Abstract
Given the importance of poor nutrition as a cause for human chronic disease, it is surprising that nutrition receives so little attention during medical school training and in clinical practice. Specific vitamins, minerals, fatty acids, amino acids and water in the diet are essential for health, and deficiencies lead or contribute to many diseases. Proper use of the dietary guidelines and nutrition facts labeling can improve nutritional status and lead to the consumption of a healthy diet. COVID-19 has altered access to nutritious foods for millions and increased awareness of the importance of diet and immune function. An improved appreciation for nutrition will improve the outcomes of clinical care.
Keywords: Diet, Nutrition, Essential nutrients, Hydration, Alcohol, Recommended dietary COVID-19
Key points
-
•
Nutrition receives little attention in health-care training but nutrition understanding is essential.
-
•
Specific vitamins, minerals, and certain other nutrients are essential for health.
-
•
The liquids that are central to our essential hydration can also influence dietary health.
-
•
Understanding how to use the dietary guidelines and nutrition facts labeling can improve nutritional status and the consumption of a healthy diet.
-
•
COVID-19 has altered access to nutritious foods for millions and increased awareness of the importance of diet and immune function.
Introduction
Suboptimal nutrition is the central pillar supporting most clinically relevant diseases; in this regard, observational data suggest that diet may be a factor in 45% of all deaths due to heart disease, stroke, and type 2 diabetes.1 Indeed preventive nutrition is central to US programs for economically disadvantaged populations such as the women, infants, and children (WIC) and other prenatal programs that help to reduce the risk of preterm birth, infant diseases, and birth defects.2 , 3 Paradoxically, in a 2008 to 2009 survey, only 26% of US Medical Schools required even a single course in nutrition and on average only 19.6 hours of instruction in nutrition were completed during the 4 years of training.4 A more recent review confirms that the number of hours spent in medical school devoted to nutrition is about 19.5 Moreover, as of this writing, the Accreditation Council for Graduate Medical Education has no requirement for nutrition education during residency or fellowship training and/or advanced specialty training including gastroenterology and cardiology.5
One objective of this article is to provide physicians with the basics of dietary requirements including a clear description of the essential nutrients that all humans require to live regardless of the growing cultural dietary melting pot that the clinician encounters and attempts to interpret. The article includes novel topics of patient interest, including the critical importance of hydration and the many types of liquids available today. Educating patients in a convincing manner to encourage them to choose the best evidence-based path to good nutrition has always been troublesome for both the patient and the physician. The reality is that in a relatively heterogeneous world of many different culturally based food choices and eating plans, there are many preconceptions about what constitutes a “healthy balanced diet and/or healthy food.” Moreover, the data-based field of nutritional genetics ensures that there cannot be any one single best path for every single patient.
Clinicians are often left to make nutrition recommendations based on those from many different “professional” organizations, whose recommendations are not always in agreement; the influence of nonprofessional opinions expressed in blogs, websites, and Television (TV) further clouds the clarity of clinical suggestions. This article provides the clinician with important data-based key information (morsels) to better understand the twenty-first century nutrition guidelines and to advise patients with tools to implement dietary change based on facts and data. Thus, the article contains a historic review of the development of National guidelines and recommendations from the US National Academy of Sciences (NAS), the United States Department of Agriculture (USDA), Centers for Disease Control (CDC) and Food and Drug Administration (FDA) to better help explain the current status of nutrition and dietary guidelines and food product labeling.
Finally, Coronavirus disease 2019 (COVID-19) has altered the public’s perception of the importance of nutrition for a healthy immune system. The article concludes with an up-to-date look at the interface between obesity, diabetes, and other examples of malnutrition and a description of how nutritional status is a major factor associated with in increased risk of severe COVID-19-related medical complications.
Links Between Diet and Disease: Essential Nutrients
Vitamins and minerals
Links between diet and disease have been recorded as early as 1500 bc when ancient Egyptians ate liver (rich in vitamin A) as a cure for night blindness.6 The term, “scurvy,” meaning swollen mouth, was documented in the Middle Ages. Certainly, the importance of isolating citrus fruits to prevent scurvy was a major breakthrough in the eighteenth century.7 However, it was not until the early years of the twentieth century that the 11 individual vitamins were isolated and their chemical formulas were determined. By 1948, all of the vitamins were discovered and chemically identified and are summarized in Table 1 .8 Thus, we remain in the discovery period for how these essential nutrients (defined as molecules that cannot be synthesized by our own bodies and are essential for life) affect our health as well as our responses to deficiencies, diseases, and injury.
Table 1.
Vitamins and their key deficiency disease symptoms. Fat soluble vitamins are colored red; B vitamins are colored blue
| Vitamin | Deficiency Symptom(s) |
|---|---|
| A (retinol) | Night blindness, xerophthalmia |
| Thiamin (B1) | Beriberi, polyneuropathy, Wernicke’s encephalopathy |
| Riboflavin (B2) | Glossitis, dermatitis |
| Niacin | Pellagra, diarrhea, mental disturbance |
| B6 (pyridoxine) | Macrocytic anemia, depression convulsions |
| B12 (cobalamin) | Macrocytic anemia, peripheral neuritis, spinal cord degeneration |
| Biotin | Dermatitis, axorexia, muscular pain |
| Pantothenic acid | Nervous and intestinal disorders |
| Folic acid | Anemia, macrocytic anemia |
| C (ascorbic acid) | Scurvy, sore gums, capillary bleeding |
| D (cholecalciferol) | Rickets, bone deformity, tetany |
| E (tocopherol) | Hemolytic anemia, neuromuscular dysfunction |
| K (phylloquinone) | Decreased blood clotting, bleeding |
Modified From: Vitamin Intake and Health, edited by S.K. Gaby, A. Bendich, V. N. Singh, L. J. Machlin, 1991, pp 1-16.8
Vitamins are not the only essential nutrients for humans. By definition, all mineral elements that are found in the human body are essential as no one has yet synthesized an element. There are 2 classifications of essential mineral elements, major and trace. The major mineral elements include calcium, phosphorus, potassium, sodium, and magnesium. The trace elements include sulfur, iron, chlorine, cobalt, copper, zinc, manganese, molybdenum, iodine, and selenium. Each of the 15 minerals has their own constellation of deficiency symptoms such as iron deficiency anemia and osteoporosis due to calcium deficiency (Table 2 ).9 We are still learning about the essentiality of trace minerals as can be seen by the inclusion of chromium for the first time as essential nutrient in the 2001 edition of the US Dietary Reference Intakes (DRIs).10
Table 2.
