Diana had terrible nights, with restless sleep and haunting nightmares. Her coworkers joked about how easily she would startle. She tried to avoid any thoughts and feelings about her childhood, especially about her father. She had a sense that she deserved to be hurt but she had no idea why. She sometimes felt unreal, like she existed only from the neck up—her body didn’t feel like it was there at all.
To her therapist, Diana appeared calm, almost flat, though inside her mind felt busy. When the conversation turned to childhood, Diana felt like she was watching from outside her body. It sounded like someone inside her head was screaming to shut up—it isn’t safe. There was crying inside that felt like it belonged to someone else. She couldn’t tell whether she was hearing her thoughts out loud or actually hearing voices inside her head, saying that she caused the abuse—she was bad. When she told her therapist about what her father had done, Diana felt like an observer while someone else from inside was speaking. She knew this wasn’t possible, but that’s still how it felt. She worried that she was losing her mind. This couldn’t be real…could those things really have happened to her as a child?
As he listened to her story, the therapist also felt confused. Diana had intact reality testing, so this wasn’t psychosis, but what else could it be? It reminded him of multiple personality disorder, but wasn’t that kind of a made-up thing?
One of the earliest people to wrestle with this tension was Pierre Janet, a brilliant Parisian scholar and clinician, renowned for his ability to differentiate genuine from feigned symptoms (1). Beginning in the late 1800s, Janet’s career focused mostly on so-called hysterical women, many of whom experienced dissociative symptoms, including double consciousness.1 Remarkably, 100 years before George Engel coined the term, Janet offered a biopsychosocial formulation of what we would now call dissociative identity disorder (DID): These individuals had experienced traumatic events that they had banished from consciousness but that nevertheless continued to influence their thoughts and actions; moreover, these events led to bodily manifestations (1). It would take almost a century for scientists to begin to understand how trauma changed biology.
A major reason no one studied this for so long had to do with Janet’s most famous contemporary, Sigmund Freud. Initially, Freud agreed with Janet’s observations—he believed that hysteria was related to traumatic experiences and, in particular, childhood sexual abuse. However, amidst a professional rivalry with Janet, Freud abandoned these original ideas and instead asserted that hysterical symptoms were the result of repressed sexual fantasies rather than actual traumatic events. The reason for this shift remains controversial. In part, Freud couldn’t believe that sexual abuse could be so prevalent: “Surely such widespread perversions against children are not very probable” (2).
For a long time, clinicians favored Freud’s repressed trauma fantasy as the central cause of hysteria, and interest in the field remained muted. Then, two major sociopolitical events in the United States reminded Americans of both the prevalence and impact of trauma: the return of Vietnam War veterans suffering from what would ultimately be called posttraumatic stress disorder (PTSD); and the rise of second-wave feminism shedding light on domestic violence and childhood abuse. Finally, people were ready to pay attention to trauma-spectrum disorders. Rigorous research began.
The most obvious hypothesis was that stress systems must be dysregulated in some way. At the time, though, researchers had to rely on indirect measurements of these systems, such as excreted metabolites in a 24-hour urine collection (3). While some early findings were encouraging, results were conflicting. Soon it became clear that the problem was one of timescale: individuals with PTSD might be physiologically normal except during the discrete times when they were triggered. A 24-hour window for biomarker collection was too long. The researchers needed an approach with a faster time resolution.
A crucial methodological breakthrough came with the development of neuroimaging and, ultimately, symptom provocation paradigms. The idea was simple: researchers asked participants to narrate their traumatic experiences and then played back these recordings during the scan; the researchers could then acquire measures of brain activity while the individuals were actively symptomatic. Early data were incredibly encouraging—as expected, they showed increased autonomic arousal and hyperactive amygdala activity (4,5). This matched many patients’ subjective reports of hyperarousal and reactivity. But there was a catch that emerged as time went on: some patients didn’t show this hyperactivity.
Canadian psychiatrist Ruth Lanius was intrigued by these mixed findings. At a time when most research focused on male combat veterans, Lanius was working on an inpatient unit with a broader cohort of trauma patients, including women. She wanted to understand what was happening in their brains, especially when they were most symptomatic.
