Abstract
Purpose
To evaluate medical student confidence in diagnosing dermatologic diseases in skin of color.
Methods
A voluntary supplemental module was implemented as part of the second-year dermatology curriculum at Wayne State University School of Medicine (WSU SOM) in Detroit, Michigan. The goal of the module was to ascertain whether it may increase confidence in students with their approach to diagnosing diseases in darker skin tones.
Results
Seventy-seven of 295 students (26%) completed a “Skin of Color” optional module consisting of thirteen cases of common skin pathologies in African American patients. A pre- and post-survey performed to assess students’ confidence using a five-point Likert scale. After completing the module, medical students demonstrated a statistically significant increase in confidence in diagnosing skin pathologies in skin of color.
Conclusion
Dermatology pre-clinical course work should include supplementary materials to increase student confidence in diagnosing skin diseases in darker skin tones.
Keywords: medical education, health disparities, epidemiology, skin of color
Introduction
Dermatological diseases may go unnoticed or misdiagnosed in skin of color. Although affected at a much lower incidence, people of color are more likely to die from skin cancer due to deviation in presentation or due to detection at an advanced stage.1,2 Skin of color patients face tremendous health disparities when it comes to dermatologic diseases including but not limited to: misconceptions regarding skin diseases in people of color, misdiagnosis due to insufficient training in diagnosing dermatological disease in skin of color, advanced presentation at time of diagnosis, and the lack of minority representation in dermatology.3–5
Dermatology is not emphasized in medical schools, with some medical schools devoting 10 curriculum hours or less to dermatology.6 In a survey by McKleskey, 8% of medical schools responded that instruction in dermatology was not a core requirement.7 In assessing knowledge, Ulman found that medical students had a paucity of knowledge in diagnosing and treating skin diseases, scoring 49.9% and 43%, respectively in a 15-question quiz on common skin diseases. 89% of their respondents only felt slightly confident or not confident at all in their training to accurately diagnose skin diseases.6
There are few dermatologists from underrepresented minorities (URM). Current estimates show that 4% of dermatologists self-identify as Hispanic and 3% of dermatologists self-identify as African American.8,9 The lack of diversity in dermatology is evident and is thought to contribute to the disparity in care among different ethnic groups.
There are few educational resources that underscore dermatological disease in skin of color patients. It is imperative that we innovate educational systems at the medical student level to begin to address these disparities. Medical schools should incorporate images of skin disease from patients with skin of color into their dermatology curriculum. For example, researchers examined the percent of skin of color images in core educational resources and found they ranged from 4%-19%. Furthermore, of the 370 dermatologic educational events per year, approximately 8 were dedicated to skin diseases of non-White people.10 Medical school faculty, especially in urban settings, should delve deeper into their resources to ensure medical students are receiving an education in ethnic skin diseases.
We proposed to the dermatology faculty at Wayne State University School of Medicine located in Detroit, MI that a module pertaining to skin of color be added to the second-year dermatology curriculum. In the current Musculoskeletal, Dermatology, and Peripheral Nervous System curriculum, 91% of images were lighter skin tones, and 9% were darker skin tones. With this module we hope to educate the medical students about skin disease in darker skin types.
To better serve diverse patient populations, medical students should be provided with additional resources devoted to diagnosing skin pathologies in skin of color. By enriching the dermatology curriculum through this pilot addition, future physicians can provide exceptional medical care to people of ethnic minorities and help bridge disparities in the healthcare system.
With this study, we hope to assess student confidence in diagnosing dermatological diseases, such as rashes, infections, and cancers in skin of color.
Methods
Setting and Participants
Inclusion criteria included second year medical students at Wayne State University School of Medicine enrolled in the Musculoskeletal, Dermatology, and Peripheral Nervous System course. Recruitment of students was done by invitation via e-mail by the Dermatology course director. Participation was voluntary. Students were able to access the surveys and module via Canvas (an educational platform used at Wayne State University). Exclusion criteria includes anyone who is not enrolled in the second year Musculoskeletal, Dermatology, and Peripheral Nervous System course at Wayne State University School of Medicine. Inspiration was drawn from a similar study done to increase the confidence in clinical assessment of musculoskeletal disorders.9
Design
A pre-and post-test survey-based study was carried out in second-year medical students at Wayne State University School of Medicine in Detroit, Michigan to assess confidence levels in diagnosing diseases in skin of color. Students had the option to complete an optional online module entitled “Skin of Color.” They completed a pre-test and post-test survey assessing confidence using four questions rated on a Likert scale.
