Abstract
In this research, a review of antimicrobial resistance (AMR) is conducted as part of the One Health approach. A review of publications, which included “antimicrobial resistance” and “One Health,” was conducted. Among the global health problems, AMR is the one that most clearly illustrates the One Health approach. AMR is a critical global problem affecting humans, the environment, and animals. This is related to each of these three components due to the irresponsible and excessive use of antimicrobials in various sectors (agriculture, livestock, and human medicine). Improper management of antimicrobials, inadequate control of infections, agricultural debris, pollutants in the environment, and migration of people and animals infected with resistant bacteria facilitate the spread of resistance. The study aimed to analyze the problem of AMR from a health perspective to analyze the different actors involved in One Health.
Keywords: antimicrobials, human, animals, plants
Introduction
Among global health problems, antimicrobial resistance (AMR) is the one that best illustrates the One Health approach. The One Health approach is defined as a joint effort of various disciplines that come together to provide solutions for human, animal, and environmental health [1]. AMR is linked to each of these three components due to the irresponsible and excessive use of antimicrobials in various sectors (agriculture, cattle raising, and human medicine) [2,3]. Under the pressure of antimicrobial selection, bacteria acquire resistance genes and mobile genetic elements that can spread to other bacteria of the same or different genus. When bacteria acquire resistance to antimicrobials, they also acquire a greater ability to proliferate in animals, humans, and the natural world [4]. Mismanagement of antimicrobials, inadequate infection control, agricultural debris, contaminants in the environment, and migration of people and animals infected with resistant bacteria facilitate the spread of resistance [4,5].
AMR is a critical global problem that affects human, environmental, and animal health (Figure-1). Because AMR is a complex problem, it is necessary to look at it from different disciplines to frame it within the One Health approach [6-8].
Figure-1.
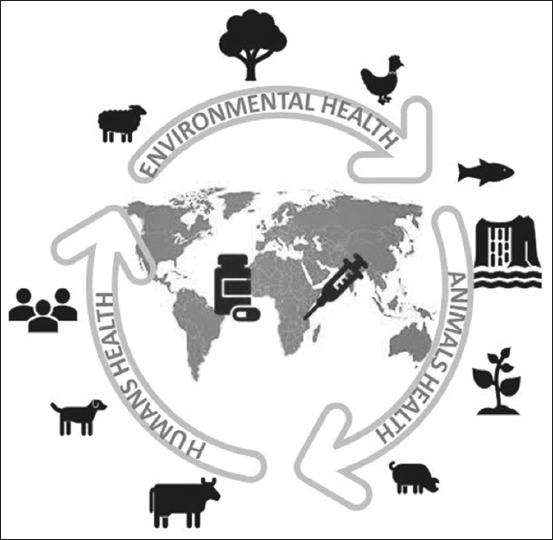
Schematic representation of the antimicrobial resistance under the perspective One Health [Source: Figure prepared by the authors].
The “One Health” approach originated in the 19th century, when Rudolf Virchow introduced the term “zoonosis,” which encompasses the relationship between human and animal health [9]. Subsequently, Calvin Schwabe made important contributions to the disciplines of public health, epidemiology, and tropical medicine. He introduced the concept of one medicine, reaffirming the close relationship between human medicine and animal medicine [10]. In 2004, the Wildlife Conservation Society held a congress to discuss the implications of disease transmission in wildlife, domestic animals, and humans. Based on this meeting, the Manhattan Principles were established to combat infectious diseases and maintain the balance of ecosystems [11].
The study aimed to analyze the problem of AMR from a health perspective to analyze the different actors involved in One Health.
Antimicrobial Resistance from the One Health Approach
Of particular concern is the rapid global spread of multidrug-resistant bacteria causing infections that cannot be treated with current antimicrobials. In 2019, the World Health Organization (WHO) identified 32 antimicrobials in hospital development, of which only six were classified as innovative. The lack of antimicrobials is affecting global health systems. Currently, infections caused by antimicrobial-resistant microorganisms are difficult to treat because antimicrobials are increasingly ineffective against these infections resulting in higher mortality rates. New antimicrobials are needed to control infections caused by the major pathogens outlined by the WHO. Now, unless the way current antimicrobials are used has not changed, these new antimicrobials will suffer the same fate as the current antimicrobials and become ineffective. Antimicrobial retention AMR has a significant impact on national economies and their health systems, as it affects the productivity of patients or caregivers due to prolonged hospital stays with high economic costs. The main factor of AMR includes improper and excessive use of antimicrobials; lack of access to clean water, sanitation, and hygiene for humans and animals; poor infection prevention and control measures in hospitals; poor access to medicines and vaccines; lack of awareness and knowledge; and irregularities with legislation [12].
