Abstract
Background
The COVID-19 pandemic has negatively impacted psychosocial well-being and mental health of students across the world. Although students are vulnerable to depression and suicidal ideation, few studies have been conducted in Uganda. This study aimed to determine the prevalence of depression and suicidal ideation, and associated factors among undergraduate university students in Uganda.
Methods
A cross-sectional study was conducted among undergraduates [N = 540; 363 males; mean age = 23.3 (± 2.64) years] recruited from four universities using an online questionnaire that explored sociodemographic factors, depression, and other associated factors. The Patient Health Questionnaire (PHQ-9) was used to assess depression, and Item 9 was used to assess suicidal ideation in the past 2 weeks. Multivariable logistic regression analyses were performed to determine the factors associated with depression and suicidal ideation.
Results
The prevalence of moderate to severe depression was 20% (n = 108) (cut-off: 10/27 based on the PHQ-9), and the prevalence of past-2-week suicidal ideation was 13.89% (n = 75) (cut-off: 1/3 based on the PHQ-9 Item 9). About half of the individuals who screened positive for depression had suicidal ideation. Factors associated with depression were: having relationship issues [adjusted odds ratio (aOR) = 1.79, 95% confidence interval (CI) = 1.13–2.81, p = 0.012], and having a history of sexual abuse (aOR = 2.06, 95% CI = 1.10–3.84, p = 0.023). Factors associated with reducing the risk of depression were: satisfaction with current academic performance (aOR = 0.50, 95% CI = 0.32–0.79, p = 0.003), and being in the fifth year of academic study (aOR = 0.16, 95% CI = 0.03–0.73, p = 0.018). Factors associated with suicidal ideation were: smoking cigarettes and/or marijuana (aOR = 4.83, 95% CI = 1.10–21.12, p = 0.037), and having financial tuition constraints (aOR = 1.85, 95% CI = 1.08–3.16, p = 0.024), However, satisfaction with current academic performance reduced the likelihood of suicidal ideation (aOR = 0.40, 95% CI = 0.23–0.70, p = 0.001).
Conclusion
Approximately one-fifth of undergraduate university students were moderately to severely depressed, especially those who had relationship issues and those with a history of sexual abuse. Suicidal ideation was common among smokers and those having financial tuition constraints. Therefore, it is recommended that the university authorities implement measures to provide psychological support for the students with problems concerning financial tuition constraints, relationships, and sexual abuse. Also, all students with depression should be screened for suicidality.
Keywords: depression, university students, sexual abuse, academic satisfaction, COVID-19, suicidal ideation
Introduction
Depression is a mental health disorder characterized by extreme sadness, feelings of emptiness, and/or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function (1). Globally, depression affects nearly 280 million people and can lead to a profound effect on all aspects of life, including a lower performance at school, poorer productivity at work, compromised relationships with family and friends, and lower ability to participate in the community (2). It was reported that Africa alone had 29.19 million cases of depression, accounting for 9% of the global depression burden (3). In Uganda, the general population prevalence was reported to be 4.6% (3). The prevalence of depression among university students in Uganda has ranged between 4.0 and 80.7% (4–7). The prevalence of depression in Uganda has been much higher among students during the coronavirus disease 2019 (COVID-19) pandemic (4) and a period characterized by marked psychological stressors and suicidality among students (8–12).
Various factors have been associated with the increased prevalence of depression among university students during the COVID-19 pandemic, including being female, precariousness, previous history of psychiatric illness, social isolation, COVID-19 illness, symptoms compatible with COVID-19, low quality of social relationships, low quality of COVID-19 information received, being a student aged 18–24 years, difficulties with paying for tuition fees prior to the pandemic, increased use of social media, internet use disorder, lack of physical activities/exercise, fear of COVID-19, poverty, and substance abuse (4, 13–16). In addition to COVID-19-related factors, several other factors have been associated with depression, including unhappy interpersonal relationships, chronic physical medical illnesses, chronic mental illnesses, low self-esteem, poor academic performance, family history of mental illness, financial constraints, insecurity at places of residence, smartphone addiction, being single, and the negative perception of the students of their learning environment (17–24). The effects of depression among students vary from mild effects such as poor academic performance (25) to very extreme events such as suicidal behaviors (9, 26–28). Previous studies have shown university students in Uganda to be at high risk of depression during the COVID-19 pandemic due to factors such as burnout, anxiety, and stress (4, 29), and such mood disorders also contribute to the increased risk of suicidal ideation (8).
Despite the introduction of peer support systems at the universities in Uganda, the prevalence of depression increased from 4.0% in 2002 to 21.5 in 2019 and 80.7% in 2020 during the first wave of the COVID-19 pandemic (4, 6, 7). This marked increase in the prevalence of depression over the years, especially during the COVID-19 pandemic, makes understanding depression among university students paramount, especially as the COVID-19 pandemic continues. Therefore, to have a better understanding of depression and suicidal ideation among students during the COVID-19 pandemic, a study among four universities in south-western Uganda was conducted during the second wave of the COVID-19 pandemic.
Materials and Methods
Study Design and Settings
This was a cross-sectional survey conducted among undergraduate university students between May 2021 and September 2021 in south-western Uganda. Participants were recruited using the convenience sampling method incorporating snowball sampling with the assistance of class coordinators and faculty representatives from the four universities: Bishop Stuart University (BSU), Kampala International University—western Uganda campus (KIU), Mbarara University of Science and Technology (MUST), and Kabale University (KU). BSU is located in Mbarara City (western Uganda) with approximately 5,800 students. KIU is located 60 km from Mbarara city with approximately 17,000 students. MUST is located in Mbarara City with approximately 4,260 students. KU is located in Kabale (in extreme south-western Uganda) with approximately 3,000 students.
Inclusion and Exclusion Criteria
The study included students in KIU, BSU, KU, and MUST, aged 18 years or above during the academic year of 2019/2020, who agreed to take part in the study.
Sample Size Calculation
Using Epi Info StatCalc for Population Surveys (Version 7.2.5.0), a population size of 30,000 undergraduate university students was used to calculate the minimum sample size required to produce statistical power of 80%. The expected frequency of depression was at 21.5% among university students (medical students) before the COVID-19 pandemic (6) at an acceptable margin of error of 5% and a design effect of 1.0. The minimum calculated sample size was 257.
Study Measures and Procedure
The online survey (hosted on Google Forms) was pretested with Makerere University students, and then used for data collection from the four study sites. Students were recruited to participate using closed students’ WhatsApp groups and student email addresses with a weblink to the survey. Initially, approximately 100 students from each university (including student leaders) were invited to participate (convenience sampling). They were also asked to distribute the questionnaire among their peers in the four universities (snowball sampling). The online questionnaire collected information concerning socio-demographic characteristics of the participants and assessed depression using the nine-item Patient Health Questionnaire (PHQ-9).
Basic Information of the Participants
Data were collected including participant age (years), gender (male or female), marital status (single, cohabiting, married, and separated/divorced), religion (Christian, Muslim, none), the university they were studying (BSU, KIU, MUST, KU), and type of living residence while at the university (home, hostel, rented house, university hall or other). In addition, academic information was collected, including college or faculty, the year of study, university tuition fee sponsor [private, government, non-government organization (NGO), loan scheme, or other], and whether the student was satisfied with their most recent academic grades. Using dichotomous (yes/no) questions, participants were also asked if they had difficulty paying tuition fees, relationship problems, and history of physical and/or sexual abuse. Similarly, data concerning health factors were obtained, such as a history of mental illness or chronic medical conditions (e.g., diabetes, hypertension, asthma, HIV, etc.), and a history of substance use (cigarette/marijuana smoking, alcohol drinking).
