Abstract
Guideline-directed medical treatment (GDMT) is the mainstay of treatment for patients with heart failure (HF). Despite compelling evidence, patient and provider adherence to these guidelines remains low. This is mostly due to the complexity of the GDMT regimen and the competing comorbid conditions. The COVID-19 pandemic has further complicated the initiation and maintenance of GDMT and overall care for patients with HF. Telemedicine will erase many of the barriers to appropriate HF care that were present before, during, and long after the COVID-19 pandemic has ended.
Keywords: Telehealth, Heart failure, Guideline medications, COVID-19
Key points
-
•
Telehealth and heart failure
-
•
Heart failure and COVID-19
-
•
Heart failure guidelines
-
•
Adherence to heart failure treatment guidelines
Abbreviations.
| COVID-19 | coronavirus disease 2019 |
| GDMT | guideline-directed medical treatment |
| ARNI | Angiotensin receptor-neprilysin inhibitor |
| B-Blocker | Beta blocker |
| AA | Aldosterone antagonist |
| SGLT-2 | Sodium-glucose cotransport-2 inhibitor |
| HF | Heart failure |
| HFrEF | Heart failure with a reduced ejection fraction |
| EF | Ejection fraction |
The coronavirus disease 2019 (COVID-19) pandemic has complicated the management of heart failure (HF), which is by itself an intricate disease to treat. Decreased medical contact, reduced social interactions, and lockdowns during this global pandemic are a few of the many factors that have made treating this medically fragile population more complex. In addition, parallels between COVID-19 infection and resulting myocardial injury have been suggested, which may further impair cardiac function and increase exacerbations.1 Finding innovative strategies to successfully treat patients with HF while keeping them safe from COVID-19 exposure is an unavoidable challenge many providers face while battling this complex virus.
Discussion
Current guideline-directed medical treatment (GDMT) for patients with HF includes the use of Entresto, an angiotensin receptor-neprilysin inhibitor (ARNI), a β-blocker (Metoprolol Succinate, Carvedilol, or Bisoprolol), an aldosterone antagonist (AA), and a sodium-glucose cotransport-2 inhibitor (SGLT-2). This regimen is complex for the patient and provider alike. Patients with HF struggle with polypharmacy and providers battle multiple comorbidities that complicate the initiation and titration of many of the guideline-directed medications. Add in a global pandemic and achieving target or optimal doses of these medications seems like an insurmountable feat.
COVID-19 and Chronic HF
Chronic comorbidities increase the risk of severe COVID-19 and experience a worse prognosis and a mortality rate of over 10%.2 Viral infections such as coronaviruses and influenza have been shown to exacerbate preexisting HF and increase HF-related hospitalizations. Severe COVID-19 infections necessitate increased cardiac performance and high cardiac output, something that patients with HF are mostly unable to produce. According to Bader and colleagues,2 established HF is an independent predictor of in-hospital death for COVID-19–infected patients.
Comorbidities
More than half of all patients with HF are diagnosed with 5 or more comorbid conditions, which compound the risk of all-cause and HF hospitalizations. The most common comorbidities found in patients with HF are hypertension (85.6%), ischemic heart disease (72.1%), hyperlipidemia (62.6%), anemia (51.2%), diabetes mellitus (47.1%), arthritis (45.6%), chronic renal insufficiency (CRI; 44.8%), chronic airway diseases (30.9%), and atrial fibrillation (28.8%).3 CRI is the largest predictor of HF outcome outside left ventricular ejection fraction. Optimal dosing of guideline-directed medications, especially renin-aldosterone-angiotensin blockers, becomes problematic when the glomerular nitration rate is low. Chronic obstructive pulmonary disease (COPD) affects one-third of all patients with HF and predicts mortality. This comorbid condition often goes undiagnosed due to dyspnea, a common finding in patients with HF, being the most frequently reported complaint. There is an underutilization of β-blockers and increased usage of steroids, which increase fluid retention in the COPD population.3
Polypharmacy
Owing to the sizable percentage of patients with HF with multiple comorbid conditions, polypharmacy, which is needing to take 5 or more medications daily, is common. Polypharmacy is associated with disability, decreased functional status, and higher incidence of drug-drug interaction effects.4 The complex medication regimen currently recommended to reduce HF mortality consists of at least 6 medications dosed up to 3 times daily. Combine that with medications used to manage other comorbid conditions, and the result is an overwhelming daily routine that patients struggle to maintain.