AMR represents a global public health problem, for which epidemiological surveillance systems have been established, aiming to promote collaborations directed at the well-being of human and animal health and the balance of the ecosystem. Several international organizations (The World Organisation for Animal Health [OIE], WHO, and the Food and Agriculture Organization of the United Nations [FAO]) have joined forces to develop a Global Action Plan on Antimicrobial Resistance-WHO [12]. Action taken in this plan included understanding the AMR from surveillance and research. The advisory group established guidelines for AMR surveillance to ensure all countries implement integrated surveillance, which will cover the use and consumption of antimicrobials in the human and animal population. These guidelines will provide a clear understanding of how AMR spreads in different settings and specific areas. It will allow to study the correlation between AMR and antimicrobial use in a different setting (animals, humans, and environment) and to assess the effect of interventions within and between sectors [13,14,15].
The Interagency Coordination Group on Antimicrobial Resistance (WHO, OIE, and FAO) on AMR presented to the UN Secretary-General in April 2019 its report entitled “We can’t: securing the future against drug-resistant infections.” In addition, a joint tripartite secretariat (FAO, OIE and WHO) was established, based at WHO, to promote multi-stakeholder collaboration on AMR. New governance structures were agreed upon, such as the global AMR leaders group, the independent AMR action reporting group and the multi-lateral collaborative platform. One of the strategies to raise awareness of the AMR problem was the launch of the “Global Antimicrobial Awareness Week”. From 2020, it is called “World Antimicrobial Awareness Week,” referring to all antimicrobials: antibiotics, antifungals, antiparasitics, and antivirals. It is a global campaign that aims to raise awareness of AMR worldwide and encourage best practices among the general population, healthcare workers, and policymakers to curb the evolution and spread of drug-resistant infections.
In 2015, WHO launched the Global Antimicrobial Resistance Surveillance System (GLASS) to fill knowledge gaps and guide strategies at all levels. GLASS was created to progressively integrate surveillance data on antimicrobials used in humans, track antimicrobial use, and understand the role of AMR in the food chain and the environment. It provides a standardized approach to collecting, analyzing, interpreting, and sharing data by country, region, and area, allowing you to monitor the status of new or existing national surveillance systems, emphasizing the representativeness and quality of the data collected. In 2017, WHO developed the list of priority pathogens to guide research and development of new antimicrobials, diagnostic tools, and vaccines. WHO annually reviews preclinical and clinical antimicrobial development projects to assess their progress against the priority pathogens. This list will be updated in 2022. Additionally, the Global Alliance for Antibiotic Research and Development is a joint initiative of WHO and the Drugs for Neglected Diseases Initiative, supporting research and development through public–private partnerships. The partnership aims to develop and implement five new treatments against drug-resistant bacteria identified by WHO as the greatest threat by 2025 [12].
Antimicrobial use in Humans, Animals, and Plants
Some antimicrobials were used for decades before resistance developed, whereas other antimicrobials developed resistance in a much shorter time. Antimicrobials with slow resistance development, especially vancomycin, were highly valued for their continued ability to treat infections that could not be treated with other commonly used antimicrobials. Today, the increasing vancomycin resistance is a concern as certain strains of bacteria that previously posed a relatively minor health risk, such as vancomycin-resistant enterococci, contribute greatly to mortality and morbidity, particularly in hospitals [6].
Antimicrobials have various uses in animals, including pets, farmed fish in aquaculture systems, bees, and farm animals. Antimicrobials are used for various purposes (therapeutic, prophylactic, and development promoters) and play an important role in animal production. The volume of antimicrobials used in animals worldwide is estimated to be greater than in humans. Most classes of antimicrobials used in humans are prescribed for animals, including classes of antimicrobials vital to human medicine, such as broad-spectrum beta-lactams and quinolones [16].
Some antimicrobials used in humans and animals (tetracycline, triazoles, and streptomycin) are used therapeutically in plants. AMR can be easily transferred between and within different ecosystems and populations; resistant zoonotic bacteria can be found in the soil; and from there, they can infect plants, vegetables, and fruits. It has been documented that the use of antimicrobials in agriculture induces antibiotic-resistant fungi transmitted from the environment to humans [17]. There are some classes of antimicrobials for human use only (carbapenems) and others for animal use only (flavophospholipol and ionophores) [18,19]. Other antimicrobials for clinical use, such as tetracycline and streptomycin, are used for prophylaxis and treatment against bacteria that cause fruit infection [20]. Antimicrobials doses used in aquaculture may be higher than those prescribed for livestock. Residues of antimicrobials remain in fish products and can remain in aquatic environments for a long time through excreta. These residues spread rapidly in water bodies, exerting selective pressure [21]. Antimicrobials are widely used as growth promoters, which is the main reason for the large volumes of antimicrobials used in the animal food industry [22].
