Abstract
Introduction
Noninvasive risk assessment is crucial in patients with COVID-19 in emergency department. Since limited data is known about the role of noninvasive parameters, we aimed to evaluate the role of a noninvasive parameter ‘SpO2/FiO2’ in independently predicting 30-day mortality in patients with COVID-19 and its prognostic utility in combination with a noninvasive score ‘CRB-65’.
Methods
A retrospective study was performed in a tertiary training and research hospital, which included 272 patients with COVID-19 pneumonia diagnosed with polymerase chain reaction in emergency department. Data on characteristics, vital signs, and laboratory parameters were recorded from electronic medical records. The primary outcome of the study was 30-day mortality, and we assessed the discriminative ability of SpO2/FiO2 in predicting mortality in patients with COVID-19 pneumonia and its prognostic utility in combination with conventional pneumonia risk assessment scores.
Results
Multivariate analysis revealed that only SpO2/FiO2 level was found to be an independent parameter associated with 30-day mortality (OR:0.98, 95% CI: 0.98–0.99, p = 0.003). PSI and CURB-65 were found to be better scores than CRB-65 in predicting 30-day mortality (AUC: 0.79 vs 0.72, p = 0.04; AUC: 0.76 vs 0.72, p = 0.01 respectively). Both SpO2/FiO2 combined with CRB-65 and SpO2/FiO2 combined with CURB-65 have good discriminative ability and seemed to be more favorable than PSI in predicting 30-days mortality (AUC: 0.83 vs 0.75; AUC: 0.84 vs 0.75), however no significant difference was found (p = 0.21 and p = 0.06, respectively).
Conclusion
SpO2/FiO2 is a promising index in predicting mortality. Addition of SpO2/FiO2 to CRB-65 improved the role of CRB-65 alone, however it performed similar to PSI. The combined noninvasive model of SpO2/FiO2 and CRB-65 may help physicians quickly stratify COVID-19 patients on admission, which is expected to be particularly important in hospitals still stressed by pandemic volumes.
Keywords: COVID-19 pneumonia, SpO2/FiO2, Pneumonia risk scores, 30 day mortality
Abbreviations: AUC, area under the curve; BUN, blood urea nitrogen; CRP, C-reactive protein; COVID-19, coronavirus disease of 2019; FiO2, Fraction of Inspired Oxygen; IQR, interquartile ranges were reported; PaO2, partial pressure of oxygen; PCR, polymerase chain reaction; PSI, Pneumonia Severity Index; SD, standard deviation; SpO2, peripheral oxygen saturation
1. Introduction
Coronavirus pandemic is still a worldwide health concern which has a high rate of mortality with new variants being developed. The increasing number of cases makes it even more important to act quickly, especially in emergency departments. Therefore, noninvasive rapid assessment has become more critical.
In patients with COVID-19, many parameters have been reported to be associated with mortality so far. Deceased patients with COVID-19 have higher levels of C-reactive protein (CRP), troponin, ferritin, and low levels of lymphocyte count [1]. Moreover, CD3+ CD8+ T cells ≤75/μL [2], IL-6 [3], and the presence of proteinuria and hematuria [4] were also found to be associated with adverse outcomes. Regarding oxygenation, PaO2/FiO2 had excellent discriminative ability in predicting mortality in patients with COVID-19 [3]. In line with these well-defined predictors, robust scoring systems have been developed [5]. In addition, conventional risk scores such as CURB-65 [6], Pneumonia Severity Index (PSI) [7], APACHE [8], and SOFA [9] score which have been widely used for community-acquired pneumonia, were also found to be useful in predicting worse outcome in COVID-19. Although these methods have proven to be effective, they all entail at least one invasive parameter and were not practical in emergency departments during the pandemic. Limited data is known regarding the role of noninvasive parameters in predicting mortality in patients with COVID-19.
As a noninvasive index, SpO2/FiO2, has an advantage in predicting the course of the patients in emergency departments and it has also been found to be useful in patients with COVID-19 [10,11]. However, it has been reported that when used alone, it has poor prognostic reliability [12]. So future studies are required to determine the contribution of SpO2/FiO2 in prognosis of patients with COVID-19 in the emergency department. Among noninvasive combined risk scores, CRB-65 which was composed of the parameters confusion, respiratory rate, blood pressure, and age, has been widely used in community-acquired pneumonia [13,14]. Furthermore, it was reported with a limited sample size that CRB-65 had good discriminative ability similar to CURB-65 in predicting the requirement for intensive support in patients with COVID-19 (AUC: 0.81 vs 0.85). However, there is an ongoing need for a noninvasive tool in predicting mortality.