Patient Health Questionnaire
Depression symptoms were assessed using the nine-item Patient Health Questionnaire (PHQ-9). Self-reported items are rated on a four-point scale ranging from 0 to 4. Each item has a discrete response such as 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. This instrument has been internationally accepted in screening for depressive symptoms with excellent psychometric properties (30, 31). In a Ugandan setting, the PHQ-9 has also been found to have excellent psychometric properties (32–34). At a cut-off of 10, it has high specificity (85%) and high sensitivity (88%) in detecting depression based on a meta-analysis by Levis et al. (31). The PHQ-9 has been used with university students in both Uganda (6) and south-western Uganda, therefore, its questions are culturally appropriate since the instrument had good internal reliability (35, 36). In addition, the instrument has been validated for online use (37). The PHQ-9 also categorizes depression in terms of severity. More specifically, 1–4 = minimal depression, 5–9 = mild depression, 10–14 = moderate depression, 15–19 = moderately severe depression, and 20–27 = severe depression (38). A cut-off score of 10 was used to determine whether participants had depressive symptoms or not. In addition, a score of one and above on Item 9, was used to indicate the presence of suicidal ideation in the past 2 weeks. In the present study, the Cronbach alpha was 0.85 for the PHQ-9.
Ethical Consideration
The present study was conducted in accordance with the Declaration of Helsinki 2013 and was approved by the Mbarara University of Science and Technology research ethics committee (MUSTREC #16/02-21). The Dean of Students at each of the four universities gave permission for data collection. Voluntary written informed consent was obtained from all participants.
Statistical Analysis
STATA version 16.0 was used for data analysis. Means and standard deviations were used to summarize continuous variables that were not normally distributed, while percentages and frequencies were used to summarize categorical variables. Student’s t-tests and chi-square tests were performed to identify differences between depression and suicidal ideation, and independent study variables. Logistic regression analysis was used to determine the variables’ association with depression and suicidal ideation. Two separate logistic regressions were conducted to determine the factors associated with depression and suicidal ideation. Factors significant at bivariate logistic regression were tested for collinearity, and those with a variance inflation factor (VIF) of less than 3 were included in a back stepwise multivariate logistic regression model. A p < 0.05 for the significance level was considered at a 95% CI.
Results
Participants
A total of 540 students were included in the final analysis. The age of the participants ranged from 18 to 40 years, with a mean of 23.3 (SD ± 2.64) years. Most of the participants were male (67.22%), and the largest number of participants were from MUST (51.48%). About half of the students were satisfied with their academic performance (48.52%) and 38.15% had difficulty paying university tuition fees (Table 1).
TABLE 1.
Distribution of the studied factors with depression and suicidal ideation (N = 540).
| Variable | n (%) | No depression (n = 432, 80%) | Depression (n = 108, 20%) | χ2 (p-value) | No suicidal ideation (n = 465, 86.11%) | Suicidal ideation (n = 75, 13.89%) | χ2 (p-value) |
| Age (mean ± SD) | 23.3 (2.64) | 23.38 ± 2.75 | 22.98 ± 2.16 | 1.40 (0.162) | 23.41 ± 2.74 | 22.61 ± 1.77 | –2.43 (0.015) |
| Sex | |||||||
| Female | 177 (32.78) | 138 (77.79) | 39 (22.03) | 0.68 (0.409) | 149 (84.18) | 28 (15.82) | 0.82 (0.365) |
| Male | 363 (67.22) | 294 (80.99) | 69 (19.01) | 316 (87.05) | 47 (12.95) | ||
| Current university | |||||||
| BSU | 59 (10.93) | 47 (79.66) | 12 (20.34) | 0.81 (0.847) | 46 (77.97) | 13 (22.03) | 3.96 (0.266) |
| KIU | 127 (23.52) | 102 (80.31) | 25 (19.69) | 112 (88.19) | 15 (11.81) | ||
| MUST | 278 (51.48) | 225 (80.94) | 53 (19.06) | 242 (87.05) | 36 (12.95) | ||
| KU | 76 (14.07) | 58 (76.32) | 18 (23.68) | 65 (85.53) | 11 (14.47) | ||
| Religion | |||||||
| Christian | 500 (92.59) | 398 (76.60) | 102 (20.40) | 0.76 (0.682) | 430 (86.00) | 70 (14.00) | 0.34 (0.844) |
| Muslim | 35 (6.48) | 30 (85.71) | 5 (14.29) | 31 (88.57) | 4 (11.43) | ||
| None | 5 (0.93) | 4 (80.00) | 1 (20.00) | 4 (80.00) | 1 (20.00) | ||
| Sponsor | |||||||
| Government | 107 (19.81) | 89 (83.18) | 18 (16.82) | 4.33 (0.363) | 97 (90.65) | 10 (9.35) | 5.12 (0.275) |
| Loan scheme | 96 (17.78) | 70 (72.92) | 26 (27.08) | 84 (87.50) | 12 (12.50) | ||
| NGO | 18 (3.33) | 14 (77.78) | 4 (22.22) | 14 (77.78) | 4 (22.22) | ||
| Private | 288 (53.33) | 235 (81.60) | 53 (18.40) | 246 (85.42) | 42 (14.58) | ||
| Others | 31 (5.74) | 24 (77.42) | 7 (22.58) | 24 (77.43) | 7 (22.58) | ||
| Area of residence | |||||||
| Home | 35 (6.48) | 30 (85.71) | 5 (14.29) | 3.20 (0.525) | 27 (77.14) | 8 (22.86) | 2.77 (0.596) |
| Hostel | 204 (37.78) | 168 (82.35) | 36 (17.65) | 177 (86.76) | 27 (13.24) | ||
| Rentals | 250 (46.30) | 192 (76.80) | 58 (23.20) | 216 (86.40) | 34 (13.60) | ||
| University hall | 45 (8.33) | 37 (82.22) | 8 (17.78) | 40 (88.89) | 5 (11.11) | ||
