Abstract
Lobular capillary hemangiomas (LCHs) are a common form of benign vascular tumors originating from the skin and subcutaneous tissues. We have described the case of a 47-year-old man who had presented with a 1-month history of a tender swelling to the right temporal region. Biopsy was performed to rule out temporal arteritis and demonstrated a subset of LCH, now formally known as intravascular LCH. We have described the occurrence of a rare subtype of LCH arising from the intravascular wall of the temporal artery. To the best of our knowledge, this is the only reported case of an intravascular LCH in the Caribbean.
Keywords: Artery, Intravascular lobular capillary hemangioma, Pyogenic granuloma, Temporal artery, Tumor, Vascular
Lobular capillary hemangiomas (LCHs), also often referred to as pyogenic granulomas, represent a well-researched form of benign vascular tumor typically confined to the skin and subcutaneous tissues of the head, neck, and upper extremities.1, 2, 3, 4, 5, 6
LCHs present as solitary, well-circumscribed, smooth, nodules or papules. Histologically, they exhibit a characteristic lobular architecture of unstratified endothelium that manifests as capillaries interspersed among an edematous fibromyxoid stroma.1, 2, 3,5,7 Their occurrence has no predilection for a particular race; however, they have been found slightly more frequently among women, children, and young adults.2,3,5,6 At present, the exact etiology and pathogenesis surrounding LCHs remain undefined, with multiple postulates leaning toward a multifactorial component encompassing both environmental and genetic influences.2,5 One of the major factors suspected of contributing to the pathogenesis of LCHs is related to the concept of a hyperproliferative response to trauma, with imbalances involving both promoters and suppressors of angiogenesis.2, 3, 4, 5, 6, 7 This concept has been supported in the literature, with numerous immunohistochemistry reports outlining the association between LCHs and increased expression of angiogenic markers, including CD31, CD34, smooth muscle actin, and factor VIII.1,2,4
Case report
A 47-year-old man was referred by his general practitioner because of the results from a right temporal artery biopsy performed to rule out temporal arteritis. He had developed a swelling to the right side of the forehead 1 month before his presentation. He had no history of trauma, and he denied any other symptoms. The swelling had not increased in size since its initial discovery. He had a history of hypertension and paroxysmal atrial fibrillation but no history of embolic phenomena. The patient provided written informed consent for the report of his case details and imaging studies.
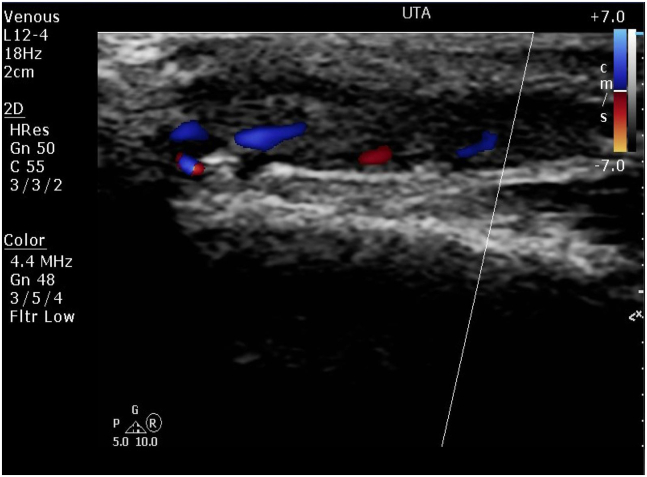
Vascular ultrasound revealed thrombosis of the right temporal artery (Fig 1). The physical examination was significant only for a 2-cm-long by 6-mm-wide soft, nontender swelling to the right temporal region, along the course of the temporal artery, which was palpable proximally and distally to the swelling. The patient underwent biopsy of the swelling, with excision of the 2-cm affected segment of the right temporal artery under local anesthesia, using an incision along the course of the artery, and was subsequently discharged.
Fig 1.
Ultrasound image showing a longitudinal section of the right temporal artery. An echogenic mass can be appreciated within the lumen of the vessel, with some degree of intralesional blood flow through the cribriform spaces.
