Abstract
Introduction:
Trans-urethral bladder surgery has gained popularity in the fields of electro-resection and laser lithotripsy, with endoscopic suturing being overlooked. Bladder defect closure using a pure trans-urethral suturing technique can provide a quick and effective solution in situations where conventional management options are not feasible.
Methods:
Here we describe this innovative novel technique developed by our group that was used to treat two different cases with bladder perforation at two different institutions. We used a 5 mm laparoscopic port with gas insufflation and a laparoscopic needle holder trans-urethrally to achieve defect closure with a monofilament 2/0 monocryl mattress suture on a small 22 mm needle.
Results:
The defects were successfully closed without any intraoperative complications. Average operative time for the technique was 18 min with minimal blood loss. Bladder closure was sustained at a median follow-up of 2 years for one of these cases.
Conclusions:
We claim that transurethral bladder suturing is quick, safe in expert hands and provides an effective option where the clinical condition/situation of the patient warrants a minimally invasive surgery approach.
Keywords: Trans-urethral bladder surgery, endoscopic surgery, cystorrhaphy, transurethral bladder suture
Introduction
Trans-oral and trans-anal endoscopic suturing is gaining popularity among specialists in the relevant end of the digestive tract. 1 Trans-urethral endoscopic bladder surgery is well established in the domain of electro-resection and the use of lasers; however, reports of trans-urethral bladder suturing (TUBS) have been stimulating so far more criticism than enthusiasm,2,3 remaining currently only applicable to animal models assessing natural orifice trans-luminal endoscopic surgery. 4 We report a modest experience of two cases of TUBS, where the technique was quick, feasible and the best possible answer to unusually complex situations.
Methods – Case presentations
Two patients were offered the minimally invasive transurethral bladder closure option from our group at two different locations, Ygia Polyclinic in Limassol, Cyprus and King’s College Hospital in London, UK.
Case 1 – Bladder tape erosion
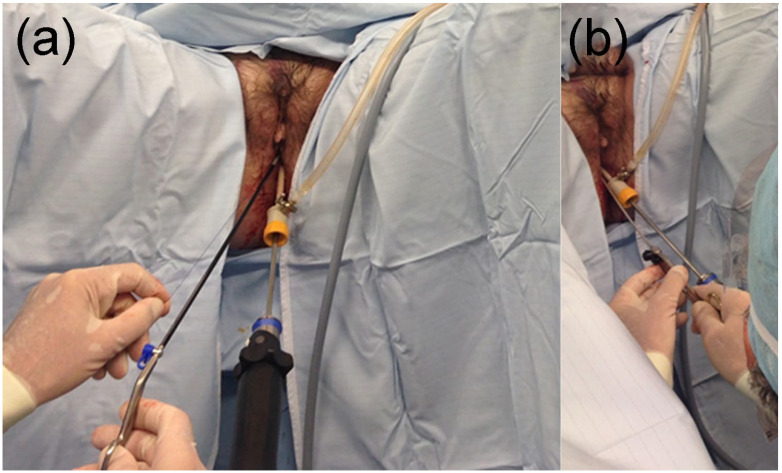
The first patient was a 74 year-old female who presented with irritative lower urinary tract symptoms and haematuria. She underwent a tension-free vaginal tape (TVT) procedure 3 years prior for stress urinary incontinence. On cystoscopy the TVT tape had eroded into the bladder near the right ureteric orifice and a concomitant multifocal transitional cell carcinoma (TCC) was seen on the left lateral bladder wall. A complete trans-urethral resection of bladder tumour (TURBT) was carried out. The histology revealed a G3pT1 TCC. In the absence of TCC recurrence at the 3 months follow-up, the decision was made to treat the eroded tape. The patient was placed in the lithotomy position under general anaesthesia. A 3 mm laparoscopic needle holder was inserted through the urethra for tape traction and the tape was excised using a resectoscope and Collins knife. Using the 3 mm laparoscopic needle holder through the urethra and a 30 degrees 5 mm laparoscopic camera through a transurethral conventional 5 mm laparoscopic port, the urothelial defect was repaired with interrupted 2/0 monocryl using extracorporeal knots and a knot pusher. The procedure was carried out with gas insufflation using a conventional CO2 laparoscopic insufflator and tubing attached either to the resectoscope or the 5 mm laparoscopic port. (Figure 1)
Figure 1.
The transurethral 5 mm laparoscopic port that allows gas insufflation and camera introduction, along with the laparoscopic knot pusher/needle holder through the urethra by the side of the port: caudal view (a) and lateral/oblique view (b).