| Others | 6 (1.11) | 5 (83.33) | 1 (16.67) | 5 (83.33) | 1 (16.67) | ||
| Marital status | |||||||
| Single | 497 (92.04) | 396 (79.68) | 101 (20.32) | 0.73 (0.695) | 427 (85.92) | 70 (14.08) | 0.55 (0.758) |
| Co-habiting | 20 (3.70) | 16 (80.00) | 4 (20.00) | 17 (85.00) | 3 (15.00) | ||
| Married | 23 (4.26) | 20 (86.98) | 3 (13.04) | 21 (91.30) | 2 (8.70) | ||
| College/faculty | |||||||
| Agriculture and environment sciences | 7 (1.30) | 5 (71.43) | 2 (28.57) | 19.53 (0.012) | 6 (85.71) | 1 (14.29) | 19.56 (0.012) |
| Business and management sciences | 27 (5.00) | 22 (81.48) | 5 (18.52) | 24 (88.89) | 3 (11.11) | ||
| Computing and information science | 10 (1.85) | 5 (50.00) | 5 (50.00) | 6 (60.00) | 4 (40.00) | ||
| Education and External Studies | 43 (7.96) | 32 (74.42) | 11 (25.58) | 34 (79.07) | 9 (20.93) | ||
| Engineering, designing, art, and technology | 34 (6.30) | 23 (67.65) | 11 (32.35) | 27 (79.41) | 7 (20.59) | ||
| Health sciences/Medicine | 322 (59.63) | 272 (84.47) | 50 (15.53) | 291 (90.37) | 31 (9.63) | ||
| Humanities and social sciences | 6 (1.11) | 3 (50.00) | 3 (50.00) | 4 (66.67) | 2 (33.33) | ||
| Law | 11 (2.04) | 10 (90.91) | 1 (9.09) | 10 (90.91) | 1 (9.09) | ||
| Others | 80 (14.81) | 60 (75.00) | 20 (25.00) | 63 (78.75) | 17 (21.25) | ||
| Year of study | |||||||
| First | 78 (14.44) | 57 (73.08) | 21 (26.92) | 14.24 (0.014) | 64 (82.05) | 14 (17.95) | 10.44 (0.064) |
| Second | 165 (30.56) | 125 (75.76) | 40 (24.24) | 135 (81.82) | 30 (18.18) | ||
| Third | 143 (26.48) | 113 (79.02) | 30 (20.98) | 124 (86.71) | 19 (13.29) | ||
| Fourth | 96 (17.78) | 82 (85.42) | 14 (14.58) | 86 (89.58) | 10 (10.42) | ||
| Fifth | 49 (9.07) | 47 (95.92) | 2 (4.08) | 48 (97.96) | 1 (2.04) | ||
| Sixth | 9 (1.67) | 8 (88.89) | 1 (11.11) | 8 (88.89) | 1 (11.11) | ||
| Smoking cigarette/marijuana | |||||||
| No | 529 (97.96) | 424 (80.15) | 105 (19.85) | 0.37 (0.542) | 458 (86.58) | 71 (13.42) | 4.74 (0.029) |
| Yes | 11 (2.04) | 8 (72.73) | 3 (27.27) | 7 (63.64) | 4 (36.36) | ||
| Drinking alcohol | |||||||
| No | 394 (72.96) | 317 (80.46) | 77 (19.54) | 0.19 (0.663) | 344 (87.31) | 50 (12.69) | 1.75 (0.186) |
| Yes | 146 (27.04) | 115 (78.77) | 31 (21.23) | 121 (82.88) | 25 (17.12) | ||
| Had relationship issues | |||||||
| No | 266 (49.26) | 228 (85.71) | 38 (14.29) | 10.70 (0.001) | 237 (89.01) | 29 (10.90) | 3.91 (0.048) |
| Yes | 274 (50.74) | 204 (74.45) | 70 (25.55) | 228 (83.21) | 46 (16.79) | ||
| Had tuition constraints | |||||||
| No | 334 (61.85) | 279 (83.53) | 55 (16.47) | 6.83 (0.009) | 298 (89.22) | 36 (10.78) | 7.08 (0.008) |
| Yes | 206 (38.15) | 153 (74.27) | 53 (25.73) | 167 (81.07) | 39 (18.93) | ||
| Satisfied academic performance | |||||||
| No | 278 (51.48) | 205 (73.74) | 73 (26.26) | 14.03 (< 0.001) | 224 (80.58) | 54 (19.42) | 14.68 (< 0.001) |
| Yes | 262 (48.52) | 227 (86.64) | 35 (13.36) | 241 (91.98) | 21 (8.02) | ||
| Been sexually abused | |||||||
| No | 483 (89.44) | 395 (81.76) | 88 (18.22) | 9.07 (0.003) | 421 (97.16) | 62 (12.84) | 4.24 (0.040) |
| Yes | 57 (10.56) | 37 (64.91) | 20 (35.09) | 44 (77.19) | 13 (22.81) | ||
| Been involved in physical fighting | |||||||
| No | 467 (86.48) | 375 (80.30) | 92 (19.70) | 0.19 (0.660) | 405 (86.72) | 62 (13.28) | 1,08 (0.298) |
| Yes | 73 (13.52) | 57 (78.08) | 16 (21.92) | 60 (82.19) | 13 (17.81) | ||
| Been managed for any mental health issues | |||||||
| No | 505 (93.52) | 408 (80.79) | 97 (19.21) | 3.06 (0.080) | 435 (86.14) | 70 (13.86) | 0.01 (0.944) |
| Yes | 35 (6.48) | 24 (68.57) | 11 (31.43) | 30 (85.71) | 5 (14.29) | ||
| Had a serious medical condition | |||||||
| No | 506 (93.70) | 408 (80.63) | 98 (19.37) | 2.01 (0.156) | 439 (86.76) | 67 (13.24) | 2.82 (0.093) |
| Yes | 34 (6.30) | 24 (70.59) | 10 (29.41) | 26 (76.47) | 8 (23.53) | ||
Prevalence of Depression and Suicidal Ideation
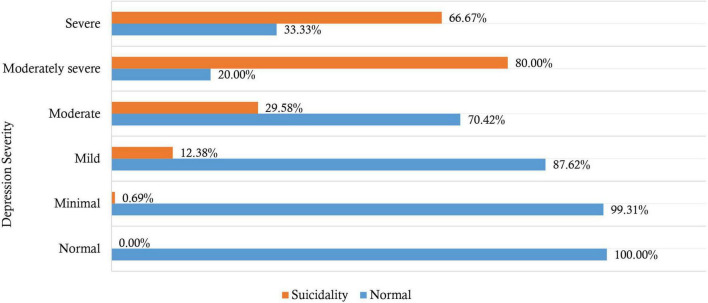
Approximately 20% (95% CI: 16.71–23.63) of the students had depression based on the PHQ-9 cut-off score of 10 out of 27. The median depression symptoms score was 5 [interquartile range (IQR) = 7]. The severity of depression symptoms was: minimal (26.67%, n = 144/540), mild (37.41%, n = 202/540), moderate (13.15%, n = 71/540), moderately severe (4.63%, n = 25/540), and severe depression (2.22%, n = 12/540). However, 15.93% (n = 86/540) had no symptoms of depression (Figure 1).
FIGURE 1.
Severity of depression and suicide ideation among Ugandan University students.
A total of 75 students (13.89%) reported suicidal ideation based on a score of one and above on Item 9 of the PHQ-9. Moreover, 10.37% had thoughts of suicide for several days in the past 2 weeks (n = 56), 1.30% had suicidal thoughts for more than half the days in the past 2 weeks (n = 7), and 2.22% had thoughts of suicide nearly every day in the past 2 weeks (n = 12). Among individuals who scored positive for depression (at a cut-off of 10), 45.37% reported suicidal ideation (n = 49/108). However, 6.02% of individuals reporting suicidal ideation screened negative for depression (n = 26/75). There was statistically significant difference between severity of depression and having suicidal ideation (χ2 = 169.14, p < 0.001). Suicidal ideation was higher among students with moderately severe depression symptoms (80.00%), followed by severe depression (66.67%) (Figure 1).