In line with these, we aimed to evaluate the role of a noninvasive parameter ‘SpO2/FiO2’ in independently predicting 30-day mortality in patients with COVID-19 and its prognostic utility in combination with the conventional pneumonia risk assessment scores.
2. Methods
2.1. Study design and setting
We conducted a retrospective cohort study at a tertiary training and research hospital. The local institutional ethics committee approved the study protocol (ethic approval number: 04.10.2021–00143257057). This study was performed in line with the Declaration of Helsinki.
2.2. Study population
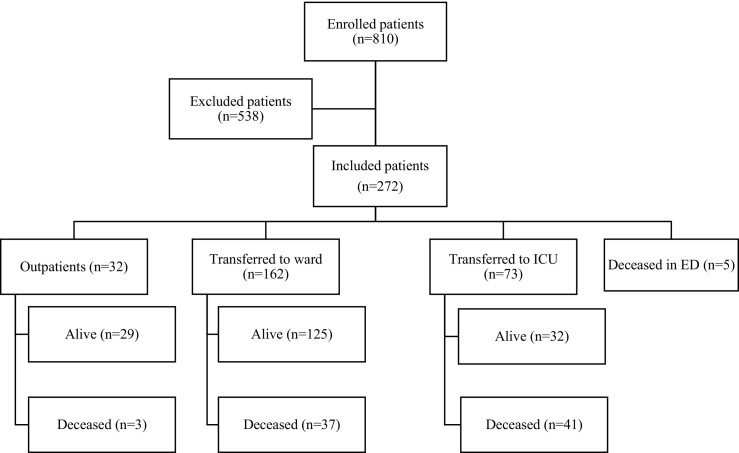
We included all patients who admitted to our emergency department in between 01.09.2020 and 01.09.2021, whose COVID-19 pneumonia was confirmed by PCR, and whose complete medical records could be obtained. Patients under the age of 18, pregnant patients, those with missing data on their medical records and those with any pathology that could impair pulse oximetry measurement such as anemia, hypothermia, nail polish, darkly pigmented skin, dyshemoglobinemia, hyperbilirubinemia, and severe hypotension were excluded (Fig. 1 ).
Fig. 1.
Patients flow chart.
Patients with COVID-19 were diagnosed with polymerase chain reaction (PCR) on nasopharyngeal swab.
COVID-19 patients were hospitalized and treated in line with the protocol published by Turkish Health Ministry of Health. Patients who were under 50 years of age, had no comorbidities, had a respiratory rate < 24 breaths per minute, had a SpO2 in room air >93%, and had no poor prognostic criteria in laboratory testing (lymphocyte count <800/μl or CRP > 10 x upper limit of normal value or ferritin >500 ng/ml or D-Dimer >1000 ng/ml) were discharged the remaining patients were hospitalized. Among them, those with any of the respiratory distress (any of the following: respiratory rate ≥ 30/min, room air SpO2 < 90%, PaO2/FiO2 < 300, SpO2 < 90% or PaO2 < 70 mmHg despite 5 l/min oxygen therapy), hemodynamic instability (systolic blood pressure < 90 mmHg, mean arterial pressure < 65 mmHg, heart rate > 100/min) presence of hypoperfusion (lactate >2 mmol, prolonged capillary refill time or cutis marmaratus), and acute organ dysfunction were admitted to the intensive care unit [15].
Patients with oxygen saturation < 90% in room air or severe respiratory distress (use of accessory muscles, inability to complete all sentences, respiratory rate > 30 breaths per minute) were considered as severe COVID-19 pneumonia [16].
30-day mortality was defined as documented death from any cause during hospitalization or within 30-days of admission to our emergency department.
2.3. Data collection
Demographics, comorbidities, initial physical findings, oxygenation status, laboratory findings at admission and 30-day mortality status were obtained from hospital database.
2.4. Oxygenation parameters and FiO2
To estimate FiO2, the interface utilized for oxygen delivery (nasal cannulas, single mask, high-concentration mask, noninvasive ventilation) and oxygen flow rate were used. FiO2 was calculated using the formula FiO2% = 4 x (oxygen flow l/min) + 21 for nasal-cannula and face mask oxygen therapy (Wettstein et al., Respir Care. 2005) The FiO2 value set in the ventilator was considered in patients who were receiving noninvasive ventilation support.
Pulse oximeters (Nihon Kohden BSM-4111 K, Japan) were used to monitor pulsed oxygen saturation. A nurse monitored the accuracy of the measurement while simultaneously visualizing the plethysmography curve. With a Siemens Healthineers RAPIDPoint® 500e, arterial blood gas measurements were performed immediately after sampling.