Common minerals and their associated deficiency symptoms
| Mineral | Deficiency Symptom(s) |
|---|---|
| Iron | Iron deficiency anemia |
| Iodine | Infancy—congenital hypothyroidism with potential cognitive loses Adults—thyroid goiter |
| Zinc | Acrodermatitis enteropathica, growth retardation, hypogeusia |
| Magnesium | Tremor, muscle spasm, nystagmus, seizures |
| Selenium | Keshan disease—cardiomyopathy |
| Calcium | Osteoporosis |
Modified From: Stephenson, T., Sanctuary, M. R. Passerrello, C.W. Human Nutrition: Science for Healthy Living. McGraw-Hill, 2022.9
Essential fats
With the clear findings that dietary deficiencies of vitamins were causing serious health issues including death, there was a strong impetus to determine if there were other essential nutrients required in the human diet. Clinical nutrition researchers in the 1930s were looking for the link between signs of deficiencies associated with the development of scaly skin, reproductive failure, growth failure, and kidney degeneration in animal models. They identified 2 more essential nutrients: the fatty acids, linoleic acid, an omega-6 fatty acid and linolenic acid, an omega-3 fatty acid. Both are the building blocks of all other fatty acids that can be synthesized in the body to varying degrees. The fatty acids are required for formation of the lipid bilayer around every cell, the synthesis of hormones, growth factors, prostaglandins and other immune factors, and many more molecules necessary for cell-to-cell communication.11 Moreover, the fat-soluble vitamins (A, E, D, and K) as well as vitamin precursors, such as fat-soluble beta-carotene (the major source of vitamin A) are best absorbed when there is fat in the diet. Even though it was well accepted that humans require consumption of these 2 essential fatty acids, even in the 1989 recommended dietary allowance (RDA) report for many reasons the subcommittee had not established an RDA for n-3 or n-6 polyunsaturated fatty acids.12 This was because essential fatty acid deficiency had been observed exclusively in patients with medical problems affecting fat intake or absorption.
Essential amino acids
In addition to the 11 vitamins, 15 minerals and 2 fatty acids, there are 9 more essential nutrients for humans and these are 9 amino acids: phenylalanine, valine, threonine, tryptophan, methionine, leucine, isoleucine, lysine, and histidine. Amino acids are the key components of all proteins.13 Certain amino acids, including some of the essential ones, have unique functions independent of protein synthesis. In total, there are 21 amino acids, 12 of which can be synthesized by humans and 9 that must be consumed. The major natural source of essential amino acids is protein, mainly animal protein for balanced amnio acid delivery. There are protein sources that do not contain all of the essential amino acids and if humans, especially infants and growing children consume protein sources that do not contain all of the essential amino acids, they will not thrive. As a result they will lose weight, develop edema, be lethargic and can lose cognitive abilities, even if there is only one of the 9 amino acids absent in the diet of a young child or an adult. Deficiency symptoms manifest themselves even when the subjects are unaware, and during a pronounced negative nitrogen balance, problems with appetite, extreme fatigue, and nervous irritability can develop.13 The essential amino acids are discussed in the text of the 1989 RDA; however, recommendations are made for total protein intake not individual essential amino acids.12
Carbohydrates
Carbohydrates represent a clinical paradox with respect to their being essential in the healthy human diet, but not an essential “nutrient” based on the classic definition. Carbohydrates consist of monosaccharides (ie, glucose), disaccharides (ie, lactose) and polysaccharides (ie, starch, glycogen and plant-fiber). Polysaccharides such as starch in a cracker are readily metabolized, whereas fiber is a carbohydrate and is not metabolized by the digestive enzymes available in the human gut.
Although adult humans have a carbohydrate RDA of 130 g/d, there are examples of populations existing on a virtually carbohydrate-free diet. The historic Inuit Eskimos of Greenland almost never developed Cardiovascular disease (CVD) or diabetes, and relied almost completely on a meat-based diet with little or no carbohydrate intake before the introduction of Western diets and diseases.14 They lived a very physically active lifestyle and survived (thrived) on the fat and protein in meat and used gluconeogenic amino acids from that meat to create the glucose required for neural function. However, between 1951 and 1961, the Inuit of Canada had a life expectancy at birth of 37 years, which was 33 years lower than the Canadian average,15 and it is possibly not surprising the possible cardiovascular disease benefits of their low-carbohydrate diet may reflect that these persons simply did not live long enough to develop cardiovascular disease. Recently, there has been increased interest in carbohydrate-free diets. However, long-term human randomized control trials that examine the safety of a carbohydrate-free diet do not exist, and most studies of low-carbohydrate diets (aka Atkins. Ketogenic, Low Carb Paleo, and so forth) are neither double blind nor last longer than a year.
Undeniably, consumption of large amounts of refined dietary carbohydrates for long periods have been consistently associated with a variety of diseases including obesity, diabetes, cancer, and cardiovascular disease. Paradoxically, persons living in the absence of dietary fiber and whole grains are also more likely to develop diseases such as colon cancer and cardiovascular disease. However, because production of a pound of meat requires at least 10 lbs of grain, it has been proposed that the dietary carbohydrates will need to become an ever more essential part of the human diet if we hope to feed our planet in an environmentally sustainable fashion.16
Increased intakes of carbohydrates have been linked with increased risk of obesity and an upper safe limit has not been uniformly agreed on. Increased obesity and fatness are well-known risk factors for cardiovascular disease and early death. Body mass index (BMI) is often used to assess fatness or whether a patient is effectively making dietary changes to facilitate improvements in adiposity. BMI is defined as the body mass (weight) divided by the square of the body height or weight in pounds divided by height in inches squared times 703. BMI categorizes adults as underweight (less than 18.5 kg/m2), normal weight (18.5–24.9), overweight (25–29.9), and obese (30 or more). The CDC growth charts predict BMI/age for children ages 2 to 20 years that help track growth and changing nutrient intake from birth to adulthood (http://www.cdc.gov/growthcharts).17 Although BMI assessment is simple and easy to perform, it may only be predictive of obesity as little as 50% of the time.18 Although BMI is predictive of overall mortality, it is not perfect, and personal fitness level (eg, Vo 2 max) is more reliable for predicting health and overall mortality, as well as more expensive.19 Changes in nutrition and exercise fitness are not always reflective of changes in BMI. There is often a clinical misunderstanding when determining if a patient is successfully changing their diet across a treatment regimen. Other articles in this series provide greater details regarding the utility of BMI for the assessment of nutrition behavioral change.
Water and other liquid sources of hydration
Water intake is necessary for human survival. Everyday physiologic functions, such as perspiration, urination, and healthy bowel movements, diminish the body’s water content, and therefore, water intake must be sufficient daily to account for these losses. For adults who are not exercising, the daily adequate intake level for women is 2.7 L (91 ounces 11.3 cups) and 3.7 L (125 ounces or 15.6 cups) from all food and beverage sources.20 Water needs can also be estimated to be 35 to 45 mL/kg/d, and during exercise, needs increase by about 1 mL water for each calorie of oxidized energy used during exercise.21 Care must be taken when estimating human water requirements because of the tremendous variations in human body weight, levels of activity, and basic health (water loss due to sweating or diarrhea), and the water content of the food consumed.