Telemedicine and HF
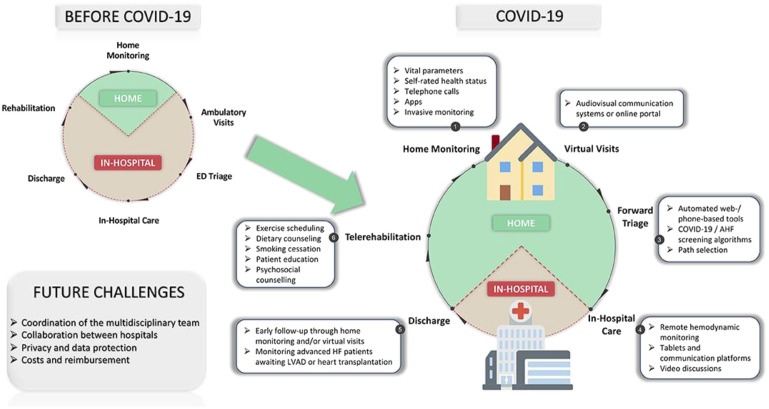
Telemedicine, the practice of delivering health care at a distance using telecommunications technologies, has increased in response to the COVID-19 pandemic. Telemedicine can safely decrease HF hospitalizations, mortality, and risk of exposure to COVID-19.5 The Heart Failure Society of America released a statement in favor of establishing virtual visits for patients with HF to ensure that the risk of COVID-19 infection is decreased while continuing to provide proper and safe follow-up for this cohort. Bader and colleagues reported that the use of telemedicine produced a decrease in the percentage of no-show visits for hospital follow-up visits 7 days after discharge (51% no-show for in-person vs 34.6% for virtual visits). Limited assessment of clinical volume overload (edema or jugular venous distension) paired with recording of daily weights, vitals, and activity tolerance can also aid in assessing symptoms and guide any medication changes. Telemedicine allows patients with chronic HF to have access to care while decreasing the risk of exposure and further spread of the virus (Fig. 1 ).
Fig. 1.
Telemedicine in patients with heart failure before and during COVID-19.
(From Tersalvi G, Winterton D, Cioffi GM, Ghidini S, Roberto M, Biasco L, Pedrazzini G, Dauw J, Ameri P and Vicenzi M (2020) Telemedicine in Heart Failure During COVID-19: A Step Into the Future. Front. Cardiovasc. Med. https://www.frontiersin.org/articles/10.3389/fcvm.2020.612818/full. Published December 2020. Accessed 10/01/2021.)
Telemedicine and GDMT
A systematic review by Yun and colleagues5 reported that telemonitoring patients with HF produces a 19% decrease in all-cause mortality but no change in the rate of hospitalization. Medication adherence and early symptom management were the most-reported reasons for the significant reduction in mortality. A randomized controlled trial by Comin-Colet and colleagues6 demonstrated that HF management using telehealth increased treatment adherence among patients, decreased rehospitalizations, and lowered health-related costs. Blood and colleagues7 stated that remote monitoring via telehealth with or without video of patients with HFrEF for uptitration of GDMT medications is feasible and cost-effective, given the titration program has specific algorithms for titration and are collaborative between a physician, a pharmacist, and an HF nurse.