2.5. Pneumonia risk assessment scores
CURB-65 score, and PSI were commonly used scores for pneumonia severity assessment. In addition, CRB-65 is a noninvasive and practical pneumonia risk assessment score [17].
CURB-65 score of 0 or 1, CRB-65 score of 0–1 and PSI class I, II, III indicates mild to moderate pneumonia, while CURB-65 score of ≥2, CRB-65 score of ≥2 and PSI class IV and V indicates severe pneumonia.
2.6. Statistical analysis
Descriptive statistics were utilized to define variables. Proportions and counts were used to report categorical data. Continuous data were expressed as mean and standard deviation (SD) if the data were normally distributed; otherwise, medians and interquartile ranges were reported (IQR).
Univariate and multivariate analysis were used to reveal independent determinants of 30-day mortality. One of the two highly correlated parameters was removed from the model to eliminate multicollinearity. The multivariate analysis did not include any parameters that are part of a scoring system. The combination of a scoring system and an independent predictor was formed with estimating predicted probabilities from logistic regression analysis. ROC analysis was used to calculate the area under the curve (AUC) of the prediction models. To compare the AUC of the prediction models, the De-long statistic was used [18]. Statistical significance was defined as a p value of less than 0.05.
3. Theory/calculation
We assessed the discriminative ability of SpO2/FiO2 in predicting mortality in patients with COVID-19 pneumonia and its prognostic utility in combination with conventional pneumonia risk assessment scores. This is a pilot study designed to see if larger studies are warranted might be used.
4. Results
We have included 272 patients with a mean ± SD age of 64.7 ± 14.7. Of these, 86 (31.6%) had mortality within 30 days. One hundred fourteen (41.9%) patients were female and 191 (70.2%) had at least one comorbidity. The most common comorbidity was hypertension (52.7%), followed by diabetes mellitus (34.6%) and ischemic heart disease (16.2%). Among the 272 patients admitted to the emergency department, 226 (83.1%) had severe pneumonia. Overall, 32 (11.8%) patients were discharged, 162 (59.6%) were admitted to a hospital ward, 73 (26.8%) were admitted to the intensive care unit and 5 (1.8%) deceased in the emergency department (Table 1 ).
Table 1.
Demographic, clinical and laboratory findings of the patients
|
All patients (n=272) |
Alive patients (n=186) |
Deceased patients (n=86) |
p value | |
|---|---|---|---|---|
| Age (years) (mean ± SD) | 64.7 ± 14.7 | 61.1 ± 14.1 | 72.7 ± 12.8 | < 0.001 |
| Female, n (%) | 114 (41.9) | 83 (44.6) | 31 (36) | 0.19 |
| Comorbidity, n (%) | ||||
| Any comorbidity | 191 (70.2) | 125(67.2) | 66 (76.7) | 0.11 |
| Hypertension | 137 (52.7) | 89 (50) | 48 (58.5) | 0.23 |
| Diabetes Mellitus | 90 (34.6) | 63 (35.4) | 27 (32.9) | 0.77 |
| Asthma | 31 (11.9) | 23 (12.9) | 8 (9.8) | 0.54 |
| COPD | 26 (10.0) | 18 (10.1) | 8 (9.8) | 1.00 |
| Ischemic heart disease | 42 (16.2) | 26 (14.6) | 16 (19.5) | 0.36 |
| Chronic renal disease | 15 (5.8) | 5 (2.8) | 10 (12.2) | 0.007 |
| Congestive heart failure | 18 (6.9) | 7 (3.9) | 11 (13.4) | 0.008 |
| Physical findings n (%) | ||||
| Respiratory rate ≥ 30/min | 85 (31.4) | 44 (23.7) | 41 (48.2) | < 0.001 |
| PaO2 < 60 mmHg | 153 (59.1) | 94 (53.1) | 59 (72) | 0.004 |
| Pulse rate ≥ 125/min | 9 (3.8) | 8 (5) | 1 (1.4) | 0.27 |