Relationship Between Depression and Other Variables
Depression (at a cut-off of 10) was significantly higher among students who (i) had relationship difficulties than those who did not (25.55% vs. 14.29%, χ2 = 10.70, p < 0.001); (ii) had difficulty in paying tuition fees than those who did not (25.73% vs. 16.47%, χ2 = 6.83, p = 0.009); (iii) had experienced sexual abuse than those who had not (35.09% vs. 18.22%, χ2 = 9.07, p = 0.003); and (iv) were from humanities and social sciences, and computer sciences and information sciences than those from other faculties (χ2 = 19.53, p = 0.012). Depression (at a cut-off of 10) was significantly lower among (i) fifth-year university students compared to other years of study (χ2 = 14.24, p = 0.014), and (ii) those satisfied with their current academic performance than those who were not (13.36% vs. 26.26%, χ2 = 14.03, p < 0.001) (Table 1).
Relationship Between Suicidal Ideation and Other Variables
The mean age of individuals reporting suicidal ideation was significantly less than those without suicidality (22.61 ± 1.77 vs. 23.41 ± 2.74, t = -2.43, p = 0.015). Suicidal ideation was significantly higher among students who (i) smoked cigarettes and/or marijuana (36.36% vs. 13.42%, χ2 = 4.74, p = 0.029); (ii) had relationship difficulties (16.79% vs. 10.90%, χ2 = 3.91, p = 0.048); (iii) had difficulty in paying university tuition fees (18.93% vs. 10.78%, χ2 = 7.08, p = 0.008); and (iv) had experienced sexual abuse (22.81% vs. 12.84%, χ2 = 4.24, p = 0.040). Suicidal ideation was significantly lower among those satisfied with their current academic performance (8.02% vs. 19.42%, χ2 = 14.68, p < 0.001) (Table 1).
Factors Associated With Depression
Table 2 shows the results of the bivariate analysis. The likelihood of depression was reduced among those (i) in the fourth and fifth year of academic study and (ii) satisfied with their current academic performance. On the other hand, the likelihood of depression was increased among those who had (i) relationship problems, (ii) difficulty paying their university tuition fees, and (iii) a history of sexual abuse. These factors were tested for collinearity, and they all had VIFs below 3, with a mean VIF of 1.04. Consequently, they were included in the final model using the backward stepwise selection method. The model had a sensitivity of 6.64%, specificity of 98.84%, a positive predictive value of 58.33%, a negative predictive value of 80.87%, and correctly classified 80.37% of depression. The goodness-of-fit p-value was 0.632, for the included five variables (Table 2).
TABLE 2.
Bivariate logistic regression analysis of factors associated with depression and suicidal ideation.
| Variable | Depression |
Suicidal ideation |
||
| Crude odds ratio (95% CI) | p-value | Crude odds ratio (95% CI) | p-value | |
| Age | 0.94 (0.86–1.03) | 0.163 | 0.86 (0.76-0.97) | 0.014 |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 0.83 (0.53–1.29) | 0.410 | 0.83 (0.48-1.31) | 0.366 |
| Current university | ||||
| BSU | 1 | 1 | ||
| KIU | 0.96 (0.44–2.07) | 0.917 | 0.47 (0.21-1.07) | 0.074 |
| MUST | 0.92 (0.46–1.86) | 0.822 | 0.53 (0.26-1.07) | 0.076 |
| KU | 1.22 (0.53–2.78) | 0.643 | 0.60 (0.25-1.45) | 0.257 |
| Religion | ||||
| Christian | 1 | 1 | ||
| Moslem | 0.65 (0.25–1.72) | 0.385 | 0.79 (0.27-2.31) | 0.671 |
| None | 0.98 (0.11–8.82) | 0.982 | 1.53 (0.17-13.94) | 0.703 |
| Sponsor | ||||
| Government | 1 | 1 | ||
| Loan scheme | 1.84 (0.93–3.62) | 0.079 | 1.39 (0.57-3.37) | 0.472 |
| NGO | 1.41 (0.42–4.79) | 0.579 | 2.77 (0.76-10.05) | 0.121 |
| Private | 1.12 (0.62–2.01) | 0.716 | 2.83 (0.98-8.20) | 0.055 |
| Others | 1.44 (0.54–3.85) | 0.465 | 1.66 (0.80-3.43) | 0.175 |
| Area of residence | ||||
| Home | 1 | 1 | ||
| Hostel | 1.29 (0.47–3.54) | 0.627 | 0.51 (0.21-1.25) | 0.142 |
| Rentals | 1.81 (0.67–4.88) | 0.240 | 0.53 (0.22-1.26) | 0.153 |
| University hall | 1.30 (0.38–4.38) | 0.675 | 0.42 (0.13-1.43) | 0.165 |
| Others | 1.20 (0.11–12.54) | 0.879 | 0.67 (0.07-6.65) | 0.736 |
| Marital status | ||||
| Single | 1 | 1 | ||
| Co-habiting | 0.98 (0.32–3.00) | 0.972 | 1.08 (0.31-3.77) | 0.908 |
| Married | 0.59 (0.17–2.02) | 0.399 | 0.58 (0.13-2.53) | 0.470 |
| College/faculty | ||||
| Agriculture and environment sciences | 1 | 1 | ||
| Business and Management sciences | 0.57 (0.08–3.82) | 0.561 | 0.75 (0.07-8.55) | 0.817 |
| Computing and information science | 2.50 (0.32–19.53) | 0.382 | 4.00 (0.34-47.11) | 0.271 |
| Education and external studies | 0.86 (0.15–5.08) | 0.867 | 1.59 (0.17-14.93) | 0.686 |
| Engineering, designing, art, and technology | 1.20 (0.20 -7.16) | 0.845 | 1.56 (0.16-15.12) | 0.703 |
| Health sciences/Medicine | 0.46 (0.09–2.43) | 0.361 | 0.64 (0.07-5.48) | 0.683 |
| Humanities and social sciences | 2.50 (0.25–24.72) | 0.433 | 3.00 (0.20-45.24) | 0.427 |
| Law | 0.25 (0.02–3.47) | 0.301 | 0.60 (0.03-11.47) | 0.734 |
| Others | 0.83 (0.15–4.64) | 0.835 | 1.62 (0.18-14.38) | 0.665 |
| Year of study | ||||
| First | 1 | 1 | ||
| Second | 0.87 (0.47–1.61) | 0.653 | 1.01 (0.50-2.05) | 0.965 |
| Third | 0.72 (0.38–1.37) | 0.317 | 0.70 (0.33-1.49) | 0.354 |
| Fourth | 0.46 (0.22–0.99) | 0.046 | 0.53 (0.22-1.27) | 0.156 |
| Fifth | 0.12 (0.03–0.52) | 0.005 | 0.09 (0.01-0.75) | 0.025 |
| Sixth | 0.34 (0.04–2.88) | 0.322 | 0.57 (0.07-4.94) | 0.611 |
| Smoking cigarette/marijuana | ||||
| No | 1 | 1 | ||
| Yes | 1.51 (0.39–5.81) | 0.545 | 3.69 (1.05-12.91) | 0.041 |
| Drinking alcohol | ||||
| No | 1 | 1 | ||
| Yes | 1.11 (0.69–1.77) | 0.663 | 1.42 (0.84-2.40) | 0.187 |
| Had relationship issues | ||||
| No | 1 | 1 | ||
| Yes | 2.06 (1.33–3.19) | < 0.001 | 1.65 (1.00-2.72) | 0.050 |
| Had tuition constraints | ||||
| No | 1 | 1 | ||
| Yes | 1.76 (1.15–2.69) | 0.009 | 1.93 (1.18-3.16) | 0.009 |
| Satisfied with academic performance | ||||
| No | 1 | 1 | ||
| Yes | 0.43 (0.28–0.68) | < 0.001 | 0.36 (0.21-0.62) | < 0.001 |
| Been sexually abused | ||||
| No | 1 | 1 | ||
| Yes | 2.43 (1.34–4.38) | 0.003 | 2.01 (1.02-3.94) | 0.043 |
| Been involved in physical fighting | ||||
| No | 1 | 1 | ||
| Yes | 1.14 (0.63–2.08) | 0.660 | 1.41 (0.73-2.73) | 0.300 |
| Been managed for any mental health issues | ||||
| No | 1 | 1 | ||
| Yes | 1.93 (0.91–4.07) | 0.085 | 1.04 (0.39-2.76) | 0.944 |
| Had serious medical condition | ||||
| No | 1 | 1 | ||
| Yes | 1.73 (0.80–3.75) | 0.161 | 2.02 (0.88-4.64) | 0.099 |
In the multivariable analysis, the factors associated with depression were having relationship problems (AOR = 1.79, 95% CI = 1.13–2.81, p = 0.012), and having a history of sexual abuse (AOR = 2.06, 95% CI = 1.10–3.84, p = 0.023). Being satisfied with current academic performance (AOR = 0.50, 95% CI = 0.32–0.79, p = 0.003), and being in the fifth year of academic study (AOR = 0.16, 95% CI = 0.03–0.73, p = 0.018) reduced the likelihood of having depression (Table 3).