Case 2 – Polytrauma
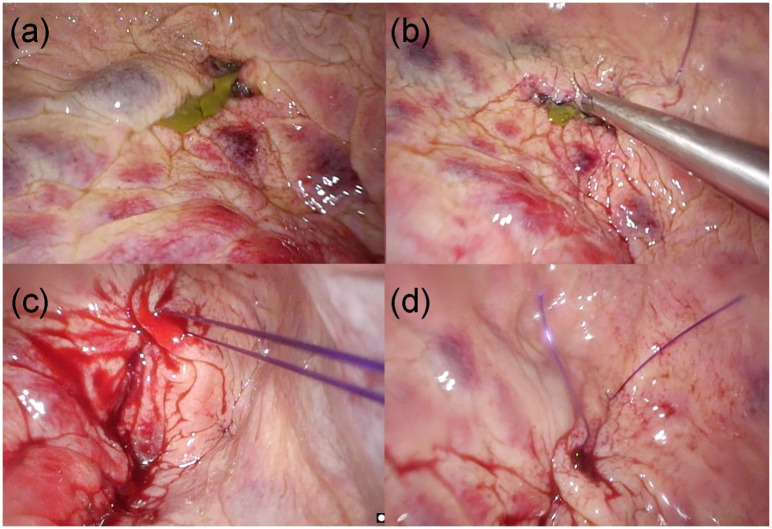
The second case was a 52-year-old lady with significant co-morbidity (ASA 3) who had attempted suicide. She was admitted unstable at our major trauma centre with unstable pelvic fracture and visible haematuria. She required emergency arterial pelvic embolisation to control pelvic bleeding, an exploratory laparotomy with splenectomy and external pelvic fixator. The kidneys were intact on CT and the bladder appeared intact on an initial cystogram obtained at the time of the emergency embolisation. 2 days post-operatively she developed clot urinary retention and peritonism. A CT-cystogram confirmed intraperitoneal bladder perforation, the timing and mechanism of which remains unclear. Considering her recently operated condition, we offered her a purely trans-urethral bladder repair. A 30 degrees 5 mm laparoscope was inserted into the bladder through a transurethral 5 mm conventional laparoscopic port which allowed bladder insufflation with CO2. A 3 mm laparoscopic needle holder was introduced by the side of the 5 mm port (Figure 1) and was used for single-handed bladder repair with interrupted 2/0 monocryl and extracorporeal sliding knots (Figure 2).
Figure 2.
The bladder perforation was identified in the first instance with perivesical fat protruding intravesically (a), a trans-urethral laparoscopic needle holder is used to achieve closure of the defect with an interrupted mattress absorbable suture (b and c), and the final outcome of closure is inspected for any immediate complications (d).
Due to the emergent situation of their conditions, their cases were briefly discussed in a multidisciplinary team setting prior to this technique being applied, with discussion of these cases in the Local Ethics Committee waived for the same urgent reasons. Informed consent included explanation of this technique prior to consideration for conversion to an open approach in the case of complications arising necessitating this.
Results
For the first case, total operating time was 90 min with no blood loss, including the time for tape excision prior to closure of the urothelium. The urothelium closure step took 21 min. A urethral catheter was left in situ for 2 days. There were no post-operative complications. She remains tape, stone and tumour free at 36 months of cystoscopic follow-up with one tumour recurrence that required resection at 24 months.
For our polytrauma case, total operating time was 15 min with no blood loss. A urethral catheter was left in situ. There were no post-operative complications related to the bladder closure.
Discussion
Minimally invasive bladder surgery is gaining popularity with conventional laparoscopy and robotic surgery largely replacing open surgery. Such techniques utilize a trans-peritoneal approach and transmural access into the bladder. This may be difficult and time-consuming and indeed risky in polytrauma or in multiply operated abdomen with dense adhesions. In such cases, one may argue that vesicoscopy is the solution as one can bypass the abdominal adhesions and gain direct access into the bladder pathology.5,6 The two reported cases are indeed unique and pose some difficulties for the vesicoscopic approach. With our polytrauma lady, the bladder perforation does not allow for adequate bladder distension and safe vesicoscopic access. In our lady with the bladder carcinoma one would be reluctant to breach the bladder wall fearing for extravesical tumour cell seeding. In such cases the natural urethral orifice offers a safe and direct access to the bladder pathology.