| SBP < 90 mmHg or DBP < 60 mmHg |
39 (15.8) | 20 (11.8) | 19 (24.4) | 0.015 |
| Laboratory parameters | ||||
| Lymphocyte count (cells/mm3) * | 1220.1 ± 107.2 | 1225.2 ± 597.9 | 1209 ± 1695.9 | 0.93 |
| Hematocrit + | 39.4 (35.9–42.7) | 40.1 (36.3–43.3) | 38.5 (34.3–42.2) | 0.04 |
| Platelet count (103/mm3) * | 234.7 ± 99.8 | 239.5 ± 98.9 | 224.4 ± 101.6 | 0.24 |
| BUN (mg/dl) * | 23.1 ± 20.7 | 14.7 (11.4–19.5) | 24.7 (13.8–38.0) | < 0.001 |
| Creatinine (mg/dl) + | 0.91 (0.74–1.19) | 0.85 (0.73–1.06) | 1.14 (0.83–1.76) | <0.001 |
| Ferritin (ng/l) * | 651 ± 669.5 | 150.1 (74.9–337.4) | 390.5(177.5–745.4) | 0.02 |
| CRP (mg/l) * | 112.9 ± 80.7 | 97.8 ± 71.6 | 146.2 ± 89.5 | < 0.001 |
| Fibrinogen (g/dl)* | 602.2 ± 157.3 | 595.4 ± 139.3 | 616 ± 190.9 | 0.57 |
| D-dimer (ng/ml) * | 1881.1 ± 2425.6 | 1492.2 ± 1854.7 | 2872.8 ± 3344.1 | 0.03 |
| AST (u/l) * | 50.2 ± 38.2 | 47.6 ± 33.3 | 55.9 ± 46.9 | 0.10 |
| ALT (u/l) + | 26 (18–38.2) | 26 (19–39.5) | 23 (13–37.5) | 0.09 |
| Blood gases and oxygenation parameters | ||||
| PaO2 (mmHg) * | 58.7 ± 16.5 | 60.8 ± 17.3 | 54.1 ± 13.4 | 0.002 |
| SaO2 (%) * | 89 ± 8.1 | 90.6 ± 6.1 | 85.5 ± 10.6 | < 0.001 |
| PaO2/FiO2 * | 203.6 ± 97.9 | 239.2 ± 89.1 | 161.4 ± 87 | < 0.001 |
| SpO2 (%) * | 88.2 ± 8.5 | 89.6 ± 7.3 | 85.2 ± 10.2 | 0.001 |
| SpO2/ FiO2 * | 309.1 ± 135 | 357.8 ± 117.2 | 258.6 ± 133.6 | < 0.001 |
| Lactate (mmol/l) + | 1.6 (1.1–2.3) | 1.45 (1.02–2.00) | 2.00 (1.40–2.95) | < 0.001 |
| pH + | 7.45 (7.40–7.48) | 7.45 (7.41–7.48) | 7.43 (7.36–7.48) | 0.027 |
| Outcome of patients, n (%) | ||||
| Discharged from ED | 32 (11.8) | 29 (15.6) | 3(3.5) | 0.004 |
| Hospital ward | 162 (59.6) | 125 (67.2) | 37 (43) | < 0.001 |
| Intensive care unit | 73 (26.8) | 32 (17.2) | 41 (47.7) | < 0.001 |
| Death in ED | 5 (1.8) | 0 (0) | 5 (5.8) | < 0.001 |
| COVID-19 severity status | ||||
| Non - severe | 46 (16.9) | 45 (24.2) | 1 (1.2) | < 0.001 |
| Severe | 226 (83.1) | 141 (75.8) | 85 (98.8) | < 0.001 |
All statistical results refer to the comparison of alive and deceased patients.
*stands for mean ± SD, +stands for median (IQR).
Abbreviations: COPD: Chronic obstructive pulmonary disease, PaO2: partial pressure of oxygen, SBP: systolic blood pressure, DBP: diastolic blood pressure, BUN: Blood Urea Nitrogen, CRP: C-reactive protein, AST: Aspartate transaminase, ALT: Alanine aminotransferase, SaO2: arterial oxygen saturation, FiO2: Fraction of Inspired Oxygen, SpO2: peripheral oxygen saturation, pH: power of hydrogen, ED: emergency department.
Deceased patients were older, more tachypneic, hypoxemic and hypotensive at admission and they were more likely to have chronic renal disease and congestive heart failure. Regarding laboratory and blood gas measurements, deceased patients have higher levels of blood urea nitrogen (BUN), creatinine, CRP, D-dimer, and lactate levels, as well as lower levels of lymphocyte count. Pao2, PaO2/FiO2, SaO2, SpO2, SpO2/FiO2 and pH levels was shown in Table 1. Univariate analysis showed that higher levels of ferritin, CRP, D-dimer, lactate, blood urea nitrogen (BUN), creatinine, and low levels of SpO2 and SpO2 /FiO2, and lymphocyte count were associated with 30-day mortality. Results of the univariate analysis were summarized in Table 1. After performing multivariate analysis, only SpO2/FiO2 level was found to be an independent parameter in predicting 30-day mortality (OR:0.98, 95% CI: 0.98–0.99, p = 0.003) (Table 2 ).
Table 2.