TABLE 3.
Multivariate logistic regression analysis of factors associated with depression and suicidal ideation.
| Variable | Depression |
Suicidal ideation |
||
| Adjusted odds ratio (95% CI) | p-value | Adjusted odds ratio (95% CI) | p-value | |
| Age | 0.88 (0.77-1.01) | 0.061 | ||
| Year of study | ||||
| First | 1 | 1 | ||
| Second | 0.89 (0.47–1.69) | 0.721 | 1.29 (0.61-2.74) | 0.503 |
| Third | 0.78 (0.40–1.53) | 0.470 | 1.07 (0.47-2.44) | 0.872 |
| Fourth | 0.53 (0.24–1.17) | 0.116 | 0.88 (0.33-2.33) | 0.797 |
| Fifth | 0.16 (0.03–0.73) | 0.018 | 0.20 (0.02-1.72) | 0.142 |
| Sixth | 0.36 (0.04–3.34) | 0.372 | 1.49 (0.14-15.23) | 0.737 |
| Smoking cigarettes and/or marijuana | ||||
| No | 1 | |||
| Yes | 4.83 (1.10-21.12) | 0.037 | ||
| Had relationship issues | ||||
| No | 1 | |||
| Yes | 1.79 (1.13–2.81) | 0.012 | ||
| Had tuition constraints | ||||
| No | 1 | 1 | ||
| Yes | 1.34 (0.85–2.11) | 0.204 | 1.85 (1.08-3.16) | 0.024 |
| Satisfied with academic performance | ||||
| No | 1 | 1 | ||
| Yes | 0.50 (0.32–0.79) | 0.003 | 0.40 (0.23-0.70) | 0.001 |
| Been sexually abused | ||||
| No | 1 | 1 | ||
| Yes | 2.06 (1.10–3.84) | 0.023 | 1.47 (0.69-3.11) | 0.314 |
Factors Associated With Suicidal Ideation
The likelihood of suicidal ideation was significantly lower among those (i) in the fifth year of academic study, (ii) satisfied with their current academic performance, and (iii) those who were older. On the other hand, the likelihood of suicidal ideation increased among those who had (i) difficulty paying their university tuition fees, (ii) a history of smoking cigarettes and/or marijuana, and (iii) a history of sexual abuse. These factors were tested for collinearity, and they all had VIFs below 3, with a mean VIF of 1.11. Consequently, they were included in the final model using the backward stepwise selection method. The model had a sensitivity of 4.00%, specificity of 100%, a positive predictive value of 100%, a negative predictive value of 86.59%, and correctly classified 86.67% of depression. The goodness-of-fit p-value was 0.934 for the included six variables (Table 2).
In the multivariable analysis, smoking cigarettes and/or marijuana (aOR = 4.83, 95% CI = 1.10–21.12, p = 0.037), and having financial tuition constraints (aOR = 1.85, 95% CI = 1.08–3.16, p = 0.024) increased the likelihood of having suicidal ideation. However, satisfaction with current academic performance reduced the likelihood of having suicidal ideation (aOR = 0.40, 95% CI = 0.23–0.70, p = 0.001) (Table 3).
Discussion
In the present cross-sectional study, students from four universities in south-western Uganda during the COVID-19 pandemic were surveyed, and the prevalence of depression (at a cut-off of 10) was 20% and suicidal ideation was 13.89%. Relationship issues and a history of sexual abuse were the two factors most significantly associated with depression among students while being in the fifth year of academic study and being satisfied with current academic performance were associated with reduced depression. Smoking cigarettes and/or marijuana, and having financial tuition constraints increased the likelihood of reporting suicidal ideation. However, similar to depression, satisfaction with the current academic performance reduced the likelihood of reporting suicidal ideation.
During the COVID-19 pandemic, higher mental health problems have been reported among students. For instance, the prevalence of depression ranged from 46.92% to 82.4% among Bangladeshi students, as reported in a systematic review (13). Moreover, a recent meta-analysis reported a pooled prevalence of 37% depression among 436,799 students in studies published before September 20, 2020 (12). However, the depression prevalence of the present study (20%) was markedly lower than the previously reported prevalence rate of 80.7% during the first wave of the pandemic (June to July 2020) in a Ugandan study among 321 university students using the 21-item Depression, Anxiety and Stress Scale (4). The difference may be because the present study used a different instrument to screen for depression, with different sensitivities and specificities for assessing depression. In addition, Najjuka et al.’s (4) study involved all university students during the complete institutional lockdown in the first wave of the pandemic, when the levels of uncertainty about the disease were higher and there was associated higher levels of depression among students as reported by other studies (14).
The prevalence of depression in the present study was higher than that reported among non-medical undergraduate university students prior to the introduction of the peer counseling services at Makerere university, 2000–2001 at 16.2%; and medical undergraduate university students following peer counseling introduction (2002) at 4.0% (7). Despite the present study being conducted during a period when peer counseling and other psychological intervention for student mental ill-health is well established among all Ugandan universities, the prevalence of depression reported by Ovuga et al. (7) may have been lower because the study was conducted before the COVID-19 pandemic—a period that significantly increased negative psychological effects among many students (11). However, the depression prevalence of 20% in the present study is slightly lower than 21.5% reported in a study done the year before the pandemic (May–July 2019) among 331 Makerere University medical students using the same instrument (6). The similarity between the study findings and Olum et al. (6), coupled with the significant difference from the only study assessing depression among university students during the pandemic in Uganda (4), could possibly indicate that students have adjusted to the COVID-19 situation and associated stressors, the so-called “new normal,” as reported by other researchers (39). Therefore, depression may be associated with other stressors rather than being pandemic-related.
