Abstract
Background
Hospital staff is at high risk of developing mental health issues during the coronavirus (COVID-19) pandemic. However, the literature lacks an overall and inclusive picture of mental health problems with comprehensive analysis among hospital staff during the COVID-19 pandemic.
Objectives
To ascertain the prevalence of anxiety, depression and other mental health outcomes as reported in original articles among hospital staff during the COVID-19 pandemic.
Design
A PRISMA 2020 and MOOSE 2000 compliant umbrella review of published meta-analyses of observational studies evaluating the prevalence of mental health problems in hospital staff during the pandemic.
Review methods
Systematic searches were conducted in PubMed/Medline, CINAHL, EMBASE, and PsycINFO from December 1st, 2019, until August 13th 2021. The random effects model was used for the meta-analysis, and the I2 index was employed to assess between-study heterogeneity. Publication bias using Egger test and LFK index was examined. Data was analyzed using STATA 17.0 software. AMSTAR-2 was applied for the quality assessment of systematic reviews, while we used GRADE to rate the quality of evidence.
Results
Forty-four meta-analyses from 1298 individual studies were included in the final analysis, encompassing the prevalence of 16 mental health symptoms. One-third of hospital workers reported anxiety (Prevalence: 29.9%, 95% CI:27.1% to 32.7%) and depression (Prevalence: 28.4%, 95% CI:25.5% to 31.3%) symptomatology, while about 40% (95% CI: 36.9% to 42.0%) suffered from sleeping disorders. Fear-related symptoms, reduced well-being, poor quality of life, and acute stress symptoms had the highest prevalence among hospital staff. However, the quality of evidence in these areas varied from low to very low. Nurses suffered more often from sleep problems and symptoms of anxiety and depression than doctors, whereas doctors reported a higher prevalence of acute stress and post-traumatic disorders. The burden of anxiety, depression, and sleep disorders was higher among female employees than their male counterparts. Remarkably, acute stress and insomnia affected more than half of first-line medical staff.
Conclusions
The prevalence of mental health problems among hospital staff during the COVID-19 pandemic is generally high, with anxiety, depression and insomnia symptoms representing the most robust evidence based on a large dataset of prevalence meta-analyses. However, there is no strong confidence in the body of evidence for each outcome assessed.
Registration
Not registered.
Tweetable abstract
The COVID-19 pandemic is having a major impact on the mental health of hospital staff. The need for support must be different for nurses and doctors @eldi12345.
Keywords: COVID-19, Mental health, Systematic review, Meta-analysis, Prevalence, Hospital staff, Doctors, Nurses, Health care
What is already known
-
•
COVID-19 pandemic is still ongoing and new variants constantly identified as well as the patient loads continue to increase.
-
•
Hospital staff is at high risk of developing mental health issues due to the pandemic.
-
•
However, the evidence for this is inconclusive, while existing studies show inconsistencies, publication, and small study biases.
What this paper adds
-
•
This review found that fear-related symptoms, low wellbeing, low quality of life, and acute stress symptoms were highest among hospital staff during the pandemic.
-
•
Nurses had the highest prevalence of sleep problems, depressive, and anxiety symptoms while doctors were those with the highest prevalence of acute stress and post-traumatic stress symptoms.
-
•
Distinct tailored supporting strategies are needed for doctors and nurses based on their symptomatology.
1. Introduction
The outbreak of the COVID-19 pandemic, which first emerged in December 2019, has negatively affected many countries, introduced changes in daily life, and posed challenges and worries across the globe (Haleem et al., 2020; Tušl et al., 2021). Furthermore, new variants of the SARS-CoV-2 coronavirus are raising concerns and fears in all countries, straining healthcare systems and impacting the decision-making of healthcare stakeholders (Moore and Offit, 2021). Data from World Health Organization (WHO) shows that as of October 19 2021, there are 4,903,911 confirmed deaths and 240,940,937 confirmed cases globally (//www.who.int/emergencies/diseases/novel-coronavirus-2019).
As a result, people's physical and mental health is being tested, especially for hospital staff who are close to the patients and burdened with caring for and tackling the COVID-19 disease (Greenberg et al., 2020; Salazar de Pablo et al., 2020). A combination of occupational and non-occupational risk factors such as insecurity, confinement measures, extensive media coverage, fear of contamination and workload under extreme pressure have profound adverse effects on the mental health of hospital staff (Greenberg et al., 2020; Kapetanos et al., 2021; Saeed et al., 2021). Doctors and nurses have been hardest hit as they are at the epicenter of the pandemic and constantly providing healthcare services (Greenberg et al., 2020; Lima et al., 2020).
Indeed, several surveys have shown increased rates of anxiety, depression, stress, and other mental health issues in this high-risk population (Alnazly et al., 2021, Aly et al., 2021, Jahrami et al., 2021a, Jahrami et al., 2021b, Kapetanos et al., 2021, Salari et al., 2020a, Salari et al., 2020b). In addition, growing evidence showed that hospital staff needed frequent and regular screening for such mental health symptoms and consistent support for them (Brooks et al., 2019; Greenberg et al., 2020) in outbreak emergencies (Chong et al., 2004; Lee et al., 2018; Zhao et al., 2021). Likewise, many organizations such as the National Institute for Health and Care Excellence advocate active surveillance of hospital staff to screen those who need assistance and provide timely psychosocial support and care to protect mental wellbeing of employees (Greenberg et al., 2020; Pfefferbaum and North, 2020).
While acknowledging the undisputed impact of COVID-19 on the mental health and wellbeing of healthcare workers, we still do not have a comprehensive portrait emerging from the meta-epidemiological data of the mental health problems that the COVID-19 pandemic is causing. This is partly due to the significant statistics variability and pitfalls in this regard and the lack of solid guidelines for conducting prevalence meta-analyses (Munn et al., 2020). The number of prevalence meta-analyses related to the mental health of hospital staff has increased markedly over the past two years (Bareeqa et al., 2021, Li et al., 2021, Marvaldi et al., 2021, Sahebi et al., 2021, Salari et al., 2020a, Salari et al., 2020b). However, despite this increase in meta-analysis studies, only one meta-epidemiological published study appears in the literature (Sahebi et al., 2021). Moreover, this is limited to the prevalence of depression and anxiety without grading the overall evidence- also known as certainty in evidence or strength of evidence. It is an assessment of the likelihood that the effect is not significantly different from what research has found; i.e. different enough that it could influence a decision (Guyatt et al., 2013).
Given this, the objective of this work was to conduct an umbrella review approach of systematic reviews with meta-analysis (Dragioti et al., 2019; Ioannidis, 2009; Sahebi et al., 2021) that have been published so far and evaluate the prevalence of mental health symptoms in hospital staff during the pandemic. Herein, we aimed to expand the scope of a typical umbrella review further assessing the strength of evidence and the extent of potential bias associated with this field of prevalence meta-analyses. The first aim was to comprehensively ascertain the overall prevalence of mental health problems in this workforce. The second aim was to examine how these prevalence meta-analyses are conducted and provide an overview of the meta-analytical methods employed by the authors for this type of meta-research. The results of this work can potentially provide aggregated data on the current impact of the pandemic on the mental health of hospital staff, primarily focusing on doctors and nurses to guide prevention and treatment policies. Finally, this work can also provide a useful overview of methodological issues and concerns related to this type of review.
2. Methods
This umbrella review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA 2020) reporting guideline (Page et al., 2021) and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines (Stroup et al., 2000) (Supplemental Material Checklists 1 and 2). In addition, the study followed an a priori protocol, available on request.
2.1. Search strategy
To retrieve potentially relevant meta-analyses, we conducted a comprehensive systematic search in PubMed/Medline, CINAHL, EMBASE, and PsycINFO. The search strategy was developed according to the population–exposure–outcome (PEO) criteria and included key and MESH terms related to COVID-19, mental health symptoms, and healthcare workers, adjusted in each database. The full search query for all databases and strings for PubMed are reported in Supplemental Material Box 1. We additionally searched MedRxiv.org for potentially relevant preprints, and hand searched the cited references of the retrieved articles. No language or setting or any other characteristic restrictions were applied. The search was limited to articles published between December 1st 2019, and August 13th 2021. Two authors (ED and DT) independently searched the databases, and in the case of disagreements, a third author (MG) resolved any conflict, reaching a consensus between the two authors.
2.2. Study selection and eligibility criteria
We included systematic reviews with meta-analysis of observational studies (i.e., cross-sectional, case–control, cohort, etc.) that examined the prevalence of mental health symptom among hospital staff during the COVID-19 pandemic. Hospital staff has been defined as anyone working in a hospital, including healthcare students doing a clinical internship.