Multivariate analysis of the parameters in predicting 30-day mortality
| OR | CI (95%) | p value | |
|---|---|---|---|
| Ferritin (ng/l) | 1.00 | 0.999–1.001 | 0.98 |
| CRP (mg/l) | 0.99 | 0.983–1.004 | 0.24 |
| D-dimer (ng/ml) | 1.00 | 1.000–1.001 | 0.09 |
| Lactate (mmol/ll) | 0.69 | 0.397–1.225 | 0.21 |
| SpO2 (%) | 0.69 | 0.801–1.001 | 0.052 |
| SpO2/ FiO2 | 0.98 | 0.980–0.996 | 0.003 |
CRP: C-reactive protein, SpO2: peripheral oxygen saturation, FiO2: Fraction of Inspired Oxygen.
4.1. Pneumonia risk scores in predicting 30-day mortality
A total of 89 patients had a CURB-65 score of ≥2 and 49 (55.1%) of them were deceased, while 152 patients had a CURB-65 score of <2 and 26 (17.1%) deceased within 30 days. Seventy-five patients had a CRB-65 score of ≥2 and 41 (54.7%) of them deceased within 30 days, whereas 171 patients had a CRB-65 score of <2 and 36 (21.1%) deceased within 30 days. Sixty-four patients had a PSI score of ≥ IV and 23 (18.3%) of them deceased, while 126 patients had a PSI score of < IV and 23 (18.3%) deceased within 30 days.
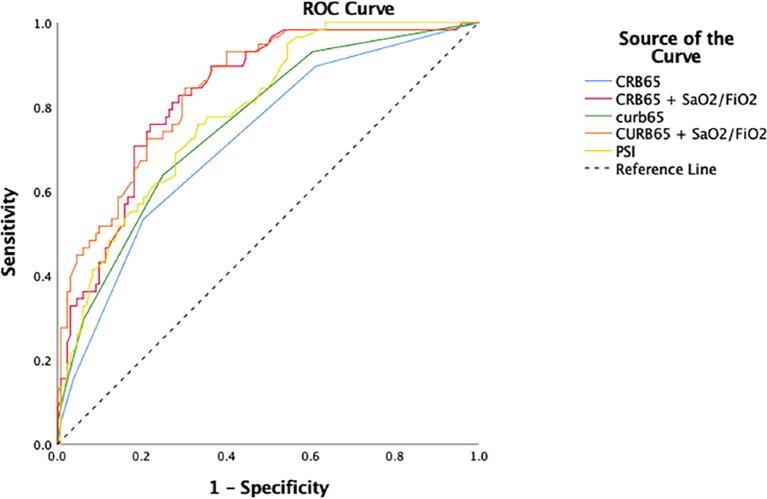
PSI, CURB-65 and CRB-65 have fair discriminative ability. PSI and CURB-65 were found to be better scores than CRB-65 in predicting 30-day mortality (AUC: 0.79 vs 0.72, p = 0.04; AUC: 0.76 vs 0.72, p = 0.01 respectively). Adding SpO2/FiO2 to CRB-65 improved the performance compared to CRB-65 alone (AUC: 0.83 vs 0.72, p = 0.001), and adding SpO2/FiO2 to CURB-65 improved the performance compared to CURB-65 alone (AUC: 0.84 vs 0.75, p = 0.001). Both SpO2/FiO2 combined with CRB-65 and SpO2/FiO2 combined with CURB-65 have good discriminative ability and seemed to be more favorable than PSI (AUC: 0.83 vs 0.75; AUC: 0.84 vs 0.75), however no significant difference was found (p = 0.21 and p = 0.06, respectively) (Table 3 , Fig. 2 ).
Table 3.
Diagnostic test performance of the risk scores in predicting 30-day mortality
| Value % (95% CI) | CRB-65 ≥ 2 | CRB-65 + SaO2/FiO2⁎ | CURB-65 ≥ 2 | CURB-65 + SaO2/FiO2⁎ | PSI ≥ IV |
|---|---|---|---|---|---|
| Sensitivity | 51 (42–65) | 81 (72–89) | 65 (53–76) | 80 (70–88) | 60 (46–73) |
| Specificity | 80 (73–86) | 72 (64–78) | 76 (69–82) | 69 (62–75) | 78 (70–85) |
| NLR | 0.6 (0.4–0.7) | 0.3 (0.2–0.4) | 0.4 (0.3–0.6) | 0.3(0.2–0.4) | 0.5 (0.3–0.7) |
| PLR | 2.5 (1.7–3.7) | 2.9 (2.2–3.7) | 2.7 (1.9–3.7) | 2.6 (2–3.2) | 2.7(1.8–4.0) |
| NPV | 79 (72–85) | 89 (84–93) | 83 (78–87) | 88 (83–92) | 82 (76–87) |
| PPV | 55 (43–66) | 57 (51–63) | 55 (47–63) | 54 (48–60) | 55 (45–64) |
| Diagnostic accuracy | 72 (66–77) | 75 (69–93) | 73 (67–78) | 72 (68–78) | 73 (66–79) |
| AUC | 72 (64–80) | 83 (77–89) | 76 (69–83) | 84 (78–90) | 79 (72–85) |
NLR: negative likelihood ratio, PLR: positive likelihood ratio, NPV: negative predictive value, PPV: positive predictive value, AUC: area under curve.
considering the most appropriate cut-off value.