Although water is the most common substance on Earth, access to drinkable, clean water remains a major concern in many regions of the world and even in the United States with respect to the problem in Flint Michigan’s struggle with tap-water lead contamination.22 Generally, tap water is safe in the United States and the best source of water, readily available, and the most cost-effective; for this reason, clinicians should promote it in the clinical setting.
Green tea consumption has been linked to reducing the risk of cancer23 and cardiovascular disease.24 A recent green tea meta-analysis by Wang and colleagues suggests that the protective relationship is strongest for green tea and slightly protective for black tea.25 Green tea consumption was found to be particularly protective against all cause mortality for those who had a prior stroke or myocardial infarct.26
Coffee consumption is considered safe and may provide several health benefits. Coffee intake may even be protective against the development of hypertension in comparison to noncoffee drinkers.27 Cardiovascular disease risk is lowest for those consuming 3 to 5 cups of caffeinated coffee per day, with consumption of more than 6 cups/d remaining relatively neutral for CVD risk.28 Moderate coffee consumption is inversely significantly associated with CVD risk, with the lowest CVD risk at 3 to 5 cups/d, and heavy coffee consumption was not associated with elevated CVD risk. In addition, recent evidence suggests that coffee consumption may be beneficial for preventing type 2 diabetes,29 a condition commonly associated with cardiovascular disease. Caffeinated coffee is also associated with improved cognitive function in persons aged older than 60 years, although the effect was not strong for consumers of decaffeinated coffee.30 Most epidemiologic studies show the absence of any appreciable association between coffee intake and most common neoplasms; indeed, an inverse relationship between coffee consumption and colorectal cancer risk may exist.31
Dairy milk has long been recognized as a way to improve calcium intake and bone health, especially when it is fortified with vitamin D. The high-calcium content in milk and its lipid content, which improves absorption of lipid-soluble vitamins, make it ideal as a medium for vitamin D fortification. Milk is also an excellent source of potassium, magnesium, and protein. The Dietary Approaches to Stop Hypertension (DASH) study suggested that low-fat dairy consumption may reduce blood pressure.32 Milk does not seem to affect overall mortality and may reduce the risk of cardiovascular disease, an effect that is probably stronger for low-fat milk.33
Nondairy milk is often preferred by patients who choose to not consume dairy milk products for a variety of reasons that include lactose intolerance, dietary preferences (vegetarian), taste, environmental sustainability, or health concerns that may or may not be supported by clinical evidence. Plant-based milks derived from almond, palm, oats, rice, and other plants have been widely accepted among consumers, with soy-milk remaining the most popular. Plant-based milks were estimated to represent upward of 13% of the total US milk market in 2020.34 Although the nutritional content of dairy (cow) milk products is relatively consistent, nutritional contents of plant-based milks are more variable making any one clinical recommendation for all plant-based milk more difficult; the differing degree of nutritional supplementation further complicates the use of any single recommendation,35 especially for children.36
Fruit juices are a popular way to increase fruit consumption because of their widespread accessibility, ease of storage, modest cost, and for hedonistic reasons (taste). The USDA recommendations at MyPlate suggest using 100% fruit juice as equivalent to a fruit serving for the purpose of the plate.37 The energy content of apple juice and orange juice (110 kcal/240 mL serving) is about 6% higher than that of cola drinks. The energy content of white grape juice is even higher, around 150 kcal/240 mL. Overconsumption of fruit or vegetable juices can lead to excess carbohydrate intake and weight gain, so caution should always be given in the clinical setting.
Sugar sweetened beverages (SSBs) intake assessed by the The National Health and Nutrition Examination Survey (NHANES) 2005 to 2006 data set for adolescents aged 13 to 19 years averaged 242 kcal/d of soft and fruit drinks that represented about 17% of daily caloric intake.38 Adult and adolescent obesities are increasing in the United States but the exact reason for this is probably multifactorial, although Sugar sweetened beverages (SSB) consumption is probably one contributing factor. In adults, consumption of SSB is positively and tightly correlated with weight gain and risk for developing metabolic syndrome as well as type 2 diabetes.39 After 24 years of follow-up, women who consumed 2 or more servings of SSBs per day had a 35% higher risk of developing coronary heart disease compared with those who consumed less than one serving/mo.40 High fructose corn syrup (HFCS) is a common sweetener used in the beverage industry, although it is often demonized in the website and blogs. Although there are health effects associated with excessive fructose intake. HFCS does not seem to contribute any more than the direct negative health effects of those related to overall higher than recommended caloric intake.41
Artificial sweeteners used in beverages have become an ever more popular alternative for caloric sweeteners in SSBs, although their health effects on even basic diseases such as obesity or weight loss remain unclear, and public ability to identify them remains very poor.42 In light of these realities, it is perhaps sensible to suggest limiting intake no more than 1 or 2 cups/d, although no soda intake is clearly preferable.
Alcohol
Moderate consumption of alcohol is generally defined as 2 drinks a day for a man or one for a woman although defining “drink equivalence” is not always simple (Fig. 1 ). Moderate alcohol consumption is protective against myocardial infarction43 and generally not associated with increased cancer risk other than the direct link between alcohol and significantly increased risk of breast cancer in women.44 , 45 Wood and colleagues (2008) observed the effect of alcohol on life expectancy in a study of 83 prospective cohort studies that included 787,000 subjects.46 Their study concluded that for persons aged between 40 and 50 years, life expectancy was longest when alcohol intake was less than 100 g/wk or intake between 0 and 1 drink per day. Alcohol consumption in greater amounts for many, and even small amounts for some, creates many social problems, such as violence and accidents, as well as fetal alcohol syndrome when consumption occurs during pregnancy. Additionally, binge drinking and/or consistent intake of alcohol intake during pregnancy is associated with significant increased risk of miscarriage and stillbirth.47 Moreover, of clinical note, alcohol consumption can lead to poor judgements that can lead to an inability to maintain healthy dietary recommendations (calories from alcohol consumption are rarely counted by consumers) and may adversely interact with the pharmacologic regimens that are important for those being treated for disease.
Fig. 1.
Equivalent beverages volumes that provide the US definition of one “drink” containing 14 g of alcohol.48
National Dietary Guidelines and Food-Related Programs
With 37 dietary components that are required for human life, it is no wonder that dietary intake, diet quality, and nutrient quantity are areas of intense research. In addition to nutrition research, several governmental and quasi-governmental organizations are responsible for setting National guidelines for dietary intake for age/sex groups including pregnancy.