We included meta-analyses reporting results both in total for hospital staff and separately for doctors, nurses, or other staff (e.g., social workers, administration staff, etc.). We considered the main analysis for all primary and secondary reported mental health outcomes from each eligible meta-analysis. Whenever a prevalence meta-analysis considered mixed populations (e.g., general population and hospital staff) or other coronavirus syndromes (e.g., SARS), it was deemed eligible only if separate results for hospital staff or for novel coronavirus (SARS-CoV-2 and the associated COVID-19) were reported. The same rule was applied when a meta-analysis reported prevalence estimates for physical and mental health outcomes.
We excluded meta-analyses that examined the prevalence of physical health symptoms solely, or meta-analyses of populations other than hospital staff, meta-analyses of intervention studies, systematic reviews of qualitative studies, systematic reviews assessing the association between variables (e.g., anxiety and work-related stigmatization), narrative reviews, scoping reviews, or systematic literature reviews without prevalence meta-analysis. Meta-analyses reporting odds ratio or relative risks as metrics were also excluded, because such metrics assess the association between an exposure and an outcome rather than the distribution of an outcome. While our search had no language restriction; nevertheless only meta-analyses published in English were finally included due to lack of translation resources for other languages.
All articles obtained from the initial literature search were entered into EndNote X9 reference manager. Then, after removing duplicates, two authors (ED and DT) independently searched the titles and abstracts for eligibility. Next, the full texts of potentially relevant articles were carefully read and assessed against the inclusion and exclusion criteria, by the same pair of authors. Any disagreement between the two authors was resolved by a consensus with a third author (MG).
2.3. Data abstraction
For the included meta-analyses, we extracted in pre-defined excel sheet the standard identifier (PMID or DOI), first authors' names, publication year, country, the study design of included primary studies, list of hospital staff evaluated (e.g., doctors, nurses, overall hospital staff, other, if specified), list of mental health outcomes assessed, number of included primary studies per meta-analysis, sample size per meta-analysis, instruments used, period of evidence reviewed, pooled prevalence data of the reported mental health outcome (± 95%CIs), pooled prevalence data from subgroup analysis (if available), and any potential sources of conflict of interest or funding sources. In addition, the definition of mental health symptoms was extracted as reported in the original meta-analyses and included anxiety symptoms, burnout, combined psychological symptoms, depressive symptoms, deleterious mental health, fear-related symptoms, insomnia or sleep disturbances, low overall well-being, low quality of life, obsessive–compulsive symptoms, phobia, post-traumatic stress, psychological distress, somatization, stress, and suicidal thoughts/ideation.
We also recorded information regarding the methods applied per meta-analyses e.g.; databases searched (number and description), protocol (registered or published), reporting guidelines used, models of meta-analysis performed and transformations, heterogeneity, and publication bias.
We used the AMSTAR (A Measurement Tool to Assess Systematic Reviews) version 2 (Shea et al., 2017) to assess the methodological quality of included meta-analyses. Independent couples of two authors (ED, DT, MM, MG) independently performed data extraction and the methodological assessment. Any disagreement throughout the processes was solved by discussion in the research team.
2.4. Data synthesis
For the first aim of our umbrella review, we pooled the individual overall prevalence in the included meta-analyses for each mental health outcome. Thus, we performed a second-order meta-analysis to reanalyze the extracted individual meta-analyses estimates (Dragioti et al., 2019; Sahebi et al., 2021). The random-effects inverse-variance model (DerSimonian and Laird, 1986) was used for meta-analysis due to expected high heterogeneity between results (Higgins et al., 2003). Heterogeneity was calculated as the I2 for each analysis, with an I2 of > 50% indicating large to very large heterogeneity (Higgins et al., 2003). Publication bias was assessed using the Eggers test (p-value < 0.10) (Egger et al., 1997), only when any outcome was reported in 10 or more included meta-analyses (Simmonds, 2015). Since Eggers tests and funnel plots might be improper in prevalence meta-analyses (Hunter et al., 2014), we additionally computed the LFK indexes and Doi plots, to detect and quantify asymmetry of study effects (Furuya-Kanamori et al., 2018).
We performed a leave-one-out sensitivity analysis to determine the influence of each meta-analysis on the overall effect and to identify influential studies. In the leave-one-out meta-analysis, multiple meta-analyses are performed by excluding one study from each analysis. It is common for studies to produce exaggerated effect sizes, which can skew the overall results. In addition, subgroup analyses were conducted whenever feasible (more on three studies) based on profession type, i.e., doctors vs nurses vs other hospital staff, males vs females, and front-line (defined as personnel who have worked during the COVID-19 pandemic to care for patients potentially infected with SARS-COV-2, but is not necessarily limited to those working in frontline units such as emergency departments COVID-19 units, or intensive care units) vs second-line hospital staff (defined as those not working in frontline units or directly exposed to COVID-19).
Data analysis was performed in STATA/SE, version 17.0 (StataCorp LLC). We also used a modified approach of the GRADE framework (Atkins et al., 2004) to rate the overall quality of the evidence on the prevalence estimates per mental health symptom as high, moderate, low or very low quality evidence based on study limitations (overall quality of the evidence identified based on AMSTAR 2), imprecision (meta-analyses sample sizes), indirectness (generalizability of included studies) and inconsistency (existence of heterogeneity and publication bias). Details are presented in Supplemental Material Box 2.
For the second aim, we used descriptive statistics to present the results. We reported means and standard deviations (SDs) or median and interquartile range (IQR), as appropriate for quantitative variables and absolute and/or relative frequencies (n, %) for the qualitative studies.
3. Results
3.1. Search results
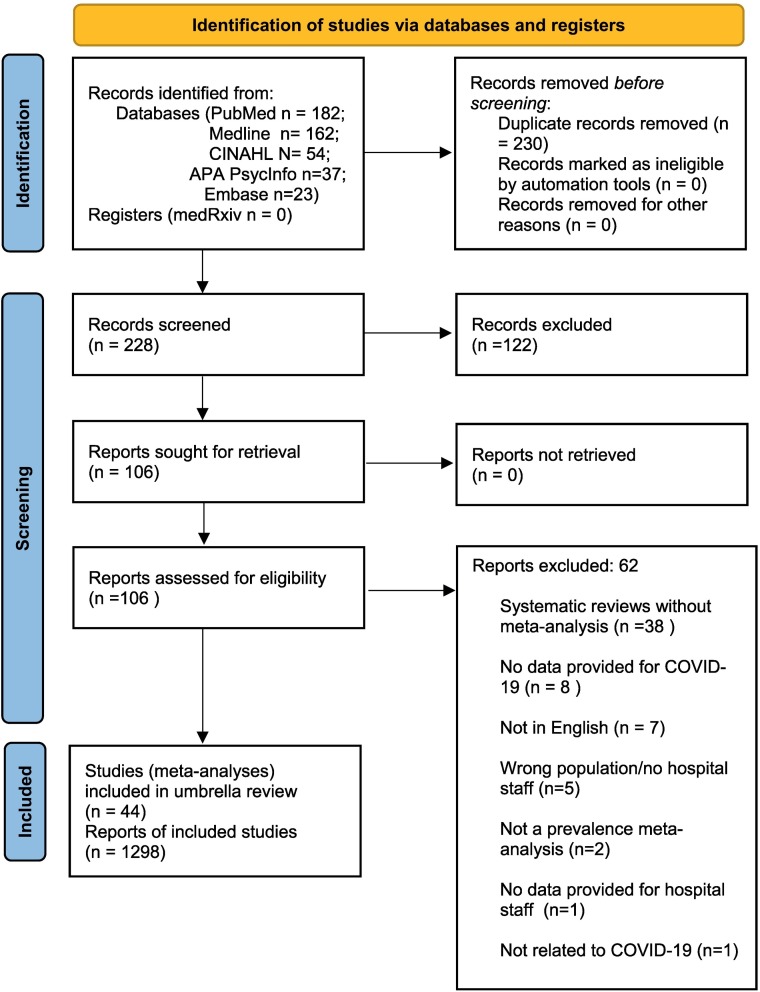
The literature search detected a total of 458 articles (228 after removal of duplicates) and after having scrutinized 106 out of 228 articles for depth eligibility, we finally included 44 articles (meta-analyses) in this umbrella review (Adibi et al., 2021, Al Maqbali et al., 2021, Alimoradi et al., 2021a, Alimoradi et al., 2021b, Arora et al., 2020, Bareeqa et al., 2021, Batra et al., 2020, Cenat et al., 2021, da Silva and Neto, 2021, Deng et al., 2021, Dong et al., 2021, Dubé et al., 2021, Dutta et al., 2021, El-Qushayri et al., 2021, Galanis et al., 2021, Hao et al., 2021, Jahrami et al., 2021a, Jahrami et al., 2021b, Krishnamoorthy et al., 2020, Li et al., 2021, Luo et al., 2020, Mahmud et al., 2021, Marvaldi et al., 2021, Nowrouzi-Kia et al., 2021, Olaya et al., 2021, Pappa et al., 2020, Phiri et al., 2021, Raoofi et al., 2021, Ren et al., 2020, Salari et al., 2020a, Salari et al., 2020b, Salazar de Pablo et al., 2020, Salehi et al., 2021, Santabárbara et al., 2021, Saragih et al., 2021, Serrano-Ripoll et al., 2021, Singh et al., 2021, Sun et al., 2021, Troglio da Silva and Neto, 2021, Varghese et al., 2021, Wu et al., 2021, Xia et al., 2021, Yan et al., 2021, Zhang et al., 2021, Zhao et al., 2021). Fig. 1 shows the study selection process and depicts the reasons for article exclusion. Details of the reasons for exclusion are annotated in Supplemental Material Table 1 and their references (see references of excluded articles in the Supplemental Material).