For instance, in the present study, depression among students was associated with having a history of sexual abuse, a finding similar to other studies among university students. It is also known that individuals who experience sexual abuse during childhood often experience associated depression in adulthood (40). In addition, the severity of depression can be accelerated by the abusive behaviors of the current sexual partner (17, 41). Since students in an abusive relationship have fewer protective factors against depression associated with a supportive romantic relationship, such as comfort, emotional support, and companionship (42). In addition, relationship problems cause significant psychological distress due to disappointment and unmet expectations (43).
Satisfaction with academic grades appeared to be a protective factor against depression and suicidal ideation. Good academic performance is associated with being successful in life (44); therefore, an individual feels positive about their future when their performance is good, and this may help protect them from depression. Conversely, poor academic performance has consistently been associated with depression (45). In Uganda, education is considered the “key to success” (46). Students are expected to meet extremely high expectations from their parents and society to succeed (47). Therefore, it is perhaps unsurprising that students with financial tuition constraints had an increased likelihood of reporting suicidal ideation because if they do not have the ability to fully pay for their university fees, they may lose hope for the future and experience suicidal ideation. However, it has also been reported that some students use their tuition fees to gamble, therefore, they have financial problems if they lose, leading to suicidal behaviors and suicide (48). In Uganda, law and medicine degree programs are pursued for a minimum of 5 years, and culturally these courses are associated with a successful future. Therefore, studying in the fifth-year means being near the end of the undergraduate studies for students, and the dream of future success in life is also nearing. Other researchers studying Ugandan university students have also reported the protective nature of being in the final year against depression during the COVID-19 pandemic (4). Also, by the time a student reaches the fifth year of study, they have been more likely to be exposed to all the conditions around campus and developed coping mechanisms against depression. For example, some have already coped with experiencing romantic breakups, poverty while on campus, and have gotten a peer support system through the friends they acquired over the years.
Just under half of the participants who screened positive for depression reported suicidal ideation in the past 2 weeks (45.37%). This was similar to 48.4% of individuals with major depressive disorder at a mental health facility in Ethiopia (49). The prevalence of suicidal ideation in the present study (13.89%) was lower than 22.7% from a study conducted among university students in another African country, Libya, during the COVID-19 pandemic in the months of April and May 2020 based on Item 9 of the PHQ-9 (50). This difference in prevalence rates may be due to the following reasons: (1) during the time of data collection, Libya was still experiencing a civil war which comes with multiple mental challenges, including thoughts of suicide, (ii) the study was done at a period when individuals worldwide were having higher levels of stress, anxiety, suicidal behaviors and other mental challenges (i.e., early stages of the pandemic) (51); and (iii) the sample only involved medical students who have been reported to experience higher suicidal behaviors compared to other students (52–54).
The prevalence of suicidal ideation in the past 2 weeks in the present study was also lower than 18.04% in a US study involving college students during the month of May 2020 (55). However, the prevalence was higher than 12.9 and 7.3% from studies among university students in China during February and March 2020, respectively (56, 57). Despite the studies in China being conducted earlier, the students were exposed to constant sources of stress during the pandemic, and they would have developed coping strategies to overcome stress complications such as depression and related suicidal behaviors. Smoking cigarettes and/or marijuana was associated with suicidal ideation, a finding consistent with other studies prior to the COVID-19 pandemic (58). Substance use increased during the COVID-19 pandemic and led to multiple mental challenges, including suicide (59–63). Many individuals use addictive substances to cope with stress, and marijuana, in particular, was believed by some Ugandans to treat COVID-19 symptoms (61). Some of the individuals trying to cope with stress by using psychoactive substances could have had suicidal ideation not secondary to the smoking of substances.
Limitations
The present study has a number of limitations. First, it was cross-sectional; therefore, causal relationships between the variables cannot be determined. Second, the study was conducted during the COVID-19 pandemic, which could also independently cause depression among some university students due to uncertainty about their academic progress, source of income, their jobs (for the employed participants), and worries about life. Third, another issue was that anyone who was given access to the survey web-link could respond to it; therefore, there is no guarantee that all responses were from university students only. Fourth, the study design relied on the participants’ memory, which is subject to recall bias. Fifth, this study did not access all the potential variables that could have led to an increase in depression among university students such as disruption of face-to-face teaching classes. Future research should explore these factors to better understand the factors related to depression and the pandemic to reduce such mental consequences in future pandemics. Finally, the study design did not allow for the determination of a true response rate since WhatsApp and emails are unable to track the number of individuals who viewed the link, especially when shared through groups.
Conclusion
The present study found a lower prevalence of depression among university students during the COVID-19 pandemic, similar to pre-pandemic prevalence among university students, and this was associated with having had relationship problems and a history of sexual abuse. However, being satisfied with current academic performance and studying in the fifth year appeared to be protective factors. Therefore, universities in Uganda should implement measures to provide psychological support for students with problems concerning tuition fee challenges, relationships, and past sexual abuse. These can include peer support groups and routine talks about dating and relationships to prepare the students for any outcome. In addition, finalists should be encouraged to mentor other students and teach them strategies to overcome some of the psychological stressors experienced while at university. Also, all students with depression should be screened for suicidal behaviors.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon reasonable request.
Ethics Statement
The studies involving human participants were reviewed and approved by the Mbarara University of Science and Technology Research Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
IA, MMK, EN, MM, JK, MK, NA, IM, NW, and GR: conception and design of the study. IA, MMK, EN, MM, JK, MK, NA, RN, IM, and NW: data collection and its coordination. GR, MAM, MG, and FB: supervision. MMK and IA: formal analysis and data cleaning. IA: initial draft. IA, MMK, EN, MM, JK, RN, MK, NA, IM, SN, NW, FB, MAM, MG, and GR: review of the manuscript. MG: final editing. All authors approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank the participants for voluntarily participating in the study. We would also like to thank the administration of the four universities; BSU, KIU, MUST, and KU, for permitting their students to participate in the study and assisting in recruiting the participants. We also appreciate Namanya Swaibu, Felix Onyango Kijoiki (deceased–due to COVID-19), Nuwahereza Edinah, Ndihabwe Innocent, Bahora Hassan, Mubangizi Abby, Nalumaga Patience Dorcus, Twongirwe Demety, Karobwa Selassie, Aryatuha Joshua, Ainembabazi James, Ssewanyana Ernest, Kushemererwa Jovaile, Nabidda Shamim, Mwanda Genitayo, Ashaba Comfort, Katya Roset, and Ahurira Celine for their contribution during data collection.