Intervention
A pre and post-survey was completed before and after the module. Three additional questions were asked following the module to assess the quality also using a Likert scale system. Students were asked open-ended questions regarding the usefulness of the module, as well as what improvements could be made. Consent was obtained via an information sheet at the beginning of the pre-and post-module surveys. The surveys were completed anonymously and voluntarily. The module included thirteen cases based on the following skin diseases: non-bullous impetigo, tinea capitis, tinea corporis, molluscum contagiosum, poison ivy, contact dermatitis, allergic contact dermatitis, atopic dermatitis, squamous cell carcinoma in situ, squamous cell carcinoma, basal cell carcinoma, acral lentiginous melanoma, discoid lupus erythematosus and vitiligo. The module presentation was case based.
Outcomes Measured/Analysis
Students were asked to report their confidence level in diagnosing rashes, infections, and cancer in skin of color before and after module completion. The total number of students enrolled in this course was 295. 145 began the pre-test and 118 completed the pre-test. The pre-test had four survey questions assessing confidence in approaching the diverse patient. The degree of confidence was assessed on a five-point Likert scale (1=very low, 2=low, 3=moderate, 4=high, 5=very high). The same questions were assessed in the post-survey to assess change in confidence. An additional five questions were asked for feedback on the usefulness of the module. Data from completed surveys was collected and stored anonymously using Qualtrics and was de-identified. Each student was given an anonymous login ID. Statistical analysis was completed using a paired two-sample t-test on Excel. There were no risks or potential to be harmed in this survey study.
IRB/Resources
Knowledge of skin disease was required. The module was developed with the guidance of WSU faculty dermatologist (Meena Moossavi). No additional training was necessary. Creating the module on an interactive platform required assistance from the medical education support team at Wayne State University School of Medicine. Creation of the survey and data collection was executed using the website Qualtrics. Materials to produce the module were obtained from VisualDx and were free to use with proper citations. The pre/post survey and intervention were approved by the Wayne State University Institutional Review Board.
Results
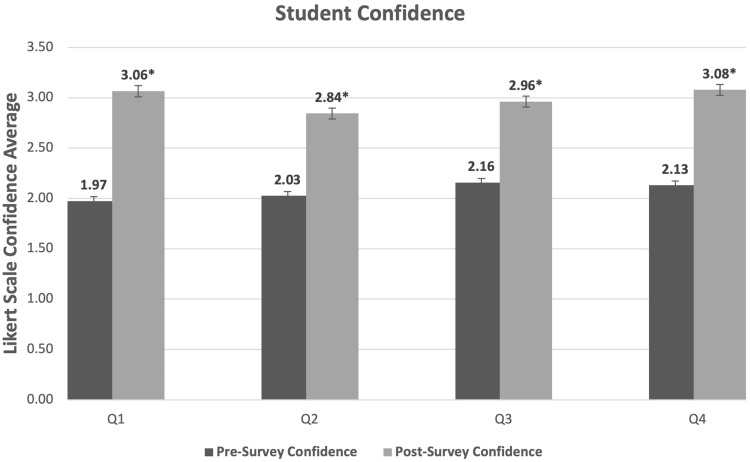
Using a 1–5 Likert scale, we measured students’ confidence in diagnosing skin infections in African Americans, confidence in diagnosing skin cancer in African Americans, confidence in recognizing differences in morbidity and mortality of dermatological conditions in African Americans and confidence in approaching skin diseases in a variety of skin tones. Table 1 demonstrates a comparison between the pre and post surveys. Four questions were used to demonstrate whether confidence improved. Confidence was assessed on a Likert scale (1–5). A paired two tailed t-test was run using Excel. A p value less than 0.05 was deemed significant. Table 2 demonstrates survey questions used to assess quality of the module appraised by the students on a 1–5 Likert scale. 1 represents “not helpful at all”, 2 “somewhat helpful”, 3 “fairly helpful”, 4 “very helpful”, and 5 “extremely helpful”.
Table 1.