Antibiotic use from the One Health Approach
Examples of antibiotics used in humans and animals
Colistin
Colistin (polymyxin B) is a highly bactericidal antibiotic that has been used by humans and animals for decades, but its systemic administration causes nephrotoxicity [23]. The use of this antibiotic is limited to treating patients with skin infections or cystic fibrosis. However, the frequency of systemic administration of colistin has been increased for treating infections caused by carbapenem-resistant bacteria (Escherichia coli and Pseudomonas aeruginosa) [24-26]. In countries where colistin is used to treat infections or as a growth promoter in animal production, excessive use of this antibiotic relative to human doses has been observed, although this varies by country [24,27,28].
Colistin resistance was initially chromosomally encoded, but in 2015, the plasmid-mediated mcr-1 gene was reported to cause colistin resistance in E. coli strains, isolated from samples of foods, animals, and blood cultures in China [29]. Additionally, the mcr-1 gene is present in other bacterial genera (P. aeruginosa, Enterobacter spp., and Klebsiella pneumoniae) [29]. Other studies have reported the presence of the mcr-1 gene in various parts of the world in bacteria isolated from environmental, animal, and surface water samples [29,30].
The emergence of colistin resistance indicates that resistance can be increased further with the use of high doses of antimicrobials as growth promoters or to treat infections. The same problem was observed when avoparcin was used as a growth promoter. Also, vancomycin, another glycopeptide used in methicillin-resistant Staphylococcus aureus (MRSA), has resulted in resistance to severe infections caused by enterococci [31,32].
Third-generation cephalosporins
These beta-lactam antibiotics are widely used in animals and humans; ceftriaxone, cefotaxime, and other cephalosporins are used to treat various infections in humans: urinary tract, abdominal, pulmonary and bloodstream infections [33]. Because of its usefulness in treating bacteria associated with AMR, this group of antibiotics has been classified as “ significant” to health [34].
Ceftiofur is the most widely used veterinary cephalosporin, followed by cefoperazone, cefovecin, and cefpodoxime. Ceftiofur is approved in many countries to treat bacterial infections, primarily in animals for human consumption. Its application is limited to parenteral use and is used in animals individually or in groups. Depending on the animal species, ceftiofur is used to treat meningitis, septicemia, pneumonia, septic arthritis, polyserositis, and metritis, among other types of infection. It is also sometimes used for respiratory diseases, prophylaxis in beef cattle, or preventing E. coli infections in broiler chickens [35].
In Europe, which has recorded data on antibiotic use for many years, approximately 18 tons of third- and fourth generation cephalosporins were used in 2017, mainly in animals intended for human consumption [28]. This represented approximately 0.2% of the total antimicrobial use in animals in Europe. In the USA, the total cephalosporin use for animals was approximately 31.44 tons in 2018 [36].
Extended-spectrum beta-lactamases are capable of inactivating third-generation cephalosporins (ceftriaxone, cefotaxime, ceftazidime) and aztreonam. The genes that code for this resistance is transferred by plasmids and transposons. AmpC beta-lactamases were first detected in chromosomes and later expressed in plasmids, indicating the presence of horizontal gene transfer among enterobacteria [37]. Resistance to E. coli and K. pneumoniae cephalosporin strains that cause serious infections are now reported in many countries. This has led to increased use of several existing antimicrobials, such as carbapenems [38].
Ceftiofur is primarily used to prevent E. coli infections and yolk sac infections [39,40]. This treatment has been shown to select strains of Salmonella resistant to cephalosporins; this bacterium causes serious diseases in humans and is associated with the consumption of contaminated poultry products [39-41]. Monitoring by the Canadian Integrated Program for AMR Surveillance revealed a temporal correlation between ceftiofur and ceftriaxone resistance in Salmonella Heidelberg strains isolated from poultry and humans [42].
Fluoroquinolones
Fluoroquinolones are a family of broad-spectrum agents used to treat respiratory and urinary tract infections and are active against many Gram-positive and Gram-negative bacteria. Resistance to fluoroquinolones is caused by loss of porins, by the presence of efflux pumps or by alteration of the target sites of DNA gyrase and topoisomerase IV. Resistance to horizontally applied quinolones was first described in 1998. The qnr gene, located in a mobile genetic element, is responsible for this type of resistance [43].
Fluoroquinolones are another class of important antimicrobials where resistance has emerged among Campylobacter jejuni isolate medications in poultry [44]. In Australia, where fluoroquinolones have never been approved for use in animal feed, strain resistance to fluoroquinolones is rare [45]. The use of fluoroquinolones in livestock has been identified as a critical area because of the importance of these antimicrobials in treating human infections. In 2017, approximately 216 tons of fluoroquinolones were used in Europe, mainly in animals meant for human consumption [28]. This represented approximately 2.4% of all antimicrobials used in animals in Europe, and the total fluoroquinolone used in animals in the USA was approximately 23.3 tons in 2018 [36].