Recommended dietary allowances and flour/bread enrichment—food fortification
The NAS was established by Congress in 1863. The Academy remains a key advisor to the federal government on scientific and technical matters. The NAS is a private, nonprofit, self-perpetuating society of distinguished scholars engaged in scientific and engineering research, dedicated to the furtherance of science and technology and to their use for the general welfare. The National Research Council, a division of the NAS, was charged with developing recommendations concerning the intake of the known essential nutrients for the American public. Recommended Dietary Allowances, published in 1941,49 was developed following the start of World War Two (WWII) in Europe when it became clear that the US would require a well-nourished population and armed services. During the same time period, in 1939, the Council on Foods of the American Medical Association recommended the addition of vitamins and minerals to “general purpose foods” to restore these to the “high natural level”. Two multinational companies had synthesized and were manufacturing the known vitamins and other companies had manufactured compounds of iron and calcium. Flour and bread companies were already adding different dietary components such as thiamin, B-complex, and nonfat dry milk to their products. Both the NRC and the Food and Drug Administration (FDA) agreed on the term “enriched” in 1941, and an enrichment formula was agreed to include thiamin, riboflavin, niacin, iron, vitamin D, and calcium. Thus, the First Edition of the RDA included recommendations for these 6 essential nutrients as well as for calories, protein, vitamin A, and ascorbic acid. The recommendations were for men and women at 3 different activity levels, moderately active, very active, and sedentary, pregnancy (second half), lactation, children (male and female) aged from less than 1 year to 20 years. The recommendations were for healthy people and examples of dietary patterns were included. The authors stressed that these recommendations were not standards and could change as new data became available.49 The RDA were revised about every 5 years. The 1968 RDA formed the basis of FDA’s initiative to include information about vitamin and mineral content of foods on food labels.50 The food label, in a particularly confusing way for consumers, labeled the single value for each nutrient (that was applicable to individuals aged 4 years and older regardless of body size) as the US RDA for that nutrient.
The tenth and last edition of the RDA was published in 1989 and contained many significant changes compared with the RDA that was last published in the ninth edition.12 The tenth edition established the RDA for vitamin K and the mineral, selenium; the RDA for folate was halved; the RDA for vitamin B12 was lowered by one-third to one-half, and the iron RDA was reduced. Because the RDAs are typically used for planning and procuring food supplies for population subgroups, including the Armed Forces and Federal prison populations, for interpreting food consumption records of individuals and populations, for establishing standards for food assistance programs, for evaluating the adequacy of food supplies in meeting national nutritional needs, for designing nutrition education programs, and for developing new products in industry, these radical changes in levels of essential nutrients were not acceptable to many nutritionists and other health professionals, and a new system was established to determine nutrient requirements. Concurrent with the publication by the NRC of the 1989 RDAs, the proceedings of a keystone meeting concerned with the role of nutrition and potential for preventing/reducing the risk of chronic diseases was published, also by the NRC.51
Dietary Reference Intakes (DRIs) from the National Academy of Sciences Institute of Medicine
During the next 8 years, many nutrition policy meetings were held culminating in the NAS’s Institute of Medicine developing new sets of guidelines not only to prevent essential nutrient deficiencies but also to determine the potential to reduce the risk of certain chronic diseases associated with dietary intakes. The new guidelines are called Dietary Reference Intakes (DRIs). The DRIs for different sets of nutrients were published during the period 1998 to 2001. As an example, the DRI for vitamin C, vitamin E, selenium, and carotenoids was published in 2001 and has not been revised to date.52 In 2011, revised DRIs were published only for calcium and vitamin D. None of the other DRIs has been revised since first published from 1998 to 2001.53
Unlike the essential nutrients, there is no universal RDA or DRI for energy (calories) because of the multitude of factors that play into an individual’s energy needs. Estimation equations for energy requirements for healthy individuals are available and provide a guideline for the number of calories required to maintain a consistent weight. These equations take into account age, sex, weight, height, and level of physical activity. Available equations include infants and young children, both boys and girls aged from 3 to 8 years and from 9 to 18 years, male and female adults, and pregnant and lactating women.54
Food plate and the United States Department of Agriculture (USDA)
Two major food-related responsibilities of the USDA are to provide food to low-income persons and their family members and to provide guidance to Americans concerning their diet choices.
Food programs: The USDA is one of the largest Federal departments and has a myriad of programs. There are many programs that directly provide food to infants, children, and adults. USDA's domestic food and nutrition assistance programs affect the daily lives of millions of people, with about 1 in 4 Americans participating in at least one program at some point during a given year. The Supplemental Nutrition Assistance Program is the Nation’s largest domestic food and nutrition assistance program for low-income Americans. The Special Supplemental Nutrition Program for WIC is the third largest USDA domestic food and nutrition assistance program. The WIC program served about 6.2 million participants per month in fiscal year 2020, including almost half of all infants born in the United States. The USDA also administers 5 other child nutrition programs: the National School Lunch Program, School Breakfast Program, Child and Adult Care Food Program, Summer Food Service Program, and After-School Snacks and Meals.
Dietary Guidelines for Americans (DGA) was first released in 1980. Since then, the DGA have become the cornerstone of Federal food and nutrition guidance.55 The DGA provide nutritional advice for Americans who are healthy or who are at risk for chronic disease but do not currently have a chronic disease.55 The Guidelines are published every 5 years by the USDA, together with the US Department of Health and Human Services. The purpose of the DGA is to help health professionals and policymakers to advise Americans about healthy choices for their diet. The current edition (2020–2025) is the first to include dietary guidelines for children from birth to 23 months and gives 4 overarching guidelines56: 1. follow a healthy dietary pattern throughout life; 2. use nutrient-dense food and beverages to reflect personal preferences, cultural traditions, and budgetary considerations; 3. meet dietary food group needs with nutrient-dense foods and beverages within calorie limits; and 4. limit foods and beverages with higher added sugars, saturated fat, and sodium, and limit alcoholic beverages. In support of these 4 guidelines, the key recommendations are as follows: avoid added sugars for infants and toddlers and limit added sugars to less than 10% of calories for those 2 years old and older; limit saturated fat to less than 10% of calories starting at age 2; limit sodium to less than 2300 mg per day (or even less if younger than 14); and limit alcoholic beverages (if consumed) to 2 drinks or less daily for men and 1 drink or less a daily for women.