Data Demonstrating the Confidence of Students Before and After Taking the Module. Four Questions Were Used to Demonstrate Whether Confidence Improved. Confidence Was Assessed on a Likert Scale (1–5). A Paired Two Tailed t-Test Was Run Using Excel. A p value Less Than 0.05 Was Deemed Significant
| Pre-Survey | Post-Survey | P-value | |
|---|---|---|---|
| Confidence in diagnosing skin infections in African Americans | 1.97 | 3.06 | p < 0.001 |
| Confidence in diagnosing skin cancer in African Americans | 2.03 | 2.84 | p < 0.001 |
| Confidence in recognizing differences in morbidity and mortality of dermatological conditions in African Americans | 2.16 | 2.96 | p < 0.001 |
| Confidence in approaching skin diseases in a variety of skin tones | 2.13 | 3.08 | p < 0.001 |
Table 2.
Mean Values and Standard Deviation of Feedback Questions on the Module Done Using the Likert Scale (1–5, 1= Not Helpful at All, 2= a Little Helpful, 3= Fairly Helpful, 4= Very Helpful 5 = Extremely Helpful)
| Mean | Standard Deviation | |
|---|---|---|
| Overall how would you rate this module? | 3.91 | 0.78 |
| How useful were the module materials (photos, cases, etc.)? | 4.22 | 0.79 |
| How helpful was this module to your understanding of the material? | 4.09 | 0.80 |
Pre-Survey
The total number of students enrolled in this course was 295. 145 began the pre-test and 118 completed the pretest. Only 77 students completed the entire module. The four pre-module questions and post-module questions appraised the student’s confidence in diagnosing skin infections and cancer in African Americans, differences in morbidity and mortality in African Americans skin diseases, and confidence in diagnosing skin diseases in a variety of skin tones. Likert scaling was used with five representing “very high” levels of confidence. Values for pre-test questions were 1.97, 2.03, 2.16, and 2.13 respectively.
Post-Survey
Post-survey questions assessing confidence were the same as used in the pre-survey. Values in the post test were 3.06, 2.84, 2.03, and 3.08. (P-values < 0.001) (Figure 1).
Figure 1.
Graphical data demonstrating the confidence of students before and after taking the module. A p value less than 0.05 was deemed significant, which is indicated on the graph with an asterisk (*).
Three additional questions were used to assess the student’s appraisal of the quality of the module. Detailed results are displayed in Table 2. The questions were as follows: “Overall how would you rate this module”, “How useful were the module materials”, “How useful was this module to your understanding of the material”. A five-point Likert scale was used for these questions with 5 representing extremely helpful, and 1 representing not helpful at all. Averages are as follows respectively: 3.91, 4.22, and 4.09.
There were two additional open-ended questions as follows: “What improvements would you make to this module?” and “Do you feel this module has changed your life in any way? If yes, please give an example.” Several students pointed out that the current curriculum needed more representation of darker skin diseases as most of the images were of Caucasian skin types. In the module, students also recommended images of darker skin tones from other backgrounds besides African Americans. Suggested improvements from the students included: include more pictures of the disease in skin of color and other skin tones, provide explanations as to why the wrong answers were wrong, make the clinical vignette less obvious. Although we were not assessing knowledge, many students were able to choose the correct answer due to classic presentations in the clinical vignette. Students suggested showing the image before the clinical vignette and requested questions on how to describe the lesions. Students overall found the module useful and were grateful to see some changes towards inclusivity in medicine.
Discussion
By the year 2050, it is estimated about 50% of the US population will include people with skin of color.2,9 Hispanics and African Americans also include more than 50% of uninsured patients and face worse health outcomes.9 In addition to disparities in access to care, there are also disparities in medical school curriculums and dermatology educational resources, creating future physicians that are unprepared to properly diagnose skin of color patients. Currently, medical school dermatology education lacks proper instruction on diagnosing skin diseases in skin of color. Diversity in medical school helps prepare students to serve diverse populations and diversify the workforce.9,11 By diversifying educational resources and the workforce, it is possible that marginalized ethnic populations can have better health outcomes.
In terms of our skin of color module, a statistically significant increase in confidence post-module was seen in diagnosing skin infections in African Americans, diagnosing skin cancer in African Americans, recognizing differences in morbidity and mortality of dermatological conditions in African Americans, and approaching skin diseases in a variety of skin tones. Students also deemed the module useful based on the results of the three feedback questions.
We hope that this pilot study is the start of increasing the ability of physicians to properly diagnose skin disease in patients of color, thus helping provide exceptional care to all people.
We recognize that there were some limitations in the study. Many students would have preferred that this module be required and not supplemental. Furthermore, attrition served as a limitation in this project. 66 students completed the pre-survey and module but failed to complete the post-survey. This could be due to the module being released when students were on an academic break. Subsequently, the students had to include their email in the pre-survey to receive an email that would contain links to the module and post-survey. If they did not include their email when completing the pre-survey, then they would not have received the module and post-survey link. In addition, had we made the module required instead of voluntary, perhaps 100% participation could have been achieved. To circumvent resistance from the student body, we were encouraged to make the module voluntary.