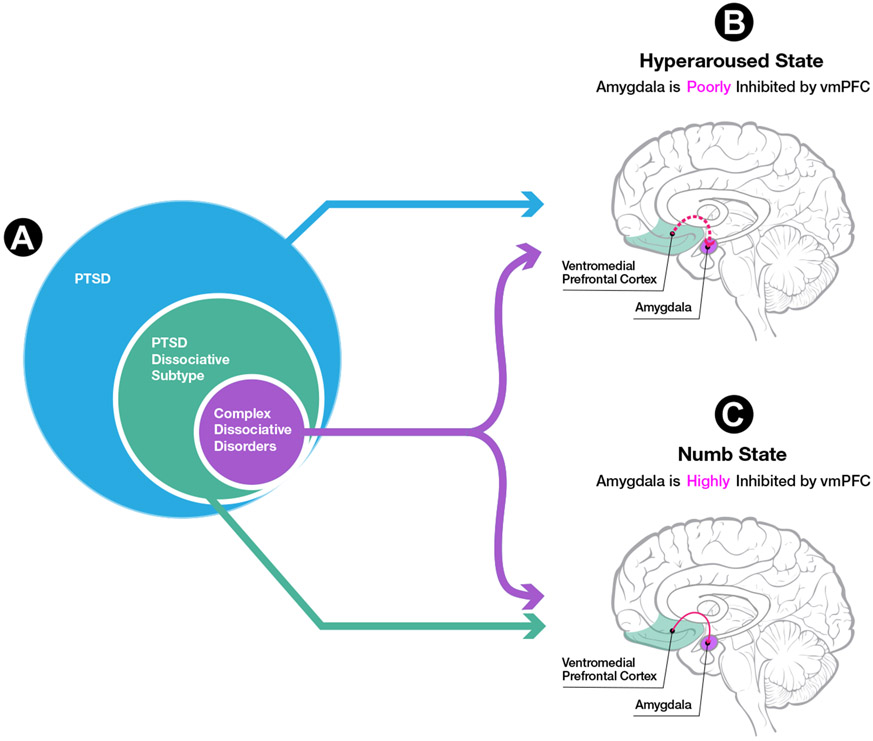
So Lanius turned to the same symptom provocation paradigm. Her first participant was a woman with a history of childhood abuse and active PTSD. Her symptoms were so severe that Lanius and the MRI technologist nervously speculated about how high her heart rate might spike during the trauma script. To their surprise, as the script was read, her heart rate steadily decreased. After the scan, the participant reported feeling numb, detached, and outside her body. Whereas historically she would have been deemed a “physiologic nonresponder” (and even excluded from some studies), Lanius realized that this wasn’t a nonresponse at all—it was the response! Lanius (5) proceeded to focus her research on these individuals with a dissociative subtype of PTSD (Figure 1). Within this group, she also identified another subset with even more severe symptomatology, reaching levels seen in complex dissociative disorders such as DID.
Figure 1.
(A) Conventional posttraumatic stress disorder (PTSD) is characterized by a dominance of hyperarousal symptoms. In contrast, 15% to 30% of individuals with PTSD have the dissociative subtype characterized by symptoms of depersonalization and derealization—that is, feeling numb and detached from their sense of self, body, and environment. Within the PTSD dissociative subtype group, approximately half of individuals have more extensive dissociative symptoms, including individuals who meet criteria for dissociative identity disorder (DID). In neuroimaging studies of DID, researchers have asked subjects to shift between two prototypical self-states: one that feels hyperaroused, emotionally flooded, and like the traumatic event happened to them personally; and one that feels numb and detached, as if the traumatic event did not happen to them personally. (B) Typical findings for conventional PTSD during symptom provocation paradigms, including increased limbic activity (e.g., amygdala) and decreased cortical emotion regulation–related activity (e.g., ventromedial prefrontal cortex [vmPFC]). Together these findings demonstrate, on average, undermodulation of emotion and arousal in conventional PTSD. Individuals with DID also exhibit this pattern in symptom provocation paradigms when they are in a hyperaroused self-state, as described above. (C) In contrast, panel (C) illustrates typical findings for the dissociative subtype of PTSD during symptom provocation paradigms, including decreased limbic activity (e.g., amygdala) and increased cortical emotion regulation-related activity (e.g., vmPFC). These findings support, on average, a pattern of emotion/arousal overmodulation in the dissociative subtype of PTSD. Individuals with DID also exhibit this overmodulation pattern in symptom provocation paradigms when they are in a numb self-state, as described above.
