damage of COVID-19 pandemic: Delayed medical care. J Card Surg. 2020;35:1345–1347. doi: 10.1111/jocs.14638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohtadi N., Chan D., Hollinshead R., Boorman R., Hiemstra L., Lo I., et al. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability: two-year follow-up with disease-specific quality-of-life outcomes. J Bone Joint Surg Am. 2014;96:353–360. doi: 10.2106/JBJS.L.01656. [DOI] [PubMed] [Google Scholar]
- 20.Moisan P., Barimani B., Antoniou J. Orthopedic Surgery and Telemedicine in Times of COVID-19 and Beyond: a Review. Curr Rev Musculoskelet Med. 2021;14:155–159. doi: 10.1007/s12178-021-09693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips M., Chang Y., Zura R., Mehta S., Giannoudis P., Nolte P., et al. Impact of COVID-19 on orthopaedic care: a call for nonoperative management. Ther Adv Musculoskelet Dis. 2020;12 doi: 10.1177/1759720X20934276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riebel G., McCabe J. Anterior shoulder dislocation: a review of reduction techniques. Am J Emerg Med. 1991;9:180–188. doi: 10.1016/0735-6757(91)90187-o. [DOI] [PubMed] [Google Scholar]
- 23.Shin D., Cho J., Kim S., Guallar E., Hwang S., Cho B., et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013;20:2468–2476. doi: 10.1245/s10434-013-2957-y. [DOI] [PubMed] [Google Scholar]
- 24.Stayner L., Cummings J., Andersen J., Jobe C. Shoulder dislocations in patients older than 40 years of age. Orthop Clin North Am. 2000;31:231–239. doi: 10.1016/s0030-5898(05)70143-7. [DOI] [PubMed] [Google Scholar]
- 25.Vogels J., Pommier N., Cursolle J.C., Belin C., Tournier C., Durandeau A. PreFix™ external fixator used to treat a floating shoulder injury caused by gunshot wound. Chir Main. 2014;33:370–374. doi: 10.1016/j.main.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 26.Wen D. Current concepts in the treatment of anterior shoulder dislocations. Am J Emerg Med. 1999;17:401–407. doi: 10.1016/s0735-6757(99)90097-9. [DOI] [PubMed] [Google Scholar]
- 27.Willemot L., De Boey S., Van Tongel A., Declercq G., De Wilde L., Verborgt O. Analysis of failures after the Bristow-Latarjet procedure for recurrent shoulder instability. Int Orthop. 2019;43 doi: 10.1007/s00264-018-4105-6. [DOI] [PubMed] [Google Scholar]
- 28.Zhang J., Ebraheim N., Lause G. Surgical treatment of proximal humeral fracture with external fixator. J Shoulder Elbow Surg. 2012;21:882–886. doi: 10.1016/j.jse.2011.07.005. [DOI] [PubMed] [Google Scholar]