Abbreviations
- BSU
Bishop Stuart University
- KIU
Kampala International University Western campus
- MUST
Mbarara University of Science and Technology
- KU
Kabale University
- PHQ-9
Patient Health Questionnaire 9.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Vol. 21. Virginia, VA: American Psychiatric Association; (2013). [Google Scholar]
- 2.World Health Organisation. Depression. (2021). Available online at: https://www.who.int/health-topics/depression#tab=tab_1 (accessed March 01, 2022). [Google Scholar]
- 3.World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. (2017). Available online at: https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf (accessed March 01, 2022). [Google Scholar]
- 4.Najjuka SM, Checkwech G, Olum R, Ashaba S, Kaggwa MM. Depression, anxiety, and stress among Ugandan university students during the COVID-19 lockdown: an online survey. Afr Health Sci. (2021) 21:1533–43. 10.4314/ahs.v21i4.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nsereko N, Musisi S, Nakigudde J, Sekiwu D. Psychosocial problems and development of psychopathology among Ugandan university students. Int J Res Stud Psychol. (2014) 3:3–16. 10.5861/ijrsp.2014.638 [DOI] [Google Scholar]
- 6.Olum R, Nakwagala FN, Odokonyero R. Prevalence and factors associated with depression among medical students at Makerere university, Uganda. Adv Med Educ Pract. (2020) 11:853–60. 10.2147/amep.S278841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ovuga E, Boardman J, Wasserman D. Undergraduate student mental health at Makerere university, Uganda. World Psychiatry. (2006) 5:51–2. [PMC free article] [PubMed] [Google Scholar]
- 8.Mamun MA. Suicide and suicidal behaviors in the context of COVID-19 pandemic in Bangladesh: a systematic review. Psychol Res Behav Manag. (2021) 14:695–704. 10.2147/PRBM.S315760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mamun MA, Al Mamun F, Hosen I, Hasan M, Rahman A, Jubayar AM, et al. Suicidality in Bangladeshi young adults during the COVID-19 pandemic: the role of behavioral factors, COVID-19 risk and fear, and mental health problems. Risk Manag Healthc Policy. (2021) 14:4051–61. 10.2147/RMHP.S330282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mamun MA, Sakib N, Gozal D, Bhuiyan AI, Hossain S, Bodrud-Doza M, et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J Affect Disord. (2021) 279:462–72. 10.1016/j.jad.2020.10.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villani L, Pastorino R, Molinari E, Anelli F, Ricciardi W, Graffigna G, et al. Impact of the COVID-19 pandemic on psychological well-being of students in an Italian university: a web-based cross-sectional survey. Glob Health. (2021) 17:39. 10.1186/s12992-021-00680-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang C, Wen W, Zhang H, Ni J, Jiang J, Cheng Y, et al. Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: a systematic review and meta-analysis. J Am Coll Health. (2021):1–8. 10.1080/07448481.2021.1960849 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 13.Al Mamun F, Hosen I, Misti JM, Kaggwa MM, Mamun MA. Mental disorders of Bangladeshi students during the COVID-19 pandemic: a systematic review. Psychol Res Behav Manag. (2021) 14:645–54. 10.2147/PRBM.S315961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Islam MA, Barna SD, Raihan H, Khan MNA, Hossain MT. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS One. (2021) 15:e0238162. 10.1371/journal.pone.0238162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun S, Goldberg SB, Lin D, Qiao S, Operario D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob Health. (2021) 17:15. 10.1186/s12992-021-00663-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2025591. 10.1001/jamanetworkopen.2020.25591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmed G, Negash A, Kerebih H, Alemu D, Tesfaye Y. Prevalence and associated factors of depression among Jimma university students. A cross-sectional study. Int J Ment Health Syst. (2020) 14:52. 10.1186/s13033-020-00384-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ithnain N, Ghazali S, Jaafar N. Relationship between smartphone addiction with anxiety and depression among undergraduate students in Malaysia. Int J Health Sci Res. (2018) 8:163–71. [Google Scholar]
- 19.Lugata S, Elinisa M, Doshi B, Kashuta RA, Hango S, Mallosa WJ, et al. Symptoms and predictors of depression among university students in the Kilimanjaro region of Tanzania: a cross-sectional study. J Ment Health. (2021) 30:255–62. 10.1080/09638237.2020.1793129 [DOI] [PubMed] [Google Scholar]
- 20.Paudel S, Gautam H, Adhikari C, Yadav DK. Depression, anxiety and stress among the undergraduate students of Pokhara Metropolitan, Nepal. J Nepal Health Res Counc. (2020) 18:27–34. 10.33314/jnhrc.v18i1.2189 [DOI] [PubMed] [Google Scholar]
- 21.Sarokhani D, Delpisheh A, Veisani Y, Sarokhani MT, Manesh RE, Sayehmiri K. Prevalence of depression among university students: a systematic review and meta-analysis study. Depress Res Treat. (2013) 2013:373857. 10.1155/2013/373857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Worku D, Dirriba AB, Wordofa B, Fetensa G. Perceived stress, depression, and associated factors among undergraduate health science students at Arsi university in 2019 in Oromia, Ethiopia. Psychiatry J. (2020) 2020:4956234. 10.1155/2020/4956234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu Z, Xu Q, Wang Y, Zhang J, Liu J, Xu F. Association of sedentary behavior and depression among college students majoring in design. Int J Environ Res Public Health. (2020) 17:3545. 10.3390/ijerph17103545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zafar U, Daud S, Khalid A. Determinants of depression among undergraduate medical students of a private medical college in Lahore. J Pak Med Assoc. (2020) 70:467–71. 10.5455/JPMA.13896 [DOI] [PubMed] [Google Scholar]
- 25.Sorberg Wallin A, Koupil I, Gustafsson JE, Zammit S, Allebeck P, Falkstedt D. Academic performance, externalizing disorders and depression: 26,000 adolescents followed into adulthood. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:977–86. 10.1007/s00127-019-01668-z [DOI] [PubMed] [Google Scholar]
- 26.Kaggwa MM, Muwanguzi M, Nduhuura E, Kajjimu J, Arinaitwe I, Kule M, et al. Suicide among Ugandan university students: evidence from media reports for 2010–2020. BJPsych Int. (2021) 18:63–7. 10.1192/bji.2021.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaggwa MM, Nuwamanya S, Ashaba S, Rukundo GZ, Harms S. An adolescent’s use of veterinary medicines: a case report exploring addiction. J Psychoact Drugs. (2021) 53:339–44. 10.1080/02791072.2021.1873466 [DOI] [PubMed] [Google Scholar]