Fig. 1.
Meta-analyses selection process.
3.2. Characteristics of included meta-analyses
The selected meta-analyses were published between 2020 and 2021 and reviewed individual studies published between November 2019 and February 2021 (Supplemental Material Table 2). Twelve meta-analyses (27%) were conducted in China, five (11%) in multiple countries and three (7%) in three countries, namely India, Canada, and Iran. Country of origin details for all 44 meta-analyses is presented in Supplemental Material Table 2. The 44 meta-analyses included a total of 1298 individual studies with a median of 23.5 studies (interquartile range [IQR] = 12.5–36.5). The total number of participants (hospital staff) was 1,491,439 with a median number of 21,866 (IQR = 10,267- 58,565). All individual studies included in the eligible meta-analyses had employed an observational study design (mainly cross-sectional). Most of them had used self-reporting validated questionnaires (Supplemental Material Table 2).
3.3. Methodological quality of included meta-analyses
The results of meta-analyses' quality assessment are presented in Supplemental Material Table 3. Half of the meta-analyses (50%) had moderate quality, 43% had low quality, and only three (7%) had critically low quality based on AMSTAR2.
3.4. Global prevalence of anxiety and depressive symptoms
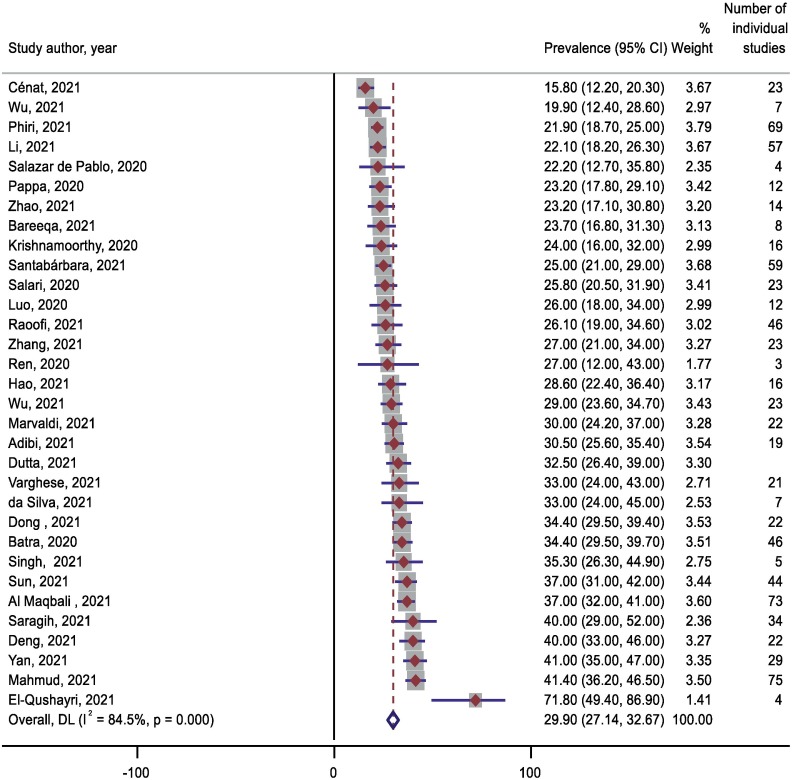
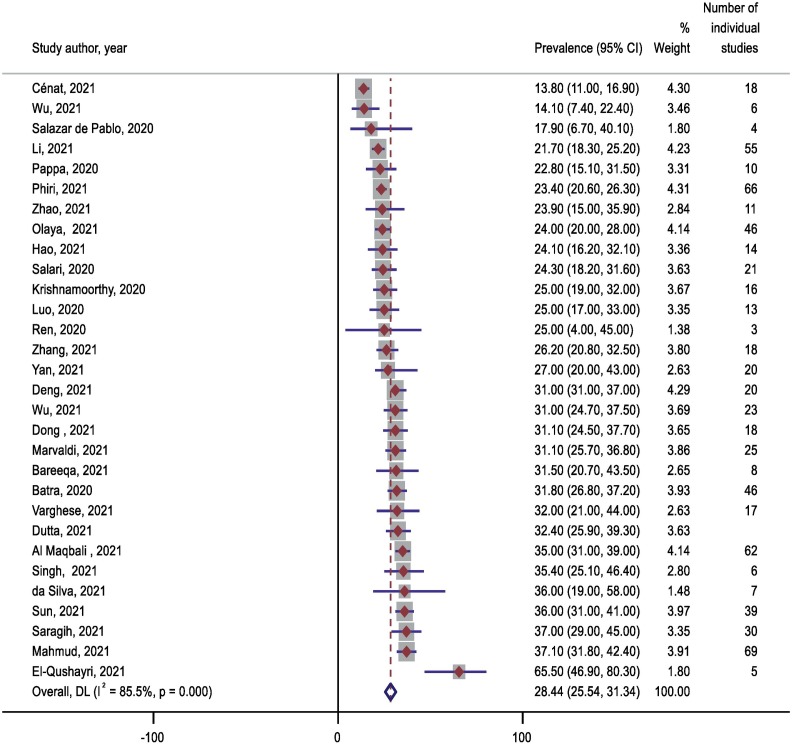
A total of 32 and 30 meta-analyses, including 838 and 696 individual primary studies, respectively, examined the prevalence of anxiety and depressive symptoms among hospital staff during the COVID-19 pandemic. The overall prevalence of anxiety symptoms (Table 1 ; Fig. 2 ) was 29.90% (95% CI: 27.14–32.67, I2 = 84.5%, P = 0.000) and the overall prevalence of depressive symptoms (Table 1; Fig. 3 ) was 28.44% (95% CI:25.54–31.34, I2 = 85.8%, P = 0.000). The lowest prevalence of anxiety was 15.9% and the highest 71.9%, while the lowest prevalence for depressive symptoms was 12.8% and the highest 65.5%. Leave-one-out sensitivity analyses showed that removal of meta-analyses had a moderate influential effect on the pooled anxiety and the depression prevalence and the range of prevalence estimates changed after excluding three meta-analyses with the largest influence (Cénat et al., 2021; El-Qushayri et al., 2021; Wu et al., 2021) (Supplementary Material Figs. 1, 2). Minor asymmetry was observed by the LKF index and Doi plot analysis indicating that the results were not significantly affected by publication bias (Supplementary Material Figs. 3, 4).
Table 1.