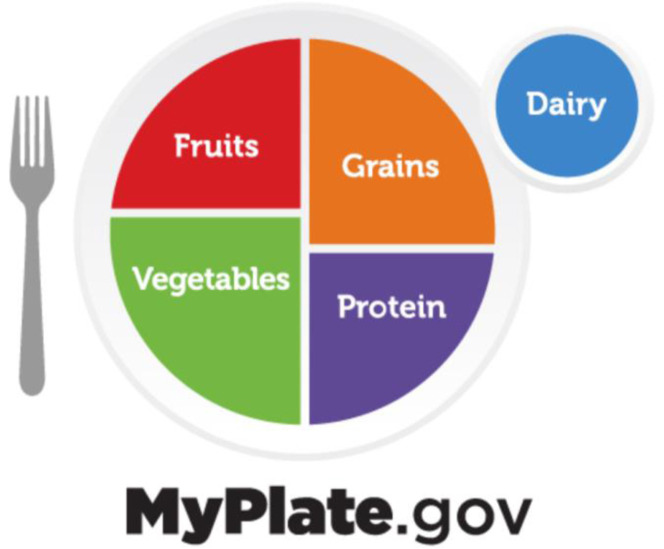
The USDA initiated the use of consumer food and meal planning guidelines in 1916 and has used many pictures, including a food wheel and food guide pyramid to help consumers understand what they should consume in each meal to meet the DGA. MyPlate.gov was first developed in 2011 and was based on the 2010 version of the DGA. The current version (Fig. 2 ) is based on the current DGA, 2020 to 2025, and attempts to indicate that half of the diet (plate) should contain fruits and vegetables for each meal.37 The 2020 to 2025 DGA advise that adults should consume 1.5 to 2 cup-equivalents of fruits and 2 to 3 cup-equivalents of vegetables daily. The latest data from the CDC indicate that in 2019, 12.3% and 10.0% of surveyed adults met fruit and vegetable intake recommendations, respectively. Meeting fruit intake recommendations was highest among Hispanic adults (16.4%) and lowest among men (10.1%). Meeting vegetable intake recommendations was highest among adults aged 51 years and older (12.5%) and lowest among adults with low income (6.8%).57
Fig. 2.
Balanced nutrition education expressed with the USDA MYPLATE image.37
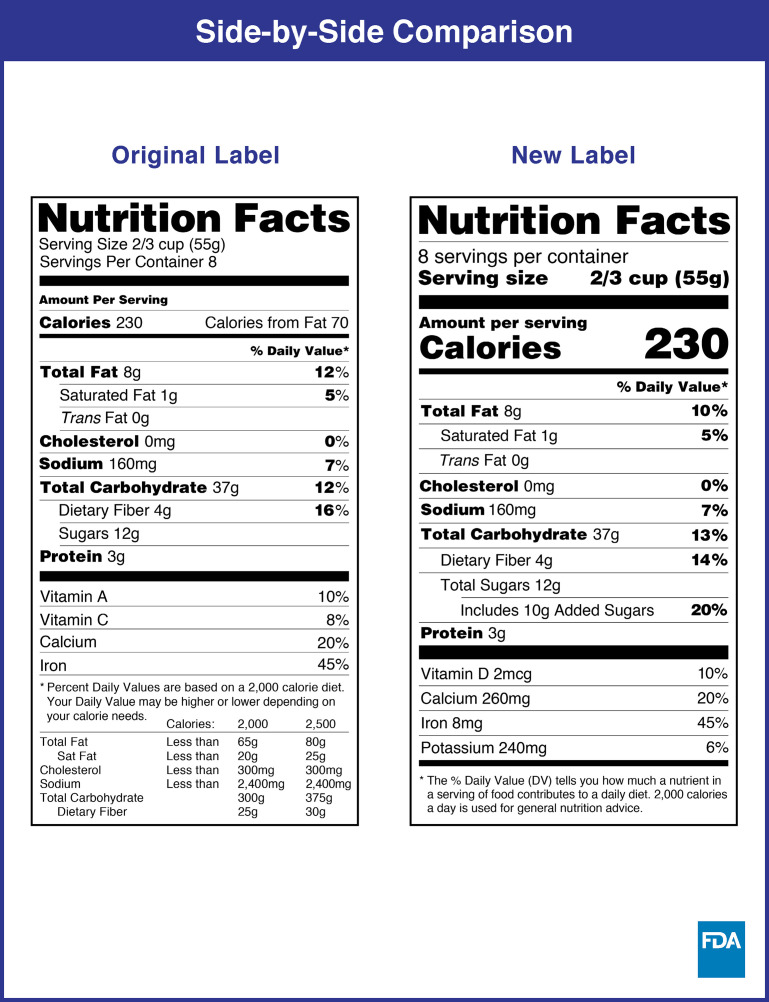
Nutrition Facts Label (NFL) use was mandated through the 1990 Nutrition Labeling and Education Act. The label has changed only slightly since its inception in 1994, with trans fat added to the nutrients required to be listed in 2006. In 2016, the FDA released revised rules for the NFL to help make the information on labels easier to understand for consumers and more relevant to today’s nutritional needs, although some evidence argues that the new label is still confusing to the consumer.58 Manufacturers with $10 million or more in annual sales were required to switch to the new label by January 1, 2020; manufacturers with less than $10 million in annual food sales had until January 1, 2021 to comply.59 Thus, the current, more complex label is a recent advancement for providing consumers more information on food labels (Fig. 3 .)59
Fig. 3.
Comparison of new and old nutrition facts labels used for consumer nutrition education.59
CDC monitors the health of the US population and at the same time, surveys the nutritional status of the population. The National Center for Health Statistics, which is under the CDC has been looking at the health and nutritional status of the US population since the 1960s. NHANES II 1976–1980, provided by the National Center for Health Statistics, is a program of studies designed to assess the health and nutritional status of adults and children in the United States. The survey is unique in that it combines interviews and physical examinations. In 1999, the survey became a continuous program that has a changing focus on a variety of health and nutrition measurements to meet emerging needs. The survey examines a nationally representative sample of about 5000 persons each year. These persons are located in counties across the country, 15 of which are visited each year. The data from the NHANES surveys provide the major documentation for the development of the US dietary recommendations and guidelines.60
Nutritional Challenges of the Evolving COVID-19 Pandemic
Food insecurity occurs when people lack consistent access to enough food for a normal active life. It was previously considered that basic nutrition has changed during these first 2 years of the COVID-19 pandemic. COVID-19 lockdowns, quarantine, and changing food delivery systems have changed food intake, eating behaviors, and dietary quality in Europe and most countries.61 The lockdown has generally increased the tendency to cook at home and has been associated with increased fruit, vegetable, legume, and water intake, with decreased red meat intake, what most clinicians would call “dietary improvement.” However, these average improvements are balanced by tremendous COVID-19-related increases in food insecurity and malnutrition experienced by those who are elderly, schoolchildren no longer coming to schools, unemployed, clinically depressed, and those in disadvantaged socio-economic status.62 It is well known that malnutrition is a risk factor for many diseases, and COVID-19 is no different.