Given the importance of cephalosporins and fluoroquinolones in treating humans and selecting drug-resistant bacteria that can be transmitted from animals to humans, the use of cephalosporins and fluoroquinolones must be restricted [39-45].
Implications for public and animal health
AMR reduces the effectiveness of antimicrobial therapy and often increases the cost incidence and severity of infection [3,46]. Currently, there is scientific evidence that the indiscriminate use of antimicrobials in the veterinary field has led to the emergence of resistant bacteria that cause infections in humans, particularly in Enterococcus spp., Campylobacter spp., Salmonella spp., and E. coli strains [31,42,44].
From the perspective of the One Health approach, resistance to cephalosporins is a good example of how antibiotics play an important role in both animal and human health. The main concern with the use of antimicrobials used in animals for therapeutic or prophylactic purposes is the spread of AMR [40]. Fluoroquinolones used in food animals are associated with quinolone resistance in Salmonella strains. Resistance to carbapenemics has been observed in Salmonella strains due to routine administration of ceftiofur [47,48].
E. coli is an important pathogen that is a common cause of bacterial infections, such as enteritis and urinary tract and bloodstream infections. AMR is a rapidly growing problem associated with E. coli infections in animals and humans, and this problem is best documented in human infection isolates, particularly in developing countries [49,50].
Severe staphylococcal infections in communities and hospital environments are mainly caused by MRSA strains responsible for various infections (skin and wound infections and bacteremia, among others) [51]. S. aureus and other staphylococcal species also affect animals [52,53]. This bacterium causes mastitis in cattle and skin infections in pigs and pets. Pathogenic MRSA strains in humans have emerged in different animal species. It is transmitted to humans through close contact with animals that are carriers of these strains [54,55].
One Health approach to combat AMR
The One Health approach is fully integrated into global efforts to address the problem of AMR. Among the many obstacles to overcome are the competing interests of multiple economic sectors and organizations involved in animal, human, and environmental health. These actors need to agree on key priorities for action, the best ways to monitor AMR and control infections, and policies that should govern antimicrobial use. Key strategies for addressing AMR from the One Health approach are described:
Conduct a global public awareness campaign to educate our society about the harm caused by the overuse and misuse of antimicrobials. Implementing effective public campaigns can reduce the number of antimicrobials prescribed.
Improve and strengthen hygiene measures and prevent the spread of infections. By improving healthcare systems and living standards, we can significantly reduce the demand for antimicrobial and thus reduce the risk of the emergence of the new resistant strain.
Reduce the unnecessary use of antimicrobials in agriculture and their dissemination to the environment. Globally, the largest amounts of antimicrobials are consumed in agriculture and aquaculture. The use of antimicrobials as prophylaxis and growth promoters should be considered dangerous and unnecessary. Furthermore, it has been documented that animal excretes a significant percentage (75%–90%) of antimicrobials without being metabolized and dispersed into the environment.
Improve global surveillance of drug resistance. The medical and scientific community needs a clear understanding of current and historical data on AMR to clarify the new mechanisms of resistance acquisition, to know definitively current cases, and to predict future threats. To do so requires a better understanding of three areas: antibiotic consumption in humans and animals, current rates of antibiotic resistance, and a better understanding of the molecular basis of AMR.
Promote new and rapid clinical diagnoses. Misdiagnoses made in public or private hospitals lead to unnecessary antibiotic prescriptions. The development of rapid and accurate diagnostic tests will allow clinicians to administer antimicrobials to patients who need them.
Promote the development and use of vaccines and alternatives. The development of vaccines directed against antibiotic-resistant bacteria that cause serious infections will reduce the number of infected patients needing antimicrobial treatment. Additional investments are currently needed to develop new vaccines and alternatives to antimicrobials such as phage therapy, probiotics, antibodies, and lysins, among others.
Recognize and increase the number of people working with infectious diseases. Addressing AMR requires skilled professionals such as microbiologists, pharmacists, infectious disease specialists, nurses, infection control specialists, veterinarians, and epidemiologists. To do this, countries must invest in the training of this human resource.
A global innovation fund for early-stage research on new treatments. More public and private investments in drug discovery research are needed to develop new treatments. A global innovation fund is needed to support research that is not commercially attractive.
Create better incentives to promote investment in new drugs and in the improvement of existing drugs. The development of new antimicrobials is unattractive to pharmaceutical companies because there are still relatively effective antimicrobials on the market. It is difficult to predict exactly how and when AMR will develop, creating uncertainty for pharmaceutical companies when making business decisions.
Build a global coalition for real action against AMR. Global action is essential to make significant progress in the fight against AMR. Putting AMR on the international political agenda and addressing it using One Health approach is important to effect change [3].