Prevalence of mental health outcomes in all hospital staff during the COVID-19 epidemic from included meta-analyses.
| Outcome | No. of meta-analyses (No. of individual studies included in meta-analyses) | Individual meta-analyses, prevalence range | Prevalence (%; 95% CI%) | P-values | Events/ Total sample size |
I2 (%) | Publication bias (Egger's p) | LFK index | GRADE |
|---|---|---|---|---|---|---|---|---|---|
| Anxiety symptoms | 32 (838) | 15.9% to 71.9% | 29.90 (27.14–32.67) | 0.000 | > 83,439/ 691,378 |
84.5 | No (0.59) | 1.39 (Minor Asymmetry) | Moderate |
| Burnout | 5 (22) | 12.6% to 37.4% | 23.32 (12.41–34.23) | 0.000 | > 7685/ 48,701 |
68.1 | NA | 4.39 (Major Asymmetry) | Low |
| Combined psychological symptoms | 2 (33) | 34.0% to 39.3% | 34.91 (25.82–44.01) | 0.000 | NA/NA | 0.0 | NA | NA | Very low |
| Deleterious mental health | 3 (9) | 11.6% to 46.1% | 43.69 (7.83–79.56) | 0.05 | > 402/3327 | 99.5 | NA | NA | Very low |
| Depressive symptoms | 30 (696) | 12.8% to 65.5% | 28.44 (25.54–31.34) | 0.000 | > 93,970/ 503,418 |
85.8 | No (0.14) | 1.76 (Minor Asymmetry) | Moderate |
| Fear-Related Symptoms | 1 (6) | NA | 67.00 (61.00–73.00) | NA | 2403/ NA |
NA | NA | NA | Very low |
| Insomnia or sleep disturbances | 26 (261) | 23.1% to 64.3% | 39.45 (36.91–42.00) | 0.000 | 21,144/ 225,874 |
75.9 | No (0.25) | 1.30 (Minor Asymmetry) | Moderate |
| Low QoL | 1 (1) | NA | 45.20 (38.10–52.40) | NA | NA/ NA |
NA | NA | NA | Very low |
| Low overall wellbeing | 1 (3) | 42.6% to 58.9% | 52.60 (43.80–61.40) | NA | NA/ NA |
NA | NA | NA | Very low |
| Obsessive–compulsive symptoms | 1 (4) | 5.3% to 33.6% | 16.20 (3.00–29.50) | NA | 98/ 1126 |
NA | NA | NA | Very low |
| Phobia | 1 (4) | 3.6% to 64.6% | 35.00 (8.60–61.40) | NA | 111/ 1126 |
NA | NA | NA | Very low |
| Post-traumatic stress | 13 (77) | 7.7% to 49.0% | 18.75 (13.92–23.57) | 0.000 | 8459/ 61,148 |
79.1 | Yes (0.00) | 5.61 (Major Asymmetry) | Low |
| Psychological distress | 9 (56) | 16.9% to 57.5% | 34.59 (23.04–46.14) | 0.000 | 11,193/ 75,676 |
85 | NA | 4.55 (Major Asymmetry) | Low |
| Somatization | 1 (4) | 1.6% to 22.0% | 10.70 (1.90–19.60) | NA | 43/ 1126 |
NA | NA | NA | Very low |
| Stress | 13 (158) | 29.1% to 66.6% | 44.30 (37.92–50.69) | 0.000 | 1432/ 127,960 |
73.8 | Yes (0.03) | 2.73(Major Asymmetry) | Low |
| Suicidal thoughts/ideation | 2 (13) | 5.8% to 6.9% | 6.17 (5.15–7.19) | 0.000 | 1233/ 17,692 |
15.4 | NA | NA | Very low |
NA = not available or applicable, CI = confidence interval, I2 = heterogeneity, LFK = Luis Furuya-Kanamori asymmetry index, QoL = quality of life.
Fig. 2.
The forest plot of overall and individual prevalence of anxiety in the included meta-analyses.
Fig. 3.
The forest plot of overall and individual prevalence of depression in the included meta-analyses.
3.5. Global prevalence of insomnia or sleep problems
Twenty-six meta-analyses, including 261 individual primary studies, examined the prevalence of insomnia and sleep problems among hospital staff during the COVID-19 pandemic. The overall prevalence of insomnia or sleep problems (Table 1; Supplementary Fig. 5) was 39.45% (95% CI: 36.91–42.00, I2 = 75.9%, P = 0.00). The lowest prevalence of insomnia or sleep problems was 23.1%, and the highest was 64.3%. Leave-one-out sensitivity analyses showed that removing meta-analyses had a moderate influential effect on the prevalence of pooled insomnia or sleep problems prevalence and the range of prevalence estimates changed after excluding seven meta-analyses with the largest influence (Batra et al., 2020; El-Qushayri et al., 2021; Phiri et al., 2021; Salazar de Pablo et al., 2020; Wu et al., 2021; Xia et al., 2021) (Supplementary Material Fig. 6). Minor asymmetry was observed by the LKF index and Doi plot analysis indicating that the results were not significantly affected by publication bias (Supplementary Material Fig. 7).
3.6. Global prevalence of psychological distress and stress
A total of 9 and 13 meta-analyses, including 56 and 158 individual primary studies, respectively, examined the prevalence of psychological distress and stress among hospital staff during the COVID-19 pandemic. The overall prevalence of psychological distress (Table 1; Supplementary Material Fig. 8) was 34.59% (95% CI: 23.04–46.14, I2 = 85.0%, P = 0.000) and the overall prevalence of stress (Table 1; Supplementary Material Fig. 9) was 44.30% (95% CI:37.92–50.69, I2 = 73.8%, P = 0.000). The lowest prevalence of psychological distress was 16.9%, and the highest was 57.5%, while the lowest prevalence for stress was 29.1% and the highest 66.6%. Leave-one-out sensitivity analyses showed that removal of meta-analyses had a moderate influential effect on the pooled psychological distress and stress prevalence and the range of prevalence estimates changed after excluding four meta-analyses with the largest influence (Batra et al., 2020; El-Qushayri et al., 2021; Marvaldi et al., 2021; Singh et al., 2021) (Supplementary Material Figs. 10, 11). Major asymmetry was observed by the LKF index and Doi plot analysis indicating that the results were significantly affected by publication bias (Supplementary Material Figs. 12, 13).
3.7. Global prevalence of other psychological symptoms
Table 1 shows the prevalence estimates of other psychological indicators among hospital staff during the COVID-19 pandemic. The lowest prevalence was found for suicidal thoughts/ideation (6.17%, 95% CI: 5.15–7.19, I2 = 15.4%, P = 0.000) and the highest for fear-related symptoms (67.00%, 95% CI: 61.00–73.00). The overall prevalence of post-traumatic stress (Table 1; Supplementary Material Fig. 14) was 18.75% (95% CI: 13.92–23.57, I2 = 79.1%, P = 0.000). Leave-one-out sensitivity analyses showed that removal of meta-analyses had a moderate influential effect on the pooled post-traumatic stress prevalence and the range of prevalence estimates changed after excluding three meta-analyses with the largest influence (Marvaldi et al., 2021; Saragih et al., 2021; Yan et al., 2021) (Supplementary Material Fig. 15). Major asymmetry was observed for post-traumatic stress and burnout by the LKF index and Doi plot analysis indicating that the results were significantly affected by publication bias (Supplementary Material Figs. 16, 17).
3.8. Subgroup analysis
Based on profession type analysis, the prevalence rates of anxiety (31.93%, 95% CI: 27.44–36.4), depressive symptoms (32.59%, 95% CI: 28.81–36.6), and insomnia or sleep disturbances (39.06%, 95% CI: 35.04–43.08), among nurses were higher than doctors and other hospital staff. Furthermore, the prevalence rates of stress (64.75%, 95% CI: 26.71–100.00) and post-traumatic stress symptoms (39.0%, 95% CI: 18.00–62.00) among doctors were higher than nurses (Table 2 ).
Table 2.