- 28.Orsolini L, Latini R, Pompili M, Serafini G, Volpe U, Vellante F, et al. Understanding the complex of suicide in depression: from research to clinics. Psychiatry Investig. (2020) 17:207–21. 10.30773/pi.2019.0171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kajjimu J, Kaggwa MM, Bongomin F. Burnout and associated factors among medical students in a public university in Uganda: a cross-sectional study. Adv Med Educ Pract. (2021) 12:63–75. 10.2147/amep.S287928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carroll HA, Hook K, Perez OFR, Denckla C, Vince CC, Ghebrehiwet S, et al. Establishing reliability and validity for mental health screening instruments in resource-constrained settings: systematic review of the PHQ-9 and key recommendations. Psychiatry Res. (2020) 291:113236. 10.1016/j.psychres.2020.113236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levis B, Benedetti A, Thombs BD, Collaboration DESD. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. 10.1136/bmj.l1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. (2013) 210:653–61. 10.1016/j.psychres.2013.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaggwa MM, Mamum MA, Najjuka SM, Muwanguzi M, Kule M, Nkola R, et al. Gambling-related suicide in East African community countries: evidence from press media reports. BMC Public Health. (2022) 22:1–13. 10.1186/s12889-021-12306-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nakku JEM, Rathod SD, Kizza D, Breuer E, Mutyaba K, Baron EC, et al. Validity and diagnostic accuracy of the Luganda version of the 9-item and 2-item patient health questionnaire for detecting major depressive disorder in rural Uganda. Glob Ment Health. (2016) 3:e20. 10.1017/gmh.2016.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bahati R, Herbert Elvis A, Cathy Denise S, Godfrey Zari R. Association between stigma and depression among urban refugees in Mbarara municipality, Southwestern Uganda. Res Sq. (2021): 10.21203/rs.3.rs-17932/v1 [DOI] [Google Scholar]
- 36.Kaggwa MM, Namatanzi B, Kule M, Nkola R, Najjuka SM, Al Mamun F, et al. Depression in Ugandan rural women involved in a money saving group: the role of spouse’s unemployment, extramarital relationship, and substance use. Int J Womens Health. (2021) 13:869–78. 10.2147/IJWH.S323636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Erbe D, Eichert HC, Rietz C, Ebert D. Interformat reliability of the patient health questionnaire: validation of the computerized version of the PHQ-9. Internet Interv. (2016) 5:1–4. 10.1016/j.invent.2016.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheng C, Wang HY, Ebrahimi OV. Adjustment to a “New Normal:” coping flexibility and mental health issues during the COVID-19 pandemic. Front Psychiatry. (2021) 12:626197. 10.3389/fpsyt.2021.626197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Phillip O, Amone-P’Olak K. The influence of self-reported childhood sexual abuse on psychological and behavioural risks in young adults at a university in Botswana. South Afr J Psychol. (2018) 49:353–63. 10.1177/0081246318801723 [DOI] [Google Scholar]
- 41.Peltzer K, Pengpid S, Tiembre I. Mental health, childhood abuse and HIV sexual risk behaviour among university students in Ivory Coast. Ann Gen Psychiatry. (2013) 12:18. 10.1186/1744-859X-12-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Farrer LM, Gulliver A, Bennett K, Fassnacht DB, Griffiths KM. Demographic and psychosocial predictors of major depression and generalised anxiety disorder in Australian university students. BMC Psychiatry. (2016) 16:241. 10.1186/s12888-016-0961-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hemesath C. Falling out of Romantic Love: A Phenomenological Study of the Meaning of Love in Marriage. Doctaorate Dissertation. Iawa State University; (2016). Available online at: https://lib.dr.iastate.edu/etd/16721/ (accessed March 01, 2022). [Google Scholar]
- 44.Shek DTL, Li X. Perceived school performance, life satisfaction, and hopelessness: a 4-year longitudinal study of adolescents in Hong Kong. Soc Indic Res. (2016) 126:921–34. 10.1007/s11205-015-0904-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nakhostin-Ansari A, Sherafati A, Aghajani F, Khonji MS, Aghajani R, Shahmansouri N. Depression and anxiety among Iranian medical students during COVID-19 pandemic. Iran J Psychiatry. (2020) 15:228–35. 10.18502/ijps.v15i3.3815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Theron L, van Rensburg A. Resilience over time: learning from school-attending adolescents living in conditions of structural inequality. J Adolesc. (2018) 67:167–78. 10.1016/j.adolescence.2018.06.012 [DOI] [PubMed] [Google Scholar]
- 47.Nakalema G, Ssenyonga J. Academic stress: its causes and results at a Ugandan University. Afr J Teach Educ. (2013) 3:1–21. 10.21083/ajote.v3i3.2762 [DOI] [Google Scholar]
- 48.Kaggwa MM, Najjuka SM, Mamun MA. The psychometrics of patient health questionnaire (PHQ-9) in Uganda: a systematic review. Front Psychiatry. (2022) 13:781095. 10.3389/fpsyt.2022.781095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Basha EA, Mengistu BT, Engidaw NA, Wubetu AD, Haile AB. Suicidal ideation and its associated factors among patients with major depressive disorder at Amanuel mental specialized hospital, Addis Ababa, Ethiopia. Neuropsychiatr Dis Treat. (2021) 17:1571–7. 10.2147/ndt.S311514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elhadi M, Buzreg A, Bouhuwaish A, Khaled A, Alhadi A, Msherghi A, et al. Psychological impact of the civil war and COVID-19 on Libyan medical students: a cross-sectional study. Front Psychol. (2020) 11:570435. 10.3389/fpsyg.2020.570435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aknin LB, De Neve J-E, Dunn EW, Fancourt DE, Goldberg E, Helliwell JF, et al. Mental health during the first year of the COVID-19 pandemic: a review and recommendations for moving forward. Perspect Psychol Sci. (2022):17456916211029964. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blacker CJ, Lewis CP, Swintak CC, Bostwick JM, Rackley SJ. Medical student suicide rates: a systematic review of the historical and international literature. Acad Med. (2019) 94:274–80. 10.1097/acm.0000000000002430 [DOI] [PubMed] [Google Scholar]
- 53.World Health Organisation. Suicide Rate Estimates, Crude Estimates by Country. (2021). Available online at: https://apps.who.int/gho/data/node.main.MHSUICIDE (accessed March 01, 2021). [Google Scholar]
- 54.Yip PSF, Zheng Y, Wong C. Demographic and epidemiological decomposition analysis of global changes in suicide rates and numbers over the period 1990–2019. Inj Prev. (2021):injuryrev–2021–044263. 10.1136/injuryprev-2021-044263 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 55.Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. (2020) 22:e22817. 10.2196/22817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xin M, Luo S, She R, Yu Y, Li L, Wang S, et al. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am Psychol. (2020) 75:607–17. 10.1037/amp0000692 [DOI] [PubMed] [Google Scholar]
- 57.Zhou S-J, Wang L-L, Qi M, Yang X-J, Gao L, Zhang S-Y, et al. Depression, anxiety, and suicidal ideation in Chinese university students during the COVID-19 pandemic. Front Psychol. (2021) 12:669833. 10.3389/fpsyg.2021.669833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seo C, Di Carlo C, Dong SX, Fournier K, Haykal K-A. Risk factors for suicidal ideation and suicide attempt among medical students: a meta-analysis. PLoS One. (2021) 16:e0261785. 10.1371/journal.pone.0261785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Enns A, Pinto A, Venugopal J, Grywacheski V, Gheorghe M, Kakkar T, et al. Substance use and related harms in the context of COVID-19: a conceptual model. Health Promot Chronic Dis Prevent Can. (2020) 40:342–9. 10.24095/hpcdp.40.11/12.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. (2020) 14:20. 10.1186/s13034-020-00329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kaggwa MM, Bongomin F, Najjuka SM, Rukundo GZ, Ashaba S. Cannabis-induced mania following COVID-19 self-medication: a wake-up call to improve community awareness. Int Med Case Rep J. (2021) 14:121–5. 10.2147/imcrj.S301246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. (2021) 26:30–9. 10.1038/s41380-020-00880-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wardell JD, Kempe T, Rapinda KK, Single A, Bilevicius E, Frohlich JR, et al. Drinking to cope during COVID-19 pandemic: the role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcohol Clin Exp Res. (2020) 44:2073–83. 10.1111/acer.14425 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon reasonable request.