COVID-19 has fundamentally changed the basic food delivery systems that determine access to our diet and the status of our resulting nutritional quality. Lockdowns and quarantines made access to raw or processed foods more complicated and potentially unsafe even for those with prior vaccination.63 Deliveries of retail grocery products through online orders can be made through Amazon, Walmart, and a variety of delivery apps and intermediary facilitators. Premade restaurant items can be delivered through Grubhub, DoorDash, Uber Eats, and a plethora of other intermediaries. Home meal kits that provide all components for prepare-at-home meals for an entire week or more can be sent in a box through the mail can through companies such as Freshly.com. However, these functionaries require economic resources, online or Wifi access, a credit card for making purchases, and online literacy. The elderly, racial minorities, single parents, and those with physical or mental handicaps including those who may not have access to food delivery resources are at greater risk of food insecurity and malnutrition,64 which is associated with increases the risk and severity of COVID-19 infection.
Nutritional needs change further when a person is infected but not hospitalized with COVID-19 because the ability to feed ones-self or access food while at home under quarantine may be impaired. In recent US study of 192,550 adults who were hospitalized for COVID-19, the duration of the COVID-19 stay for non-Intensive Care Unit (ICU) patients was 6 days and 15 days with ICU admittance with nutrition-related comorbidities at admittance including hypertension (61.5%), diabetes (38.4%), and obesity (27.4%).65 COVID-19 mechanical ventilation was typically required for 15 days (1–85 days range) and total hospital stay before discharge was 25 days (7–86 days range). Mechanical ventilation recipients require either enteral or parenteral nutrition that requires very specialized nutritional attention that is further complicated by the aforementioned COVID-19 comorbidities.66
Direct COVID-19 infection, quarantine due to contact with infected family members, or fear related to COVID-19 risk factors have led to unprecedented labor shortages and inability to monitor patient nutrition when patient monitoring needs are greatest.67 Clinical ability to tailor nutritional demands for those with hypertension, diabetes, and obesity would otherwise be paramount during an ICU stay. During longer periods of inactivity related to lockdown or hospitalization, the elderly and those on ventilators are at great risk of significant muscle wasting and sarcopenia.68 These nutritional complications are experienced at the exact time when access to intensive dietary therapy is hindered by COVID-19-dependent work force reductions and patient hospitalization overload.
Specific nutrient interactions may predict either severity of disease or the potential for protection from the clinical manifestations of COVID-19. Vitamin D is readily synthesized when the skin is exposed to direct sunlight especially during summer months; however, stay-at-home and other lockdown protocols can result in deficiencies. In this regard, low vitamin D levels have been shown to be highly correlated with increased COVID-19 infection rates and symptom severity.69 Moreover, dietary supplementation studies, such as those using zinc70 show promise as does a simple recommendation that the population seek more direct sunlight to enhance vitamin D synthesis. Because the COVID-19 cytokine storm induces a proinflammatory response, a great interest has developed in vitamins such as vitamin D, minerals such as zinc, and antioxidants such as vitamin C and glutathione for a potential role as part of COVID-19 prevention, treatment, and recovery,71 although definitive randomized intervention studies for the utility of these supplements have been negative, to date.
Summary
Approximately 80% of the major chronic diseases, such as obesity, diabetes, hypertension, and diet-related cancers, are at least partly preventable with better nutrition. Unfortunately, medical training and practice is focused on the treatment of these conditions after their diagnosis. It is critically important that both the clinician and the patient understand that humans are required to consume a varied diet that contains sufficient liquids and the essential vitamins, mineral, fats, and amino acids necessary for life. General fluency with respect to the health effects of water, tea, coffee, SSBs is also an area of intense patient interest and clinical significance. An improved understanding of the governmental organizations responsible for nutrition recommendations and the use of NFLs on food products can improve health outcomes. Growth charts, BMI, and caloric need calculations are also important clinical nutrition considerations. Finally, the complications to food availability, delivery, and nutrition assessment in relation to the ongoing COVID pandemic will continue to stress our ability to provide the most data-driven recommendations concerning nutrition for health, disease prevention, and treatment. It is clear that much needs to be done to avoid a continuation of the increase in deaths associated with many different diet-based preventable conditions. It is true that the scientific basis of nutrition recommendations is constantly changing, as is true for all science/research-based fields. This article can help the clinician understand the changes that have led to the current diet recommendations and can remind the patient that as more nutrition research is done, the recommendations will further improve their nutrition and overall health.
Clinics care points
-
•
Both the clinician and the patient understand that humans are required to consume a varied diet that contains sufficient liquids and the essential vitamins, mineral, fats, and amino acids necessary for life.
-
•
Growth charts, BMI, and caloric need calculations are also important clinical nutrition.considerations.
-
•
The complications to food availability, delivery, and nutrition assessment in relation to the ongoing COVID pandemic will continue to stress our ability to provide the most data-driven recommendations concerning nutrition for health, disease prevention, and treatment.
Acknowledgments
Disclosure
Drs T. Wilson and A. Bendich have no disclosures.
References
- 1.Micha R., Peñalvo J.L., Cudhea F., et al. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317:912–924. doi: 10.1001/jama.2017.0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Catov J.M., Bodnar L.M., Olsen J., et al. Periconceptional multivitamin use and risk of preterm or small-for-gestational-age births in the Danish National Birth Cohort. Am J Clin Nutr. 2011;94:906–912. doi: 10.3945/ajcn.111.012393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Czeizel A.E., Vereczkey A., Szabó I. Folic acid in pregnant women associated with reduced prevalence of severe congenital heart defects in their children: a national population-based case-control study. Eur J Obstet Gynecol Reprod Biol. 2015;193:34–39. doi: 10.1016/j.ejogrb.2015.06.024. [DOI] [PubMed] [Google Scholar]
- 4.Adams K.M., Kohlmeier M., Zeisel S.H. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med. 2010;85:1537–1542. doi: 10.1097/ACM.0b013e3181eab71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devries S., Willett W., Bonow R.O. Nutrition education in medical school, residency training, and practice. JAMA. 2019;321:1351–1352. doi: 10.1001/jama.2019.1581. [DOI] [PubMed] [Google Scholar]
- 6.Olsen J.A., Vitamin A. In: 2nd Edition. Machlin L.J., editor. Marcel Dekker; New York: 1991. Handbook of vitamins; pp. 2–57. [Google Scholar]
- 7.Moser U., Bendich A. In: 2nd Edition. Machlin L.J., editor. New York; 1991. Vitamin C In: Handbook of vitamins; pp. 196–232. [Google Scholar]
- 8.Vitamin intake and health, edited by Gaby S.K, Bendich A., Singh V. N., et al, 1991, pp 1-16.