Implementation of Telemedicine During COVID-19
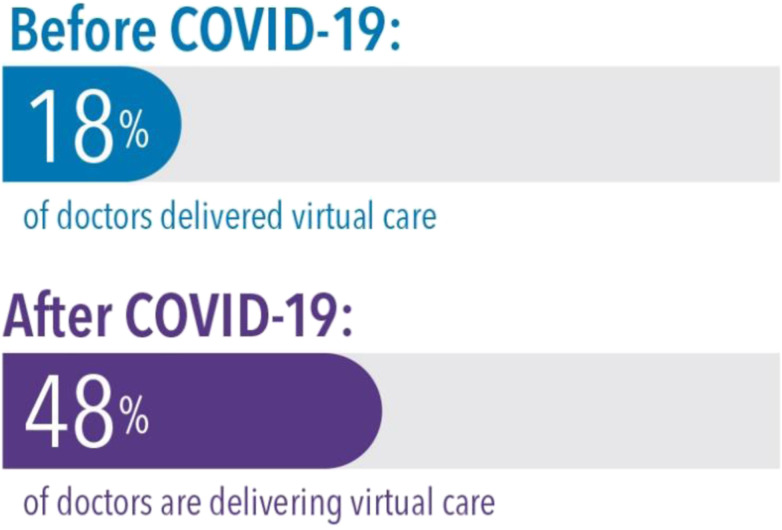
Telehealth is not new to health care providers; it was first used in the 1950s when several hospitals shared images and information via telephone.8 Before the outbreak of COVID-19, most health systems in the United States had low rates of telehealth use for ambulatory patient care. Many health care facilities have increased telehealth visits from less than 100 per day before the pandemic to more than 1000 visits per day currently (Fig. 2 ). Evidence on the use of telehealth for HF management is sparse and controversial because of the underutilization of telehealth until very recently.9 Although current findings support the use of telehealth for adults with HF, a meta-analysis by Zhu and colleagues10 suggests that further research is needed to confirm these results.
Fig. 2.
Rapid adoption in response to COVID-19.
(From Ed Lee, MD, MPH. How COVID-19 created a telehealth surge. Kaiser Permanente Business. https://business.kaiserpermanente.org/insights/telehealth/covid-19-accelerated-telehealth. Published July 28, 2020. Accessed 10/01/2021.)
Hernandez11 discovered through a retrospective chart review that telehealth was successful in increasing the number of patients with HFrEF on the appropriate GDMT medications and decreasing HF hospitalizations. The findings also highlighted opportunities for education about the GDMT medications and their appropriate use. The results of this project also provided evidence that it is possible to initiate these medications despite comorbidities. Her11 review found a 5% increase in patients on appropriate GDMT medications, and this is consistent with the current evidence regarding chronic illness management using telehealth. A systematic review by Kruse and colleagues12 found that using telehealth for cardiovascular disease management reduced hospital admissions and readmissions but failed to find statistical significance from any of the included articles. Greenhalgh and colleagues13 found through their systematic review that telehealth was superior in disease-modifying medication titration to higher, more effective doses as compared with standard care.
Telehealth can be used to manage the full spectrum of patients with HF, including those with reduced EF, preserved EF, and across all stages (A-D). The visits can manage new or worsening symptoms of HF, medication titration, hospital discharge follow-up, and new test results. Health care workers represent 20% of COVID-19 cases, and telehealth allows providers who require quarantine but remain well to continue to manage patients.14 Patients with HF experience many barriers to attending in-person visits, including poor exercise tolerance, difficulty in transporting oxygen, and lack of transportation. Telehealth removes these hurdles, and many believe it will become the norm after the COVID-19 crisis.14
Summary
The use of GDMT for improving HFrEF outcomes is well supported by current practice guidelines and evidence. However, recent literature shows that adherence to the guidelines for HFrEF treatment remains low for the provider and patient. Telehealth removes barriers to care for patients with HF and has demonstrated lower hospitalization rates and increased patient satisfaction. Treatment adherence is increased when telehealth is used, and this leads to better success with GDMT titration. Owing to the COVID-19 pandemic, many health care systems quickly implemented telehealth to continue to manage the HF population while reducing potential COVID-19 exposure. GDMT utilization will increase, and hospitalizations will decrease with the use of telehealth despite COVID-19.