Conclusion
To combat AMR, it is important to support a “One Health” approach (human, animal, plant, and environmental health). This requires accelerating global progress, innovating to secure the future, collaborating for more effective action, investing in sustainable response, and strengthening global governance and accountability. Most classes of antibiotics are available for use in humans and animals. AMR can be reduced when antimicrobials are used only as a treatment, rarely for prophylaxis, and never as growth promoters. Success will require strict and efficient control of the types and amounts of antimicrobials used in medical practice and monitoring and controlling the proliferation of resistant bacteria that spread to the environment.
Authors’ Contributions
CMAA: Suggested the concept of the study. MEVM: Drafted and critically revised the manuscript. MGL and BQC: Reviewed and revised the manuscript. All authors read and approved the final manuscript.
Acknowledgments
The authors thank the Mexican National Council on Science and Technology (CONACyT) for supporting this work [grant number: 290618].
Competing Interests
The authors declare that they have no competing interests.
References
- 1.World Health Organization. Antimicrobial Resistance:Global Report on Surveillance. 2014. [Retrieved on 13-03-2022]. WHO, https://apps.who.int/iris/handle/10665/112642 .
- 2.Laxminarayan R, Duse A, Wattal C, Zaidi A.K.M, Wertheim H.F.L, Sumpradit N, Vlieghe E, Hara G.L, Gould I.M, Goossens H, Greko C, So A.D, Bigdeli M, Tomson G, Woodhouse W, Ombaka E, Peralta A.Q, Qamar F.N, Mir F, Kariuki S, Bhutta Z.A, Coates A, Bergstrom R, Wright G.D, Brown E.D, Cars O. Antibiotic resistance—The need for global solutions. Lancet Infect Dis. 2013;13(12):1057–1098. doi: 10.1016/S1473-3099(13)70318-9. [DOI] [PubMed] [Google Scholar]
- 3.O'Neill J. Tackling drug-resistant infections globally:Final report and recommendations the review on antimicrobial resistance. 2016:10–84. [Google Scholar]
- 4.Collignon P, Beggs J.J, Walsh T.R, Gandra S, Laxminarayan R. Anthropological and socioeconomic factors contributing to global antimicrobial resistance:a univariate and multivariable analysis. Lancet Planet Heal. 2018;2(9):398–405. doi: 10.1016/S2542-5196(18)30186-4. [DOI] [PubMed] [Google Scholar]
- 5.Bürgmann H, Frigon D, Gaze W.H, Manaia C.M, Pruden A, Singer A.C, Smets B. F, Zhang T. Water and sanitation:an essential battlefront in the war on antimicrobial resistance. FEMS Microbiol Ecol. 2018;94(9):1–14. doi: 10.1093/femsec/fiy101. [DOI] [PubMed] [Google Scholar]
- 6.Collignon P.J, McEwen S.A. One Health—Its importance in helping to better control antimicrobial resistance. Trop Med Infect Dis. 2019;4(1):22. doi: 10.3390/tropicalmed4010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kimani T, Kiambi S, Eckford S, Njuguna J, Makonnen Y, Rugalema G, Morzaria S.P, Lubroth J, Fasina F.O. Expanding beyond zoonoses:the benefits of a national One Health coordination mechanism to address antimicrobial resistance and other shared health threats at the human-animal-environment interface in Kenya. Rev Sci Tech. 2019;38(1):155–171. doi: 10.20506/rst.38.1.2950. [DOI] [PubMed] [Google Scholar]
- 8.Shrestha K, Acharya K.P, Shrestha S. One Health:The interface between veterinary and human health. Int J One Health. 2018;4(1):8–14. [Google Scholar]
- 9.Centers for Disease Control and Prevention. One Health Basics. History. CDC Atlanta, GA. 2016. [Retrieved on 13-03-2022]. Available at: http://www.cdc.gov/onehealth/basics/history/index.html .
- 10.Schwabe C.W. Veterinary Medicine and Human Health. Baltimore, MD, USA: The Williams &Wilkins Company; 1964. [Google Scholar]
- 11.Wildlife Conservation Society. The Manhattan Principles. 2004. [Retrieved on 13-03-2022]. Available at: http://www.cdc.gov/onehealth/pdf/manhattan/twelve_manhattan_principles.pdf .