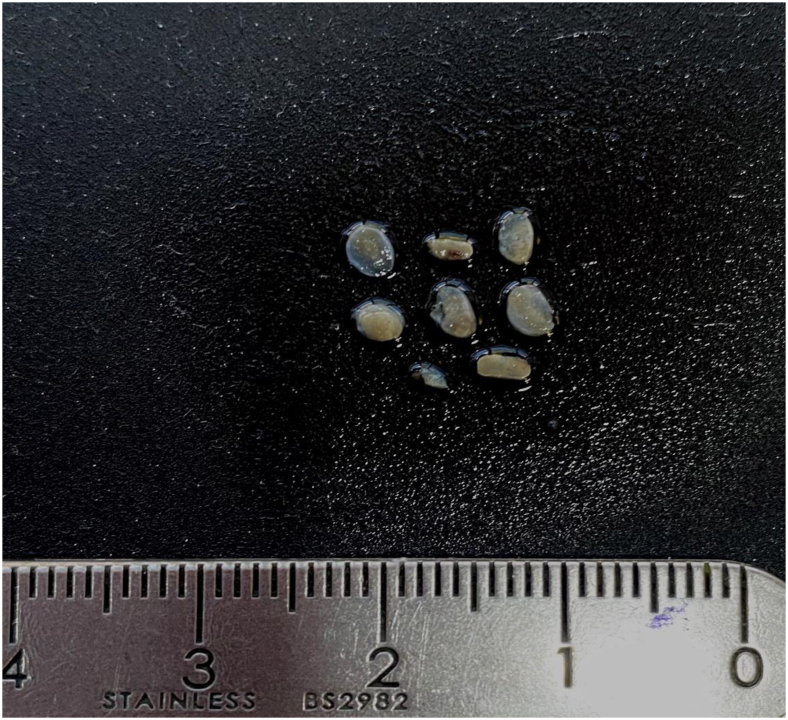
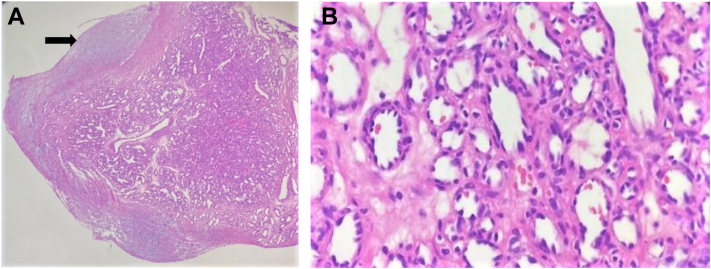
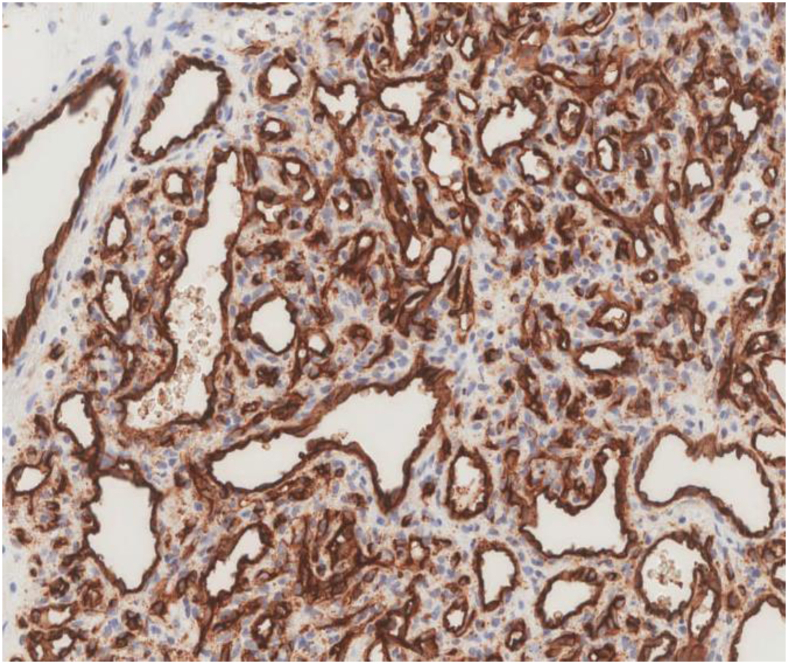
Gross pathologic sectioning of the specimen revealed multiple pieces of tan-gray tissue (Fig 2). Microscopic examination of hematoxylin-eosin–stained sections exhibited a nodular vascular lesion composed of small capillaries arranged in a lobular fashion, and the specimen was diagnosed as an intravascular LCH (Fig 3). The blood investigation results, including measurement of inflammatory markers such as C-reactive protein and the erythrocyte sedimentation rate, were normal. Immunohistochemistry demonstrated strong cytoplasmic positivity for CD31, CD34, and factor VIII (Fig 4).