Dutch neuroscientist Simone Reinders was interested in just this subset. She was familiar with a series of small studies that had pointed to electrophysiological differences in individuals with DID, especially in the temporal lobe (6). She was also aware of media depictions of multiple personality disorder that had spurred significant controversy—to the point of people questioning whether multiple personality disorder (now called DID) was even a real condition. Despite this controversy, Reinders (7) used modern neuroimaging approaches to meticulously demonstrate patterns of brain structure and function in DID that partially overlapped with patterns in PTSD. She was also able to demonstrate distinct patterns of activation that were consistent with compartmentalization of self-states (Figure 1) (7). Overall, her work placed DID on a continuum with PTSD, showing that it was both biologically “real” and phenomenologically distinct.
After more than a century, science is finally catching up with the experiences of front-line clinicians. Janet’s original formulation was prescient. DID is, in fact, a complex, biopsychosocial syndrome—an alternative neurodevelopmental pathway that can emerge with chronic childhood maltreatment (8). The core clinical feature is a disruption to the sense of self and mind. Under ordinary circumstances, children gradually coalesce a cohesive sense of self; however, in the context of trauma, individuals with the capacity to dissociate (perhaps based on genetic factors) can be left with discrete self-states that patients describe as feeling like they’re “not me” (8). These “not me” feelings are largely experienced internally and, contrary to media portrayal, often not observable externally. In addition, as Diana illustrated, individuals with DID experience both conventional PTSD symptoms and also amnesia, depersonalization, and derealization. This qualitative description is now supported by the neuroimaging literature (6).
Practical applications of this work abound. Contemporary neuroimaging approaches may identify a brain fingerprint of DID (9,10). This would further dispel uncertainty about the veracity of DID as a distinct biological entity and help connect patients with effective, specialized treatment. Moreover, imaging findings may point the way toward neuromodulatory targets that could improve function in dysregulated circuits.
At the end of the day, a robust understanding of DID helps address one of the most challenging aspects of clinical care. Survivors of abuse may both doubt the reality of their traumatic experiences and even disavow having DID. These feelings may cause others to collude with the denial. To accept the diagnosis of DID means accepting both the individual horror and the societal implications of “widespread perversions against children.” A contemporary understanding of DID will enable more clinicians to tolerate situations that engender intense countertransference, to connect empathically, and to communicate thoughtfully and effectively with patients—thereby helping them understand their condition and available treatment.
A painful truth is that misplaced doubt over the existence of DID has prevented people from accessing effective treatment. Ironically, despite Freud’s polarizing views on hysteria, modern versions of his talk therapy—relational trauma therapy—can successfully treat DID. With the right treatment, individuals like Diana can learn to trust their feelings and experience their thoughts and bodies as their own.
Acknowledgments and Disclosures
Clinical Commentaries are produced in collaboration with the National Neuroscience Curriculum Initiative (NNCI). DAR, in his dual roles as Executive Director of the NNCI and as Education Editor of Biological Psychiatry, manages the development of these commentaries but plays no role in the decision to publish each commentary. The NNCI is funded in part by the Deeda Blair Research Initiative Fund for Disorders of the Brain through support to the Foundation for the National Institutes of Health and by National Institutes of Health Grant No. R44 MH115546-01. DAR is supported by R25 MH071584-11 and by the National Center for PTSD, Clinical Neuroscience Division. MLK reports unpaid membership on the Scientific Committee for the International Society for the Study of Trauma and Dissociation (ISSTD), support from National Institute of Mental Health Grant No. R01 MH119227, and support from McLean Hospital’s Trauma Scholar Fund. LAML reports unpaid membership on the Scientific Committee for ISSTD, support from National Institute of Mental Health Grant No. K01 MH118467, and support from McLean Hospital’s Julia Kasparian Fund for Neuroscience Research. The ISSTD and the National Institute of Mental Health were not involved in the preparation of the manuscript.