Comparison of prevalence of mental health outcomes in hospital staff during the COVID-19 epidemic by subpopulations.
| Outcome | Subgroup | No. of meta-analyses (No. of individual studies included in meta-analyses) | Individual meta-analyses prevalence range | Prevalence (%; 95% CI%) | I2 (%) | Q (p-value) |
|---|---|---|---|---|---|---|
| Anxiety symptoms | Doctors | 8 (90) | 17.0% to 41.0% | 26.69 (19.76–33.62) | 82.5 | 4.97 (0.08) |
| Nurses | 10 (145) | 22.8% to 44.1% | 31.93 (27.44–36.42) | 70.6 | ||
| Other hospital staff | 3 (24) | 19.9% to 39.80% | 24.16 (18.76–29.57) | 0.0 | ||
| Depressive symptoms | Doctors | 7 (72) | 24.0% to 40.4% | 30.87 (24.86–36.87) | 78.7 | 18.00 (0.00) |
| Nurses | 9 (124) | 25.0% to 42.4% | 32.59 (28.81–36.6) | 29.1 | ||
| Other hospital staff | 2 (21) | 14.1% to 20.6% | 16.89 (10.58–23.20) | 75.3 | ||
| Insomnia or sleep disturbances | Doctors | 4 (24) | 34.5% to 41.6% | 37.23 (32.61–41.86) | 0.0 | 5.57 (0.06) |
| Nurses | 6 (45) | 34.8% to 43.0% | 39.06 (35.04–43.08) | 0.0 | ||
| Other hospital staff | 1 (2) | NA | 31.80 (27.15–36.45) | NA | ||
| Stress | Doctors | 3 (13) | 42.0% to 93.0% | 64.75 (26.71–100.00) | 95.5 | 1.73 (0.42) |
| Nurses | 4 (71) | 40.6% to 51.0% | 45.48 (41.01–49.94) | 0.0 | ||
| Other hospital staff | 1 (8) | NA | 36.40 (15.80–57.00) | NA | ||
| Post-traumatic stress | Doctors | 1 (2) | NA | 39.0 (18.00–62.00) | NA | |
| Nurses | 1 (3) | NA | 18.60 (4.80–38.30) | NA | ||
| Anxiety symptoms | Male HS | 5 (27) | 14.3% to 44.2% | 31.28 (19.86–42.71) | 79.7 | 0.98 (0.32) |
| Female HS | 5 (27) | 26.6% to 50.0% | 38.70 (29.45–47.95) | 64.9 | ||
| Depressive symptoms | Male HS | 5 (28) | 20.3% to 40.9% | 30.25 (20.54–39.96) | 55.8 | 1.22 (0.27) |
| Female HS | 5 (28) | 26.9% to 43.4% | 36.92 (30.10–43.75) | 21.8 | ||
| Insomnia or sleep disturbances | Male HS | 2 (8) | 24.0% to 28.6% | 25.98 (21.52–30.45) | 64.0 | 2.34 (0.13) |
| Female HS | 2 (8) | 29.0% to 36.70% | 32.82 (25.28–40.37) | 97.3 | ||
| Anxiety symptoms | Front-line HS | 11 (101) | 19.8% to 45.0% | 33.31 (28.47–38.15) | 61.7 | 1.65 (0.20) |
| Second-line HS | 5 (25) | 24.7% to 37.0% | 28.77 (23.82–33.72) | 0.0 | ||
| Depressive symptoms | Front-line HS | 11 (87) | 23.6% to 53.0% | 31.85 (26.95–36.75) | 61.8 | 0.01 (0.93) |
| Second-line HS | 5 (26) | 19.6% to 46.0% | 31.41 (23.53–39.29) | 64.9 | ||
| Insomnia or sleep disturbances | Front-line HS | 2 (16) | 47.0% to 57.4% | 50.56 (39.97–61.14) | 0.0 | 1.95 (0.16) |
| Second-line HS | 1 (4) | NA | 40.00 (29.65–50.35) | NA | ||
| Stress | Front-line HS | 2 (18) | 46.0% to 93.7% | 69.68 (23.23–100) | 99.2 | – |
| Second-line HS | – | – | – | – |
NA = not available, CI = confidence interval, I2 = heterogeneity, HS = Hospital staff, Q = Cochran's Q test of group differences.
Based on sex analysis, the prevalence rates of anxiety (38.70%, 95% CI: 29.45–47.95), depressive symptoms (36.92%, 95% CI:30.10–43.75), and insomnia or sleep disturbances (32.82%, 95% CI: 25.28–40.37), among female hospital staff were higher than male hospital staff. In addition, frontline hospital staff also displayed higher prevalence rates of anxiety (33.31%, 95% CI: 28.47–38.15) and insomnia or sleep disturbances (50.56%, 95% CI: 39.97–61.14) than second-line hospital staff (Table 2).
3.9. Quality of the evidence – GRADE
We rated the overall quality of the evidence to be moderate for anxiety, depression and insomnia or sleep problems prevalence and low and or very low for the other mental health symptoms, indicating that further research could alter our results (Table 1).
3.10. Methodological considerations
Twenty-seven out of 44 meta-analyses (61.4%) published or registered a protocol (mainly in PROSPERO database and only one published a protocol in a scientific journal), and 39 (86.3%) used a reporting guideline, including PRISMA (n = 38, 86.4%) and MOOSE (n = 1, 2.3%). Seven meta-analyses used both PRISMA and MOOSE, while three used the Cochrane Handbook for Systematic Reviews of Interventions alongside PRISMA. In 41 meta-analyses (93.2%), the authors described their funding sources and only in three meta-analyses (6.8%), no funding was reported.
The median number of databases searched per meta-analysis was 5.5 (IQR 4–7). The most common database in all meta-analyses (100%) was PubMed. However, two meta-analyses (4.5%) used only one database (i.e., PubMed), and six (13.6%) used the Cochrane Library as an additional source of searching, even though this database was limited to interventional studies. Nine of them (20.4%) were restricted to only Chinese studies. Thirty meta-analyses (n = 30, 68.2%) reported the full search strategy and used at least one database. However, 11 meta-analyses (25.0%) partly reported the search strategy (presented only the terms or keywords used, but not how it was designed per database), and three meta-analyses (6.8%) did not report any search strategy.
In all meta-analyses, the most common instruments were: Generalized Anxiety Disorder Assessment, Zung's Self-Rating Anxiety Scale, COVD-19 Anxiety Scale, The State–Trait Anxiety Inventory, Hospital Anxiety and Depression Scale, Stanford Acute Stress Reaction Questionnaire, Global stress Index, Self-reported Stressor and Incidence Questionnaire, Perceived Stress Scale, Hamilton Depression Rating Scale, Zung's Self-Rating Depression Scale, Patient Health Questionnaire, Depression Anxiety Stress Scale, Impact of Event Scale, PTSD Checklist-Civilian version, Insomnia Severity Index, and Pittsburgh Sleep Quality Index. However, no meta-analysis or individual study has used any formal diagnostic criteria (e.g., ICD-10 or DSM).
All but three meta-analyses (n = 41, 93.2%) assessed the methodological quality of included studies, but only nine (20.5%) used it as an inclusion criterion. Moreover, only 21 meta-analyses (47.7%) reported that at least two independent reviewers assessed the methodological quality of included studies. The checklists used for assessing the methodological quality of included studies also varied. The most common checklists were NOS (n = 10, 22.7%), STOBE (n = 7, 15.9%), the JBI Appraisal Checklist for Prevalence Studies appraisal tool (n = 5, 11.3%), and the Agency for Healthcare Research and Quality (AHRQ; n = 5, 11.3%). No prevalence meta-analysis assesses whether the quality of the reported evidence was high, moderate, low, or very low, using appropriate guidelines such as the GRADE approach (Guyatt et al., 2008).
All meta-analyses (n = 44, 100%) employed a random-effects model (REM). However, only 13 (29.5%) reported the variance estimator used (i.e., DerSimonian-Laird method), and 14 (31.8%) reported the model of transformation used (i.e., Double arcsine or logit). I2 was the most common index for assessing heterogeneity. Subgroup or sensitivity analysis was performed in 33 meta-analyses (75.0%) and meta-regression in half of them (n = 22; 50.0%).
4. Discussion
This comprehensive umbrella review detected 44 meta-analyses that evaluated the prevalence of mental health symptoms in hospital staff during the COVID-19 pandemic. The most commonly studied symptoms across all meta-analyses were anxiety, depression, insomnia or sleep problems, acute stress, and post-traumatic stress. Notably, other mental health symptoms including, burnout, ill-being, somatization of stress, and suicidal thoughts/ideation are neglected from the literature. Among hospital staff, doctors and nurses were also the most studied population. There is moderate evidence that approximately 30% of hospital staff suffered from symptoms of anxiety and depression, while about 40% of the staff suffered from insomnia or sleep problems. Our work, furthermore, indicated that hospital staff experienced an array of mental health symptoms with fear-related symptoms, acute stress, reduced wellbeing and poor quality of life, being the most affected areas. However, the quality of the evidence in these areas ranged from low to very low due to the small number of included primary studies and the consequent presence of publication bias. Overall, the results of the present study confirm that the COVID-19 pandemic has had a profound negative effect on the mental health of hospital staff (Olaya et al., 2021; Pappa et al., 2020; Raoofi et al., 2021). Moreover, the results underscore the need to regularly assess the mental health of hospital staff and apply tailored prevention and supporting strategies to this population (Greenberg et al., 2020; Pappa et al., 2020; Pfefferbaum and North, 2020).