- 9.Stephenson T., Sanctuary M.R., Passerrello C.W. McGraw-Hill; New York City, New York: 2022. Human nutrition: science for healthy living. [Google Scholar]
- 10.Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and chromium. Institute of medicine (US) panel on micronutrients. National Academies Press; Washington (DC): 2001. Chromium; pp. 197–223. [PubMed] [Google Scholar]
- 11.Lands, W.E.M. Polyunsaturated fatty acid effects on cellular interactions. In: Micronutrients in health and in disease prevention, edited by Bendich A and Butterworth C E, New York: 1991, pp 9-34.
- 12.National Research Council . 10th edition. The National Academies Press; Washington (DC): 1989. Recommended dietary allowances. [DOI] [Google Scholar]
- 13.Rose W.C., Haines W.J., Warner D.T. The amino acid requirements of man. III. The role of isoleucine; additional evidence concerning histidine. J Biol Chem. 2016;193:605–612. [PubMed] [Google Scholar]
- 14.Dinicolantonio J.J. Increase in the intake of refined carbohydrates and sugar may have led to the health decline of the Greenland Eskimos. Open Heart. 2016;3(2):e000444. doi: 10.1136/openhrt-2016-000444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Statistics Canada Health reports. modified 2015 82-003-x 19(1) https://www150.statcan.gc.ca/n1/pub/82-003-x/2008001/article/10463/4149059-eng.htm Available at: Accessed January 10, 2022.
- 16.Schulz R., Slavin J. Perspective: defining carbohydrate quality for human health and environmental sustainability. Adv Nutr. 2021;12:1108–1121. doi: 10.1093/advances/nmab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics Growth charts. centers for disease control and prevention. https://www.cdc.gov/growthcharts/ Available at. Accessed February 22, 2022.
- 18.Romero-Corral A., Somers V.K., Sierra-Johnson J., et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) 2008;32:959–966. doi: 10.1038/ijo.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barry V.W., Baruth M., Beets M.W., et al. Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis. 2014;56(4):382–390. doi: 10.1016/j.pcad.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 20.National Academies of Sciences, Engineering, and Medicine . The National Academies Press; Washington (DC): 2005. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. [DOI] [Google Scholar]
- 21.Vivanti A.P. Origins for the estimations of water requirements in adults. Eur J Clin Nutr. 2012;66:1282–1289. doi: 10.1038/ejcn.2012.157. [DOI] [PubMed] [Google Scholar]
- 22.Bellinger D.C. Lead contamination in flint--an abject failure to protect public health. N Engl J Med. 2016;374:1101–1103. doi: 10.1056/NEJMp1601013. [DOI] [PubMed] [Google Scholar]
- 23.Carlson J.R., Bauer B.A., Vincent A., et al. Reading the tea leaves: anticarcinogenic properties of (-)-epigallocatechin-3-gallate. Mayo Clin Proc. 2007;82:725–732. doi: 10.4065/82.6.725. [DOI] [PubMed] [Google Scholar]
- 24.Basu A., Lucas E.A. Mechanisms and effects of green tea on cardiovascular health. Nutr Rev. 2007;65:361–375. doi: 10.1301/nr.2007.aug.361-375. [DOI] [PubMed] [Google Scholar]
- 25.Wang Z.M., Zhou B., Wang Y.S., et al. Black and green tea consumption and the risk of coronary artery disease: a meta-analysis. Am J Clin Nutr. 2011;93:506–515. doi: 10.3945/ajcn.110.005363. [DOI] [PubMed] [Google Scholar]
- 26.Teramoto M., Muraki I., Yamagishi K., et al. Green tea and coffee consumption and all-cause mortality among persons with and without stroke or myocardial infarction. Stroke. 2021;52:957–965. doi: 10.1161/STROKEAHA.120.032273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miranda A.M., Goulart A.C., Benseñor I.M., et al. Coffee consumption and risk of hypertension: a prospective analysis in the cohort study. Clin Nutr. 2021;40:542–549. doi: 10.1016/j.clnu.2020.05.052. [DOI] [PubMed] [Google Scholar]
- 28.Ding M., Bhupathiraju S.N., Satija A., et al. Long-term coffee consumption and risk of cardiovascular disease: a systematic review and a dose-response meta-analysis of prospective cohort studies. Circulation. 2014;129:643–659. doi: 10.1161/CIRCULATIONAHA.113.005925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Santos R.M., Lima D.R. Coffee consumption, obesity and type 2 diabetes: a mini-review. Eur J Nutr. 2016;55:1345–1358. doi: 10.1007/s00394-016-1206-0. [DOI] [PubMed] [Google Scholar]
- 30.Dong X., Li S., Sun J., et al. Association of coffee, decaffeinated coffee and caffeine intake from coffee with cognitive performance in older adults: national health and nutrition examination survey (NHANES) 2011-2014. Nutrients. 2020;12:840. doi: 10.3390/nu12030840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alicandro G., Tavani A., La Vecchia C. Coffee and cancer risk: a summary overview. Eur J Cancer Prev. 2017;26:424–432. doi: 10.1097/CEJ.0000000000000341. [DOI] [PubMed] [Google Scholar]
- 32.Appel L.J., Moore T.J., Obarzanek E., et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 33.Soedamah-Muthu S.S., Ding E.L., Al-Delaimy W.K., et al. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose–response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011;93:158–171. doi: 10.3945/ajcn.2010.29866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Good Food Institute. U.S Retail market data for the plant-based industry. https://gfi.org/marketresearch/#:∼:text=Plant%2Dbased%20milk%20is%20the,%2C%20growing%2045%25%20since%202019 Available at. Accessed: January 18, 2022.