We thank Richard Chefetz for his help during the preparation of this manuscript and Phoenix Rances Wang for their graphical design assistance. The first phrase in the article title is from the poem “I Am Not I” by Juan Ramón Jiménez.
LAML reports spousal intellectual property payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals unrelated to the present work. DAR and MLK report no biomedical financial interests or potential conflicts of interest.
Footnotes
Note: we use the word “hysteria” in its historical context, while acknowledging it as problematic.
Contributor Information
Lauren A.M. Lebois, McLean Hospital, Belmont, Massachusetts; Department of Psychiatry, Harvard Medical School, Boston, Massachusetts
David A. Ross, Department of Psychiatry, Yale University School of Medicine, New Haven, Connecticut
Milissa L. Kaufman, McLean Hospital, Belmont, Massachusetts; Department of Psychiatry, Harvard Medical School, Boston, Massachusetts
References
- 1.Ellenberger HF (1970). The Discovery of the Unconscious: The History and Evolution of Dynamic Psychiatry, vol. 1. New York: Basic Books. [Google Scholar]
- 2.Freud S (1985): Letter from Freud to Fliess, September 21, 1897. In: Masson JM, editor. The Complete Letters of Sigmund Freud to Wilhelm Fliess, 1887-1904. Cambridge, MA, and London, England: The Belknap Press of Harvard University Press, 264–267. [Google Scholar]
- 3.Yehuda R, Southwick S, Giller EL, Ma X, Mason JW (1992): Urinary catecholamine excretion and severity of PTSD symptoms in Vietnam combat veterans. J Nerv Ment Dis 180:321–325. [DOI] [PubMed] [Google Scholar]
- 4.Rauch SL, van der Kolk BA, Fisler RE, Alpert NM, Orr SP, Savage CR, et al. (1996): A symptom provocation study of posttraumatic stress disorder using positron emission tomography and script-driven imagery. Arch Gen Psychiatry 53:380–387. [DOI] [PubMed] [Google Scholar]
- 5.Lanius RA, Boyd JE, McKinnon MC, Nicholson AA, Frewen P, Vermetten E, et al. (2018): A review of the neurobiological basis of trauma-related dissociation and its relation to cannabinoid-and opioid-mediated stress response: A transdiagnostic, translational approach. Curr Psychiatry Rep 20:118–132. [DOI] [PubMed] [Google Scholar]
- 6.Lebois LAM, Kaplan C, Palermo CA, Pan X, Kaufman ML (2022): A grounded theory of dissociative identity disorder: Placing DID in mind, brain, and body. In: Dorahy M, Gold S, editors. Dissociation and the Dissociative Disorders: Past, Present, Future. Routledge, New York. [Google Scholar]
- 7.Reinders AATS, Willemsen ATM, den Boer JA, Vos HPJ, Veltman DJ, Loewenstein RJ (2014): Opposite brain emotion-regulation patterns in identity states of dissociative identity disorder: A PET study and neurobiological model. Psychiatry Res 223:236–243. [DOI] [PubMed] [Google Scholar]
- 8.Putnam FW (2016): The Way We Are: How States of Mind Influence Our Identities, Personality and Potential for Change. London: International Psychoanalytic Books. [Google Scholar]
- 9.Reinders AATS, Marquand AF, Schlumpf YR, Chalavi S, Vissia EM, Nijenhuis ERS, et al. (2018): Aiding the diagnosis of dissociative identity disorder: Pattern recognition study of brain biomarkers. Br J Psychiatry 215:536–544. [DOI] [PubMed] [Google Scholar]
- 10.Lebois LAM, Li M, Baker JT, Wolff JD, Wang D, Lambros AM, et al. (2021): Large-scale functional brain network architecture changes associated with trauma-related dissociation. Am J Psychiatry 178:165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]