In our study, the prevalence of anxiety and depression was 29.9% and 28.4%, respectively. A similar pattern of results was obtained in Sahebi et al.'s work (Sahebi et al., 2021). Their umbrella review, including seven meta-analyses, found a prevalence of anxiety and depression of 24.94% and 24.83%, respectively. Insomnia or sleep problems and stress were also high in hospital staff (40% and 44%). Concerning post-traumatic stress disorder, our results suggest that the prevalence among hospital staff was 19%. However, these figures are much lower than those reported in previous meta-analyses. For example, El-Qushayri et al., including ten studies (El-Qushayri et al., 2021), found a prevalence of anxiety of 72%, followed by stress (66%), depression (65%), and insomnia (58%). Another systematic review, including 38 studies, found that post-traumatic stress disorder had the highest prevalence (49%) among health care providers during the COVID-19 pandemic (Saragih et al., 2021). These discrepancies can be partly explained by the fact that meta-analysis of proportions heavily depended on the number of events, the total population, and the number of included studies (Nyaga et al., 2014). Adding to this, a recent meta-analysis found that with increasing the sample size the prevalence of depression and anxiety decreased (Salari et al., 2020a, Salari et al., 2020b).
Another explanation is that most of the studies included in previous systematic reviews were performed during the first six months of the outbreak of the COVID-19 pandemic, where much worry and uncertainty existed, and people tried to adjust themselves to live with this emergency (Novelli et al., 2020). Unfortunately, there are no official data before the pandemic or repeated measurements over time to have a robust estimation, and therefore our results were influenced by this event. Comparisons between hospital staff and the general population have reported conflicting results (Huang and Zhao, 2020, Jahrami et al., 2021a, Jahrami et al., 2021b, Luo et al., 2020, Singh et al., 2021, Zhang et al., 2020). Another systematic review also suggested that the global severity of mental health problems among health professionals increased over time (Mahmud et al., 2021). Nevertheless, since a worldwide pooled lifetime prevalence of mental health problems in hospital staff is lacking, we cannot confirm or reject this hypothesis.
Planned comparisons between professions revealed that the pandemic affected doctors and nurses differently. This was not the case for comparisons between female and male staff as well as front-line and second-line hospital staff. Specifically, we found that the prevalence of insomnia or sleep problems, anxiety and depressive symptoms was higher among nurses than among doctors. On the other hand, doctors had a higher prevalence of stress and post-traumatic stress than nurses, but they did not reach statistical significance. These findings partly contrast with abundant literature showing that nurses were more vulnerable to stress (Luo et al., 2020) but are in line with the notion that nurses would suffer from poor mental health outcomes with numerous factors influencing them (Galanis et al., 2021; Varghese et al., 2021). We speculate that this might be due to the different responsibilities, health care tasks, and working hours between the two professions.
Our study failed to confirm that female hospital staff had a statistically significant higher prevalence of anxiety, depression, and sleep problems. Other studies have shown that the female sex is a risk factor for developing severe depression and anxiety among hospital staff (Qiu et al., 2020; Shahid et al., 2020; Varghese et al., 2021). Female participants from the general population are also more likely to report higher levels of anxiety and depression than their male counterparts before (Cavanagh et al., 2017) and after the COVID-19 pandemic (Qiu et al., 2020). The prevalence of insomnia or sleep problems (50.5%) and acute stress (64.8%) was higher in front-line hospital staff regardless of profession, but without statistical significance. These findings also contradict some previous work (Cai et al., 2020, Meo et al., 2021, Salari et al., 2020a, Salari et al., 2020b) but align with others (Liang et al., 2020). The most probable reason for these discrepancies is the lack of a control group. For example, some meta-analyses have included solely front-line staff (Salari et al., 2020a, Salari et al., 2020b). This may be the reason why we did not find significant differences. However, it is important to note that the evidence was lacking for other professions or other combinations of comparisons in terms of severity of symptoms and detailed gender differences such as female nurses vs female doctors or front-line nurses vs frontline doctors etc. Future studies should examine in depth the mental health burden among hospital staff professions.
Intriguingly, our umbrella review found substantial discrepancies in conducting, reporting, risk of bias assessment, and data synthesis in this body of research. Although most meta-analyses followed the PRISMA guidelines, there is an ongoing discussion if this guideline is appropriate for reporting prevalence meta-analysis (Borges Migliavaca et al., 2020). Another major controversial area is the risk of bias assessment of the included studies and the diverse checklists and tools used to assess their bias. However, it was encouraging that only a very low number of publications did not appraise the included studies quality. Another important finding is that solid meta-analytical synthesizing methods are lacking, and the large heterogeneity cannot be accurately explained. The different measurement scales used to collect mental health outcomes may account for the significant heterogeneity observed (Alba et al., 2016).
Furthermore, we identified various reasons for the low overall evidence in this regard, namely; a) most of meta-analyses included moderate or low-quality studies (mainly cross-sectional designs), b) most of the included studies were conducted in a specific context, China, c) there was considerable inconsistency in the prevalence estimates, with high heterogeneity and publication bias, and d) there was a lack of prevalence estimates for the most of mental health outcomes with few exceptions. These methodological considerations highlighted the importance of improving the design and execution of prevalence meta-analyses and developing and validating a reporting tool.
4.1. Limitations
This is the first umbrella review examining the largest dataset of prevalence meta-analyses of the effects of COVID-19 on hospital staff's mental health currently available. Our large sample size, the solid methodology, and the grading of evidence are additional strengths. Our study also sheds light on the methodological discrepancies in this body of research. A major source of limitation is the exclusion of non-English articles, the low quality of included studies in meta-analyses and the cross-sectional study design with self-reported measurements, and convenience sampling. However, we pinpointed the overall available evidence showing the drawbacks observed here and suggesting that it is crucial to rely on well conducted primary and secondary studies, but this is not always the case. As we mentioned, the evidence is lacking for many outcomes, professions, and direct comparisons. This prevented us from examining for heterogeneity sources, although this is out of the scope of an umbrella review. Our study also failed to identify reasons that might affect the manifestation of these mental health symptoms as most of the studies did not examine the underlying causes. Finally, we cannot find a trend of symptoms over time or show whether these mental health symptoms are similar or different before the pandemic.
5. Conclusions
On this basis, we conclude that the impact of the COVID-19 pandemic on the mental health of hospital staff is generally high. Nurses are affected most by symptoms related to anxiety, depression, and sleep problems, while doctors are affected most by symptoms related to stress and post-traumatic stress disorder. These findings confer great opportunities for stratifying the mental health needs by profession to detect high-risk professions and provide timely and effective treatment approaches based on their symptomatology. An increasing number of meta-analyses are currently performed to investigate the prevalence and the factors potentially associated with the mental health impact in hospital staff. Our study findings also confer great opportunities for the development of meta-analytical methods of prevalence data.
Ethical approval
Not applicable. This is a meta-research work from published literature and formal consent is not required.
Data availability statement
All data generated or analyzed during this study are fully available in published cited literature and included in this article and its supplementary information files.
Funding
This work has not received any funding.
CRediT authorship contribution statement
Elena Dragioti: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing –review & editing. Dimitrios Tsartsalis: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing –review & editing. Manolis Mentis: Data curation, Writing –review & editing. Stefanos Mantzoukas: Data curation, Writing –review & editing. Mary Gouva: Data curation, Writing –review & editing. All authors approved the final version of the study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnurstu.2022.104272.