- 12.World Health Organization. Global action plan on antimicrobial resistance. Geneva: WHO; 2015. [Retrieved on 13-03-2022]. Available at: http://www.who.int/antimicrobial-resistance/publications/globalaction-plan/en/ [Google Scholar]
- 13.World Health Organization. Integrated surveillance of antimicrobial resistance in foodborne bacteria. Geneva: WHO; 2017. [Retrieved on 13-03-2022]. Available at: http://www.who.int/foodsafety/publications/agisar_guidance2017/en/ [Google Scholar]
- 14.Magouras I, Carmo L.P, Stärk K.D, Schüpbach-Regula G. Antimicrobial usage and resistance in livestock:where should we focus? Front Vet Sci. 2017;15(4):148. doi: 10.3389/fvets.2017.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Queenan K, Häsler B, Rushton J.A. One Health approach to antimicrobial resistance surveillance:is there a business case for it? Int J Antimicrob Agents. 2016;48(4):422–427. doi: 10.1016/j.ijantimicag.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Jans C, Sarno E, Collineau L, Meile L, Stärk K.D.C, Stephan R. Consumer exposure to antimicrobial-resistant bacteria from food at Swiss retail level. Front Microbiol. 2018;6(9):362. doi: 10.3389/fmicb.2018.00362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Food and Agriculture Organization (FAO) Antimicrobial resistance and foods of plant origin summary report of an FAO meeting of experts FAO antimicrobial resistance working group. 2018. Available at: www.fao.org/antimicrobial-resistance .
- 18.Food and Agriculture Organization (FAO) Drivers, dynamics and epidemiology of antimicrobial resistance in animal or production. 2016. Available at: http://www.fao.org/3/a-i6209e.pdf .
- 19.Van Boeckel T.P, Brower C, Gilbert M, Grenfell B.T, Levin S.A, Robinson T.P, Teillant A, Laxminarayan R. Global trends in antimicrobial use in food animals. Proc Natl Acad Sci. 2015;112(18):5649–5654. doi: 10.1073/pnas.1503141112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sundin G.W, Wang N. Antibiotic resistance in plant-pathogenic bacteria. Annu Rev Phytopathol. 2018;56(1):161–180. doi: 10.1146/annurev-phyto-080417-045946. [DOI] [PubMed] [Google Scholar]
- 21.Watts J.E, Schreier H.J, Lanska L, Hale M.S. The rising tide of antimicrobial resistance in aquaculture:Sources, sinks and solutions. Mar Drugs. 2017;15(6):158. doi: 10.3390/md15060158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehdi Y, Létourneau-Montminy M.P, Gaucher M.L, Chorfi Y, Suresh G, Rouissi T, Brar S.K, Côté C, Ramirez A.A, Godbout S. Use of antibiotics in broiler production:global impacts and alternatives. Anim Nutr. 2018;4(2):170–178. doi: 10.1016/j.aninu.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Falagas M.E, Kasiakou S.K. Toxicity of polymyxins:A systematic review of the evidence from old and recent studies. Crit Care. 2006;10(1):1–13. doi: 10.1186/cc3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fernandes M.R, Moura Q, Sartori L, Silva K.C, Cunha M.P, Esposito F, Lopes R, Otutumi L.K, Gonçalves D.D, Dropa M, Matté M.H, Monte D.F, Landgraf M, Francisco G.R, Bueno M.F, de Oliveira-Garcia D, Knöbl T, Moreno A.M, Lincopan N. Silent dissemination of colistin-resistant Escherichia coli in South America could contribute to the global spread of the mcr-1 gene. Euro Surveill. 2016;21(17):30214. doi: 10.2807/1560-7917.ES.2016.21.17.30214. [DOI] [PubMed] [Google Scholar]
- 25.Karaaslan A, Çağan E, Kepenekli K.E, Atıcı S, Akkoç G, Yakut N, Demir S.Ö, Soysal A, Bakır M. Intravenous colistin use for multidrug-resistant Gram-negative infections in pediatric patients. Balkan Med J. 2016;33(6):627–632. doi: 10.5152/balkanmedj.2016.16210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wi Y.M, Choi J.Y, Lee J.Y, Kang C.I, Chung D.R, Peck K.R, Song J.H, Ko K.S. Emergence of colistin resistance in Pseudomonas aeruginosa ST235 clone in South Korea. Int J Antimicrob Agents. 2017;49(6):767–769. doi: 10.1016/j.ijantimicag.2017.01.023. [DOI] [PubMed] [Google Scholar]
- 27.Liu Y.Y, Wang Y, Walsh T.R, Yi L.X, Zhang R, Spencer J, Doi Y, Tian G, Dong B, Huang X, Yu L.F, Gu D, Ren H, Chen X, Lv L, He D, Zhou K, Liang Z, Liu J.H, Shen J. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China:A microbiological and molecular biological study. Lancet Infect Dis. 2016;16(2):161–168. doi: 10.1016/S1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- 28.European Medicines Agency (2019) European Surveillance of Veterinary Antimicrobial Consumption. 'Sales of veterinary antimicrobial agents in 31 European countries in 2017'. (EMA/294674/2019) [Google Scholar]