Fig. 2.
ROC curves of the risk scores in predicting 30-day mortality.
5. Discussion
In our study, we evaluated the role of noninvasive risk parameters and scores in predicting 30-day mortality in patients with COVID-19. We revealed that the noninvasive parameter ‘SpO2/FiO2’ was the only independent parameter in predicting 30-day mortality and using combined model including SpO2/FiO2 and the noninvasive risk score ‘CRB-65’ improved the mortality prediction compared to CRB-65 alone. The discriminative ability of the combined model was found to be higher than PSI, however the difference was not statistically significant.
Oxygenation status is the most important parameter to determine the prognosis in patients with COVID-19 [19]. However, inflammation markers and the severity of pulmonary involvement on chest imaging were found to be associated with worse outcomes, their prediction capability was possibly due to their effects on oxygenation. PaO2/FiO2 was a useful index to accurately show the oxygenation although and its was also showed that this oxygenation index has high discriminative ability in predicting mortality in a well-designed study with 123 COVID-19 patients (AUC: 0.895, 95% CI: 0.826–0.943, p < 0.001) [3]. Despite these advantages, it is an invasive test and not practical enough to be used in crowded emergency department settings.
The noninvasive parameter ‘SpO2/FiO2’ was found to be correlated with PaO2/FiO2 in patients with COVID-19 pneumonia [20,21]. According to a multicentric study with a large cohort of patients, SpO2/FiO2 was demonstrated as a reliable parameter in predicting early need for invasive mechanical ventilation [22]. However, this association was not tested after preforming adjustment of other potential confounders. In a prospective cohort study with 180 COVID-19 patients, multivariate logistic regression analysis was performed to reveal the predictors of mortality in patients with COVID-19 and along with age and renal function, SpO2/FiO2 remained significant [23]. Similarly, Roozeman et al., showed that SpO2/FiO2 had an independent association with 28-day mortality and found to be a good alternative to PaO2/FiO2 in invasively ventilated patients with COVID-19 using a larger sample size (n = 867) [24]. Besides SpO2/FiO2 offers an advantage over arterial blood gas sampling in dynamic monitoring throughout follow-up, in addition to being noninvasive and allowing for early evaluation [25]. Despite its numerous advantages, including high discriminative ability, practicality, noninvasiveness, and repeatability, SpO2/FiO2 alone may not be used as a predictor of mortality. [12]. The fact that SpO2/FiO2 does not provide an estimate of breathing and consciousness effort could be one of the possible reasons. So, we assessed the role of existing risk scores combined with SpO2/FiO2. To our knowledge, this is the first study evaluating the risk models that includes existing risk scores and SpO2/FiO2. In our study, we revealed that SpO2/FiO2 was found to be an independent predictor (OR: 0.98, p= 0.003). This means that each additional increase of one unit in SpO2/FiO2 is associated with an 2% decrease in the odds of a patient having a mortal course. Since ‘SpO2/FiO2’ can take a wide range of values, its impact on mortality is expected to be clinically significant.
Regarding risk scores, PSI is a well-known predictor of mortality in patients with COVID-19 [6,26]. In our study, its discriminative ability was found to be high (AUC: 0.79), in line with the literature. However, it is not a practically useful score during the pandemic. Similarly, while CURB-65 is also powerful in predicting mortality in COVID-19 patients, it also includes an invasive blood test parameter. On the other hand, CRB-65 is a noninvasive score and reported to be useful in patients with COVID-19 in the emergency department [27]. We found that the combined model including SpO2/FiO2, and CRB-65 have a good performance in predicting mortality.
Our study was limited due to its single centered and a retrospective nature. Second, there could be a maturation bias based on rapidly developing treatment approaches during one year. Third, severity of thoracic involvement on chest imaging and radiological patterns were not taken into account. Lastly, we used estimated FiO2 which may not always be accurate, as the flow rates provided by the oxygen support devices are likely to be lower than the predicted FiO2.