Minimally invasive surgery at its infancy was only feasible with multiple access ports and multiple instruments with the classical instrument triangulation. Triangulation makes instrument handling easier but is not always feasible; this has been overcome by practice, experience and improved technique. Single access minimally invasive surgery with modified and improved laparoscopic instruments was proposed by some enthusiasts but did not gain much popularity due to an increased demand in surgical laparoscopic skills. Maybe the single site robotic platform and improved technology will popularize again single site minimally invasive surgery. 5
The female urethra as an accessory/additional route has been utilized and reported by our group and others during vesicoscopy.6–8 This reduces the number of suprapubic ports and limits instrument clashing. This technique is not applicable in males given the long and tortuous course of the male urethra. The urethra as a sole route for natural orifice bladder reconstructive surgery has not previously been reported. An initial approach of two cases of transurethral cystoscopy assisted bladder closure (cystorrhaphy) for vesico-vaginal/vesico-cutaneous fistulas were reported by McKay. 2 With the technique not gaining popularity among peers as it involved additional suprapubic access to assist the suturing steps. The technique was later modified by the same author, who described the use of an arthroscope/small laparoscope for vesicoscopy and trans-urethral cystorrhaphy using a laparoscopic needle holder, with variable outcomes. 3
Our reported cases suggest that this is feasible, quick and safe and may indeed be the solution to complex cases. We have used small conventional endoscopic and laparoscopic instruments. The technique requires advanced laparoscopic skills such as single hand laparoscopic suturing due to limitation in number of instruments and also extracorporeal sliding knot techniques. One may argue that in the first case, with the eroded tape, a transurethral endoscopic tape electro-resection or tape lasering may have been all that was required. However, we recently reported the higher success of vesicoscopic tape removal when the urothelial defect is closed over a completely excised tape. 6 The transurethral access we here report replicates the vesicoscopic technique without the need of additional bladder access for instrumentation/visualisation. Further investigation in the long term complications is warranted prior to widespread utilisation of this method.
Conclusions
TUBS is an interesting concept which we have demonstrated to be safe, effective and feasible and should complement all the other minimally invasive techniques for bladder surgery.
Footnotes
Author’s note: Philippe Grange is also affiliated with Johnson and Johnson Gmbh, Norderstedt, Germany.
Author contribution: FG: Manuscript writing, data collection, figure preparation, video editing. CK: Manuscript writing, data collection, figure preparation. JM: Manuscript editing, data collection. PG: Manuscript writing, data collection, technique development.
Consent: Written informed consent was obtained from the patients for publication of images and video recordings.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: Phillipe Grange received funding for research, lecturing and/or advice or consultancies from Johnson & Johnson, Olympus and OR Productivity. The other authors report no relevant financial interests.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: FG is supported as an Academic Clinical Fellow by the National Institute of Health Research and NHS Blood and Transplant at the University of Cambridge. PG received funding for research from Johnson & Johnson, Olympus and OR Productivity. The rest of the authors received no financial support for the research, authorship and/or publication of this article.
ORCID iDs: Fanourios Georgiades  https://orcid.org/0000-0003-0440-2720
https://orcid.org/0000-0003-0440-2720
Philippe Grange  https://orcid.org/0000-0002-2884-5772
https://orcid.org/0000-0002-2884-5772
Supplemental material: Supplemental material for this article is available online.
References
- 1. Kumar N, Abu Dayyeh BK, Lopez-Nava Breviere G, et al. Endoscopic sutured gastroplasty: procedure evolution from first-in-man cases through current technique. Surg Endosc 2018; 32: 2159–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McKay HA. Vesicovaginal and vesicocutaneous fistulas: transurethral suture cystorrhaphy as a new closure technique. J Urol 1997; 158: 1513–1516. [DOI] [PubMed] [Google Scholar]
- 3. McKay HA. Transurethral suture cystorrhaphy for repair of vesicovaginal fistulas: evolution of a technique. Int Urogynecol J Pelvic Flood Dysfunct 2001; 12: 282–287. [DOI] [PubMed] [Google Scholar]
- 4. Oliveira C, Autorino R, Ferreira C, et al. Novel method of full-thickness bladder closure with an endoscopic suturing machine: a survival study in a porcine model. BJU Int 2015; 115: 330–335. [DOI] [PubMed] [Google Scholar]
- 5. Autorino R, Cadeddu JA, Desai MM, et al. Laparoendoscopic single-site and natural orifice transluminal endoscopic surgery in urology: a critical analysis of the literature. Eur Urol 2011; 59: 26–45. [DOI] [PubMed] [Google Scholar]
- 6. Grange P, Kouriefs C, Georgiades F, et al. Eroded tape: a case of an early vesicoscopy rather than laser melting. Urology 2017; 102: 247–251. [DOI] [PubMed] [Google Scholar]
- 7. Grange P, Giarenis I, Rouse P, et al. Combined vaginal and vesicoscopic collaborative repair of complex vesicovaginal fistulae. Urology 2014; 84: 950–954. [DOI] [PubMed] [Google Scholar]
- 8. Roslan M, Markuszewski MM. Transvesical laparoendoscopic single site surgery to remove surgical materials penetrating the bladder: initial clinical experience in 9 female patients. J Urol 2013; 190: 909–915. [DOI] [PubMed] [Google Scholar]