- 29.Wang R, van Dorp L, Shaw L.P, Bradley P, Wang Q, Wang X, Jin L, Zhang Q, Liu Y, Rieux A, Dorai-Schneiders T, Weinert L.A, Iqbal Z, Didelot X, Wang H, Balloux F. The global distribution and spread of the mobilized colistin resistance gene mcr-1. Nat Commun. 2018;9(1):1179. doi: 10.1038/s41467-018-03205-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Irrgang A, Roschanski N, Tenhagen B.A, Grobbel M, Skladnikiewicz-Ziemer T, Thomas K, Roesler U, Käsbohrer A. Prevalence of mcr-1 in E. coli from livestock and food in Germany, 2010–2015. PLoS ONE. 2016;11(7):1–10. doi: 10.1371/journal.pone.0159863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bager F, Madsen M, Christensen J, Aarestrup F.M. Avoparcin used as a growth promoter is associated with the occurrence of vancomycin-resistant Enterococcus faecium on Danish poultry and pig farms. Prev Vet Med. 1997;31(1):95–112. doi: 10.1016/s0167-5877(96)01119-1. [DOI] [PubMed] [Google Scholar]
- 32.Rybak M.J, Le J, Lodise T.P, Levine D.P, Bradley J.S, Liu C, Mueller B.A, Pai M.P, Wong-Beringer A, Rotschafer J.C, Rodvold K.A, Maples H.D, Lomaestro B.M. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections:a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am J Health-Syst Pharm. 2020;77(11):835–864. doi: 10.1093/ajhp/zxaa036. [DOI] [PubMed] [Google Scholar]
- 33.Temkin E, Fallach N, Almagor J, Gladstone B.P, Taconelli E, Carmeli Y. Estimating the number of infections caused by antibiotic-resistant Escherichia coli and Klebsiella pneumoniae in 2014:a modelling study. Lancet Glob Health. 2018;6(9):969–979. doi: 10.1016/S2214-109X(18)30278-X. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization (2017). Advisory Group on Integrated Surveillance of Antimicrobial Resistance (AGISAR) Critically Important Antimicrobials for Human Medicine, 5th revision. WHO, Geneva. [Retrieved on 13-03-2022]. Available at: http://who.int/foodsafety/publications/antimicrobials-fifth/en/
- 35.Gibbons J.F, Boland F, Egan J, Fanning S, Markey B.K, Leonard F.C. Antimicrobial resistance of faecal Escherichia coli isolates from pig farms with different durations of in-feed antimicrobial use. Zoonoses Public Health. 2016;63(3):241–250. doi: 10.1111/zph.12225. [DOI] [PubMed] [Google Scholar]
- 36.Food and Drug Administration (FDA). Summary report on antimicrobials sold or distributed for use in food-producing animals. FDA, Department of Health and Human Services. Washington, DC. 2018 [Google Scholar]
- 37.Madec J.Y, Haenni M, Nordmann P, Poirel L. Extended-spectrum b-lactamase/AmpC- and carbapenemase-producing Enterobacteriaceae in animals:a threat for humans? Clin Microbiol Infect. 2017;23(11):826–833. doi: 10.1016/j.cmi.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 38.Mughini-Gras L, Dorado-García A, van Duijkeren E, van den Bunt G, Dierikx C.M, Bonten M.J.M, Bootsma M.C.J, Schmitt H, Hald T, Evers E.G, de Koeijer A, van Pelt W, Franz E, Mevius D.J, Heederik D.J.J. Attributable sources of community-acquired carriage of Escherichia coli containing b-lactam antibiotic resistance genes:a population-based modelling study. Lancet Planet Health. 2019;3(8):357–369. doi: 10.1016/S2542-5196(19)30130-5. [DOI] [PubMed] [Google Scholar]
- 39.Lee S, Teng L, DiLorenzo N, Weppelmann T.A, Jeong K.C. Prevalence and molecular characteristics of extended-spectrum and AmpC b-Lactamase producing Escherichia coli in grazing beef cattle. Front Microbiol. 2020;10:3076. doi: 10.3389/fmicb.2019.03076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saraiva M, Filho A, Neto O, Silva N.M.V, Givisiez P.E.N, Gebreyes W.A, Oliveira C.J.B. Off-label use of ceftiofur in one-day chicks triggers a short-term increase of ESBL producing E. coli in the gut. PLoS ONE. 2018;13(9):1–9. doi: 10.1371/journal.pone.0203158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carson C, Li Z.X, Agunos A, Loest D, Chapman B, Finley R, Mehrotra M, Sherk L.M, Gaumond R, Irwin R. Ceftiofur-resistant Salmonella enterica serovar Heidelberg of poultry origin –a risk profile using the Codex framework. Epidemiol Infect. 