Appendix A. Supplementary data
Supplementary material
References
- Adibi A., Golitaleb M., Farrahi-Ashtiani I., Pirani D., Yousefi K., Jamshidbeigi Y., Sahebi A. The prevalence of generalized anxiety disorder among health care workers during the COVID-19 pandemic: a systematic review and Meta-analysis. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.658846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Maqbali M., Al Sinani M., Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J. Psychosom. Res. 2021;141 doi: 10.1016/j.jpsychores.2020.110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alba A.C., Alexander P.E., Chang J., MacIsaac J., DeFry S., Guyatt G.H. High statistical heterogeneity is more frequent in meta-analysis of continuous than binary outcomes. J. Clin. Epidemiol. 2016;70:129–135. doi: 10.1016/j.jclinepi.2015.09.005. [DOI] [PubMed] [Google Scholar]
- Alimoradi Z., Broström A., Tsang H.W.H., Griffiths M.D., Haghayegh S., Ohayon M.M., Lin C.Y., Pakpour A.H. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: a systematic review and meta-analysis. EClinicalMedicine. 2021;36 doi: 10.1016/j.eclinm.2021.100916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimoradi Z., Gozal D., Tsang H.W.H., Lin C.Y., Broström A., Ohayon M.M., Pakpour A.H. Gender-specific estimates of sleep problems during the COVID-19 pandemic: systematic review and meta-analysis. J. Sleep Res. 2021;e13432 doi: 10.1111/jsr.13432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alnazly E., Khraisat O.M., Al-Bashaireh A.M., Bryant C.L. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0247679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aly H.M., Nemr N.A., Kishk R.M., Elsaid N. Stress, anxiety and depression among healthcare workers facing COVID-19 pandemic in Egypt: a cross-sectional online-based study. BMJ Open. 2021;11(4) doi: 10.1136/bmjopen-2020-045281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora T., Grey I., Östlundh L., Lam K.B.H., Omar O.M., Arnone D. The prevalence of psychological consequences of COVID-19: a systematic review and meta-analysis of observational studies. J. Health Psychol. 2020;1359105320966639 doi: 10.1177/1359105320966639. [DOI] [PubMed] [Google Scholar]
- Atkins D., Best D., Briss P.A., Eccles M., Falck-Ytter Y., Flottorp S., Guyatt G.H., Harbour R.T., Haugh M.C., Henry D., Hill S., Jaeschke R., Leng G., Liberati A., Magrini N., Mason J., Middleton P., Mrukowicz J., O'Connell D., Oxman A.D., Phillips B., Schünemann H.J., Edejer T., Varonen H., Vist G.E., Williams J.W., Jr., Zaza S. Grading quality of evidence and strength of recommendations. Bmj. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bareeqa S.B., Ahmed S.I., Samar S.S., Yasin W., Zehra S., Monese G.M., Gouthro R.V. Prevalence of depression, anxiety and stress in China during COVID-19 pandemic: a systematic review with meta-analysis. Int. J. Psychiatry Med. 2021;56(4):210–227. doi: 10.1177/0091217420978005. [DOI] [PubMed] [Google Scholar]
- Batra K., Singh T.P., Sharma M., Batra R., Schvaneveldt N. Investigating the psychological impact of COVID-19 among healthcare workers: a Meta-analysis. Int. J. Environ. Res. Public Health. 2020;17(23) doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges Migliavaca C., Stein C., Colpani V., Barker T.H., Munn Z., Falavigna M., on behalf of the Prevalence Estimates Reviews – Systematic Review Methodology, G How are systematic reviews of prevalence conducted? A methodological study. BMC Med. Res. Methodol. 2020;20(1):96. doi: 10.1186/s12874-020-00975-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Rubin G.J., Greenberg N. Traumatic stress within disaster-exposed occupations: overview of the literature and suggestions for the management of traumatic stress in the workplace. Br. Med. Bull. 2019;129(1):25–34. doi: 10.1093/bmb/ldy040. [DOI] [PubMed] [Google Scholar]
- Cai H., Tu B., Ma J., Chen L., Fu L., Jiang Y., Zhuang Q. Psychological impact and coping strategies of frontline medical staff in Hunan between January and march 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh A., Wilson C.J., Kavanagh D.J., Caputi P. Differences in the expression of symptoms in men versus women with depression: a systematic review and meta-analysis. Harv. Rev. Psychiatry. 2017;25(1):29–38. doi: 10.1097/HRP.0000000000000128. [DOI] [PubMed] [Google Scholar]
- Cenat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Dalexis R.D., Goulet M.A., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Dalexis R.D., Goulet M.A., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong M.Y., Wang W.C., Hsieh W.C., Lee C.Y., Chiu N.M., Yeh W.C., Huang O.L., Wen J.K., Chen C.L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- da Silva F.C.T., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: a systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;104 doi: 10.1016/j.pnpbp.2020.110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Y., Chen Y., Zhang B. Different prevalence trend of depression and anxiety among healthcare workers and general public before and after the peak of COVID-19 occurred in China: a meta-analysis. Asian J. Psychiatr. 2021;56 doi: 10.1016/j.ajp.2021.102547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dong F., Liu H.L., Yang M., Lu C.L., Dai N., Zhang Y., Robinson N., Liu J.P. Immediate psychosocial impact on healthcare workers during COVID-19 pandemic in China: a systematic review and meta-analysis. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.645460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragioti E., Solmi M., Favaro A., Fusar-Poli P., Dazzan P., Thompson T., Stubbs B., Firth J., Fornaro M., Tsartsalis D., Carvalho A.F., Vieta E., McGuire P., Young A.H., Shin J.I., Correll C.U., Evangelou E. Association of antidepressant use with adverse health outcomes: a systematic umbrella review. JAMA Psychiatry. 2019;76(12):1241–1255. doi: 10.1001/jamapsychiatry.2019.2859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé J.P., Smith M.M., Sherry S.B., Hewitt P.L., Stewart S.H. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta A., Sharma A., Torres-Castro R., Pachori H., Mishra S. Mental health outcomes among health-care workers dealing with COVID-19/severe acute respiratory syndrome coronavirus 2 pandemic: a systematic review and meta-analysis. Indian J. Psychiatry. 2021;63(4):335–347. doi: 10.4103/psychiatry.IndianJPsychiatry_1029_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Qushayri A.E., Dahy A., Reda A., Mahmoud M.A., Abdel Mageed S., Kamel A.M.A., Ghozy S. A closer look to the high burden of the psychiatric disorders among health care workers (HCWs) in Egypt during COVID-19 outbreak: a meta-analysis of 3137 HCWs. Epidemiol. Health. 2021;43:1–8. doi: 10.4178/epih.e2021045. (e2021045) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuya-Kanamori L., Barendregt J.J., Doi S.A.R. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid. Based Healthc. 2018;16(4):195–203. doi: 10.1097/XEB.0000000000000141. [DOI] [PubMed] [Google Scholar]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J. Adv. Nurs. 2021;77(8):3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. Bmj. 2020;368 doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Kunz R., Vist G.E., Falck-Ytter Y., Schünemann H.J. What is "quality of evidence" and why is it important to clinicians? Bmj. 2008;336(7651):995–998. doi: 10.1136/bmj.39490.551019.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G., Oxman A.D., Sultan S., Brozek J., Glasziou P., Alonso-Coello P., Atkins D., Kunz R., Montori V., Jaeschke R., Rind D., Dahm P., Akl E.A., Meerpohl J., Vist G., Berliner E., Norris S., Falck-Ytter Y., Schünemann H.J. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J. Clin. Epidemiol. 2013;66(2):151–157. doi: 10.1016/j.jclinepi.2012.01.006. [DOI] [PubMed] [Google Scholar]
- Haleem A., Javaid M., Vaishya R. Effects of COVID-19 pandemic in daily life. Curr. Med. Res. Pract. 2020;10(2):78–79. doi: 10.1016/j.cmrp.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao Q., Wang D., Xie M., Tang Y., Dou Y., Zhu L., Wu Y., Dai M., Wu H., Wang Q. Prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and Meta-analysis. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.567381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter J.P., Saratzis A., Sutton A.J., Boucher R.H., Sayers R.D., Bown M.J. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014;67(8):897–903. doi: 10.1016/j.jclinepi.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Ioannidis J.P. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Cmaj. 2009;181(8):488–493. doi: 10.1503/cmaj.081086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrami H., BaHammam A.S., AlGahtani H., Ebrahim A., Faris M., AlEid K., Saif Z., Haji E., Dhahi A., Marzooq H., Hubail S., Hasan Z. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021;25(1):503–511. doi: 10.1007/s11325-020-02135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrami H., BaHammam A.S., Bragazzi N.L., Saif Z., Faris M., Vitiello M.V. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J. Clin. Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapetanos K., Mazeri S., Constantinou D., Vavlitou A., Karaiskakis M., Kourouzidou D., Nikolaides C., Savvidou N., Katsouris S., Koliou M. Exploring the factors associated with the mental health of frontline healthcare workers during the COVID-19 pandemic in Cyprus. PLoS One. 2021;16(10) doi: 10.1371/journal.pone.0258475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy Y., Nagarajan R., Saya G.K., Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Scherer N., Felix L., Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0246454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Y., Chen M., Zheng X., Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 2020;133 doi: 10.1016/j.jpsychores.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima C.K.T., Carvalho P.M.M., Lima I., Nunes J., Saraiva J.S., de Souza R.I., da Silva C.G.L., Neto M.L.R. The emotional impact of coronavirus 2019-nCoV (new coronavirus disease) Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmud S., Hossain S., Muyeed A., Islam M.M., Mohsin M. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: a rapid systematic review and meta-analysis. Heliyon. 2021;7(7) doi: 10.1016/j.heliyon.2021.e07393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marvaldi M., Mallet J., Dubertret C., Moro M.R., Guessoum S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021;126:252–264. doi: 10.1016/j.neubiorev.2021.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo S.A., Alkhalifah J.M., Alshammari N.F., Alnufaie W.S. Comparison of generalized anxiety and sleep disturbance among frontline and second-line healthcare workers during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18(11) doi: 10.3390/ijerph18115727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore J.P., Offit P.A. SARS-CoV-2 vaccines and the growing threat of viral variants. JAMA. 2021;325(9):821–822. doi: 10.1001/jama.2021.1114. [DOI] [PubMed] [Google Scholar]
- Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. JBI Manual for Evidence Synthesis. 2020. Chapter 5: systematic reviews of prevalence and incidence. [Google Scholar]
- Novelli G., Biancolella M., Mehrian-Shai R., Erickson C., Godri Pollitt K.J., Vasiliou V., Watt J., Reichardt J.K.V. COVID-19 update: the first 6 months of the pandemic. Hum. Genom. 2020;14(1):48. doi: 10.1186/s40246-020-00298-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowrouzi-Kia B., Sithamparanathan G., Nadesar N., Gohar B., Ott M. Factors associated with work performance and mental health of healthcare workers during pandemics: a systematic review and meta-analysis. J. Public Health (Oxf). 2021:1–9. doi: 10.1093/pubmed/fdab173. (fdab173) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyaga V.N., Arbyn M., Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch. Public Health. 2014;72(1):39. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaya B., Pérez-Moreno M., Bueno-Notivol J., Gracia-García P., Lasheras I., Santabárbara J. Prevalence of depression among healthcare workers during the COVID-19 outbreak: a systematic review and meta-analysis. J. Clin. Med. 2021;10(15) doi: 10.3390/jcm10153406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Phiri P., Ramakrishnan R., Rathod S., Elliot K., Thayanandan T., Sandle N., Haque N., Chau S.W., Wong O.W., Chan S.S., Wong E.K., Raymont V., Au-Yeung S.K., Kingdon D., Delanerolle G. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine. 2021;34 doi: 10.1016/j.eclinm.2021.100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raoofi S., Pashazadeh Kan F., Rafiei S., Khani S., Hosseinifard H., Tajik F., Masoumi M., Raoofi N., Ahmadi S., Aghalou S., Torabi F., Dehnad A., Hoseinipalangi Z., Rezaei S., Shabaninejad H., Ghashghaee A. Anxiety during the COVID-19 pandemic in hospital staff: systematic review plus meta-analysis. BMJ Support. Palliat. Care. 2021:1–9. doi: 10.1136/bmjspcare-2021-003125. [DOI] [PubMed] [Google Scholar]
- Ren X., Huang W., Pan H., Huang T., Wang X., Ma Y. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 2020;91(4):1033–1045. doi: 10.1007/s11126-020-09796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed R., Amin F., Talha M., Randenikumara S., Shariff I., Durrani N., Salman S. COVID-19 pandemic prevalence and risk factors for depression among health care workers in South Asia. Asia Pac. J. Public Health. 2021;33(8):935–939. doi: 10.1177/10105395211002324. [DOI] [PubMed] [Google Scholar]
- Sahebi A., Nejati-Zarnaqi B., Moayedi S., Yousefi K., Torres M., Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Khazaie H., Hosseinian-Far A., Ghasemi H., Mohammadi M., Shohaimi S., Daneshkhah A., Khaledi-Paveh B., Hosseinian-Far M. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Glob. Health. 2020;16(1):92. doi: 10.1186/s12992-020-00620-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Khazaie H., Hosseinian-Far A., Khaledi-Paveh B., Kazeminia M., Mohammadi M., Shohaimi S., Daneshkhah A., Eskandari S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum. Resour. Health. 2020;18(1):100. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo G., Vaquerizo-Serrano J., Catalan A., Arango C., Moreno C., Ferre F., Shin J.I., Sullivan S., Brondino N., Solmi M., Fusar-Poli P. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 2020;275:48–57. doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salehi M., Amanat M., Mohammadi M., Salmanian M., Rezaei N., Saghazadeh A., Garakani A. The prevalence of post-traumatic stress disorder related symptoms in coronavirus outbreaks: a systematic-review and meta-analysis. J. Affect. Disord. 2021;282:527–538. doi: 10.1016/j.jad.2020.12.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Bueno-Notivol J., Lipnicki D.M., Olaya B., Pérez-Moreno M., Gracia-García P., Idoiaga-Mondragon N., Ozamiz-Etxebarria N. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saragih I.D., Tonapa S.I., Saragih I.S., Advani S., Batubara S.O., Suarilah I., Lin C.J. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int. J. Nurs. Stud. 2021;121 doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Ripoll M.J., Zamanillo-Campos R., Castro A., Fiol-de Roque M.A., Ricci-Cabello I. Insomnia and sleep quality in healthcare workers fighting against COVID-19: a systematic review of the literature and meta-analysis. Actas Esp. Psiquiatr. 2021;49(4):155–179. [PubMed] [Google Scholar]
- Shahid H., Haider M.Z., Taqi M., Gulzar A., Zamani Z., Fatima T., Khalid Y., Ahmed Z., Nadeem H.A., Anwer F. COVID-19 and its psychological impacts on healthcare staff - a multi-centric comparative cross-sectional study. Cureus. 2020;12(11) doi: 10.7759/cureus.11753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., Moher D., Tugwell P., Welch V., Kristjansson E., Henry D.A. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj. 2017;358 doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmonds M. Quantifying the risk of error when interpreting funnel plots. Syst. Rev. 2015;4:24. doi: 10.1186/s13643-015-0004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R.K., Bajpai R., Kaswan P. COVID-19 pandemic and psychological wellbeing among health care workers and general population: a systematic-review and meta-analysis of the current evidence from India. Clin. Epidemiol. Glob. Health. 2021;11 doi: 10.1016/j.cegh.2021.100737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. Jama. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Sun P., Wang M., Song T., Wu Y., Luo J., Chen L., Yan L. The psychological impact of COVID-19 pandemic on health care workers: a systematic review and meta-analysis. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.626547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troglio da Silva F.C., Neto M.L.R. Psychiatric disorders in health professionals during the COVID-19 pandemic: a systematic review with meta-analysis. J. Psychiatr. Res. 2021;140:474–487. doi: 10.1016/j.jpsychires.2021.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tušl M., Brauchli R., Kerksieck P., Bauer G.F. Impact of the COVID-19 crisis on work and private life, mental well-being and self-rated health in German and Swiss employees: a cross-sectional online survey. BMC Public Health. 2021;21(1):741. doi: 10.1186/s12889-021-10788-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varghese A., George G., Kondaguli S.V., Naser A.Y., Khakha D.C., Chatterji R. Decline in the mental health of nurses across the globe during COVID-19: a systematic review and meta-analysis. J. Glob. Health. 2021;11:05009. doi: 10.7189/jogh.11.05009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia L., Chen C., Liu Z., Luo X., Guo C., Liu Z., Zhang K., Liu H. Prevalence of sleep disturbances and sleep quality in Chinese healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.646342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan H., Ding Y., Guo W. Mental health of medical staff during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Psychosom. Med. 2021;83(4):387–396. doi: 10.1097/PSY.0000000000000922. [DOI] [PubMed] [Google Scholar]
- Zhang W.R., Wang K., Yin L., Zhao W.F., Xue Q., Peng M., Min B.Q., Tian Q., Leng H.X., Du J.L., Chang H., Yang Y., Li W., Shangguan F.F., Yan T.Y., Dong H.Q., Han Y., Wang Y.P., Cosci F., Wang H.X. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020;89(4):242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Li W., Li H., Zhang C., Luo J., Zhu Y., Wu H., Zhu Z., Xu Y., Wang J., Li C. Prevalence and dynamic features of psychological issues among Chinese healthcare workers during the COVID-19 pandemic: a systematic review and cumulative meta-analysis. Gen. Psychiatr. 2021;34(3) doi: 10.1136/gpsych-2020-100344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y.J., Jin Y., Rao W.W., Li W., Zhao N., Cheung T., Ng C.H., Wang Y.Y., Zhang Q.E., Xiang Y.T. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J. Affect. Disord. 2021;287:145–157. doi: 10.1016/j.jad.2021.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
All data generated or analyzed during this study are fully available in published cited literature and included in this article and its supplementary information files.