Fig 2.
Photograph of gross specimen after sectioning revealing multiple pieces of tan-gray tissue.
Fig 3.
A, Photomicrograph of hematoxylin-eosin–stained sections showing a nodular vascular lesion composed of small capillaries arranged in a lobular fashion. The lesion in some parts appeared to be bordered by a vessel wall (black arrow). Fragments of unremarkable vessel walls were also present (original magnification ×40). B, Photomicrograph of vascular channels lined with endothelial cells devoid of atypia and containing occasional erythrocytes (hematoxylin-eosin stain, original magnification ×400).
Fig 4.
Immunohistochemistry exhibited strong diffuse positive cytoplasmic staining for CD31 in lesional cells.
Discussion
In 1979, a case series by Cooper et al7 became the first to officially provide information on a rare subset of these LCHs arising from the vascular lumen of 18 patients.2,3,5, 6, 7 Now formally recognized by the International Society for the Study of Vascular Anomalies as intravascular LCHs (IVLCHs), they represent a very rare entity in the differential diagnosis of vascular pathology, as is evidenced by the paucity of literature surrounding their occurrence.1, 2, 3,5,7
A total of 64 documented cases have been reported since their discovery in 1979.1,3,7 Of these 64 cases, 62 referred to lesions originating from the venous system and 2 referred to lesions arising from an arterial wall.
In 2020, Blaya et al1 described the occurrence of an IVLCH arising from the superior vena cava of a 30-year-old woman. One decade earlier, Maher3 had described a similar occurrence arising from the right external jugular vein of a 41-year-old woman. Six years later, in 2016, Matsuzaki et al4 described an acute presentation of severe right upper extremity edema in a 73-year-old man that was subsequently determined to have resulted from an obstruction to the right subclavian vein secondary to an IVLCH.
Although previous studies have reported vascular tumors arising from the temporal artery, the occurrence of an IVLCH arising within this region has remained a clinical rarity. In 1994, Margo et al8 reported the case of a 27-year-old man who had presented acutely with a tender nodule to the right temporal region, a familiar clinical presentation concerning for temporal arteritis. However, the results from the biopsy provided evidence, not only for the occurrence of a temporal IVLCH, but, more strikingly, also an IVLCH arising from an arterial wall.
To the best of our knowledge, the present case represents only the second occurrence of a temporal IVLCH. More importantly, it encapsulates both an unusual location for vascular tumors and an unusual differential diagnosis regarding temporal artery pathology in general.
Historically, the presence of LCHs has been associated with preexisting cases of trauma, viruses, medications, arteriovenous malformations, and cytogenetic abnormalities.2, 3, 4, 5, 6 We have described the case of a 47-year-old man with hypertension, paroxysmal atrial fibrillation, and an acute tender swelling to the right temporal region. However, our patient reported no significant antecedent events. In addition, similar to the case reported by Margo et al8 in 1994, our case illustrates a challenging clinical presentation because the historical and physical features both proved to be more suggestive of an inflammatory phenomenon than a neoplastic process.