2019;147:1–20. doi: 10.1017/S0950268819001778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dutil L, Irwin RJ, Finley R, Ng LK, Avery BP, Boerlin P, Bourgault A.M, Cole L, Daignault D, Desruisseau A, Demczuk W, Hoang L, Horsman G.B, Ismail J, Jamieson F, Maki A, Pacagnella A, Pillai D.R. Ceftiofur resistance in Salmonella enterica serovar Heidelberg from chicken meat and humans, Canada. Emerg Infect Dis. 2010;16(1):48–54. doi: 10.3201/eid1601.090729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hooper D.C, Jacoby G.A. Mechanisms of drug resistance:quinolone resistance. Ann Y Acad Sci. 2015;1354(1):12–31. doi: 10.1111/nyas.12830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nelson J.M, Chiller T.M, Powers J.H, Angulo F.J. Fluoroquinolone resistant Campylobacter species and the withdrawal of fluoroquinolones from use in poultry:a public health success story. Clin Infect Dis. 2007;44(7):977–980. doi: 10.1086/512369. [DOI] [PubMed] [Google Scholar]
- 45.Abraham S, Sahibzada S, Hewson K, Laird T, Abraham R, Pavic A, Truswell A, Lee T, O'Dea M, Jordan D. Emergence of fluoroquinolone-resistant Campylobacter jejuni and Campylobacter coli among Australian chickens in the absence of fluoroquinolone use. Appl Environ Microbiol. 2020;86(8):1–11. doi: 10.1128/AEM.02765-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sharma C, Rokana N, Chandra M, Singh B.P, Gulhane R.D, Gill J.P.S, Ray P, Puniya A.K, Panwar H. Antimicrobial resistance:Its surveillance, impact, and alternative management strategies in dairy animals. Front Vet Sci. 2018;4(237):1–27. doi: 10.3389/fvets.2017.00237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cui M, Zhang P, Li J, Sun C, Song L, Zhang C, Zhao Q, Wu C. Prevalence and characterization of fluoroquinolone-resistant Salmonella isolated from an integrated broiler chicken supply chain. Front Microbiol. 2019;10(1865):1–8. doi: 10.3389/fmicb.2019.01865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mollenkopf D.F, Stull J.W, Mathys D.A, Bowman A.S, Feicht S.M, Grooters S.V, Daniels J.B, Wittum T.E. Carbapenemase-producing Enterobacteriaceae recovered from the environment of a swine farrow-to-finish operation in the United States. Antimicrob Agents Chemother. 2017;61(2):1–9. doi: 10.1128/AAC.01298-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guzmán M, Salazar E, Cordero V, Castro A, Villanueva A, Rodulfo H, De Donato M. Multidrug resistance and risk factors associated with community-acquired urinary tract infections caused by Escherichia coli in Venezuela. Biomedica. 2019;39(1):96–107. doi: 10.7705/biomedica.v39i2.4030. [DOI] [PubMed] [Google Scholar]
- 50.Uzodi A.S, Lohse C.M, Banerjee R. Risk factors for and outcomes of multidrug-resistant Escherichia coli infections in children. Infect Dis Ther. 2017;6(2):245–257. doi: 10.1007/s40121-017-0152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hassoun A, Linden K.P, Friedman B. Incidence, prevalence, and management of MRSA bacteremia across patient populations—a review of recent developments in MRSA management and treatment. Crit Care. 2017;21(1):1–10. doi: 10.1186/s13054-017-1801-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oreiby A, Khalifa H, Eid A, Ahmed A, Shimamoto T, Shimamoto T. Clinical and molecular characterization of both methicillin-resistant and sensitive Staphylococcus aureus mastitis. J. Hellenic Vet Med Soc. 2019;70(3):1743–1748. [Google Scholar]
- 53.Reddy B.S, Kumari K.N, Sivajothi S. Methicillin-resistant Staphylococcus aureus (MRSA) isolated from dogs with recurrent pyoderma. J Dairy Vet Anim Res. 2016;3(2):62–65. [Google Scholar]
- 54.Bernier-Lachance J, Arsenault J, Usongo V, Parent E, Labrie J, Jacques M, Malouin F, Archambault M. Prevalence and characteristics of livestock-associated methicillin-resistant Staphylococcus aureus (LA-MRSA) isolated from chicken meat in the province of Quebec, Canada. PLoS ONE. 2020;15(1):1–19. doi: 10.1371/journal.pone.0227183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kinross P, Petersen A, Skov R, van Hauwermeiren E, Pantosti A, Laurent F, Voss A, Kluytmans J, Struelens M.J, Heuer O, Monnet D.L. Livestock-associated methicillin-resistant Staphylococcus aureus (MRSA) among human MRSA isolates, European Union/European Economic Area countries, 2013. Euro Surveill. 2017;22(44):1–13. doi: 10.2807/1560-7917.ES.2017.22.44.16-00696. [DOI] [PMC free article] [PubMed] [Google Scholar]