- 35.Craig W.J., Brothers C.J., Mangels R. Nutritional content and health profile of single-serve non-dairy plant-based beverages. Nutrients. 2021:14162. doi: 10.3390/nu14010162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collard K.M., McCormick D.P. A nutritional comparison of cow's milk and alternative milk products. Acad Pediatr. 2021;21:1067–1069. doi: 10.1016/j.acap.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 37.MyPlate. US Department of Agriculture. https://www.myplate.gov/eat-healthy/fruits Available at:
- 38.Popkin B.M. Patterns of beverage use across the lifecycle. Physiol Behav. 2010;100:4–9. doi: 10.1016/j.physbeh.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malik V.S., Popkin B.M., Bray G.A., et al. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33:2477–2483. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fung T.T., Malik V., Rexrode K.M., et al. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr. 2009;89:1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zafar M.I., Frese M., Mills K.E. Chronic fructose substitution for glucose or sucrose in food or beverages and metabolic outcomes: an updated systematic review and meta-analysis. Front Nutr. 2021;8:647600. doi: 10.3389/fnut.2021.647600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson T., Murray B., Price T., et al. Non-nutritive (Artificial) sweetener knowledge among university students. Nutrients. 2019;11:E2201. doi: 10.3390/nu11092201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mukamal K.J., Jensen M.K., Grønbaek M., et al. Drinking frequency, mediating biomarkers, and risk of myocardial infarction in women and men. Circulation. 2005;112:1406–1413. doi: 10.1161/CIRCULATIONAHA.105.537704. [DOI] [PubMed] [Google Scholar]
- 44.Cao Y., Willett W.C., Rimm E.B., et al. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ. 2015;18:351. doi: 10.1136/bmj.h4238. h4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Willett W.C. In: Preventive nutrition. 5th edition. Bendich A., Deckelbaum R.J., editors. Humana Press, Springer/Nature; New York: 2015. Public health benefits of preventive nutrition: global perspective; pp. 25–46. [Google Scholar]
- 46.Wood A.M., Kaptoge S., Butterworth A.S., et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018;391:1513–1523. doi: 10.1016/S0140-6736(18)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gosdin L.K., Deputy N.P., Kim S.Y., et al. Alcohol consumption and binge drinking during pregnancy among adults aged 18–49 years — United States, 2018–2020. MMWR Morb Mortal Wkly Rep. 2022;71:10–13. doi: 10.15585/mmwr.mm7101a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Institute of Standards and Technology How do you know your food’s nutrition label is accurate? National Institute on Alcohol Abuse and Alcoholism. National Institutes of Health. US Department of Health and Human Services. Rethinking Drinking. http://rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/What-counts-as-a-drink/Whats-A-Standard-Drink.aspx Available at: Accessed: January 7, 2022.
- 49.National Research Council . The National Academies Press; Washington (DC): 1941. Recommended dietary allowances. Available at: [DOI] [Google Scholar]
- 50.National Research Council (U.S) National Academy of Sciences-National Research Council; Washington (DC): 1968. Food and nutrition board. Recommended dietary allowances; a report of the food and nutrition board. [Google Scholar]
- 51.National Research Council . National Academies Press; Washington (DC): 1989. Diet and health: implications for reducing chronic disease risk. Report of the committee on diet and health, food and nutrition board, commission on life sciences; p. 750. [Google Scholar]
- 52.Dietary reference intakes (DRIS): recommended intakes for individuals, food and nutrition board, institute of medicine. National Academies; 2004. [Google Scholar]
- 53.The development of DRIS 1994-2004: lessons learned and new challenges: workshop summary. institute of medicine. The National Academies Press; Washington (DC): 2008. Available at: [DOI] [Google Scholar]
- 54.Mifflin M.D., St Jeor S.T., Hill L.A., et al. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–247. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 55.United States Department of Agriculture . Government Printing Office; Washington (DC): 1980. United States department of health and human services nutrition and your health: dietary guidelines for Americans. [Google Scholar]
- 56.United States Department of Health and Human Services, United States Department of Agriculture Dietary Guidelines for Americans, 2015–2020. Washington (DC): United States Department of Health and Human Services and United States Department of Agriculture; 2015. Contract No.: HHS-ODPHP-2015-2020-01-DGA-A Home and Garden Bulletin No. 232.
- 57.Lee S.H., Moore L.V., Park S., et al. Adults meeting fruit and vegetable intake recommendations-united states, 2019. MMWR Morb Mortal Wkly Rep. 2022;71:1–9. doi: 10.15585/mmwr.mm7101a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim E.J., Ellison B., Prescott M.P., et al. Consumer comprehension of the nutrition facts label: a comparison of the original and updated labels. Am J Health Promot. 2021;35:648–657. doi: 10.1177/0890117120983128. [DOI] [PubMed] [Google Scholar]
- 59.U.S. DEPARTMENT OF AGRICULTURE Food labeling. economic research service. https://www.ers.usda.gov/topics/food-choices-health/consumer-information-and-labeling/food-labeling/#labels Available at: Accessed February 23, 2022.
- 60.Center for Disease Control About the national health and nutrition examination survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm Available at: Accessed January 19, 2022.
- 61.Mignogna C., Costanzo S., Ghulam A., et al. Impact of nationwide lockdowns resulting from the first wave of the COVID-19 pandemic on food intake, eating behaviours and diet quality: a systematic review. Adv Nutr. 2021:nmab130. doi: 10.1093/advances/nmab130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Choi S.L., Men F. Food insecurity associated with higher COVID-19 infection in households with older adults. Public Health. 2021;200:7–14. doi: 10.1016/j.puhe.2021.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dana L.M., Hart E., mcaleese A., et al. Factors associated with ordering food via online meal ordering services. Public Health Nutr. 2021;24:5704–5709. doi: 10.1017/S1368980021001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Keeble M., Adams J., Bishop T.R.P., et al. Socioeconomic inequalities in food outlet access through an online food delivery service in England: A cross-sectional descriptive analysis. Appl Geogr. 2021;133:102498. doi: 10.1016/j.apgeog.2021.102498. j.apgeog.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nguyen N.T., Chinn J., Nahmias J., et al. Outcomes and mortality among adults hospitalized with COVID-19 at US medical centers. JAMA Netw Open. 2021;4:e210417. doi: 10.1001/jamanetworkopen.2021.0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thibault R., Seguin P., Tamion F., et al. Nutrition of the COVID-19 patient in the intensive care unit (ICU): a practical guidance. Crit Care. 2020;24:447. doi: 10.1186/s13054-020-03159-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Defense department will help relieve 2 Minnesota hospitals. https://www.mprnews.org/story/2021/11/17/defense-department-will-help-relieve-2-minnesota-hospitals Available at: Accessed January 6, 2022.
- 68.Wierdsma N.J., Kruizenga H.M., Konings L.A., et al. Poor nutritional status, risk of sarcopenia and nutrition related complaints are prevalent in COVID-19 patients during and after hospital admission. Clin Nutr ESPEN. 2021;43:369–376. doi: 10.1016/j.clnesp.2021.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yisak H., Ewunetei A., Kefale B., et al. Effects of vitamin D on COVID-19 infection and prognosis: a systematic review. Risk Manag Healthc Policy. 2021;14:31–38. doi: 10.2147/RMHP.S291584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cereda G., Ciappolino V., Boscutti A., et al. Zinc as a neuroprotective nutrient for COVID-19-related neuropsychiatric manifestations: a literature review. Adv Nutr. 2021;11:nmab110. doi: 10.1093/advances/nmab110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fiorino S., Gallo C., Zippi M., et al. Cytokine storm in aged people with cov-2: possible role of vitamins as therapy or preventive strategy. Aging Clin Exp Res. 2020;32:2115–2131. doi: 10.1007/s40520-020-01669-y. [DOI] [PMC free article] [PubMed] [Google Scholar]