Clinics care points
-
•
Telehealth allows providers who require quarantine but remain well to continue to manage patients.14
-
•
Patients with HF experience many barriers to attending in-person visits, including poor exercise tolerance, difficulty in transporting oxygen, and lack of transportation, and telehealth removes these hurdles.14
-
•
A systematic review by Zhu and colleagues10 reported that telemonitoring patients with HF produces a 19% decrease in all-cause mortality but no change in the rate of hospitalization
-
•
Telemedicine safely reduces health care use by reducing emergency room visits.10
-
•
Telemedicine medication titrations are just as successful as traditional, in-person titrations.10
Disclosure
The author has nothing to disclose.
References
- 1.Tersalvi G., Winterton D., Cioffi G.M., et al. Telemedicine in heart failure during COVID-19: a step into the future. Front Cardiovasc Med. 2020;7:313. doi: 10.3389/fcvm.2020.612818. Accessed September 25, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bader F., Manla Y., Atallah B., et al. Heart failure and COVID-19. Heart Fail Rev. 2021;26:1–10. doi: 10.1007/s10741-020-10008-2. Accessed September 25, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iyngkaran P., Liew D., Neil C., et al. Moving from heart failure guidelines to clinical practice: gaps contributing to readmissions in patients with multiple comorbidities and older age. Clin Med Insights Cardiol. 2018:1–13. doi: 10.1177/1179546818809358. Accessed October, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatt A.S., Niteesh C.K. Evidence-based prescribing and polypharmacy for patients with heart failure. Ann Intern Med. 2021:1–3. doi: 10.7326/M21-1427. Accessed September 25, 2021. [DOI] [PubMed] [Google Scholar]
- 5.Yun J.E., Park J.E., Park H.Y., et al. Comparative effectiveness of telemonitoring versus usual care for heart failure: a systematic review and meta-analysis. J Card Fail. 2018;24(1):19–28. doi: 10.1016/j.cardfail.2017.09.006. Accessed September 27, 2021. [DOI] [PubMed] [Google Scholar]
- 6.Comín-Colet J., Enjuanes C., Verdú-Rotellar J.M., et al. Impact on clinical events and healthcare costs of adding telemedicine to multidisciplinary disease management programmes for heart failure: results of a randomized controlled trial. J Telemed Telecare. 2016;22(5):282–295. doi: 10.1177/1357633X15600583. Accessed September 25, 2021. [DOI] [PubMed] [Google Scholar]
- 7.Blood A.J., Fischer C.M., Fera L.E., et al. Rationale and design of a navigator-driven remote optimization of guideline-directed medical therapy in patients with heart failure with reduced ejection fraction. Clin Cardiol. 2019;43(1):4–13. doi: 10.1002/clc.23291. Accessed September 27, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teoli D., Aeddula N.R. NCBI Bookshelf; 2020. Telemedicine.https://www.ncbi.nlm.nih.gov/books/NBK535343/ Available at: Accessed October 1, 2021. [Google Scholar]
- 9.Wosik J., Fudim M., Cameron B., et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. Accessed September 27, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu Y., Gu X., Xu C. Effectiveness of telemedicine systems for adults with heart failure: a meta-analysis of randomized controlled trials. Heart Fail Rev. 2020;25:231–243. doi: 10.1007/s10741-019-09801-5. Accessed September 27, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hernandez L. Diss. University of Louisiana at Lafayette; Lafayette, Louisiana: 2021. The impact of telehealth on guideline directed medical treatment for people with heart failure.https://www.proquest.com/openview/b26fb45dd140a3b166e0146ab181d3fc/1?pq-origsite=gscholar&cbl=18750&diss=y Available at: Accessed October 1, 2021. [Google Scholar]
- 12.Kruse C., Fohn J., Wilson N., et al. Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: systematic review. JMIR Med Inform. 2020;8(8):e20359. doi: 10.2196/20359. Available at: https://doi.org/10.2196/20359. Accessed September 25, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenhalgh T., A’Court C., Shaw S. Understanding heart failure; explaining telehealth – a hermeneutic systematic review. BMC Cardiovasc Disord. 2017;17:156. doi: 10.1186/s12872-017-0594-2. Accessed September 27, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorodeski E.Z., Goyal P., Cox Z.L., et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020;26(6):448–456. doi: 10.1016/j.cardfail.2020.04.008. Accessed September 27, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]