The use of imaging in the diagnostic workup of these swellings, specifically ultrasound, has, in the past, proved to be useful but deceptive, with histopathologic examination the only real method of arriving at a definitive diagnosis.1, 2, 3,5 Nevertheless, the ultrasound features (Fig 1) remained consistent with previously documented cases and are suggestive of an IVLCH. Intralesional vascularity will typically discern IVLCH from thrombosis, with regions of poor echogenicity seen amidst a homogeneous background.3, 4, 5 In addition to vascular ultrasound, various imaging modalities have proved beneficial in the diagnostic workup. Previous reports have outlined the use of magnetic resonance venography as a valuable diagnostic tool.3, 4, 5 However, regardless of whether the features are consistent with thrombus or tumor, surgical resection remains the treatment of choice.1, 2, 3,5
IVLCHs and their development are not known to be associated with thrombosis; however, there are recognized forms of vascular tumors that do share a temporal relationship. Intravascular papillary endothelial hyperplasia, often referred to as a Masson tumor, have historically been suspected to arise from thrombus resolution.7,9 Similarly, only one case of a Masson tumor has been previously documented, which originated from the temporal artery of 75-year-old man in the setting of a suspected superficial temporal artery aneurysm.9
Conclusions
LCHs represent a well-recognized form of benign vascular tumor. The presence of these tumors arising from the vascular system remains an uncommon phenomenon, with only a few cases previously documented.1, 2, 3, 4, 5, 6 Furthermore, with respect to temporal artery pathology, vascular tumors have also been seldom encountered, with reports only pertaining to intravascular papillary endothelial hyperplasia (Masson tumor), epithelioid hemangioendotheliomas, and angiolymphoid hyperplasia with eosinophilia.9 Nevertheless, our case has provided additional evidence regarding an important, albeit rare, entity for the differential diagnosis surrounding temporal artery pathology and, hence, reinforces the need to consider LCHs in the differential diagnosis of superficial swellings. At present, our case represents the only reported presentation of its kind in Barbados and the Caribbean.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Blaya E., Vento V., Kuntz S., Bruyns L., Ohana M., Weingertner N., et al. Intravenous lobular capillary haemangioma (pyogenic granuloma) of the superior vena cava: case report and literature review. EJVES Vasc Forum. 2021;50:32–36. doi: 10.1016/j.ejvsvf.2020.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou H., Zhang J., Yang P., Jiang L., Zhang Y., Wang H., et al. Intravenous lobular capillary hemangioma: report of a case and review of literature. Int J Clin Exp Pathol. 2016;9:6397–6401. [Google Scholar]
- 3.Maher A. Intravenous lobular capillary hemangioma. Ann Vasc Surg. 2010;24:951.e13–951.e15. doi: 10.1016/j.avsg.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Matsuzaki K., Yuki I., Masayoshi O., Tomomi N., Akihiko I., Taisuke K., et al. Intravenous lobular capillary hemangioma in the subclavian vein. Ann Thorac Surg. 2016;102:427–429. doi: 10.1016/j.athoracsur.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Pradhan S., Bazan H., Salem R., Gusberg R.J. Intravenous lobular capillary hemangioma originating in the iliac veins: a case report. J Vasc Surg. 2008;47:1346–1349. doi: 10.1016/j.jvs.2008.01.049. [DOI] [PubMed] [Google Scholar]
- 6.Gummerer M. Case report: intravenous capillary haemangioma, a cause of painless palpable mass in the forearm. Dermatol Case Rep. 2020;5:161. [Google Scholar]
- 7.Cooper P.H., McAllister H.A., Helwig E.B. Intravenous pyogenic granuloma: a study of 18 cases. Am J Surg Pathol. 1979;3:221–228. doi: 10.1097/00000478-197906000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Margo C.E. Intravascular hemangioma of the temporal artery. Arch Ophthalmol. 1994;112:1024. doi: 10.1001/archopht.1994.01090200026011. [DOI] [PubMed] [Google Scholar]
- 9.Chapman S., Peter C., Zak W., Scaife M., Murdoch G., Eslami M.H. Masson tumor (intravascular papillary endothelial hyperplasia) arising in a superficial temporal artery aneurysm. J Vasc Surg Cases Innov Techn. 2019;5:388–391. doi: 10.1016/j.jvscit.2019.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]