Regrettably, we did not assess for knowledge which would have been more quantifiable than confidence and may have proven a more substantial impact.
General medical education needs to discuss the lack of representation in dermatology with regards to medical education on darker skin tones. The results of this study suggest that a simple, cost-effective learning module can greatly increase the confidence of the next generation of physicians in approaching skin of color dermatology patients. One suggestion is to include an equal percentage of images of lighter and darker skin tones, and side by side comparisons for each skin pathology in the dermatology curriculum. Further research is required to investigate other approaches to increasing inclusivity in dermatology medical student courses.
Conclusion
The addition of a supplementary module to the preclinical dermatology pathophysiology focused on skin diseases in darker skin tones increased the confidence of the students who finished the module. Course directors should consider using this as a framework to develop materials to increase the confidence of the medical student in approaching the diverse dermatology patient.
Acknowledgments
Ms. Amy Dozier, the associate director of the medical education support team, who assisted in designing the module and posting the materials online to Canvas for the medical students to access.
Funding Statement
There is no funding to report.
Statement of Ethics
This study was performed in accordance with ethical guidelines of the Declaration of Helsinki. Ethical approval to conduct this study was obtained from the Institutional Review Board (IRB-20-04-215B) of Wayne State University, Detroit, MI. Consent requirement was waived as no patient materials were used in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hogue L, Harvey VM. Basal cell carcinoma, squamous cell carcinoma, and cutaneous melanoma in skin of color patients. Dermatol Clin. 2019;37(4):519–526. doi: 10.1016/j.det.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 2.Gupta AK, Bharadwaj M, Mehrotra R. Skin cancer concerns in people of color: risk factors and prevention. Asian Pac J Cancer Prev. 2016;17(12):5257–5264. doi: 10.22034/APJCP.2016.17.12.5257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buster KJ, Stevens EI, Elmets CA. Dermatologic health disparities. Dermatol Clin. 2012;30(1):53–viii. doi: 10.1016/j.det.2011.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Voorhees AS, Enos CW. Diversity in dermatology residency programs. J Investig Dermatol Symp Proc. 2017;18(2):S46–S49. doi: 10.1016/j.jisp.2017.07.001 [DOI] [PubMed] [Google Scholar]
- 5.Akhiyat S, Cardwell L, Sokumbi O. Why dermatology is the second least diverse specialty in medicine: how did we get here? Clin Dermatol. 2020;38(3):310–315. doi: 10.1016/j.clindermatol.2020.02.005 [DOI] [PubMed] [Google Scholar]
- 6.Ulman CA, Binder SB, Borges NJ. Assessment of medical students’ proficiency in dermatology: are medical students adequately prepared to diagnose and treat common dermatologic conditions in the United States? J Educ Eval Health Prof. 2015;12:18. doi: 10.3352/jeehp.2015.12.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCleskey PE, Gilson RT, DeVillez RL. Medical student core curriculum in dermatology survey. J Am Acad Dermatol. 2009;61(1):30–35.e4. doi: 10.1016/j.jaad.2008.10.066 [DOI] [PubMed] [Google Scholar]
- 8.Oyesanya T, Grossberg AL, Okoye GA. Increasing minority representation in the dermatology department: the Johns Hopkins experience. JAMA Dermatology. 2018;154(10):1133–1134. doi: 10.1001/jamadermatol.2018.2018 [DOI] [PubMed] [Google Scholar]
- 9.Pritchett EN, Pandya AG, Ferguson NN, Hu S, Ortega-Loayza AG, Lim HW. Diversity in dermatology: roadmap for improvement. J Am Acad Dermatol. 2018;79(2):337–341. doi: 10.1016/j.jaad.2018.04.003 [DOI] [PubMed] [Google Scholar]
- 10.Ebede T, Papier A. Disparities in dermatology educational resources. J Am Acad Dermatol. 2006;55(4):687–690. doi: 10.1016/j.jaad.2005.10.068 [DOI] [PubMed] [Google Scholar]
- 11.Hinojosa JA, Pandya AG. Diversity in the dermatology workforce. Semin Cutan Med Surg. 2016;36(4):242–245. doi: 10.12788/j.sder.2016.063 [DOI] [PubMed] [Google Scholar]