6. Conclusions
In conclusion, this retrospective study, including a large cohort of patients with COVID-19 pneumonia admitted to the emergency department, showed that SpO2/FiO2 is a promising index in predicting mortality. Addition of SpO2/FiO2 to CRB-65 improved the role of CRB-65 alone, however it performed similar to PSI. The combined noninvasive model of SpO2/FiO2 and CRB-65 may help physicians quickly stratify COVID-19 patients on admission, which is expected to be particularly important in hospitals still stressed by pandemic volumes.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Merve Osoydan Satici: Writing – review & editing, Writing – original draft, Validation, Supervision, Software, Project administration, Methodology, Formal analysis, Conceptualization. Mehmet Muzaffer İslam: Writing – review & editing, Writing – original draft, Project administration, Methodology, Formal analysis, Conceptualization. Celal Satici: Writing – review & editing, Writing – original draft, Supervision, Software, Methodology, Formal analysis, Conceptualization. Cemre Nur Uygun: Writing – review & editing, Writing – original draft, Visualization, Investigation, Data curation. Enis Ademoglu: Writing – review & editing, Writing – original draft, Resources, Investigation, Data curation. İbrahim Altunok: Writing – review & editing, Writing – original draft, Software, Resources, Investigation, Data curation, Conceptualization. Gokhan Aksel: Writing – review & editing, Writing – original draft, Supervision, Conceptualization. Serkan Emre Eroglu: Writing – review & editing, Writing – original draft, Supervision, Conceptualization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Shi C., Wang L., Ye J., Gu Z., Wang S., Xia J., et al. Predictors of mortality in patients with coronavirus disease 2019: a systematic review and meta-analysis. BMC Infect Dis. 2021;21(1) doi: 10.1186/s12879-021-06369-0. [Dec 1] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du R.H., Liang L.R., Yang C.Q., Wang W., Cao T.Z., Li M., et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020 May;1(55):5. doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gu Y., Wang D., Chen C., Lu W., Liu H., Lv T., et al. PaO 2/FiO 2 and IL-6 are risk factors of mortality for intensive care COVID-19 patients. Scient Rep [Internet] 2021;11(1) doi: 10.1038/s41598-021-86676-3. https://pubmed.ncbi.nlm.nih.gov/33795768/ Dec 1 [cited 2022 Jan 16]. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L., et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020 May 1;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marcolino M.S., Pires M.C., Ramos L.E.F., Silva R.T., Oliveira L.M., Carvalho R.L.R., et al. ABC 2-SPH risk score for in-hospital mortality in COVID-19 patients: development, external validation and comparison with other available scores. Int J Infect Dis. 2021 Sep;1(110):281–308. doi: 10.1016/j.ijid.2021.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lazar Neto F., Marino L.O., Torres A., Cilloniz C., Meirelles Marchini J.F., Garcia de Alencar J.C., et al. Community-acquired pneumonia severity assessment tools in patients hospitalized with COVID-19: a validation and clinical applicability study. Clin Microbiol Infect. 2021 Jul 1;27(7):1037.e1–1037.e8. doi: 10.1016/j.cmi.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Satici C., Demirkol M.A., Sargin Altunok E., Gursoy B., Alkan M., Kamat S., et al. Performance of pneumonia severity index and CURB-65 in predicting 30-day mortality in patients with COVID-19. International journal of infectious diseases: IJID. 2020 Sep 1;98:84–89. doi: 10.1016/j.ijid.2020.06.038. https://pubmed.ncbi.nlm.nih.gov/32553714/ [cited 2022 Jan 27]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alsaei A., Onyambu S., Mateen P., Javed M.A., Coriasso C., Khan A., et al. Predicting mortality in COVID-19: comparison of APACHE IV, MEWS, and mSOFA. Crit Care Med. 2021 Jan;49(1):102. [Google Scholar]
- 9.Raschke R.A., Agarwal S., Rangan P., Heise C.W., Curry S.C. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA. 2021 Apr 13;325(14):1469–1470. doi: 10.1001/jama.2021.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwack W.G., Lee D.S., Min H., Choi Y.Y., Yun M., Kim Y., et al. Evaluation of the SpO2/FiO2 ratio as a predictor of intensive care unit transfers in respiratory ward patients for whom the rapid response system has been activated. PLoS One. 2018;13(7):1–11. doi: 10.1371/journal.pone.0201632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prakash J., Bhattacharya P.K., Yadav A.K., Kumar A., Tudu L.C., Prasad K. ROX index as a good predictor of high flow nasal cannula failure in COVID-19 patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. J Crit Care. 2021;66:102–108. doi: 10.1016/j.jcrc.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gonius A., Albaar T.M., Rahma F.N., Widowati A.R. SaO2 / FiO2 ratio as mortality predictor in COVID-19: a meta-analysis. Pakistan J Med Health Sci. 2021;14(4):1564–1567. [Google Scholar]
- 13.McNally M., Curtain J., O’Brien K.K., Dimitrov B.D., Fahey T. Validity of British Thoracic Society guidance (the CRB-65 rule) for predicting the severity of pneumonia in general practice: systematic review and meta-analysis. Br J Gen Pract. 2010;60(579) doi: 10.3399/bjgp10X532422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dwyer R., Hedlund J., Henriques-Normark B., Kalin M. Improvement of CRB-65 as a prognostic tool in adult patients with community-acquired pneumonia. BMJ Open Respir Res. 2014 Jul 8;1(1):38. doi: 10.1136/bmjresp-2014-000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.T.C. Sağlık Bakanlığı Bilimsel Danışma Kurulu Çalışması. Halk Sağlığı Genel Mudurlugu; Ankara: 2021 july. COVID-19 (SARS-CoV-2 ENFEKSİYONU) ERİŞKİN HASTA TEDAVİSİ. [Google Scholar]
- 16.WHO (World Health Organization) vol. 18. November 2021. Guideline clinical management of COVID-19 patients: Living guideline. [Google Scholar]
- 17.Bont J., Hak E., Hoes A.W., Macfarlane J.T., TJM Verheij. Predicting Death in Elderly Patients With Community-Acquired Pneumonia: A Prospective Validation Study Reevaluating the CRB-65 Severity Assessment Tool. Archives of Internal Medicine [Internet] 2008 Jul 14;168(13):1465–1468. doi: 10.1001/archinte.168.13.1465. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/414343 [cited 2022 Feb 1]. Available from: [DOI] [PubMed] [Google Scholar]
- 18.DeLong E.R., DeLong D.M., Clarke-Pearson D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988 Sep;44(3):837. [PubMed] [Google Scholar]
- 19.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (London, England) 2020 Mar 28;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar A., Aggarwal R., Khanna P., Kumar R., Singh A.K., Soni K.D., et al. Correlation of the SpO2/FiO2 (S/F) ratio and the PaO2/FiO2 (P/F) ratio in patients with COVID-19 pneumonia. Med Int. 2021 Nov [Google Scholar]
- 21.Catoire P., Tellier E., de la Rivière C., Beauvieux M.C., Valdenaire G., Galinski M., et al. Assessment of the SpO2/FiO2 ratio as a tool for hypoxemia screening in the emergency department. Am J Emerg Med. 2021 Jun;1(44):116. doi: 10.1016/j.ajem.2021.01.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alberdi-Iglesias A., Martín-Rodríguez F., Ortega Rabbione G., Rubio-Babiano A.I., Núñez-Toste M.G., Sanz-García A., et al. Role of SpO2/FiO2 Ratio and ROX Index in Predicting Early Invasive Mechanical Ventilation in COVID-19. A Pragmatic, Retrospective, Multi-Center Study. Biomedicines. 2021 Aug 1;9(8) doi: 10.3390/biomedicines9081036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.von Vopelius-Feldt J., Watson D., Swanson-Low C., Cameron J. 2020. Estimated Sp02/Fio2 ratio to predict mortality in patients with suspected COVID-19 in the emergency department: A prospective cohort study. [Google Scholar]
- 24.Roozeman J.-P., Mazzinari G., Serpa Neto A., Hollmann M.W., Paulus F., Schultz M.J., et al. Prognostication using SpO2/FiO2 in invasively ventilated ICU patients with ARDS due to COVID-19 – insights from the PRoVENT-COVID study. J Crit Care. 2022 Apr;1(68):31–37. doi: 10.1016/j.jcrc.2021.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu X., Jiang L., Chen T., Wang Y., Zhang B., Hong Y., et al. Continuously available ratio of SpO2/FiO2serves as a noninvasive prognostic marker for intensive care patients with COVID-19. Respir Res. 2020;21(1):1–4. doi: 10.1186/s12931-020-01455-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradley J., Sbaih N., Chandler T.R., Furmanek S., Ramirez J.A., Cavallazzi R. Pneumonia severity index and CURB-65 score are good predictors of mortality in hospitalized patients with SARS-CoV-2 community-acquired pneumonia. Chest. 2021 Nov;161(4):927–936. doi: 10.1016/j.chest.2021.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Su Y., Wei Tu G., Jie Ju M., Ji Yu S., Li Zheng J., Guang Ma G., et al. Comparison of CRB-65 and quick sepsis-related organ failure assessment for predicting the need for intensive respiratory or vasopressor support in patients with COVID-19. The. J Inf Secur. 2020;81(4):647. doi: 10.1016/j.jinf.2020.05.007. [Oct 1] [DOI] [PMC free article] [PubMed] [Google Scholar]